Abstract
Background
Evidence for the positive effects of physiotherapy for persons with Parkinson's disease (PwPD) is rapidly increasing. However, little is known about the provision of physiotherapy for PwPD in everyday practice. The objective of this study was to gain insight into the nature of physiotherapeutic care for PwPD in hospitals, primary care units, and community services in Sweden.
Methods
A web‐based survey was sent out to 2956 members of the Swedish Association of Physiotherapists, including questions about treatment, measurement tools, multi‐professional collaborations, adherence to physiotherapy guidelines, professional expertise, and needs for gaining expertise regarding PwPD.
Results
Of the 1189 physiotherapists who completed the survey, 705 were treating 1 or more PwPD per month in hospitals (21%), in primary care units (37%), and in the community (42%). Physiotherapy frequently targeted a wide range of musculoskeletal and mobility impairments; however, freezing of gait and pain were less frequently treated. Measurement tools recommended for PwPD were infrequently used, and there was a preference for single‐item questions/tools compared with multi‐item instruments. Collaboration with other health care professionals for the rehabilitation of PwPD was rare and was more evident in hospitals than in primary care units and the community. Adherence to physiotherapy guidelines was poor, and most respondents reported that they treated too few PwPD to retain their expertise and they perceived a need to increase their knowledge and skills about physiotherapy for PwPD.
Conclusion
The current findings emphasize the need to strengthen expertise regarding the assessment and treatment of PwPD among physiotherapists in Sweden and to apply strategies endorsing multi‐professional collaboration for PD rehabilitation.
Keywords: Parkinson's disease, physiotherapy, rehabilitation, survey
Because of the complex nature of Parkinson's disease (PD), comprehensive and specialized care in a multi‐professional manner is vital for people with Parkinson's disease (PwPD).1, 2 However, despite optimal medical and neurosurgical treatment,3 PwPD suffer from activity limitations and restrictions in societal participation, which often decrease quality of life.4 To tackle these impairments, PwPD are recommended for referral to a physiotherapist.5, 6, 7
The aim of physiotherapy for PwPD is to maximize functional ability and minimize secondary complications through rehabilitation within a context of education and person‐centered treatment.6 According to the European Physiotherapy Guidelines for PwPD, physiotherapy interventions often target body functions (muscular strength, posture, and joint mobility) and activity limitations (balance, transfers, gait, and physical capacity).8 Adequate recognition of impairments within these areas (i.e., by the use of standardized measurement tools)9 is crucial to identify individuals at risk of adverse events (e.g., falling, physical deterioration) and to decide on optimal treatment methods. Physiotherapy treatment for PwPD is individualized to target patients’ needs and treatment changes as the disease progresses.8 Specifically, physiotherapy commonly aims to retain physical capacity or prevent secondary conditions in the early phases of the disease.8 Activity limitations are targeted by specific interventions (e.g., balance, gait, and transfer exercises) in the mid‐stages, and secondary complications (e.g., pressure sores and contractures) are prevented in the late stage.8, 10, 11 In recent years, evidence endorsing physiotherapy for PwPD has increased considerably,5, 6, 7 and evidenced‐based recommendations for physiotherapy have been developed.8
Despite these advances, little is known about the provision of physiotherapy for PwPD in everyday practice. Two previous surveys conducted in the Netherlands showed that physiotherapists often focused on different impairments of gait, balance, transfers, posture, and physical capacity by providing interventions on an individual basis in the therapist's practice.12, 13 In those studies from 2004 and 2009, the physiotherapists reported limited PD expertise12, 13 and knowledge about the role of other health care professionals.12 Although these surveys have provided important information about physiotherapy for PwPD, their findings might not be generalizable to health care systems in other countries.
In Sweden, different sectors of the health care system provide care for approximately 22,000 PwPD.14 Regarding the delivery of physiotherapy for PwPD in the Swedish health care system, physiotherapists in hospitals often provide consultations and specialized care, physiotherapists at primary care units often deliver specific treatments, whereas physiotherapists in the community provide rehabilitation services delivered in the home or in nursing home settings. Furthermore, in Sweden, PwPD can either receive physiotherapy treatment through a referral from their physician or seek physiotherapy treatment without a referral. Better insight into the provision of physiotherapy for PwPD across the spectrum of health care is warranted to identify potential needs for improvement of the services delivered. The overall aim of the present study was therefore to gain insight into the nature of physiotherapy for PwPD in hospitals, primary care units, and community services in Sweden. Specifically, we aimed to explore the expertise of physiotherapists, treatment characteristics and targets, the utilization of recommended measurement tools, collaborations with other health care professionals, adherence to physiotherapy guidelines and protocols, as well as the need for continued professional development regarding the treatment of PwPD.
Materials and Methods
Participants
A web‐based, structured questionnaire was sent to all physiotherapists registered as members of the Neurology (n = 1009), Health of the Elderly (n = 1383), and Primary Care (n = 930) sections of the Swedish Association of Physiotherapists in September 2015. Of the total number of registered physiotherapists in Sweden (approximately 20,000), about 60% are members of the Swedish Association of Physiotherapists. The included sections were selected because their affiliated physiotherapists are those most likely to treat PwPD in a range of Swedish care settings (i.e., in hospitals, primary care units, and the community). This study was approved by the Regional Board of Ethics in Stockholm (2015/570‐32); all participants provided informed consent before being given access to the questionnaire. All physiotherapists who were members of the Neurology; Health of the Elderly, and Primary Care sections of the Swedish Association of Physiotherapists served as a reference group regarding the descriptive characteristics of our sample (i.e., sex, age, and highest level of education).15
Construction of the Web Survey
Development of the survey was inspired by a Dutch questionnaire, which explored the “learning needs, barriers, and unmet needs” of physiotherapists working with PwPD.16 Questions about potential barriers and facilitators to the provision of optimal physiotherapy treatment were inspired by the Consolidated Framework for Implementation Research.17 To ensure face and content validity, the initial survey was pilot tested among 7 physiotherapists with clinical and research expertise in PD. The responders from that pilot study provided feedback about clinical relevance, structure, and wording of the questions and response categories. Based on this feedback, the questionnaire was modified by the research team.
Procedure: Web Survey
An e‐mail that included a unique hyperlink to a web survey was sent to each physiotherapist. The web survey took approximately 10 minutes to complete, and respondents were required to choose from multiple‐choice answers on a 2‐point, 3‐point, 4‐point, or 5‐point scale. The web survey was available for 4 weeks and could only be answered once by each individual. Up to 4 reminder e‐mails were sent to nonresponders during this period.
Content of the Survey and Data Management
The initial questions in the web survey investigated work setting (i.e., hospital, primary care unit, and community), demographics (sex and age), and level of highest education. Response categories for age were <30 years, ≥30 to 40 years, >40 to 50 years, >50 to 60 years, and >60 years; and the response categories for highest education were Master of Science, Clinical Specialist, and Doctor of Philosophy. In the Swedish context, a Clinical Specialist is a physiotherapist with a Master of Science degree and at least 5 years of working experience, including 3 years of supervised practice within their specialist field. The subsequent questions were divided into 6 domains, which are detailed in Supporting Table S1 (see online supporting information). Briefly, the first domain focused on physiotherapist expertise in relation to years of work experience, perceived PD expertise and treatment volume (i.e., the number of PwPD treated per month and the perceived number needed to treat to retain expertise). For the latter item, we calculated the number of physiotherapists who perceived that they treated too few PwPD in order to retain their expertise. In contrast to previous studies that targeted treatment volume per year,12 we used a time frame of 1 month, because we expected it would be easier for respondents to recall treatment volume for this period. The second domain addressed treatment characteristics, covering questions about treatment forms (individual/group/combined), treatment duration (i.e., the number of treatment sessions per treatment period), and targets of physiotherapy treatment for PwPD.8 The targets of physiotherapy treatment were purposively selected to include a mix between body impairments (e.g., posture and range of motion) and activity limitations (e.g., transfers) as well as between more generic domains (e.g., balance and gait) and more PD‐specific impairments (e.g., freezing of gait). The third domain covered the utilization of standardized measurement tools for PwPD, including measurement tools that are recommended for PwPD,8, 9 translated into Swedish, and accessible to physiotherapists in Sweden. The recommended measurement tools addressed balance control (the Berg Balance Scale [BBS] and the Mini Balance Evaluation Systems Test [Mini‐BESTest]), mobility (the Timed Up and Go [TUG]), lower extremity functioning (the 5 Times Sit to Stand test [FTSST]), gait (the 10‐Meter Walk test [10MWT], and the Freezing of Gait Questionnaire [FOG‐Q]), fear of falling (the Falls Efficacy Scale‐International [FES‐I]), balance confidence (Activities Balance Confidence [ABC]), and physical capacity (the 6‐Minute Walk Distance [6MWD]).
The fourth domain addressed whether physiotherapists collaborated with other health care professions (physician, nurse, occupational therapist, social worker, and speech therapist) while treating PwPD. In accordance with the national guidelines for PD from the National Board of Health and Welfare in Sweden, physiotherapists who reported collaboration with a physician, a nurse, and at least 2 additional health care professionals were considered to treat PwPD in a multi‐professional manner.18 The physiotherapists were also asked about their insight into the role of other health care professionals treating PwPD. The fifth domain explored the application of the European physiotherapy guidelines for PD8 or local treatment protocols (i.e., a document originating from the actual workplace) to guide their clinical work. In addition, we asked about potential barriers (i.e., accessibility and user friendliness) for using PD protocols/guidelines. The sixth domain investigated the needs for gaining increased expertise regarding theoretical knowledge about PD as well as skills regarding the assessment (e.g., measurement tools) and treatment of PwPD.
The data obtained from the web survey were categorized as either binominal or ordinal (see Supporting Table S1) and were presented descriptively. Physiotherapists treating at least 1 PwPD per month were included in the analysis, and data are presented separately for the different work settings (hospitals, primary care units, and community) as numbers and percentages for each category.
Results
Response and Sample Characteristics
Of the 2956 surveys that reached a recipient, 1189 physiotherapists (40% response rate) completed the survey (see Fig. 1). Of the responding physiotherapists, 705 (59%) were treating at least 1 PwPD per month and thus were included in the analysis. For this group, the most common work setting was the community (42%), followed by primary care units (37%), and hospitals (21%). Sex, age, and educational level of the study sample and the targeted population are presented in Table 1.
Figure 1.
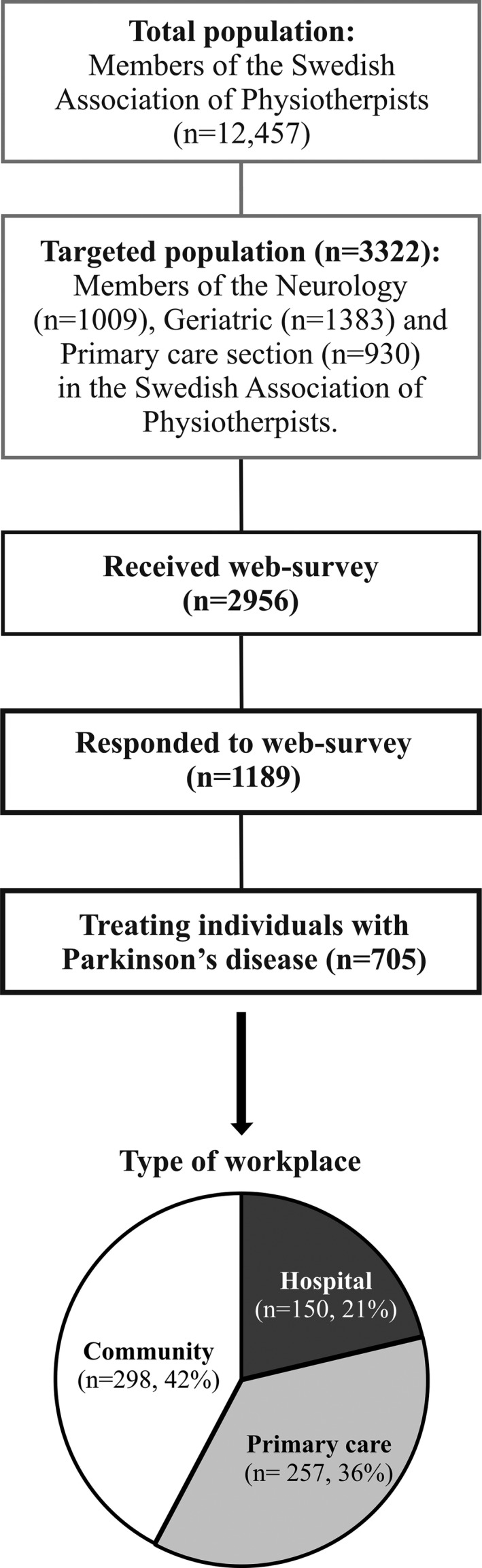
This flow chart illustrates the targeted population, the number of physiotherapists who received the web survey, the response rate, as well as the proportion who were treating persons with Parkinson's disease and their work setting.
Table 1.
Demographics and educational level of the study sample and the targeted population
| Variable | Study sample: No. (%) | ||||
|---|---|---|---|---|---|
| Hospital (n = 150) | Primary care, n = 257 | Community, n = 298 | All, n = 705 | Population, n = 3322 | |
| Women | 134 (89) | 223 (87) | 259 (90) | 616 (87) | 2872 (86) |
| Age, y | |||||
| <30 | 12 (8) | 34 (13) | 50 (17) | 96 (14) | 687 (21) |
| >30–40 | 33 (22) | 53 (21) | 90 (30) | 176 (25) | 834 (25) |
| >40–50 | 54 (36) | 67 (26) | 74 (25) | 195 (28) | 843 (25) |
| >50–60 | 40 (26) | 64 (25) | 65 (22) | 169 (24) | 658 (20) |
| >60 | 9 (6) | 38 (15) | 16 (5) | 63 (9) | 300 (9) |
| Education | |||||
| Master of Science | 14 (9) | 23 (9) | 7 (2) | 44 (6) | 233 (7) |
| Clinical specialist | 10 (7) | 23 (9) | 1 (0.5) | 34 (5) | 216 (7) |
| Doctor of Philosophy | 5 (3) | 4 (2) | — | 9 (1) | 37 (1) |
Expertise of Physiotherapists
Working experience was similar in all work settings, with the majority of physiotherapists reporting >10 years of clinical experience (Table 2). Irrespective of their work setting, the majority of physiotherapists (range, 52%‐84%) treated 1 or 2 PwPD per month, but a minority (range, 13%‐23%) perceived that the number of PwPD they treated was sufficient to retain their expertise (Table 2). In addition, 50%, 56%, and 68% of the therapists in the hospitals, primary care units, and community, respectively, reported that they treated too few PwPD to retain their expertise.
Table 2.
Professional expertise among physiotherapists, treatment characteristics, and needs for gaining expertise regarding Parkinson's disease in different work settings
| Variable | Study sample: No. (%) | |||
|---|---|---|---|---|
| Hospital, n = 150 | Primary care, n = 257 | Community, n = 298 | All, n = 705 | |
| Working experience, years | ||||
| 1–5 | 18 (12) | 45 (18) | 71 (24) | 134 (19) |
| 6–0 | 24 (16) | 40 (16) | 58 (19) | 122 (17) |
| >10 | 107 (71) | 171 (67) | 167 (56) | 445 (63) |
| Sufficient PD expertise | 120 (80) | 191 (74) | 172 (58) | 483 (69) |
| PwPD, patients per months | ||||
| 1–2 | 78 (52) | 180 (70) | 251 (84) | 509 (72) |
| 3–5 | 39 (26) | 44 (17) | 44 (15) | 127 (18) |
| ≥6 | 33 (22) | 33 (13) | 3 (1) | 69 (10) |
| PwPD needed to treat, patients per months | ||||
| 1–2 | 20 (13) | 60 (23) | 68 (23) | 148 (21) |
| 3–5 | 81 (54) | 136 (53) | 163 (55) | 380 (54) |
| ≥6 | 49 (33) | 61 (24) | 62 (21) | 177 (24) |
| Form of treatment | ||||
| Individual | 96 (64) | 155 (60) | 254 (85) | 505 (72) |
| Group | 10 (7) | 7 (3) | 5 (2) | 22 (3) |
| Individual and group | 40 (27) | 90 (35) | 33 (11) | 163 (23) |
| Treatment duration, no. of sessions | ||||
| 1–2 | 41 (27) | 4 (2) | 66 (22) | 111 (16) |
| 3–5 | 37 (25) | 39 (15) | 73 (24) | 149 (21) |
| ≥6 | 66 (44) | 210 (82) | 145 (49) | 421 (60) |
| Needs for gaining PD expertise | ||||
| Theoretical knowledge | 110 (73) | 191 (74) | 240 (81) | 541 (77) |
| Skills | 125 (83) | 204 (79) | 268 (90) | 597 (85) |
| Measurement tools | 126 (84) | 222 (86) | 269 (90) | 617 (88) |
PD, Parkinson's disease; PwPD, persons with Parkinson's disease.
Treatment Characteristics and Targets
In hospitals and primary care units, physiotherapy was delivered in an approximately 60:40 distribution between individual and group treatment (see Table 2). In the community, physiotherapy was predominantly (85%) given on an individual basis. Longer treatment durations (≥6 sessions) were most prevalent (82%) in primary care units, whereas there was greater variation between diverse treatment durations in hospitals and in the community (Table 2). As illustrated in Fig. 2, physiotherapy treatments were frequently targeted towards improving a wide variety of disabilities whereas freezing of gait and pain were treated by <35% of the physiotherapists.
Figure 2.
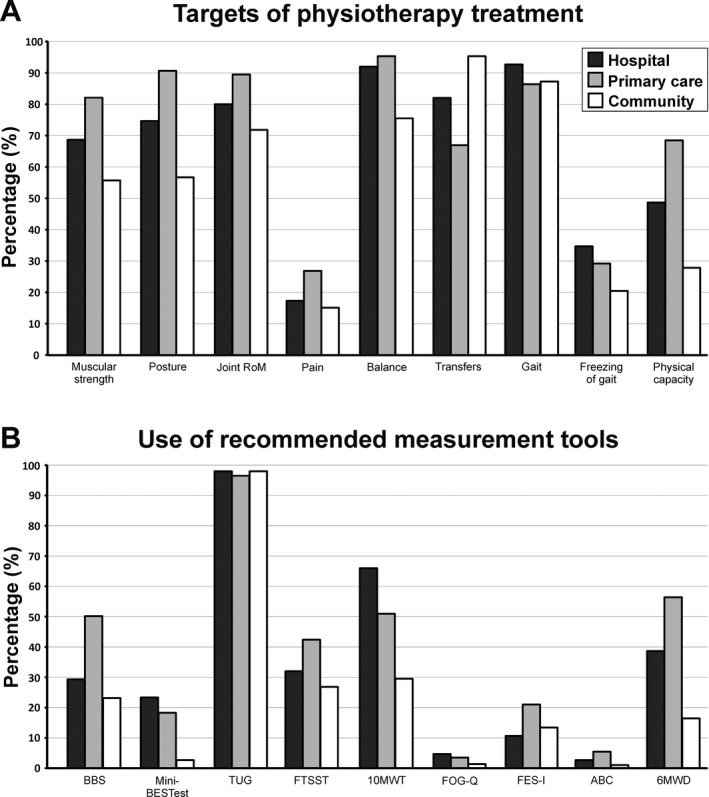
A: Targets of physiotherapy treatment and (B:) the use of recommended measurement tools for persons with Parkinson's disease in different work settings. Data represent the frequency (%) of physiotherapists per work setting who were treating a specific disability (i.e., “quite often” or “very often”) and using a specific outcome measure (i.e., “sometimes”, “quite often,” or “very often”). RoM indicates range of motion; BBS, Berg Balance Scale; Mini‐BESTest, Mini‐Balance Evaluation Systems Test; TUG, Timed Up and Go; FTSST, 5 Times Sit to Stand; 10MWT; 10‐Meter Walk test; FOG‐Q, Freezing of Gait Questionnaire; FES‐I, Falls Efficacy Scale‐ International; ABC, Activities Balance Confidence scale; 6MWD; 6‐Minute Walk Distance.
Use of Standardized Measurement Tools
A majority (range, 71‐79%) of physiotherapists that worked in hospitals and primary care units reported that they used standardized measurement tools when assessing PwPD, whilst the corresponding proportion was 50% in the community. However, measurement tools recommended for PwPD were used infrequently and single‐item questions/tools were more often used than multi‐items instruments. As illustrated in Fig. 2B, the TUG test was the most common outcome measure (used by ≥97% of the physiotherapists in all work settings). The BBS, the FTSST and the 10MWT were also utilized in all work settings but less frequently than the TUG test (range, 27‐66%). In hospitals and primary care units, the Mini‐BESTest and the 6MWT were used by 18‐23% and 39‐56% of the physiotherapists, respectively, whereas these were less frequently used (range, 3‐16%) by physiotherapists in the community. Furthermore, the FES‐I was used by 21% of physiotherapists in primary care units but to a lesser extent (11‐13%) by physiotherapists working in hospitals and the community. The ABC‐scale and the FOG‐Q were used to a limited extent (<5%) in all work settings.
Collaboration with Other Health Care Professionals
Overall, physiotherapy treatment of PwPD in collaboration with other healthcare professionals was more common in hospitals than in primary care units and the community (see Fig. 3). This difference between work settings was especially pronounced for multi‐professional collaboration, i.e., 38% in hospitals versus 8% and 1% of the physiotherapists working in primary care units and the community, respectively. Limited insight regarding the role of other health care professionals was also most frequently reported among physiotherapists working in the community (60%), followed by primary care units (44%) and hospitals (23%). In line with this, 80% of the physiotherapists that worked in hospitals collaborated with a physician. The corresponding values for primary care units and the community were 39% and 13%, respectively. Physiotherapists in primary care units predominantly collaborated with occupational therapists whereas collaboration with nurses and occupational therapists was most common in the community. However, collaboration with social workers and speech therapists was uncommon in primary care units (range, 15‐19%) and almost non‐existent in the community (1%).
Figure 3.
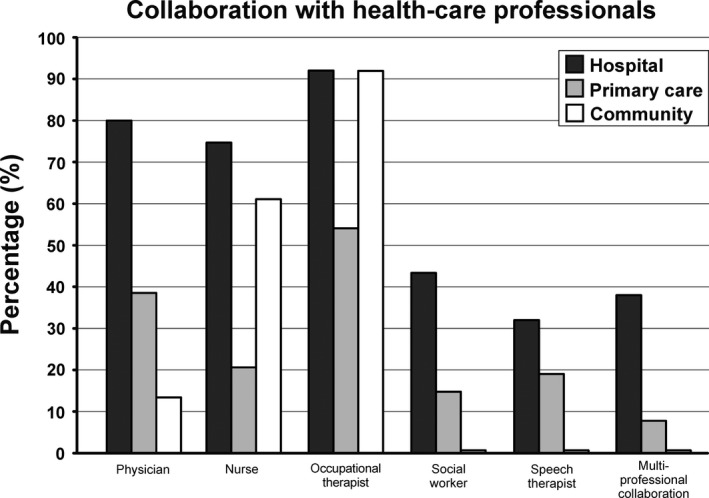
The percentage of physiotherapists per work setting who reported collaboration with other health care professionals and a multi‐professional collaboration (i.e., collaboration with a physician, nurse, and 2 additional health care professionals) while treating persons with Parkinson's disease.
Adherence to Guidelines and Protocols
A minority of physiotherapists in hospitals (19%) reported that they used the European guidelines for physiotherapy while treating PwPD and this was even less common in primary care units (11%) and the community (3%). Local protocols for treatment of PwPD were used by 49% of physiotherapists in hospitals whilst the corresponding proportions were 35% in primary care units and 24% in the community. Barriers to using guidelines for treating PwPD were similar between work settings; approximately one of three physiotherapists (range, 29‐33%) reported accessibility as a barrier whereas one of four (range, 23‐24%) found guidelines to be comprehensive and difficult to interpret.
Needs for Gaining Expertise Regarding PD
Irrespective of work setting, a majority of the physiotherapists perceived a need to increase their knowledge about PD (range, 74‐96%), skills about the assessment and treatment of PwPD (range, 79‐90%) and measurement tools (range, 84‐90%).
Discussion
The present study sheds light on physiotherapy provision across work settings in the Swedish health care system. As PD is a complex heterogeneous disease,19 adequate assessment and optimal selection of physiotherapeutic interventions8 require PD‐specific knowledge and skills. However, consistent with findings by Nijkrake et al., which found that physiotherapists in the Netherlands treated <10 PwPD per year,12 most physiotherapists in our study treated approximately 10 to 20 PwPD per year and perceived that they had limited PD‐specific expertise regarding physiotherapy for PwPD. Moreover, PwPD have expressed a need for increasing the accessibility to health care professionals with PD‐expertise.20, 21 Accordingly, the present findings highlight the need to strengthen the PD‐specific expertise regarding assessment and treatment of PwPD among physiotherapists in Sweden.
Although physiotherapists in Sweden treated a wide range of PD impairments and activity limitations few physiotherapists treated freezing of gait. This despite that freezing of gait is a devastating feature related to falls22, 23 and present among approximately 50% in the mild to moderate stage of PD.24 This was an unexpected finding, partly due the drastic nature of freezing of gait but also as physiotherapeutic interventions have shown to be beneficial for freezing of gait, e.g. cued task‐specific training.25, 26 Contrasting the findings for freezing of gait, a majority (>80%) of the physiotherapists in our study reported that they treated gait. As “gait” represents a more generic target for treatment compared to “freezing of gait”, we believe that this discrepant result was caused by the high proportion of non PD‐specialists among the respondents. Similarly, few physiotherapists (≤ 27%) in our study treated pain in their management of PwPD. Although 70% and 40% of PwPD report musculoskeletal and dystonic pain, respectively27 pain remains often untreated by the health care professionals.28, 29 Therefore, to improve the management and treatment of pain for PwPD, implementing a multidisciplinary approach including physicians and rehabilitation experts (e.g. tailored exercise prescription by physiotherapists)30 has recently been proposed.31 We speculate that limited PD‐expertise among physiotherapists in the present study is a potential reason for why freezing of gait and pain often remained untreated. Still, the link between expertise and clinical decision making among physiotherapists requires further investigation.
Despite the uncertainty regarding the efficacy for multi‐professional care of PwPD2, 32, 33, 34 there is a strong belief that the complexity of PD is best managed through comprehensive multi‐disciplinary care.1 Our data clearly show that a majority of the physiotherapists in our sample were treating PwPD in the absence of a multi‐professional context, or at best together with a physician, nurse or occupational therapist. In fact, the finding that only 1 to 8% of physiotherapists in primary care units and the community treated PwPD in a multi‐professional manner (see Fig. 3) is quite remarkable and concerning. Physiotherapists in these work settings, similar to findings from the Netherlands,12 also reported limited insight into the role of other health care professional treating PwPD which has been highlighted as a barrier for multi‐professional care.1 Importantly, our study captured data on an individual level; however it is likely that the actual barriers for multi‐professional care arise from the organization providing health care. Therefore, future studies focusing on barriers for multi‐professional collaboration at multiple levels of health care (e.g. the structure of the organization of health care, national guidelines and decision makers) are warranted.
In line with previous findings from the field of rehabilitation,35, 36 infrequent use of recommended measurement tools for PwPD was observed among physiotherapists in the present study. Noteworthy, the limited utilization of these recommended tools was most evident for more time‐consuming multi‐item tools (e.g. BBS and Mini‐BESTest) and tools targeting fall‐related psychological issues (e.g. FES‐I and ABC). The latter finding is somewhat surprising since FES‐I and ABC are self‐administered questionnaires that could be administered before seeing the physiotherapist. We speculate that the infrequent use of these measurement tools mirror the limited PD expertise perceived by a majority of physiotherapists in this study. Alternatively, as more generic tools were frequently used by physiotherapists (e.g. TUG) it is possible that physiotherapists prioritize tools that can be used across different patient groups. Furthermore, physiotherapists in Sweden primarily used local protocol as guidance for treatment of PwPD whereas few physiotherapists adhered to the European guidelines for physiotherapy.8 Although our study provides an indication of the barriers for using guidelines by physiotherapists (i.e. accessibility and comprehensiveness) the reasons for poor compliance is still inconclusive. However, we acknowledge that our study was conducted approximately 9 months after the publication of the European physiotherapy guidelines for PD was published and we thereby suggests future studies to follow‐up on compliance to these guidelines in European countries. Nevertheless, it is reasonable to highlight the need to facilitate adherence to measurement tools and physiotherapy guidelines as both are important for transparency and quality of care.8, 37
Our results also reveal variations in the provision of physiotherapeutic interventions across work settings. Specifically, physiotherapy was provided in a nearly 60:40 distribution between individual and group treatment in hospitals and primary care units. On the contrary, in line with findings by Keus et al.,13 physiotherapists in the community predominantly (88%) treated PwPD on an individual basis. Longer treatment durations (>6 weeks) of PwPD were more common at primary care units (82%) compared to hospitals (44%) and the community (49%). We believe that the diversity of physiotherapy between work settings represents the different roles of these services in the Swedish health care system. Intuitively, extended treatment periods including a mix of individual and group treatment match the role of primary care units as providers of PD specific treatment whilst shorter treatment periods in the community fulfil their primary role of providing rehabilitation services delivered in the home or in nursing home settings. As physiotherapy in hospitals was more varied regarding treatment form and duration, the role of physiotherapy provided at hospitals likely entails a divided role between specialized consultancy (e.g. acute assessments and care) and out‐patient care. While this survey has provided important insight and areas for improvement in the current physiotherapy care in Sweden for PwPD, future studies should focus on whether these findings transfer to other health care systems.
This study presents with some methodology considerations that require attention. Importantly, we were not aiming to recruit a representative sample of all physiotherapists working in Sweden instead we aimed to explore physiotherapy provision among therapists who treated PwPD on a regularly basis. This led to a study sample which constituted 24% of the targeted population (705 out of 2596 physiotherapists). This, combined with the relative low response rate of 40%, may limit the generalizability of this work. On the other hand, there are approximately 22 000 PwPD in Sweden14 and it seems reasonable that our study sample of 705 responders serve as the core group of physiotherapists providing care for PwPD in Sweden. In line with this, the distribution between gender, age and highest level of education were similar between the study sample and the targeted population (see Table 1).15 Finally, we acknowledge the methodological limitations of surveys; i.e. the reported physiotherapy practice may not necessary reflect actual practice as the results of surveys are likely to rely on the interpretation of questions. Further, some items were formulated with a leading tone (e.g. “I have limited insight” and “guidelines are difficult to interpret”) which could have negatively affected respondents’ perception of their expertise or physiotherapy treatment.
In conclusion, our findings emphasize the need to strengthen the expertise regarding assessment and treatment of PwPD among physiotherapists in Sweden and to apply strategies endorsing multi‐professional collaborations for PD rehabilitation. In order to offer expert physiotherapy care for PwPD, it is important to provide PD‐specific education to physiotherapists and implement national guidelines. This survey further indicates a need among physiotherapists in Sweden, especially among those working in the community, for professional development regarding physiotherapy for PwPD. We encourage future investigations of barriers for multi‐professional collaboration, compliance to physiotherapy guidelines and utility of measurement tools, as well as studies of the link between expertise and clinical decision making among physiotherapists treating PwPD.
Author Roles
1. Research Project: A. Conception, B. Organization, C. Execution; 2. Statistical Analysis: A. Design, B. Execution, C. Review and Critique; 3. Manuscript Preparation: A. Writing the First Draft, B. Review and Critique.
D.C.: 1C, 2A, 2B, 3A
B.L.: 1A, 1C, 2A, 2C, 3B
M.H.: 1A, 2A, 2C, 3B
M.H.N.: 1A, 2C, 3B
E.F.: 1A, 1B, 1C, 2A, 2C, 3B
Disclosures
Ethical Compliance Statement: We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.Funding Sources and Conflict of Interest: This study was supported by the Swedish Research Council;, the Swedish Research Council for Health, Working Life and Welfare (FORTE); “Vårdalstiftelsen,” and the Swedish Parkinson Foundation. The authors report no conflicts of interest.Financial Disclosures for the previous 12 months: David Conradsson was employed at the Karolinska Institutet, McGill University, and the Karolinska University Hospital. Breiffni Leavy was employed at the Karolinska Institutet and the Stockholms Sjukhem Foundation. Maria Hagströmer was employed at the Karolinska Institutet and the Karolinska University Hospital. Maria H. Nilsson was employed at the Faculty of Medicine, Lund University. Erika Franzén was employed at the Karolinska Institutet, the Stockholms Sjukhem Foundation, and the Karolinska University Hospital.
Supporting information
Table S1. Domains, item descriptions, and responses included in the 6 sections of the web survey.
Acknowledgements
We thank Kamilla Nylund and the physiotherapists who participated in development of the web survey as well as the Swedish Association of Physiotherapists for their collaboration.
Supporting information may be found in the online version of this article.
Relevant disclosures and conflicts of interest are listed at the end of this article.
References
- 1. Post B, van der Eijk M, Munneke M, Bloem BR. Multidisciplinary care for Parkinson's disease: not if, but how!. Postgrad Med J 2011;87:575–578. [DOI] [PubMed] [Google Scholar]
- 2. van der Marck MA, Bloem BR, Borm GF, Overeem S, Munneke M, Guttman M. Effectiveness of multidisciplinary care for Parkinson's disease: a randomized, controlled trial. Mov Disord 2013;28:605–611. [DOI] [PubMed] [Google Scholar]
- 3. Horstink M, Tolosa E, Bonuccelli U, et al. Review of the therapeutic management of Parkinson's disease. Report of a joint task force of the European Federation of Neurological Societies (EFNS) and the Movement Disorder Society‐European Section (MDS‐ES). Part II: late (complicated) Parkinson's disease. Eur J Neurol 2006;13:1186–1202. [DOI] [PubMed] [Google Scholar]
- 4. Schrag A, Jahanshahi M, Quinn N. How does Parkinson's disease affect quality of life? A comparison with quality of life in the general population. Mov Disord 2000;15:1112–1118. [DOI] [PubMed] [Google Scholar]
- 5. Allen NE, Sherrington C, Paul SS, Canning CG. Balance and falls in Parkinson's disease: a meta‐analysis of the effect of exercise and motor training. Mov Disord 2011;26:1605–1615. [DOI] [PubMed] [Google Scholar]
- 6. Tomlinson CL, Patel S, Meek C, et al. Physiotherapy versus placebo or no intervention in Parkinson's disease. Cochrane Database Syst Rev 2013;7:CD002817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shen X, Wong‐Yu IS, Mak MK. Effects of exercise on falls, balance, and gait ability in Parkinson's disease: a meta‐analysis. Neurorehabil Neural Repair 2016;30:512–527. [DOI] [PubMed] [Google Scholar]
- 8. Keus S, Munneke M, Graziano M, et al. European physiotherapy guideline for Parkinson's disease: development and implementation. Mov Disord 2014;29:S537. [Google Scholar]
- 9. Bloem BR, Marinus J, Almeida Q, et al. Measurement instruments to assess posture, gait, and balance in Parkinson's disease: critique and recommendations. Mov Disord 2016;31:1342–1355. [DOI] [PubMed] [Google Scholar]
- 10. Keus SH, Munneke M, Nijkrake MJ, Kwakkel G, Bloem BR. Physical therapy in Parkinson's disease: evolution and future challenges. Mov Disord 2009;24:1–14. [DOI] [PubMed] [Google Scholar]
- 11. Morris ME, Martin CL, Schenkman ML. Striding out with Parkinson disease: evidence‐based physical therapy for gait disorders. Phys Ther 2010;90:280–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nijkrake MJ, Keus SH, Oostendorp RA, et al. Allied health care in Parkinson's disease: referral, consultation, and professional expertise. Mov Disord 2009;24:282–286. [DOI] [PubMed] [Google Scholar]
- 13. Keus SH, Bloem BR, Verbaan D, et al. Physiotherapy in Parkinson's disease: utilisation and patient satisfaction. J Neurol 2004;251:680–687. [DOI] [PubMed] [Google Scholar]
- 14. Lökk J, Borg S, Svensson J, Persson U, Ljunggren G. Drug and treatment costs in Parkinson's disease patients in Sweden. Acta Neurol Scand 2012;125:142–147. [DOI] [PubMed] [Google Scholar]
- 15. Swedish Association of Physiotherapists . Statistics of Physiotherapists Working in Sweden. Stockholm, Sweden: Swedish Association of Physiotherapists; 2015. [Google Scholar]
- 16. Keus SHJ, Wallraf J, Burfeind FRM, Munneke M. Learning Needs and Barriers in the Physiotherapeutic Care in Parkinson Disease–A Starting Point for a European Guideline. Amsterdam; Netherlands: European School of Physiotherapy; 2011. [Google Scholar]
- 17. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. National Board of Health and Welfare . Care in Multiple Sclerosis and Parkinson's Disease‐Summary of Areas for Improvement. Stockholm, Sweden: National Board of Health and Welfare; 2016. [Google Scholar]
- 19. Jankovic J. Parkinson's disease: clinical features and diagnosis. J Neurol Neurosurg Psychiatry 2008;79:368–376. [DOI] [PubMed] [Google Scholar]
- 20. Nilsson MH, Iwarsson S, Thordardottir B, Haak M. Barriers and facilitators for participation in people with Parkinson's disease. J Parkinson Dis 2015;5:983–992. [DOI] [PubMed] [Google Scholar]
- 21. Dorsey ER, Voss TS, Shprecher DR, et al. A US survey of patients with Parkinson's disease: satisfaction with medical care and support groups. Mov Disord 2010;25:2128–2135. [DOI] [PubMed] [Google Scholar]
- 22. Paul SS, Canning CG, Sherrington C, Lord SR, Close JC, Fung VS. Three simple clinical tests to accurately predict falls in people with Parkinson's disease. Mov Disord 2013;28:655–662. [DOI] [PubMed] [Google Scholar]
- 23. Latt MD, Lord SR, Morris JG, Fung VS. Clinical and physiological assessments for elucidating falls risk in Parkinson's disease. Mov Disord 2009;24:1280–1289. [DOI] [PubMed] [Google Scholar]
- 24. Tan DM, McGinley JL, Danoudis ME, Iansek R, Morris ME. Freezing of gait and activity limitations in people with Parkinson's disease. Arch Phys Med Rehabil 2011;92:1159–1165. [DOI] [PubMed] [Google Scholar]
- 25. Mak MK, Hui‐Chan CW. Cued task‐specific training is better than exercise in improving sit‐to‐stand in patients with Parkinson's disease: A randomized controlled trial. Mov Disord 2008;23:501–509. [DOI] [PubMed] [Google Scholar]
- 26. Nieuwboer A, Kwakkel G, Rochester L, et al. Cueing training in the home improves gait‐related mobility in Parkinson's disease: the RESCUE trial. J Neurol Neurosurg Psychiatry 2007;78:134–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Beiske AG, Loge JH, Ronningen A, Svensson E. Pain in Parkinson's disease: prevalence and characteristics. Pain 2009;141:173–177. [DOI] [PubMed] [Google Scholar]
- 28. Chaudhuri KR, Prieto‐Jurcynska C, Naidu Y, et al. The nondeclaration of nonmotor symptoms of Parkinson's disease to health care professionals: an international study using the Nonmotor Symptoms Questionnaire. Mov Disord 2010;25:704–709. [DOI] [PubMed] [Google Scholar]
- 29. Ha AD, Jankovic J. Pain in Parkinson's disease. Mov Disord 2012;27:485–491. [DOI] [PubMed] [Google Scholar]
- 30. Allen NE, Moloney N, van Vliet V, Canning CG. The rationale for exercise in the management of pain in Parkinson's disease. J Parkinsons Dis 2015;5:229–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Geroin C, Gandolfi M, Bruno V, Smania N, Tinazzi M. Integrated approach for pain management in Parkinson disease. Curr Neurol Neurosci Rep 2016;16:28. [DOI] [PubMed] [Google Scholar]
- 32. Tickle‐Degnen L, Ellis T, Saint‐Hilaire MH, Thomas CA, Wagenaar RC. Self‐management rehabilitation and health‐related quality of life in Parkinson's disease: a randomized controlled trial. Mov Disord 2010;25:194–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wade DT, Gage H, Owen C, Trend P, Grossmith C, Kaye J. Multidisciplinary rehabilitation for people with Parkinson's disease: a randomised controlled study. J Neurol Neurosurg Psychiatry 2003;74:158–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. van der Marck MA, Munneke M, Mulleners W, et al. Integrated multidisciplinary care in Parkinson's disease: a non‐randomised, controlled trial (IMPACT). Lancet Neurol 2013;12:947–956. [DOI] [PubMed] [Google Scholar]
- 35. Haigh R, Tennant A, Biering‐Sorensen F, et al. The use of outcome measures in physical medicine and rehabilitation within Europe. J Rehabil Med 2001;33:273–278. [DOI] [PubMed] [Google Scholar]
- 36. Torenbeek M, Caulfield B, Garrett M, Van Harten W. Current use of outcome measures for stroke and low back pain rehabilitation in five European countries: first results of the ACROSS project. Int J Rehabil Res 2001;24:95–101. [DOI] [PubMed] [Google Scholar]
- 37. Jette DU, Halbert J, Iverson C, Miceli E, Shah P. Use of standardized outcome measures in physical therapist practice: perceptions and applications. Phys Ther 2009;89:125–135. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Domains, item descriptions, and responses included in the 6 sections of the web survey.


