Abstract
Background and Objective:
Some patients who undergo laparoscopic hysterectomy request overnight admission for pain management, thus increasing costs for a surgery that is safe for same-day discharge. We wanted to evaluate whether a paracervical block of bupivacaine with epinephrine before laparoscopic supracervical hysterectomy would decrease overnight admission rates, postoperative pain, and pain medication requirement
Methods:
This was a randomized, double-blind, placebo-controlled, parallel-group trial (Canadian Task Force classification I) at an academic medical center. Patients undergoing laparoscopic supracervical hysterectomy were randomized to a 20-mL paracervical injection of either 0.25% bupivacaine with epinephrine or 20 mL normal saline before skin incision. All providers, except the circulating nurse, were blinded. The primary outcome was overnight hospital admission rate. Secondary outcomes included postoperative pain medication use and pain scores. Analysis included t test, χ2, Wilcoxon, and ANOVA.
Results:
One hundred thirty-two patients were enrolled—68 in the treatment group and 64 in the placebo group. Demographics were similar between groups. The unplanned overnight admission rate was 34% for the treatment group and 27% for the placebo group (P = .25). After discharge, the treatment group used on average 8.5 tablets of narcotics, whereas the placebo group used 11.7 tablets (P = .07). The treatment group took 13.1 tablets of nonnarcotic analgesics compared to 11.2 in the placebo group (P = .57). Both groups reported similar pain scores.
Conclusion:
Paracervical block with bupivacaine and epinephrine before laparoscopic supracervical hysterectomy did not decrease overnight admission rate or affect postoperative pain. Postoperative opiate use was minimally decreased.
Keywords: Laparoscopic supracervical hysterectomy, Overnight admission, Paracervical block, Post-operative pain, Preemptive analgesia
INTRODUCTION
Hysterectomy is one of the most commonly performed surgeries in the United States, with more than 370,000 performed each year.1 Same-day discharge for laparoscopic hysterectomy has been shown to be safe.2–6 However, some patients request an overnight admission for pain management.7,8 With the increasing cost of medical care and the current focus on the rising abuse of opiates, a means of decreasing hospital stay and opiate use would have great importance. Preemptive analgesia, which seeks to prevent postoperative pain by administration of an adequate level of analgesia before tissue injury, thus inhibiting central sensitization to the painful stimulus,9,10 may help decrease pain in the postoperative period so that patients feel comfortable enough to leave the hospital within hours of surgery. Several routes of preemptive analgesia have been studied in gynecologic surgery, including port site injections, long acting opioids, neuromodulators, intraperitoneal bupivacaine, and paracervical block.11–15
The paracervical block has been used for first trimester terminations with success in reducing intraoperative, but not postoperative, pain.16 Patients who underwent vaginal hysterectomy and received a paracervical block had lower postoperative pain in the first 3–6 hours compared with placebo.17,18 By hours 12 and 24, there was no longer a difference in reported pain scores between the groups.
The goals of our study were to evaluate whether patients who receive a paracervical block of bupivacaine with epinephrine at the onset of laparoscopic supracervical hysterectomy would have lower overnight admission rates, with less postsurgical pain and less pain medication than patients who receive a paracervical injection of normal saline.
The trial was registered with clinicaltrials.gov (NCT01534416).
MATERIALS AND METHODS
This randomized, double-blind, placebo-controlled, parallel-group trial was conducted at an academic medical center from February 2012 through December 2013. The study was approved by the Institutional Review Board; CONSORT guidelines were followed.19 Written informed consent was obtained before the study. We recruited patients 18 years of age and older, who were scheduled to undergo a laparoscopic supracervical hysterectomy for benign indications. Women who did not meet the criteria, had suspected malignant disease, or were not appropriate candidates for laparoscopic surgery were excluded. All procedures were performed by a single surgeon assisted by fellows in minimally invasive gynecologic surgery, fellows in female pelvic medicine and reconstructive surgery, and residents.
The patients were randomized to receive a paracervical injection of either 0.25% bupivacaine with 1:200,000 epinephrine (BE group) or normal saline (NS group). Randomization was performed with a computer-generated plan with random blocks in a 1:1 ratio. The group allocation was concealed in an opaque, sealed envelope before starting the study. The envelope was opened by the circulating nurse who prepared the syringe. All other care providers and patients were blinded to the study group.
The paracervical injection was administered by the attending surgeon after intubation but before first skin incision. All patients received general anesthesia with paralysis and intubation in a standardized fashion. The paracervix was injected with 20 mL of the assigned solution in equal parts at 2, 5, 7, and 10 o'clock. The solution was injected with a size 22 spinal needle with the injection being performed at a depth of 2 cm, just under the epithelium at the specified sites. The supracervical hysterectomy was performed with one 10-mm umbilical port and two 5-mm lateral ports and included modified McCall's culdoplasty, power morcellation, and routine cystoscopy. All skin incision sites were injected with 5 mL 0.5% bupivacaine before each incision. No other preoperative anesthesia was administered. Concomitant procedures, such as a bilateral salpingo-oophorectomy or sacrocervicopexy, were allowed in our study as long as the same ports were used as for the hysterectomy. Intraoperative anesthesia care and medications were standardized by the anesthesia team. All patients were given intraoperative prophylactic nausea treatment with intravenous dexamethasone 4 mg and ondansetron 4 mg. Patients received acetaminophen 1000 mg and ketorolac 30 mg at the end of the procedure, unless medically contraindicated. After surgery, patients were transferred to the postanesthesia care unit (PACU). All patients had been counseled in the office that they should go home the day of the surgery, barring any complications, but that their insurance allowed them to stay 23 hours and that the time of discharge would be up to them. They were only considered admitted if they remained over 12 hours. In the recovery room, patients were given oral oxycodone 5 mg/acetaminophen 325 mg on request and additional IV boluses of morphine 5 mg, as needed.
The primary outcome was rate of overnight admission. The indication for admission was recorded. Secondary outcomes were postoperative pain medication use in the PACU and in the first 14 days after surgery, pain scores, intraoperative estimated blood loss (EBL), and complications. Blood loss was estimated by the attending surgeon. Patients were given a prescription for hydrocodone 7.5 mg/ibuprofen 200 mg. They were instructed to take either the combined opiate/ibuprofen or ibuprofen 200-mg tabs alone as needed for pain and to record the type and number of pain medications they took each day for 2 weeks. Pain scores based on a 10-point Likert visual analog scale (VAS),20 were recorded at 1, 2, and 4 hours and 1 and 2 days after the operation. Patients were called 1–2 days after surgery, and pain scores were recorded. The patients were seen in the office 2 weeks after surgery. Complications were recorded up to 6 weeks according to the Clavien-Dindo classification system.21
The study was powered by desiring a 50% decrease in overnight admissions from the previously found rate of 67%. An enrollment of 132 patients was needed to demonstrate this difference with 80% power.
Continuous, normally distributed variables were summarized by using the mean and SD, with comparison between the BE and NS groups made by 2-sample t test. Continuous variables with skewed distributions were summarized by using the median and range (minimum–maximum), with comparison between groups evaluated with a Wilcoxon rank sum test. VAS pain scores were evaluated at various postoperative time points, and the change over time was compared between groups by using a mixed model approach, which accounts for the correlation of repeated measures within a subject. Categorical variables were summarized as counts, and percentages and comparison between groups was made with a 2-sample χ2 test. The average number of pain medication tablets used over the 14-day period after surgery was compared between groups by using a negative binomial regression model. All statistical analyses were conducted with SAS Version 9.4 (Cary, North Carolina, USA). Hypothesis testing was 2-sided and performed at the 5% level of significance.
RESULTS
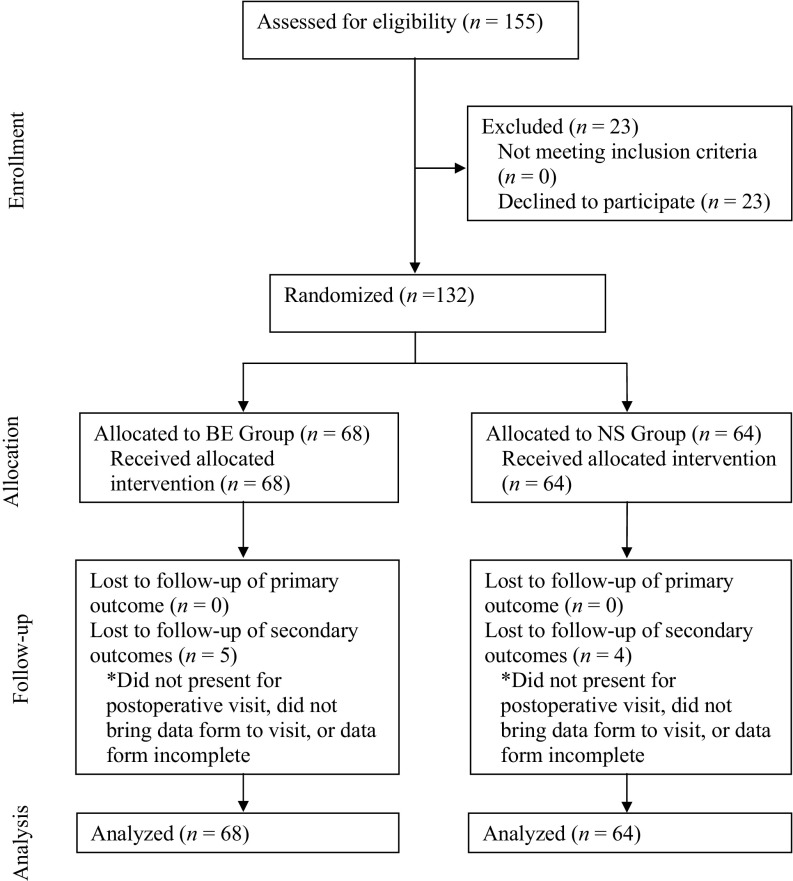
One hundred fifty-five patients met inclusion criteria and were offered enrollment (Figure 1). Of the 132 patients who consented, 68 were randomized to the BE group and 64 to the NS group. All patients received the assigned paracervical injection, and no patients were excluded after randomization.
Figure 1.
Study flow: progress of patients through the phases of the trial.
Table 1 shows the baseline characteristics of our study population; there were no significant differences between groups. The mean age was 48.4 ± 9.2 years in the BE group and 47.8 ± 9.3 years in the NS group (P = .68), and the mean body mass index (BMI) was 27.2 ± 5.7 kg/m2 in the BE group and 29.1 ± 6.9 kg/m2 in the NS group (P = .10). The population was diverse, with approximately half being nonwhite. The most common indications for hysterectomy were fibroids (67.4%), menorrhagia (65.2%), and pelvic pain (41.7%). Some patients had more than one surgical indication. Concomitant procedures (Table 2) were performed in half of the patients in each group and were most commonly adhesiolysis, unilateral or bilateral salpingooophorectomy, and sacrocervicopexy.
Table 1.
Baseline Characteristics of Study Population
| Characteristics | BE Group (n = 68) | NS Group (n = 64) |
|---|---|---|
| Age (years) | 48.4 ± 9.2 | 47.8 ± 9.3 |
| BMI (kg/m2) | 27.2 ± 5.7 | 29.1 ± 6.9 |
| Parity | ||
| 0 | 21 (31) | 24 (38) |
| 1 | 10 (15) | 10 (16) |
| 2 | 22 (32) | 19 (30) |
| ≥3 | 15 (22) | 11 (17) |
| Race | ||
| White | 36 (54) | 28 (44) |
| Black | 12 (18) | 20 (32) |
| Hispanic | 13 (19) | 10 (16) |
| Asian | 4 (6) | 3 (5) |
| Other | 2 (3) | 2 (4) |
| Surgical indication | ||
| Fibroids | 7 (10) | 9 (14) |
| Bleeding | 2 (3) | 1 (2) |
| Prolapse | 14 (21) | 8 (13) |
| Pain | 4 (6) | 1 (2) |
| Other | 0 (0) | 3 (5) |
| Fibroids and bleeding | 19 (28) | 14 (22) |
| Fibroids, bleeding, and pain | 18 (27) | 23 (36) |
| Bleeding & pain | 4 (6) | 5 (8) |
| Uterine size (weeks) | 13.7 ± 5.5 | 14.2 ± 4.6 |
| Preoperative hematocrit (%) | 36.8 ± 4.0 | 36.6 ± 4.2 |
| Admission planned* (%) | 5 (7) | 1 (2) |
All data are means ± SD or n (%). P > .05 for all characteristics.
*All planned admissions were for nonmedical indications (ie, patient anxiety, living far from hospital).
Table 2.
Perioperative Data
| Variable | BE Group (n = 68) | NS Group (n = 64) | P |
|---|---|---|---|
| Unplanned admission | 23 (34%) | 17 (27%) | .25 |
| Operating time (min)* | 89 (69–116) | 99 (73.5–117) | .39 |
| Estimated blood loss (mL)* | 100 (50–150) | 100 (100–200) | .04 |
| Mass of specimen (g)† | 377.5 (34–2000) | 443.5 (36–2670) | .49 |
| Concomitant procedure, (%)‡ | |||
| None | 34 (50) | 32 (50) | .99 |
| Adhesiolysis | 9 (13) | 12 (19) | .39 |
| USO/BSO | 10 (15) | 10 (16) | .88 |
| Sacrocervicopexy | 13 (19) | 7 (11) | .19 |
| Cystectomy | 2 (3) | 3 (5) | .67 |
| Endometriosis excision | 5 (7) | 4 (6) | .99 |
| Other | 6 (9) | 6 (9) | .99 |
| Complications (Dindo grade), % | .46 | ||
| 1 | 4 (6) | 8 (12.5) | |
| 2 | 16 (24) | 14 (22) | |
| ≥3§ | 1 (1) | 0 (0) |
All data are n (%), unless otherwise specified.
BSO, bilateral salpingo-oophorectomy; USO, unilateral salpingo-oophorectomy.
*Median [q1–q3];
†median (range).
‡Some patients had more than one concomitant procedure.
§Complication was Grade 3b. Patient developed stress incontinence requiring a midurethral sling.
The overall overnight admission rate was not significantly different between the BE and NS groups (41% vs 28%, respectively; P = .12). When excluding admissions for social reasons and not pain control, the rates were also similar between the groups (34% in the BE group and 27% in the NS group; P = .25). All of the admissions were at the request of the patients, most often for pain management. Of the 37 patients who requested admission, 20 (54%) were for pain management: 10 in the BE group and 11 in the NS group. Other reasons for elective 23-hour admission were late timing of surgery (n = 3), failed voiding trial (n = 3), weakness/dizziness (n = 2), and nausea (n = 3).
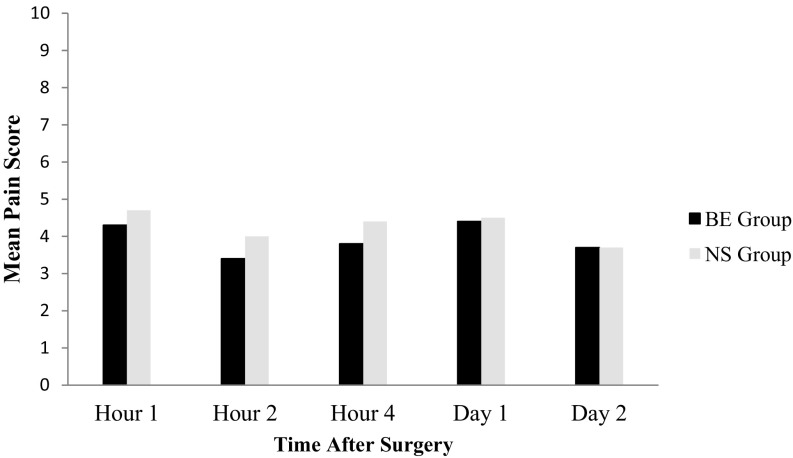
Pain scores at hours 1, 2, and 4 and on days 1 and 2 after surgery were not significantly different between the groups (Figure 2). Of the patients who ±requested admission in the BE group, the mean pain scores at 1 hour were comparable to those who were discharged (4.7 ± 2.9 vs 3.9 ± 2.2, respectively; P = .20). At 2 hours after surgery, the mean score of admitted patients was 4.3 ± 2.5 and that of discharged patients was 2.7 ± 1.8 (P = .01). In the NS group the patients who elected to stay had a mean 1-hour pain score of 5.1 ± 2.0 versus discharged patients' score of 4.5 ± 2.4 (P = .37). At 2 hours, the mean pain score was 4.5 ± 2.4 in patients choosing to stay versus 3.8 ± 2.3 (P = .34) in those who went home.
Figure 2.
Mean postoperative pain scores. Mean pain scores using a visual analog scale at hours 1, 2, and 4 and days 1 and 2 after surgery.
Pain medication use was similar in the PACU (Table 3). In the first 14 days after surgery, patients in the BE group consumed a mean of 8.48 tablets of opiates, whereas the NS group used a mean of 11.72 tablets (P = .07). The BE group took a mean of 13.14 tablets of ibuprofen compared to 11.20 in the NS group (P = .57).
Table 3.
Postoperative Pain Medication
| Variable | BE Group |
NS Group |
P | ||
|---|---|---|---|---|---|
| (n = 68) | (n = 64) | ||||
| PACU analgesic, n (%) | 68 | 64 | .92 | ||
| Fentanyl | 12 (18) | 12 (19) | |||
| Fentanyl + oxycodone | 28 (41) | 25 (39) | |||
| Fentanyl + other | 7 (10) | 4 (6) | |||
| Oxycodone | 9 (13) | 8 (13) | |||
| Oxycodone + other | 0 (0) | 1 (1) | |||
| None | 10 (15) | 10 (16) | |||
| Other | 2 (3) | 4 (6) | |||
| PACU antiemetic | 68 | 32 (47) | 64 | 24 (38) | .27 |
| PACU fentanyl dose, μg (range)* | 47 | 100 [50–100] | 41 | 100 (50–100) | .58 |
| PACU oxycodone dose, mg (range)* | 37 | 10 [5–10] | 33 | 10 (5–10) | .51 |
| Postoperative days on narcotics, n (range)† | 62 | 2 (0–11) | 59 | 3 (0–14) | .26 |
| Postoperative days on OTC analgesics, n (range)† | 62 | 2 (0–14) | 58 | 3 (0–14) | .32 |
| 14-Day postoperative number of narcotic tablets (mean ± SD)* | 63 | 8.48 ± 1.02 | 60 | 11.72 ± 1.48 | 0.07 |
| 14-Day postoperative number of OTC tablets‡ | 63 | 13.14 ± 2.59 | 60 | 11.20 ± 2.27 | 0.57 |
OTC, over-the-counter. All data are n (%), unless otherwise specified.
*Median [q1, q3];
†median (range);
‡mean ± SE (from negative binomial model).
The median number of days that patients reported taking opiates was 2 in the BE group and 3 in the NS group (P = .26). Ibuprofen was consumed for a mean of 2 days in the BE group and for 3 days in the NS group (P = .32). When each postoperative day was examined, the mean number of opiate tablets consumed was significantly lower in the BE group on days 8 and 9, with each difference amounting to less than 1 tablet. There was no significant difference in the mean number of ibuprofen tablets between groups on any day (Table 4).
Table 4.
Mean Tablets of Pain Medication Consumed on Postoperative Days 1–10
| Postoperative Day | Narcotics |
P | OTC Analgesics |
P | ||
|---|---|---|---|---|---|---|
| BE Group (n = 63) | NS Group (n = 60) | BE Group (n = 63) | NS Group (n = 60) | |||
| 1 | 3.29 | 3.66 | 0.48 | 1.21 | 0.54 | 0.15 |
| 2 | 2.17 | 2.72 | 0.28 | 1.63 | 1.13 | 0.36 |
| 3 | 1.32 | 1.73 | 0.31 | 1.97 | 1.33 | 0.26 |
| 4 | 0.71 | 1.18 | 0.14 | 1.75 | 1.78 | 0.95 |
| 5 | 0.45 | 0.67 | 0.40 | 1.10 | 1.60 | 0.28 |
| 6 | 0.25 | 0.47 | 0.16 | 1.06 | 1.32 | 0.61 |
| 7 | 0.11 | 0.35 | 0.05 | 1.02 | 0.68 | 0.40 |
| 8 | 0.06 | 0.27 | 0.03 | 0.87 | 0.55 | 0.43 |
| 9 | 0.03 | 0.22 | 0.04 | 0.65 | 0.53 | 0.76 |
| 10 | 0.05 | 0.20 | 0.06 | 0.49 | 0.47 | 0.93 |
All data are mean number of tablets from a negative binomial model.
The number of patients taking any number of opiates was similar between groups, except on day 8 (Table 5), when 5% of patients in the BE group took opiates versus 17% in the NS group (P = .03). Ibuprofen was taken by similar numbers of patients on all days.
Table 5.
Number of Patients Using Pain Medication on Postoperative Days 1–10
| Postoperative Day | Narcotics |
P | OTC Analgesics |
P | ||
|---|---|---|---|---|---|---|
| BE Group (n = 63) | NS Group (n = 60) | BE Group (n = 63) | NS Group (n = 60) | |||
| 1 | 52 (83%) | 52 (88%) | .38 | 17 (27%) | 10 (17%) | .20 |
| 2 | 43 (68%) | 39 (65%) | .70 | 24 (38%) | 18 (30%) | .34 |
| 3 | 28 (44%) | 33 (55%) | .24 | 29 (46%) | 22 (37%) | .29 |
| 4 | 19 (30%) | 26 (43%) | .13 | 28 (44%) | 26 (43%) | .90 |
| 5 | 13 (21%) | 15 (25%) | .56 | 19 (30%) | 28 (47%) | .06 |
| 6 | 12 (19%) | 13 (22%) | .72 | 15 (24%) | 24 (40%) | .05 |
| 7 | 5 (8%) | 11 (18%) | .09 | 16 (25%) | 16 (27%) | .87 |
| 8 | 3 (5%) | 10 (17%) | .03 | 12 (19%) | 12 (20%) | .89 |
| 9 | 2 (3%) | 6 (10%) | .16 | 9 (14%) | 11 (18%) | .54 |
| 10 | 3 (5%) | 7 (12%) | .20 | 9 (14%) | 10 (17%) | .71 |
All data are n (%). OTC, over-the-counter.
The median EBL of the BE group was 100 mL (interquartile range, 50–150 mL) and 100 mL in the NS group (interquartile range, 100–200 mL), which was statistically significant (P = .04). Seven patients had an EBL greater than 500 mL (5.3%), 4 in the BE group and 3 in the NS group. No patient required a blood transfusion.
Complication rates were similar between groups (Table 2). Most complications were Dindo grade 1 or 2, including urinary tract infection, incisional infection, and urinary retention. During surgery, there was a small bowel mesenteric hematoma caused by the Veress needle that did not require surgical management in the NS group and a skin laceration from the morcellator in the BE group. There were 3 cases (2.3%) of cervical infection, 2 in the BE group and 1 in the NS group. One patient in the BE group had a seizure of unknown etiology on postoperative day 2 that required an emergency department visit but not admission. There was 1 emergency department visit for nausea, vomiting, and headache in a patient in the BE group and no readmissions in either group. There were no conversions to laparotomy; however, 1 patient had an extension of the umbilical incision to facilitate removal of an ovarian fibrothecoma (NS group).
DISCUSSION
We did not find a significant difference in the admission rate of patients who received the paracervical block compared to those who received placebo. To achieve statistical power in our study, we used a 67% admission rate after laparoscopic supracervical hysterectomy. This number is obviously high compared with current admission rates but was the historical rate at our institution before our study The unplanned admission rates of 34% in the BE group and 27% in the NS group were both, in fact, substantially lower than the prestudy rate. This reduction in admissions may reflect an ever-increasing acceptance among patients of same-day discharge in addition to changes in counseling secondary to increased confidence in the safety of same-day discharge. Our overall same-day discharge is less than that in 2 recent studies from California that reported rates greater than 91% for laparoscopic supracervical hysterectomy.5,6 This may reflect differences in acceptance of same-day discharge by patients in the Northeast compared to the those on the West Coast or differences in counseling by providers, which can influence whether a patient is motivated to be discharged.22 Although it is obviously important to decrease pain medication use after surgery, the ultimate goal is earlier discharge, and this was therefore chosen as the primary outcome. Although patients have the option to stay 23 hours after surgery, they were all counseled that they were expected to go home the same day. Although the decision to stay in the hospital may be multifactorial and therefore confound the results, its importance made it the primary outcome.
The postoperative pain scores in our population were similar to what has been reported.23 More than half of patients who elected to be admitted overnight did so for pain management, despite both groups having similar pain scores and using the same amount of opiates in the PACU. This study did not have sufficient power to show a difference in pain scores; a difference might be found in a larger sample size.
Patients in both groups used opiates for a median duration of 2–3 days which was 1–2 days less than was reported in another study.23 This result provides support for the fast recovery time after laparoscopic supracervical hysterectomy, which is valuable in counseling patients regarding what to expect after surgery.
The median EBL was 100 mL in both groups with a significant P-value, because the statistical analysis of the distribution of data took into account the first and third quartile values when calculating the median. The clinical value of this difference is minimal. The reduced EBL was probably due to the epinephrine, as vasopressin injected before vaginal hysterectomy has been shown to reduce blood loss.24
There were no detected complications attributable to the use of bupivacaine or epinephrine. Our study had a higher complication rate than has been published, consisting mostly of minor complications.1 This could be explained by a more thorough monitoring of minor complications. There were no readmissions in the 6 weeks after surgery, which is lower than the reported rate.6
Strengths of the study include the randomized, double-blind, placebo-controlled design and a large sample size with a diverse patient population. We had only 9 patients with missing postoperative pain and medication data: 5 in the BE group and 4 in the NS group. Having a single attending surgeon perform all the surgeries and the paracervical injections maintained consistency; however, this is a limitation as the outcome is less generalizable to other surgeons. Also, these results may not apply to total hysterectomies. We allowed concomitant procedures such as sacrocervicopexy at the time of hysterectomy, as the randomization process should distribute these procedures equally between the BE and NS groups, and the additional procedures should not affect our outcomes. The final limitation of the study is that the circulating nurse was not blinded to the treatment. It was cost prohibitive to the study to get the study injection from the research pharmacy. The circulating nurse had no further interaction with the patient after leaving the operating room, and we believe that this would have no impact on our results.
The paracervical block of bupivacaine with epinephrine administered before laparoscopic supracervical hysterectomy was not effective at decreasing hospital admissions and did not have a clinically significant impact on postoperative pain, pain medication consumption, or decreased blood loss.
Contributor Information
Rachel L. Barr Grzesh, Department of Obstetrics, Gynecology and Reproductive Science, Division of Gynecology.
Alejandro D. Treszezamsky, Department of Obstetrics, Gynecology and Reproductive Science, Division of Gynecology.
Suzanne S. Fenske, Department of Obstetrics, Gynecology and Reproductive Science, Division of Gynecology.
Lauren G. Rascoff, Department of Obstetrics, Gynecology and Reproductive Science, Division of Gynecology.
Erin L. Moshier, Division of Biostatistics, Department of Preventive Medicine, Icahn School of Medicine at Mount Sinai, New York, New York, USA..
Charles Ascher-Walsh, Department of Obstetrics, Gynecology and Reproductive Science, Division of Gynecology.
References:
- 1. Rosero EB, Kho KA, Joshi GP, Giesecke M, Schaffer JI. Comparison of robotic and laparoscopic hysterectomy for benign gynecologic disease. Obstet Gynecol. 2013;122:778–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Thiel J, Gamelin A. Outpatient total laparoscopic hysterectomy. J Am Assoc Gynecol Laparosc. 2003;10:481–483. [DOI] [PubMed] [Google Scholar]
- 3. Lee SJ, Calderon B, Gardner GJ, et al. The feasibility and safety of same-day discharge after robotic-assisted hysterectomy alone or with other procedures for benign and malignant indications. Gynecol Oncol. 2014;133:552–555. [DOI] [PubMed] [Google Scholar]
- 4. Schiavone MB, Herzog TJ, Ananth CV, et al. Feasibility and economic impact of same-day discharge for women who undergo laparoscopic hysterectomy. Am J Obstet Gynecol. 2012;207:382.e1–e9. [DOI] [PubMed] [Google Scholar]
- 5. Alperin M, Kivnick S, Poon KYT. Outpatient laparoscopic hysterectomy for large uteri. J Minim Invasive Gynecol. 2012;19:689–694. [DOI] [PubMed] [Google Scholar]
- 6. Perron-Burdick M, Yamamoto M, Zaritsky E. Same-day discharge after laparoscopic hysterectomy. Obstet Gynecol. 2011;117:1136–1141. [DOI] [PubMed] [Google Scholar]
- 7. Morrison JE, Jr, Jacobs VR. Outpatient laparoscopic hysterectomy in a rural ambulatory surgery center. J Am Assoc Gynecol Laparosc. 2004;11:359–364. [DOI] [PubMed] [Google Scholar]
- 8. Lieng M, Istre O, Langebrekke A, Jungersen M, Busund B. Outpatient laparoscopic supracervical hysterectomy with assistance of the lap loop. J Minim Invasive Gynecol. 2005;12:290–294. [DOI] [PubMed] [Google Scholar]
- 9. Kelly DJ, Ahmad M, Brull SJ. Preemptive analgesia II: recent advances and current trends. Can J Anesth. 2011;48:1091–1101. [DOI] [PubMed] [Google Scholar]
- 10. Kissin I. Preemptive analgesia. Anesthesiology. 2000;93:1138–1143. [DOI] [PubMed] [Google Scholar]
- 11. Ke RW, Portera SG, Bagous W, Lincoln SR. A randomized, double-blinded trial of preemptive analgesia in laparoscopy. Obstet Gynecol. 1998;92:972–975. [DOI] [PubMed] [Google Scholar]
- 12. Alessandri F, Lijoi D, Mistrangelo E, Nicoleti A, Ragni N. Effect of presurgical local infiltration of levobupivacaine in the surgical field on postsurgical wound pain in laparoscopic gynecological surgery. Acta Obstetr Gynecol. 2006;85:844–849. [DOI] [PubMed] [Google Scholar]
- 13. Ghezzi F, Cromi A, Bergamini V, et al. Preemptive port site local anesthesia in gynecologic laparoscopy: a randomized, controlled trial. J Minim Invasive Gynecol. 2005;12:210–215. [DOI] [PubMed] [Google Scholar]
- 14. Gupta N, Dadhwal V, Mittal S. Combined intraperitoneal instillation and port site infiltration of local anaesthetic (bupivacaine) for postoperative analgesia in women undergoing daycare diagnostic gynaecological laparoscopy. Eur J Obstet Gynecol Reprod Biol. 2010;161:109–110. [DOI] [PubMed] [Google Scholar]
- 15. Malhotra N, Chanana C, Roy KK, Kumar S, Rewari V, Sharma JB. To compare the efficacy of two doses of intraperitoneal bupivacaine for pain relief after operative laparoscopy in gynecology. Arch Gynecol Obstet. 2007;276:323–326. [DOI] [PubMed] [Google Scholar]
- 16. Renner R-M, Nichols MD, Jensen JT, Li H, Edelman AB. Paracervical block for pain control in first-trimester surgical abortion. Obstet Gynecol. 2012;119:1030–1037. [DOI] [PubMed] [Google Scholar]
- 17. Long JB, Eiland RJ, Hentz JG, et al. Randomized trial of preemptive local analgesia in vaginal surgery. Int Urogynecol J. 2009;20:5–10. [DOI] [PubMed] [Google Scholar]
- 18. O'Neal MG, Beste T, Shackelford DP. Utility of preemptive local analgesia in vaginal hysterectomy. Am J Obstet Gynecol. 2003;189:1539–1542. [DOI] [PubMed] [Google Scholar]
- 19. Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010;152:726–732. [DOI] [PubMed] [Google Scholar]
- 20. Bieri D, Reeve RA, Champion GD, Addicoat L, Ziegler JB. The Faces Pain Scale for the self-assessment of the severity of pain experienced by children: development, initial validation, and preliminary investigation for ratio scale properties. Pain. 1990;41:139–150. [DOI] [PubMed] [Google Scholar]
- 21. Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sutton C. Past, present and future of hysterectomy. J Minim Invasive Gynecol. 2010;17:421–435. [DOI] [PubMed] [Google Scholar]
- 23. El Hachem L, Acholonu UC, Jr, Nezhat FR. Postoperative pain and recovery after conventional laparoscopy compared with robotically assisted laparoscopy. Obstet Gynecol. 2013;121:547–553. [DOI] [PubMed] [Google Scholar]
- 24. Ascher-Walsh CJ, Capes T, Smith J, Michels A. Cervical vasopressin compared with no premedication and blood loss during vaginal hysterectomy: a randomized controlled trial. Obstet Gynecol. 2009;113:313–318. [DOI] [PubMed] [Google Scholar]