Abstract
Introduction
Nowadays, gambling disorder (GD) is a worldwide health issue and there is a growing need to both improve our understanding of this disorder and to tailor specific interventions for its treatment. Moreover, theoretical models and preliminary empirical results suggest that difficulty in regulating emotional states might be involved in GD. However, literature describing clinical and theoretical aspects of emotional dysregulation among pathological gamblers (PGs) shows a lack of systematic description.
Objectives
We aimed to provide, within an exhaustive theoretical framework of emotion regulation (ER) processing, empirical evidence supporting a conceptual model of GD as an ER affliction.
Methods
We commented on empirical evidence on the relationship between ER and GD in the light of two main conceptual models of emotion (dys)regulation.
Results
The results suggest there are actual deficits of ER processing among PGs, manifesting themselves through different ways and in different steps of the ER timeline. In addition, dysregulation of positive emotions may play a central role in GD. From a clinical point of view, we pointed out that deficits in ER might be multiple in nature and an assessment for GD should be accurate to identify the specific components accounting for the development and maintenance of the disorder. It should also orientate the clinician in selecting therapeutic objectives.
Conclusions
The nature of emotional states that are difficult to regulate might account for the GD severity and indicate the subtype of PGs the patient belongs to. Treatment programs should be tailored on the specificity of PGs.
Keywords: gambling disorder, emotion regulation, alexithymia, impulsivity, metacognition
Introduction
Gambling disorder (GD), with its prevalence rate of 0.12%–5.8% (Calado & Griffiths, 2016), is currently considered a major public health issue. Noteworthy, diagnostic criteria include a reference to a modification of mood tone and emotional experience, suggesting that gambling serves as a regulator of dysphoric affects (Rosenberg & Feder, 2014). Theoretically, most authors attempting to understand the psychological factors underlying GD have often indirectly suggested the centrality of failures in emotion regulation (ER; Blaszczynski & Nower, 2002; Jacobs, 1986; Lesieur, 2001; McCormick, 1988; McDougall, 2004; Olsen, Lugo, & Sutterlin, 2015; Sharpe, 2002). ER refers to a transdiagnostic construct that is relevant to a wide range of disorders and is defined as the ability to modulate valence, intensity, or time course of one’s emotional experience and expression coherently with one’s goals and desires (Garofalo, Velotti, & Zavattini, 2013; Gross, 1998; Thompson, 1990; Velotti & Garofalo, 2015). Some theories argued for an involvement of specific components of emotion dysregulation in definite impairments of pathological gamblers’ (PGs) psychological functioning. For instance, the somatic markers theory of addiction (Olsen et al., 2015) stated that difficulties in emotion processing account for abnormal decision-making in GD.
In addition, literature (Milosevic & Ledgerwood, 2010) suggested that the nature of ER motivations underlying gambling activity differentiates between groups of PGs. For instance, McCormick (1988) distinguished between over-stimulated gamblers who gamble in order to decrease level of arousal and understimulated gamblers who gamble in order to modify a state of boredom, experienced as unbearable. This idea has further been integrated with the hypothesis that early learning experiences (i.e., frequent or big wins) lead to dysfunctional gambling behavior because of their association with a modification of arousal levels (Sharpe, 2002). Similarly, Lesieur (2001) differentiated between action seekers, having high levels of sensation-seeking and gambling in order to thrill and experience adrenaline and escape seekers gamblers, with high levels of depressed mood and gambling to escape from negative emotional states. In addition, the Blaszczynski and Nower’s (2002) pathways model of GD differentiated between three subtypes of PGs, namely the behaviorally conditioned, the emotionally vulnerable, and the antisocial-impulsivist. The second one is characterized by premorbid depression and/or anxiety and gambles essentially to escape from dysphoric mood states. On the contrary, the third subtype shows high impulsivity, low tolerance for boredom, and antisocial personality traits. Finally, the biopsychosocial model of Sharpe (2002) further extended these considerations, arguing that horse race gamblers, with high levels of sensation-seeking, would gamble in order to relieve from boredom, whereas slot machines gamblers would gamble to escape from stress and dysphoric mood.
Research evidenced that groups of PGs differ in relation to comorbidities (Suomi, Dowling, & Jackson, 2014). Whereas one subtype is thought to frequently suffer from depressive or anxious disorders, another would be more subject to substance abuse or cluster B personality disorder. Preliminary contributions indicate that emotional dysregulation might be involved in the relationship between GD and psychiatric conditions as mood and anxiety disorders (Lorains, Cowlishaw, & Thomas, 2011), pathological narcissism (Rogier & Velotti, 2018), borderline personality disorder (Brown, Allen, Dowling, Allen, & Dowling, 2015), and antisocial personality disorder (Blum, Leppink, & Grant, 2017; Rogier, Velotti, & Zavattini, 2017). An exhaustive model of ER-processing failures among PGs might aid in the identification of common features accounting for specific comorbidities and potential pathways by which psychiatric disorders lead to the development or maintenance of GD.
As a whole, different models referred to a multiplicity of ER deficits accounting for distinct features of GD. However, the literature describing clinical and theoretical aspects of emotional dysregulation among PGs shows a lack of systematic description within a coherent theoretical framework. For example, such models did not explain the relationships between these deficits and GD. Indeed, the processes leading to the use of gambling as an emotional regulation strategy are not clear. In addition, authors often used vague descriptions of ER deficits involved in GD, resulting in a confused understanding of the topic. It is necessary to clearly identify the nature of such variables for optimal clinical interventions. There is quite a difference in asserting that the treatment should focus on alexithymia features (i.e., a difficulty to identify and verbally express own feelings) or emotional impulsivity (i.e., a tendency to act rashly when experiencing emotional states). To bridge such gaps, the present paper offers a comment on empirical evidence supporting the relationship between ER and GD in the framework of exhaustive and refined models of dysregulation of emotions. Throughout the following sections, we will argue that GD can be conceptualized as an ER affliction in the sense that deficits in ER-processing account for etiology and maintenance of GD. Our main objective was to use validated models of ER to provide a detailed description of ER failures among PGs, adding hypotheses toward the relationship between these failures and development and maintenance of GD. In doing so, we attempted to explain how specific failures in ER act as vulnerability factors for the development of GD. In addition, we wanted to show that peculiar mechanisms of emotion dysregulation characterize and maintain GD throughout their interaction with other central cognitive, behavioral, and interpersonal variables. Finally, we suggested that an ER framework is able to explain heterogeneity within the PGs category, shedding light on the differences between subtypes of PGs and their specific comorbidities.
Methods
To achieve the aims of the study, we integrated validated models of ER-processing failures within the current understanding of GD. In doing so, we reviewed ER literature and selected two main models of ER. Within the range of ER models, researchers deserved a particular attention to the proposal of Gratz and Roemer (2004), successfully applied to the understanding of both well-being (Balzarotti, Biassoni, Villani, Prunas, & Velotti, 2016; Velotti, Garofalo, Bottazzi, & Caretti, 2017) and psychopathology (Aldao, Nolen-Hoeksema, & Schweizer, 2010; Garofalo, Holden, Zeigler-Hill, & Velotti, 2016; Garofalo & Velotti, 2015, 2017; Velotti et al., 2016). Indeed, the model avoids risks related to a vague definition of emotion dysregulation providing an integrative conceptualization of difficulties in ER. The authors assert that the construct of ER should go beyond modulation of arousal or emotional expression and encompass other components as awareness, understanding, and acceptance of emotions as well as the ability to act in desired ways regardless of emotional state. Noteworthy, the model underlines that healthy ER should consist in the capacity to modulate rather than eliminate aversive emotional states. In line with these assumptions, the authors identified four main components of emotional dysregulation, namely (a) an impaired awareness and understanding of emotions, (b) a difficulty in accepting emotional states, (c) a poor ability to refrain from impulsive behavior when experiencing negative emotional states, and (d) an inadequate perception of effective and available ER strategies.
Despite its utility, this approach suffers from important limitations, failing to describe the processual nature of healthy ER. A process model of ER seems useful to identify potential waterfall effects between different ER dysfunctions, shedding light on the components that should be targeted with priority by clinical interventions. In this sense, an exhaustive model of ER in GD would avoid errors in the selection of the strategic objectives and would prevent inefficacy of clinical interventions. Thus, we thought to complete our understanding of ER in GD using the model developed by Gross and John (2003). A model which asserts that ER process goes through a timeline consisting of five points, namely (a) situation selection, (b) situation modification, (c) attentional deployment, (d) cognitive change, and (e) response modulation. ER strategies implemented during the first four points are labeled “antecedent-focused” strategies, as the modification is carried out before the elicitation of the emotional state. On the contrary, strategies belonging to the last category are labeled “response-focused,” targeting an emotional state already raised. Recently, Sheppes, Suri, and Gross (2015) extended the model by asserting that ER processes, emerging after the arousal of emotional states, can be understood as the result of three main stages (Identification, Selection, and Implementation) with the first being preparatory for the following. Furthermore, each stage is thought to be composed of three successive operations, namely Perception, Valuation, and Action. In the Identification stage, the individual has first to adequately represent emotional state and the general goal of a regulated emotional response (Perception step). Then, during the Valuation operation, the emotional and regulated states received a value in term of costs and benefits. If the regulated state receives sufficient positive valuations, the general ER signal is activated (Action step). Supposing that this stage leads to the decision to regulate the emotional state, ER processes of the Selection stage are activated to determinate the nature of the general regulatory category that has to be used. In this stage, if the individual correctly represents available general regulatory categories (Perception step), he would be able to access to the next step, which consists of the valuation of benefits and costs related to these categories (Valuation step). If the balance benefits/costs is positive, the regulatory category would be activated (Action step). The final stage (Implementation) determines the nature of specific regulatory strategies that are to be used. Again, the individual has to correctly represent the available range of ER strategies (Perception step), to evaluate each of them in terms of benefits and costs (Valuation step) and to execute the selected one (Action step).
Given the heuristical value of these two main models of emotion (dys)regulation, our hypotheses toward the relationships between ER and GD have been discussed following the timeline model of Sheppes et al. (2015) of healthy ER processing and integrating the concepts related to specific emotion dysregulation components described in the Gratz and Roemer’s model (2004).
Results
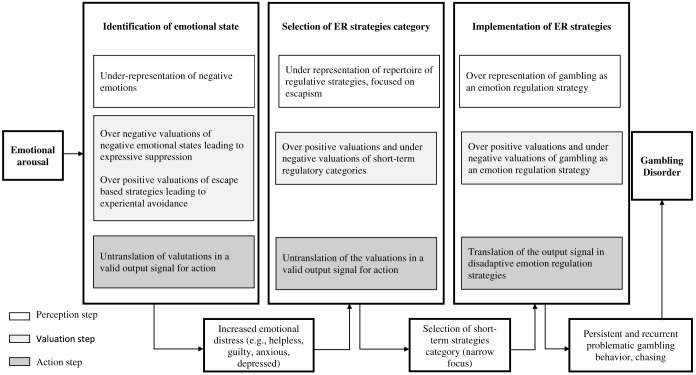
As illustrated in Figure 1, we found that empirical contributions support the hypothesis that specific failures among the three main stages of ER-processing account for the development and the maintenance of GD.
Figure 1.
Potential failures in the three main steps of ER-processing accounting for gambling disorder
Failures in the Identification stage
According to Sheppes et al. (2015), potential failures of ER processes might be identified in the early Identification stage, which occurs after the arousal of an emotional state and ends with the decision to regulate it or not.
Failures in the Perception step
Decision to regulate an emotional state or not is primarily related to the capacity to adequately represent emotions. As suggested by different empirical evidence, this ability may be impaired in individuals suffering from GD.
To this point, results drawn from studies investigating the link between GD and alexithymia are insightful. Most studies found a higher level of alexithymia in samples of PGs compared to samples of healthy subjects (Lumley & Roby, 1995; Parker, Wood, Bond, & Shaughnessy, 2005; Toneatto, Lecce, & Bagby, 2009). However, the results related to the specific dimensions of alexithymia are in contrast with some studies that find that PGs have poorest capacity to verbally express their feelings compared to control groups (Aïte et al., 2014; Parker et al., 2005; Toneatto et al., 2009) and with other studies that fail to find significant differences (Lumley & Roby, 1995). Similarly, whereas in some studies, PGs showed a normal capacity to identify emotional states; most researches evidenced a specific deficit in theses capacities (Lumley & Roby, 1995; Parker et al., 2005). Finally, research often showed significant and positive relationships between alexithymia and the severity of GD (Cosenza, Baldassare, Matarazzo, & Nigro, 2014; Elmas, Cesur, & Oral, 2017; Gori et al., 2016; Mitrovic & Brown, 2009; Parker et al., 2005).
In addition, several studies investigated the topic throughout the use of the Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004). This instrument evaluates different aspects of emotion dysregulation, such as lack of emotional awareness and emotional clarity, which fit well with the description of failures in the capacity to adequately represent emotional states. Surprisingly, some studies failed to show significant associations between GD and a general deficit in ER capacities (Ciccarelli, Nigro, Griffiths, Cosenza, & D’Olimpio, 2016; Schreiber, Grant, & Odlaug, 2012). On the other side, scholars reported empirical data supporting the hypothesis of general difficulties to regulate negative emotional states among PGs (Elmas et al., 2017; Poole, Kim, Dobson, & Hodgins, 2017; Rogier & Velotti, 2018). For example, the study of Estévez, Herrero, Sarabia, and Jauregui (2014) showed that almost all DERS subscales were significantly related to GD severity. However, because of methodological limitation of the study (related to GD measure), the interpretation of such results should be cautious. More reliable data supporting a connection between emotion dysregulation and GD came to light with a study carried out by Jauregui, Estevez, and Urbiola (2016), indicating high levels of emotion dysregulation among PGs as well as a positive correlation between the DERS’s scores and GD severity. However, the authors showed that non-awareness and non-clarity factors were not significantly related to the severity of GD. On the contrary, two studies (Rogier & Velotti, 2018; Williams, Grisham, Erskine, & Cassedy, 2012) found that the DERS’s subscales significantly correlated with the severity of the disorder suggesting that PGs may suffer from a difficulty in identifying and discriminating their own feelings.
As argued by Olsen et al. (2015), a difficulty to identify one’s own emotional states may lead to an impairment in decision-making. This issue is particularly relevant in relation to GD where the individual seems unable to use the information contained in an aversive emotional state related to a negative external feedback. In other words, the negative emotion related to a loss might not be used to interrupt gambling behavior and consequently favor chasing behavior.
Failures in the Valuation step
An accurate representation of emotional states is not sufficient to successfully decide whether to carry forward the emotional regulation process or not. Once the individual has perceived the emotional state, he has to evaluate costs and benefits related to both the maintenance of the emotion and a regulated state. As stressed by Sheppes et al. (2015), overestimating emotional states, together with positive beliefs toward efforts to escape from them, may lead to an overregulation of emotional states. As previously stated, an overregulation of negative emotional states is believed to be maladaptive, because it might lead to their intensification and preclude the possibility to use the information contained in emotions, which are useful for behaving in an adaptive way (Damasio, 1999).
Several empirical evidence suggest that PGs may experience failures in such thresholds. For example, some studies (Jauregui, Estevez, et al., 2016; Williams et al., 2012), which use the non-acceptance DERS’ subscale, showed that individuals with GD have a difficulty in accepting their own emotional states in a non-judgmental way, reacting with shame and disappointment. Similar results have been brought by scholars who investigated mindfulness capacity among PGs. Mindfulness refers to the ability to bring awareness and non-judgmental acceptance to one’s present moment experience of thoughts, emotions, and bodily sensations (Bishop et al., 2004). Interestingly, mindfulness is negatively related to GD severity (Lakey, Campbell, Brown, & Goodie, 2007; Reid, Di Tirro, & Fong, 2014; Riley, 2012), suggesting that PGs may have a deficit in the ability to accept emotional states in a non-judgmental way. In addition, studies on metacognition capacities among PGs provided preliminary evidence that GD severity may be related to positive beliefs toward the need to control thoughts (Jauregui, Urbiola, & Estevez, 2016; Lindberg, Fernie, & Spada, 2011; Mansueto et al., 2016; Spada & Roarty, 2015). PGs often believe that certain types of thoughts have to be suppressed, and this has been demonstrated by Riley (2012), which reported high levels of thought suppression among PGs. As outlined by Sheppes et al. (2015), disproportionate negative valuation of emotions (i.e., non-acceptance and poor mindfulness) together with disproportionate positive valuations of efforts to escape emotions have been thought to overactivate ER mechanisms and consequently lead to experiential avoidance (Sheppes et al., 2015). To this point, it has been showed that experiential avoidance mediates the link between thought suppression and mindfulness with GD severity (Riley, 2012). These failures may act as vulnerability factors for GD as an overregulation of negative emotional states (leading to heightened emotional arousal) and difficulty to accept them (leading to secondary negative emotional states), thereby increasing the ER demand the individual has to front.
Failures in the Action step
Once emotions have been correctly represented and a valuation toward the opportunity to regulate them or not has been formulated, the individual has to adequately translate such valuations in a valid output signal for action. At this point, a number of reasons may account for a failure and consequently make an obstacle for the correct ER process. Helplessness refers to the belief that, in front of adverse stimuli, the individual has no ways to control it and he has no choice but endure it. Interestingly, it has been noted that helplessness is particularly common among PGs (McCormick, 1994). Coherently with the reformulated learned helplessness theory (Abramson, Seligman, & Teasdale, 1978), GD severity is positively related to a tendency to attribute negative events to internal, global, and stable causes (McCormick & Taber, 1988). This attributional style has been related to poor malleability beliefs toward emotions in depressed individuals, leading to a view of emotions as unknowable and uncontrollable (Kneeland, Dovidio, Joormann, & Clark, 2016). Moreover, pessimistic attribution styles have been related to dysfunctional ER strategies (e.g., rumination), which in turn are associated with chasing among adult gamblers (Atlas & Peterson, 1990). Despite positive valuations of a regulated state and negative valuations of the current emotional states, PGs who experience helplessness may be unable to translate such valuations into action. Consequently, the more intense the emotional states, the less able a PG would be to achieve this threshold.
As a whole, failures in the Identification stage may account for GD because of resulting heightened arousal levels and impairments in decision-making. In addition, these elements shed light on frequent comorbidities observed between GD and other psychiatric conditions. Indeed, alexithymic features as well as experiential avoidance have been related to some of these co-occurring disorders as depression (Li, Zhang, Guo, & Zhang, 2015; Sloan et al., 2017), anxiety disorders (De Berardis et al., 2008; Newman & Llera, 2011), and borderline personality disorder (Lysaker et al., 2017; Sloan et al., 2017; Vaddiparti & Cottler, 2017). As such, ER deficits among the Identification stage of ER processing offer a potential explanation of the pathway by which these disorders lead to the development of GD.
Failures in the Selection stage
Once an individual has correctly achieved the Identification step and decided to regulate his emotional state, he has to select the more appropriate category of ER strategy to use. Again, literature suggests that PGs experience important failures among these stages.
Failures in the Perception step
To adequately decide which of the ER categories fits better with the intent to regulate emotional states, individuals need to have a correct representation of available general regulatory categories. At this level, PGs may have a limited representation of regulatory options. For example, Williams et al. (2012) and Rogier and Velotti (2018) found that GD severity was positively and significantly related to a limited capacity to access effective regulation strategies. In this sense, an underrepresentation of general regulatory categories may conceal some adaptive choices and favor extreme decisions promoting the goal of escaping self-awareness. Recent studies examining the endorsement of gambling as an escape among PGs converge toward this hypothesis (Weatherly & Cookman, 2014). In line with this reasoning, a misrepresentation of available regulatory categories may be due to a poor confidence in the ability to effectively use some of them. For example, an individual may be aware of the existence of cognitive change regulation strategies that would be an effective choice but considers himself unable to use them and consequently he would not represent them within the range of available regulatory categories. Poor self-efficacy predicts emotional dysregulation (Luberto, Cotton, McLeish, Mingione, & O’Bryan, 2014) and positive expectations toward the success of ER predict better ER performance (Bigman, Mauss, Gross, & Tamir, 2016). Directly related to this point, preliminary results showed that GD severity is related to the belief of being unable to refuse gambling when experiencing an emotional state, positive or negative (Casey, Oei, Melville, Bourke, & Newcombe, 2008). As a result, PGs may suffer from a narrow focus on escape strategies category, resulting in an underrepresentation of other available and effective regulatory categories.
Failures in the Valuation step
Despite failures in previous steps being relevant to the explanation of ER difficulties among PGs, an important role may be played by dysfunctions in the process of evaluating benefits and costs of specific regulatory categories.
The Theory of Urgency, developed by Cyders and Smith (2008a) and successfully applied to GD, seems specifically insightful. Referring to a neurobiological description of the relationship between emotions, ER, and action (Davidson, 2003), the authors assert that, within the range of variables that mediate the occurrence of an emotional state and the inhibition of its behavioral correspondent, the capacity to focus on long-term interests may be central. Indeed, an individual would inhibit an impulsive behavior related to an emotional state because of his anticipation of another one related to the frustration or the achievement of a long-term goal. However, a poor capacity to focus on course of action providing long-term benefits and a converse tendency to behave in order to obtain immediate return may invalid such ER processing. In that sense, positive past reinforcements related to escape strategies may contribute to erroneous and high valuations of the escape regulatory category (Petry, 2005). In relation to it, research focusing on the role of cognitive impulsivity among GD suggests that PGs may have difficulty in adequately planning the consequences of their behaviors by underestimating the costs of an impulsive action (Passanisi & Pace, 2017). In line with this result, some authors found a positive association between severity of GD and difficulty in pursuing goal-directed behaviors when experiencing a negative emotional state (Williams et al., 2012). Moreover, impulsive action among PGs has been related to an abnormally high focus on reward compared to the normal population (Kräplin et al., 2014).
This last point may offer an additional perspective from which discuss the issue related to the classification of GD as an addiction disorder or as an impulse control disorder (ICD). Indeed, in ICDs, behavior is thought to be pursued as a result of negative reinforcements (decreasing anxiety or stress), whereas in substance addiction, the behavior involves pleasure, being intrinsically rewarding and resulting from positive reinforcements (Fauth-Bühler, Mann, & Potenza, 2017). However, we underline that abnormal reward sensitivity plays an important role in the ER dysfunctions emerging in this step. In this perspective, cognitive impulsivity would account for GD because of its association with excessive reward sensitivity, adding further support to the classification of GD as an addiction disorder.
Failures in the Action step
The final step of the Selection process consists in triggering the general regulatory category selected. Having a clear representation and making an accurate valuation of an adaptive regulatory category are not sufficient: especially for adaptive but cognitively expensive regulatory categories, it is not assumed that individuals have the abilities required to apply them. For example, Sheppes et al. (2015) underline that cognitive change regulation strategies need perspective-taking capacities and an intact theory of mind. Despite perspective-taking is fundamentally different from cognitive reappraisal (Dunn, Billotti, Murphy, & Dalgleish, 2009), difficulties in the capacity to be objective or to view the adverse stimulus as a detached, third-person observer may alter cognitive reappraisal attempts (Webb, Miles, & Sheeran, 2012). Actually, PGs showed impaired perception of emotions in others (Kornreich et al., 2016), poor empathy, and interpersonal perspective-taking (Tomei, Besson, & Grivel, 2017). In line with this, some noted that low empathy was positively related to gambling as an escape (Weatherly & Miller, 2013). Moreover, the relationship between gambling behavior and antropomorphization of slot machines, resulting from erroneous mind attributions and being a typical cognitive bias of PGs, has been showed to relevantly increase under the influence of intense emotional arousal (Riva, Sacchi, & Brambilla, 2015).
Failures in the Selection stage probably account for the process by which deficits in ER processing lead PGs to select the escape strategies category to regulate emotional states. Noteworthy, these deficits appear to be the important candidates in the explanation of some comorbidities in GD. First, an excessive narrow focus on ER escape-based strategies is probably favored by depressive symptoms. Preliminary results indicated that depression leads to gambling behavior throughout a decreased gambling refusal self-efficacy (Takamatsu, Martens, & Arterberry, 2016). Then, high impulsivity has been indicated as a common risk factor for bipolar disorder (Saddichha & Schuetz, 2014), cluster B personality disorders (American Psychiatric Association, 2013), and attention-deficit hyperactivity disorder (Davtian, Reid, & Fong, 2012). In addition, dysfunctions in reward sensitivity might explain the frequent co-occurrence of GD with bipolar (Nusslock et al., 2012) and antisocial personality disorders (Morgan, Bowen, Moore, & van Goozen, 2014). In addition, depression seems to increase abnormal responses to monetary rewards among PGs (Fauth-Bühler et al., 2014). Finally, impaired theory of mind has been showed to characterize both major depression and borderline personality disorder, potentially acting as a vulnerability factor for the development of GD (Richman & Unoka, 2015)
Failures in the Implementation stage
Once Identification and Selection stages have been achieved, ER processing goes through a final level, which consists of the decision of which specific ER tactic is to be used (Sheppes et al., 2015). In relation to GD, a number of hypotheses regarding the nature of potential failures occurring in the Implementation stage can be formulated.
Failures in the Perception step
To make a successful decision, one must correctly represent the range of available regulatory tactics belonging to the broader regulatory category that was previously selected.
Interestingly, Hudson, Jacques, and Stewart (2013) divided gamblers into three categories according to predominant motivation, resulting in two categories related to emotional motives. They pointed out the presence of attentive biases congruent with the motivation categories. In this way, the study opened the possibility of a link between some perceptive aspects and the use of gambling as an ER strategy, specifically evident at high levels of severity of the disorder. Therefore, the study suggested that specific attentive biases underline an erroneous representation of the available range of ER strategies among PGs.
Failures in the Valuation step
The representation of available regulatory tactics is followed by their evaluations, in term of costs and benefits in order to formulate an optimal choice.
Again, research on metacognitions among PGs brought interesting results. Some studies indicate that PGs have high levels of positive beliefs toward the use of perseverative thinking (Jauregui, Urbiola, et al., 2016; Mansueto et al., 2016; Spada & Roarty, 2015). More closely related to the addictive behavior, it seems that, as previously discussed for alcohol drinking (Cooper, Frone, Russell, & Mudar, 1995; Garofalo & Velotti, 2015), PGs have high expectancies toward the efficiency of gambling as a regulatory strategy. For example, Spada, Giustina, Rolandi, Fernie, and Caselli (2015) examined metacognitive beliefs toward gambling and showed that PGs consider gambling as a useful strategy to improve cognitive-emotional state. Finally, a very recent study indicated that specific metacognition beliefs about gambling were significantly associated with GD severity among a sample of PGs (Caselli et al., 2018).
In line with these results, studies examining self-reported motivations for gambling are specifically insightful. Two studies (MacLaren, Harrigan, & Dixon, 2012; Shead & Hodgins, 2009) evidenced that most PGs described themselves as motivated by a positive valuation of gambling activity due to its capacity to regulate negative or positive emotional states. In addition, Weatherly and Cookman (2014) observed that gambling to escape from negative emotions strongly predicted GD severity and was positively predicted by every subscale of the DERS.
Finally, empirical evidence shows that PGs have an impaired awareness toward their success in gambling task (Brevers et al., 2014), failing to objectively evaluate the negative consequences of gambling activity. Such results confirmed previous research on typical overconfidence bias among PGs (Fortune & Goodie, 2012; Goodie, 2005). Therefore, high expectancies toward the benefits associated with gambling activities (in terms of emotional relief) seem to be combined with a pathological underestimation of the potential costs of such ER tactic among PGs.
Failures in the Action step
The final step in the ER processing requires the ability to trigger the specific regulatory tactic that was previously selected. In addition to the gambling behavior, PGs may implement other maladaptive ER strategies, reinforcing gambling behavior, and increasing ER challenges.
Surprisingly, PGs in the study by Williams et al. (2012), which showed high levels of emotional dysregulation, did not differ from healthy participants in the measure of reappraisal or suppression. Similarly, Barrault, Bonnaire, and Herrmann (2017), among their sample of regular poker players, did not find any association between ER strategies and GD severity. On the contrary, Navas et al. (2017) observed that PGs were particularly inclined to suppress the expression of emotional states, compared with healthy subjects. The results brought by Canale, Verzeletti, Cavallari, Pastore, and Santinello (2013) confirmed such findings but underlined that the use of reappraisal was not associated with GD severity. However, the frequency of gambling among women correlated positively with the tendency to reformulate the meaning of a situation in order to reduce its emotional impact (reappraisal). This result, apparently counterintuitive, may be explained by the fact that focusing on positive aspects of an aversive situation may be counterproductive in a context of gambling, leading the individual to chase. In line with this conclusion, Heilman, Crişan, Miclea, Miu, and Houser (2010) brought similar results examining the effect of reappraisal and suppression in a task of decision-making. Researchers found that the use of reappraisal toward negative emotions was associated with the reduction of risk avoidance and consequently with the promotion of risky decisions. This data goes in the same direction of studies where reappraisal has been found to reduce arousal related to risk aversion (Sokol-Hessner et al., 2009). Similarly, Navas, Verdejo-García, López-Gómez, Maldonado, and Perales (2016) observed that PGs were more inclined to use positive refocusing strategy than the healthy subjects. Researchers highlight that this strategy involves the displacement of attention from negative emotions without a cognitive processing of information related to the causes of the emotion. The study also evidenced that gamblers made a great use of dysfunctional cognitive-type ER strategies, such as catastrophizing and self-blame. On the contrary, Pace, Zappulla, Di Maggio, Passanisi, and Craparo (2015) found that PGs made a minor use of reappraisal compared to both non-PGs and problematic gamblers, whereas differences did not emerge in relation to suppression. Such discrepancy may be due to the nature of the sample, probably encompassing slot machines gamblers only in a minor measure.
As a whole, failures in the Implementation stage lead the individual to select and implement gambling behavior as an ER strategy. Moreover, some of these failures might be reinforced in case of specific comorbidities. For example, individuals with narcissistic personality disorder suffer from abnormal overconfidence toward their performance and may be specifically vulnerable to fail in the valuation of costs related to gambling behavior (Lakey, Rose, Campbell, & Goodie, 2008). Finally, similarities in metacognitive dysfunctions among GD and traditional addictions (Spada, Caselli, Nikčević, & Wells, 2015) suggest that common impairments in the Implementation stage of ER processing could partially account for their frequent co-occurrence.
Discussion
Our paper aimed to provide, within an exhaustive theoretical framework of ER processing, empirical evidence supporting a conceptual model of GD as an ER affliction. At this point of the paper, we are allowed to draw some conclusions. First, the research evidences actual deficits of ER processes among the addicted gamblers, manifested in different ways and in different stages of the ER timeline. The studies suggest that PGs fail to functionally achieve the Identification stage because of a deficit in emotional awareness, a difficulty in accepting emotional states and a poor ER self-efficacy. Then, failures in the Selection stage may arise from a narrow and rigid focus on escape strategies, a preference for short-term reward strategies and from impaired perspective taking and theory of mind. Finally, dysfunctions in the Implementation of regulatory tactics may occur due to attentive biases related to gambling, positive metacognitive beliefs toward gambling as a regulation strategy, and an excessive expressive suppression of emotional states. We evidenced that different deficits in ER processing may lead to the development and the maintenance of GD throughout their interaction with cognitive, behavioral, and interpersonal variables. Furthermore, this conceptual model appears a helpful framework in the understanding of comorbidity in GD. Indeed, we shed light on common ER impairments underlying these disorders and on potential pathways by which they lead to the development of GD.
However, we evidenced that empirical data concerning the relationship between ER and GD are sometimes inconsistent (Ciccarelli et al., 2016; Schreiber et al., 2012). The contrasting nature of results in the GD field is potentially due to the excessive heterogeneity of this category. In relation to ER framework, it means that the relationship between emotion dysregulation and GD should be understood in the light of this heterogeneity. For example, subtyping models of GD often pointed out a central issue, mostly neglected by studies investigating the relationships between ER and GD: the regulation of positive emotions. It has been argued that difficulties to regulate positive emotional states account for psychopathology (Carl, Soskin, Kerns, & Barlow, 2013) and especially for addiction (Carroll & Huxley, 1994). In line with this, a subtype of PGs is often described as seeking strong sensation and excitement and as gambling to increase mood tone (Blaszczynski & Nower, 2002; Lesieur, 2001; Sharpe, 2002), suggesting peculiar difficulties in the regulation of positive emotions.
Several preliminary studies investigated the role of dysregulation of positive emotion in relation to GD. In situation selection and modification, PGs may have an excessive approach to positive emotions as indicated by high levels of reward sensitivity and low sensitivity to punishment (Gaher, Hahn, Shishido, Simons, & Gaster, 2015; Loxton, Nguyen, Casey, & Dawe, 2008; van Holst, van den Brink, Veltman, & Goudriaan, 2010). Another important variable that accounts for the selection of situation is affective forecasting, which is the process of anticipating the hedonic consequences of future events. In the general population, the impact bias refers to the adaptive tendency to overestimate the intensity of emotional reactions when anticipating an adverse event. Interestingly, Willner-Reid, Smith, Jones, and MacLeod (2012) noted that low levels of impact bias among PGs account for an exaggerate motivation to approach to hedonistic but potentially risky situations. In addition, attentional deployment dysfunctions may account for GD as some studies suggested that PGs have an excessive attendance to positive stimuli (Hudson et al., 2013; Molde et al., 2010). In relation to the processes of cognitive changes for positive emotionality, we previously discussed evidence suggesting that PGs excessively employ reappraisal and positive refocusing to upregulate positive emotions (Navas et al., 2016, 2017). Finally, response-focused strategies in relation to positive emotions have been associated with GD as wishful thinking (Jauregui, Onaindia, & Estévez, 2017; Scannell, Quirk, Smith, Maddern, & Dickerson, 2000) and emotional expression (Jauregui et al., 2017). Furthermore, interesting results came from the multidimensional investigation of impulsivity among PGs. The construct of positive urgency, developed by Cyders and Smith (2008a), fits well with the idea that PGs have difficulty in responding in an adaptive way to intense and positive emotional states. Actually, several studies showed that GD is related to high levels of this impulsive trait (Blain, Richard Gill, & Teese, 2015; Cyders & Smith, 2008b; Haw, 2017; Steward et al., 2017) and that positive urgency discriminates between at-risk and not-at-risk gamblers (Cyders et al., 2007).
However, differentiating PGs subtypes according to the valence of emotional states that they struggle to regulate may be an artificial and misleading way of reasoning, failing to restitute the complexity of ER processing in psychological functioning. For instance, Stewart, Zack, Collins, and Klein (2008) examined whether affective motivations for gambling were congruent with motivations for alcohol abuse. In some individuals, the motivation for drinking was coherent with the motivation for gambling as the use of alcohol to relieve oneself from negative emotional states. However, PGs who gamble to increase emotional activation drink to front negative but not positive emotional states. Such result highlights that a subtype of PGs may have a difficulty regulating positive emotions, self-medicated throughout gambling, and a difficulty in regulating negative emotions compensated with alcohol use. In other words, ER difficulties among PGs do not seem consistent and may concern both negative and positive emotions. In addition, this framework is a useful perspective from which disentangle the question of the classification (impulse control vs. addiction disorders) of GD, providing further understanding of the role of both positive and negative reinforcements accounting for the disorder. Therefore, it seems rather more convincing to assert that difficulty in regulating negative emotional states would be a common factor shared by all gamblers, whereas difficulty in regulating positive emotions would be an additional characteristic of only a subtype of gamblers. Again, it highlighted the proficiency of the use of ER framework in the study of GD, promising in its capacity to shed light on aspects still unknown of the disorder and to provide a coherent appreciation of the complexity of the issue in the whole population of PGs.
From a clinical point of view, our model of GD as an ER affliction suggests some interesting implications. We underlined that gambling activity may develop within a previous deficit in ER capacities serving as a regulator of intense emotional states. However, we pointed out that such deficits might be multiple in nature and assessment for GD should consequently be accurate in order to identify the specific components that account for the development and maintenance of the disorder as well as for the potential comorbidity with other psychopathologies. Noteworthy, if several deficits in ER are identified, dysfunctions related to the Identification stage, as alexithymic features, should be treated with priority. For example, it would be ineffective to address a problem of emotional impulsivity without previously treating a difficulty in emotional awareness. In addition, we argued that the nature of emotional states, which are difficult to regulate, might account for the severity of the disorder and be an indicator of which subtype of PGs the patient belongs to. At this point, treatment programs should be tailored to the specificity of PGs. For example, interventions that target a difficulty in regulating negative emotional states might be useful for the emotionally vulnerable and the antisocial-impulsivity subtypes of gamblers, whereas only this last category might also benefit from a treatment focusing on the difficulty to regulate positive emotions.
Some of the conclusions just presented need further empirical evidence to be considered more than just hypothetical suppositions. First, future studies should attempt to further explain the contrasting nature of the results obtained in studies investigating alexithymia and impulsivity as in researches examining ER capacities of PGs through the use of the DERS and the ERQ. Moreover, empirical studies are urged to better examine the role of dysregulation of positive emotions and its relationship with dysregulation of negative emotions in GD. Then, these studies should consider the role of comorbidity with disorders that may be related to GD and dysregulation of both negative (such as depression and anxiety) and positive (such as antisocial personality disorder) emotional states. For example, further research is requested to explore the dysregulative role of helplessness and pessimism played in GD, controlling for the effect of depression. In relation to this, the useful constructs of emotional malleability and ER self-efficacy would be specifically proficient. In addition, there is a lack of studies that examine attentive biases of PGs toward emotional stimuli (both positive and negative) related to ER capacities. Such a line of research would allow an increased understanding of potential failures in the Perception step of ER processing. Moreover, despite promising preliminary results, few studies investigate the role of metacognition among PGs and none in relation to ER: such a gap has to be fulfilled in order to better understand whether metacognitive beliefs actually play a role in emotion dysregulation among PGs (Velotti, Rogier, & Lysaker, 2018). In addition, in relation to positive emotion dysregulation, no studies investigated the use of specific emotional strategies, such as savoring (Bryant, 2003) among PGs. Finally, our paper did not focus on another relevant topic related to ER, namely flexibility in the use of ER strategies. Indeed, as previously stated (Rogier, Garofalo, & Velotti, 2017; Velotti, Garofalo, & Zavattini, 2013), flexibility is an important characteristic of healthy ER processes. As such, further attention should be paid to the monitoring and switching capacities of PGs in order to better understand the ER deficits underlying the disorder.
Funding Statement
Funding sources: None.
Authors’ contribution
GR was involved in study concept and design, review of literature, interpretation of data, and manuscript drafting. PV was involved in study concept and design, analysis and interpretation of literature, study supervision, critical revision, and manuscript drafting.
Conflict of interest
The authors declare no conflict of interest.
References
- Aïte A., Barrault S., Cassotti M., Borst G., Bonnaire C., Houdé O., Moutier S. (2014). The impact of alexithymia on pathological gamblers’ decision making: A preliminary study of gamblers recruited in ‘sportsbook’ casinos. Cognitive and Behavioral Neurology, 27(2), 59–67. doi: 10.1097/WNN.0000000000000027 [DOI] [PubMed] [Google Scholar]
- Abramson L. Y., Seligman M. E., Teasdale J. D. (1978). Learned helplessness in humans: Critique and reformulation. Journal of Abnormal Psychology, 87(1), 49–74. doi: 10.1037/0021-843X.87.1.49 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Aldao A., Nolen-Hoeksema S., Schweizer S. (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30(2), 217–237. doi: 10.1016/j.cpr.2009.11.004 [DOI] [PubMed] [Google Scholar]
- Atlas G. D., Peterson C. (1990). Explanatory style and gambling: How pessimists respond to losing wagers. Behaviour Research and Therapy, 28(6), 523–529. doi: 10.1016/0005-7967(90)90139-A [DOI] [PubMed] [Google Scholar]
- Balzarotti S., Biassoni F., Villani D., Prunas A., Velotti P. (2016). Individual differences in cognitive emotion regulation: Implications for subjective and psychological well-being. Journal of Happiness Studies, 17(1), 125–143. doi: 10.1007/s10902-014-9587-3 [DOI] [Google Scholar]
- Barrault S., Bonnaire C., Herrmann F. (2017). Anxiety, depression and emotion regulation among regular online poker players. Journal of Gambling Studies, 33(4), 1039–1050. doi: 10.1007/s10899-017-9669-3 [DOI] [PubMed] [Google Scholar]
- Bigman Y. E., Mauss I. B., Gross J. J., Tamir M. (2016). Yes I can: Expected success promotes actual success in emotion regulation. Cognition and Emotion, 30(7), 1380–1387. doi: 10.1080/02699931.2015.1067188 [DOI] [PubMed] [Google Scholar]
- Bishop S. R., Lau M., Shapiro S., Carlson L., Anderson N. D., Carmody J., Segal Z., Abbey S., Speca M., Velting D., Devins G. (2004). Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11(3), 230–241. doi: 10.1093/clipsy.bph077 [DOI] [Google Scholar]
- Blain B., Richard Gill P., Teese R. (2015). Predicting problem gambling in Australian adults using a multifaceted model of impulsivity. International Gambling Studies, 15(2), 239–255. doi: 10.1080/14459795.2015.1029960 [DOI] [Google Scholar]
- Blaszczynski A., Nower L. (2002). A pathways model of problem and pathological gambling. Addiction, 97(5), 487–499. doi: 10.1046/j.1360-0443.2002.00015.x [DOI] [PubMed] [Google Scholar]
- Blum A. W., Leppink E. W., Grant J. E. (2017). Neurocognitive dysfunction in problem gamblers with co-occurring antisocial personality disorder. Comprehensive Psychiatry, 76, 153–159. doi: 10.1016/j.comppsych.2017.05.004 [DOI] [PubMed] [Google Scholar]
- Brevers D., Cleeremans A., Bechara A., Greisen M., Kornreich C., Verbanck P., Noël X. (2014). Impaired metacognitive capacities in individuals with problem gambling. Journal of Gambling Studies, 30, 141–152. doi: 10.1007/s10899-012-9348-3 [DOI] [PubMed] [Google Scholar]
- Brown M., Allen J., Dowling N., Allen J. S., Dowling N. A. (2015). The application of an etiological model of personality disorders to problem gambling. Journal of Gambling Studies, 31(4), 1179–1199. doi: 10.1007/s10899-014-9504-z [DOI] [PubMed] [Google Scholar]
- Bryant F. B. (2003). Savoring Beliefs Inventory (SBI): A scale for measuring beliefs about savoring. Journal of Mental Health, 12(2), 175–196. doi: 10.1080/0963823031000103489 [DOI] [Google Scholar]
- Calado F., Griffiths M. D. (2016). Problem gambling worldwide: An update and systematic review of empirical research (2000–2015). Journal of Behavioral Addictions, 5(4), 592–613. doi: 10.1556/2006.5.2016.073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canale N., Verzeletti C., Cavallari G., Pastore M., Santinello M. (2013). Il gioco d’azzardo problematico: Il ruolo dei fattori cognitivi e affettivi in un campione di studenti universitari [Problematic gambling: The role of cognitive and affective factors among university students]. Psicoterapia Cognitiva E Comportamentale, 19(3), 289–308. [Google Scholar]
- Carl J. R., Soskin D. P., Kerns C., Barlow D. H. (2013). Positive emotion regulation in emotional disorders: A theoretical review. Clinical Psychology Review, 33(3), 343–360. doi: 10.1016/j.cpr.2013.01.003 [DOI] [PubMed] [Google Scholar]
- Carroll D., Huxley J. A. (1994). Young people and fruit machine gambling. In Legg C. R., Booth D. A. (Eds.), Appetite: Neural and behavioural bases (pp. 285–304). New York, NY: Oxford University Press. [Google Scholar]
- Caselli G., Fernie B. A., Canfora F., Mascolo C., Ferrari A., Antonioni M., Giustina L., Donato G., Marcotriggiani A., Bertani A., Altieri A., Pellegrini E., Spada M. M. (2018). The metacognitions about gambling questionnaire: Development and psychometric properties in community and clinical populations. Psychiatry Research, 261, 367–374. doi: 10.1016/j.psychres.2018.01.018 [DOI] [PubMed] [Google Scholar]
- Casey L. M., Oei T. S., Melville K. M., Bourke E., Newcombe P. A. (2008). Measuring self-efficacy in gambling: The Gambling Refusal Self-Efficacy Questionnaire. Journal of Gambling Studies, 24(2), 229–246. doi: 10.1007/s10899-007-9076-2 [DOI] [PubMed] [Google Scholar]
- Ciccarelli M., Nigro G., Griffiths M. D., Cosenza M., D’Olimpio F. (2016). Research paper: Attentional biases in problem and non-problem gamblers. Journal of Affective Disorders, 198, 135–141. doi: 10.1016/j.jad.2016.03.009 [DOI] [PubMed] [Google Scholar]
- Cooper M. L., Frone M. R., Russell M., Mudar P. (1995). Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology, 69(5), 990–1005. doi: 10.1037/0022-3514.69.5.990 [DOI] [PubMed] [Google Scholar]
- Cosenza M., Baldassarre I., Matarazzo O., Nigro G. (2014). Youth at stake: Alexithymia, cognitive distortions, and problem gambling in late adolescents. Cognitive Computation, 6(4), 652–660. doi: 10.1007/s12559-014-9274-z [DOI] [Google Scholar]
- Cyders M. A., Smith G. T. (2008a). Emotion-based dispositions to rash action: Positive and negative urgency. Psychological Bulletin, 134(6), 807–828. doi: 10.1037/a0013341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders M. A., Smith G. T. (2008b). Clarifying the role of personality dispositions in risk for increased gambling behavior. Personality and Individual Differences, 45(6), 503–508. doi: 10.1016/j.paid.2008.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders M. A., Smith G. T., Spillane N. S., Fischer S., Annus A. M., Peterson C. (2007). Integration of impulsivity and positive mood to predict risky behavior: Development and validation of a measure of positive urgency. Psychological Assessment, 19(1), 107–118. doi: 10.1037/1040-3590.19.1.107 [DOI] [PubMed] [Google Scholar]
- Damasio A. R. (1999). The feeling of what happens: Body and emotion in the making of consciousness. New York, NY: Harcourt Brace. [Google Scholar]
- Davidson R. J. (2003). Darwin and the neural bases of emotion and affective style. Annals of the New York Academy of Sciences, 1000(1), 316–336. doi: 10.1196/annals.1280.014 [DOI] [PubMed] [Google Scholar]
- Davtian M., Reid R. C., Fong T. W. (2012). Investigating facets of personality in adult pathological gamblers with ADHD. Neuropsychiatry, 2(2), 163–174. doi: 10.2217/npy.12.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Berardis D., Campanella D., Nicola S., Gianna S., Alessandro C., Chiara C., Valchera A., Marilde C., Salerno R. M., Ferro F. (2008). The impact of alexithymia on anxiety disorders: A review of the literature. Current Psychiatry Reviews, 4(2), 80–86. doi: 10.2174/157340008784529287 [DOI] [Google Scholar]
- Dunn B. D., Billotti D., Murphy V., Dalgleish T. (2009). The consequences of effortful emotion regulation when processing distressing material: A comparison of suppression and acceptance. Behaviour Research and Therapy, 47(9), 761–773. doi: 10.1016/j.brat.2009.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmas H. G., Cesur G., Oral E. T. (2017). Alexithymia and pathological gambling: The mediating role of difficulties in emotion regulation. Türk Psikiyatri Dergisi, 28(1), 1–7. doi: 10.5080/u13779 [DOI] [PubMed] [Google Scholar]
- Estévez G. A., Herrero F. D., Sarabia G. I., Jauregui B. P. (2014). El papel mediador de la regulacion emocional entre el juego patologico, uso abusivo de Internet y videojuegos y la sintomatologia disfuncional en jovenes y adolescentes [Mediating role of emotional regulation between impulsive behavior in gambling, Internet and videogame abuse, and dysfunctional symptomatology in young adults and adolescents]. Adicciones, 26(4), 282. doi: 10.20882/adicciones.26 [DOI] [PubMed] [Google Scholar]
- Fauth-Bühler M., Mann K., Potenza M. N. (2017). Pathological gambling: A review of the neurobiological evidence relevant for its classification as an addictive disorder. Addiction Biology, 22(4), 885–897. doi: 10.1111/adb.12378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fauth-Bühler M., Zois E., Vollstädt-Klein S., Lemenager T., Beutel M., Mann K. (2014). Insula and striatum activity in effort related monetary reward processing in gambling disorder: The role of depressive symptomatology. NeuroImage: Clinical, 6, 243–251. doi: 10.1016/j.nicl.2014.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortune E. E., Goodie A. S. (2012). Cognitive distortions as a component and treatment focus of pathological gambling: A review. Psychology of Addictive Behaviors, 26(2), 298–310. doi: 10.1037/a0026422 [DOI] [PubMed] [Google Scholar]
- Gaher R. M., Hahn A. M., Shishido H., Simons J. S., Gaster S. (2015). Associations between sensitivity to punishment, sensitivity to reward, and gambling. Addictive Behaviors, 42, 180–184. doi: 10.1016/j.addbeh.2014.11.014 [DOI] [PubMed] [Google Scholar]
- Garofalo C., Holden C. J., Zeigler-Hill V., Velotti P. (2016). Understanding the connection between self-esteem and aggression: The mediating role of emotion dysregulation. Aggressive Behavior, 42(1), 3–15. doi: 10.1002/ab.21601 [DOI] [PubMed] [Google Scholar]
- Garofalo C., Velotti P. (2015). Alcohol misuse in psychiatric patients and nonclinical individuals: The role of emotion dysregulation and impulsivity. Addiction Research & Theory, 23(4), 294–300. doi: 10.3109/16066359.2014.987758 [DOI] [Google Scholar]
- Garofalo C., Velotti P. (2017). Negative emotionality and aggression in violent offenders: The moderating role of emotion dysregulation. Journal of Criminal Justice, 51, 9–16. doi: 10.1016/j.jcrimjus.2017.05.015 [DOI] [Google Scholar]
- Garofalo C., Velotti P., Zavattini G. C. (2013). Lo studio della regolazione delle emozioni: Prospettive future [The study of the emotion regulation: Future directions]. Giornale Italiano Di Psicologia, 40(2), 247–262. doi: 10.1421/74555 [DOI] [Google Scholar]
- Goodie A. S. (2005). The role of perceived control and overconfidence in pathological gambling. Journal of Gambling Studies, 21(4), 481–502. doi: 10.1007/s10899-005-5559-1 [DOI] [PubMed] [Google Scholar]
- Gori A., Craparo G., Caretti V., Giannini M., Iraci-Sareri G., Bruschi A., Janiri L., Ponti L., Tani F. (2016). Impulsivity, alexithymia and dissociation among pathological gamblers in different therapeutic settings: A multisample comparison study. Psychiatry Research, 246, 789–795. doi: 10.1016/j.psychres.2016.10.046 [DOI] [PubMed] [Google Scholar]
- Gratz K. L., Roemer L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. doi: 10.1023/B:JOBA.0000007455.08539.94 [DOI] [Google Scholar]
- Gross J. J. (1998). The emerging field of emotion regulation: An integrative review. Review of General Psychology, 2(3), 271–299. doi: 10.1037/1089-2680.2.3.271 [DOI] [Google Scholar]
- Gross J. J., John O.P. (2003). Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Personality and Social Psychology, 85(2), 348–362. doi: 10.1037/0022-3514.85.2.348 [DOI] [PubMed] [Google Scholar]
- Haw J. (2017). Impulsivity predictors of problem gambling and impaired control. International Journal of Mental Health and Addiction, 15(1), 154–165. doi: 10.1007/s11469-015-9603-9 [DOI] [Google Scholar]
- Heilman R., Crişan L., Miclea M., Miu A., Houser D. (2010). Emotion regulation and decision making under risk and uncertainty. Emotion, 10(2), 257–265. doi: 10.1037/a0018489 [DOI] [PubMed] [Google Scholar]
- Hudson A., Jacques S., Stewart S. H. (2013). Selective attention to emotional pictures as a function of gambling motives in problem and nonproblem gamblers. Psychology of Addictive Behaviors, 27(4), 1079. doi: 10.1037/a0031863 [DOI] [PubMed] [Google Scholar]
- Jacobs D. F. (1986). A general theory of addictions: A new theoretical model. Journal of Gambling Behavior, 2(1), 15–31. doi: 10.1007/BF01019931 [DOI] [Google Scholar]
- Jauregui P., Estevez A., Urbiola I. (2016). Pathological gambling and associated drug and alcohol abuse, emotion regulation, and anxious-depressive symptomatology. Journal of Behavioral Addictions, 5(2), 251–260. doi: 10.1556/2006.5.2016.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jauregui P., Onaindia J., Estévez A. (2017). Adaptive and maladaptive coping strategies in adult pathological gamblers and their mediating role with anxious-depressive symptomatology. Journal of Gambling Studies, 33(4), 1081–1097. doi: 10.1007/s10899-017-9675-5 [DOI] [PubMed] [Google Scholar]
- Jauregui P., Urbiola I., Estevez A. (2016). Metacognition in pathological gambling and its relationship with anxious and depressive symptomatology. Journal of Gambling Studies, 32(2), 675–688. doi: 10.1007/s10899-015-9552-z [DOI] [PubMed] [Google Scholar]
- Kneeland E. T., Dovidio J. F., Joormann J., Clark M. S. (2016). Emotion malleability beliefs, emotion regulation, and psychopathology: Integrating affective and clinical science. Clinical Psychology Review, 45, 81–88. doi: 10.1016/j.cpr.2016.03.008 [DOI] [PubMed] [Google Scholar]
- Kornreich C., Saeremans M., Delwarte J., Noël X., Campanella S., Verbanck P., Ermer E., Brevers D. (2016). Impaired non-verbal emotion processing in pathological gamblers. Psychiatry Research, 236, 125–129. doi: 10.1016/j.psychres.2015.12.020 [DOI] [PubMed] [Google Scholar]
- Kräplin A., Dshemuchadse M., Behrendt S., Scherbaum S., Goschke T., Bühringer G. (2014). Dysfunctional decision-making in pathological gambling: Pattern specificity and the role of impulsivity. Psychiatry Research, 215(3), 675–682. doi: 10.1016/j.psychres.2013.12.041 [DOI] [PubMed] [Google Scholar]
- Lakey C. E., Campbell W. K., Brown K. W., Goodie A. S. (2007). Dispositional mindfulness as a predictor of the severity of gambling outcomes. Personality and Individual Differences, 43(7), 1698–1710. doi: 10.1016/j.paid.2007.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakey C. E., Rose P., Campbell W. K., Goodie A. S. (2008). Probing the link between narcissism and gambling: The mediating role of judgment and decision-making biases. Journal of Behavioral Decision Making, 21(2), 113–137. doi: 10.1002/bdm.582 [DOI] [Google Scholar]
- Lesieur H. R. (2001, October). Cluster analysis of types of inpatient pathological gamblers. Dissertation Abstracts International, 62, 2065. [Google Scholar]
- Li S., Zhang B., Guo Y., Zhang J. (2015). The association between alexithymia as assessed by the 20-item Toronto Alexithymia Scale and Depression: A meta-analysis. Psychiatry Research, 227(1), 1–9. doi: 10.1016/j.psychres.2015.02.006 [DOI] [PubMed] [Google Scholar]
- Lindberg A., Fernie B. A., Spada M. M. (2011). Metacognitions in problem gambling. Journal of Gambling Studies, 27(1), 73–81. doi: 10.1007/s10899-010-9193-1 [DOI] [PubMed] [Google Scholar]
- Lorains F. K., Cowlishaw S., Thomas S. A. (2011). Prevalence of comorbid disorders in problem and pathological gambling: Systematic review and meta-analysis of population surveys. Addiction, 106(3), 490–498. doi: 10.1111/j.1360-0443.2010.03300.x [DOI] [PubMed] [Google Scholar]
- Loxton N. J., Nguyen D., Casey L., Dawe S. (2008). Reward drive, rash impulsivity and punishment sensitivity in problem gamblers. Personality and Individual Differences, 45(2), 167–173. doi: 10.1016/j.paid.2008.03.017 [DOI] [Google Scholar]
- Luberto C. M., Cotton S., McLeish A. C., Mingione C. J., O’Bryan E. M. (2014). Mindfulness skills and emotion regulation: The mediating role of coping self-efficacy. Mindfulness, 5(4), 373–380. doi: 10.1007/s12671-012-0190-6 [DOI] [Google Scholar]
- Lumley M. A., Roby K. J. (1995). Alexithymia and pathological gambling. Psychotherapy and Psychosomatics, 63(3–4), 201–206. doi: 10.1159/000288960 [DOI] [PubMed] [Google Scholar]
- Lysaker P. H., George S., Chaudoin-Patzoldt K. A., Pec O., Bob P., Leonhardt B. L., Vohs J. L., James A. V., Wickett A., Buck K. D., Dimaggio G. (2017). Contrasting metacognitive, social cognitive and alexithymia profiles in adults with borderline personality disorder, schizophrenia and substance use disorder. Psychiatry Research, 257(2017), 393–399. doi: 10.1016/j.psychres.2017.08.001 [DOI] [PubMed] [Google Scholar]
- Mansueto G., Pennelli M., De Palo V., Monacis L., Sinatra M., De Caro M. (2016). The role of metacognition in pathological gambling: A mediation model. Journal of Gambling Studies, 32(1), 93–106. doi: 10.1007/s10899-014-9519-5 [DOI] [PubMed] [Google Scholar]
- MacLaren V., Harrigan K., Dixon M. (2012). Gambling motives and symptoms of problem gambling in frequent slots players. Journal of Gambling Issues, (27), 1–13. doi: 10.4309/jgi.2012.27.8 [DOI] [Google Scholar]
- McCormick R. A. (1988). Pathological gambling: A parsimonious need state model. Journal of Gambling Behavior, 3(4), 257–263. doi: 10.1007/BF01019885 [DOI] [Google Scholar]
- McCormick R. A. (1994). The importance of coping skill enhancement in the treatment of the pathological gambler. Journal of Gambling Studies, 10(1), 77–86. doi: 10.1007/BF02109780 [DOI] [PubMed] [Google Scholar]
- McCormick R. A., Taber J. I. (1988). Attributional style in pathological gamblers in treatment. Journal of Abnormal Psychology, 97(3), 368–370. doi: 10.1037/0021-843X.97.3.368 [DOI] [PubMed] [Google Scholar]
- McDougall J. (2004). L’economie psychique de l’addiction [The psychic economy of addiction]. Revue Française De Psychanalyse, 68(2), 511–527. doi: 10.3917/rfp.682.0511 [DOI] [Google Scholar]
- Milosevic A., Ledgerwood D. M. (2010). The subtyping of pathological gambling: A comprehensive review. Clinical Psychology Review, 30(8), 988–998. doi: 10.1016/j.cpr.2010.06.013 [DOI] [PubMed] [Google Scholar]
- Mitrovic D. V., Brown J. (2009). Poker mania and problem gambling: A study of distorted cognitions, motivation and alexithymia. Journal of Gambling Studies, 25(4), 489–502. doi: 10.1007/s10899-009-9140-1 [DOI] [PubMed] [Google Scholar]
- Molde H., Pallesen S., Sætrevik B., Hammerborg D. K., Laberg J. C., Johnsen B. (2010). Attentional biases among pathological gamblers. International Gambling Studies, 10(1), 45–59. doi: 10.1080/14459791003652501 [DOI] [Google Scholar]
- Morgan J. E., Bowen K. L., Moore S. C., van Goozen S. M. (2014). The relationship between reward and punishment sensitivity and antisocial behavior in male adolescents. Personality and Individual Differences, 63, 122–127. doi: 10.1016/j.paid.2014.01.054 [DOI] [Google Scholar]
- Navas J., Perales J., Verdejo-Román J., Perandrés-Gómez A., Contreras-Rodríguez O., Albein-Urios N., Verdejo-García A. (2017). Trait and neurobiological underpinnings of negative emotion regulation in gambling disorder. Addiction, 112(6), 1086–1094. doi: 10.1111/add.13751 [DOI] [PubMed] [Google Scholar]
- Navas J. F., Verdejo-García A., López-Gómez M., Maldonado A., Perales J. C. (2016). Gambling with rose-tinted glasses on: Use of emotion-regulation strategies correlates with dysfunctional cognitions in gambling disorder patients. Journal of Behavioral Addictions, 5(2), 271–281. doi: 10.1556/2006.5.2016.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman M. G., Llera S. J. (2011). A novel theory of experiential avoidance in generalized anxiety disorder: A review and synthesis of research supporting a contrast avoidance model of worry. Clinical Psychology Review, 31(3), 371–382. doi: 10.1016/j.cpr.2011.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nusslock R. R., Almeida J. R., Forbes E. E., Versace A., Frank E., LaBarbara E. J., Klein C. R., Phillips M. L. (2012). Waiting to win: Elevated striatal and orbitofrontal cortical activity during reward anticipation in euthymic bipolar disorder adults. Bipolar Disorders, 14(3), 249–260. doi: 10.1111/j.1399-5618.2012.01012.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen V. V., Lugo R. G., Sutterlin S. (2015). The somatic marker theory in the context of addiction: Contributions to understanding development and maintenance. Psychology Research and Behavior Management, 8, 187. doi: 10.2147/PRBM.S68695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace U., Zappulla C., Di Maggio R., Passanisi A., Craparo G. (2015). Characteristics of regular gamblers in Italy: The role of control and emotion regulation. Clinical Neuropsychiatry, 12(5), 111–117. [Google Scholar]
- Parker J. A., Wood L. M., Bond B. J., Shaughnessy P. (2005). Alexithymia in young adulthood: A risk factor for pathological gambling. Psychotherapy and Psychosomatics, 74(1), 51–55. doi: 10.1159/000082027 [DOI] [PubMed] [Google Scholar]
- Passanisi A., Pace U. (2017). The unique and common contributions of impulsivity and decision-making strategies among young adult Italian regular gamblers. Personality and Individual Differences, 105, 24–29. doi: 10.1016/j.paid.2016.09.029 [DOI] [Google Scholar]
- Petry N. M. (2005). Pathological gambling: Etiology, comorbidity, and treatment. Washington, DC: American Psychological Association. [Google Scholar]
- Poole J. C., Kim H. S., Dobson K. S., Hodgins D. C. (2017). Adverse childhood experiences and disordered gambling: Assessing the mediating role of emotion dysregulation. Journal of Gambling Studies, 33(4), 1187–1200. doi: 10.1007/s10899-017-9680-8 [DOI] [PubMed] [Google Scholar]
- Reid R. C., Di Tirro C., Fong T. W. (2014). Mindfulness in patients with gambling disorders. Journal of Social Work Practice in the Addictions, 14(4), 327–337. doi: 10.1080/1533256X.2014.958493 [DOI] [Google Scholar]
- Richman M. J., Unoka Z. (2015). Mental state decoding impairment in major depression and borderline personality disorder: Meta-analysis. The British Journal of Psychiatry, 207(6), 483–489. doi: 10.1192/bjp.bp.114.152108 [DOI] [PubMed] [Google Scholar]
- Riley B. (2012). Experiential avoidance mediates the association between thought suppression and mindfulness with problem gambling. Journal of Gambling Studies, 30(1), 163–171. doi: 10.1007/s10899-012-9342-9 [DOI] [PubMed] [Google Scholar]
- Riva P., Sacchi S., Brambilla M. (2015). Humanizing machines: Anthropomorphization of slot machines increases gambling. Journal of Experimental Psychology: Applied, 21(4), 313–325. doi: 10.1037/xap0000057 [DOI] [PubMed] [Google Scholar]
- Rogier G., Garofalo C., Velotti P. (2017). Is emotional suppression always bad? A matter of flexibility and gender differences. Current Psychology. doi: 10.1007/s12144-017-9623-7 [DOI] [Google Scholar]
- Rogier G., Velotti P. (2018). Narcissistic implications in gambling disorder: The mediating role of emotion dysregulation. Journal of Gambling Studies. doi: 10.1007/s10899-018-9759-x [DOI] [PubMed] [Google Scholar]
- Rogier G., Velotti P., Zavattini G. C. (2017). Gioco d’azzardo ed antisocialità: Riflessioni su un’emergenza sociale [Gambling and antisocial behavior: Considerations about a social urgency]. Giornale Italiano di Psicologia, 44(2), 219–248. doi: 10.1421/87328 [DOI] [Google Scholar]
- Rosenberg M. P., Feder P. C. (2014). Behavioral addictions: Criteria, evidence, and treatment. Burlington, NJ: Academic Press. [Google Scholar]
- Saddichha S., Schuetz C. (2014). Is impulsivity in remitted bipolar disorder a stable trait? A meta-analytic review. Comprehensive Psychiatry, 55(7), 1479–1484. doi: 10.1016/j.comppsych.2014.05.010 [DOI] [PubMed] [Google Scholar]
- Scannell E. D., Quirk M. M., Smith K., Maddern R., Dickerson M. (2000). Females’ coping styles and control over poker machine gambling. Journal of Gambling Studies, 16(4), 417–432. doi: 10.1023/A:1009484207439 [DOI] [PubMed] [Google Scholar]
- Schreiber L. N., Grant J. E., Odlaug B. L. (2012). Emotion regulation and impulsivity in young adults. Journal of Psychiatric Research, 46(5), 651–658. doi: 10.1016/j.jpsychires.2012.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharpe L. (2002). A reformulated cognitive-behavioral model of problem gambling. Clinical Psychology Review, 22(1), 1–25. doi: 10.1016/S0272-7358(00)00087-8 [DOI] [PubMed] [Google Scholar]
- Shead N. W., Hodgins D. C. (2009). Affect-regulation expectancies among gamblers. Journal of Gambling Studies, 25(3), 357–375. doi: 10.1007/s10899-009-9131-2 [DOI] [PubMed] [Google Scholar]
- Sheppes G., Suri G., Gross J. J. (2015). Emotion regulation and psychopathology. Annual Review of Clinical Psychology, 11, 379–405. doi: 10.1146/annurev-clinpsy-032814-112739 [DOI] [PubMed] [Google Scholar]
- Sloan E., Hall K., Moulding R., Bryce S., Mildred H., Staiger P. (2017). Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: A systematic review. Clinical Psychology Review, 57, 141–163. doi: 10.1016/j.cpr.2017.09.002 [DOI] [PubMed] [Google Scholar]
- Sokol-Hessner P., Hsu M., Curley N. G., Delgado M. R., Camerer C. F., Phelps E. A. (2009). Thinking like a trader selectively reduces individuals’ loss aversion. Proceedings of the National Academy of Sciences of the United States of America, 106(13), 5035–5040. doi: 10.1073/pnas.0806761106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spada M. M., Caselli G., Nikčević A. V., Wells A. (2015). Metacognition in addictive behaviors. Addictive Behaviors, 44, 9–15. doi: 10.1016/j.addbeh.2014.08.002 [DOI] [PubMed] [Google Scholar]
- Spada M. M., Giustina L., Rolandi S., Fernie B. A., Caselli G. (2015). Profiling metacognition in gambling disorder. Behavioural and Cognitive Psychotherapy, 43(5), 614–622. doi: 10.1017/S1352465814000101 [DOI] [PubMed] [Google Scholar]
- Spada M., Roarty A. (2015). The relative contribution of metacognitions and attentional control to the severity of gambling in problem gamblers. Addictive Behaviors Reports, 1(C), 7–11. doi: 10.1016/j.abrep.2015.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steward T., Mestre-Bach G., Fernández-Aranda F., Granero R., Perales J. C., Navas J. F., Soriano-Mas C., Bano M., Fernandez-Formoso J. A., Martin-Romera V., Mechon J. M., Jiménez-Murcia S. (2017). Delay discounting and impulsivity traits in young and older gambling disorder patients. Addictive Behaviors, 71, 96–103. doi: 10.1016/j.addbeh.2017.03.001 [DOI] [PubMed] [Google Scholar]
- Stewart S. H., Zack M., Collins P., Klein R. M. (2008). Subtyping pathological gamblers on the basis of affective motivations for gambling: Relations to gambling problems, drinking problems, and affective motivations for drinking. Psychology of Addictive Behaviors, 22(2), 257–268. doi: 10.1037/0893-164X.22.2.257 [DOI] [PubMed] [Google Scholar]
- Suomi A., Dowling N. A., Jackson A. C. (2014). Problem gambling subtypes based on psychological distress, alcohol abuse and impulsivity. Addictive Behaviors, 39(12), 1741–1745. doi: 10.1016/j.addbeh.2014.07.023 [DOI] [PubMed] [Google Scholar]
- Takamatsu S. K., Martens M. P., Arterberry B. J. (2016). Depressive symptoms and gambling behavior: Mediating role of coping motivation and gambling refusal self-efficacy. Journal of Gambling Studies, 32(2), 535–546. doi: 10.1007/s10899-015-9562-x [DOI] [PubMed] [Google Scholar]
- Thompson R. A. (1990). Emotion and self-regulation. In Thompson R. A. (Ed.), Nebraska symposium on motivation, 1988: Socioemotional development. Current theory and research in motivation (Vol. 36, pp. 367–467). Lincoln, NE: University of Nebraska Press. [PubMed] [Google Scholar]
- Tomei A., Besson J., Grivel J. (2017). Linking empathy to visuospatial perspective-taking in gambling addiction. Psychiatry Research, 250, 177–184. doi: 10.1016/j.psychres.2016.12.061 [DOI] [PubMed] [Google Scholar]
- Toneatto T., Lecce J., Bagby M. (2009). Alexithymia and pathological gambling. Journal of Addictive Diseases, 28(3), 193–198. doi: 10.1080/10550880903014775 [DOI] [PubMed] [Google Scholar]
- Vaddiparti K., Cottler L. B. (2017). Personality disorders and pathological gambling. Current Opinion in Psychiatry, 30(1), 45. doi: 10.1097/YCO.0000000000000300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Holst R. J., van den Brink W., Veltman D. J., Goudriaan A. E. (2010). Why gamblers fail to win: A review of cognitive and neuroimaging findings in pathological gambling. Neuroscience and Biobehavioral Reviews, 34(1), 87–107. doi: 10.1016/j.neubiorev.2009.07.007 [DOI] [PubMed] [Google Scholar]
- Velotti P., Garofalo C. (2015). Personality styles in a non-clinical sample: The role of emotion dysregulation and impulsivity. Personality and Individual Differences, 79, 44–49. doi: 10.1016/j.paid.2015.01.046 [DOI] [Google Scholar]
- Velotti P., Garofalo C., Bottazzi F., Caretti V. (2017). Faces of shame: Implications for self-esteem, emotion regulation, aggression, and well-being. The Journal of Psychology, 151(2), 171–184. doi: 10.1080/00223980.2016.1248809 [DOI] [PubMed] [Google Scholar]
- Velotti P., Garofalo C., D’Aguanno M., Popolo R., Salvatore G., Dimaggio G. (2016). Mindfulness moderates the relationship between aggression and antisocial personality disorder traits: Preliminary investigation with an offender sample. Comprehensive Psychiatry, 64, 38–45. doi: 10.1016/j.comppsych.2015.08.004 [DOI] [PubMed] [Google Scholar]
- Velotti P., Garofalo C., Zavattini G. C. (2013). The study of the emotion regulation: Future directions. Giornale Italiano di Psicologia, 2, 247–262. doi: 10.1421/74555 [DOI] [Google Scholar]
- Velotti P., Rogier G., Lysaker P. (2018). Psychiatric illness interview for gambling addiction: Analysis of metacognition abilities. Manuscript in preparation. [Google Scholar]
- Weatherly J. N., Cookman M. L. (2014). Investigating several factors potentially related to endorsing gambling as an escape. Current Psychology: A Journal for Diverse Perspectives on Diverse Psychological Issues, 33(3), 422–433. doi: 10.1007/s12144-014-9220-y [DOI] [Google Scholar]
- Weatherly J. N., Miller K. B. (2013). Exploring the factors related to endorsing gambling as an escape. International Gambling Studies, 13(1), 52–64. doi: 10.1080/14459795.2012.703214 [DOI] [Google Scholar]
- Webb T. L., Miles E., Sheeran P. (2012). Dealing with feeling: A meta-analysis of the effectiveness of strategies derived from the process model of emotion regulation. Psychological Bulletin, 138(4), 775–808. doi: 10.1037/a0027600 [DOI] [PubMed] [Google Scholar]
- Williams A. D., Grisham J. R., Erskine A., Cassedy E. (2012). Deficits in emotion regulation associated with pathological gambling. British Journal of Clinical Psychology, 51(2), 223–238. doi: 10.1111/j.2044-8260.2011.02022.x [DOI] [PubMed] [Google Scholar]
- Willner-Reid J., Smith N., Jones H. B., MacLeod A. K. (2012). Affective forecasting in problem gamblers. International Gambling Studies, 12(3), 295–307. doi: 10.1080/14459795.2012.671841 [DOI] [Google Scholar]