Abstract
Background:
Although rhinovirus infection is associated with increased risks of acute and chronic respiratory outcomes during childhood compared with respiratory syncytial virus (RSV), the underlying mechanisms remain unclear. We aimed to determine differences in nasal airway microRNA profiles and their downstream effects between infants with rhinovirus and RSV bronchiolitis.
Methods:
As part of multicenter cohort study of infants hospitalized for bronchiolitis, we examined nasal samples obtained from 16 infants with rhinovirus and 16 infants with RSV. We tested nasal airway samples using microarrays to profile global microRNA expression and determine the predicted regulation of targeted transcripts. We also measured gene expression and cytokines for NFκB pathway components.
Results:
Between the virus groups, 386 microRNAs were differentially expressed (FDR<0.05). In infants with rhinovirus, the NFκB pathway was highly ranked as a predicted target for these differentially expressed microRNAs compared with RSV. Pathway analysis using measured mRNA expression data validated that rhinovirus infection had up-regulation of NFκB family (RelA and NFκB2) and down-regulation of inhibitor κB family. Infants with rhinovirus had higher levels of NFκB-induced type-2 cytokines (IL-10 and IL-13; FDR<0.01).
Conclusions:
In infants with bronchiolitis, rhinovirus and RSV infections had different nasal airway microRNA profiles associated with NFκB signaling.
INTRODUCTION
Bronchiolitis is an important public health problem in the US.(1) Indeed, bronchiolitis is the leading cause of hospitalizations for US infants, with approximately 130,000 hospitalizations each year.(1) In addition to this acute morbidity, bronchiolitis has associated chronic morbidity; 30%−40% of infants hospitalized with bronchiolitis develop childhood asthma.(2) Analyses of the two major causative viruses (rhinovirus and respiratory syncytial virus [RSV]) suggest that rhinovirus infection is associated with distinct host immune response profiles,(3) and with different risks of acute (e.g., bronchiolitis severity) and chronic (e.g., incident asthma) respiratory outcomes during childhood when compared to RSV infection.(2) Although these studies suggest that respiratory virus infection and airway immune response modulation are associated with respiratory outcomes in infants with bronchiolitis, the underlying mechanisms of these links remain unclear.(4)
The recent discovery of interactions between innate and adaptive immune responses in the airway is beginning to reveal potential mechanisms – e.g., viral-induced programming of airway immune response via epigenetic changes involving microRNAs.(5) MicroRNAs comprise a large family of highly conserved, non-coding, short single-stranded RNAs that regulate approximately 60% of protein-encoding genes via promoting mRNA degradation or inhibiting translation.(6) Although the literature remains sparse, we recently demonstrated that rhinovirus infection elicits expression of specific microRNAs (e.g., miR-155) in the nasal airway of young children.(7) Additionally, studies have reported that rhinovirus infection not only activates NFκB signaling pathway,(8–11) but also subsequently induces airway hyperreactivity.(12) No prior study, however, has compared the microRNA profiles and their downstream signaling pathways between the two major respiratory viruses – rhinovirus and RSV – in children.
To address this knowledge gap, we examined infants hospitalized for bronchiolitis enrolled into a multicenter cohort study to determine the difference in the nasal airway microRNA profiles and their downstream effects (gene and cytokine expression) between rhinovirus and RSV infections. Specifically, we hypothesized that, compared to RSV infections, rhinovirus infections would be associated with distinctive microRNA signatures that up-regulate NFκB signaling in the nasal airway of infants with bronchiolitis.
METHODS
Study design, setting, and participants
We analyzed data from an ongoing multicenter prospective cohort study of infants (age <1 year) with severe bronchiolitis – the 35th Multicenter Airway Research Collaboration (MARC-35).(13–17) MARC-35 is coordinated by the Emergency Medicine Network (EMNet), a collaboration of 245 participating hospitals. Using a standardized protocol, site investigators at 17 sites across 14 U.S. states enrolled 1,016 infants hospitalized with an attending physician diagnosis of bronchiolitis during three consecutive bronchiolitis seasons from November 1 to April 30 (2011–2014). Bronchiolitis was defined by the American Academy of Pediatrics guidelines: acute respiratory illness with some combination of rhinitis, cough, tachypnea, wheezing, crackles, and retractions.(18) We excluded infants with known heart-lung disease, immunodeficiency, immunosuppression, or gestational age <32 weeks, those who were transferred to a participating hospital >24 hours after the original hospitalization, or those who were consented >24 hours after hospitalization. All patients were treated at the discretion of the treating physicians. The institutional review board at each of the participating hospitals approved the study. Written informed consent was obtained from the parent or guardian.
In the present study, we randomly selected 16 infants with sole rhinovirus infection and 16 infants with sole RSV infection (i.e., no co-infecting viruses) from the MARC-35 cohort, and investigated global microRNA and mRNA expression as well as cytokine levels in the nasal airway.
Data collection
At the index hospitalization, site investigators conducted a structured interview that assessed patients’ demographic characteristics, medical and family history, and details of the acute illness. Emergency department and hospital chart reviews provided further clinical data, such as vital signs, physical examination, medical management, and disposition. Review of medical records was performed, after successful completion of training (lecture, practice charts), by board-certified physicians (e.g., from pediatric pulmonary, allergy/immunology). All data were reviewed at the EMNet Coordinating Center at Massachusetts General Hospital (Boston, MA), and site investigators were queried about missing data and discrepancies identified by manual data checks.
Based on evidence that nasal airway inflammatory response is indicative of that in the lower respiratory tract,(19–21) we investigated nasal airway specimens. Trained investigators collected nasal swabs from the anterior nares, using a standardized protocol,(22) within 24 hours of hospitalization. Both nares were swabbed with a single nylon, pediatric FLOQSwab (Copan, Brescia, Italy). Nasal airway specimens were tested for 1) respiratory viruses, including rhinovirus and RSV, using real-time polymerase chain reaction (PCR) assays, 2) microRNA expression, and 3) mRNA expression, as well as 4) cytokine levels.
RNA extraction and microRNA microarray
Total RNA from the nasal airway specimens was isolated using a Norgen RNA/DNA Purification Kit (Norgen Biotek, Thorold, ON, Canada) and amplified using a Seramir Exosome RNA Amplification Kit (System Biosciences, Palo Alto, CA). MicroRNA quality was determined by Nanodrop1000 (Thermo Scientific, Wilmington, DE) with absorbance ratios for UV 260/280 ≥2.0 and 260/230 between 1.8 and 2.2. Samples meeting quality control criteria were hybridized to Affymetrix GeneChip microRNA 4.0 arrays (Affymetrix, Santa Clara, CA). Resulting data were analyzed in Expression Console using RMA+DMBG (Affymetrix) then exported to Partek Genomics Suite (Partek Inc., St. Louis, MO) for the analyses.
mRNA measurement
Although NFκB measurements are typically performed in cell-based systems with reporter constructs(23) the MARC-35 nasal swab specimens were not cell-based and thus required a different approach. For these specimens, we measured mRNAs and cytokines not only for the components of NFκB signaling pathway, but also for inflammatory mediators reliably induced by NFκB as an indirect measure of NFκB activity.(24–26)
To test the changes in NFκB signaling-related mRNAs as a result of nasal airway microRNA differences, we first prepared cDNA from the RNA extracted from the nasal airway specimens and preamplified NFκB-specific genes by using the RT2 PreAMP cDNA Synthesis Kit (Qiagen, Valencia, CA). The preamplified cDNA was input into the RT2 Profiler™ PCR Array for Human NFκB Signaling Pathway (Qiagen), a qRT-PCR array that allows for the simultaneous mRNA profiling of 84 genes related to NFκB signaling, in addition to housekeeping genes. An array for each case was run on an ABI 7900HT Fast Real-Time PCR System (Applied BioSystems, Carlsbad, CA) and data were analyzed using the RT2 Profiler PCR Array Data Analysis software, version 3.5 (Qiagen).
Cytokine measurement
To test the differences in ten NFκB signaling-related cytokine expression (GM-CSF, IFNγ, IL-1β, IL-2, IL-6, IL-7, IL-8, IL-10, IL-13, and TNFα) between the two virus groups, we tested nasal airway specimen supernatants using the Milliplex MAP Human High Sensitivity T-cell Panel Premixed magnetic bead-based assay (EMD Millipore, Billerica, MA) on the MAGPIX® System (EMD Millipore). Data were analyzed using the Milliplex Analyst 5.1 software (EMD Millipore).
Statistical analyses
All nasal airway samples passed quality control tests and were used for the microRNA analysis. Processed microRNA data were normalized using generalized log non-linear transformations. Differences in the microRNA expression profiles between rhinovirus and RSV groups were examined using principal coordinates analysis (PCoA) with the Bray-Curtis distance as well as unsupervised hierarchical clustering using Spearman’s rank correlation similarity and the Ward’s algorithm. Benjamini-Hochberg false discovery rate (FDR) multiple test correction was applied. Both analyses were carried out in RStudio (RStudio Inc., Boston, MA).
To identify microRNAs and mRNAs that are differentially expressed between the two virus groups, we performed analysis of variance in Partek Genomics Suite version 6.6 (Partek Inc., St. Louis, MO). Next, to investigate the cumulative effects of microRNAs on the gene expression regulation among infants with rhinovirus infection (in comparison to those with RSV), we uploaded the differentially expressed microRNAs into Ingenuity Pathway Analysis (IPA). We carried all microRNAs that had a P<0.10 and a fold difference of >4.0 cutoff into the IPA analysis. Targets of microRNAs were determined using the IPA microRNA Target Filter, which identifies experimentally validated microRNA-mRNA interactions from TarBase, miRecords, and biomedical literature, and predicted microRNA-mRNA interactions from TargetScan. We used a conservative filter, using only experimentally validated and highly conserved predicted mRNA targets for each microRNA. We used these mRNA targets in the Core Pathway Analyses, which identified relationships among the mRNAs in our dataset. Canonical pathways, novel networks, and common upstream regulators were then queried for overlap with our differentially expressed microRNA gene target list. Last, we compared the difference in pathway enrichment between the virus groups using the Benjamini-Hochberg FDR multiple test correction.
In addition to the IPA analysis, we also used miRTarVis (27) to visualize the microRNA-target mRNA expression interaction network. This bioinformatic approach integrates microRNA and mRNA expression profiles, and predicts targets of microRNA by adopting Bayesian inference, MINE analyses, conventional correlation, and mutual information analyses. Lastly, to examine the downstream effect of microRNAs, we used the Mann-Whitney U test to determine differences in the NFκB signaling-related cytokine levels between the virus groups.
RESULTS
Study population
As a part of an ongoing multicenter prospective cohort study, we examined nasal airway samples from 16 infants with rhinovirus bronchiolitis and 16 infants with RSV bronchiolitis. In the current investigation, the analytic and nonanalytic cohorts had no significant differences in most patient characteristics (P>0.05; Supplemental Table S1), except the analytic cohort had a relatively higher proportion of hypoxemia upon presentation (P=0.02). Of 32 infants in the analytic cohort, the median age was 3 months (IQR, 2–7 months), 69% were male, and 50% were non-Hispanic white. Between the virus groups, there were no significant differences in the baseline patient characteristics, clinical presentation, or hospitalization course (all P>0.10; Table 1).
Table 1.
Characteristics and clinical presentation of infants hospitalized for bronchiolitis by associated viral infection
| Variables | Rhinovirus n=16 |
RSV n=16 |
P-value |
|---|---|---|---|
| Baseline characteristics | |||
| Age (month) | 0.91 | ||
| <2 | 4(25) | 5(31) | |
| 2–5.9 | 7(44) | 6(38) | |
| 6–12 | 5(31) | 5(31) | |
| Male sex | 13 (81) | 9(56) | 0.13 |
| Race/ethnicity | 0.51 | ||
| Non-Hispanic white | 6(38) | 10 (63) | |
| Non-Hispanic black | 4(25) | 3(19) | |
| Hispanic | 5(31) | 3(19) | |
| Other | 1(6) | 0(0) | |
| Parental history of asthma | 6(38) | 3(19) | 0.43 |
| Maternal smoking during | 2(13) | 2(13) | 0.99 |
| pregnancy | |||
| Mode of birth | 0.26 | ||
| Vaginal birth | 9(56) | 12 (75) | |
| C-section | 7(44) | 4(25) | |
| Prematurity (gestational age, 32–37 weeks) | 5(31) | 3(19) | 0.69 |
| Previous breathing problems before the index hospitalization* | 5(31) | 4(25) | 0.99 |
| History of eczema | 2(13) | 4(25) | 0.65 |
| Ever attended daycare | 4(25) | 4(25) | 0.99 |
| Aeroallergen sensitization† | 0(0) | 0(0) | — |
| Food sensitization† | 5(31) | 1(6) | 0.17 |
| Other children at home | 14 (88) | 11(69) | 0.39 |
| Mostly breastfed for the first 3 months of age | 11(69) | 10 (63) | 0.71 |
| Smoke exposure at home | 3(19) | 1(6) | 0.60 |
| Antibiotic use before index hospitalization | 7(44) | 4(25) | 0.26 |
| Corticosteroid use before index hospitalization | 5(31) | 2(13) | 0.39 |
| Clinical presentation | |||
| Duration of breathing problem before the index hospitalization (day), median (IQR) | 3(1–11) | 3 (3–5) | 0.78 |
| Weight at presentation (kg), median (IQR) | 7.3 (5.0–8.2) | 6.2 (4.8–6.8) | 0.29 |
| Respiratory rate at presentation (per minute), median (IQR) | 48 (40–61) | 44 (34–65) | 0.63 |
| Oxygen saturation at presentation | 0.87 | ||
| <90% | 4(25) | 3(19) | |
| 90%−93% | 2(13) | 1(6) | |
| ≥94% | 9(56) | 11(69) | |
| Unknown | 1(6) | 1(6) | |
| Retractions on examination | 0.65 | ||
| None | 4(25) | 3(19) | |
| Mild | 4(25) | 7(44) | |
| Moderate/severe | 8(50) | 6(38) | |
| Wheezing on examination | 9(56) | 10 (63) | 0.72 |
| Received antibiotics during prehospitalization visit | 1(6) | 2(13) | 0.99 |
| Received corticosteroids during pre-hospitalization visit | 4(25) | 1(6) | 0.33 |
| Hospitalization course | |||
| Intensive care use† | 3(19) | 3(19) | 0.99 |
| Hospital length-of-stay ≥3 days | 7(44) | 9(56) | 0.48 |
| Hospital length-of-stay (day), median (IQR) | 2 (2–4) | 3 (2–3) | 0.68 |
Data are no. (%) of infants unless otherwise indicated. Patient characteristics, clinical presentation, and hospital course were compared by virus using chi-square test, Fisher’s exact test, or Wilcoxon rank-sum test, as appropriate.
Abbreviations: RSV, respiratory syncytial virus; IQR, interquartile range; n/a, not applicable
Defined as an infant having cough that wakes him/her at night and/or causes emesis, or when the child has wheezing or shortness of breath without cough
Defined as admission to intensive care unit and/or use of mechanical ventilation (continuous positive airway pressure ventilation and/or intubation)
Nasal airway microRNA expression profile differs by infecting virus
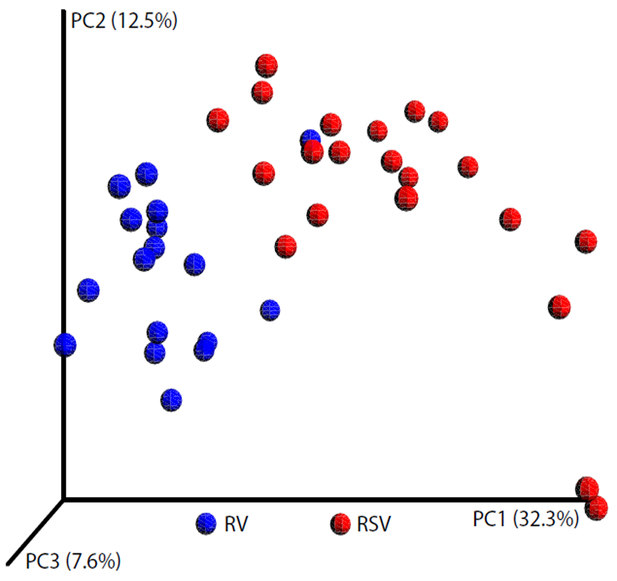
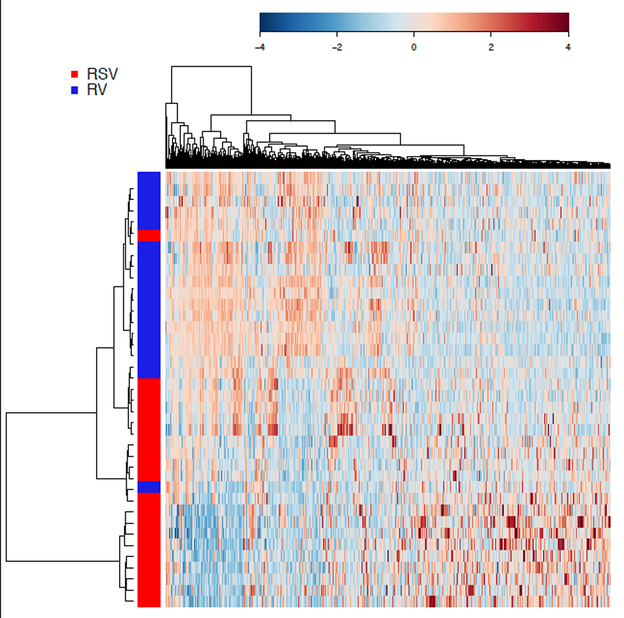
The analysis of global microRNA expression identified 2,758 microRNAs in the nasal airway of infants hospitalized for bronchiolitis. Of these microRNAs, 386 were differentially expressed between the two virus groups (P<0.05 with FDR correction). In the PCoA plot (Figure 1), the microRNA expression profiles almost completely separated infants with rhinovirus bronchiolitis from those with RSV bronchiolitis. Similarly, the unsupervised hierarchical clustering segregated most patients from each viral group (Figure 2).
Figure 1. Principal coordinates analysis plot comparing nasal airway microRNA profiles in infants with rhinovirus bronchiolitis and those with RSV bronchiolitis.
To show the differences in nasal airway microRNA profiles among infants with bronchiolitis, principal coordinates analysis (PCoA) plot based on the Bray-Curtis distance was generated. Each dot represents the overall microRNA expression in each infant. The distance between infants indicates their dissimilarity. The PCoA revealed that infants cluster together according to their viral etiology. In addition to 16 samples with rhinovirus and 16 with RSV, six technical replicates were also included in the analysis. Abbreviations: RV, rhinovirus; RSV, respiratory syncytial virus.
Figure 2. Unsupervised hierarchical clustering of the expression of identified microRNAs in nasal airway of infants with bronchiolitis.
The heatmap of 2,758 microRNAs that are identified in the nasal airway was generated using the Spearman’s rank correlation similarity and the Ward’s clustering algorithm. The microRNA expression profiles almost completely separated infants with rhinovirus bronchiolitis from those with RSV bronchiolitis. The color bar indicates the standardized expression of each microRNA to a mean of 0. Upregulated microRNAs have positive values and are displayed as red. Downregulated microRNAs have negative values and are displayed as blue. The differences in microRNA expression between rhinovirus and RSV are summarized in Supplemental Table S2. Abbreviations: RV, rhinovirus; RSV, respiratory syncytial virus.
Infants with rhinovirus bronchiolitis had specific nasal airway microRNA signature that enhances NFκB signaling pathway
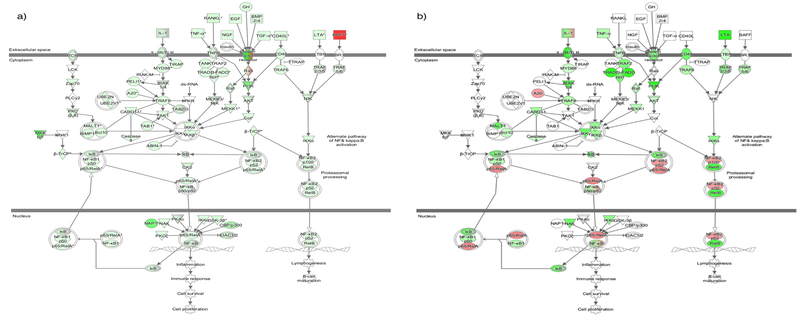
To investigate the cumulative effects of virus-specific microRNA profiles on gene expression, the differentially expressed microRNAs were used for IPA analysis. As hypothesized a priori, the NFκB pathway was highly ranked as a predicted target for these differentially expressed microRNAs (P<0.0001 with FDR correction; Supplemental Table S2). Of 180 genes in the NFκB pathway, 137 genes were predicted to be targeted by these microRNAs. As shown in Figure 3a, infants with rhinovirus bronchiolitis had predicted down-regulation of the inhibitor κB (IκB) family, the major inhibitory proteins of the NFκB signaling pathway, when compared to infants with RSV bronchiolitis. To validate our inference of the microRNAs’ cumulative effects on the NFκB signaling pathway, we also measured the global expression of 84 genes related to NFκB signaling in the nasal airway. Consistent with the predicted regulation of NFκB signaling pathway, the pathway analysis using the measured mRNA expression data (Figure 3b) also demonstrated that infants with rhinovirus bronchiolitis had down-regulation of IκB. In contrast, these infants had up-regulation of RelA (p65) and NFκB2 (p100/p52) – proteins in the NFκB family.
Figure 3. NFκB signaling pathway in the nasal airway comparing infants with rhinovirus bronchiolitis to those with RSV bronchiolitis.
a) Predicted up- and down-regulation of target transcripts in the NFκB signaling pathway. The canonical pathway for NFκB signaling was highly ranked as a target for the microRNAs in infants with rhinovirus bronchiolitis compared to those with RSV bronchiolitis. The green color indicates predicted down-regulation of transcripts targeted by differentially expressed microRNAs in the nasal airway of infants with rhinovirus bronchiolitis compared to those in infants with RSV; the red color indicates predicted up-regulation. Genes are targeted by multiple microRNAs.
b) Measured up- and down-regulation of target transcripts in the NFκB signaling pathway via RT-PCR.
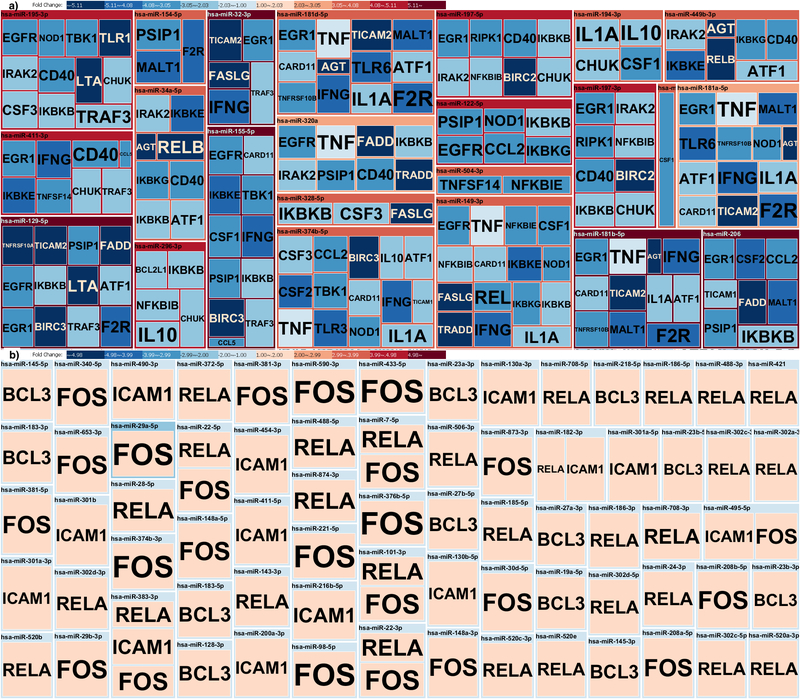
Likewise, the integrated analysis of microRNA and mRNA expression with the use of miRTarVis demonstrated consistent findings (Figures 4a and 4b). For example, infants with rhinovirus bronchiolitis had up-regulation of multiple microRNAs that down-regulate expression of NFKBIB (the gene encoding IκB-β) – e.g., hsa-miR-149–3p (4.2-fold increase; P<0.001), hsa-miR-197–3p (5.5-fold increase; P<0.001), hsa-miR-197–5p (4.3-fold increase; P<0.001), and hsa-miR-296–3p (5.3-fold increase; P<0.001) – when compared to infant with RSV infection (Figures 4a and Supplemental Table S3). Similarly, infants with rhinovirus had up-regulation of microRNAs targeting another IκB family gene, NFKBIE – e.g., hsa-miR-149–3p (4.2-fold increase; P<0.001) and hsa-miR-504–3p (4.1-fold increase; P<0.001). Last, in these patients, hsa-miR-155–5p expression was also up-regulated (4.3-fold increase; P<0.001). By contrast, infants with rhinovirus infection had down-regulation of many microRNAs targeting RELA, the gene encoding RelA, when compared to infants with RSV infection (Figure 4b and Supplemental Table S3). Likewise, these infants had down-regulation of multiple microRNAs targeting FOS, expression of which is known to be up-regulated by the NFκB pathway in conjunction with the extracellular signal-regulated kinase pathway.(28, 29)
Figure 4. Integrated analysis of microRNA and mRNA expressions of NFκB signaling pathway in nasal airway of infants with bronchiolitis.
Treemap of predicted microRNA-target (mRNA) interaction was depicted by the use of miRTarVis, which identifies microRNA-mRNA pairs with an expression value. Normalized, background-subtracted microRNA-mRNA expression profile data were imported into miRTarVis (rhinovirus infection compared to RSV infection). The color gradient indicates the magnitude of the fold change in microRNA and mRNA expression (red, up-regulation; blue, down-regulation). The size (area) of each box represents the frequency of that finding. The shape is designed to automatically fit into the overall structure of the figure.
a) Pairs of up-regulated microRNAs (in red) and down-regulated mRNA (in blue). Notably, infants with rhinovirus bronchiolitis had up-regulation of multiple microRNAs (e.g., hsa-miR-149–3p, hsa-miR-197–3p, hsa-miR-197–5p, hsa-miR-296–3p) targeting NFKBIB, thereby predicting the down-regulation of NFKBIB, a gene encoding inhibitor κB family.
b) Pairs of down-regulated microRNAs (in blue) and up-regulated mRNA (in red). Notably, infants with rhinovirus bronchiolitis had down-regulation of multiple microRNAs targeting RELA, thereby predicting the up-regulation of RELA, the gene encoding RelA (one of the proteins in the NFκB family).
We also measured ten NFκB-regulated cytokines in the nasal airway. Infants with rhinovirus bronchiolitis had higher levels of IL-10 and IL-13 compared to those infants with RSV bronchiolitis (both P<0.05 with FDR correction; Supplemental Table S4). The production of IL-10 and IL-13 is known to be induced by the NFκB signaling pathway.(30, 31)
DISCUSSION
In this analysis of the data from an ongoing multicenter cohort of infants with bronchiolitis, we found that the nasal airway microRNA profiles differ between infants infected with rhinovirus and RSV. We also found that, infants with rhinovirus infection had an altered microRNA profile that is predicted to greatly enhance the NFκB signaling pathway when compared to infants with RSV infection. This finding was mirrored by the observations that the rhinovirus-related microRNA signature is associated with measured down-regulation of IκB family genes and up-regulation of NFκB genes. Consistent with the literature,(32) infants with rhinovirus infection had higher levels of NFκB-induced type-2 cytokines (IL-10 and IL-13) in comparison to those with RSV infection. To the best of our knowledge, this is the first investigation to have examined the difference in microRNA signatures between rhinovirus and RSV and its downstream effects in the setting of severe viral respiratory infection.
The literature indicates that microRNAs help maintain the normal development of the airways and lung in infancy, and throughout childhood help fine-tune airway inflammatory processes, including respiratory infections and asthma.(4) Indeed, emerging evidence, mostly from in vitro investigations, has shown that RSV infection, through altering microRNA expression in airway epithelium, modulates immune responses in the airway.(33, 34) While the research on rhinovirus infection-related perturbations in microRNA expression is sparse, we recently examined the microRNA expression in the nasal airway of ten young children (aged <3 years) with PCR-confirmed rhinovirus infection, and found that rhinovirus infection induces miR-155 when compared to ten healthy children.(7) In the current study, we also demonstrate up-regulation of this microRNA among infants with rhinovirus infection in comparison to those with RSV. Studies have shown that miR-155 has critical roles in type-2 pro-asthmatic responses, including Th2 priming,(35) type-2 immune polarization,(36) modulation of responses to IL-13,(37) and allergic airway inflammation.(38) Our study corroborates previous reports linking respiratory virus infection, microRNA-related immune modulation, and asthma. Our data extend these prior studies by demonstrating that rhinovirus infection-related microRNA signatures enhance the NFκB signaling pathway in infants during an important period of lung development (median age of 3 months).
The clinically relevant implication that rhinovirus infection-related perturbation of microRNA expression and activated NFκB signaling pathway may impact acute (e.g., bronchiolitis severity) and chronic (e.g., development of childhood asthma) bronchiolitis morbidity warrants further clarification. Multiple studies have reported that rhinovirus infection not only activates the NFκB signaling pathway,(8–11) but also subsequently induces airway hyperresponsiveness.(12) In addition, activation of the NFκB signaling pathway within the airway epithelium has been implicated in asthma pathobiology (e.g., allergic airway inflammation, airway hyperresponsiveness, and fibrotic airway remodeling) in animal models.(39, 40) Additionally, studies of adults with asthma have demonstrated that enhanced NFκB signaling, normally transient due to concurrent induction of the inhibitor κB, is persistent with resulting pathologic changes in immune cell cytokine/chemokine secretion.(41, 42) Furthermore, Panganiban et al., by profiling the microRNA expression in 35 adults with asthma, found that these patients had specific microRNA signatures (e.g., up-regulation of miR-155) and that the targeted genes were involved in the NFκB signaling pathway.(43) These data suggest a potential causal relationship between rhinovirus infection-induced programing of airway cells (i.e., epigenetic changes via microRNAs inducing NFκB signaling mediators), and the development of asthma in young children. However, it is also possible that the altered airway microRNA profiles and enhanced NFκB signaling in the setting of rhinovirus infection may simply be a marker of an individual who is prone to develop childhood asthma. Additionally, the underlying mechanisms linking severe virus infection to incident asthma may differ among different asthma phenotypes (e.g., atopic versus non-atopic asthma).(2) Notwithstanding this complexity, the identification of distinct airway microRNA profiles and enhanced NFκB signaling pathway in infants with rhinovirus is an important advance.
Several potential limitations of our study should be taken into account. First, bronchiolitis involves inflammation of the lower airway from which specimen sampling is ethically and technically challenging in infants. Although our study was based on the nasal airway samples, the literature has reported strong correlations between upper and lower airway virology,(44) gene expression,(19, 20) and inflammatory mediators.(21) Therefore, the microRNA and inflammatory profiles in the nasal airway are likely indicative of those in the lower airways. Second, as our samples were not cell-based, we did not measure NFκB activity per se. Nevertheless, we measured the gene expression for the components of NFκB signaling pathway, as well as the cytokines (e.g., IL-10, IL-13) for inflammatory mediators induced by NFκB. Third, the observed differences in microRNA profiles may be attributable to potential differences in cellular profiles by virus. However, we removed cellular RNAs by filtering cells. Fourth, the present study design precluded us from examining the relation between longitudinal patterns of the microRNA-mediated airway immune modulation and respiratory health in children (e.g., development of asthma). To address this question, the study population is currently being followed to 6 years of age with nasal airway specimen sampling at multiple time-points. Fifth, we did not have the data of a “control” group, such as healthy infants without respiratory virus infection. Yet, the study objective was not to evaluate the role of microRNA on the development of bronchiolitis (yes/no) but to determine the virus-specific pathobiology involving airway microRNAs within infants with bronchiolitis (rhinovirus vs. RSV). Sixth, while the current study demonstrated the findings to be consistent by examining both predicted and measured gene expression, external validation would be necessary to confirm these observations. Lastly, we must generalize our findings cautiously beyond infants who had severe bronchiolitis. Nonetheless, our data remain highly relevant for 130,000 children hospitalized for bronchiolitis in the US each year.(1)
CONCLUSIONS
In this multicenter cohort study of infants hospitalized with bronchiolitis, we found that nasal airway microRNA profiles differ between the two most common viruses causing bronchiolitis, rhinovirus and RSV. Our data also demonstrated that infants with rhinovirus infection had an altered microRNA profile that is predicted to enhance the NFκB signaling pathway. Conversely, infants with RSV infection had a microRNA profile that is predicted to have a downregulated NFκB signaling pathway. These findings were validated by the observation that microRNA signature in rhinovirus infection is associated with measured up-regulation of NFκB genes and down-regulation of IκB family genes. Additionally, infants with rhinovirus had higher levels of NFκB-induced type-2 cytokines (IL-10 and IL-13) compared to those with RSV infection. In conjunction with prior studies, our data suggest a potential mechanism linking rhinovirus infection and bronchiolitis-related chronic morbidities – i.e., rhinovirus infection-induced programing of airway cells, via epigenetic changes involving microRNAs, induces NFκB signaling mediators and unique immune response profiles. Our data should facilitate further mechanistic investigations to disentangle the complex web of viral pathogens, microRNA regulation, and host immune responses in the airway of young children with bronchiolitis.
Supplementary Material
Acknowledgements:
The authors thank Ashley Sullivan, Courtney Tierney, and Janice Espinola, at the EMNet Coordinating Center (Massachusetts General Hospital, Boston, MA), and all of the site investigators and study staff for their valuable contributions to the MARC-35 study. We also thank Dr. Alkis Togias at the National Institutes of Health (Bethesda, MD) for helpful comments about the study results. Lastly, we thank the participating families for making all of this possible.
Disclosures:
Funding:
This study was supported by the grants UG3 OD-023253, U01 AI-087881, R01 AI-114552, R01 AI-108588, R01 AI-127507, R21 HL-129909, and K12 HL-119994 from the National Institutes of Health (Bethesda, MD). The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Statement of financial support:
This study was supported by the grants UG3 OD-023253, U01 AI-087881, R01 AI-114552, R01 AI-108588, R01 AI-127507, R21 HL-129909 and K12 HL-119994 from the National Institutes of Health (Bethesda, MD). The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Competing interests:
Dr. Mansbach has provided bronchiolitis-related consultation for Regeneron. Dr. Piedra received research grants from Gilead, Janssen Vaccines and Prevention, Novavax, and Regeneron, and provided bronchiolitis-related consultation for Ablynx, LFB, MedImmune, Novavax, and Regeneron. The other authors have no financial relationships relevant to this article to disclose.
Personal financial interests:
Dr. Mansbach has provided bronchiolitis-related consultation for Regeneron. Dr. Piedra received research grants from Gilead, Janssen Vaccines and Prevention, Novavax, and Regeneron, and provided bronchiolitis-related consultation for Ablynx, LFB, MedImmune, Novavax, and Regeneron. The other authors have no financial relationships relevant to this article to disclose.
Category of study:
Translational
REFERENCES
- 1.Hasegawa K, Tsugawa Y, Brown DF, Mansbach JM, Camargo CA Jr., Trends in bronchiolitis hospitalizations in the United States, 2000–2009. Pediatrics. 2013;132(1):28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hasegawa K, Mansbach JM, Camargo CA Jr. Infectious pathogens and bronchiolitis outcomes. Expert Rev Anti Infect Ther 2014;12(7):817–28. [DOI] [PubMed] [Google Scholar]
- 3.Mejias A, Dimo B, Suarez NM, et al. Whole blood gene expression profiles to assess pathogenesis and disease severity in infants with respiratory syncytial virus infection. PLoS Med. 2013;10(11):e1001549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hasegawa K, Dumas O, Hartert TV, Camargo CA Jr. Advancing our understanding of infant bronchiolitis through phenotyping and endotyping: Clinical and molecular approaches. Exp Rev Respir Med. 2016;10(8):891–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Foster PS, Plank M, Collison A, et al. The emerging role of microRNAs in regulating immune and inflammatory responses in the lung. Immunological reviews. 2013;253(1):198–215. [DOI] [PubMed] [Google Scholar]
- 6.Friedman RC, Farh KK, Burge CB, Bartel DP. Most mammalian mRNAs are conserved targets of microRNAs. Genome Res. 2009;19(1):92–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gutierrez MJ, Gomez JL, Perez GF, et al. Airway Secretory microRNAome Changes during Rhinovirus Infection in Early Childhood. PLoS One. 2016;11(9):e0162244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ilarraza R, Wu Y, Skappak CD, Ajamian F, Proud D, Adamko DJ. Rhinovirus has the unique ability to directly activate human T cells in vitro. J Allergy Clin Immunol. 2013;131(2):395–404. [DOI] [PubMed] [Google Scholar]
- 9.Papi A, Contoli M, Adcock IM, et al. Rhinovirus infection causes steroid resistance in airway epithelium through nuclear factor kappaB and c-Jun N-terminal kinase activation. J Allergy Clin Immunol. 2013;132(5):1075–85 e6. [DOI] [PubMed] [Google Scholar]
- 10.Bartlett NW, Slater L, Glanville N, et al. , Belvisi M, Papi A, Kotenko SV, Johnston SL, Edwards MR. Defining critical roles for NF-kappaB p65 and type I interferon in innate immunity to rhinovirus. EMBO Mol Med. 2012;4(12):1244–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hewson CA, Haas JJ, Bartlett NW, et al. Rhinovirus induces MUC5AC in a human infection model and in vitro via NF-kappaB and EGFR pathways. Eur Respir J. 2010;36(6):1425–35. [DOI] [PubMed] [Google Scholar]
- 12.Girkin J, Hatchwell L, Foster P, et al. CCL7 and IRF-7 Mediate Hallmark Inflammatory and IFN Responses following Rhinovirus 1B Infection. J Immunol. 2015;194(10):4924–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hasegawa K, Mansbach JM, Ajami NJ, et al. Association of nasopharyngeal microbiota profiles with bronchiolitis severity in infants hospitalized for bronchiolitis. Eur Respir J. 2016;48:1329–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stewart CJ, Mansbach JM, Wong MC, et al. Associations of nasopharyngeal metabolome and microbiome with severity among infants with bronchiolitis: A multi-omic analysis. Am J Respir Crit Care Med. 2017. [online ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hasegawa K, Mansbach JM, Ajami NJ, et al. Serum cathelicidin, nasopharyngeal microbiota, and disease severity in infants hospitalized with bronchiolitis. J Allergy Clin Immunol. 2016. [online ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mansbach JM, Hasegawa K, Henke DM, et al. Respiratory syncytial virus and rhinovirus severe bronchiolitis are associated with distinct nasopharyngeal microbiota. J Allergy Clin Immunol. 2016;137(6):1909–13 e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hasegawa K, Mansbach JM, Ajami NJ, et al. The relationship between nasopharyngeal CCL5 and microbiota on disease severity among infants with bronchiolitis. Allergy. 2017. [online ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ralston SL, Lieberthal AS, Meissner HC, et al. American Academy of Pediatrics. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014;134(5):e1474–502. [DOI] [PubMed] [Google Scholar]
- 19.Poole A, Urbanek C, Eng C, et al. Dissecting childhood asthma with nasal transcriptomics distinguishes subphenotypes of disease. J Allergy Clin Immunol. 2014;133(3):670–8 e12. Epub 2014/02/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sridhar S, Schembri F, Zeskind J, et al. Smoking-induced gene expression changes in the bronchial airway are reflected in nasal and buccal epithelium. BMC Genomics. 2008;9:259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McDougall CM, Blaylock MG, Douglas JG, Brooker RJ, Helms PJ, Walsh GM. Nasal epithelial cells as surrogates for bronchial epithelial cells in airway inflammation studies. Am J Respir Cell Mol Biol. 2008;39(5):560–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lambert SB, Ware RS, Cook AL, et al. Observational Research in Childhood Infectious Diseases (ORChID): a dynamic birth cohort study. BMJ Open. 2012;2(6). Epub 2012/11/03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Damsker JM, Dillingham BC, Rose MC, et al. VBP15, a glucocorticoid analogue, is effective at reducing allergic lung inflammation in mice. PLoS One. 2013;8(5):e63871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kerr DM, Harhen B, Okine BN, Egan LJ, Finn DP, Roche M. The monoacylglycerol lipase inhibitor JZL184 attenuates LPS-induced increases in cytokine expression in the rat frontal cortex and plasma: differential mechanisms of action. Br J Pharmacol. 2013;169(4):808–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yagi O, Aoshiba K, Nagai A. Activation of nuclear factor-kappaB in airway epithelial cells in patients with chronic obstructive pulmonary disease. Respiration. 2006;73(5):610–6. [DOI] [PubMed] [Google Scholar]
- 26.Read MA, Whitley MZ, Williams AJ, Collins T. NF-kappa B and I kappa B alpha: an inducible regulatory system in endothelial activation. J Exp Med. 1994;179(2):503–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jung D, Kim B, Freishtat RJ, Giri M, Hoffman E, Seo J. miRTarVis: an interactive visual analysis tool for microRNA-mRNA expression profile data. BMC Proc. 2015;9(Suppl 6 Proceedings of the 5th Symposium on Biological Data): S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tu YC, Huang DY, Shiah SG, Wang JS, Lin WW. Regulation of c-Fos gene expression by NF-kappaB: a p65 homodimer binding site in mouse embryonic fibroblasts but not human HEK293 cells. PLoS One. 2013;8(12):e84062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fujioka S, Niu J, Schmidt C, et al. NF-kappaB and AP-1 connection: mechanism of NF-kappaB-dependent regulation of AP-1 activity. Mol Cell Biol. 2004;24(17):7806–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hinz M, Lemke P, Anagnostopoulos I, et al. Nuclear factor kappaB-dependent gene expression profiling of Hodgkin’s disease tumor cells, pathogenetic significance, and link to constitutive signal transducer and activator of transcription 5a activity. J Exp Med. 2002;196(5):605–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cao S, Zhang X, Edwards JP, Mosser DM. NF-kappaB1 (p50) homodimers differentially regulate pro- and anti-inflammatory cytokines in macrophages. J Biol Chem. 2006;281(36):26041–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jartti T, Paul-Anttila M, Lehtinen P, et al. Systemic T-helper and T-regulatory cell type cytokine responses in rhinovirus vs. respiratory syncytial virus induced early wheezing: an observational study. Respir Res. 2009;10:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Thornburg NJ, Hayward SL, Crowe JE Jr. Respiratory syncytial virus regulates human microRNAs by using mechanisms involving beta interferon and NF-kappaB. mBio. 2012;3(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Inchley CS, Sonerud T, Fjaerli HO, Nakstad B. Nasal mucosal microRNA expression in children with respiratory syncytial virus infection. BMC Infect Dis. 2015;15:150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zech A, Ayata CK, Pankratz F, et al. MicroRNA-155 modulates P2R signaling and Th2 priming of dendritic cells during allergic airway inflammation in mice. Allergy. 2015;70(9):1121–9. [DOI] [PubMed] [Google Scholar]
- 36.Okoye IS, Czieso S, Ktistaki E, et al. Transcriptomics identified a critical role for Th2 cell-intrinsic miR-155 in mediating allergy and antihelminth immunity. Proc Natl Acad Sci USA. 2014;111(30):E3081–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martinez-Nunez RT, Louafi F, Sanchez-Elsner T. The interleukin 13 (IL-13) pathway in human macrophages is modulated by microRNA-155 via direct targeting of interleukin 13 receptor alpha1 (IL13Ralpha1). J Biol Chem. 2011;286(3):1786–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Malmhall C, Alawieh S, Lu Y, et al. MicroRNA-155 is essential for T(H)2-mediated allergen-induced eosinophilic inflammation in the lung. J Allergy Clin Immunol. 2014;133(5):1429–38, 38 e1–7. [DOI] [PubMed] [Google Scholar]
- 39.Tully JE, Hoffman SM, Lahue KG, et al. Epithelial NF-kappaB orchestrates house dust mite-induced airway inflammation, hyperresponsiveness, and fibrotic remodeling. J Immunol. 2013;191(12):5811–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ather JL, Hodgkins SR, Janssen-Heininger YM, Poynter ME. Airway epithelial NF-kappaB activation promotes allergic sensitization to an innocuous inhaled antigen. Am J Respir Cell Mol Biol. 2011;44(5):631–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hart LA, Krishnan VL, Adcock IM, Barnes PJ, Chung KF. Activation and localization of transcription factor, nuclear factor-kappaB, in asthma. Am J Respir Crit Care Med. 1998;158(5 Pt 1): 1585–92. [DOI] [PubMed] [Google Scholar]
- 42.Gagliardo R, Chanez P, Mathieu M, et al. Persistent activation of nuclear factor-kappaB signaling pathway in severe uncontrolled asthma. Am J Respir Crit Care Med. 2003;168(10):1190–8. [DOI] [PubMed] [Google Scholar]
- 43.Panganiban RP, Wang Y, Howrylak J, et al. Circulating microRNAs as biomarkers in patients with allergic rhinitis and asthma. J Allergy Clin Immunol. 2016;137(5):1423–32. [DOI] [PubMed] [Google Scholar]
- 44.Mosser AG, Vrtis R, Burchell L, et al. Quantitative and qualitative analysis of rhinovirus infection in bronchial tissues. Am J Respir Crit Care Med. 2005;171(6):645–51. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.