Abstract
Background
Surgical care represents an important source of opioid prescribing and chronic use, but rates of prolonged opioid use following pediatric procedures remain unclear. We describe the rates and risk factors for new persistent opioid use in patients after common cleft operations.
Methods
We examined claims from the Truven Marketscan databases from January 1, 2010 to December 31, 2014. We included opioid-naive patients ages 8 to 25, who underwent one of 10 cleft-related procedures. Patients were considered opioid-naïve if they had no opioid prescription fills in the 11 months prior to the perioperative period. We obtained a random sample of age-matched, non-surgical patients from the same dataset to be used as a control group. Included cleft patients had no procedural codes six months following surgery. All included patients filled an opioid prescription during the perioperative period, defined as 30 days before and 14 days after surgery. The primary outcome was new persistent opioid use, which is defined as continued opioid prescription fills between 90 and 180 days after the procedure.
Results
This cohort included 2,039 cleft patients and 2,100 control patients. The incidence of new persistent opioid use following surgery was 4.4% and 0.1% in the control group. Higher odds of opioid use three months beyond surgery were associated with distractor placement (OR 5.34, CI 2.00–14.24, p=0.001). Increasing age (OR 1.11, CI 1.04–1.17, p=0.001) and presence of a gastrointestinal comorbidity (OR 7.37, CI 1.49–36.54, p=0.014) were also associated with new persistent use.
Conclusions
New persistent opioid use occurs after cleft-related procedures and could lead to chronic use in children, adolescents, and young adults.
Keywords: analgesics, opioid, cleft, craniofacial, orthognathic
INTRODUCTION
The opioid epidemic constitutes an immense public health problem in the United States, devastating countless American lives over the last two decades [1]. An increasing number of opioids have been prescribed over this time period, totaling 259 million in 2012 alone. This amounted to four times the number of opioid prescriptions distributed in 1999 [2]. Not surprisingly, the increasing quantity of opioids in public circulation has culminated in dire consequences. Opioids resulted in over 1.3 million hospitalizations in 2014 [3] and over 20,000 overdose deaths in 2015 [4]. The total financial burden levied on society by overdose, abuse, and dependence is estimated to be over $78 billion [5]. In response to the escalating crisis, legislation passed in 49 states initiated close monitoring of prescription drugs [6].
Interestingly, opioid prescribing for surgical pain in the acute post-operative period has been shown to significantly contribute to persistent narcotic use in the future, regardless of procedure type [7]. As such, post-operative prescribing habits remain an ongoing area of scrutiny to better safeguard opioid naïve patients from addiction after surgery. However, while narcotic prescribing patterns in the post-operative period have been studied recently in the adult population, even less is known about persistent use after surgery in children and young adults. Recent research demonstrated that some abdominal procedures have been linked to persistent use in the pediatric population, with increased risk for persistent use associated with colectomy and cholecystectomy [8]. However, the literature lacks any data on persistent opioid use after other pediatric procedures, such as operations performed in children with cleft lip and/or cleft palate (CLCP). Given the impact of deformity and the need for multiple surgeries, significant psychological issues accompany these patients, therefore differentiating them from the general surgery population and perhaps increasing their risk for persistent opioid use [9,10].
In this study, we analyzed national claims data to measure the rate of persistent opioid use in children, adolescents, and young adults after common cleft-related operations and determine important risk factors for persistent use in this particular patient population.
MATERIALS AND METHODS
Data Source and Study Cohort
After obtaining exemption from the Institutional Review Board, we analyzed the Truven Health MarketScan Research Databases, which capture patient-level pharmacy claims and medical services. These databases reflect care for approximately 50 million employees across the country, including that of their children. To obtain our cohort, we reviewed the databases from January 1, 2010 to December 31, 2014. Patients between the ages of 8–25 who underwent any of the pre-selected cleft-related operations were included. The selected operations were 1) distraction osteogenesis, 2) palatoplasty, 3) repair of nasolabial/oral-nasal fistula, 4) alveolar cleft bone graft, 5) cleft lip/nose revision, 6) cleft rhinoplasty, 7) pharyngeal flap, 8) lengthening of palate with island flap, 9) adjacent tissue transfer, and 10) orthognathic procedures. Procedures not universally associated with facial clefts required an accompanying cleft lip and/or cleft palate ICD-9 code (749.0, 749.1, or 749.2). Orthognathic procedures performed with dentofacial anomaly ICD-9 codes (524.9, 524.50, 524.89, 524.00) were included. If patients underwent more than one procedure in the same day, the patient was categorized by the most painful procedure (determination made by KGB and CJV). Operations usually performed in infancy (cleft lip and palate repairs) were excluded, given the extremely low likelihood of persistent opioid use afterwards.
In order to ensure an opioid-naïve cohort, all included patients were required to have continuous insurance coverage during the 12 months prior to the procedure and 6 months after, as well as no pharmacy claims reflecting opioid prescriptions during the 11 months prior to surgery. To eliminate patients with persistent use secondary to additional operations, any subsequent codes for anesthesia or additional surgical procedures within six months after the index surgical procedure resulted in exclusion. Any patients who did not fill an opioid prescription within the defined perioperative period, 30 days before and 14 days after surgery, were also excluded. For a comparison cohort of patients who did not undergo surgery, we identified a random sample of 2,100 of the 5,392,859 non-surgical patients ages 8 to 25 years in Truven Health Marketscan®. Patients in the control group were assigned a random fictitious surgery date during the study period, and the three inclusion criteria, including continuous insurance coverage, no additional procedures, and opioid-naïve status, were applied.
Persistent opioid use was the primary outcome, defined as continued prescription fills between 90 and 180 days after surgery. Patient characteristics potentially associated with persistent use were examined, such as mental health diagnoses, pain disorders, Feudtner complex chronic conditions [11], and sociodemographic factors.
Statistical Analysis
Descriptive statistics were performed for both the study and control population, including type of surgery, patient demographics, and mental health diagnoses. A multivariable logistic regression model was used to estimate odds ratios (ORs) and to identify patient factors associated with increased risk of persistent opioid use. The analysis was conducted using SAS 9.4. Statistical significance was set at p=0.05.
RESULTS
A total of 2,039 patients (mean age: 14.9 ± 4.8 years) were retrieved from the database using our inclusion criteria. Most patients in the surgical cohort were male (57.4%), whereas most were female in the control group (50.2%). There were significantly more Feudtner complex conditions in the surgical group (Table 1). The percentage of patients with depression, anxiety, drug and substance abuse, and other mental conditions was higher in the surgical cohort compared with the control group. The most common procedure types in the cohort were alveolar cleft bone graft (24.7%), placement of distractors (17.9%), and cleft lip/nose revision (17.6%).
Table 1.
Characteristics of study population.
| Surgical Population (n=2,039) | Control Population (n=2,100) | |||
|---|---|---|---|---|
| N | % Total | N | % Total | |
| Age | ||||
| 8–12 | 730 | 35.8% | 614 | 29.2% |
| 13–17 | 680 | 33.3% | 698 | 33.2% |
| 18–20 | 329 | 16.1% | 336 | 16.0% |
| 21–25 | 300 | 14.7% | 452 | 21.5% |
| Sex | ||||
| Male | 1171 | 57.4% | 1045 | 49.8% |
| Female | 868 | 42.6% | 1055 | 50.2% |
| Geographic Region | ||||
| Northeast | 342 | 16.8% | 459 | 21.9% |
| North Central | 498 | 24.4% | 489 | 23.3% |
| South | 789 | 38.7% | 686 | 32.7% |
| West | 374 | 18.3% | 421 | 20.0% |
| Unknown | 36 | 1.8% | 45 | 2.1% |
| Type of Surgery | ||||
| Distraction osteogenesis | 364 | 17.9% | ||
| Palatoplasty | 66 | 3.2% | ||
| Repair of nasolabial/oral-nasal fistula | 33 | 1.6% | ||
| Alveolar cleft bone graft | 504 | 24.7% | ||
| Cleft lip/nose revision | 358 | 17.6% | ||
| Cleft rhinoplasty | 341 | 16.7% | ||
| Pharyngeal flap | 108 | 5.3% | ||
| Adjacent tissue transfer | 28 | 1.4% | ||
| Orthognathic procedures | 237 | 11.6% | ||
| Number of Procedures | ||||
| One | 1596 | 78.3% | ||
| More than One | 443 | 21.7% | ||
| Feudtner Pediatric complex chronic conditions | ||||
| Neurologic and Neuromuscular | 23 | 1.1% | 12 | 0.6% |
| Cardiovascular | 58 | 2.8% | 21 | 1.0% |
| Respiratory | 105 | 5.1% | 1 | 0.0% |
| Renal and Urologic | 6 | 0.3% | 3 | 0.1% |
| Gastrointestinal | 13 | 0.6% | 3 | 0.1% |
| Hematologic or immunologic | 15 | 0.7% | 4 | 0.2% |
| Metabolic | 32 | 1.6% | 22 | 1.0% |
| Other Congenital or Genetic Defect | 120 | 5.9% | 33 | 1.6% |
| Malignancy | 65 | 3.2% | 33 | 1.6% |
| Premature and Neonatal | 0 | 0.0% | 1 | 0.0% |
| Other conditions | 15 | 0.7% | 4 | 0.2% |
| Chronic Pain Disorders | 125 | 6.1% | 73 | 3.5% |
| Mental Condition | ||||
| Depression | 32 | 1.6% | 29 | 1.4% |
| Anxiety | 60 | 2.9% | 40 | 1.9% |
| Drug & Substance Abuse | 35 | 1.7% | 14 | 0.7% |
| Other Mental Cond. | 45 | 2.2% | 22 | 1.0% |
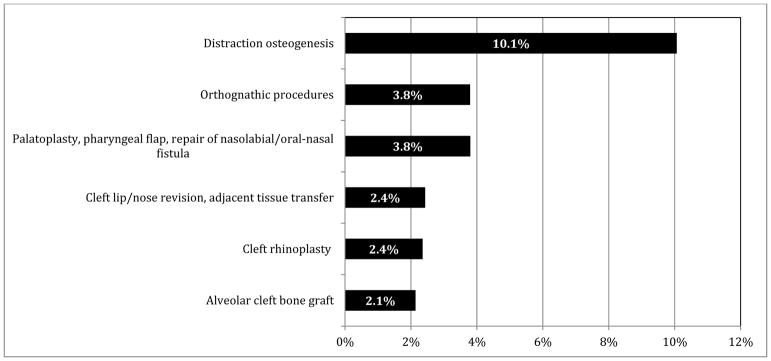
The incidence of new persistent opioid use in the surgical cohort was 4.4%, compared with only 0.1% in the randomly generated control group. Unadjusted rates of persistent use are included in Table 2, with the highest rates seen in patients undergoing distraction and patients undergoing palatoplasty, pharyngeal flap, or fistula repair. Procedures were combined to protect patient privacy, due to the small numbers of persistent users within each procedure type. The logistic regression model fit adequately using Hosmer – Lemeshow goodness-of-fit test (p=0.7.49) with c-statistic 0.773. After adjusting for relevant covariates, increasing age was found to be a significant risk factor, with the odds of persistent use increasing by 11% with each additional year (Table 3). Persistent use did not vary by gender on bivariate analysis, and thus was not included in the regression. Living in regions outside the Northeast (North Central, South, West) was associated with increased odds of new persistent use (Table 3). Having a chronic gastrointestinal (GI) condition was also associated with increased odds of persistent post-operative use (OR 7.37, CI 1.49–36.54, p=0.014), but persistent use was not correlated with other chronic conditions, depression, or chronic pain issues. Odds of persistent use were not increased if more than one procedure was performed (OR 1.41, CI 0.63–3.20, p=0.40). Only distractor placement was associated with increased odds of persistent use (OR 5.34, CI 2.00–14.24, p=0.001). Adjusted probability of persistent use was 10.1% after distractor placement, and 3.8% after both orthognathic procedures and intraoral soft tissue procedures (palatoplasty, pharyngeal flap, fistula repair) (Figure 1).
Table 2.
Unadjusted rates of persistent use, by procedure.
| Type of Surgery | # Persistent use | % Persistent use |
|---|---|---|
| Distraction osteogenesis | 46 | 12.6% |
| Palatoplasty for cleft palate, Pharyngeal flap, Repair of nasolabial/oral-nasal fistula | 7 | 3.3% |
| Alveolar cleft bone graft | 7 | 1.4% |
| Cleft lip/nose revision, Adjacent tissue transfer | 11 | 2.8% |
| Cleft rhinoplasty | 7 | 2.1% |
| Orthognathic procedures | 12 | 5.1% |
| TOTAL | 90 | 4.4% |
Table 3.
Multivariable logistic regression for persistent opioid use.
| Coef (β) | Odds Ratio (OR) | 95% CI OR | P-value | |
|---|---|---|---|---|
| Age | 0.10 | 1.11 | 1.04 – 1.17 | 0.001 |
| Geographic Region (ref: Northeast) | ||||
| North Central | 0.90 | 2.46 | 1.02 – 5.93 | 0.045 |
| South | 0.97 | 2.63 | 1.14 – 6.08 | 0.023 |
| West | 1.17 | 3.22 | 1.33 – 7.77 | 0.009 |
| Unknown | 1.08 | 2.94 | 0.56 – 15.46 | 0.202 |
| Type of Surgery (ref: Alveolar cleft bone graft) | ||||
| Distraction osteogenesis | 1.68 | 5.34 | 2.00 – 14.24 | 0.001 |
| Palatoplasty, pharyngeal flap, repair of nasolabial/oral-nasal fistula | 0.61 | 1.84 | 0.61 – 5.52 | 0.279 |
| Cleft lip/nose revision, adjacent tissue transfer | 0.13 | 1.14 | 0.42 – 3.06 | 0.796 |
| Cleft rhinoplasty | 0.10 | 1.11 | 0.29 – 4.25 | 0.882 |
| Orthognathic procedures | 0.60 | 1.83 | 0.61 – 5.47 | 0.279 |
| More than one surgery | 0.30 | 1.35 | 0.62 – 2.95 | 0.446 |
| Feudtner Pediatric Complex Chronic Conditions | ||||
| Respiratory | −1.49 | 0.22 | 0.03 – 1.74 | 0.152 |
| Gastrointestinal | 2.00 | 7.37 | 1.49 – 36.54 | 0.014 |
| Other Congenital or Genetic Defect | 0.60 | 1.83 | 0.77 – 4.37 | 0.175 |
| Chronic Pain | −0.43 | 0.65 | 0.28 – 1.54 | 0.330 |
| Mental Condition: Depression | 0.83 | 2.29 | 0.80 – 6.57 | 0.123 |
Figure 1.
Adjusted rates of persistent opioid use by procedure type.
DISCUSSION
A consensus statement released by the American Pain Society and the American Academy of Pain Medicine in 1996 claimed that the risk of new opioid addiction was low and tolerance an uncommon problem [12]. Unfortunately, the reality of the opioid crisis in the United States stands in stark contrast to these conclusions, even impacting adolescents and young adults exposed to opioids [13]. Currently, young adults ages 18–25 are responsible for the greatest amount of opioid abuse compared with other age groups [14], with addiction rates six times higher in 2014 than 2001 [15]. Regarding younger users, adolescent consumption of non-heroin opioids has nearly doubled over the last ten years [16], with 267,000 teens using pain relievers for non-medical purposes [17]. Tragically, overdose deaths in both adolescents and young adults have increased more than three fold between 1999 and 2014 [18]. As increasing amounts of opioids have become available, opioid-related admissions in adolescents increased at a similar rate between 1995 and 2005 [19] with treatment outcomes characterized by frequent relapses and program non-compliance [20]. These adolescents are also at increased risk for poor psychosocial outcomes and other health risk behaviors [21], and long-term prognosis is poor compared with adolescents using other substances [22]. Furthermore, opioid misuse in adolescents frequently escalates to heroin use, with 80% of heroin users admitting to prior opioid consumption [23].
A more recently understood contributor to opioid dependence is perioperative opioid prescribing for surgical pain. This phenomenon has been demonstrated in general surgical procedures, as well as hand and orthopedic surgery [7,24,25]. These studies also demonstrate that persistent use is more heavily influenced by patient-level factors than by procedure type, indicating that severity of surgical pain is unlikely related to opioid dependence [7]. These authors cited mental health disorders, in addition to chronic pain diagnoses, as predisposing patients to opioid misuse after surgery. Since the literature lacks specifics on provider prescribing patterns, promoting awareness of patient-level variables that increase the odds of persistent opioid use remains a critical strategy for avoiding opioid dependence in surgical patients.
In this cohort, increasing age, having a chronic GI condition, and living outside the Northeast increased patients’ odds for persistent opioid use after cleft-related operations. Age has previously been correlated with substance abuse in the non-cleft population and should impact our prescribing patterns in older pediatric patients [26,27]. Regarding GI conditions, increased odds of chronic opioid use have been found in pediatric patients with inflammatory bowel disease, and even greater odds of chronic use were associated with accompanying high utilization of health care services and psychological impairment [28]. Moreover, pathways of chronic GI pain initiated by inflammation sometimes persist despite resolution of inflammation, rendering symptom treatment difficult. Such entities necessarily fall under the broad category of functional abdominal pain, without an identifiable etiology [29]. Unfortunately, no drugs exist to specifically target pain in these difficult patients, and current available evidence suggests poor efficacy of antidepressants, antiepileptics, and antispasmodics compared with placebo [29]. As such, patients with CLCP and a GI comorbidity may continue to use opioids and refill prescriptions after surgery in an attempt to control their abdominal pain. With respect to regional risk, geographic variation in opioid prescribing has been previously described, but causation remains unknown [30]. Regional variation is unlikely secondary to meaningful differences between populations, but rather reflects the failure to standardize opioid prescribing [31].
Of the procedures studied, distraction was associated with higher odds of opioid use more than 90 days after surgery. After acute surgical pain has been controlled during the latency phase of distraction, patients may experience renewed or worsened pain during the activation phase. Furthermore, trauma to the pin sites, sleeping on the distractor, and distractor removal in clinic may also cause additional pain, resulting in liberal opioid prescription refills. While many of these patients undergo distractor removal by three months, transitioning to a non-opioid pain medication early on must be considered in those who have not undergone removal.
Both for individual patients and society as a whole, it is critical to eradicate trends of opioid dependence in children, adolescents, and young adults after surgery. Heightened awareness of this problem amongst cleft and craniofacial surgeons will serve to decrease the rate of persistent opioid use after these operations. The suspicion for persistent use after surgery has likely been far too low to prompt a shift toward more conservative opioid prescribing. Clear evidence of persistent use in a somewhat surprising patient population renders the need for thoughtful prescribing even more imperative. Intentionally switching to acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs) as early as possible after surgery would help to mitigate the rates of persistent use seen in this study [32,33]. Finally, the value of patient and parent education on the risks of opioids and proper pain expectations cannot be minimized. Even if surgeons alter their own prescribing patterns, some patients may seek opioid prescriptions from other providers if they 1) fail to appreciate the risks of medications prescribed and/or 2) inappropriately anticipate having minimal to no pain after surgery.
CONCLUSIONS
As top public health officials conclude that the opioid epidemic is worsening [34], it is incumbent upon all healthcare providers to acknowledge their own contributions to the problem, no matter how improbable opioid dependence may seem in their respective patient populations. Despite caring for a largely pediatric population, craniofacial surgeons must consider the potential for opioid misuse in children, adolescents, and young adults undergoing cleft-related operations. More conservative opioid prescribing in vulnerable patients, transitioning to non-narcotic pain medications quickly after surgery, and increasing patient education all remain essential for ameliorating the impact of the opioid crisis in cleft patients.
Footnotes
Conflicts of Interest and Sources of Funding: Katelyn G. Bennett is currently supported by the National Institute of Dental and Craniofacial Research (1F32DE027604-01). Jennifer F. Waljee is supported by Michigan Department of Health and Human Services (MDHHS) (E20180672-00). For the remaining authors, none are declared.
References
- 1.Dart RC, Surratt HL, Cicero TJ, et al. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015;372(3):241–8. doi: 10.1056/NEJMsa1406143. [DOI] [PubMed] [Google Scholar]
- 2.Scully RE, et al. Defining Optimal Length of Opioid Pain Medication Prescription After Common Surgical Procedures. JAMA Surg. 2017 doi: 10.1001/jamasurg.2017.3132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. [Accessed December 22, 2017];Hospitals are clogged with patients struggling with opioids. Available at: https://www.nytimes.com/2017/08/21/health/hospitals-opioid-epidemic-patients.html.
- 4. [Accessed on December 22, 2017];Opioid Addiction 2016 Facts and Figures. Available at: https://www.asam.org/docs/default-source/advocacy/opioid-addiction-disease-facts-figures.pdf.
- 5.Florence CS, Zhou C, Luo F, Xu L. The Economic Burden of Prescription Opioid Overdose, Abuse, and Dependence in the United States, 2013. Med Care. 2016;54(10):901–6. doi: 10.1097/MLR.0000000000000625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Home and recreational safety: laws by state. Atlanta: Centers for Disease Control and Prevention; [Accessed October 6, 2017]. Available at: http://www.cdc.gov/HomeandRecreationalSafety/Poisoning/laws/state/index.html. [Google Scholar]
- 7.Brummett CM, Waljee JF, Goesling J, et al. New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harbaugh CM, Lee JS, Hu HM, et al. Persistent Opioid Use Among Pediatric Patients After Surgery. Pediatrics. 2018 Jan;141(1) doi: 10.1542/peds.2017-2439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu L, Wang W, Yang L, Zhang H. The effects of Y-shaped conchal cartilage transplantation on the correction of nasal deformity secondary to cleft lip and its influence on mental health. Exp Ther Med. 2017;14(4):3549–3554. doi: 10.3892/etm.2017.4994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kapp-Simon KA. Psychological issues in cleft lip and palate. Clin Plast Surg. 2004;31(2):347–52. doi: 10.1016/S0094-1298(03)00134-2. [DOI] [PubMed] [Google Scholar]
- 11.Feudtner C, Christakis DA, Connell FA. Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington State, 1980–1997. Pediatrics. 2000;106(1 Pt 2):205–9. [PubMed] [Google Scholar]
- 12.Von Korff M, Kolodny A, Deyo RA, Chou R. Long-term opioid therapy reconsidered. Ann Intern Med. 2011;155:325–328. doi: 10.1059/0003-4819-155-5-201109060-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. [Accessed on October 6, 2017];Battling opioid addiction in adolescents. Available at: https://health.usnews.com/health-care/patient-advice/articles/2017-08-01/battling-opioid-addiction-in-adolescents.
- 14. [Accessed December 22, 2017];Abuse of prescription drugs affects young adults most. Available at: https://www.drugabuse.gov/related-topics/trends-statistics/infographics/abuse-prescription-rx-drugs-affects-young-adults-most.
- 15. [Accessed December 22, 2017];Opioid addiction skyrockets in young adults, but few get treatment meds. Available at: https://www.cbsnews.com/news/opioid-addiction-young-adults-few-get-suboxone-treatment-drugs/
- 16. [Accessed on October 6, 2017];Monitoring the future national results on adolescent drug use: Overview of Key Findings, 2011. Available at: http://www.monitoringthefuture.org/pubs/monographs/mtf-overview2011.pdf.
- 17.Center for Behavioral Health Statistics and Quality. [Accessed October 6, 2017];Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health. 2016 (HHS Publication No. SMA 16-4984, NSDUH Series H-51). Available at: http://www.samhsa.gov/data/
- 18.Saloner B, Feder KA, Krawczyk N. Closing the Medication-Assisted Treatment Gap for Youth With Opioid Use Disorder. JAMA Pediatr. 2017;171(8):729–731. doi: 10.1001/jamapediatrics.2017.1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Substance Abuse and Mental Health Services Administration (SAMHSA) Office of Applied Studies (OAS) [Accessed October 6, 2017];Admissions aged 12–17 by primary substance of abuse: TEDS 1995–2005, Table 5.1a. 2006 Available at: http://wwwdasis.samhsa.gov/teds05/TEDSAd2k5Tbl5.1a.htm.
- 20.Marsch LA, Bickel WK, Badger GJ, et al. Comparison of pharmacological treatments for opioid-dependent adolescents: a randomized controlled trial. Arch Gen Psychiatry. 2005;62:1157–64. doi: 10.1001/archpsyc.62.10.1157. [DOI] [PubMed] [Google Scholar]
- 21.Godley MD, Passetti LL, Subramaniam GA, Funk RR, Smith JE, Meyers RJ. Adolescent Community Reinforcement Approach implementation and treatment outcomes for youth with opioid problem use. Drug Alcohol Depend. 2017;174:9–16. doi: 10.1016/j.drugalcdep.2016.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Subramaniam G, Stitzer MA, Woody G, Fishman MJ, Kolodner K. Clinical characteristics of treatment seeking adolescents with opioid versus cannabis/alcohol use disorders. Drug Alcohol Depend. 2009;99:141–149. doi: 10.1016/j.drugalcdep.2008.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers—United States, 2002–2004 and 2008–2010. Drug Alcohol Depend. 2013;132(1–2):95–100. doi: 10.1016/j.drugalcdep.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 24.Johnson SP, Chung KC, Zhong L, et al. Risk of Prolonged Opioid Use Among Opioid-Naive Patients Following Common Hand Surgery Procedures. J Hand Surg Am. 2016;41(10):947–957 e3. doi: 10.1016/j.jhsa.2016.07.113. [DOI] [PubMed] [Google Scholar]
- 25.Goesling J, Moser SE, Zaidi B, et al. Trends and predictors of opioid use after total knee and total hip arthroplasty. Pain. 2016;157(6):1259–65. doi: 10.1097/j.pain.0000000000000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Simkin DR. Adolescent substance use disorders and comorbidity. Pediatr Clin North Am. 2002;49(2):463–77. doi: 10.1016/s0031-3955(01)00014-1. [DOI] [PubMed] [Google Scholar]
- 27.Deykin EY, Levy JC, Wells V. Adolescent depression, alcohol and drug abuse. Am J Public Health. 1987;77(2):178–82. doi: 10.2105/ajph.77.2.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Buckley JP, Cook SF, Allen JK, Kappelman MD. Prevalence of chronic narcotic use among children with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2015;13(2):310–315 e2. doi: 10.1016/j.cgh.2014.07.057. [DOI] [PubMed] [Google Scholar]
- 29.Miranda A, Saps M. The use of non-narcotic pain medication in pediatric gastroenterology. Paediatr Drugs. 2014;16(4):293–307. doi: 10.1007/s40272-014-0080-6. [DOI] [PubMed] [Google Scholar]
- 30.Paulozzi LJ, Mack KA, Hockenberry JM. Variation among states in prescribing of opioid pain relievers and benzodiazepines—United States, 2012. J Safety Res. 2014 Dec;51:125–9. doi: 10.1016/j.jsr.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 31.Morden NE, Munson JC, Colla CH, et al. Prescription opioid use among disabled Medicare beneficiaries: intensity, trends, and regional variation. Med Care. 2014 Sep;52(9):852–9. doi: 10.1097/MLR.0000000000000183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oltman J, et al. Multimodal Analgesia in Outpatient Head and Neck Surgery: A Feasibility and Safety Study. JAMA Otolaryngol Head Neck Surg. 2017 doi: 10.1001/jamaoto.2017.1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Warren JA, Militsakh O, D’Agostino M, et al. Effect of Multimodal Analgesia on Opioid Use After Open Ventral Hernia Repair. J Gastrointest Surg. 2017 doi: 10.1007/s11605-017-3529-4. [DOI] [PubMed] [Google Scholar]
- 34. [Accessed on October 6, 2017];Opioid epidemic ‘getting worse instead of better,’ public health officials warn. Available at: http://www.courierpostonline.com/story/news/politics/2017/10/05/opioid-epidemic-getting-worse-instead-better-public-health-officials-warn/732192001/