Abstract
Objectives
The aims of this cross-sectional study were to assess the prevalence of Internet addiction (IA) in a clinical sample of adolescents with attention-deficit hyperactivity disorder (ADHD) and to detect the moderating effects of co-occurring oppositional defiant disorder/conduct disorder (ODD/CD) on the association between ADHD and IA.
Methods
The study group comprised 119 adolescent subjects who were consecutively referred to our outpatient clinic with a diagnosis of ADHD. The Turgay DSM-IV-Based Child and Adolescent Disruptive Behavioral Disorders Screening and Rating Scale (T-DSM-IV-S) was completed by parents, and subjects were asked to complete the Internet Addiction Scale (IAS).
Results
The IAS results indicated that 63.9% of the participants (n = 76) fell into the IA group. Degree of IA was correlated with hyperactivity/impulsivity symptoms but not with inattention symptoms. As compared to the ADHD-only group (without comorbid ODD/CD), ADHD + ODD/CD subjects returned significantly higher scores on the IAS.
Conclusions
As adolescents with ADHD are at high risk of developing IA, early IA detection and intervention is of great importance for this group. In addition, adolescents with ADHD + ODD/CD may be more vulnerable to IA than those in the ADHD-only group and may need to be more carefully assessed for IA.
Keywords: Internet addiction, adolescents, ADHD, oppositional defiant disorder, conduct disorder
Introduction
In recent decades, the Internet has become an essential part of our daily lives. Despite various advantages, such as unlimited access to information exchange and social communication, some negative impacts of Internet use have also been identified (Wang et al., 2011; Zboralski et al., 2009). Excessive or problematic Internet use or Internet addiction (IA) is among the terms most commonly used when referring to maladaptive patterns of Internet use leading to clinically significant impairment or distress (An et al., 2014; Xu et al., 2012). IA is characterized by symptoms that include spending excessive time or longer than initially intended online, along with compulsive behaviors, unsuccessful attempts at cessation or control, lying about the extent of one’s use of the Internet, use to cope or escape problems, and preoccupation with the Internet when one is offline (Brezing, Derevensky, & Potenza, 2010). The estimated worldwide prevalence of adolescent IA ranges between 1.6% and 36.7% (Ko, Yen, Yen, Chen, & Chen, 2012). This wide discrepancy in prevalence rates may be explained by methodological differences and by variations in Internet access across different countries (Ho et al., 2014; Yu & Shek, 2013).
IA has been linked to various psychiatric conditions, including depression and suicidal ideation (Chang, Chiu, Lee, Chen, & Miao, 2014; Cho, Sung, Shin, Lim, & Shin, 2013; Jang, Hwang, & Choi, 2008; Kim et al., 2006; Ko, Yen, Chen, Yeh, & Yen, 2009; Lin et al., 2014; Park, Hong, Park, Ha, & Yoo, 2013; Tsitsika et al., 2011), anxiety (Cho et al., 2013), social phobia (Ko et al., 2009), obsessive–compulsive symptoms, hostility, aggression, problematic alcohol use, substance use (Ko et al., 2012), self-injurious behavior (Lam, Peng, Mai, & Jing, 2009), and, in particular, attention-deficit hyperactivity disorder (ADHD; Ko et al., 2012; Yen, Chou, Liu, Yang, & Hu, 2014; Yılmaz, Hergüner, Bilgiç, & Işık, 2015; Yoo et al., 2004). According to Bozkurt, Coskun, Ayaydin, Adak, and Zoroglu (2013), ADHD is the most prevalent (83.3%) axis-1 disorder among the adolescents referred for IA. In addition, in a two-year longitudinal study of Taiwanese adolescents, ADHD (along with hostility) was found to be the most significant predictor of IA (Ko et al., 2009).
It is well established that oppositional defiant disorder (ODD) and conduct disorder (CD) are the most prevalent comorbid psychiatric disorders among children and adolescents with ADHD (Pliszka, 2007). There is evidence that presence of comorbid ODD/CD is associated with increased risk of substance-use disorders in adolescents with ADHD (Lee, Humphreys, Flory, Liu, & Glass, 2011; Molina & Pelham, 2003). As in the case of substance-use disorders, observed rates of ODD and CD were greater in adolescents referred for IA than in the general population (American Psychiatric Association [APA], 2013; Bozkurt et al., 2013). To the best of our knowledge, however, no study has examined the effects of co-occurring disruptive behavior disorders on IA severity in adolescents with ADHD.
As mentioned above, a growing body of evidence indicates a strong link between ADHD and IA. However, as the majority of these studies have been conducted in Asia, there is a need for studies in other countries to investigate whether cultural differences influence Internet use among young people with ADHD (Weiss, Baer, Allan, Saran, & Schibuk, 2011) and whether co-occurring ODD/CD increases the risk of IA in adolescents with ADHD. The aims of this cross-sectional study were to evaluate the prevalence of IA in a clinical sample of adolescents with ADHD and to detect the moderating effects of co-occurring ODD/CD on the association between ADHD and IA.
Methods
Participants
Participants were recruited from a clinical sample of adolescents aged 12–17 years who were consecutively referred to our outpatient clinic in Istanbul, Turkey between March 2013 and September 2014 and diagnosed with ADHD. Those who were drug-free for at least 6 months or who never used any medication for ADHD were invited to participate in the study after obtaining their legal guardians’ approval. All those who were invited (138 adolescents, aged 12–17 years) agreed to participate. Of those, 19 were omitted because of incomplete data. Those receiving any ADHD medication or psychotherapeutic treatment for ADHD and those with comorbid substance use disorder or any psychotic disorder, bipolar disorder, mental retardation, or pervasive developmental disorder were not included in the study.
Diagnosis
ADHD, ODD, and CD diagnoses were based on the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; APA, 2000) criteria and comprehensive information from a clinical examination, which included interviews with both youth and parent and review of psychiatric, psychometric, and educational records. All of the interviews were conducted by child and adolescent psychiatrists with at least 9 years experience of disruptive behavioral disorders.
Data collection tools
The study data were collected using a sociodemographic information form, the Turgay DSM-IV-Based Child and Adolescent Disruptive Behavioral Disorders Screening and Rating Scale (T-DSM-IV-S), and the Internet Addiction Scale (IAS).
Sociodemographic information form
This form was prepared by the authors to collect data on the adolescent’s gender, current age, and smoking status, and on the parents’ age and educational level.
T-DSM-IV-S
This scale was developed by Turgay (1994) and was adapted for Turkish use by Ercan, Amado, Somer, and Cikoglu (2001). The T-DSM-IV-S is based on DSM-IV (APA, 2000) diagnostic criteria; 9 items assess inattention, 9 assess hyperactivity/impulsivity (HA/IM), 8 assess opposition/defiance, and 15 assess conduct disorder. Symptoms are scored by assigning a severity estimate for each on a 4-point Likert-type scale (0 = not at all, 1 = just a little, 2 = quite a bit, and 3 = very much). The scale was completed by parents in this study.
IAS
The scale consists of 35 items, with four subfactors defined as “withdrawal,” “controlling difficulty,” “disorder in functionality,” and “social isolation.” The IAS was developed in Turkish by Günüç and Kayri (2010); a pool of items was developed to determine factors responsible for addiction, and a trial scale was developed from this pool based on expert opinion during the development phase. The validity of the scale was tested by a pilot trial. A validity and reliability study was subsequently conducted with 754 high-school students from seven provinces, and the scale’s validity and reliability was found to be high (Cronbach’s α coefficient of internal consistency = .94). Attitudes were assessed on a 5-point Likert scale (5 = fully agree, 4 = agree, 3 = neutral, 2 = do not agree, and 1 = definitely do not agree). Minimum and maximum possible scores are 35 and 175, respectively.
In a study conducted in Turkey, Üneri and Tanıdır (2011) used the IAS to assess the prevalence of IA among the high-school students. Based on the results, they divided their sample into four groups. Subjects who scored over 81 were assigned to the addictive group; those who scored between 67 and 81 were assigned to the addiction risk group; those who scored between 53 and 66 were assigned to the threshold group; and those who scored less than 53 were assigned to the non-addictive group. In this study, as our sample consisted of adolescents from a similar age group, the cut-off point determined by Üneri and Tanıdır (2011) was used to identify IA.
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences, version 16.0 (SPSS Inc., Chicago, IL). The sample was described in terms of frequencies and percentages for discrete variables and means and standard errors for continuous variables. Student’s t-test was used to compare mean values between groups, and χ2 and Fisher’s exact test were used to compare rates between groups. Pearson’s method was used for correlation analyses. One-way analysis of variance was used to compare IAS scores between ADHD subgroups. A p value of <.05 was considered to be statistically significant.
Ethics
The study was approved by the Medical Ethics Committee of the Bakirkoy Research and Training Hospital for Psychiatric and Neurological Disorders. Both adolescents and parents signed informed consent forms prior to participation in the study.
Results
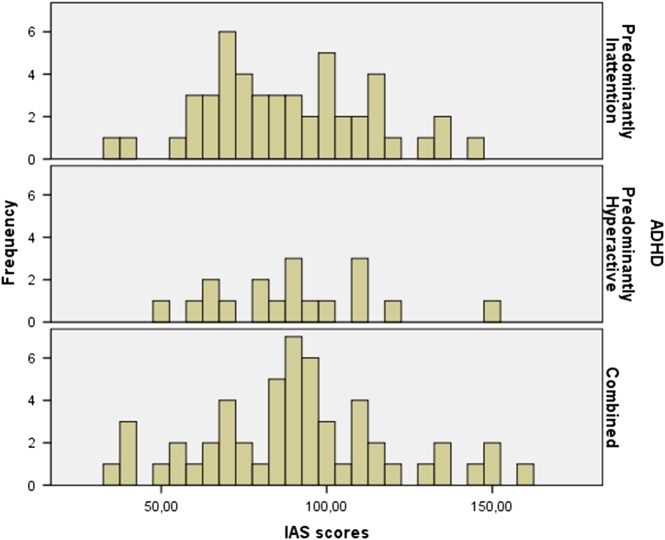
The mean IAS score was 89.8 ± 26.7 (range: 35–159), and 63.9% of the participants were found to have IA (Figure 1 shows distributions of IAS scores in each ADHD subtype group.). Table 1 summarizes the participants’ demographic features, ADHD subtypes, T-DSM-IV-S scores, frequency of IA, presence of comorbid ODD and/or CD, severity of IA symptoms, Internet usage habits, and smoking status.
Figure 1.
Distribution of Internet Addiction Scale (IAS) scores
Table 1.
Demographic features, T-DSM-IV-S scores, IAS scores, Internet-using habits and smoking status of the participants
| N (%) | Mean ± SD | |
|---|---|---|
| Age | 119 | 14.8 ± 1.3 |
| Sex | ||
| Female | 30 (25.2) | |
| Male | 89 (74.8) | |
| ADHD subtypes | ||
| Predominantly inattention | 48 (40.3) | |
| Predominantly hyperactive | 18 (15.1) | |
| Combined | 53 (44.5) | |
| Comorbid ODD/CD | ||
| Yes | 41 (34.5) | |
| No | 78 (65.5) | |
| Comorbid ODD | ||
| Yes | 76 (63.9) | |
| No | 43 (36.1) | |
| Comorbid CD | ||
| Yes | 27 (22.7) | |
| No | 92 (77.3) | |
| T-DSM-IV-S | ||
| Inattention | 16.97 ± 5.27 | |
| Hyperactivity/impulsivity | 13.47 ± 6.33 | |
| ODD | 12.93 ± 5.91 | |
| CD | 5.42 ± 5.49 | |
| Total | 48.89 ± 17.26 | |
| IAS | 89.8 ± 26.7 | |
| Internet addiction | ||
| Yes | 76 (63.9) | |
| No | 43 (36) | |
| Personal computer | ||
| Yes | 76 (63.9) | |
| No | 43 (36.1) | |
| Internet connection at home | ||
| Yes | 99 (83.2) | |
| No | 20 (16.8) | |
| Time spent on Internet | ||
| 0–4 | 71 (59.7) | |
| 4–8 | 31 (26.1) | |
| ≥8 | 17 (14.3) | |
| Smoking status | ||
| Smoker | 23 (19.3) | |
| Non-smoker | 95 (79.8) | |
Note. SD: standard deviation; ADHD: attention-deficit hyperactivity disorder; ODD: oppositional defiant disorder; CD: conduct disorder; T-DSM-IV-S: Turgay DSM-IV-Based Child and Adolescent Disruptive Behavioral Disorders Screening and Rating Scale; IAS: Internet Addiction Scale.
No statistically significant difference was found between the IAS scores of females and males (p = .391). There was no statistically significant correlation between having a personal computer and having a home Internet connection, smoking status, ADHD subtypes, and IAS scores (p = .463, .411, .422, and .837, respectively). There was a statistically significant correlation between time spent online and presence of comorbid ODD and/or CD with IAS scores (p = .001 and .001, respectively) (Table 2). There was a statistically significant correlation between ODD/CD comorbidity and presence of IA. The odds ratios of IA in ADHD + ODD or ADHD + CD groups were 3.22 and 4.23 (95% confidence interval), respectively (Table 3).
Table 2.
The associations between demographic features, Internet-using habits, smoking status, and ADHD subtypes and presence of comorbid ODD/CD and IAS scores
| IAS scores | p | Effect size | |
|---|---|---|---|
| Sex | |||
| Female | 93.4 ± 25.2 | .391 | 0.18 |
| Male | 88.6 ± 27.2 | ||
| Personal computer | |||
| Yes | 91.2 ± 27.8 | .463 | 0.14 |
| No | 87.4 ± 24.9 | ||
| Internet connection at home | |||
| Yes | 88.9 ± 26.9 | .411 | 0.20 |
| No | 94.3 ± 26 | ||
| Time spent on Internet | |||
| 0–4 | 80 ± 23.6 | ||
| 4–8 | 98.5 ± 22.8 | .001 | 0.23 |
| ≥8 | 114.5 ± 25.3 | ||
| Smoking | |||
| Yes | 93.6 ± 23.8 | .422 | 0.19 |
| No | 88.6 ± 27.4 | ||
| ADHD subtypes | |||
| Predominantly inattention | 88.1 ± 25 | 0.01 | |
| Predominantly hyperactive | 89.9 ± 23.9 | .837 | |
| Combined | 91.3 ± 29.4 | ||
| Comorbid ODD/CD | |||
| Yes | 95.6 ± 27 | .001 | 0.68 |
| No | 78.7 ± 22.4 | ||
| Comorbid ODD | |||
| Yes | 95.6 ± 27.3 | .001 | 0.65 |
| No | 79.4 ± 22.2 | ||
| Comorbid CD | |||
| Yes | 106 ± 29.8 | .001 | 0.87 |
| No | 85 ± 23.8 | ||
Note. Bold values represents p < .05. ADHD: attention-deficit hyperactivity disorder; ODD: oppositional defiant disorder; CD: conduct disorder; IAS: Internet Addiction Scale.
Table 3.
The associations between ODD/CD comorbidity and presence of Internet addiction
| Internet addiction | |||
|---|---|---|---|
| p | OR | 95% CI | |
| ADHD + ODD | .005 | 3.22 | 1.46–7.07 |
| ADHD + CD | .010 | 4.23 | 1.35–13.22 |
Note. ADHD: attention-deficit hyperactivity disorder; ODD: oppositional defiant disorder; CD: conduct disorder; OR:odds ratio; 95% CI: 95% confidence interval.
There was no significant correlation between age, T-DSM-IV-S inattention scores, and IAS scores (r = −.90, p = .33 and r = .146, p = .112, respectively). There were statistically significant correlations between T-DSM-IV-S HA/IM, T-DSM-IV-S opposition defiance, T-DSM-IV-S conduct disorder, and T-DSM-IV-S total scores and IAS scores (r = .185, p = .043; r = .331, p = .001; r = .387, p = .001; and r = .349, p = .001, respectively) (Table 4).
Table 4.
The association between IAS scores, age, and T-DSM-IV-S scores
| IAS scores | ||
|---|---|---|
| r | p | |
| Age | −.90 | .33 |
| T-DSM-IV-S | ||
| Inattention | .146 | .112 |
| HA/IM | .185 | .043 |
| ODD | .331 | .001 |
| CD | .387 | .001 |
| Total | .349 | .001 |
Note. Bold values represents p < .05. IAS: Internet Addiction Scale; T-DSM-IV-S: Turgay DSM-IV-Based Child and Adolescent Disruptive Behavioral Disorders Screening and Rating Scale; HA/IM: hyperactivity/impulsivity; ODD: oppositional defiant disorder; CD: conduct disorder.
Discussion
In this study, 63.9% of those adolescents with ADHD (n = 76) were found to have IA, which is higher than the previously reported prevalence rates of IA among Turkish high-school students (10.1%–24.2%) (Günüç & Kayri, 2010; Üneri & Tanıdır, 2011; Yılmaz et al., 2015). Our results align with previous findings indicating an increased risk of IA in adolescents with ADHD. However, we found prevalence rates substantially higher than those reported in two earlier studies (15.7% and 32.7%) (Yen et al., 2014; Yoo et al., 2004) of children and adolescents with ADHD. Unlike previous research, this study recruited all participants from adolescents who were not receiving any type of treatment for ADHD. It was suggested in one previous report (Han et al., 2009) that an 8-week course of methylphenidate treatment could reduce the severity of Internet video gameplay among children with ADHD. In the previous samples, medical and/or psychotherapeutic treatment may have resulted in reduction of IA symptoms and frequency. In addition, our outpatient clinic mainly serves patients from lower socioeconomic backgrounds, and it has been suggested that poorer social support is linked with greater risk of IA. For that reason, participants’ socioeconomic status may account for the increase in IA in our sample (Tsai et al., 2009). As the above studies were performed in Asian countries, cultural differences may also have contributed to the discrepancy in prevalence rates.
ADHD and IA may be linked through various biological and/or psychological mechanisms. In particular, several cognitive and behavioral problems observed in individuals with ADHD have been shown to be associated with impairments in the reward processing system. Children with ADHD appear to have a strong preference for immediate rather than delayed reward, even when the delayed reward is larger. This can be explained by an aversion to waiting and a decreased sensitivity to cues that predict reward (Luman et al., 2009; Umemoto, Lukie, Kerns, Müller, & Holroyd, 2014). Yoo et al. (2004) suggested that individuals who are less satisfied with natural rewards tend to resort to substance abuse as a way of seeking enhanced stimulation of the reward pathway; in the same way, IA may serve as another “unnatural” (immediate) reward. There is also emerging evidence that Internet-use disorder is associated with structural or functional impairment of the orbitofrontal cortex, dorsolateral prefrontal cortex, anterior cingulate cortex, and posterior cingulate cortex – regions that are known to be associated with the processing of reward, motivation, memory, and cognitive controls (Park, Han, & Roh, 2017; Zhu, Zhang, & Tian, 2015). In the daily lives of children with ADHD, IA may also serve as a compensatory activity for poor social skills, interpersonal difficulties, low self-esteem, and lack of pleasure (Yen et al., 2014; Yoo et al., 2004).
In this study, symptoms of HA/IM (but not of inattention) were found to be correlated with degree of IA. As impulsivity and loss of control over Internet use are among the most prominent psychological features of individuals with IA (Young, 2004), it is unsurprising that HA/IM domains are associated with IA. In earlier studies, Cao, Su, Liu, and Gao (2007), Cao and Su (2007), and Wu et al. (2013) have reported an association between hyperactivity and impulsivity and IA among Chinese adolescents. However, the literature reports inconsistent results regarding the effects of ADHD symptom domains on degree of IA; some studies report a stronger relation to inattention, whereas others emphasize HA/IM (Bozkurt et al., 2013; Chou, Liu, Yang, Yen, & Hu, 2015; Yen et al., 2014; Yılmaz et al., 2015; Yoo et al., 2004). Similar inconsistencies arose in studies of the association between substance-use disorders and ADHD (Molina & Pelham, 2003; Lee & Hinshaw, 2006). In a meta-analytic review of prospective association of ADHD and substance-use disorders, Lee et al. (2011) hypothesized that inattention and hyperactivity may be differentially related to substance-use disorders, and the same hypothesis seems applicable to IA.
The studies have shown that 54%–84% of children and adolescents with ADHD have co-morbid ODD, and a sizeable proportion of these patients were expected to develop CD (Pliszka, 2007). Consistent with the existing data, 65.5% of the cases in our sample had comorbid ODD/CD with ADHD. As in the case of substance-use disorders (Lee et al., 2011), our findings indicate that comorbid ODD or CD increases the risk of IA in adolescents with ADHD. Dysfunctions of the prefrontal cortex are also thought to play an important role in the pathogenesis of ODD/CD (Fahim et al., 2011). Children and adolescents with conduct disorder exhibit a tendency toward risk taking and reckless behavior, indicating difficulties with decision-making and impulsivity. They are also more vulnerable to substance abuse, potentially reflecting an altered sensitivity of reward mechanisms and persistent selection of options with short-term benefits, despite negative long-term consequences (Fairchild et al., 2009). It has also been argued that ADHD + ODD substantially differs from ADHD-only in terms of neurocognitive functioning (Luman et al., 2009), and ODD/CD comorbidity is hypothesized to account for most of the associations between delay aversion and ADHD (Antrop et al., 2006). Moreover, aggression (one of the key symptoms in ODD/CD) and IA have been shown to be closely related, and IA is often accompanied by aggression. There is evidence that IA and aggression share a number of common neural substrates and neuromodulators; key neural substrates of aggression, such as the prefrontal cortex and the limbic system, are located in brain regions that also relate to IA (Hahn & Kim, 2014). Altogether with the aforementioned alterations in the brain’s reward system in IA, it seems possible that ODD/CD comorbidity may increase the risk of IA among adolescents with ADHD. In addition, poor family functioning, problems in school bonding, low academic achievement, and deviant peer relationships are among the main risk factors for substance use in adolescents with ADHD + ODD/CD (Lopez et al., 2008), and the same risk factors may also be linked to behavioral addictions in these individuals.
The prevalence of smoking in patients with ADHD ranges from 15% to 19% (Pliszka, 2007), and in line with these findings, 19.3% of our participants reported that they smoked cigarettes. Previous studies have shown that cigarette smoking increases the risk of substance use among both typically developing children and those with ADHD (Groenman et al., 2013). For that reason, Groenman et al. (2013) suggested that nicotine use could be considered a gateway to other drugs. Similarly, in a longitudinal study, Chang et al. (2014) suggested that smoking was a predictor of IA in adolescents. However, in their study of high-school students, Üneri and Tanıdır (2011) found no significant association between IA and smoking behavior, and in this study, we found no significant correlation between smoking status and IA in adolescents with ADHD.
Several limitations of this study must be acknowledged. First, as the cross-sectional design prevents us from clearly defining the direction of the casual relationship between ADHD, ODD/CD, and IA, prospective longitudinal studies are needed to clarify the temporal relationship. Second, any generalization of the results is limited by the lack of a control group comprising non-clinically referred adolescents or adolescents referred for other mental health problems. Third, IA was diagnosed on the basis of a self-report questionnaire, which may compromise the validity of diagnosis. However, as it seems more plausible that adolescents would minimize their problems with Internet use, the higher observed rate of IA in our sample seems to exclude this issue. Finally, our results were not controlled for other predictive variables such as comorbid depression and/or anxiety disorder or familial risk factors that may also have affected the prevalence and severity of IA in adolescents with ADHD.
Conclusions
IA can result in serious dysfunction in an individual’s academic and work performance, as well as in their family life, social relationships, physical health, and psychological well-being (Shek & Yu, 2012). IA may also worsen outcomes in the adolescents with ADHD who already have marked impairments in terms of scholastic adjustment and peer and familial relations (APA, 2013). In line with existing evidence (Weiss et al., 2011), the present findings confirm the significance of early detection and intervention of IA in the adolescents with ADHD. These findings also suggest that adolescents with ADHD + ODD/CD may be more vulnerable to IA than those with ADHD only and may need to be more carefully assessed in this regard. Further prospective studies are needed to more fully understand the associations between IA, ADHD, and ODD/CD. Finally, pre- and posttreatment studies evaluating IA symptoms in adolescents with ADHD only or with ADHD+ODD/CD may help to determine whether ADHD treatment reduces the risk of IA in both groups.
Funding Statement
Funding sources: No financial support was received for this study.
Authors’ contribution
HG, CT, HA, and OSU contributed to study concept and design. HG, CT, HA, AGK, CM, MKB, and MT contributed to data collection. CT and NB contributed to statistical analysis. HG, CT, AGK, CM, NB, and OSU contributed to analysis and interpretation of data. HG, CT, and MKB contributed to manuscript writing process. OSU contributed to study supervision. All authors had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of interest
The authors declare no conflict of interest.
References
- American Psychiatric Association [APA]. (2000). Diagnostic and statistical manual of mental disorders (DSM-IV) (4th ed., text rev.). Washington, DC: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association [APA]. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Association. [Google Scholar]
- An J., Sun Y., Wan Y., Chen J., Wang X., Tao F. (2014). Associations between problematic Internet use and adolescents’ physical and psychological symptoms. Journal of Addiction Medicine, 8(4), 282–287. doi: 10.1097/ADM.0000000000000026 [DOI] [PubMed] [Google Scholar]
- Antrop I., Stock P., Verté S., Wiersema J. R., Baeyens D., Roeyers H. (2006). ADHD and delay aversion: The influence of non-temporal stimulation on choice for delayed rewards. Journal of Child Psychology and Psychiatry and Allied Disciplines, 47(11), 1152–1158. doi: 10.1111/j.1469-7610.2006.01619.x [DOI] [PubMed] [Google Scholar]
- Bozkurt H., Coskun M., Ayaydin H., Adak İ., Zoroglu S. S. (2013). Prevalence and patterns of psychiatric disorders in referred adolescents with Internet addiction. Psychiatry and Clinical Neurosciences, 67(5), 352–359. doi: 10.1111/pcn.12065 [DOI] [PubMed] [Google Scholar]
- Brezing C., Derevensky J. L., Potenza M. N. (2010). Non-substance-addictive behaviors in youth: Pathological gambling and problematic Internet use. Child and Adolescent Psychiatric Clinics of North America, 19(3), 625–641. doi: 10.1016/j.chc.2010.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao F., Su L. (2007). Internet addiction among Chinese adolescents: Prevalence and psychological features. Child: Care, Health and Development, 33(3), 275–281. doi: 10.1111/j.1365-2214.2006.00715.x [DOI] [PubMed] [Google Scholar]
- Cao F., Su L., Liu T., Gao X. (2007). The relationship between impulsivity and Internet addiction in a sample of Chinese adolescents. European Psychiatry, 22(7), 466–471. doi: 10.1016/j.eurpsy.2007.05.004 [DOI] [PubMed] [Google Scholar]
- Chang F.-C., Chiu C.-H., Lee C.-M., Chen P.-H., Miao N.-F. (2014). Predictors of the initiation and persistence of Internet addiction among adolescents in Taiwan. Addictive Behaviors, 39(10), 1434–1440. doi: 10.1016/j.addbeh.2014.05.010 [DOI] [PubMed] [Google Scholar]
- Cho S.-M., Sung M.-J., Shin K.-M., Lim K. Y., Shin Y.-M. (2013). Does psychopathology in childhood predict Internet addiction in male adolescents? Child Psychiatry & Human Development, 44(4), 549–555. doi: 10.1007/s10578-012-0348-4 [DOI] [PubMed] [Google Scholar]
- Chou W.-J., Liu T.-L., Yang P., Yen C.-F., Hu H.-F. (2015). Multi-dimensional correlates of Internet addiction symptoms in adolescents with attention-deficit/hyperactivity disorder. Psychiatry Research, 225(1–2), 122–128. doi: 10.1016/j.psychres.2014.11.003 [DOI] [PubMed] [Google Scholar]
- Ercan E. S., Amado S., Somer O., Cikoglu S. (2001). Dikkat eksikliği hiperaktivite bozukluğu ve yıkıcı davranış bozuklukları için bir test bataryası geliştirme calışması [Development of a test battery for attention deficit hyperactivity and disruptive behavior disorders]. Turkish Journal of Child and Adolescent Mental Health, 8(3), 132–144. doi: 10.5455/apd.186583 [DOI] [Google Scholar]
- Fahim C., He Y., Yoon U., Chen J., Evans A., Pérusse D. (2011). Neuroanatomy of childhood disruptive behavior disorders. Aggressive Behavior, 37(4), 326–337. doi: 10.1002/ab.20396 [DOI] [PubMed] [Google Scholar]
- Fairchild G., van Goozen S. H. M., Stollery S. J., Aitken M. R. F., Savage J., Moore S. C., Goodyer I. M. (2009). Decision making and executive function in male adolescents with early-onset or adolescence-onset conduct disorder and control subjects. Biological Psychiatry, 66(2), 162–168. doi: 10.1016/j.biopsych.2009.02.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groenman A. P., Oosterlaan J., Rommelse N., Franke B., Roeyers H., Oades R. D., Sergeant J. A., Buitelaar J. K., Faraone S. V. (2013). Substance use disorders in adolescents with attention deficit hyperactivity disorder: A 4-year follow-up study. Addiction, 108(8), 1503–1511. doi: 10.1111/add.12188 [DOI] [PubMed] [Google Scholar]
- Günüç S., Kayri M. (2010). TÜRKİYE’Deİnternet BağimliliProfili Veİnternet BağimliliÖlçeğinGeliştirilmesi: GeçerliGüvenirlik Çalişmasi [The profile Of Internet dependency in Turkey and development Of Internet Addiction Scale: Study Of validity and reliability]. Hacettepe Üniversitesi Eğitim Fakültesi Dergisi (H.U. Journal of Education), 39(2009), 220–232. [Google Scholar]
- Hahn C., Kim D.-J. (2014). Is there a shared neurobiology between aggression and Internet addiction disorder? Journal of Behavioral Addictions, 3(1), 12–20. doi: 10.1556/JBA.3.2014.1.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han D. H., Lee Y. S., Na C., Ahn J. Y., Chung U. S., Daniels M. A., Haws C. A., Renshaw P. F. (2009). The effect of methylphenidate on Internet video game play in children with attention-deficit/hyperactivity disorder. Comprehensive Psychiatry, 50(3), 251–256. doi: 10.1016/j.comppsych.2008.08.011 [DOI] [PubMed] [Google Scholar]
- Ho R. C., Zhang M. W., Tsang T. Y., Toh A. H., Pan F., Lu Y., Cheng C., Yip P. S., Lam L. T., Lai C. M., Watanabe H., Mak K. K. (2014). The association between Internet addiction and psychiatric co-morbidity: A meta-analysis. BMC Psychiatry, 14(1), 183. doi: 10.1186/1471-244X-14-183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang K. S., Hwang S. Y., Choi J. Y. (2008). Internet addiction and psychiatric symptoms among Korean adolescents. Journal of School Health, 78(3), 165–171. doi: 10.1111/j.1746-1561.2007.00279.x [DOI] [PubMed] [Google Scholar]
- Kim K., Ryu E., Chon M.-Y., Yeun E.-J., Choi S.-Y., Seo J.-S., Nam B.-W. (2006). Internet addiction in Korean adolescents and its relation to depression and suicidal ideation: A questionnaire survey. International Journal of Nursing Studies, 43(2), 185–192. doi: 10.1016/j.ijnurstu.2005.02.005 [DOI] [PubMed] [Google Scholar]
- Ko C.-H., Yen J.-Y., Chen C.-S., Yeh Y.-C., Yen C.-F. (2009). Predictive values of psychiatric symptoms for Internet addiction in adolescents. Archives of Pediatrics & Adolescent Medicine, 163(10), 937. doi: 10.1001/archpediatrics.2009.159 [DOI] [PubMed] [Google Scholar]
- Ko C.-H., Yen J.-Y., Yen C.-F., Chen C.-S., Chen C.-C. (2012). The association between Internet addiction and psychiatric disorder: A review of the literature. European Psychiatry, 27(1), 1–8. doi: 10.1016/j.eurpsy.2010.04.011 [DOI] [PubMed] [Google Scholar]
- Lam L. T., Peng Z., Mai J., Jing J. (2009). The association between Internet addiction and self-injurious behaviour among adolescents. Injury Prevention, 15(6), 403–408. doi: 10.1136/ip.2009.021949 [DOI] [PubMed] [Google Scholar]
- Lee S. S., Hinshaw S. P. (2006). Predictors of adolescent functioning in girls with attention deficit hyperactivity disorder (ADHD): The role of childhood ADHD, conduct problems, and peer status. Journal of Clinical Child and Adolescent Psychology, 35(3), 356–368. doi: 10.1207/s15374424jccp3503_2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S. S., Humphreys K. L., Flory K., Liu R., Glass K. (2011). Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: A meta-analytic review. Clinical Psychology Review, 31(3), 328–341. doi: 10.1016/j.cpr.2011.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin I.-H., Ko C.-H., Chang Y.-P., Liu T.-L., Wang P.-W., Lin H.-C., Huang M.-F., Yeh Y. C., Chou W. J., Yen C. F. (2014). The association between suicidality and Internet addiction and activities in Taiwanese adolescents. Comprehensive Psychiatry, 55(3), 504–510. doi: 10.1016/j.comppsych.2013.11.012 [DOI] [PubMed] [Google Scholar]
- Lopez B., Schwartz S. J., Prado G., Huang S., Rothe E. M., Wang W., Pantin H. (2008). Correlates of early alcohol and drug use in Hispanic adolescents: Examining the role of ADHD with comorbid conduct disorder, family, school, and peers. Journal of Clinical Child & Adolescent Psychology, 37(4), 820–832. doi: 10.1080/15374410802359676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luman M., Van Noesel S. J. P., Papanikolau A., Van Oostenbruggen-Scheffer J., Veugelers D., Sergeant J. A., Oosterlaan J. (2009). Inhibition, reinforcement sensitivity and temporal information processing in ADHD and ADHD+ODD: Evidence of a separate entity? Journal of Abnormal Child Psychology, 37(8), 1123–1135. doi: 10.1007/s10802-009-9334-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina B. S. G., Pelham W. E. (2003). Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. Journal of Abnormal Psychology, 112(3), 497–507. doi: 10.1037/0021-843X.112.3.497 [DOI] [PubMed] [Google Scholar]
- Park B., Han D. H., Roh S. (2017). Neurobiological findings related to Internet use disorders. Psychiatry and Clinical Neurosciences, 71(7), 467–478. doi: 10.1111/pcn.12422 [DOI] [PubMed] [Google Scholar]
- Park S., Hong K.-E. M., Park E. J., Ha K. S., Yoo H. J. (2013). The association between problematic Internet use and depression, suicidal ideation and bipolar disorder symptoms in Korean adolescents. Australian & New Zealand Journal of Psychiatry, 47(2), 153–159. doi: 10.1177/0004867412463613 [DOI] [PubMed] [Google Scholar]
- Pliszka S. (2007). Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 46(7), 894–921. doi: 10.1097/chi.0b013e318054e724 [DOI] [PubMed] [Google Scholar]
- Shek D. T. L., Yu L. (2012). Internet addiction phenomenon in early adolescents in Hong Kong. The Scientific World Journal, 2012, 1–9. Retrieved from http://www.hindawi.com/journals/tswj/2012/104304/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai H. F., Cheng S. H., Yeh T. L., Shih C. C., Chen K. C., Yang Y. C., Yang Y. K. (2009). The risk factors of Internet addiction – A survey of university freshmen. Psychiatry Research, 167(3), 294–299. doi: 10.1016/j.psychres.2008.01.015 [DOI] [PubMed] [Google Scholar]
- Tsitsika A., Critselis E., Louizou A., Janikian M., Freskou A., Marangou E., Kormas G., Kafetzis D. (2011). Determinants of Internet addiction among adolescents: A case-control study. The Scientific World Journal, 11, 866–874. doi: 10.1100/tsw.2011.85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turgay A. (1994). Disruptive Behavior DisordersChild and Adolescent Screening and Rating Scales for Children, Adolescents, Parents and Teachers. West Blomfield, MI: Integrative Therapy Institute Publication. [Google Scholar]
- Umemoto A., Lukie C. N., Kerns K. A., Müller U., Holroyd C. B. (2014). Impaired reward processing by anterior cingulate cortex in children with attention deficit hyperactivity disorder. Cognitive, Affective, & Behavioral Neuroscience, 14(2), 698–714. doi: 10.3758/s13415-014-0298-3 [DOI] [PubMed] [Google Scholar]
- Üneri Ö. Ş., Tanıdır C. (2011). Bir grup lise öğrencisinde internet bağımlılığı değerlendirmesi: Kesitsel bir çalışma [Evaluation of Internet addiction in a group of high school students: A cross-sectional study]. Dusunen Adam: The Journal of Psychiatry and Neurological Sciences, 24(4), 265–272. doi: 10.5350/DAJPN2011240402 [DOI] [Google Scholar]
- Wang H., Zhou X., Lu C., Wu J., Deng X., Hong L. (2011). Problematic Internet use in high school students in Guangdong Province, China. PLoS One, 6(5), e19660. doi: 10.1371/journal.pone.0019660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss M. D., Baer S., Allan B. A., Saran K., Schibuk H. (2011). The screens culture: Impact on ADHD. Attention Deficit and Hyperactivity Disorders, 3(4), 327–334. doi: 10.1007/s12402-011-0065-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X., Chen X., Han J., Meng H., Luo J., Nydegger L., Wu H. (2013). Prevalence and factors of addictive Internet use among adolescents in Wuhan, China: Interactions of parental relationship with age and hyperactivity-impulsivity. PLoS One, 8(4), e61782. doi: 10.1371/journal.pone.0061782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J., Shen L., Yan C., Hu H., Yang F., Wang L., Kotha S. R., Zhang L. N., Liao X. P., Zhang J., Ouyang F. X., Zhang J. S., Shen X. M. (2012). Personal characteristics related to the risk of adolescent Internet addiction: A survey in Shanghai, China. BMC Public Health, 12(1), 1106. doi: 10.1186/1471-2458-12-1106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen C.-F., Chou W.-J., Liu T.-L., Yang P., Hu H.-F. (2014). The association of Internet addiction symptoms with anxiety, depression and self-esteem among adolescents with attention-deficit/hyperactivity disorder. Comprehensive Psychiatry, 55(7), 1601–1608. doi: 10.1016/j.comppsych.2014.05.025 [DOI] [PubMed] [Google Scholar]
- Yılmaz S., Hergüner S., Bilgiç A., Işık Ü. (2015). Internet addiction is related to attention deficit but not hyperactivity in a sample of high school students. International Journal of Psychiatry in Clinical Practice, 19(1), 18–23. doi: 10.3109/13651501.2014.979834 [DOI] [PubMed] [Google Scholar]
- Yoo H. J., Cho S. C., Ha J., Yune S. K., Kim S. J., Hwang J., Chung A., Sung Y. H., Lyoo I. K. (2004). Attention deficit hyperactivity symptoms and Internet addiction. Psychiatry and Clinical Neurosciences, 58(5), 487–494. doi: 10.1111/j.1440-1819.2004.01290.x [DOI] [PubMed] [Google Scholar]
- Young K. S. (2004). Internet addiction: A new clinical phenomenon and its consequences. American Behavioral Scientist, 48(4), 402–415. doi: 10.1177/0002764204270278 [DOI] [Google Scholar]
- Yu L., Shek D. T. L. (2013). Internet addiction in Hong Kong adolescents: A three-year longitudinal study. Journal of Pediatric and Adolescent Gynecology, 26(3), S10–S17. doi: 10.1016/j.jpag.2013.03.010 [DOI] [PubMed] [Google Scholar]
- Zboralski K., Orzechowska A., Talarowska M., Darmosz A., Janiak A., Janiak M., Florkowski A., Gałecki P. (2009). The prevalence of computer and Internet addiction among pupils. Postpy higieny i medycyny doświadczalnej (Online), 63, 8–12. Retrieved from http://www.phmd.pl/fulltxt.php?ICID=878550 [PubMed] [Google Scholar]
- Zhu Y., Zhang H., Tian M. (2015). Molecular and functional imaging of Internet addiction. BioMed Research International, 2015, 1–8. doi: 10.1155/2015/965386 [DOI] [PMC free article] [PubMed] [Google Scholar]