Abstract
Objective
The aim of this study was to identify factors associated with perforated acute appendicitis in geriatric patients at the emergency department (ED).
Patients and methods
The medical records of 223 consecutive patients aged >60 years with acute appendicitis between 2006 and 2017 were retrospectively reviewed. Patients were grouped into those with perforated and non-perforated appendicitis. A comparison was made between the two groups in regard to baseline characteristics, clinical presentation, physical examination, time from onset of symptoms to ED arrival, time from ED arrival to operation, postoperative complications, hospital length of stay, and mortality. Significant factors associated with perforated appendicitis were examined using univariate and multivariate analyses by logistic regression.
Results
A total of 78 (35%) patients had perforated appendicitis. Four significant factors associated with perforated appendicitis were as follows: 1) time duration from onset of symptoms to ED arrival >24 hours (OR 2.49, CI 1.33–4.68); 2) heart rate ≥90 beats/minute (OR 1.93, CI 1.04–3.59); 3) respiratory rate ≥20 breaths/minute (OR 2.54, CI 1.33–4.84); and 4) generalized guarding (OR 12.58, CI 1.43–110.85).
Conclusion
Time duration from onset of symptoms to ED arrival >24 hours, heart rate ≥90 beats/minute, respiratory rate ≥20 breaths/minute, and generalized guarding were the significant factors associated with perforated acute appendicitis in geriatric patients.
Keywords: perforated appendicitis, geriatric, emergency department
Introduction
Abdominal pain in geriatric patients is a common clinical presentation at the emergency department (ED). Five percent of this population had acute appendicitis.1,2 Emergency appendectomy was the third most common reason for abdominal surgery in geriatric patients.1,2 The diagnosis of acute appendicitis in geriatric patients is difficult, and there were 5% diagnostic errors in the ED because of atypical presentations.3,4 The incidence of perforated acute appendicitis is high at 40%–70%,3 with increased postoperative complications and mortality. Therefore, an early and accurate diagnosis of perforated appendicitis at the ED is challenging for emergency physicians (EPs) to improve patient safety and outcomes.4,5 The aims of this study were to identify the risk factors associated with perforated acute appendicitis in geriatric patients and evaluate the postoperative complications, hospital length of stay (LOS), and mortality rate.
Patients and methods
Study design and setting
This was a retrospective study at Songklanagarind Hospital, which is a tertiary university hospital. The data were collected from January 2006 to August 2017. The inclusion criteria were as follows: 1) elderly (aged >60 years as defined by the Elderly Person Act of Thailand 2003) who visited the ED; 2) patients who underwent an operation at Songklanagarind Hospital; and 3) patients whose pathological results confirmed the diagnosis of acute appendicitis. The exclusion criteria were acute appendicitis and referred in from other hospitals. Ethics approval was obtained from the institutional ethics committee board of the Faculty of Medicine at Prince of Songkla University. According to our institutional review board protocol, the requirement for informed consent was waived because the participants had no more than minimal risk and standard treatment procedures were followed. All research information was kept as confidential data in an encrypted file with a password with limited access to the data by only the researcher and assistant.
When the patients present at the ED, the EP evaluates the history and physical examination and obtains laboratory results to make the provisional diagnosis. This study reported localized and generalized guarding as signs of peritonitis. Localized guarding at the right lower quadrant means confinement to a demarcated region of the peritoneal cavity at the right lower quadrant and is often associated with acute appendicitis. Generalized guarding affects the entire abdomen, which indicates that the inflammation is widespread throughout the entire abdomen and is more life-threatening than localized guarding. The diagnostic tools the EP uses are fever >38°C, right lower abdominal pain, increased white blood cell (WBC) count ≥10,000/μL, and Alvarado scores.
In the case of acute appendicitis, the EP will prepare preoperative management and consult the surgeon. It is the surgeon’s decision whether to perform further imaging investigations, such as abdominal ultrasonography (US) or abdominal computerized tomography (CT). The results of imaging are reported by the radiologist. After diagnosis, the patient undergoes open appendectomy or laparoscopic appendectomy and the diagnosis is confirmed by pathological results.
Data collection
The data collected from the medical records included the patient’s baseline characteristics, clinical presentations, physical examination, investigations, provisional diagnosis, and pathological diagnosis. The patients were categorized into two groups: 1) perforated group (free or contained perforation and abscess formation) and 2) non-perforated group (acute inflammation and suppurative, strangulated, or gangrenous appendicitis).
Outcome measurements
The primary outcome measure was to identify the factors associated with perforated acute appendicitis in geriatric patients. The secondary outcomes were postoperative complications, hospital LOS, and mortality rate.
Statistical analyses
Statistical analyses were conducted using R software version 3.2.2. Continuous variables were analyzed and reported as median, while discrete variables were reported as percentage. All data were based on nonparametric frequency distributions. The univariate model analyzed the baseline characteristics, clinical presentation, physical examination, laboratory results, and the duration of time from onset of symptoms to ED arrival. The data were compared in subjects with and without perforation. The duration of time from ED arrival to operation was analyzed using the log-rank test. Continuous variables were compared using the Mann–Whitney U test. Categorical variables were compared using the c2 or Fisher’s exact test as indicated. Significant factors associated with perforated appendicitis (P<0.2) identified during univariate analysis were introduced into a logistic regression model with backward stepwise selection. First-order interaction terms with combinations of all independent predictors were introduced into the multivariate model one at a time. Generally, interaction terms were considered with statistical significance set at P<0.05 and no significant interaction between the included variables in the final logistic regression models. Modeling results are shown as OR with 95% CI. A two-tailed P-value of <0.05 was selected as the level of statistical significance.
Results
In this study, 223 patients met the inclusion criteria. Seventy-eight patients (35%) had perforated appendicitis. The percentages of patients who were male, older, and presented with underlying disease were greater in the perforated group (Table 1).
Table 1.
Baseline characteristics of the patients
| Characteristic | Perforated group (n=78) | Non-perforated group (n=145) | Total (N=223) | P-value |
|---|---|---|---|---|
| Age, years, median (IQR) | 70 (64–76.8) | 68 (63–74) | 68 (64–75) | 0.127 |
| Sex | 0.097 | |||
| Male | 41 (52.6) | 58 (40.0) | 99 (44.4) | |
| Female | 37 (47.4) | 87 (60.0) | 124 (55.6) | |
| Underlying disease | 61 (78.2) | 95 (65.5) | 156 (70) | 0.069 |
| Hypertension | 34 (43.6) | 54 (37.2) | 88 (39.5) | 0.435 |
| Diabetes mellitus | 14 (17.9) | 17 (11.7) | 31 (13.9) | 0.281 |
| Heart disease | 9 (11.5) | 11 (7.6) | 20 (9) | 0.46 |
| Pulmonary disease | 3 (3.8) | 7 (4.8) | 10 (4.5) | 1.00 |
| Cerebrovascular disease | 2 (2.6) | 8 (5.5) | 10 (4.5) | 0.50 |
| Cognitive disorder | 1 (1.3) | 1 (0.7) | 2 (0.9) | 1.00 |
| Chronic kidney disease | 3 (3.8) | 0 (0) | 3 (1.3) | 0.042 |
| Connective tissue disease | 1 (1.3) | 0 (0) | 1 (0.4) | 0.35 |
Note: Data are presented as n (%) unless indicated otherwise.
Abbreviation: IQR, interquartile range.
The median (interquartile range [IQR]) time duration from onset of symptoms to arrival at the ED in the perforated group was longer than that in the non-perforated group (24 hours [17.2–48] vs 19 hours [9.1–24]) with a statistical significance. In the perforated group, the initial presentations of fever, right lower abdominal pain, and migratory pain occurred in 32.1%, 70.5%, and 25.6% of the cases, respectively. On physical examination, the significant vital signs were heart rate ≥90 beats/minute (52.6% vs 35.2%, P=0.018) and respiratory rate ≥20 breaths/minute (75.6% vs 51.7%, P<0.001). Table 2 shows that generalized guarding was found in 10.3% of patients with a statistical significance. In the perforated group, leukocytosis (WBC count ≥10,000 cells/μL) was found in 71.8% of patients and bandemia (band cells >10%) was found in 25% of patients. In addition, 21.8% of the patients who had perforated appendicitis had Alvarado scores ≤4 points and 80.8% had an atypical presentation.
Table 2.
Comparison of clinical presentation, physical examination, and laboratory test
| Variable | Perforated group (n=78) | Non-perforated group (n=145) | Total (N=223) | P-value |
|---|---|---|---|---|
| Time duration from onset of symptoms to ED arrival, hours, median (IQR) | 24 (17.2–48) | 19 (9.1–24) | 24 (11.5–30.6) | <0.01 |
| Time duration from onset of symptoms to ED arrival >24 hours | 36 (46.2) | 36(24.8) | 72 (32.3) | 0.02 |
| Fever | 25 (32.1) | 38 (26.2) | 63 (28.3) | 0.42 |
| Right lower abdominal pain | 55 (70.5) | 115 (79.3) | 170 (76.2) | 0.191 |
| Migratory pain | 20 (25.6) | 49 (33.8) | 69 (30.9) | 0.27 |
| Nausea/vomiting | 43 (55.1) | 73 (50.3) | 116 (52) | 0.58 |
| Anorexia | 17 (21.8) | 20 (13.8) | 37 (16.6) | 0.179 |
| Heart rates ≥90 beats/minute | 41 (52.6) | 51 (35.2) | 92 (41.3) | 0.018 |
| Respiratory rates ≥20 breaths/minute | 59 (75.6) | 75 (51.7) | 134 (60.1) | <0.001 |
| SBP ≥90 mmHg | 78 (100) | 144 (99.3) | 222 (99.6) | 1 |
| Right lower abdominal tenderness | 67 (85.9) | 135 (93.1) | 202 (90.6) | 0.27 |
| Rebound tenderness | 55 (70.5) | 105 (72.4) | 160 (71.7) | 0.27 |
| Localized guarding at right lower abdominal quadrant | 10 (12.8) | 10 (6.9) | 20 (9) | 0.218 |
| Generalized guarding | 8 (10.3) | 1 (0.7) | 9 (4) | 0.001 |
| Leukocytosis (WBC count ≥10,000/μL) | 56 (71.8) | 114 (78.6) | 170 (76.2) | 0.329 |
| Neutrophils >75% median (IQR) | 81 (74–87) | 81 (75–87) | 81 (75–87) | 0.914 |
| Band cells >10% | 8 (25) | 3(10.3) | 11 (18) | 0.249 |
| Alvarado score (points) | 0.37 | |||
| ≤4 | 17 (21.8) | 22 (15.2) | 39 (17.5) | |
| 5–6 | 30 (38.5) | 54 (37.2) | 84 (37.7) | |
| ≥7 | 31 (39.7) | 69 (47.6) | 100 (44.8) | |
| Presentation | ||||
| Typical presentation | 15 (19.2) | 22 (15.2) | 37 (16.6) | 0.556 |
| Atypical presentation | 63 (80.8) | 123 (84.8) | 186 (83.4) | 0.556 |
Notes: Data are presented as n (%) unless indicated otherwise. Values <0.05 are statistically significant.
Abbreviations: ED, emergency department; IQR, interquartile range; SBP, systolic blood pressure; WBC, white blood cell.
The provisional diagnosis of acute appendicitis by the EP was correct in 90.6% of patients, and a missed diagnosis occurred in 9.4% of patients. The most common missed diagnosis was gut obstruction (Table 3). A total of 80 (35.9%) patients had abdominal US that detected acute appendicitis in 57.5% of patients, undetected perforated appendicitis in 16 patients (20%), and 18 (22.5%) patients needed further abdominal CT. In all, 97 (43.5%) patients had an abdominal CT. Abdominal CT for diagnosis of perforated appendicitis had a sensitivity, specificity, and accuracy of 60.5%, 96.61%, and 82.5%, respectively.
Table 3.
Comparison of provisional diagnosis and definitive diagnosis
| Provisional diagnosis by EP | Total (N=223) | Definitive diagnosis of acute appendicitis
|
|
|---|---|---|---|
| Perforated group | Non-perforated group | ||
| Acute appendicitis | 202 | 63 (28.25) | 139 (62.33) |
| Gut obstruction | 9 | 9 (4.03) | 0 |
| Peritonitis | 5 | 5 (2.24) | 0 |
| Acute diverticulitis | 6 | 1 (0.44) | 5 (2.24) |
| Acute gastroenteritis | 1 | 1 (0.44) | 0 |
Note: Data are presented as n (%).
Abbreviation: EP, emergency physician.
Multivariate analysis revealed that the significant risk factors associated with perforated appendicitis were time duration >24 hours from onset of symptom to ED arrival, heart rate ≥90 beats/minute, respiratory rate ≥20 breaths/minute, and generalized guarding (Table 4).
Table 4.
Multivariate analysis by logistic regression if perforated appendicitis occurred
| Variable | Crude OR (95% CI) | Adjusted OR (95% CI) | P-value |
|---|---|---|---|
| Time duration from onset of symptoms to ED arrival >24 hours | 2.6 (1.45–4.65) | 2.49 (1.33–4.68) | 0.004 |
| Heart rates ≥90 beat/minute | 2.04 (1.17–3.58) | 1.93 (1.04–3.58) | 0.035 |
| Respiratory rates ≥20 breaths/minute | 2.9 (1.57–5.34) | 2.54 (1.33–4.84) | 0.004 |
| Presented with generalized guarding | 16.46 (2.02–134.17) | 12.58 (1.43–110.85) | 0.004 |
Note: Values <0.05 are statistically significant.
Abbreviation: ED, emergency department.
The overall median time duration from ED arrival to operation was 7.27 hours in the perforated group, which was significantly longer than that in the non-perforated group (Figure 1). Time duration from ED arrival to operation >6 hours was a significant factor associated with perforated acute appendicitis (adjusted OR 2.1, 95% CI 1.13–3.9; P=0.017).
Figure 1.
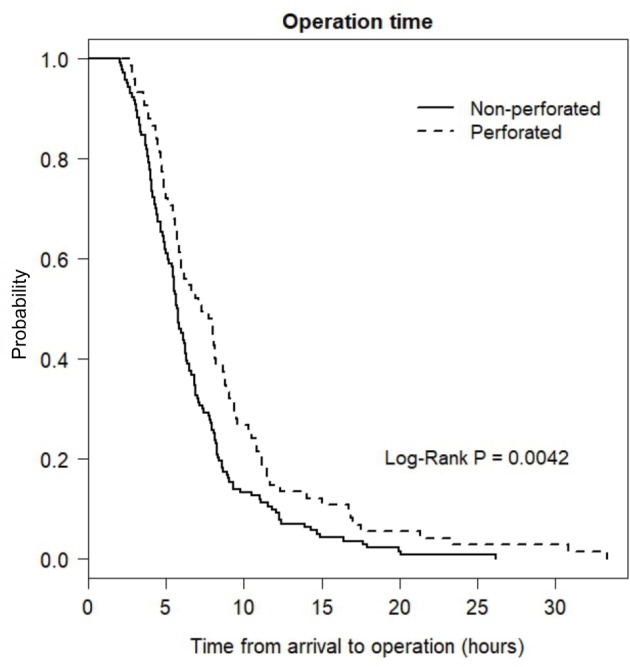
Time from ED arrival to operation between the two groups.
Note: The median values in the non-perforated group and perforated group were 5.72 and 7.27 hours, respectively.
Abbreviation: ED, emergency department.
The total percentage of postoperative complications was 4.03%, and the significant postoperative complication in the perforated group was wound dehiscence (5.1%; P=0.014). The median hospital LOS was 6.5 days in the perforated group and 3 days in the non-perforated group. The mortality rate was 0 (Table 5).
Table 5.
Postoperative complications, hospital LOS, and mortality
| Outcome | Perforated group (n=78) | Non-perforated group (n=145) | Total (N=223) | P-value |
|---|---|---|---|---|
| Surgical wound infection | 2 (2.6) | 1 (0.7) | 3 (1.3) | 0.281 |
| Wound dehiscence | 4 (5.1) | 0 (0) | 4 (1.8) | 0.014 |
| Abdominal infection/collection | 2 (2.6) | 0 (0) | 2 (0.9) | 0.121 |
| Hospital LOS, days, median (IQR) | 6.5 (5–7) | 3 (3–5) | 4 (3–6) | <0.001 |
Notes: Data are presented as n (%) unless indicated otherwise. Values <0.05 are statistically significant.
Abbreviations: LOS, length of stay; IQR, interquartile range.
Discussion
In this study, 16.6% of geriatric patients had the typical triad presentation of fever, right lower abdominal pain, and leukocytosis of acute appendicitis. The incidence of perforated acute appendicitis was 35%, which was similar to previous studies.6–8 Time duration >24 hours from onset of symptoms to ED arrival was a significant factor associated with the perforated group (OR 2.49, CI 1.33–4.68). This result was within the range of the 1.23- to 4.21-fold increased risk for perforated acute appendicitis from previous studies.1,6–8 In this study, fever was not a significant factor in the perforated group, which differed from other studies.1,6,8 Heart rate ≥90 beats/minute (OR 1.93, CI 1.04–3.58) and respiratory rate ≥20 breaths/minute (OR 2.54, CI 1.33–4.84) were the significant vital signs in the perforated group, which corresponded to systemic inflammatory response. The patients who had perforated acute appendicitis had right lower abdominal pain and rebound tenderness on abdominal examination (70%–90%), which were the same as in previous studies.1,6,8 Generalized guarding and signs of peritonitis were significant factors associated with perforated acute appendicitis (OR 12.58, CI 1.43–110.85).
The Alvarado score can be used as a tool for the diagnosis of acute appendicitis. If the score is ≤4 points, it is unlikely to be acute appendicitis. A score of 5–6 points is compatible with acute appendicitis, and a score ≥7 points is probably acute appendicitis.9 In this study, 17.5% of all patients who had an Alvarado score ≤4 points had acute appendicitis, and 43.6% of these patients had perforated acute appendicitis. The study of Shchatsko et al10 suggested using an alterative Alvarado score in geriatric patients that considered higher risk for acute appendicitis if the score was ≥5 points. However, high Alvarado scores do not correlate with severity and accuracy for diagnosis of acute appendicitis.8,11,12 Therefore, the EP should avoid using the Alvarado score only for the diagnosis of acute appendicitis in geriatric patients. The abdominal CT in this study had a specificity of 96.6 and an accuracy of 82.5, which was as high as in previous studies6,8,12 and is the preferred test for diagnosis.
The time duration was >6 hours from ED arrival to operation. This study showed a 2.1-fold increased risk associated with perforated acute appendicitis, which was consistent with longer ED LOS for an increased risk of perforation,1,8 but this study did not identify causes that affected ED LOS.
For the secondary outcomes, the significant postoperative complication in the perforated group was wound dehiscence. The median hospital LOS in the perforated group was 6.5 days, which was significantly longer than that in the non-perforated appendicitis patients (similar to previous studies1,5,6,12).
The retrospective nature of this study was a limitation. We were unable to collect some data such as the waiting time from ED registration to see a doctor, laboratory waiting time, and the time duration from ED arrival to surgical consultation, which influenced the time duration of ED LOS. A prospective study to evaluate the process of care and waiting time may find a shorter time duration from ED arrival to operation, which would improve the quality of care for geriatric patients.
Conclusion
The EP should consider the diagnosis of perforated appendicitis in geriatric patients who present with a time duration >24 hours from the onset of symptoms to ED arrival, heart rate ≥90 beats/minute, respiratory rate ≥20 breaths/minute, and on physical examination showed generalized guarding.
What is already known on this topic?
Several studies have shown factors to predict perforated acute appendicitis in geriatric patients at an ED.
What this study adds?
This study focuses on the vital signs of patients and identifies the factors associated with perforated acute appendicitis.
Acknowledgments
The authors thank Kingkarn Waiyanak for searching articles and retrieval, Glenn K. Shingledecker for his help in editing the manuscript, and the Faculty of Medicine for funding this research.
Footnotes
Author contributions
Nuraianee Arwae performed the literature research, study design, data collection, data analysis, data interpretation, and writing of the manuscript. Siriwimon Tantarattanapong did the study design, critical revision and writing manuscript. Both authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Sheu BF, Chiu TF, Chen JC, Tung MS, Chang MW, Young YR. Risk factors associated with perforated appendicitis in elderly patients presenting with signs and symptoms of acute appendicitis. ANZ J Surg. 2007;77(8):662–666. doi: 10.1111/j.1445-2197.2007.04182.x. [DOI] [PubMed] [Google Scholar]
- 2.Lunca S, Bouras G, Romedea NS. Acute appendicitis in the elderly patient: diagnostic problems, prognostic factors and outcomes. Rom J Gastroenterol. 2004;13(4):299–303. [PubMed] [Google Scholar]
- 3.Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196–205. doi: 10.1016/j.annemergmed.2006.06.035. [DOI] [PubMed] [Google Scholar]
- 4.Othong R, Wuthisuthimethawee P, Vasinanukorn P. Emergency department diagnosis of acute abdominal pain in elderly patients. Songkla Med J. 2010;28(1):31–42. [Google Scholar]
- 5.Saber A, Gad MA, Ellabban GM. Patient Safety in Delayed Diagnosis of Acute Appendicitis. Surg Sci. 2011;02(06):318–321. [Google Scholar]
- 6.Omari AH, Khammash MR, Qasaimeh GR, Shammari AK, Yaseen MKB, Hammori SK. Acute appendicitis in the elderly: risk factors for perforation. World J EmergSurg. 2014;9(1):6. doi: 10.1186/1749-7922-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Storm-Dickerson TL, Horattas MC. What have we learned over the past 20 years about appendicitis in the elderly? Am J Surg. 2003;185(3):198–201. doi: 10.1016/s0002-9610(02)01390-9. [DOI] [PubMed] [Google Scholar]
- 8.Apisarnthanarak P, Suvannarerg V, Pattaranutaporn P, Charoensak A, Raman SS, Apisarnthanarak A. Alvarado score: can it reduce unnecessary CT scans for evaluation of acute appendicitis? Am J Emerg Med. 2015;33(2):266–270. doi: 10.1016/j.ajem.2014.11.056. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz SI, Shires GT, Spencer FC, Daly JM, Fisher JE, Galloway AC. Principles of Surgery. 10th ed. New York, NY, USA: McGraw-Hill; 2015. [Google Scholar]
- 10.Shchatsko A, Brown R, Reid T, Adams S, Alger A, Charles A. The Utility of the Alvarado Score in the Diagnosis of Acute Appendicitis in the Elderly. Am Surg. 2017;83(7):793–798. [PubMed] [Google Scholar]
- 11.Young YR, Chiu TF, Chen JC, et al. Acute appendicitis in the octogenarians and beyond: a comparison with younger geriatric patients. Am J Med Sci. 2007;334(4):255–259. doi: 10.1097/MAJ.0b013e3180ca8eea. [DOI] [PubMed] [Google Scholar]
- 12.Sirikurnpiboon S, Amornpornchareon S. Factors Associated with Perforated Appendicitis in Elderly Patients in a Tertiary Care Hospital. Surg Res Pract. 2015;2015:847681–6. doi: 10.1155/2015/847681. [DOI] [PMC free article] [PubMed] [Google Scholar]


