Abstract
Magnetic resonance imaging (MRI) is an extremely useful tool for the detection and characterization of numerous pathologic processes. Although patients can benefit from the use of MRI, claustrophobia is a major issue in some cases. This fear alone can lead to cancellation of the scanning procedure in some cases and the need for conscious sedation in others. Patient anxiety during the scan can also lead to increased motion-related artifacts on the images with associated degradation of the diagnostic quality of the study. To alleviate these problems, our team developed a virtual reality (VR) tool (app) to educate patients about MRI and simulate the experience of actually being scanned. The app is totally immersive and incorporates both the visual and auditory sensations that patients encounter during an MRI scan. Patients also learn about potential conditions and implanted devices that may preclude the safe performance of the examination. This VR tool not only educates patients about MRI and its importance in their care, but also allows them to virtually experience what it is like to have a MRI scan. This technology has the potential to decrease both claustrophobic cancellations and patient anxiety before a MRI scan.
Keywords: virtual MRI, virtual reality MRI, MRI patient preparation, VR apps in medicine, MRI claustrophobia
Introduction
We reviewed the data on claustrophobia in our adult patient population that had undergone magnetic resonance imaging (MRI) scans performed and assessed the need for conscious sedation in patients undergoing MRI studies. At our institution, the scanning procedure of ∼1.6% patients has been terminated prematurely owing to patients complaining of claustrophobia and/or discomfort, and a significant proportion of patients require conscious sedation to undergo the scanning procedure. Others have reported similar findings of claustrophobic cancellations and the need for nurse-assisted conscious sedation in patients undergoing MRI scans, with a range from 3.8% at our center to 14.3% in the literature (1–5). We realized there was an opportunity to improve care by making our patients aware of what the procedure is like in advance of the study. There have been many studies showing that desensitization therapy using virtual reality (VR) as a tool is an effective means of treating phobias (6–10). Our team designed a tool that can be used by patients before undergoing an MRI scanning. The goal was to determine if we can apply the same desensitization techniques used to treat other phobias with VR to patients undergoing MRI scanning. We assembled a team of expert programmers, digital video artists, and physicians to design the tool to educate patients about the risks and benefits of MRI and also to let them experience what it is like to be inside the scanner. Using state-of-the-art techniques, the application (app) was made versatile enough to use with either a dedicated VR device or as a downloadable app that can be powered by a standard smart phone worn on an inexpensive headset such as Google Cardboard or any other similar type of device (Figure 1).
Figure 1.

The virtual reality (VR) magnetic resonance imaging (MRI) app is downloaded to a smart phone and placed in any of a variety of low-cost headsets. This makes the app easy to distribute and deploy.
Methodology
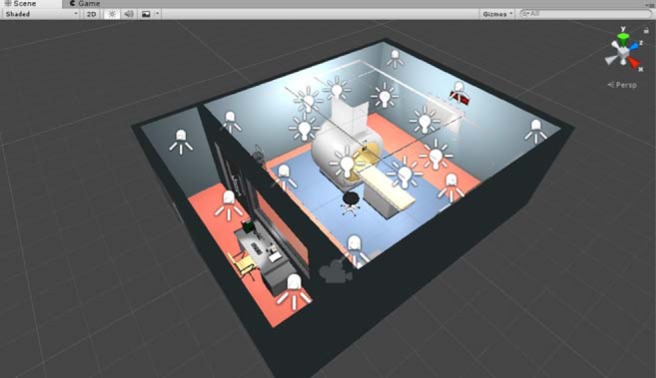
To create a realistic virtual MRI experience, our team needed to model the magnetic resonance (MR) unit and also the environment around the scanner. This included the scanning table and the room where the scanning takes place. Our development process began by acquiring 3D models of MRI machines used in practice. These data were used to create the virtual MR machine. The room size dimensions were modeled in-house by 3D artists. From these models, an entire VR environment was constructed using the Unity game engine (Figure 2).
Figure 2.

The programmers and 3D artists were able to create a virtual scanning environment using the actual dimensions of the scanner and scanning table. The programming was performed using the Unity game engine.
Owing to the claustrophobic nature of an MRI machine, it was important to get an accurate proximity of the patient experiencing the simulation to the walls of the MRI machine's bore. This involves simulating a virtual camera in a fully 3D scene. Some methods, like 360 video, which rely on filming real-world environments, create too much distortion for the space to feel accurate. With 360 video, objects that are filmed close to the 360 camera can appear enormous and with severe warping. To create a more realistic experience in the app, our team used a 3D environment with virtual cameras placed in the 3D space. This functions more like a 3D game environment, allowing us to simulate the experience more closely to what a patient would experience in real life (Figure 3).
Figure 3.
To create a more realistic experience in the app, our team used a 3D environment with virtual cameras placed in the 3D space. This functioned more like a 3D game environment, allowing us to simulate the experience more closely to what a patient would experience in real life. A 360 video capture can create too much distortion for the space to feel accurate for the user.
The team's overall objective was to create as realistic of a simulation of the MRI patient experience as possible. To accomplish this goal, we needed to capture sounds that a patient would hear while being scanned. Our development team recorded the sounds within the actual scanner. The sounds that play throughout the simulation were recorded on-site from a real MRI machine and then placed in the VR scene to create a spatial audio. The scene was then programmed to move the patient into the bore of the MRI machine when the gyroscope in the mobile device recognizes the patient is in a lying position. The simulation then waits a designated amount of time inside the bore, before easing the patient out of the scanner. In the programming process, virtual cameras are placed where the subject's eyes would be in the 3D scene, with parameters for adjusting focal length used to eliminate any distortion (Figure 4). While the duration of the simulation is only a fraction of the time a real MRI would take, we anticipate that the experience provided may be sufficient to expose patients to the claustrophobic feeling of a real MRI machine with the goal of reducing anxiety. Patients may also decide to interact with the simulation multiple times to become further desensitized to a fear of the scanning procedure.
Figure 4.
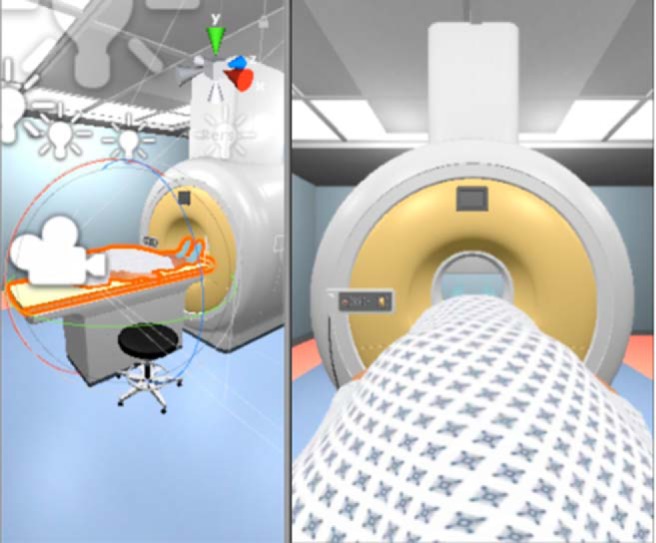
Virtual cameras were placed where the subject's eyes would be in the 3D scene, with parameters for adjusting focal length used to eliminate any distortion. The image on the left shows the placement of the virtual cameras, and the image on the right is what the patient would see with the cameras at that angle.
Results and Discussion
Although clinicians may view MRI as harmless, many patients report anxiety about the procedure and experience claustrophobia because of the confining nature of the gantries. Brennan et al. asked adult patients to rate their anxiety following completion of an MRI scan, and (35%) reported feeling anxious, as opposed to relaxed, during the scan. They noted, “50% experienced anxiety upon being positioned within the bore of the imaging machine. The most frequent sources of distress were the inability to move (65%), the length of the procedure (61%), the size of the scanner ‘tunnel’ (48%), and the feeling of being closed in (44%)” (10). The group at the University of Vienna conducted a study to determine the effect of prescan anxiety and motion artifacts on subsequent MRI scans (11). Although general anxiety alone did not appear to increase the probability of motion artifacts on MRI, patients who stated that they were “worried” about the “technical apparatus” had significantly increased motion-related artifacts that impaired diagnosis, 11.5% as compared with 3.2% in the group that did not express concern about the scanner. A meta-analysis reported in Radiography in 2015 noted that, “the rate of claustrophobic reactions, either as refusal to undertake the scan, or early scan termination due to a claustrophobic event, ranged from 0.46% to 5.29%” (12). Educational interventions such as video demonstrations and telephone interviews before MRI have been shown to be effective methods to reduce patient anxiety (13).
Sedation can also be used in conjunction with an MRI examination, but this procedure is not without risk. For example, a study published in the British Journal of Anesthesia reported a 2.9% hypoxemia rate in children needing sedation for computed tomography or MRI (14). The same article noted that there was excessive motion on 12% of sedated patients. In the current state, patients with the potential for claustrophobia are heterogeneously identified by the ordering providers and are given oral sedatives. In patients with a likelihood for severe claustrophobia, their MRI appointment is scheduled with nurse-monitored intravenous conscious sedation. However, it is common for patients with claustrophobia to not be identified in advance, resulting in diagnostic and scheduling errors that have an impact on clinical care and patient satisfaction.
At our institution, ∼1.6% of patients have studies terminated prematurely owing to the complaint of claustrophobia, and/or discomfort, and a significant proportion of patients—3.8%—required nurse-supervised conscious sedation to undergo the study procedure. Other studies have reported similar findings of claustrophobic cancellations and the need for nurse-assisted conscious sedation in patients undergoing MRI scanning (1–5). Sedation increases both the risk and the cost of the procedure. While patient anxiety can also negatively affect the overall image quality, it remains unclear if sedation can improve the image quality through decreased motion.
Conclusion
There have been many studies showing that desensitization therapy using VR as a tool is an effective means of treating phobias (6–10). There clearly is an opportunity to improve care by making our patients aware of what to expect during the procedure in advance of actually having the scan. Although we will make this tool available to patients as a downloadable app for educational purposes, we anticipate that it will be the most effective if the device is made available for use at key referral clinics and at our MRI facilities. We plan to identify patients that previously needed conscious sedation or those who express concerns about claustrophobia. Patients will be offered the use of the VR app during their clinic visit or at our center before their MRI scanning appointment. Claustrophobic cancellations negatively affect MRI facilities owing to the associated lost revenue. In addition, claustrophobic patients who are scanned often have image degradation owing to motion impairing the diagnostic quality of the study. For these reasons, our goal was to develop a novel app to educate patients about MRI and to use VR as a desensitization tool in patients who have anxiety related to the procedure. If the tool proves effective at decreasing claustrophobic cancellations, it will provide a significant value proposition to MRI centers. A clinical trial is currently being planned to determine the effectiveness of the VR app in decreasing anxiety, claustrophobic cancellations, and the need for conscious sedation.
Acknowledgments
We wish to thank Ruti Volk who leads the Patient Education and Health Literacy Program at the University of Michigan for her advice and guidance. We also want to acknowledge Sara Eskandari and Thomas Bartlett for their development work, and Matias Vilaplana for his contribution to the sound production. This project was funded by a University of Michigan PEAC Grant.
Disclosures: No disclosures to report.
Conflict of Interest: The authors have no conflict of interest to declare.
Footnotes
- MRI
- Magnetic resonance imaging
- VR
- virtual reality
- MR
- magnetic resonance
References
- 1. Murphy KJ, Brunberg JA. Adult claustrophobia, anxiety and sedation in MRI. Magn Reson Imaging. 1997;15:51–54. [DOI] [PubMed] [Google Scholar]
- 2. Thorpe S, Salkovskis PM, Dittner A. Claustrophobia in MRI: the role of cognitions. Magn Reson Imaging. 2008;26:1081–1088. [DOI] [PubMed] [Google Scholar]
- 3. Meléndez JC, McCrank E. Anxiety-Related Reactions Associated With Magnetic Resonance Imaging Examinations. JAMA. 1993;270:745–747. [DOI] [PubMed] [Google Scholar]
- 4. Sarji SA, Abdullah BJ, Kumar G, Tan AH, Narayanan P. Failed magnetic resonance imaging examinations due to claustrophobia. Australas Radiol. 1998;42:293–295. [DOI] [PubMed] [Google Scholar]
- 5. Dewey M, Schink T, Dewey CF. Claustrophobia during magnetic resonance imaging: cohort study in over 55,000 patients. J Magn Reson Imaging. 2007;26:1322–1327. [DOI] [PubMed] [Google Scholar]
- 6. Rothbaum BO, Hodges LF, Kooper R, Opdyke D, Williford JS, North M. Effectiveness of computer-generated (virtual reality) graded exposure in the treatment of acrophobia. Am J Psychiatry. 1995;152:626–628. [DOI] [PubMed] [Google Scholar]
- 7. Parsons TD, Rizzo AA. Affective outcomes of virtual reality exposure therapy for anxiety and specific phobias: a meta-analysis. J Behav Ther Exp Psychiatry. 2008;39:250–261. [DOI] [PubMed] [Google Scholar]
- 8. Morina N, Ijntema H, Meyerbröker K, Emmelkamp PM. Can virtual reality exposure therapy gains be generalized to real-life? A meta-analysis of studies applying behavioral assessments. Behav Res Ther. 2015;74:18–24. [DOI] [PubMed] [Google Scholar]
- 9. Price M, Mehta N, Tone EB, Anderson PL. Does engagement with exposure yield better outcomes? Components of presence as a predictor of treatment response for virtual reality exposure therapy for social phobia. J Anxiety Disord. 2011;25:763–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brennan SC, Redd WH, Jacobsen PB, Schorr O, Heelan RT, Sze GK, Krol G, Peters BE, Morrissey JK. Anxiety and panic during magnetic resonance scans. Lancet. 1988;2:512. [DOI] [PubMed] [Google Scholar]
- 11. Dantendorfer K, Amering M, Bankier A, Helbich T, Prayer D, Youssefzadeh S, Alexandrowicz R, Imhof H, Katschnig H. A study of the effects of patient anxiety, perceptions and equipment on motion artifacts in magnetic resonance imaging. Magn Reson Imaging. 1997;15:301–306. [DOI] [PubMed] [Google Scholar]
- 12. Munn Z, Moola S, Lisy M, Riitano D, Murphy F. Claustrophobia in magnetic resonance imaging: a systematic review and meta-analysis. Radiography. 2015;21:e59–e63. [Google Scholar]
- 13. Tugwell JR, Goulden N, Mullins P. Alleviating anxiety in patients prior to MRI: a pilot single-centre single-blinded randomised controlled trial to compare video demonstration or telephone conversation with a radiographer versus routine intervention. Radiography. 2018;24:122–129. [DOI] [PubMed] [Google Scholar]
- 14. Malviya S. Voepel-Lewis T, Edevik OP, Rockwell DT, Wong JH, Tait AR. Sedation and general anaesthesia in children undergoing MRI and CT: adverse events and outcomes. Br J Anaesth. 2000;84:743–748. [DOI] [PubMed] [Google Scholar]


