Abstract
There has been a remarkable improvement in the treatment strategy of secundum atrial septal defect (ASD) over the last few decades. Indebted to the improvement in device technology and procedural techniques, transcatheter closure of ASD is currently accepted as the treatment of choice in most patients with secundum ASD. Recent generation devices enable easy and safe deployment of device with the properties of adequate flexibility, re-capturability and repositioning. Use of biocompatible materials with improved device design and refined equipment finish may promote re-endothelialization and reduce potential damage to nearby structures. Most of currently available devices show excellent efficacy and comparable outcome with its own advantages and disadvantages. In addition to improvement of device properties and performance, there has been distinct improvement in procedural technique from numerous experiences of device closure of ASD. Nowadays there are well established principles regarding patient selection, pre-procedural evaluation, step-by-step details of procedure as well as post-procedural follow-up. However, an operator may encounter pitfalls in closing complex lesions such as large defect, rim deficiencies and multiple defects, so every operator has to be familiar with each available device, general principle as well as special issues for complex lesions.
Keywords: Atrial septal defect (ASD), device closure, septal occluder device
Introduction
Atrial septal defect (ASD) is one of the most common congenital heart diseases (CHDs) and accounts for the most common CHD in adults (1). There has been a shift of paradigm for therapeutic strategy of ASD over the last decades. Techniques and devices for transcatheter treatment have been evolved and refined; as a result, device closure of ASD is currently accepted as the treatment of choice in most patients with secundum ASD, showing excellent efficacy as well as lower complication rate comparing to surgery (2,3).
Extensive experiences have verified safety and usefulness of the procedure, and established general principle for device closure of ASD including patient selection, peri-procedural assessment as well as procedural technique with various measures to prevent potential complications. However, unanticipated difficulties and un-negligible risks may be encountered during this “usually straightforward” procedure, and every effort has to be made to promote the efficacy and safety of the procedure on the basis of accurate knowledge for procedural principles, solutions for specific problems as well as characteristic features of available devices.
Principles and issues of device closure of ASD
Patient selection is an important initial step for a successful treatment. Procedure in the catheterization laboratory may be summarized stepwise; (I) hemodynamic study and assessment of morphologic characteristics of the defect; (II) establishment of procedural strategy including procedure-guiding modality and equipment to be used; (III) selection of optimal type and size of device; (IV) device implantation with cautions for potential complications including air embolism, damage to cardiac/vascular structures; (V) post-implantation assessment of the final result. After a successful procedure, appropriate patient education and follow-up are also essential parts of the treatment. Details and special considerations for each step of the procedure have well been described previously (4). There are individual issues which are often in debate including procedure-guiding modalities, sizing the defect, and closing complex defects.
Issues on imaging guidance and defect sizing
Although there have been studies reporting device closure guided only by either fluoroscopy or echocardiography (5-7), it is generally recommended to perform the procedure under both fluoroscopic and echocardiographic guidance. For echocardiographic guidance, transesophageal echocardiography (TEE) has long been the standard modality for ASD closure. However, intracardiac echocardiography (ICE) is gradually replacing the role of TEE recently. Transthoracic echocardiography (TTE) may also be used especially in patients with good windows for echocardiography such as small children (8).
There has been debate on the necessity of balloon sizing for selection of device size. Balloon sizing may be skipped in suitable defects with sufficient surrounding rims (9); however, it has long been regarded as an essential step of the procedure (10). Indeed, balloon sizing may provide more information than averaged size of the defect including compliance of surrounding rims and presence of additional defect.
While the balloon stretched diameter or balloon occlusive diameter were used in balloon sizing in the past, currently stop flow diameter (SFD) is recommended as the standard measurement to avoid oversizing (11). In self-centering devices such as the Amplatzer Septal Occluder (ASO) (St. Jude Medical, St. Paul, MN, USA), the recommended device size is the same or slightly larger (<2 mm) than the SFD. Nevertheless, the selection for device size should be individualized considering deficiency of rims, spatial relationship with nearby cardiac structures and size of the heart. In cases with aortic rim deficiency, the usual recommendation is to avoid an “oversized” device because of the potential risk of erosion (11). On the other hand, in cases with inferior vena cava (IVC) rim deficiency with higher risk of device embolization, use of an “undersized” device should be avoided. In case of using a non-self-centering device such as the Gore Septal Occluder (GSO) (WL Gore & Associates, Inc., Flagstaff, AZ, USA), a device twice the size of the defect is recommended (12), and the GSO is not recommended for defects >18 mm (13).
Complex lesions
Large defect
Large size of the defect may be the most common cause of difficulties in ASD closure using a device. The main problems are prolapse of left atrial (LA) disk of the device into the right atrium (RA) before proper positioning in the septum (14) and difficulty in sizing the defect. Device size is frequently selected by estimation rather than measurement of balloon diameter due to non-visualization of the whole defect in a single echocardiographic plane, difficulty in stabilization of the sizing balloon (melon-seeding or milking) and unavailability of sizing balloon larger than 34 mm.
Various modified implantation techniques have been suggested to overcome the problem with LA disk prolapse (Table 1). An operator should be familiar with his/her own technique to overcome this problem. The balloon-assisted technique may be helpful even in cases when other methods failed.
Table 1. Various technical modifications to prevent left atrial disk prolapse during device positioning.
| 1. Waist deployment in LA |
| 2. Rotation of sheath in LA (15) |
| 3. Bending (pre-shaping) (15)/cutting of sheath tip (16) |
| 4. RUPV technique (14,17) |
| Hypomochlion technique, LA roof technique |
| 5. LUPV technique (14) |
| 6. Stiff sheath (dilator) technique (18) |
| 7. Use of Hausdorf-Lock sheath (14) |
| 8. Balloon-assisted technique (19-21) |
| 9. Straight side-hole delivery sheath technique (22) |
| 10. Steerable sheath technique (23) |
| 11. Use of JR coronary guiding catheter (24) |
LA, left atrium; LUPV, left pulmonary vein; RUPV, right upper pulmonary vein; JR, Judkin’s right.
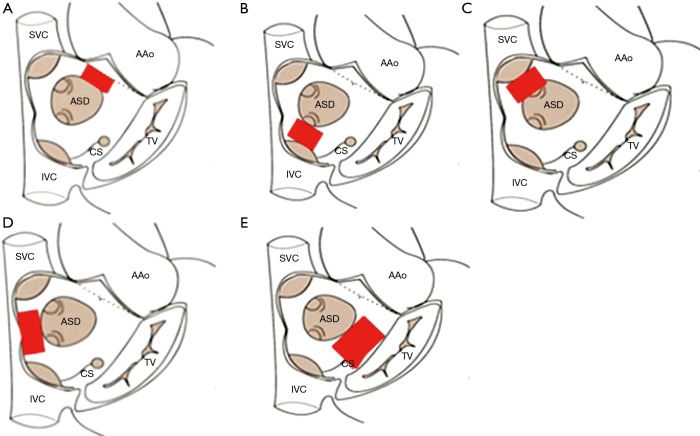
Rim deficiencies (Figure 1A,B,C,D,E)
Figure 1.
The locations of rim deficiencies: (A) aortic rim, (B) IVC rim, (C) SVC rim deficiency, (D) posterior rim, (E) atrioventricular valve rim. SVC, superior vena cava; IVC, inferior vena cava; ASD, atrial septal defect; CS, coronary sinus; AAo, ascending aorta; TV, tricuspid valve.
Deficiency in the surrounding rim(s) is frequently associated with large defects, and may potentially increase the risk of complications such as device embolization, erosion and encroachment of device onto nearby cardiac structures.
Aortic rim (antero-superior rim, Figure 1A) deficiency is most common rim deficiency (25) and device implantation is frequently interfered by LA disk prolapse. Erosion risk is higher in aortic rim deficiency as well as device oversizing (11), thus device selection has to be refrained from undue oversizing.
IVC rim (posteroinferior rim, Figure 1B) deficiency is second most common among rim deficiencies and associated with higher risk of device embolization (26). In case with this rim deficiency, under-sizing of the device may further increase the risk of device embolization, and should be avoided. It is difficult to visualize IVC rim with TEE guidance, so ICE is preferable imaging modality in patients with IVC rim deficiency (27); however, so called ‘modified retroflexed view’ may be helpful to visualize IVC rim with TEE guidance (28).
Superior vena cava (SVC) rim (posterosuperior rim, Figure 1C) deficiency is a rare condition and may interfere with device positioning (29). When the rim deficiency is extended from SVC rim to aortic rim, this indicates the defect is located superiorly in the atrial roof and may carry higher risk of erosion (11,30).
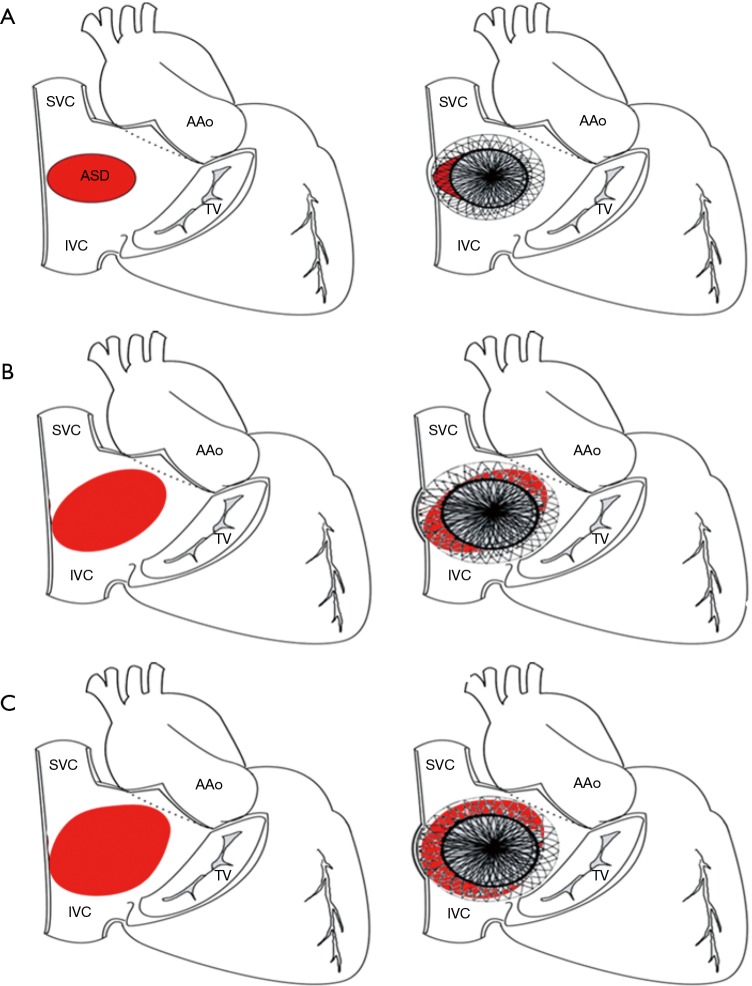
In case with posterior rim (Figure 1D) deficiency, the feasibility of device closure may be decided by the extent of rim deficiency (Figure 2). In the presence of rim deficiency in large area from IVC to posterior rim, the risk of device embolization is very high and this condition may preclude device closure.
Figure 2.
Illustration of feasible (A), borderline (B) and unfeasible (C) defect for device closure in posterior rim deficiency. For the defects with posterior rim deficiency, the extent of rim deficiency determines feasibility of device closure, so the clear anatomic definition is very important. SVC, superior vena cava; IVC, inferior vena cava; AAo, ascending aorta; TV, tricuspid valve.
In atrioventricular valve rim (Figure 1E) deficiency, encroachment of device onto the mitral and/or tricuspid valve is a potential problem. This is a concern especially in infants and young children because of the inherent design of Amplatzer-type devices which have a relatively larger disk-rim width in smaller devices. In case of device encroachment onto the valve, it is generally recommended not to implant a device. There is an extremely rare documented case of erosion on mitral valve (31).
Multiple defects
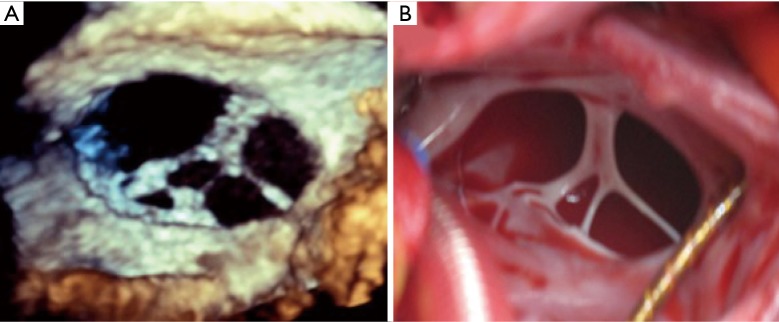
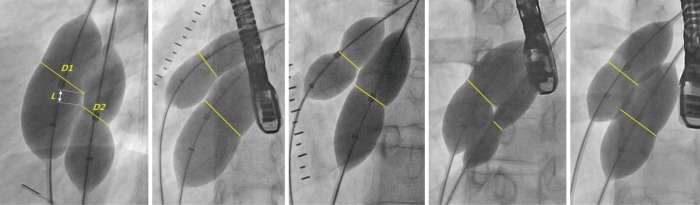
There are many challenges or considering factors when planning closure of multiple ASDs, including numbers/size of the defect, location/spatial relationship between the defects, properties of supporting rims or intervening septum as well as presence of septal aneurysm. Ultimately, understanding the accurate anatomy and properties of surrounding/intervening rims of multiple defects is the cornerstone of successful device closure. To overcome these problems, proper use of real time 3-dimensional (RT3D) echocardiography may be helpful (32,33). RT3D echocardiography enables visualization of the wide ranged septum in a single view in the echocardiography and provides instantaneous understanding of the anatomy as well as identification of complex morphology and spatial relationship between multiple defects (Figure 3). Temporary balloon occlusion test may also be useful to investigate compliance of surrounding rims and intervening septum, as well as to predict changes of the defects and rims after device implantation. Also, a careful observation of fluoroscopic images with balloon sizing may provide additional information on the spatial relationship between the defects and intervening septum (Figure 4). In case of device closure of multiple defects using multiple devices, the optimal combination of devices based on the comprehensive information from RT3D echocardiography and balloon occlusion test is required to prevent unfavorable interference between multiple devices (Figure 5). Usually, a small additional defect adjacent to a larger defect (<7 mm in distance) can also be closed by implantation of a single device in the major defect (34). When the additional defect is also sizable or defects are in distance each other, use of multiple devices is required. For multi-fenestrated defects with a large septal aneurysm, patch-like closure using a non-self-centering device may be a good option (Figure 6).
Figure 3.
Real time 3-dimensional (RT3D) echocardiography is very useful to assess morphologic characteristics for multiple defects. Note the similarity between the realistic image from RT3D echocardiography (A) and actual image of the defect from the surgical field (B).
Figure 4.
Careful observation of fluoroscopic image with balloon sizing may provide additional anatomic information on the defects and intervening septum.
Figure 5.
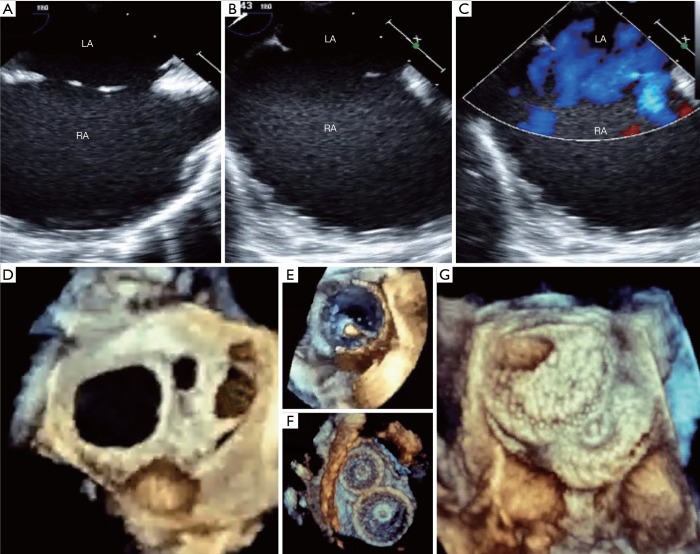
Advantages of real time 3-dimensional (RT3D) transesophageal echocardiography (TEE) guidance in device closure of multiple ASDs. True anatomy of multiple defects is difficult to understand by 2-dimensional (2D) TEE images even in multiple views (A,B) with color flow Doppler (C), however the anatomic characteristics including number of the defect, shape/size of each defect and spatial relationship between the defects are clearly shown on RT3D image (D). RT3D echocardiography also provides excellent images during balloon sizing (E) and post-assessment of the device position (F,G). LA, left atrium; RA, right atrium.
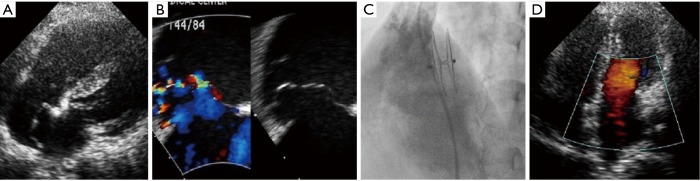
Figure 6.
Patch-like closure using non-self-centering device is a good option for multi-fenestrated defects with a large septal aneurysm. Transthoracic echocardiography (A) and transesophageal echocardiography (B) shows multi-fenestrated defects with a large septal aneurysm. A 35mm cribriform device (C) was implanted in the center hole of the aneurysm instead of larger eccentric hole to achieve a complete coverage of base of the septal aneurysm. Follow-up echocardiography shows a patch-like closure of defects and septal aneurysm (D).
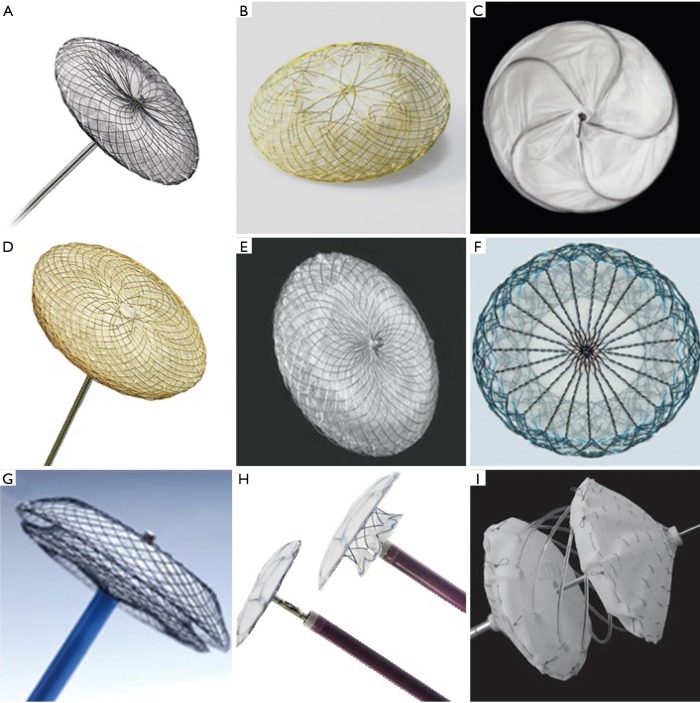
Currently available devices for ASD closure (Figure 7)
Figure 7.
Currently available devices for atrial septal defect closure. (A) Amplatzer Septal Occluder; (B) Occlutech Figulla Flex II device; (C) Gore Cardioform Septal Occluder; (D) Cocoon Septal Occluder; (E) CeraFlex ASD device; (F) Nit Occlud ASD-R device; (G) Cardi-O-Fix Septal Occluder; (H) Ultracept II ASD Occluder and (I) Carag Bioresorbable Septal occluder.
ASO (Figure 7A, Table 2)
Table 2. Comparison of commonly used devices.
| Devices | Approval/distribution/No. of shipment or implantation | Advantages | Disadvantages | Considerations |
|---|---|---|---|---|
| Amplatzer Septal Occluder | FDA/Worldwide/>500,000 | General familiarity | Most of the reported cases of erosion | Adverse events have been extensively investigated |
| Largest experience with accumulated data including long-term safety | Nickel release | Non-self-centering version is also available (cribriform devices) | ||
| Widest range of sizes | Stiff device-cable coupling—device jumping on release | |||
| Occlutech Figulla Flex II ASD Occluder | CE mark/>80 countries/>50,000 including previous generation devices | Soft and flexible braiding —conforms to the defect —may reduce erosion risk |
Fewer available sizes | Usually regarded as a softer device than ASO |
| Larger delivery sheaths | Non-self-centering version is also available (uniform devices) | |||
| Less experience and data—lack of long term data | Order-made fenestrated device is available | |||
| Flexible delivery system: 50°angulation + shapeable cable —less tension and jump on release |
||||
| Less material, no hub on LA disk smaller RA hub | ||||
| Titanium oxide coated surface | ||||
| Gore Cardioform Septal Occluder | FDA (CE mark)/15 countries/>8,000; >33,000 including HSO | Less exposure of metal to blood stream | Cannot close >18 mm defect | Non-self-centering device |
| Softer device with less metal content; not likely cause erosion | Only 4 available sizes relatively larger delivery system for smaller defects | |||
| Thinner device profile | Rigid coupling between device and control catheter before unlocking | |||
| Good alignment to the septum after locking of occluder (retrieval is still possible if mis-positioned) | Less experience and data—lack of long term data | |||
| Cocoon Septal Occluder | CE mark/22 countries/>40,000 | Nano-platinum coated surface —prevent nickel release —enhance radio-opacity and biocompatibility |
Stiff device-cable coupling—device jumping on release | Usually regarded as a softer device than ASO |
| Softer and lighter device—may reduce erosion risk | Fewer available sizes | |||
| Larger delivery sheaths | ||||
| Less experience and data—lack of long term data | ||||
| CeraFlex ASD Occluder | CE mark/>50 countries/>170,000 including previous generations | Titanium nitride coated surface | Fewer available sizes | Usually regarded as a softer device than ASO |
| Available largest device —up to 42 mm | Larger delivery catheters | |||
| Less experience and data—lack of long term data |
ASO, Amplatzer septal occluder; CE, Conformité Européenne; FDA, Food and Drug Administration.
The ASO is the first self-expanding double-disk device with central connecting waist composed of nitinol-wire-mesh. The disks and waist were sewn with a Dacron patch to promote complete occlusion and endothelialization. The device allowed easy and straightforward deployment due to its self-centering, repositionable, and recapturable characteristics. The ASO solved many limitations of previous devices such as the non-negligible rate of residual shunt and frame fracture, and is regarded as a prototype device for many newer devices. The device size is determined by the waist size; there are 27 device sizes from 4 to 40 mm (in 1-mm increments between 4 to 20 mm and 2-mm increments between 20 to 40 mm). The corresponded delivery sheath sizes range from 6 to 12 French (Fr).
Initial study showed excellent success rate of 95.7% and low major and total adverse effect of 1.6% and 7.2% respectively (3). The subsequent MAGIC study and IMPACT registry reported compatible success and complication (35,36). Largest experience has been accumulated in ASO, but the risk of erosion has been issued (37) since it can be fatal and may occur delayed. The exact rate is still unclear, but the estimated rate is about 0.1 to 0.3 (38). Reported risk factors include aortic rim deficiency, superiorly located ASD, over-sizing of device, septal malalignment, dynamic ASD and lower patient weight: device size ratio (11,30,37-40), and the most probable mechanism is abrasion due to seesaw movement according to the cardiac cycle (37), although the exact mechanism is unclear or not known.
Recommendations to avoid erosion should be followed (11) and comprehensive evaluation by echocardiography during follow-up is warranted (30,40).
The ASO “cribriform” is a specially designed non-self-centering device for multi-fenestrated defects with 4 available sizes from 18 to 40 mm.
Occlutech Figulla Flex II ASD Occluder (Figure 7B)
Figulla Flex II ASD Occluder (FSO, Occlutech GmbH, Jena, Germany) is the third generation Occlutech device for ASD closure with a flexible titanium-oxide coated nitinol-mesh and double-disk design similar to ASO. FSO has minimized metal contents especially in the LA disk and no clamping hub on the LA disk, which may provide more flexible and less traumatic feature. The FSO has a distinct release mechanism resembling a bioptome which enables flexible movement between the device and delivery cable. The delivery cable is also shapeable for a better alignment between the device and septum.
There are 20 device size options from 4 to 40 mm (1–1.5-mm increments between 4 and 21 mm, 3-mm increments between 21 and 39 mm, and 40 mm). Retrospective comparison studies showed a compatible efficacy and safety comparing to ASO (41,42). The largest study with FSO, the IRFACODE study, showed a 98% success rate in 1395 patients and a 97.3% complete closure rate at 1 year (43). The major complication rate was minimal (n=8, <1%). Erosion has not yet been reported with this device. The disadvantages are its relatively limited size options (20 vs. 27 sizes in ASO) and requirement of a slightly larger delivery sheath than in ASO devices.
A fenestrated device for closure of ASD with pulmonary hypertension or risk of masked left ventricular restriction is available on an order-made basis.
GSO (Figure 7C)
The GSO is a non-self-centering double disk device composed of platinum filled nitinol wire framework covered with an expanded polytetrafluoroethylene (ePTFE) membrane to promote rapid endothelialization. The GSO is preloaded as a package of the device and whole delivery system. The delivery system has improved for easier delivery and position compared to that of the previous Helex Septal Occluder (HSO). There are 4 device sizes from 15 to 30 mm with 5-mm increments. It is generally recommended that the device size should be more than twice the defect size and the GSO is not suitable for defects over 18 mm due to the non-self-centering feature. Owing to its flexibility with minimal metal content which may prevent erosion, the device is preferred to close smaller defects especially with aortic rim deficiency or those in small children (44). Clinical studies verified efficacy and safety of this device in closing ASDs with various morphologies such as aortic rim deficiency, septal aneurysm and multiple defects in selected patients with feasible anatomy (12,13,45).
The Gore Cardioform ASD Occluder (GAO) is a self-centering version of GSO which consists of a helical nitinol-wire frame covered with ePTFE to treat larger ASDs. The available sizes are 27, 32, 37, 44, and 48 mm and designed to treat defects from 8 to 35 mm. Although this device is not commercially available yet, the initial clinical result showed the safety and efficacy of the GAO (46). The risk factor for procedural failure in GAO implantation was a larger defect size, especially a size larger than 27 mm by balloon sizing.
CeraFlex ASD Occluder (Figure 7D)
CeraFlex (LifeTech Scientific Co., Shenzhen, China), the 4th generation ASD device from LifeTech, is a nitinol-wire-mesh device coated with titanium nitride. This device is preloaded as a package and has a similar feature to other nitinol-wire-mesh devices such as self-expanding property and double-disk design with central waist. Ceraflex has couple of shared features with FSO; a coated surface of nitinol-wire, flexible connection between the device and delivery cable, and no hub on LA disk. A total of 19 sizes are available from 6 to 42 mm with 2-mm increments, and the delivery sheath sizes range from 8 to 14 Fr. A comparative study between Ceraflex and ASO showed comparable success rate, safety and efficacy (47). The disadvantages are its relatively limited size options (19 vs. 27 sizes in ASO) and the requirement of a slightly larger delivery sheath than with ASO devices.
Cocoon Septal Occluder (Figure 7E)
The Cocoon Septal Occluder (Vascular Innovations Co., Nonthaburi, Thailand) is a self-expanding double-disk device consists of a nano-platinum coated nitinol device filled with polypropylene fabric. The device is quite similar to ASO in terms of device design except for the nano-platinum-coated surface which prevents nickel release to the blood stream (48), promotes biocompatibility and enhances radio-opacity on fluoroscopy. There are 17 device options ranging from 8 to 40 mm with 2-mm increments and the delivery sheath sizes range from 7 to 14 Fr. European multicenter study reported an excellent result with procedural success rate of 100% and no complication in 92 patients (49). This device has been described as softest and lightest currently available device with less metal-to-septum ratio than other devices (49). The disadvantages are its relatively limited size options (17 vs. 27 sizes in ASO) and the requirement of a slightly larger delivery sheath than with ASO devices.
Nit-Occlud ASD-R (Figure 7F)
The Nit-Occlud ASD-R (NOA-R) (pfm Medical, Cologne, Germany) is a double-disk, self-expandable, self-centering device; however, the device characteristics are quite different from other nitrol-mesh devices. NOA-R has reduced amount of metal on the left atrial disk without clamping or screwing hub on either side of the atrial disks and has a “reverse configuration” of the single-nitinol-layer on the LA disk (the “R” on the product name indicates this). These characteristics may allow more flexible and conformable device positioning on the septum. The release mechanism is unique as it is “snare-like,” which includes a central locking wire and a pusher with a distal wire noose (50). A total of 12 sizes are available from 8 to 30 mm with 2-mm increments, and the delivery sheath sizes range from 8 to 14 Fr.
A multicenter study showed a 98.6% (73/74 patients) success rate with one case of complete heart block (50). Device retrieval is more difficult because of the no-hub design (50); however, retrieval of the device may be feasible using a special technique (snare and wire technique) with an oversized sheath (51). Two cases of erosion including one lethal case were reported (52,53). The disadvantages (are its relatively limited size options (12 vs. 27 sizes in ASO), and the requirement of a slightly larger delivery sheath than with ASO devices and inability to close larger defects.
Cardi-O-Fix Septal Occluder (Figure 7G)
The Cardi-O-Fix septal occluder (Starway Medical Technology, Beijing, China) is a self expandible double disk design device consists of nitinol wire mesh filled with polyester fabric sewn to waist and each disk. This device is structurally similar to the ASD, however this device has two different versions of products with or without clamping hub on the LA disk. A total of 27 sizes are available from 4 to 40 mm (1-mm increment between 4 to 20 mm and 2-mm increment between 20 to 40 mm), and the delivery sheath sizes range from 7 to 14 Fr. A comparative study between this device and ASO showed comparable outcome and lower cost with Cardi-O-Fix device (US$ 4,100 vs. US$ 5,900, P<0.001) (54). The disadvantages may include less experience/data with this device and the requirement of a slightly larger delivery sheath than with ASO.
Ultracept II ASD Occluder (Figure 7H)
The last generation of CARDIA ASD closure device, the Ultracept II ASD Occluder (Cardia, Eagan, MN, USA) is a double-round disk, self-centering, low profile device. It has a nitinol frame with a polyvinyl alcohol (PVA) coating to reduce thrombus formation. A total of 15 sizes are available from 6 to 34 mm with 2-mm increments, and the delivery sheath sizes range from 9 to 11 Fr. Several cases of PVA-membrane perforation or degradation were reported (55-57), which were also reported with the previous generation device (58). Despite comprehensive investigations on the PVA membrane, the mechanism of degradation has not been identified. Some authors emphasized that the interventionist should be aware of this rare complication (57).
Carag Bioresorbable Septal occluder (Figure 7I)
Carag Bioresorbable Septal Occluder (CBRO) (CARAG AG, Baar, Switzerland) is a self-centering, double disk device without any metal framework, composed of poly lactic-co-glycolic acid (59). Endothelialization of the device seems to be completed within 3 months, while the device usually starts to be resorbed after 6 months and completely resolved within 2 years. CBRO has 3 size options: small for 4–12 mm defects, intermediate for 13–20 mm, and large for 21–25 mm. Preliminary data showed an excellent efficacy of CBRO with successful outcome in all ten patients, 4 with ASD and 6 with patent foramen ovale (60).
Conclusions
Transcatheter closure of secundum ASD is the treatment of choice in most patients with feasible anatomy. An operator should be familiar with principles of the procedure, solutions for procedural difficulty, cautions to avoid complications and detailed knowledge on the available equipments to promote safety and efficacy of this versatile therapy.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol 2002;39:1890-900. 10.1016/S0735-1097(02)01886-7 [DOI] [PubMed] [Google Scholar]
- 2.Cowley CG, Lloyd TR, Bove EL, et al. Comparison of results of closure of secundum atrial septal defect by surgery versus Amplatzer septal occluder. Am J Cardiol 2001;88:589-91. 10.1016/S0002-9149(01)01750-7 [DOI] [PubMed] [Google Scholar]
- 3.Du ZD, Hijazi ZM, Kleinman CS, et al. Comparison between transcatheter and surgical closure of secundum atrial septal defect in children and adults: results of a multicenter nonrandomized trial. J Am Coll Cardiol 2002;39:1836-44. 10.1016/S0735-1097(02)01862-4 [DOI] [PubMed] [Google Scholar]
- 4.Al-Qbandi M, Cao QL, Hijazi ZM. Atrial septal defect: Amplazter-type ASD Occluders. In: Sievert H, Qureshi SA, Wilson N, et al. editors. Interventions in structural, valvular, and congenital heart disease. 2nd ed. CRC Press, 2015:437-47. [Google Scholar]
- 5.Praz F, Wahl A, Schmutz M, et al. Safety, feasibility, and long-term results of percutaneous closure of atrial septal defects using the amplatzer septal occluder without periprocedural echocardiography. J Invasive Cardiol 2015;27:157-62. [PubMed] [Google Scholar]
- 6.Ewert P, Berger F, Daehnert I, et al. Transcatheter closure of atrial septal defects without fluoroscopy: feasibility of a new method. Circulation 2000;101:847-9. 10.1161/01.CIR.101.8.847 [DOI] [PubMed] [Google Scholar]
- 7.Tzifa A, Gordon J, Tibby SM, et al. Transcatheter atrial septal defect closure guided by colour flow Doppler. Int J Cardiol 2011;149:299-303. 10.1016/j.ijcard.2010.01.014 [DOI] [PubMed] [Google Scholar]
- 8.Baruteau AE, Hascoet S, Fraisse A. Transthoracic echocardiography is a safe alternative for assessment and guidance of transcatheter closure of secundum atrial septal defect in children. J Thorac Dis 2017;9:1247-56. 10.21037/jtd.2017.04.47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang JK, Tsai SK, Lin SM, et al. Transcatheter closure of atrial septal defect without balloon sizing. Catheter Cardiovasc Interv 2008;71:214-21. 10.1002/ccd.21308 [DOI] [PubMed] [Google Scholar]
- 10.Kazmouz S, Kenny D, Cao QL, et al. Transcatheter closure of secundum atrial septal defects. J Invasive Cardiol 2013;25:257-64. [PubMed] [Google Scholar]
- 11.Amin Z, Hijazi ZM, Bass JL, et al. Erosion of Amplatzer septal occluder device after closure of secundum atrial septal defects: review of registry of complications and recommendations to minimize future risk. Catheter Cardiovasc Interv 2004;63:496-502. 10.1002/ccd.20211 [DOI] [PubMed] [Google Scholar]
- 12.Søndergaard L, Loh PH, Franzen O, et al. The first clinical experience with the new GORE(R) septal occluder (GSO). EuroIntervention 2013;9:959-63. 10.4244/EIJV9I8A160 [DOI] [PubMed] [Google Scholar]
- 13.Smith B, Thomson J, Crossland D, et al. UK multicenter experience using the Gore septal occluder (GSO(TM)) for atrial septal defect closure in children and adults. Catheter Cardiovasc Interv 2014;83:581-6. 10.1002/ccd.25216 [DOI] [PubMed] [Google Scholar]
- 14.Varma C, Benson LN, Silversides C, et al. Outcomes and alternative techniques for device closure of the large secundum atrial septal defect. Catheter Cardiovasc Interv 2004;61:131-9. 10.1002/ccd.10700 [DOI] [PubMed] [Google Scholar]
- 15.Harper RW, Mottram PM, McGaw DJ. Closure of secundum atrial septal defects with the Amplatzer septal occluder device: techniques and problems. Catheter Cardiovasc Interv 2002;57:508-24. 10.1002/ccd.10353 [DOI] [PubMed] [Google Scholar]
- 16.Spies C, Boosfeld C, Schrader R. A modified Cook sheath for closure of a large secundum atrial septal defect. Catheter Cardiovasc Interv 2007;70:286-9. 10.1002/ccd.21082 [DOI] [PubMed] [Google Scholar]
- 17.Kannan BR, Francis E, Sivakumar K, et al. Transcatheter closure of very large (>or= 25 mm) atrial septal defects using the Amplatzer septal occluder. Catheter Cardiovasc Interv 2003;59:522-7. 10.1002/ccd.10575 [DOI] [PubMed] [Google Scholar]
- 18.Wahab HA, Bairam AR, Cao QL, et al. Novel technique to prevent prolapse of the Amplatzer septal occluder through large atrial septal defect. Catheter Cardiovasc Interv 2003;60:543-5. 10.1002/ccd.10686 [DOI] [PubMed] [Google Scholar]
- 19.Dalvi BV, Pinto RJ, Gupta A. New technique for device closure of large atrial septal defects. Catheter Cardiovasc Interv 2005;64:102-7. 10.1002/ccd.20248 [DOI] [PubMed] [Google Scholar]
- 20.Pillai AA, Rangaswamy Balasubramanian V, Selvaraj R, et al. Utility of balloon assisted technique in trans catheter closure of very large (>/=35 mm) atrial septal defects. Cardiovasc Diagn Ther 2014;4:21-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Narin N, Baykan A, Argun M, et al. New modified balloon-assisted technique to provide appropriate deployment in the closure of large secundum atrial septal defect using amplatzer septal occluder in children. J Invasive Cardiol 2014;26:597-602. [PubMed] [Google Scholar]
- 22.Kutty S, Asnes JD, Srinath G, et al. Use of a straight, side-hole delivery sheath for improved delivery of Amplatzer ASD occluder. Catheter Cardiovasc Interv 2007;69:15-20. 10.1002/ccd.20953 [DOI] [PubMed] [Google Scholar]
- 23.Djer MM, Ramadhina NN, Idris NS, et al. Transcatheter closure of atrial septal defects in adolescents and adults: technique and difficulties. Acta Med Indones 2013;45:180-6. [PubMed] [Google Scholar]
- 24.Fu YC, Cao QL, Hijazi ZM. Device closure of large atrial septal defects: technical considerations. J Cardiovasc Med (Hagerstown) 2007;8:30-3. 10.2459/01.JCM.0000247432.74699.47 [DOI] [PubMed] [Google Scholar]
- 25.Podnar T, Martanovic P, Gavora P, et al. Morphological variations of secundum-type atrial septal defects: feasibility for percutaneous closure using Amplatzer septal occluders. Catheter Cardiovasc Interv 2001;53:386-91. 10.1002/ccd.1187 [DOI] [PubMed] [Google Scholar]
- 26.Mathewson JW, Bichell D, Rothman A, et al. Absent posteroinferior and anterosuperior atrial septal defect rims: Factors affecting nonsurgical closure of large secundum defects using the Amplatzer occluder. J Am Soc Echocardiogr 2004;17:62-9. 10.1016/j.echo.2003.09.018 [DOI] [PubMed] [Google Scholar]
- 27.Koenig P, Cao QL, Heitschmidt M, et al. Role of intracardiac echocardiographic guidance in transcatheter closure of atrial septal defects and patent foramen ovale using the Amplatzer device. J Interv Cardiol 2003;16:51-62. 10.1046/j.1540-8183.2003.08003.x [DOI] [PubMed] [Google Scholar]
- 28.Remadevi KS, Francis E, Kumar RK. Catheter closure of atrial septal defects with deficient inferior vena cava rim under transesophageal echo guidance. Catheter Cardiovasc Interv 2009;73:90-6. 10.1002/ccd.21756 [DOI] [PubMed] [Google Scholar]
- 29.Kammache I, Mancini J, Ovaert C, et al. Feasibility of transcatheter closure in unselected patients with secundum atrial septal defect, using Amplatzer devices and a modified sizing balloon technique. Catheter Cardiovasc Interv 2011;78:665-74. 10.1002/ccd.23077 [DOI] [PubMed] [Google Scholar]
- 30.Amin Z. Echocardiographic predictors of cardiac erosion after Amplatzer septal occluder placement. Catheter Cardiovasc Interv 2014;83:84-92. 10.1002/ccd.25175 [DOI] [PubMed] [Google Scholar]
- 31.Santoro G, Bigazzi MC, Lacono C, et al. Transcatheter closure of complex atrial septal defects: feasibility and mid-term results. J Cardiovasc Med (Hagerstown) 2006;7:176-81. 10.2459/01.JCM.0000203852.82643.f2 [DOI] [PubMed] [Google Scholar]
- 32.Johri AM, Witzke C, Solis J, et al. Real-time three-dimensional transesophageal echocardiography in patients with secundum atrial septal defects: outcomes following transcatheter closure. J Am Soc Echocardiogr 2011;24:431-7. 10.1016/j.echo.2010.12.011 [DOI] [PubMed] [Google Scholar]
- 33.Silvestry FE, Cohen MS, Armsby LB, et al. Guidelines for the Echocardiographic Assessment of Atrial Septal Defect and Patent Foramen Ovale: From the American Society of Echocardiography and Society for Cardiac Angiography and Interventions. J Am Soc Echocardiogr 2015;28:910-58. 10.1016/j.echo.2015.05.015 [DOI] [PubMed] [Google Scholar]
- 34.Szkutnik M, Masura J, Bialkowski J, et al. Transcatheter closure of double atrial septal defects with a single Amplatzer device. Catheter Cardiovasc Interv 2004;61:237-41. 10.1002/ccd.10753 [DOI] [PubMed] [Google Scholar]
- 35.Everett AD, Jennings J, Sibinga E, et al. Community use of the amplatzer atrial septal defect occluder: results of the multicenter MAGIC atrial septal defect study. Pediatr Cardiol 2009;30:240-7. 10.1007/s00246-008-9325-x [DOI] [PubMed] [Google Scholar]
- 36.Moore JW, Vincent RN, Beekman RH, 3rd, et al. Procedural results and safety of common interventional procedures in congenital heart disease: initial report from the National Cardiovascular Data Registry. J Am Coll Cardiol 2014;64:2439-51. 10.1016/j.jacc.2014.09.045 [DOI] [PubMed] [Google Scholar]
- 37.Diab K, Kenny D, Hijazi ZM. Erosions, erosions, and erosions! Device closure of atrial septal defects: how safe is safe? Catheter Cardiovasc Interv 2012;80:168-74. 10.1002/ccd.24517 [DOI] [PubMed] [Google Scholar]
- 38.Crawford GB, Brindis RG, Krucoff MW, et al. Percutaneous atrial septal occluder devices and cardiac erosion: a review of the literature. Catheter Cardiovasc Interv 2012;80:157-67. 10.1002/ccd.24347 [DOI] [PubMed] [Google Scholar]
- 39.McElhinney DB, Quartermain MD, Kenny D, et al. Relative Risk Factors for Cardiac Erosion Following Transcatheter Closure of Atrial Septal Defects: A Case-Control Study. Circulation 2016;133:1738-46. 10.1161/CIRCULATIONAHA.115.019987 [DOI] [PubMed] [Google Scholar]
- 40.Mallula K, Amin Z. Recent changes in instructions for use for the Amplatzer atrial septal defect occluder: how to incorporate these changes while using transesophageal echocardiography or intracardiac echocardiography? Pediatr Cardiol 2012;33:995-1000. 10.1007/s00246-012-0323-7 [DOI] [PubMed] [Google Scholar]
- 41.Godart F, Houeijeh A, Recher M, et al. Transcatheter closure of atrial septal defect with the Figulla((R)) ASD Occluder: a comparative study with the Amplatzer((R)) Septal Occluder. Arch Cardiovasc Dis 2015;108:57-63. 10.1016/j.acvd.2014.09.005 [DOI] [PubMed] [Google Scholar]
- 42.Roymanee S, Promphan W, Tonklang N, et al. Comparison of the Occlutech (R) Figulla (R) septal occluder and Amplatzer (R) septal occluder for atrial septal defect device closure. Pediatr Cardiol 2015;36:935-41. 10.1007/s00246-015-1103-y [DOI] [PubMed] [Google Scholar]
- 43.Haas NA, Soetemann DB, Ates I, et al. Closure of Secundum Atrial Septal Defects by Using the Occlutech Occluder Devices in More Than 1300 Patients: The IRFACODE Project: A Retrospective Case Series. Catheter Cardiovasc Interv 2016;88:571-81. 10.1002/ccd.26497 [DOI] [PubMed] [Google Scholar]
- 44.Grohmann J, Hohn R, Fleck T, et al. Transcatheter closure of atrial septal defects in children and adolescents: single-center experience with the GORE(R) septal occluder. Catheter Cardiovasc Interv 2014;84:E51-7. 10.1002/ccd.25494 [DOI] [PubMed] [Google Scholar]
- 45.Grohmann J, Wildberg C, Zartner P, et al. Multicenter midterm follow-up results using the gore septal occluder for atrial septal defect closure in pediatric patients. Catheter Cardiovasc Interv 2017;89:E226-32. 10.1002/ccd.26881 [DOI] [PubMed] [Google Scholar]
- 46.de Hemptinne Q, Horlick EM, Osten MD, et al. Initial clinical experience with the GORE(R) CARDIOFORM ASD occluder for transcatheter atrial septal defect closure. Catheter Cardiovasc Interv 2017;90:495-503. 10.1002/ccd.26907 [DOI] [PubMed] [Google Scholar]
- 47.Astarcioglu MA, Kalcik M, Sen T, et al. Ceraflex versus Amplatzer occluder for secundum atrial septal defect closure. Multicenter clinical experience. Herz 2015;40 Suppl 2:146-50. 10.1007/s00059-014-4192-0 [DOI] [PubMed] [Google Scholar]
- 48.Lertsapcharoen P, Khongphatthanayothin A, Srimahachota S, et al. Self-expanding platinum-coated nitinol devices for transcatheter closure of atrial septal defect: prevention of nickel release. J Invasive Cardiol 2008;20:279-83. [PubMed] [Google Scholar]
- 49.Thanopoulos BD, Biasco L, Dardas P, et al. Catheter closure of atrial septal defects using the Cocoon septal occluder: preliminary results of a European multicenter study. Int J Cardiol 2014;177:418-22. 10.1016/j.ijcard.2014.09.006 [DOI] [PubMed] [Google Scholar]
- 50.Peirone A, Contreras A, Ferrero A, et al. Immediate and short-term outcomes after percutaneous atrial septal defect closure using the new nit-occlud ASD-R device. Catheter Cardiovasc Interv 2014;84:464-70. 10.1002/ccd.25434 [DOI] [PubMed] [Google Scholar]
- 51.Granja MA, Peirone A, Barbosa JD, et al. ASD-R PFM device. In: Sievert H, Qureshi SA, Wilson N, et al. editors. Interventions in Structural, Valvular and Congenital Heart Disease. 2nd ed. Boca Raton: CRC Press, 2015;Chap 53:463-8. [Google Scholar]
- 52.Bulut MO, Yucel IK, Kucuk M, et al. Initial Experience with the Nit-Occlud ASD-R: Short-Term Results. Pediatr Cardiol 2016;37:1258-65. 10.1007/s00246-016-1426-3 [DOI] [PubMed] [Google Scholar]
- 53.Kister T, Dahnert I, Lurz P. Fatal Erosion Atrial Septal Defect Device. Catheter Cardiovasc Interv 2016;87:951-4. 10.1002/ccd.26219 [DOI] [PubMed] [Google Scholar]
- 54.Saritas T, Kaya MG, Lam YY, et al. A comparative study of Cardi-O-Fix septal occluder versus Amplatzer septal occluder in percutaneous closure of secundum atrial septal defects. Catheter Cardiovasc Interv 2013;82:116-21. 10.1002/ccd.23301 [DOI] [PubMed] [Google Scholar]
- 55.Ramoğlu MG, Ucar T, Tutar E. Early malfunction of polyvinyl alcohol membrane of septal occluder. Catheter Cardiovasc Interv 2016;87:E151-3. 10.1002/ccd.26057 [DOI] [PubMed] [Google Scholar]
- 56.Bozyel S, Sahin T, Dervis E, et al. A massive left-to-right shunt due to delayed spontaneous perforation of polyvinyl alcohol membrane of atrial septal occluder. Turk Kardiyol Dern Ars 2017;45:541-4. [DOI] [PubMed] [Google Scholar]
- 57.Labombarda F, Roule V, Beygui F. Delayed spontaneous perforation of polyvinyl alcohol membrane-Covered atrial septal defect closure devices. Catheter Cardiovasc Interv 2017;89:E141-4. 10.1002/ccd.26704 [DOI] [PubMed] [Google Scholar]
- 58.Bartel T, Bonaros N, Muller S. Device failure weeks to months after transcatheter closure of secundum type atrial septal defects. Heart 2010;96:1603. 10.1136/hrt.2009.185942 [DOI] [PubMed] [Google Scholar]
- 59.Nassif M, Abdelghani M, Bouma BJ, et al. Historical developments of atrial septal defect closure devices: what we learn from the past. Expert Rev Med Devices 2016;13:555-68. 10.1080/17434440.2016.1182860 [DOI] [PubMed] [Google Scholar]
- 60.Sievert H, Söderberg B, Mellmann A, et al. First human use and intermediate follow-up of a septal occluder with a bioresorbable framework. EuroPCR, 2015;Paris. [Google Scholar]