Abstract
Introduction:
We aim to present a modified technique and outcomes of a novel method allowing for direct visualization of the reservoir placement during a penoscrotal inflatable penile prosthesis (IPP).
Methods:
Out of165 patients who underwent IPP placement from August 2012 to March 2015, 157 underwent a modified technique and comprised the cohort of this study. A Deaver's retractor was placed lateral to the penis and over the pubic bone to allow for direct visualization of the tissues overlying the lower abdomen. After dissecting through the superficial layers, the Deaver's was slowly advanced, allowing for visualization of the fascia, which was incised. Using blunt dissection, a space for the reservoir was created between the bladder and the pubic bone. The reservoir was then placed safely into this space and the Deaver's retractor was removed.
Results:
The causes of ED in the study cohort included postprostatectomy ED (n = 107), organic impotence (n = 40), Peyronie's disease (n = 3), ED following cystoprostatectomy (n = 2), ED due to spinal cord injury (n = 2), ED resulting from priapism (n = 2), and ED after pelvic injury (n = 1); all of which were refractory to medical management. The median age of study population was 66 years and the mean (standard deviation) operative time was 72.8 (14.7) min. Eighty percent of the procedures were performed on outpatient basis. Complication rates were low (<5%), with four infections, one proximal pump migration, one scrotal hematoma, and one urinary tract infection.
Conclusion:
The modified technique for placement of the IPP's spherical reservoir under direct visualization through a penoscrotal incision is quick, safe, and effective.
INTRODUCTION
Erectile dysfunction (ED) impacts a significant proportion of men annually in the United States. Common etiologies of ED include medical comorbidities and pelvic surgeries. Less common reasons for developing ED include spinal cord injuries, postpriapism ED, or Peyronie's disease. Initial management generally consists of phosphodiesterase-5 inhibitors. When they fail, other treatments including vacuum erection devices, intraurethral alprostadil, and intracorporeal injections are offered. Implantable penile prostheses are offered in the treatment of ED when medical management fails.
Inflatable penile prostheses (IPPs) have been used since initially being described in the 1970s. Infrapubic, perineal, and penoscrotal techniques for the insertion of IPP have been described, with the first report of a single-incision penoscrotal approach being published in 2003.[1] Placement of the reservoir of the IPP can either be performed blindly or often requires a counter-incision to ensure appropriate placement and to minimize the risk of complications. Classically, the groups placing the reservoir through a single penoscrotal incision have placed it blindly, after puncturing through the transversalis fascia and developing a space for the reservoir either sharply or bluntly in the space of Retzius.[2,3] Blind placement can be associated with bowel or bladder injuries, damage to the iliac vessels, reservoir herniation, and post-operative inguinal hernia.[2,3] Due to this, some advocate for ectopic placement of the reservoir, particularly in the setting of prior pelvic surgeries. Placement of the reservoir under direct vision through a penoscrotal incision has not been previously described. In an attempt to optimize the surgical efficiency and minimize the complications, we present a modified technique and outcomes of a novel method allowing for direct visualization of the reservoir placement during a penoscrotal IPP.
METHODS
After obtaining institutional review board approval of this retrospective study, all patients who underwent placement of an IPP performed by a single surgeon (MJM) between August 2012 and March 2015 were identified for inclusion in the study. Their charts were retrospectively reviewed to extract information including age, etiology of erectile function, surgical history, surgical technique, location of reservoir placement, length of hospital stay, and postoperative complications. A total of 165 patients were identified. Of these, 157 underwent a modified technique for direct visualization of the reservoir placement during the study period and comprised the primary cohort of this study. All IPP placements were American Medical Systems 700 devices (Minneapolis, MN, USA). The patients were selected to undergo IPP placement after failing medical management of ED and requesting placement of the prosthetic device.
Intraoperative considerations and surgical technique
Instruments
The instruments used were a standard minor surgery set for an IPP with a Lone Star retractor.
Position and incision
The patients were placed in the supine position and were administered general anaesthesia in all the cases. A standard transverse 3-cm penoscrotal incision was made in all the cases.
Corporotomies
Subcutaneous tissue was divided, and the ventral surface of the urethra and corporal bodies was exposed. 3-0 PDS stay sutures were placed in each corporal body, and corporotomies were made. The corporal bodies were dilated proximally and then distally. Crossover was examined and the corpora were measured with a Furlow introducer.
Reservoir placement
While the device was being prepped, a Deaver's retractor was placed over the right side of the penoscrotal incision and was used to retract the incision superior to the pubic bone [Figure 1]. Under direct visualization, a small incision was made in the transversalis fascia and the dissection was performed until the space of Retzius was entered [Figure 2]. The spherical reservoir was then deployed into the space of Retzius and was filled to 65 mL [Figure 3].
Figure 1.
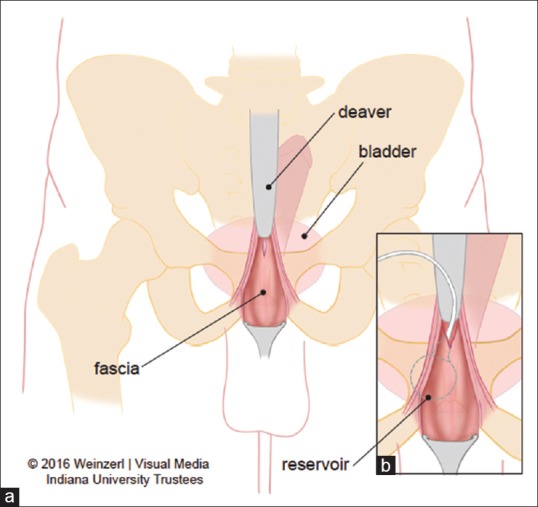
Schematic of reservoir placement under direct visualization (a) Location of deaver compared with fascia and site of incision of the fascia. (b) Placement of the resevoir under direct visualization through the fascia with the deaver in place.
Figure 2.
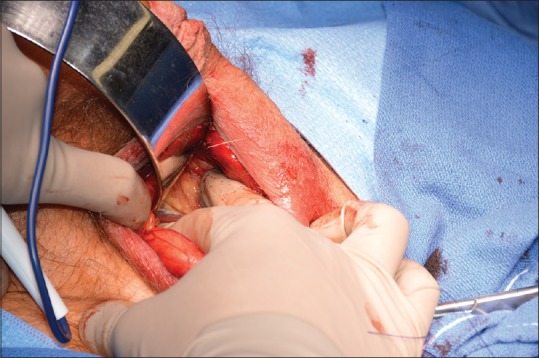
Direct visualization of incision using Deaver's retractor placed over the right side of the penoscrotal incision retracting the incision superior to the pubic bone
Figure 3.
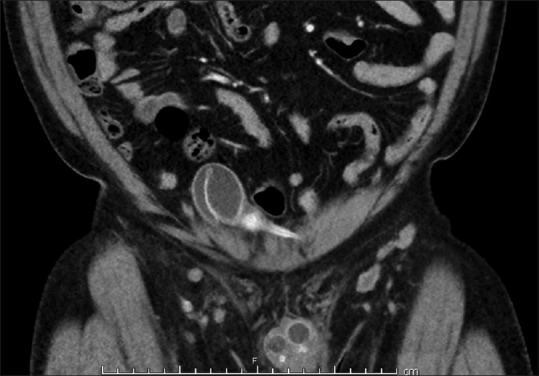
Coronal image of the reservoir placement via direct visualization
Case conclusion
The implant cylinders were deployed into each corporal body, and the stay sutures were used to close the corporotomies. After test inflation, connections to the reservoir were made. The scrotal pocket was then developed and the pump was placed. After copious irrigation, the incision was closed in multiple layers, the implant was inflated to 75% rigidity, and a mummy wrap was applied.
Postoperative management and follow-up
A Foley's catheter was kept in place overnight and was removed either while the patient was hospitalized or at home after appropriate teaching. The patients were discharged to home on 14 days of trimethoprim-sulfamethoxazole and a clinic follow-up was scheduled after 3 weeks.
Outcomes and complications
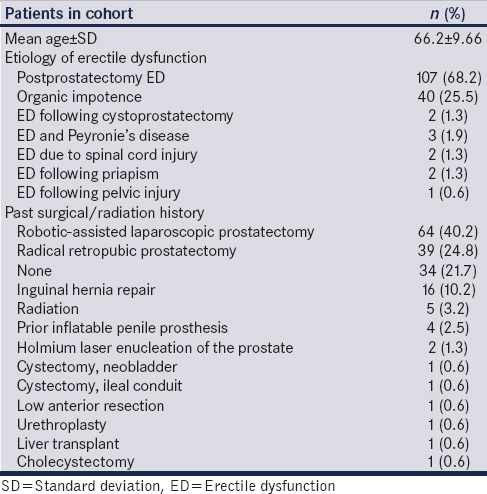
During the study period, 165 patients underwent IPP placement. 157 (95.2%) patients had their reservoirs placed in the space of Retzius via the described approach. Table 1 shows the demographic and the preoperative characteristics of the patients. The mean age was 66.2 (standard deviation [SD] 9.66, range 30–83) years.
Table 1.
Patient demographics and preoperative characteristics (n=157)
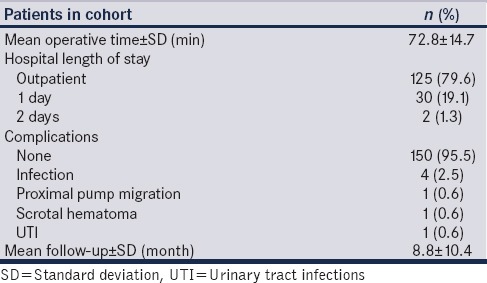
IPP reservoir placement via the direct vision approach was performed with a mean operative time of 72.8 min (SD 14.7, range 54–108 min). The vast majority of procedures (79.6%) were performed on an outpatient basis and the complication rates were low (4.5%), with only 2.5% of the patients developing an infection postoperatively [Table 2]. Full details of perioperative details and outcomes are displayed in Table 2. The mean follow-up period was 8.8 months (SD 10.4).
Table 2.
Intraoperative and postoperative characteristics (n=157)
Eight patients (4.8%) underwent ectopic placement of the IPP reservoir during the study period. Two patients had prior radical retropubic prostatectomy (RRP) and inguinal hernia repair, three patients had previous cystectomy with neobladder creation, one had prior robotic prostatectomy, one had a Monti catheterizable channel, and one did not have previous surgeries. In each of these cases, the direct visualization approach was attempted but could not be performed due to scar tissue, and therefore, ectopic placement of the reservoir was considered a safer alternative.
DISCUSSION
IPP and under vision placement of the reservoir into the space of Retzius is possible through a single penoscrotal incision with acceptable peri-operative outcomes. This technique compares favourably with the available literature in terms of complication rates. In patients undergoing an IPP, a postoperative infection rate of 1%–3% has been previously reported.[2,4,5] Our post operative infection rate (2.5%) compares favourably. Also, the blind placement of the reservoir into the space of Retzius may be complicated by postoperative inguinal hernia,.[2,3,5] This novel method allows for direct visualisation of the pump placement and hence avoids hernia formation. In the current study, at a mean follow-up of 8.8months, no patient developed a hernia, although one patient had proximal pump migration. Another uncommon but devastating injury during blind placement of reservoir is a vascular injury.[3] By virtue of direct visualization, this catastrophic complication can be avoided.
There was some concern that this approach may be challenging in patients with prior significant mobilization of the space of Retzius, such as in the cases of RRPs. However, we could perform the modified approach in the majority of the cases, and post RRP ED comprised the second largest group of patients in this study. By placing the reservoir through the same penoscrotal incision as the IPP and under direct vision, we were able to safely and efficiently complete the procedure in most of the patients, despite the majority of them having had a prior pelvic surgery. Although, this study is limited by relatively small number of patients; this is one of the first descriptions of direct visualization of the reservoir placement through a single penoscrotal incision and was associated with comparable peri-operative outcomes.
CONCLUSION
Placement of an IPP through a single penoscrotal incision with direct visualization of the reservoir placement into the space of Retzius is feasible and protects against catastrophic complications caused by blind placement. It is quick, safe, and effective and is a beneficial technique to be incorporated into prosthetic urologists’ armamentarium.
Footnotes
Financial support and sponsorship: Nil.
Conflicts of interest: There are no conflicts of interest.
REFERENCES
- 1.Wilson S, Delk J, 2nd, Henry GD, Siegel AL. New surgical technique for sphincter urinary control system using upper transverse scrotal incision. J Urol. 2003;169:261–4. doi: 10.1016/S0022-5347(05)64082-7. [DOI] [PubMed] [Google Scholar]
- 2.Capoccia EM, Phelps JN, Levine LA. Modified inflatable penile prosthesis reservoir placement into space of Retzius: Comparing outcomes in men with or without prior pelvic surgery. J Sex Med. 2017;14:968–73. doi: 10.1016/j.jsxm.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 3.Levine LA, Hoeh MP. Review of penile prosthetic reservoir: Complications and presentation of a modified reservoir placement technique. J Sex Med. 2012;9:2759–69. doi: 10.1111/j.1743-6109.2012.02807.x. [DOI] [PubMed] [Google Scholar]
- 4.Gupta NK, Ring J, Trost L, Wilson SK, Köhler TS. The penoscrotal surgical approach for inflatable penile prosthesis placement. Transl Androl Urol. 2017;6:628–38. doi: 10.21037/tau.2017.07.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilson SK, Delk JR., 2nd Inflatable penile implant infection: Predisposing factors and treatment suggestions. J Urol. 1995;153:659–61. [PubMed] [Google Scholar]


