Using a standardized metric on a well-characterized sample, we document high, sustained levels of pathological grief in mothers after SIDS and identify potential screening targets.
Abstract
Video Abstract
BACKGROUND:
The loss of a child is associated with elevated grief severity, and sudden infant death syndrome (SIDS) is the leading cause of postneonatal mortality in the United States. The diagnosis of prolonged grief disorder (PGD) has gained broader acceptance and use. Little is known about PGD in mothers after SIDS.
METHODS:
Between May 2013 and July 2016, we assessed 49 SIDS-bereaved mothers living in informal settlements near Cape Town, South Africa, and on the Pine Ridge Indian Reservation and 359 SIDS-bereaved mothers affiliated with SIDS parent-support organizations in the United States, United Kingdom, Australia, New Zealand, and the Netherlands. We examined PGD symptom severity and diagnostic prevalence rates between the samples and other significant grief indicators during the period 2 to 48 months after the deaths of their infants.
RESULTS:
Extremely high, persistent, and similar rates of PGD were found in both samples at every time interval. The prevalence of PGD was 50.0% in either sample (mean months from loss: 20.5 vs 24.9). Daily, intrusive emotional pain or yearning was found in 68.1% of subjects; yearning was significantly associated with emotional pain (P < .0001). Role confusion and anger were the most prevalent symptoms, reported by the majority at every time interval. Rates of role confusion, anger, and diminished trust in others remained constant. Acceptance was less prevalent than other grief indicators at every interval.
CONCLUSIONS:
Severe symptoms and heightened risk for PGD was seen in mothers after their infants died of SIDS, with discernible symptom profiles. Given their involvement with families after SIDS, pediatricians may have a unique role in identifying this problem and helping address its consequences.
What’s Known on This Subject:
The death of a child is associated with high levels of grief in the child’s parents. Prolonged grief disorder affects health and well-being and may influence the lives of remaining and subsequent children in a family.
What This Study Adds:
Half of the mothers suffered from prolonged grief disorder in the 4 years after their infants’ deaths from SIDS, with daily, intrusive emotional pain or yearning in 68.1%. Their specific grief-related symptoms may be potential targets for screening and referral.
Sudden infant death syndrome (SIDS) continues to be a prevalent cause of infant mortality. This category of infant death has a crude mortality rate of 0.9 in 1000 live births1 and is the leading cause of postneonatal mortality in infants 28 to 364 days of life in the United States. Lacking preparation or warning, a seemingly healthy infant is discovered dead without apparent cause. Pediatricians make significant contributions to the prevention of SIDS.2 They are also closely involved in the unfortunate cases when SIDS does occur, with a unique perspective on the burdens to parents and their young families in its aftermath. Consequently, pediatric researchers have historically conducted research on the psychological consequences of SIDS and its ongoing impact on the family after this loss.3–10
Grief is the emotional response to the death of a loved one. It is a normal consequence of profound interpersonal loss yet involves extreme cognitive and emotional symptoms in most bereaved individuals.11 A significant minority of bereaved individuals experience a more enduring grief response that exceeds social norms and causes impairment in daily functioning. Prolonged grief disorder (PGD), formerly called complicated grief and alternately called persistent complex bereavement disorder,12 is diagnosed as a pathologic response at the extreme of grief and is distinct from posttraumatic stress disorder or depression.13 PGD involves the persistence of separation distress, characterized by significant emotional pain and yearning in addition to cognitive, emotional, and behavioral symptoms >6 months after a significant loss.14 A recent meta-analysis found PGD in 9.8% of bereaved persons 1 year after loss.15 PGD has been documented in populations worldwide.16–18 It is associated with diminished health and quality of life.14 PGD criteria are included as an appendix in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition under persistent complex bereavement disorder12 and will be included in the International Classification of Diseases, 11th Revision.19
The experience of grief is unique to each loss, but certain factors predict more significant grief-related morbidity. Grief may be understood as an attachment response, and close kinship is a significant risk factor.20 The bond between a parent and a young, dependent child is the prototypical attachment bond,21 and the death of a child has been shown to cause extreme and long-lasting grief in parents.22–24 Mothers in particular are at risk for especially severe grief.25–27 Other risk factors for more difficult grief include sudden death,28 a lack of preparation,29 and the death of a dependent, younger child30 as well as poverty and previous losses.31 These risk factors for more severe grief are also specific aspects of a SIDS death and risk factors for SIDS. Researchers who study parents whose infants died of SIDS describe a difficult experience during bereavement32 with a lasting, often unrecognized, impact on the parents’ daily lives.33
Hypothesizing that a SIDS death would predict a severe grief response, here we investigate the prevalence and symptom presentation of PGD in mothers whose infants died of SIDS. We studied grief in 2 cross-sectional samples of mothers whose infants had died of SIDS in the previous 2 to 48 months, examining rates of PGD in settings with different degrees of socially determined risk based on poverty, education, and other factors. We investigated correlates of PGD and other grief indicators in the combined, heterogeneous sample of bereaved mothers to understand their grief-related symptoms.
Methods
Subjects were recruited through 2 sampling methods. Subjects in the Prenatal Alcohol in SIDS and Stillbirth (PASS) Research Network sample were women enrolled in the PASS Research Network, which is a study of women at high risk for stillbirth and infant loss from Cape Town, South Africa, and the northern Great Plains of the United States that is funded by the National Institute on Alcohol Abuse and Alcoholism and the Eunice Kennedy Shriver National Institute of Child Health and Human Development.34 The women were enrolled when their infants died of SIDS between May 2013 and July 2016. Surveys were administered by professional project staff. Bereaved mothers in the International Society for the Study and Prevention of Perinatal and Infant Death (ISPID) sample were recruited from mailing lists of parent organizations affiliated with ISPID. ISPID recruitment began in September 2014 and was completed in July 2016. ISPID enrollment was by response to notices on Web sites or in newsletters, and surveys were completed online. Potential participation in the ISPID sample was estimated to be 1600 based on mailing list estimates.
Measures
For a PGD scale, we used the Parental Bereavement Questionnaire (PBQ), which is a modification of the Prolonged Grief Disorder 13-Item Scale (PG-13)35 that has been adapted for language specific to the loss of an infant. The PBQ, like the PG-13, is used to assess diagnostic criteria for PGD by using items scaled from 1 to 5 for the frequency or degree of a symptom, with 1 indicating the absence of a symptom and 5 indicating experiencing the symptom almost always or to an overwhelming extent. Constituent symptoms of separation distress (yearning and emotional pain), and cognitive, emotional, and behavioral symptoms were surveyed, including confusion about one’s role in life or diminished sense of self, difficulty accepting the loss, avoidance of reminders about the reality of the loss, inability to trust others since the loss, difficulty moving on with life (eg, making new friends and pursuing interests), emotional numbness since the loss, and feeling stunned, dazed, or shocked by the loss. The source PG-13 items were found to have a sensitivity of 1.00 and specificity of 0.99 for PGD.14 Adaptations incorporating parent-specific language into the PG-13 were pilot tested on a sample of parents in Massachusetts,36 and input from local focus groups was used to increase reliability for local language preferences specific to Cape Town. Additional items used to assess indicators of disbelief, yearning, anger, isolation, depression, and acceptance as well as salient demographic and comorbidity data were also included. When multiple surveys were administered over time because of other components of the research protocol, the earliest response at >6 months from the loss was used. This research was approved by institutional review boards at Dana-Farber Cancer Institute (protocol 13-207); at the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Maryland; at Stellenbosch University in Stellenbosch, South Africa; at Sanford Health in Sioux Falls, South Dakota; and of the Oglala Sioux Tribe.
Statistical Analysis
Material deprivation in South African participants was estimated by using the South African upper-bound poverty line,37 an estimated income level below which the purchase of food and daily essentials puts a household in jeopardy of not meeting the daily minimum energy intake of 2100 kcal (R753 [South African rands] or $57 [US dollars] per month). Material deprivation in ISPID and northern Great Plains participants was determined by an inability to financially meet monthly obligations for necessities and US poverty income levels.
Point prevalence for PGD by using established criteria14 was determined in 6-month groupings, and 95% confidence intervals (CIs) were calculated. To compare samples, logistic regressions were used to model interactions between the sample and time for specific symptoms and PGD, and then we investigated the effect of sample and controlled for time. In an analysis of the combined samples, we examined correlations between the intensity of emotional pain and the intensity of yearning, plotted them on a heat graph, and tested by logistic regression using yearning as the outcome and pain as the predictor. Point prevalences of the cognitive, emotional, and behavioral symptoms of PGD were calculated at 6-month time groupings. Point prevalences for grief indicators of disbelief, yearning, anger, depression, and acceptance (considered to be the stages of grief)38 were calculated at 6-month time groupings.
Results
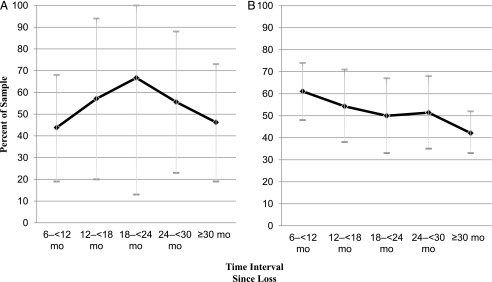
Demographic data and risk factors for PGD in the samples are presented in Table 1. The PASS enrollment included 49 bereaved mothers. Five mothers were lost to follow-up. The sample was largely not white (94% were predominantly multiracial Cape Coloured; n = 39) and poor (73% were in jeopardy of malnourishment), and 10% of participants had an education beyond high school. Approximately 40% had experienced a previous stillbirth or another child loss. PGD symptom criteria were found in 49.0% of the sample, and its prevalence exceeded 43.8% at every time interval (Fig 1). The ISPID sample included 372 participants, but 65 were excluded because the time since the loss was outside study criteria. The ISPID sample was largely white, better educated, and more materially secure. Approximately 35% had experienced a previous child or pregnancy loss. PGD symptom criteria were found in 42.3% of the ISPID sample, and its prevalence exceeded 41.3% at every time interval. In both samples, the rate of PGD was 50.0% when mothers with deaths that occurred more recently than 6 months, and thus by definition without PGD, were excluded (mean months from loss: PASS = 20.5, SD = 11.2, minimum = 6, maximum = 45; ISPID = 24.9, SD = 12.8, minimum = 6, maximum = 48). Internal consistency of the PBQ was α = .92 (n = 356).
TABLE 1.
Key Demographic Features of the Samples
| PASS Mothers | PASS Mothers With PGD | ISPID Mothers | ISPID Mothers With PGD | Total With PGD | |
|---|---|---|---|---|---|
| No. (%) | 49 | 24 (49.0) | 307 | 130 (42.3) | 154 (43.3) |
| Age at loss, y, mean | 26.1 | 26.7 | 24.7 | 24.0 | 24.4 |
| White race, % | 6.0 | 0 | 93.0 | 88.2 | 76.4 |
| Education beyond high school, % | 10 | 20.7 | 77.5 | 69.8 | 62.9 |
| Material deprivation, median income | 73% material deprivation | 75.8% material deprivation | 20.8% material deprivation, $31–$75 000 | 21.0% material deprivation, $31–$75 000 | 22.5% material deprivation |
| Previous loss, % | 39.6 | 20.8 | 34.5 | 34.0 | 32.0 |
| Months since loss | |||||
| 2–<6 | 1 | — | 47 | — | — |
| 6–<12 | 16 | 7 | 54 | 33 | 40 |
| 12–<18 | 7 | 4 | 35 | 19 | 23 |
| 18–<24 | 3 | 2 | 34 | 17 | 19 |
| 24–<30 | 9 | 5 | 35 | 18 | 23 |
| ≥30 | 13 | 6 | 102 | 43 | 49 |
—, not applicable.
FIGURE 1.
A, Point prevalence of PGD in the PASS sample. B, Point prevalence of PGD in the ISPID sample. Point prevalences of PGD in the PASS and ISPID samples and 95% CIs by time from loss (as a percent of the cross-sectional sample) are shown.
There was no statistical difference between the samples in PGD constituent symptom profiles. We found no significant interaction effects between time and sample by symptom except for the shocked symptom (P = .01), for which PASS mothers reported less shock. We found no significant differences in risk of PGD by sample when controlling for months since the loss (P = .81; odds ratio = 0.92; 95% CI = 0.49–1.73). On the basis of these similarities, we combined the samples for subsequent analysis.
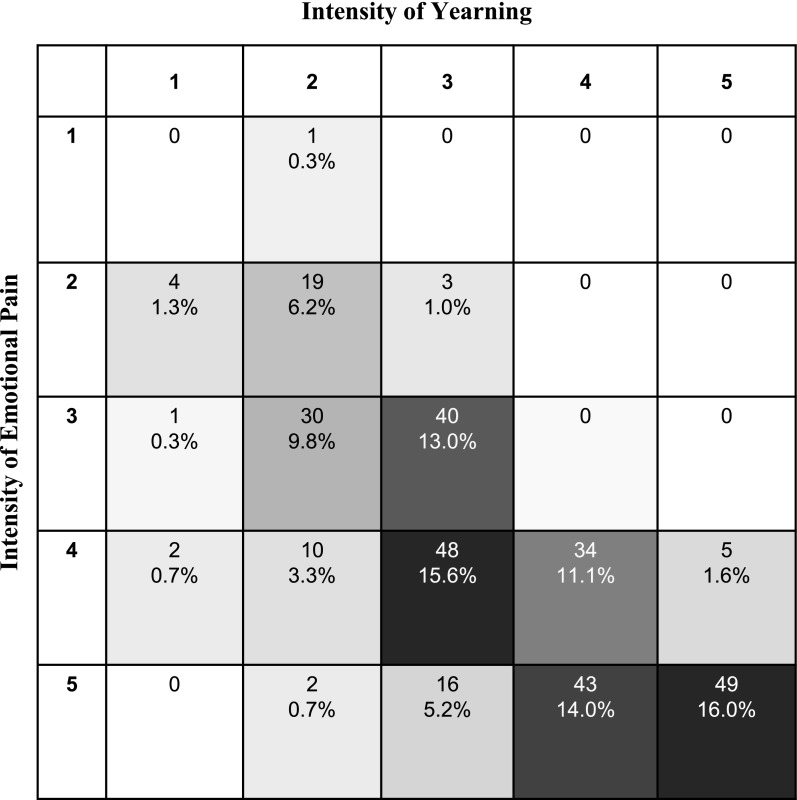
In the combined sample, 42.7% of subjects reported daily, intrusive feelings of both yearning and emotional pain, and this increased to 68.1% if either symptom was present, thus meeting the PGD diagnostic criteria for separation distress (Fig 2). There was a 7.7-fold increase in the odds of increased yearning for each unit increase in emotional pain (95% CI = 5.8–10.1; P < .0001).
FIGURE 2.
Cardinal signs of separation distress and their relative intensity. A heat graph showing the intensity of yearning and/or intensity of emotional pain in mothers 6 to 48 months after their infants’ deaths is shown. Intensity is reported on a 1-to-5 scale, capturing absent to daily intrusive experiences. Yearning was significantly associated with emotional pain. Odds ratios increased and became highly significant with greater symptom intensity.
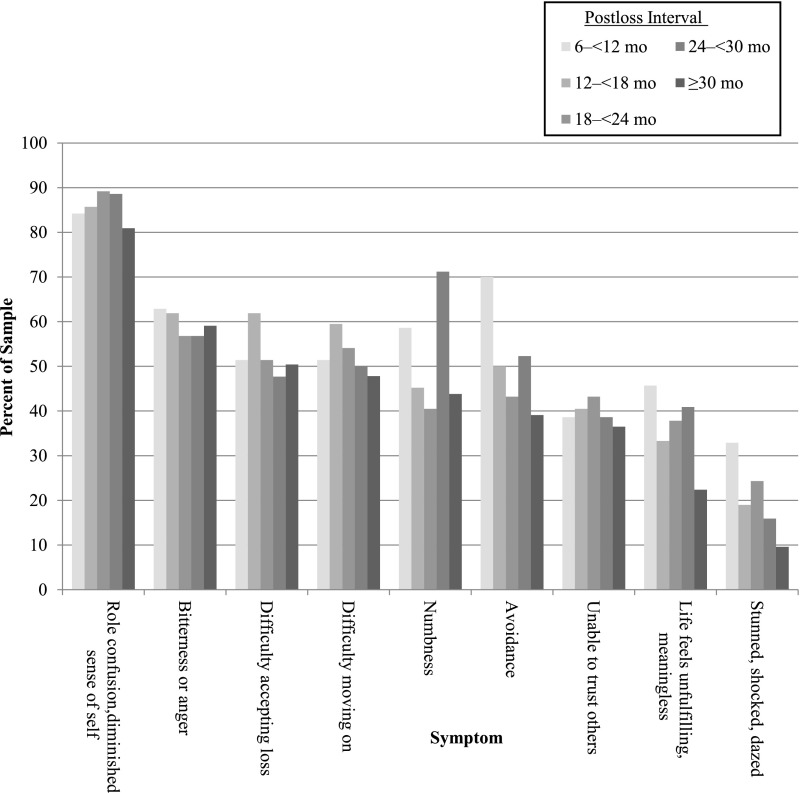
Reports of daily or disabling cognitive, emotional, and behavioral symptoms of PGD included highly prevalent role confusion and diminished sense of self (80.9%–89.2%) and bitterness or anger (56.8%–62.9%). The data revealed that the point prevalence for role confusion and diminished sense of self, anger or bitterness, and the inability to trust others remained relatively constant at each time interval, and the prevalence of avoidance, feelings of meaninglessness, shock, and numbness decreased over time. We did not formally assess these patterns because the cross-sectional design of the study limits any conclusions about individual subjects over time (Fig 3).
FIGURE 3.
Cognitive, emotional, and behavioral symptoms of PGD. Symptoms included in diagnostic criteria for PGD are shown as a percent of the time interval sample. Symptoms are highly prevalent and are shown in decreasing prevalence. Different patterns of persistence or improvement in specific symptoms can be noted.
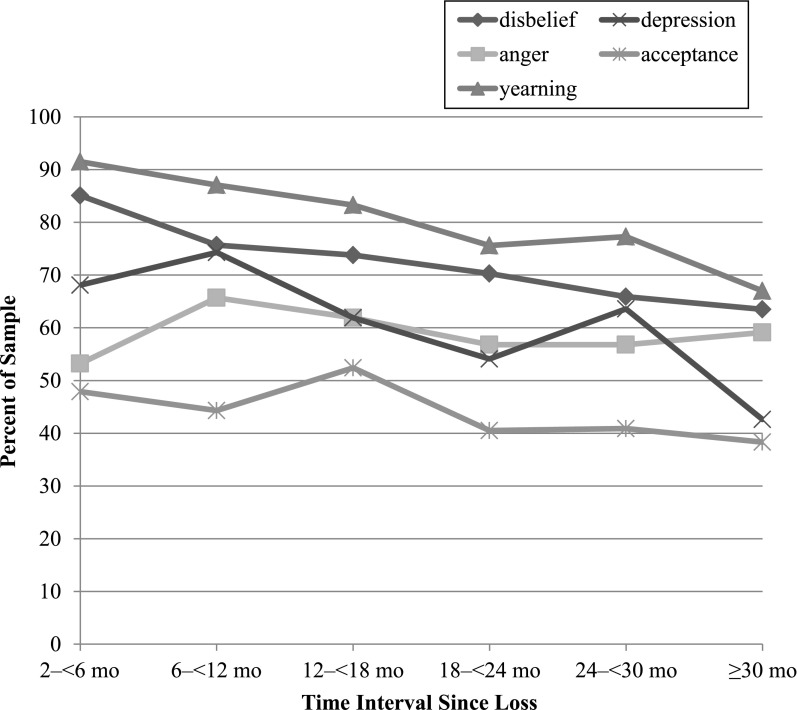
Maternal acknowledgment of grief indicators described in stage theories showed decreases in the mean reported severity of negative symptoms, but yearning, anger, and disbelief remained high (Fig 4). Yearning remained the most prevalent grief indicator. Levels of acceptance remained lower than other indicators.
FIGURE 4.
Symptoms associated with stage theories of grief. Historical grief indicators are related to the stage theories of grief. Acceptance was never more prevalent than negative grief indicators.
Discussion
In this study of maternal grief after the sudden and unexpected death of an infant, we document a population at high risk for significant grief-related pathology, specifically PGD. In comparison with the prevalence of 9.8% in bereaved adult life partners 1 year after a loss,15 57.1% of these young mothers had PGD at 1 year and 41.3% had PGD in their third year postloss. By using a standardized metric on 2 well-characterized samples, similar levels of grief-related pathology were found despite striking differences in social circumstances. Specific patterns of grief-related symptoms emerged that may prove informative in recognizing and addressing the difficult burdens on these bereaved young women.
Separation distress illustrates the intrusive, ongoing consequences of grief in these women. These are painful pangs of grief, and although not a mental disorder per se, they are a cardinal feature of pathologic grief.39 Although persistent yearning and emotional pain has been found in other research on bereaved parents,40 the high rates of PGD observed here reveals its prominence during adaptation to this loss. Theoretically, the strength and severity of separation distress reveals the importance of attachment bonds between mothers and their deceased infants. Clinically, their emotional burden remains underrecognized in medical settings, where its implications are likely to be important,41 influencing a woman’s bonding experience in a subsequent pregnancy or their parenting of other children. Current clinical practice in obstetrics and pediatrics may not attend to this morbidity in the settings where bereaved mothers present themselves, but given the fact that young adults are poor users of personal health care,42 few other opportunities exist to intervene on PGD. Even in settings where supportive medical and mental health relationships directed toward grief are established during the time leading up to a child’s death, bereaved parents report difficulties discussing their experiences of loss and seeking assistance to support them in their grief.40 Marginalized parents are especially likely to feel a lack of professional support,40 an observation that has special relevance to the demographics of SIDS, which additionally carries a stigma of blame that other diseases do not share.
Few cognitive and emotional symptoms of PGD resolved decisively, as might be inferred from the general understanding provided by stage models of grief, although stage models are meant to explain normal grief. In our research, we identified categories of highly prevalent symptoms, symptoms that appeared to continue at consistent levels, and symptoms that diminished at successive time intervals. It may be helpful for pediatricians to inquire about role confusion, anger, and feeling stuck or unable to “get over” the loss (accepting loss or moving on) during clinical encounters involving their surviving and subsequent children. Role confusion, anger, and a lack of trust in others are aspects of coping that seem least likely to change over time and may represent therapeutic targets for referral once identified. Bereaved mothers may be relieved to know that feelings of shock, avoidance, or meaninglessness are likely to improve. As in other maternal conditions, an established pediatrician has unique access to this problem.43,44
Researchers of stage models of grief,45 which involve grief indicators such as disbelief, anger, yearning, depression, and acceptance, generally maintain that negative indicators peak in intensity within 6 months and then decline as acceptance increases while also finding that acceptance is the most frequently affirmed grief indicator at any time after a loss.38 In this research, there was no time when acceptance exceeded negative grief indicators, whereas anger and yearning related to their infants’ deaths and absence were found to be present at least weekly throughout the study periods in most of the mothers. This would imply that the general emphasis in grief counseling on acceptance as an indicator of the resolution of grief may be problematic for mothers who experience a SIDS loss. Offering reassurances about developing acceptance may not prove helpful as a consolation. In conducting interviews with participants, we observed that mothers objected to questions about acceptance, pointing out that there is no replacement or moving on from their infants, which also preserves their deep identification as their children’s protector and nurturer. Anecdotally, audiences of bereaved mothers in a number of settings explained that the emphasis on acceptance fails to recognize their challenges as mothers who are responsible for maintaining memories and the value of their deceased children’s lives. They shared the difficulties they face over time as their deceased infants are less remembered or considered, noting that it contributes to their anger and inability to embrace acceptance.
Risk factors for prolonged grief include those related to the nature of the loss and to the circumstances and resources of the bereaved.46 Our methodology included 2 samples with starkly different social circumstances. The similar patterns of grief in these samples invite consideration of the relative contribution of social determinants as opposed to attachment bonds in PGD. It reveals that the challenges a mother, as a mother, faces after the death of her small, dependent infant are profound regardless of resources and disenfranchisement, and this reflects the fundamentality of the relationship that is altered.
This research has several limitations. The 2 samples were combined to enhance the sample size and generalizability, but each had different biases. The PASS sample was selected because it concentrates the risk factors PGD shares with SIDS, notably poverty, race, and alcohol use, recognizing the importance of the risk factors and also the generally limited recruitment of disenfranchised populations in this area of research. There was little ascertainment bias beyond the initial choice of the community to be studied. Despite this relevance for SIDS, however, we anticipated concerns about the representativeness of their experiences and also included a more typically studied end of the sociodemographic spectrum with greater resources and supports, the ISPID sample. Selection bias in the ISPID sample was due to recruitment from mothers who were affiliated with SIDS support organizations, who had the psychological capacity to seek bereavement support (not necessarily counseling), and possessed the resources to participate in an online survey. Despite these potential biases, responses were not significantly different between these 2 samples with highly dissimilar social determinants. Because of this, our findings are consistent with one conclusion of grief research: although culture and circumstances may influence the expression of grief, there is a core behavioral response to loss that is conserved regardless of setting.47 This study is also limited by its cross-sectional design, which precludes conclusions about longitudinal trajectories. Associations, but not causality, can be established, notably with regard to social determinants, and confounders may be unequally distributed. The number of observations limits the statistical power to assess trends.
In historic terms, contemporary times are the first in human history when the death of a child is a rare event,48 adding isolation to the high, persistent levels of grief found among parents whose young children have died of a variety of causes.23,49–52 The role of this isolation in the development of their symptoms is unclear. The fact that PGD is present in such a significant proportion of these bereaved women also raises important questions about the PGD diagnostic framework in this population because it might not be accurate to describe the symptoms as abnormal (nonnormative) when so many experience them. The high prevalence of PGD may reflect limitations in the diagnostic criteria but alternatively may reflect a largely unrecognized crisis in psychological health. This population, at an extreme boundary of newly embraced diagnostic criteria, warrants careful consideration.
Conclusions
PGD is common, distressing, and persistent in mothers whose infants have died of SIDS, with discernible symptom profiles. These findings have implications for the health and well-being of mothers of deceased infants. In considering young families, implications may extend to other dependent children living in their households, with consequences across varied levels of resources and social circumstances. Future researchers should confirm these observations in prospective longitudinal studies, investigate PGD after other child losses, examine the impact of subsequent births on PGD, and consider the grief of fathers. Pediatricians, in their role with families in the aftermath of SIDS, may be in a unique position to identify this problem and help diminish its consequences.
Glossary
- CI
confidence interval
- ISPID
International Society for the Study and Prevention of Perinatal and Infant Death
- PASS
Prenatal Alcohol in SIDS and Stillbirth
- PBQ
Parental Bereavement Questionnaire
- PGD
prolonged grief disorder
- PG-13
Prolonged Grief Disorder 13-Item Scale
- SIDS
sudden infant death syndrome
Footnotes
Dr Goldstein conceptualized and designed the study, designed the data collection instruments, coordinated and supervised data collection, conducted the data analysis and interpretation of data, drafted the initial manuscript, and reviewed and revised the manuscript; Dr Prigerson conceptualized and designed the study, designed the data collection instruments, and reviewed and revised the manuscript; Ms Human and Ms Tobacco designed the data collection instruments, collected data, and reviewed and revised the manuscript; Ms Lederman conducted the data analysis and interpretation of data and reviewed and revised the manuscript; Drs Elliott, Odendaal, and Kinney and Ms Angal coordinated and supervised data collection and critically reviewed the manuscript; Drs Lichtenthal and Morris critically reviewed and revised the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported in part by the Bode Wolfe Memorial Fund, CJ First Candle, and National Institutes of Health grants U01HD055154, U01HD045935, U01HD055155, U01HD045991, and U01AA016501. Funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute on Alcohol Abuse and Alcoholism, and the National Institute on Deafness and Other Communication Disorders. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Centers for Disease Control and Prevention; National Center for Health Statistics Compressed mortality files, 1999-2016. Available at: http://wonder.cdc.gov/cmf-icd10.html. Accessed October 17, 2017
- 2.Moon RY; Task Force on Sudden Infant Death Syndrome . SIDS and other sleep-related infant deaths: evidence base for 2016 updated recommendations for a safe infant sleeping environment. Pediatrics. 2016;138(5):e20162940. [DOI] [PubMed] [Google Scholar]
- 3.Bergman AB. Crib deaths exact needless toll of grief in infants’ families. Hosp Top. 1969;47(2):69–73 [PubMed] [Google Scholar]
- 4.Bergman AB, Pomeroy MA, Beckwith JB. The psychiatric toll of the sudden infant death syndrome. GP. 1969;40(6):99–105 [PubMed] [Google Scholar]
- 5.Green M. Psychological aspects of sudden unexpected death in infants and children. Review and commentary. Pediatr Clin North Am. 1974;21(1):113–114 [DOI] [PubMed] [Google Scholar]
- 6.Mandell F, McAnulty E, Reece RM. Observations of paternal response to sudden unanticipated infant death. Pediatrics. 1980;65(2):221–225 [PubMed] [Google Scholar]
- 7.Ostfeld BM, Ryan T, Hiatt M, Hegyi T. Maternal grief after sudden infant death syndrome. J Dev Behav Pediatr. 1993;14(3):156–162 [PubMed] [Google Scholar]
- 8.Vance JC, Najman JM, Thearle MJ, Embelton G, Foster WJ, Boyle FM. Psychological changes in parents eight months after the loss of an infant from stillbirth, neonatal death, or sudden infant death syndrome—a longitudinal study. Pediatrics. 1995;96(5, pt 1):933–938 [PubMed] [Google Scholar]
- 9.Dent A, Condon L, Blair P, Fleming P. A study of bereavement care after a sudden and unexpected death. Arch Dis Child. 1996;74(6):522–526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garstang J, Griffiths F, Sidebotham P. Parental understanding and self-blame following sudden infant death: a mixed-methods study of bereaved parents’ and professionals’ experiences. BMJ Open. 2016;6(5):e011323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lindemann E. Symptomatology and management of acute grief. 1944. Am J Psychiatry. 1994;151(suppl 6):155–160 [DOI] [PubMed] [Google Scholar]
- 12.Maciejewski PK, Maercker A, Boelen PA, Prigerson HG. “Prolonged grief disorder” and “persistent complex bereavement disorder”, but not “complicated grief”, are one and the same diagnostic entity: an analysis of data from the Yale Bereavement Study. World Psychiatry. 2016;15(3):266–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boelen PA, van de Schoot R, van den Hout MA, de Keijser J, van den Bout J. Prolonged grief disorder, depression, and posttraumatic stress disorder are distinguishable syndromes. J Affect Disord. 2010;125(1–3):374–378 [DOI] [PubMed] [Google Scholar]
- 14.Prigerson HG, Horowitz MJ, Jacobs SC, et al. Prolonged grief disorder: psychometric validation of criteria proposed for DSM-V and ICD-11 [published correction appears in PLoS Med. 2013;10(12). PLoS Med. 2009;6(8):e1000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lundorff M, Holmgren H, Zachariae R, Farver-Vestergaard I, O’Connor M. Prevalence of prolonged grief disorder in adult bereavement: a systematic review and meta-analysis. J Affect Disord. 2017;212:138–149 [DOI] [PubMed] [Google Scholar]
- 16.Xiu D, Maercker A, Woynar S, Geirhofer B, Yang Y, Jia X. Features of prolonged grief symptoms in Chinese and Swiss bereaved parents. J Nerv Ment Dis. 2016;204(9):693–701 [DOI] [PubMed] [Google Scholar]
- 17.Heeke C, Stammel N, Knaevelsrud C. When hope and grief intersect: rates and risks of prolonged grief disorder among bereaved individuals and relatives of disappeared persons in Colombia. J Affect Disord. 2015;173:59–64 [DOI] [PubMed] [Google Scholar]
- 18.Schaal S, Jacob N, Dusingizemungu JP, Elbert T. Rates and risks for prolonged grief disorder in a sample of orphaned and widowed genocide survivors. BMC Psychiatry. 2010;10:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maercker A, Brewin CR, Bryant RA, et al. Proposals for mental disorders specifically associated with stress in the International Classification of Diseases-11. Lancet. 2013;381(9878):1683–1685 [DOI] [PubMed] [Google Scholar]
- 20.Boelen PA. The centrality of a loss and its role in emotional problems among bereaved people. Behav Res Ther. 2009;47(7):616–622 [DOI] [PubMed] [Google Scholar]
- 21.Bowlby J. Loss: Sadness and Depression. Vol 3 New York, NY: Basic Books; 1980 [Google Scholar]
- 22.Rando TA. Parental Loss of a Child. Champaign, IL: Research Press; 1986 [Google Scholar]
- 23.Lannen PK, Wolfe J, Prigerson HG, Onelov E, Kreicbergs UC. Unresolved grief in a national sample of bereaved parents: impaired mental and physical health 4 to 9 years later. J Clin Oncol. 2008;26(36):5870–5876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rogers CH, Floyd FJ, Seltzer MM, Greenberg J, Hong J. Long-term effects of the death of a child on parents’ adjustment in midlife. J Fam Psychol. 2008;22(2):203–211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cleiren M, Diekstra RF, Kerkhof AJ, van der Wal J. Mode of death and kinship in bereavement: focusing on “who” rather than “how”. Crisis. 1994;15(1):22–36 [PubMed] [Google Scholar]
- 26.Michon B, Balkou S, Hivon R, Cyr C. Death of a child: parental perception of grief intensity - end-of-life and bereavement care. Paediatr Child Health. 2003;8(6):363–366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goodenough B, Drew D, Higgins S, Trethewie S. Bereavement outcomes for parents who lose a child to cancer: are place of death and sex of parent associated with differences in psychological functioning? Psychooncology. 2004;13(11):779–791 [DOI] [PubMed] [Google Scholar]
- 28.Keesee NJ, Currier JM, Neimeyer RA. Predictors of grief following the death of one’s child: the contribution of finding meaning. J Clin Psychol. 2008;64(10):1145–1163 [DOI] [PubMed] [Google Scholar]
- 29.McCarthy MC, Clarke NE, Ting CL, Conroy R, Anderson VA, Heath JA. Prevalence and predictors of parental grief and depression after the death of a child from cancer. J Palliat Med. 2010;13(11):1321–1326 [DOI] [PubMed] [Google Scholar]
- 30.Middleton W, Raphael B, Burnett P, Martinek N. A longitudinal study comparing bereavement phenomena in recently bereaved spouses, adult children and parents. Aust N Z J Psychiatry. 1998;32(2):235–241 [DOI] [PubMed] [Google Scholar]
- 31.Kersting A, Brähler E, Glaesmer H, Wagner B. Prevalence of complicated grief in a representative population-based sample. J Affect Disord. 2011;131(1–3):339–343 [DOI] [PubMed] [Google Scholar]
- 32.Dyregrov K, Nordanger D, Dyregrov A. Predictors of psychosocial distress after suicide, SIDS and accidents. Death Stud. 2003;27(2):143–165 [DOI] [PubMed] [Google Scholar]
- 33.Dyregrov A, Dyregrov K. Long-term impact of sudden infant death: a 12- to 15-year follow-up. Death Stud. 1999;23(7):635–661 [DOI] [PubMed] [Google Scholar]
- 34.Dukes KA, Burd L, Elliott AJ, et al. ; PASS Research Network . The safe passage study: design, methods, recruitment, and follow-up approach. Paediatr Perinat Epidemiol. 2014;28(5):455–465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Prigerson HG, Vanderwerker LC, Maciejewski PK. A Case for Inclusion of Prolonged Grief Disorder in DSM-V. Washington, DC: American Psychological Association; 2008 [Google Scholar]
- 36.Goldstein R, Rimer KP. Parents’ views of their child’s end-of-life care: subanalysis of primary care involvement. J Palliat Med. 2013;16(2):198–202 [DOI] [PubMed] [Google Scholar]
- 37.Statistics South Africa Methodological Report on Rebasing of National Poverty Lines and Development of Pilot Provincial Poverty Lines. Pretoria, South Africa: Statistics South Africa; 2015 [Google Scholar]
- 38.Maciejewski PK, Zhang B, Block SD, Prigerson HG. An empirical examination of the stage theory of grief. JAMA. 2007;297(7):716–723 [DOI] [PubMed] [Google Scholar]
- 39.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed Arlington, VA: American Psychiatric Publishing, Inc; 2013 [Google Scholar]
- 40.Lichtenthal WG, Corner GW, Sweeney CR, et al. Mental health services for parents who lost a child to cancer: if we build them, will they come? J Clin Oncol. 2015;33(20):2246–2253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stroebe M, Schut H, Stroebe W. Health outcomes of bereavement. Lancet. 2007;370(9603):1960–1973 [DOI] [PubMed] [Google Scholar]
- 42.Fortuna RJ, Robbins BW, Halterman JS. Ambulatory care among young adults in the United States. Ann Intern Med. 2009;151(6):379–385 [DOI] [PubMed] [Google Scholar]
- 43.Earls MF; Committee on Psychosocial Aspects of Child and Family Health American Academy of Pediatrics . Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics. 2010;126(5):1032–1039 [DOI] [PubMed] [Google Scholar]
- 44.van der Zee-van den Berg AI, Boere-Boonekamp MM, Groothuis-Oudshoorn CGM, IJzerman MJ, Haasnoot-Smallegange RME, Reijneveld SA. Post-up study: postpartum depression screening in well-child care and maternal outcomes. Pediatrics. 2017;140(4):e20170110. [DOI] [PubMed] [Google Scholar]
- 45.Kubler-Ross E. On Death and Dying. New York, NY: Collier Book/Macmillan Publishing Co; 1970 [Google Scholar]
- 46.Stroebe MS, Folkman S, Hansson RO, Schut H. The prediction of bereavement outcome: development of an integrative risk factor framework. Soc Sci Med. 2006;63(9):2440–2451 [DOI] [PubMed] [Google Scholar]
- 47.Stroebe M, Schut H. The dual process model of coping with bereavement: rationale and description. Death Stud. 1999;23(3):197–224 [DOI] [PubMed] [Google Scholar]
- 48.Centers for Disease Control and Prevention Healthier mothers and babies. MMWR Morb Mortal Wkly Rep. 1999;48(38):849–858 [PubMed] [Google Scholar]
- 49.Kreicbergs UC, Lannen P, Onelov E, Wolfe J. Parental grief after losing a child to cancer: impact of professional and social support on long-term outcomes. J Clin Oncol. 2007;25(22):3307–3312 [DOI] [PubMed] [Google Scholar]
- 50.Meert KL, Shear K, Newth CJL, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network . Follow-up study of complicated grief among parents eighteen months after a child’s death in the pediatric intensive care unit. J Palliat Med. 2011;14(2):207–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Alam R, Barrera M, D’Agostino N, Nicholas DB, Schneiderman G. Bereavement experiences of mothers and fathers over time after the death of a child due to cancer. Death Stud. 2012;36(1):1–22 [DOI] [PubMed] [Google Scholar]
- 52.Kristensen P, Dyregrov K, Dyregrov A, Heir T. Media exposure and prolonged grief: a study of bereaved parents and siblings after the 2011 Utøya Island terror attack. Psychol Trauma. 2016;8(6):661–667 [DOI] [PubMed] [Google Scholar]