Abstract
Atypical femoral fractures (AFF) are stress or ‘insufficiency’ fractures, often complicated by the use of bisphosphonates or other bone turnover inhibitors. While these drugs are beneficial for the intact osteoporotic bone, they probably prevent a stress fracture from healing which thus progresses to a complete fracture.
Key features of atypical femoral fractures, essential for the diagnosis, are: location in the subtrochanteric region and diaphysis; lack of trauma history and comminution; and a transverse or short oblique configuration.
The relative risk of patients developing an atypical femoral fracture when taking bisphosphonates is high; however, the absolute risk of these fractures in patients on bisphosphonates is low, ranging from 3.2 to 50 cases per 100,000 person-years.
Treatment strategy in patients with AFF involves: radiograph of the contralateral side (computed tomography and magnetic resonance imaging should also be considered); dietary calcium and vitamin D supplementation should be prescribed following assessment; bisphosphonates or other potent antiresorptive agents should be discontinued; prophylactic surgical treatment of incomplete AFF with cephalomedullary nail, unless pain free; cephalomedullary nailing for surgical fixation of complete fractures; avoidance of gaps in the lateral and anterior cortex; avoidance of varus malreduction.
Cite this article: EFORT Open Rev 2018;3:494-500. DOI: 10.1302/2058-5241.3.170070.
Keywords: atypical femoral fractures, bisphosphonate, complications, osteoporosis, treatment
Introduction
The introduction of bisphosphonates into osteoporosis therapy was a great breakthrough, leading to a remarkable reduction of fracture incidence and improvement of prognosis.1 Since the effect is caused by a reduction of bone turnover, long-term use is associated with an altered bone structure and biomechanics.2 As a direct consequence, the occurrence of atypical femoral fractures has been described and linked to a negative side-effect of antiresorptive therapy.3 Considering the large population benefitting from this pharmacotherapy, the incidence of this fracture entity is rather low.4 However, the difficult diagnosis caused by initially mild symptoms and slight radiological changes combined with a problematic therapy drives the need for guidelines to be established. The treatment challenges the alertness of the orthopaedic surgeon not only regarding the kind of osteosynthesis but also the patient’s medication, which should aim for avoidance of bone remodelling over-suppression.5 Although the first encouraging steps have been made towards an evidence-based therapy,6 the results must be interpreted with caution, considering the rareness of such an event. The purpose of this review is to give an overview on definition, pathogenesis, epidemiology, diagnosis, and state-of-the-art treatment of atypical femoral fractures, mainly following the long-term use of bisphosphonates.
Definition based on major and minor features
The diagnosis follows major and minor criteria, which were originally described by the Task Force of the American Society for Bone and Mineral Research (ASBMR) in 2010 and updated in 2014.7 The features of atypical femur fractures are: location mainly in the subtrochanteric region and diaphysis; the lack of trauma history and comminution; and a transverse or short oblique configuration (Table 1). Furthermore, the definition discriminates complete fractures with typical medial spikes from incomplete fractures involving only the lateral cortex, correlating with the site of the highest biomechanical stress. Minor features include radiological signs such as periosteal reaction and an increased cortical thickness, prodromal symptoms, bilateral occurrence, and delayed healing. Moreover, patients can have typical co-morbidities such as vitamin D deficiency, and be taking typical drugs such as bisphosphonates.
Table 1.
Major features: all major features are required to satisfy the case definition of atypical femur fracture
| Major features: |
|---|
| Located anywhere along the femur from just distal to the lesser trochanter to just proximal to the supracondylar flare |
| Associated with no trauma or minimal trauma, as in a fall from a standing height or less |
| Transverse or short oblique configuration |
| Noncomminuted |
| Complete fractures extend through both cortices and may be associated with a medial spike; incomplete fractures involve only the lateral cortex |
Pathogenesis
Principally, the pathogenesis and development of atypical femur fractures follows the concept of a stress or insufficiency fracture.7 Features such as a general transverse orientation, the lack of comminution, and the localized cortical thickening at the fracture site support this. The pathogenesis also correlates with typical clinical signs such as bilaterality, and prodromal pain. Furthermore, similar fracture types have been described in other bone diseases with decreased bone turnover such as hypophosphatasia13 and osteopetrosis.14
Bisphosphonates
Bisphosphonates are widely used to prevent osteoporotic fragility fractures. The clinical effect, which is documented with level I evidence,1 is based on the inhibition of osteoclasts. There are most likely several mechanisms contributing to the efficacy of these drugs, such as direct cytotoxicity,15 inhibition of osteoclast attachment,16 inhibition of osteoclast maturation,17 and direct intracellular impacts.18 The summary of these effects inhibits the bone turnover, which is beneficial, because degradation outweighs new bone formation with increasing age. One side-effect of the decreased osteoclast function is an impaired natural repair capacity. Therefore, the long-term use of bisphosphonates causes exponential accumulation of bone microdamage over time.19 Furthermore, the suppression of bone turnover alters bone mineral and matrix properties by increasing mineralization. This is actually visible as an increased thickness of the cortex. The resulting augmented strength and stiffness of the bone makes the skeletal structures at the same time more brittle20 and, therefore, more susceptible to fragility fractures. The suppressed bone turnover also increases the mean tissue age, leading to higher concentrations of advanced glycation end-products within the extracellular collagen matrix. This contributes to a raised brittleness of bone following long periods of bisphosphonate treatment21 as well.
Other causes
Although the occurrence of atypical femoral fractures has primarily been associated with the intake of bisphosphonates, these fractures have also been described in patients with no exposure to these drugs. Recently, a fracture was reported following daily ibandronate prescribed for bone metastases in breast cancer.22 Since the application of antiresorptive drugs in these patients is also employed in long-term settings, this phenomenon is expected to become more and more apparent and common.23 Furthermore, in a Phase III multicentre, randomized, double-blind, placebo-controlled trial, reporting data for 10-year treatment with denosumab in postmenopausal women with osteoporosis, two cases of atypical femoral fractures were identified.24 In summary, other pharmacological treatments which decrease bone turnover apparently have the same consequences regarding the risk for this special fracture type. Additionally, other systemic diseases such as non-Hodgkin’s lymphoma may cause similar structural bone changes, leading to atypical femoral fractures (AFF).25 The occurrence of these special femoral fractures has been linked also to bone diseases such as hypophosphatasia,26 pycnodysostosis27 and osteopetrosis,28 vitamin D deficiency, and rheumatoid arthritis,7 since these diseases directly affect the bone structure in a similar way to bisphosphonates.
Other medications: glucocorticoids (GC), proton pump inhibitors (PPI)
Long-term use of both GC and PPI has been linked to a variety of side-effects, which also are related to bone metabolism. Proton pump inhibitor intake changes resorption and may lead to different forms of malnutrition, which has been associated with an increased general risk of fractures.29 Furthermore, several studies also associated AFF risk with PPI use.30 However, there was no correlation with fracture location.31 Similarly, long-term use of GC is known to cause osteoporosis. Recommendations include treating with calcium and vitamin D plus an additional osteoporosis medication (oral bisphosphonate preferred) in adults at moderate-to-high fracture risk.32 Since therefore the intake of bisphosphonates is frequently combined with GC, the isolated influence of GC is still under discussion. However, the importance of both medications in relation to the occurrence of AFF was rated by the ASBMR as high, so it was included in the definition as one of the minor criteria.7
Genetic mutations
Although the mechanisms of bisphosphonate action have a probable connection to atypical femur fractures, it remains unclear why this complication affects only some patients. Therefore, the search for underlying genetic predispositions is ongoing. Based on a whole-exome sequencing, a GGPS1 mutation was related to susceptibility to bisphosphonate-related atypical femoral fractures.33 Furthermore, genetic variants coding for collagen type I (COL1A2) were also suggested to account for a possible genetic susceptibility to these fractures.34 Since atypical femoral fractures occur in a variety of other situations, further forms of predisposition are likely to be discovered in future. Recently, the case of an 18-year-old patient with juvenile osteoporosis based on X-linked osteoporosis due to a PLS3 mutation was reported, who developed a low trauma femoral fracture after a nine-year period of bisphosphonate use.35
Epidemiology and predisposing factors
The relative risk of patients with atypical femoral fractures taking bisphosphonates is high; however, the absolute risk of these fractures in patients on bisphosphonates is low, ranging from 3.2 to 50 cases per 100,000 person-years. Long-term use may be associated with higher risk of about 100 per 100,000 person-years.7 In a Korean multicentre study, bone mineral density, prodromal symptoms, and medication history for osteoporosis were retrospectively analysed in 76 cases of atypical femoral fracture.4 Twenty-two patients (28.9%) suffered from prodromal symptoms, 43 (56.5%) had delayed fracture union, and bilateral femoral fractures developed in 23 (30.2%). Besides prolonged and continuous use of bisphosphonates, long-term use of glucocorticoids, and a higher body mass index (BMI) were identified as risk factors predisposing to atypical femur fractures.38 Moreover, aspects with an influence on biomechanics such as anterolateral femoral bowing and loss of thigh muscle seem to have an influence on the occurrence of these fractures.39
Evaluation and diagnosis
Incomplete and complete fractures
The characteristic features of AFF, including ‘the dreaded black line’ have been noticed in patients receiving bisphosphonate therapy,40 and comparison of different features eventually led to the definition provided by the ASBMR in 2010.7 This is very helpful in cases of complete fracture, but impending fractures must also be diagnosed and treated before they become complete.
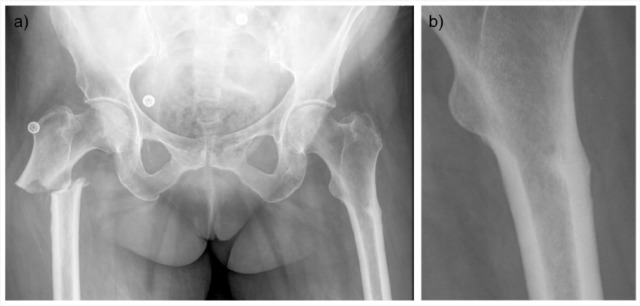
Recognizing impending fractures is challenging and requires a high index of suspicion for any patient with a history of osteoporosis, especially, but not exclusively, if currently or recently treated with bisphosphonates or other prophylactic medication and complaining of thigh or groin pain, even if they received treatment for only a brief period. When suspicious of incomplete AFF, careful radiographic exploration for features suggestive of impending fractures on hip and pelvic radiographs should occur. In patients with a complete fracture, the contralateral side should also be radiographed and carefully inspected for transverse fracture lines in lateral cortex, beaking and other characteristic signs of atypical femoral fracture (Fig. 1), since 40% or more have bilateral involvement.41 The sensitivity and specificity for these signs are generally high, especially for transverse fracture lines, lack of comminution and localized periosteal or endosteal thickening of the lateral cortex (‘beaking’).42
Fig. 1.
(a) Bilateral atypical femur fracture, complete on the right side and incomplete on the left; (b) Enlargement of incomplete fracture showing periosteal or endosteal thickening of the lateral cortex (‘beaking’).
In cases with normal radiographs on the contralateral side, but where there is still clinical suspicion, computed tomography (CT) should be considered, since fracture lines, not visible on radiographs, might be diagnosed. Lee et al36 have shown that patients with a subsequent AFF have a thicker lateral cortex in the subtrochanteric region of the femur on CT before the fracture event, than bisphosphonate (BP) users who did not sustain a femoral fracture, and than BP-naïve patients. Thus, CT might be used for the early detection of AFF in long-term BP users. Periosteal and endosteal oedema can be visible using magnetic resonance imaging (MRI) and might also be indicative of an impending fracture and might be used in conservative follow-up of impending fractures.43
Femoral morphology
The first manifestation of radiological changes related to atypical femur fractures are visible at the lateral cortex, the location with the highest bending stress. Quantitative CT analyses are able to show that long-term users of bisphosphonates with a subsequent fracture have a thicker subtrochanteric lateral cortex with a higher bone mineral density compared with patients who did not sustain a femoral fracture.36 This is associated with a higher lateral femoral bowing angle with a vertex located at the site of the later subtrochanteric fracture.37
Histological and micro-CT
Micro-CT scanning and histological evaluation of biopsies from patients with atypical femur fractures or from a sheep model of fatigue fracture demonstrated a higher diameter of Haversian canals and diffuse microdamage as a result of higher local stresses and reduced natural repair capacity.8,9
Atypical manifestations
Usually, the term atypical femoral fracture is reserved for the untreated bone.7 However, the criteria leading to the definition can also be fulfilled in peri-prosthetic femoral fractures.10,11 Furthermore, some authors have suggested that manifestation is also possible in the intracapsular part of the femur neck.12
Prophylactic treatment
Impending fractures, as defined by the ASBMR, have an elevated risk of progressing to a complete fracture, as high as 28.3% within six months after diagnosis. Subtrochanteric location, functional pain and a radiolucent line of more than 50% of the lateral cortex were identified as risk factors for occurrence of a complete fracture.44 Prophylactic surgical treatment with cephalomedullary nail seems to be effective, both in preventing progression to complete fracture and in reducing hospital stay.45 It also seems that fractures heal faster when treated surgically.46 Progression to complete fracture and pain refractory to non-surgical treatment reduce the success rate of non-surgical treatment of incomplete fractures to approximately 50%.46
The ASBMR recommends that patients with incomplete fractures and no pain, or those with periosteal thickening but no cortical lucency, should limit weight-bearing and avoid vigorous activity. Reduced activity should be continued until there is no bone oedema detected on an MRI or no increased activity detected on a bone scan.7
Surgical treatment and complications
Cephalomedullary nailing (Fig. 2) is the preferred method for surgical fixation of complete and incomplete AFF.5,47 However, plate fixation and other methods may come into consideration depending on fracture location. It should be kept in mind that a greater percentage of fractures treated with plate fixation (31.3%) require revision surgery than fractures treated with intramedullary nailing (12.9%).5
Fig. 2.
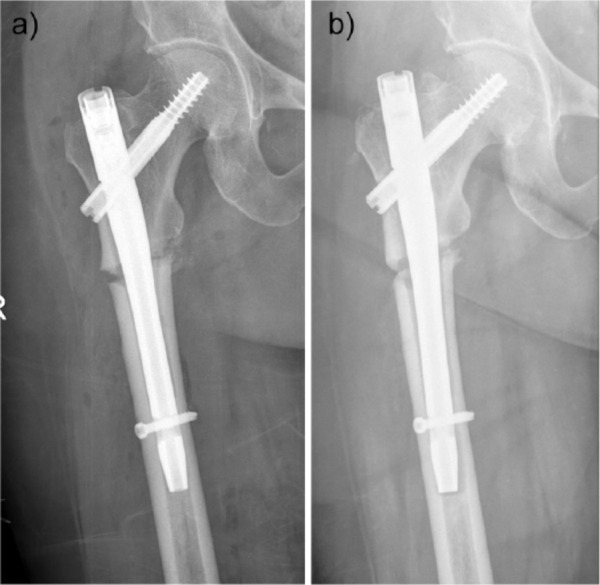
(a) Fracture fixed with gap in lateral cortex; (b) Eleven months, no signs of healing, nail is migrating lateral at the distal end.
Several studies show increased healing time for AFF. Lee et al48 showed that only 63% of 46 fractures healed within six months, but 95.7% subsequently healed without any further surgery. Egol et al46 found 98% healing within 12 months of surgical treatment, almost two-thirds returned to self-reported baseline function. The same study also found that malreduction was associated with delayed healing. Other studies have not been able to achieve the same high healing rate. A recent review by Koh et al5 including 733 patients with 834 fractures showed an overall healing rate of 85% and a revision rate of 12.6%.
Lim et al49 tested 46 variables for association with healing time longer than six months or non-union. High BMI and subtrochanteric fracture location were significantly associated with delayed healing time, but these factors are not controllable. More interesting was that delayed union or non-union was significantly associated with postoperative gaps at the fracture site, primarily at the lateral or anterior cortex (Fig. 2).
Failing to restore the anatomical neck-shaft angle, when reducing and fixing AFF, has also been shown to cause significant longer healing time.50 In cases of excessive bowing, anatomical reduction might require special techniques or implants.51 Iatrogenic intraoperative fractures and implant failures are also more frequent compared with typical femur fractures.52
The literature suggests that surgical treatment of AFF is more complex than that of typical femoral fractures, healing time is prolonged and reduction and surgical technique is more demanding, leaving little room for error.
Medical treatment and other options
For patients with AFF in either form, a stress reaction, stress fracture, incomplete or complete subtrochanteric or femoral shaft fracture, bisphosphate or other potent antiresorptive agents should be discontinued. Dietary calcium and vitamin D status should be assessed, and adequate supplementation prescribed.7 Simple fixation without optimizing bone metabolic profile and stopping any possible influencing factors may prevent healing53 and even cause failure in these cases.54 Whether the antiresorptive agents should be discontinued permanently or could be resumed after a ‘drug holiday’55 of three to five years is unknown.
Teriparatide (TPTD), a recombinant form of parathyroid hormone (PTH), enhances bone healing in patients with delayed healing or non-union and is, in theory, a good option for supplement treatment in patients with bisphosphonate-associated AFF, since bone turnover is suppressed in these cases. There is only limited clinical evidence on the use of TPTD56 in treatment of AFF, and while anecdotal evidence of the beneficial effect exists, there are also anecdotal case reports of TPTD failure to prevent AFF.54 So TPTD’s role in the treatment of AFF is still unknown and it should not be used routinely.
The use of low-intensity pulsed ultrasound (LIPUS)57 and bone marrow aspirate concentrate58 has been reported in small retrospective series and case control series, but evidence is still too limited to conclude any beneficial effect.
Conclusions
Atypical femoral fractures (AFFs) located in the subtrochanteric region and diaphysis of the femur have been reported in patients taking bisphosphates and other antiresorptive drugs, but they also occur in patients with no exposure to these drugs. It seems that these fractures follow the concept of a stress or insufficiency fracture, often complicated by the use of bisphosphonates or other bone turnover inhibitors. The diagnosis follows major and minor criteria, which were originally described by the Task Force of the American Society for Bone and Mineral Research (ASBMR). The risk of suffering a fracture is very low, even after long term use of bisphosphonate, but the diagnosis should lead to discontinuation. The treatment of complete and incomplete fractures is surgical fixation in most cases; observation is recommended only in cases where there is no pain. Further studies on optimal treatment of incomplete fractures and antiresorptive treatment after AFF are still needed.
Take-home messages
The diagnosis of ‘atypical femoral fracture’ should be made according to ASBMR criteria (Table 1)
The pathogenesis follows the concept of a stress or insufficiency fracture
Atypical femoral fractures are often seen in patients treated with bisphosphates, but can also occur in other patients
Radiograph of the contralateral side is essential when AFF is diagnosed
Dietary calcium and vitamin D status should be assessed, and adequate supplementation prescribed
Bisphosphonates or other potent antiresorptive agents should be discontinued
Incomplete fractures should be treated with prophylactic nailing in most cases
Complete fractures should be treated with stable fixation, avoiding fracture gaps and restoration of anatomical neck-shaft angle
Footnotes
ICMJE Conflict of interest statement: M. Schultz Larsen declares travel/accommodation/meeting expenses from the EFORT Trauma Education group, activity outside the submitted work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Wells GA, Cranney A, Peterson J, et al. Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev 2008;1:CD001155. [DOI] [PubMed] [Google Scholar]
- 2. Geissler JR, Bajaj D, Fritton JC. American Society of Biomechanics Journal of Biomechanics Award 2013: cortical bone tissue mechanical quality and biological mechanisms possibly underlying atypical fractures. J Biomech 2015;48:883–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kharwadkar N, Mayne B, Lawrence JE, Khanduja V. Bisphosphonates and atypical subtrochanteric fractures of the femur. Bone Joint Res 2017;6:144–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kang JS, Won YY, Kim JO, et al. Atypical femoral fractures after anti-osteoporotic medication: a Korean multicenter study. Int Orthop 2014;38:1247–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Koh A, Guerado E, Giannoudis PV. Atypical femoral fractures related to bisphosphonate treatment: issues and controversies related to their surgical management. Bone Joint J 2017;99-B:295–302. [DOI] [PubMed] [Google Scholar]
- 6. Greenspan SL, Vujevich K, Britton C, et al. Teriparatide for treatment of patients with bisphosphonate-associated atypical fracture of the femur. Osteoporos Int 2018;29:501–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2014;29:1–23. [DOI] [PubMed] [Google Scholar]
- 8. Brock GR, Chen JT, Ingraffea AR, et al. The effect of osteoporosis treatments on fatigue properties of cortical bone tissue. Bone Rep 2015;2:8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Somford MP, van Ruijven LJ, Kloen P, Bakker AD. Histological and micro computed tomography analysis of a femoral stress fracture associated with prolonged bisphosphonate use. Clin Cases Miner Bone Metab 2017;14:92–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Woo SB, Choi ST, Chan WL. Atypical periprosthetic femoral fracture: a case report. J Orthop Surg (Hong Kong) 2016;24:269–272. [DOI] [PubMed] [Google Scholar]
- 11. Lee K-J, Min B-W, Jang H-K, Ye H-U, Lim K-H. Periprosthetic atypical femoral fracture-like fracture after hip arthroplasty: a report of three cases. Hip Pelvis 2015;27:187–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Khan SK, Savaridas T, Hemers JS, Maarouf Z, Orgee JM, Orr MM. Atraumatic intracapsular neck of femur fractures after prolonged bisphosphonate treatment: a new atypical variant? Clin Cases Miner Bone Metab 2016;13:38–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sutton RAL, Mumm S, Coburn SP, Ericson KL, Whyte MP. ‘Atypical femoral fractures’ during bisphosphonate exposure in adult hypophosphatasia. J Bone Miner Res 2012;27:987–994. [DOI] [PubMed] [Google Scholar]
- 14. Birmingham P, McHale KA. Case reports: treatment of subtrochanteric and ipsilateral femoral neck fractures in an adult with osteopetrosis. Clin Orthop Relat Res 2008;466:2002–2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Boonekamp PM, van der Wee-Pals LJ, van Wijk-van Lennep MM, Thesing CW, Bijvoet OL. Two modes of action of bisphosphonates on osteoclastic resorption of mineralized matrix. Bone Miner 1986;1:27–39. [PubMed] [Google Scholar]
- 16. Carano A, Teitelbaum SL, Konsek JD, Schlesinger PH, Blair HC. Bisphosphonates directly inhibit the bone resorption activity of isolated avian osteoclasts in vitro. J Clin Invest 1990;85:456–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Löwik CW, van der Pluijm G, van der Wee-Pals LJ, van Treslong-De Groot HB, Bijvoet OL. Migration and phenotypic transformation of osteoclast precursors into mature osteoclasts: the effect of a bisphosphonate. J Bone Miner Res 1988;3:185–192. [DOI] [PubMed] [Google Scholar]
- 18. Plasmans CM, Jap PH, Kuijpers W, Slooff TJ, Wijers M. Influence of a diphosphonate on the cellular aspect of young bone tissue. Calcif Tissue Int 1980;32:247–266. [DOI] [PubMed] [Google Scholar]
- 19. Allen MR, Iwata K, Phipps R, Burr DB. Alterations in canine vertebral bone turnover, microdamage accumulation, and biomechanical properties following 1-year treatment with clinical treatment doses of risedronate or alendronate. Bone 2006;39:872–879. [DOI] [PubMed] [Google Scholar]
- 20. Donnelly E, Meredith DS, Nguyen JT, et al. Reduced cortical bone compositional heterogeneity with bisphosphonate treatment in postmenopausal women with intertrochanteric and subtrochanteric fractures. J Bone Miner Res 2012;27:672–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Vashishth D, Gibson GJ, Khoury JI, Schaffler MB, Kimura J, Fyhrie DP. Influence of nonenzymatic glycation on biomechanical properties of cortical bone. Bone 2001;28:195–201. [DOI] [PubMed] [Google Scholar]
- 22. Espey R, Grimes S, Heyburn G, Kealey WD. The first reported case of atypical femoral fracture caused by daily ibandronate prescribed for bone metastases in breast cancer. BMJ Case Rep 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ota S, Inoue R, Shiozaki T, et al. Atypical femoral fracture after receiving antiresorptive drugs in breast cancer patients with bone metastasis. Breast Cancer 2017;24:601–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bone HG, Wagman RB, Brandi ML, et al. 10 years of denosumab treatment in postmenopausal women with osteoporosis: results from the phase 3 randomised FREEDOM trial and open-label extension. Lancet Diabetes Endocrinol 2017;5:513–523. [DOI] [PubMed] [Google Scholar]
- 25. Saviola G, Prometti P, Ferrari PR, Dalle Carbonare LG. Atypical femoral fracture as first sign of non-hodgkin lymphoma: case report with a brief review of the literature. Clin Ter 2016;167:188–190. [DOI] [PubMed] [Google Scholar]
- 26. Whyte MP. Atypical femoral fractures, bisphosphonates, and adult hypophosphatasia. J Bone Miner Res 2009;24:1132–1134. [DOI] [PubMed] [Google Scholar]
- 27. Yates CJ, Bartlett MJ, Ebeling PR. An atypical subtrochanteric femoral fracture from pycnodysostosis: a lesson from nature. J Bone Miner Res 2011;26:1377–1379. [DOI] [PubMed] [Google Scholar]
- 28. Kumbaraci M, Karapinar L, Incesu M, Kaya A. Treatment of bilateral simultaneous subtrochanteric femur fractures with proximal femoral nail antirotation (PFNA) in a patient with osteopetrosis: case report and review of the literature. J Orthop Sci 2013;18:486–489. [DOI] [PubMed] [Google Scholar]
- 29. Nishtala PS, Soo L. Proton pump inhibitors utilisation in older people in New Zealand from 2005 to 2013. Intern Med J 2015;45:624–629. [DOI] [PubMed] [Google Scholar]
- 30. Kim D, Sung Y-K, Cho S-K, Han M, Kim Y-S. Factors associated with atypical femoral fracture. Rheumatol Int 2016;36:65–71. [DOI] [PubMed] [Google Scholar]
- 31. Hyodo K, Nishino T, Kamada H, Nozawa D, Mishima H, Yamazaki M. Location of fractures and the characteristics of patients with atypical femoral fractures: analyses of 38 Japanese cases. J Bone Miner Metab 2017;35:209–214. [DOI] [PubMed] [Google Scholar]
- 32. Buckley L, Guyatt G, Fink HA, et al. 2017 American College of Rheumatology guideline for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res (Hoboken) 2017;69:1095–1110. [DOI] [PubMed] [Google Scholar]
- 33. Roca-Ayats N, Balcells S, Garcia-Giralt N, et al. GGPS1 mutation and atypical femoral fractures with bisphosphonates. N Engl J Med 2017;376:1794–1795. [DOI] [PubMed] [Google Scholar]
- 34. Funck-Brentano T, Ostertag A, Debiais F, et al. Identification of a p.Arg708Gln variant in COL1A2 in atypical femoral fractures. Joint Bone Spine 2017;84:715–718. [DOI] [PubMed] [Google Scholar]
- 35. van de, Laarschot DM, Zillikens MC. Atypical femur fracture in an adolescent boy treated with bisphosphonates for X-linked osteoporosis based on PLS3 mutation. Bone 2016;91:148–151. [DOI] [PubMed] [Google Scholar]
- 36. Lee SH, Lee YH, Suh J-S. Lateral cortical thickening and bone heterogeneity of the subtrochanteric femur measured with quantitative CT as indicators for early detection of atypical femoral fractures in long-term bisphosphonate users. AJR Am J Roentgenol 2017;209:867–873. [DOI] [PubMed] [Google Scholar]
- 37. Yoo H, Cho Y, Park Y, Ha S. Lateral femoral bowing and the location of atypical femoral fractures. Hip Pelvis 2017;29:127–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Koh JH, Myong JP, Yoo J, et al. Predisposing factors associated with atypical femur fracture among postmenopausal Korean women receiving bisphosphonate therapy: 8 years’ experience in a single center. Osteoporos Int 2017;28:3251–3259. [DOI] [PubMed] [Google Scholar]
- 39. Shin WC, Moon NH, Jang JH, Park KY, Suh KT. Anterolateral femoral bowing and loss of thigh muscle are associated with occurrence of atypical femoral fracture: effect of failed tension band mechanism in mid-thigh. J Orthop Sci 2017;22:99–104. [DOI] [PubMed] [Google Scholar]
- 40. Porrino JA, Jr, Kohl CA, Taljanovic M, Rogers LF. Diagnosis of proximal femoral insufficiency fractures in patients receiving bisphosphonate therapy. AJR Am J Roentgenol 2010;194:1061–1064. [DOI] [PubMed] [Google Scholar]
- 41. Schilcher J, Aspenberg P. Incidence of stress fractures of the femoral shaft in women treated with bisphosphonate. Acta Orthop 2009;80:413–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Adams AL, Xue F, Chantra JQ, et al. Sensitivity and specificity of radiographic characteristics in atypical femoral fractures. Osteoporos Int 2017;28:413–417. [DOI] [PubMed] [Google Scholar]
- 43. Png MA, Koh JSB, Goh SK, Fook-Chong S, Howe TS. Bisphosphonate-related femoral periosteal stress reactions: scoring system based on radiographic and MRI findings. AJR Am J Roentgenol 2012;198:869–877. [DOI] [PubMed] [Google Scholar]
- 44. Min B-W, Koo K-H, Park Y-S, et al. Scoring system for identifying impending complete fractures in incomplete atypical femoral fractures. J Clin Endocrinol Metab 2017;102:545–550. [DOI] [PubMed] [Google Scholar]
- 45. Banffy MB, Vrahas MS, Ready JE, Abraham JA. Nonoperative versus prophylactic treatment of bisphosphonate-associated femoral stress fractures. Clin Orthop Relat Res 2011;469:2028–2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Egol KA, Park JH, Prensky C, Rosenberg ZS, Peck V, Tejwani NC. Surgical treatment improves clinical and functional outcomes for patients who sustain incomplete bisphosphonate-related femur fractures. J Orthop Trauma 2013;27:331–335. [DOI] [PubMed] [Google Scholar]
- 47. Bogdan Y, Tornetta P, III, Einhorn TA, et al. Healing time and complications in operatively treated atypical femur fractures associated with bisphosphonate use: a multicenter retrospective cohort. J Orthop Trauma 2016;30:177–181. [DOI] [PubMed] [Google Scholar]
- 48. Lee K-J, Yoo JJ, Oh K-J, et al. Surgical outcome of intramedullary nailing in patients with complete atypical femoral fracture: a multicenter retrospective study. Injury 2017;48:941–945. [DOI] [PubMed] [Google Scholar]
- 49. Lim H-S, Kim C-K, Park Y-S, Moon Y-W, Lim S-J, Kim S-M. Factors associated with increased healing time in complete femoral fractures after long-term bisphosphonate therapy. J Bone Joint Surg Am 2016;98:1978–1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Cho J-W, Oh C-W, Leung F, et al. Healing of atypical subtrochanteric femur fractures after cephalomedullary nailing: which factors predict union? J Orthop Trauma 2017;31:138–145. [DOI] [PubMed] [Google Scholar]
- 51. Park Y-C, Song H-K, Zheng X-L, Yang K-H. Intramedullary nailing for atypical femoral fracture with excessive anterolateral bowing. J Bone Joint Surg Am 2017;99:726–735. [DOI] [PubMed] [Google Scholar]
- 52. Prasarn ML, Ahn J, Helfet DL, Lane JM, Lorich DG. Bisphosphonate-associated femur fractures have high complication rates with operative fixation. Clin Orthop Relat Res 2012;470:2295–2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Maheshwari AV, Yarmis SJ, Tsai J, Jauregui JJ. Progression of bisphosphonate-associated impending atypical femoral fracture despite prophylactic cephalomedullary nailing: a case report and review of literature. J Clin Orthop Trauma 2016;7:92–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Nguyen HH, Milat F, Ebeling PR. A new contralateral atypical femoral fracture despite sequential therapy with teriparatide and strontium ranelate. Bone Rep 2017;6:34–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Anagnostis P, Paschou SA, Mintziori G, et al. Drug holidays from bisphosphonates and denosumab in postmenopausal osteoporosis: EMAS position statement. Maturitas 2017;101:23–30. [DOI] [PubMed] [Google Scholar]
- 56. Im G-I, Lee S-H. Effect of teriparatide on healing of atypical femoral fractures: a systemic review. J Bone Metab 2015;22:183–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lee SY, Niikura T, Iwakura T, Fukui T, Kuroda R. Clinical experience with the use of low-intensity pulsed ultrasound (LIPUS) in the treatment of atypical femoral fractures. J Orthop Trauma 2017;31:S2. [DOI] [PubMed] [Google Scholar]
- 58. Lovy AJ, Kim JS, Di Capua J, et al. Intramedullary nail fixation of atypical femur fractures with bone marrow aspirate concentrate leads to faster union: a case-control study. J Orthop Trauma 2017;31:358–362. [DOI] [PubMed] [Google Scholar]