Abstract
Background
Treatment of advanced‐stage idiopathic Parkinson's disease (PD) is a demanding challenge, and in Germany, medication regimen adjustments are often made during inpatient stays. Admissions often follow an acute worsening of symptoms and functioning. In order to reduce long and expensive inpatient stays, and to provide more frequent consultations, a 24/7 live stream telemedicine home treatment service was established.
Methods
A pilot study was conducted in which laptops were distributed to 50 patients for 1 year to see whether such a service was feasible (in terms of patient participation and compliance) and whether this intervention affected the patient's condition, measured in UPDRS, Mini–Mental Status Examination (MMSE), 39‐item Parkinson's Disease Questionnaire (PDQ39), and H & Y Scale.
Results
Seventy‐two percent (36) of the patients were compliant and did not experience technical issues. Patients lived, on average, 198 ± 183 km away from the specialist clinic. In total, 264 video conversations took place with 6.9 ± 7.2 (0–29) calls per patient. We found a significant improvement in PDQ39 scores, but not in UPDRS, MMSE, or H & Y scores, at 1 year.
Conclusions
Our data shows that 24/7 live stream telemedicine is feasible and can help to improve quality of life. However, a detailed preliminary review of the patient's willingness to use such a service should be made to obtain the best results. Improvement of the technical setup and network coverage would facilitate an improved service and increase efficiency.
Keywords: Parkinson's disease, telemedicine, live‐stream, UPDRS, PDQ39
Idiopathic Parkinson's disease (PD) is a therapeutically challenging condition, especially in advanced stages.1 There are unpredictable intervals between increasing ON and OFF periods,2 and extensive medication regimens require frequent adjustments.
In Germany, patients are primarily treated by either neurologists in specialist outpatient clinics or by general practitioners. However, for patients with advanced‐stage PD, unpredictable and rapid changes in symptoms are a common problem, which often cannot be witnessed in those short appointments. Doctors then commonly refer these patients to acute care hospitals or rehabilitation centers for inpatient care in order to observe them for a longer period. Inpatient stays are expensive and often do not recreate the challenges patients are confronted with in their day‐to‐day environment. Thus, the hospital adjusted medication regimen is not always appropriate in the home environment.
A direct observation of the patient in their home with a dynamic live streaming of the patient's movements along with an audio line could give an exact idea of the patient's condition in their normal environment and thus provide a pertinent solution to their problem. Telemedical systems can meet these requirements by enabling remote video and audio live streaming and have already proven their efficacy in acute stroke care.3
First attempts to use telemedicine for PD care date back to the 1990s,4 but the video quality was not adequate. Larger studies in 2001 and 2004 with more than 150 participants had cohorts with general neurological conditions.5, 6 Now, various telemedicine studies are taking a look at PD in particular,7, 8 but cohorts are often small and the observation period is short or without sufficient video quality. One study9 reported an improvement in patients’ UPDRS scores, but only offline video recordings were used and the program only lasted 30 days.
However, none of these studies used a setup that is available whenever the patient requires immediate assistance for an acute problem related to PD. The physician contacted should not only be able to view the patient's clinical signs within a very short time, but also to discuss the problem directly. In order to provide immediate access to specialist advice, we designed a novel telemedicine system based on a portable laptop that would allow patients to make a live stream video call and contact a specialized center where a telemedicine service was available 24/7.
Thus, a display of acute symptoms would be possible and could be witnessed by PD specialists. Changes in medication could be prescribed by live stream calls and short‐term effects could be monitored afterward, especially for rapid‐acting PD drugs.
Additionally, disease progression could be monitored on a regular basis by the same specialist over the period of 1 year. Consequently, traveling time for patients decreases and specialists may see their patients more often, but with more‐focused consultations given that they have a recent detailed picture of their situation.
The aim of our study was to examine the feasibility of such a 24/7 live stream telemedicine home treatment for PD and its effect on clinical outcomes.
Patients and Methods
Patient Population
This study was designed as an exploratory pilot study. Because we intended to look at patients with advanced‐stage PD, the following inclusion criteria for patient recruitment were set: minimum 5 years of diagnosed PD; minimum 5 years of PD treatment and medication; as well as H & Y Scale Stage 3 or higher. Exclusion criteria were: history of stroke; history of heart failure or New York Heart Association score >3; and pre‐existing dementia and intake of more than four non‐Parkinson drugs. The study was approved by the medical faculty of the Friedrich Alexander University Erlangen.
Every selected patient received the free 24/7 live stream telemedicine home treatment service for 1 year. The selection process took place between October 2010 and September 2011, then the target of 50 participants was achieved. The day of setting up the audio and video system at the patient's home was defined as day 1 of the 1‐year course. The patients for this study were selected at the m&I Fachklinik Ichenhausen rehabilitation Centre (a specialized PD rehabilitation center), based on the inclusion and exclusion criteria, and were asked to join the program at the end of a 2‐week inpatient stay. During this period, the diagnosis of PD was reconfirmed in each patient based on clinical features and dopamine response. Patients were examined by a team of three board‐certified neurologists (with a minimum of 8 years of expertise in the management of PD). All data were collected by the end of September 2012.
Outcome Measures
The following criteria were defined to assess feasibility: compliance measured by dropout rate; technical problems measured by the time the system was unavailable and calls that were prematurely interrupted; as well as satisfaction of patients and physicians measured by a telemedicine questionnaire and willingness to pay for such a setup in the future. Secondary outcomes were: number of technical service interventions and duration of patient calls.
The PD telemedicine questionnaire was intended to measure the level of satisfaction not only with the telemedicine setup and its technology, but also with the medical care and subjective health status, all on a scale from 1 to 6, with 1 being very good and 6 being very poor (according to the German School Rating System).
To assess the clinical course of the patient, we used the following standard scales: UPDRS, Mini–Mental Status Examination (MMSE), H&Y, and 39‐item Parkinson's Disease Questionnaire 39 (PDQ39).
The MMSE and the PDQ39 were evaluated at the beginning and after 12 months whereas all other scores were evaluated at 1, 3, 6, 9, and 12 months in standardized clinical consultations. Interviews at the beginning and after 12 months were conducted in person by the study physician and a trained medical student, whereas interviews at other points of time were conducted through the telemedicine system. To adopt the UPDRS for use in a telemedical setup, the two items of the questionnaire that require physical contact (rigidity and retropulsion) were excluded. The maximum score of the UPDRS therefore was reduced from 199 to 191 points. This modified UPDRS questionnaire based on visual impression alone was published by Abdolahi et al.10 and has proven to be reliable and valid.
The PDQ39 was analyzed within its subdomains: mobility (10 questions, number [#] 1–10); activities of daily living (6, #11–16); emotional well‐being (6, #17–22); stigma (4, #23–26); social support (3, #27–29); cognition (4, #30–33); communication (3, #34–36); and bodily discomfort (3, #37–39).
Intervention
The technical setup comprised a specially configured laptop for each patient with a wide‐angle camera, headset, and a notebook bag (see Fig. 1), as well as three additional laptops for the supervising doctors. The software interface was configured by silberstern GmbH Company (Kempten, Germany).
Figure 1.

Telemedicine setup with laptop and wide‐angle camera.
Uploading patient video data required an internet speed of at least 350 Kbits/s, whereas downloading video data required a minimum of 550 Kbit/s. The doctor's laptop had the same requirements for downloading data, but only needed 200 to 300 Kbit/s for uploading. In Germany, these speeds are usually achievable with standard Digital Subscriber Line (DSL) Internet contracts.
Patients who were identified as having an inadequate internet connection were provided with mobile broadband modems. These used the Universal Mobile Telecommunications System, also known as 3G. If data speed after installation of a mobile broadband modem was still insufficient for a live stream call, participants had to drop out.
Multiple measures were taken to ensure data safety and patient confidentiality. A client server network, Virtual Private Network (VPN) encryption of servers, firewalls, anonymized patient data, password secured doctor's laptop, prohibition of livestream video data storage, and a locked server room under video surveillance were used to ensure data privacy. The technical equipment, data transmission, as well as the study protocol were certified by the Bavarian State for Data Privacy and Information Security. All patients gave voluntary informed consent for participation in the study and to data collection. Approval of an institutional review board was obtained in retrospect.
For ease of use, a specialized interface was designed that took the impairment of motor functions into account. To establish a connection with the doctor's laptop, the patient only needed to press any key on the left half of the keyboard, whereas to end the session, any key on the right side of the keyboard. Motoric tasks, like entering a login or password, were not required. A wide‐angle camera was installed in patients’ homes to make motoric skills and gait more better viewable than with the integrated Video Graphics Array camera. The live stream video connection allowed for color images with only a minor time lag, so that fluent conversations and videos were possible. The telemedicine user interface was the only installed application on the laptop, making only a connection between the patient's and doctor's laptop possible.
A typical live stream call took place as follows: When a patient intended to conduct a live stream video conference with a neurologist, the first step was to call the office of the neurological department and ask for a video conference. The neurologist on duty was informed about the video conference request and accessed to the doctor's laptop to answer the call. Of course, also, appointments for a later point in time could be made. Once both parties agreed on a video conference call, they switched their laptops on and ran the telemedicine live stream application. Pressing any key on the left half of the keyboard on the patient's laptop and clicking the “start” button on the doctor's laptop initiated the search for a secured VPN connection on each device. Once the connection was established, the camera started transmitting the images. After discussing the patient's issues, the connection was ended by pressing a key on the right side of the keyboard on the patient's laptop or clicking on the “stop” button on the doctor's laptop. After the conversation, the doctor documented the conversation and an updated list of medication (if any) was sent to the patient by postal service. Furthermore, a follow‐up call was made after 2 weeks to see how the patient responded to the new regimen.
Three physicians participated in the telemedicine service, all board‐certified neurology consultants with at least 8 years of expertise in treatment of PD. The service was available 24 hours, 7 days a week.
Data Analysis
The statistical analysis for this article was conducted as follows: Quantitative variables are quoted as mean ± standard deviations and qualitative variables are quoted as numbers and percentages. For the comparison of MMSE and H & Y scores at the beginning and end of the examination, a paired Student t test was used. UPDRS scores were analyzed using the Friedman test. For the analysis of PDQ39 subgroups, we used a Student t test to compare baseline with 12‐month scores, P values were then multiplied with the number of subgroups (8), and thus Bonferroni adjusted. The threshold for statistical significance was set to P < 0.05.
Results
Sixty patients were invited to participate in the study. Ten patients did not wish to take part, resulting in a cohort of 50 patients. The mean age of the patients at the beginning of the study was 68.2 ± 7.3 years; 33 patients were male and 17 female. The youngest patient was 47 years old, and the oldest was 82. The year of initial diagnosis was 2000 ± 4.3, and mean H & Y stage at the beginning was 3.1 ± 0.3. Of the 50 participants, 31 originated from Bavaria and the other patients from elsewhere in Germany. One patient moved to South Korea, and because of a good Internet connection, he continued to receive treatment by telemedicine live stream service. The average distance to the specialist clinic was 198 ± 183 km within Germany.
Thirty‐nine patients used their own DSL connection. Eleven patients required a mobile broadband modem (3G), either attributed to lack of data speed with their own connection or because they did not have an Internet connection. During the 1‐year course of the study, 14 of the 50 patients dropped out for various reasons (see Table 1), leaving 36 who remained compliant and who did not face any technical issues. Notably, the majority of the drop outs (10 of 14) occurred during the first 2 weeks. Technical reasons for a dropout in 5 of those cases were attributed to issues concerning modem installation and establishing a sufficient data connection. Five patients changed their mind about participation on arrival of the installation team or within 2 weeks of installation.
Table 1.
Reasons for dropout
| Time | Reason | Technical issues | Dropouts total |
|---|---|---|---|
| Refusal to continue participation | |||
| Within first 2 weeks | 5 | 5 | 10 |
| Within 3 months | 0 | 2 | 2 |
| Within 6 months | 1 | 1 | 2 |
| 7 months or later | 0 | 0 | 0 |
| One year total | 6 | 8 | 14 |
In total, 264 video conversations (VCs) were conducted during the 1‐year trial with a mean of 6.9 ± 7.2 (0 to a maximum of 29) talks per patient. The duration of VCs ranged from 10 to 40 minutes, the mean delay from patient's call to initiation of VC was 6.7 ± 2.9 minutes. The range of the VC lag time was 0 to 4 seconds.
Five participants did not use the system actively despite fully functioning service, and 3 of them needed repeated instructions for the device. Technical problems occurred in eight devices, four of which concerned the internet provider, two the mobile broadband modem, one the laptop itself, and another one could be ascribed to a lack of compliance. Fortunately, all of the technical problems could be fixed by the service team. At the patients request a proportion of conversations (13; 4.9%) were held by telephone instead of possible VCs.
Overall satisfaction with the technology was rated as 2.2 ± 1.0 (1–6; 1 = very good, 6 = very bad). The medical support provided by the doctors was rated as 1.8 ± 0.6. At the end of the trial, 27 (75.0%) of the 36 patients who completed the study after 1 year would have liked to continue with the home treatment, 8 (22.2%) did not feel a continuation would be useful for them personally, and 1 (2.8%) did not make a comment. Twenty‐one (58.3%) patients would be willing to pay for the telemedicine service and could imagine a monthly charge of 65.7 ± 60.8 Euros (€).
Furthermore, the three supervising doctors were asked about their personal experiences with the telemedicine service. According to them, topics for which the patients requested VCs were medication, worsening of movement, and overall condition. Two hundred nineteen (83%) of the talks resulted in a change of medication. For the telemedicine home treatment service, they gave a rating of 1.3 ± 0.4 (1–6, 1 = very good, 6 = very bad). The efforts as a supervising doctor were rated 2.7 ± 0.5 (1–6, 1 = very little effort, 6 = lots of efforts).
Neurological scores of the 36 patients remaining in the study for the duration demonstrated the following results: Mean MMSE did not show any changes, from 28.4 ± 2.1 at the beginning to 28.5 ± 2.4 after 1 year (t (35) = −0.400; P = 0.692, t test). H & Y scores showed a slight, significant worsening, 3.1 ± 0.3 in the beginning to 3.3 ± 0.4 after 1 year (t (35) = −2.376; P = 0.023, t test). When looking at the UPDRS figures over time, one can see a small, but not significant, improvement of UPDRS scores (see Fig. 2).
Figure 2.
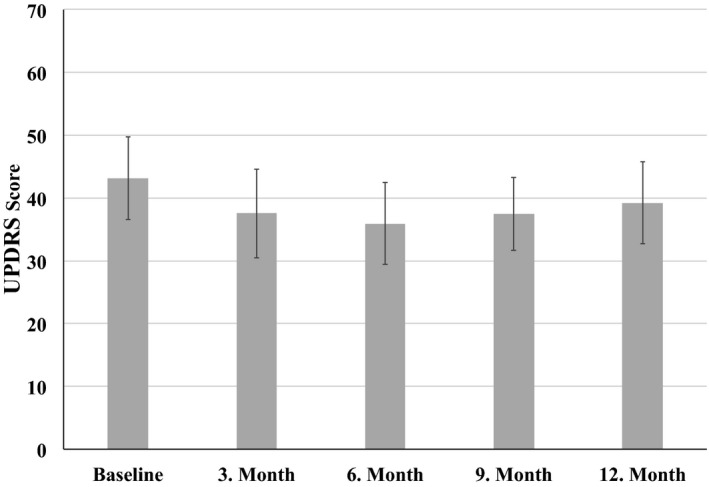
Results of the UPDRS, gathered at the beginning and after 3, 6, 9, and 12 months (mean ± standard error; χ² = 4,881; df = 4; P = 0.300, Friedman test). Error bars represent the standard error.
The results of the PDQ39 demonstrated a significant improvement from a mean of 46.7 ± 23.6 at the beginning to 38.1 ± 20.5 after 1 year of telemedicine treatment (t (35) = 2.164; P = 0.04, t test). Changes in the PDQ39 subdomains were also analyzed; for details, see Figure 3.
Figure 3.
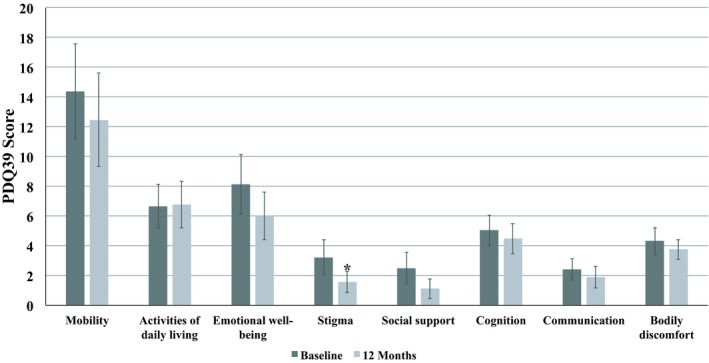
Results of the PDQ39 subdomain comparison between baseline and 12 months, analyzed with the Student t test, Bonferroni adjusted. Mobility (t (35) = 1.468; P = 1.0), activities of daily living (t (35) = −0.145; P = 1.0), emotional well‐being (t (35) = 2.051; P = 0.41), stigma (t (35) = 3.099; P = 0.040), social support (t (35) = 2.754; P = 0.09), cognition (t (35) = 0.989; P = 1.0), communication (t (35) = 1.505; P = 1.0), and bodily discomfort (t (35) = 1.235; P = 1.0). *Significant decrease with P ≤ 0.05; error bars represent the standard error.
Discussion
This is the first report on a 24/7 live stream telemedicine home care service for patients with PD.
Previous studies already demonstrated subjective and objective advantages of a telemedicine setup using recorded videos, which were later examined by professionals.9 A live stream connection is now eliminating the delay between recording, evaluating the videos, and informing the patients about changes in therapy. Thus, it can provide instant help in acute problems.
Our results show that establishing a functioning live stream telemedicine home treatment system is feasible. We were able to establish a functioning 24/7 service for 72% of participants for 1 year with a good patient satisfaction rate. A high level of satisfaction was also reported in previous studies.11 Twenty‐one participants would be willing to pay more than 50€ monthly for the service.
However, a detailed preliminary evaluation of the Internet connection speed and the patient's intention to use such a service should be made before setting up the system, given that 5 of the 10 dropouts, which occurred in the first few days or weeks, could be attributed to data speed problems and the other 5 to lack of compliance or loss of interest.
One disadvantage of a telemedicine approach is that a physical examination is not possible. Examination of rigidity, retropulsion, reflexes, and other statuses is only viable by physical contact. However, there are also ways of assessing a PD patient's condition based on only visual information. Abdolahi et al.10 created a modified UPDRS for telemedicine purposes, which is based on visual impressions only and has been shown to be reliable and valid.
Considering that PD is a degenerative disease, the findings of stable, and even slightly improving, UPDRS scores are positive even if not statistically significant. We think that a high rate of medication adjustments (83% of calls) might have prevented a deterioration of clinical condition and UPDRS scores.
PDQ39 analysis showed a significant increase of more than 8 points in 1 year, indicating an improvement in quality of life. When analyzing the questionnaire's subdomains, the biggest change occurred in the domains of stigma, emotional well‐being, and social support, which may be interpreted as a sign of improved quality of care, especially in terms of social support by better connection to caregivers.
With technological support to PD medical care already being tested in “wearable technology”12, 13 or using smartphones for tremor detection,14 technical progress will allow a more‐complex monitoring of PD patients, even at home. By combining these inventions with an audio‐visual live stream connection, a multimodal telemedicine system for monitoring and treatment of PD could be developed. Further studies are needed to define the prerequisites for such a system and assess the effect of it within the health care system.
Author Roles
(1) Research Project: A. Conception, B. Organization, C. Execution; (2) Statistical Analysis: A. Design, B. Execution, C. Review and Critique; (3) Manuscript Preparation: A. Writing of the First Draft, B. Review and Critique.
G.D.: 1A, 1C, 2B, 3A
J.D.: 1A, 1B
H.D.: 1D, 2C
E.W.: 1B
R.K.: 1B, 1C
R.H.: 1A, 2A, 2C, 3B
Disclosures
Ethical Compliance Statement: We confirm that we have read the journal's position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
Funding Sources and Conflicts of Interest: The study was financially supported by the Bavarian State Ministry of Health, the Deutsche Parkinson Vereinigung e.V. and Deutsche Stiftung Neurologie. The authors report no conflicts of interest.
Financial Disclosures for previous 12 months: Rene Handschu received a research grant from the Bavarian State Ministry of Health (Munich, Germany), honoraria as a speaker at Biogen Corp. (Grafelburg, Germany) and Mundipharma GmbH (Limburg, Germany) and has stock options in Siemens Corp (Munich, Germany).
Acknowledgments
We thank Mr. Daniel Lohse and Mr. Alexander Slowak for setting up the telemedicine system at the patients’ homes and Mrs. Gisela Pfannenstiel and Ms. Marina Berger for organizing patient follow‐up calls and schedules. Finally, we thank the patients and their families, without whose support none of this research would have been possible.
Relevant disclosures and conflicts of interest are listed at the end of this article.
References
- 1. Kulisevsky J, Luquin MR, Arbelo JM, et al. Advanced Parkinson's disease: clinical characteristics and treatment (part 1) [Article in Spanish]. Neurologia 2013;28:503–521. [DOI] [PubMed] [Google Scholar]
- 2. Schrag A, Dodel R, Spottke A, et al. Rate of clinical progression in Parkinson's disease. A prospective study. Mov Disord 2007;22:938–945. [DOI] [PubMed] [Google Scholar]
- 3. Handschu R, Scibor M, Wacker A, et al. Feasibility of certified quality management in a comprehensive stroke care network using telemedicine: STENO project. Int J Stroke 2014;9:1011–1016. [DOI] [PubMed] [Google Scholar]
- 4. Hubble JP, Pahwa R, Michalek DK, et al. Interactive video conferencing: a means of providing interim care to Parkinson's disease patients. Mov Disord 1993;8:380–382. [DOI] [PubMed] [Google Scholar]
- 5. Chua R, Craig J, Wootton R, et al. Randomized control trial of telemedicine for new neurological outpatient referrals. J Neurol Neurosurg Psychiatry 2001;71:63–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Criag J, Chua R, Russel C, et al. A cohort study of early neurological consultation by telemedicine on the care of neurological inpatients. J Neurol Neurosurg Psychiatry 2004;75:1031–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dorsey ER, Venkataraman V, Grana MJ, et al. Randomized controlled clinical trial of “virtual house calls” for Parkinson disease. JAMA Neurol 2013;70:565–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Samii A, Ryan‐Dykes P, Tsukuda RA, et al. Telemedicine for delivery of health care in Parkinson's disease. J Telemed Telecare 2006;12:16–18. [DOI] [PubMed] [Google Scholar]
- 9. Marzinzik F, Wahl M, Doletschek CM, et al. Evaluation of a telemedical care programme for patients with Parkinson's disease. J Telemed Telecare 2012;18:322–327. [DOI] [PubMed] [Google Scholar]
- 10. Abdolahi A, Scoglio N, Killoran A, et al. Potential reliability and validity of a modified version of the Unified Parkinson's Disease Rating Scale that could be administered remotely. Parkinsonism Relat Disord 2013;19:218–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Venkataraman V, Donohue SJ, Biglan KM, et al. Virtual visits for Parkinson disease: a case series. Neurol Clin Pract 2014;4:146–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bonato P. Advances in wearable technology and its medical applications. Conf Proc IEEE Eng Med Biol Soc 2010;2010:2021–2024. [DOI] [PubMed] [Google Scholar]
- 13. Patel S, Lorincz K, Hughes R, et al. Analysis of feature space for monitoring persons with Parkinson's disease with application to a wireless wearable sensor system. Conf Proc IEEE Eng Med Biol Soc 2007;2007:6291–6294. [DOI] [PubMed] [Google Scholar]
- 14. Daneault JF, Carignan B, Codère C, et al. Using a smart phone as a standalone platform for detection and monitoring of pathological tremors. Front Human Neurosci 2012;6:357. [DOI] [PMC free article] [PubMed] [Google Scholar]


