Abstract
Prior trauma, current stress, and poor social support contribute to youth mental health problems. As daily stressors often increase in the aftermath of traumatic events, trauma could plausibly impact psychopathology not only directly but also indirectly via ongoing stress. In this study, we examined the relative roles of trauma and daily stressors in mental health outcomes in 753 Sri Lankan adolescents residing in areas impacted by the 2004 tsunami. In 2008, participants completed measures of trauma exposure, daily stressors, social support, posttraumatic stress symptoms (PTSS), emotional and behavioral problems (EBP), and functional impairment; a subsample (n = 89) repeated these assessments 16 months later. Regression models revealed positive associations between cumulative trauma and all three mental health measures. Significant variance in these associations could be explained indirectly, via daily stressors. For PTSS, the indirect effect accounted for 26.1% of the total effect of trauma, unstandardized coefficient ab = 0. 739, 95% CI [0.459, 1.122]. For EBP this percentage was 42.4%, ab = 0.287, 95% CI [0.189, 0. 404], and for functional impairment 70.0%, ab = 0.072, 95% CI [0.049, 0.121]. Indirect effects on impairment were strongest when perceived social support was low. Although we also present evidence that pathways between stressors and psychopathology may have been bidirectional, findings support the notion that adolescents' daily stressors are important transmitters of the impact of traumatic events and highlight the need for interventions focused not only on trauma processing but also on reducing current stress and improving social support.
Resumen
Spanish Abstracts by Asociación Chilena de Estrés Traumático (ACET)
El impacto relativo de las experiencias traumáticas y los estresores diarios en los resultados de salud mental en los adolescentes de Sri Lanka
IMPACTO EN LA SALUD MENTAL DE TRAUMA Y LOS ESTRESORES DIARIOS
El trauma previo, el estrés actual y el apoyo social deficiente contribuyen a los problemas de salud mental de los jóvenes. Como los factores estresantes diarios a menudo aumentan después de los eventos traumáticos, el trauma podría tener un impacto plausible en la psicopatología no solo directa sino también indirectamente, a través del estrés continuo. En este estudio, examinamos los roles relativos del trauma y los factores estresantes diarios en los resultados de salud mental en 753 adolescentes de Sri Lanka que residen en el área afectada por el tsunami de 2004. En 2008, los participantes completaron medidas de exposición al trauma, factores estresantes diarios, apoyo social, síntomas de estrés postraumático (SEPT), problemas emocionales y de comportamiento (EBP en sus siglas en inglés) y deterioro funcional; una submuestra (n = 89) repitió estas evaluaciones 16 meses después. Los modelos de regresión revelaron asociaciones positivas entre el trauma acumulado y las tres medidas de salud mental. La variación significativa en estas asociaciones podría explicarse indirectamesnte, a través de factores estresantes diarios. Para SEPT, el efecto indirecto representó el 26.1% del efecto total del trauma, coeficiente no estandarizado ab = 0. 739, IC del 95% [0.459, 1.122]. Para EBP este porcentaje fue 42.4%, ab = 0.287, IC 95% [0.189, 0. 404], y para deterioro funcional 70.0%, ab = 0.072, IC 95% [0.049, 0.121]. Los efectos indirectos sobre el deterioro fueron más fuertes cuando el apoyo social percibido fue bajo. Aunque también presentamos evidencia de que las vías entre estresores y psicopatología pueden haber sido bidireccionales, los hallazgos respaldan la noción de que los factores estresantes diarios de los adolescentes son transmisores importantes del impacto de eventos traumáticos y resaltan la necesidad de intervenciones enfocadas no solo en el procesamiento del trauma sino también en la reducción del estrés actual y en mejorar el apoyo social.
抽象
Traditional and Simplified Chinese Abstracts by the Asian Society for Traumatic Stress Studies (AsianSTSS)
簡體及繁體中文撮要由亞洲創傷心理研究學會翻譯
The Relative Impact of Traumatic Experiences and Daily Stressors on Mental Health Outcomes in Sri Lankan Adolescents
Traditional Chinese
標題: 創傷經歷和日常壓力源對斯里蘭卡青少年心理的相對影響
撮要: 過往的創傷、當前的壓力以及缺乏社會支持, 都能導致青少年有心理問題。由於經歷創傷事件後日常壓力源一般都會提升, 創傷有可能透過持續的壓力直接和間接地影響個人的精神病理學。斯里蘭卡曾於2004年發生海嘯, 本研究透過753名居於受影響地區的青少年其心理狀況, 檢視創傷和日常壓力源帶來的相對影響。樣本於2008年進行以下測量:創傷經歷、日常壓力源、社會支持、創傷後壓力症狀(PTSS)、情緒和行為問題(EBP)、功能性損傷。16個月後, 一群子樣本(n = 89)再次進行以上測量。迴歸模型均顯示累積創傷跟其他3項心理健康測量有正向關連, 而日常壓力源能間接解釋這些關連之間顯著的方差。在PTSS方面, 這種間接效應解釋了創傷總效應的26.1%(非標準化迴歸係數ab = 0. 739, 95% CI [0.459, 1.122]);在EBP方面則為42.4% (ab = 0.287, 95% CI [0.189, 0. 404]);功能性損傷方面為70.0% (ab = 0.072, 95% CI [0.049, 0.121])。當社會支持感知為低水平時, 功能性損傷的間接效應便最強。雖然本研究提供了證據, 顯示壓力源與精神病理學之間的路徑可能為雙向性, 可是, 結果反映青少年的日常壓力源為創傷事件影響裡重要的遞質, 凸顯干預治療不應只針對處理創傷, 更應針對減輕當前壓力和提高社會支持。
Simplified Chinese
标题: 创伤经历和日常压力源对斯里兰卡青少年心理的相对影响
撮要: 过往的创伤、当前的压力以及缺乏社会支持, 都能导致青少年有心理问题。由于经历创伤事件后日常压力源一般都会提升, 创伤有可能透过持续的压力直接和间接地影响个人的精神病理学。斯里兰卡曾于2004年发生海啸, 本研究透过753名居于受影响地区的青少年其心理状况, 检视创伤和日常压力源带来的相对影响。样本于2008年进行以下测量:创伤经历、日常压力源、社会支持、创伤后压力症状(PTSS)、情绪和行为问题(EBP)、功能性损伤。16个月后, 一群子样本(n = 89)再次进行以上测量。回归模型均显示累积创伤跟其他3项心理健康测量有正向关连, 而日常压力源能间接解释这些关连之间显著的方差。在PTSS方面, 这种间接效应解释了创伤总效应的26.1%(非标准化回归系数ab = 0. 739, 95% CI [0.459, 1.122]);在EBP方面则为42.4% (ab = 0.287, 95% CI [0.189, 0. 404]);功能性损伤方面为70.0% (ab = 0.072, 95% CI [0.049, 0.121])。当社会支持感知为低水平时, 功能性损伤的间接效应便最强。虽然本研究提供了证据, 显示压力源与精神病理学之间的路径可能为双向性, 可是, 结果反映青少年的日常压力源为创伤事件影响里重要的递质, 凸显干预治疗不应只针对处理创伤, 更应针对减轻当前压力和提高社会支持。
Each year, millions of children around the globe are exposed to trauma. Although it is well established that exposure to trauma leads to a wide range of mental health problems, variation in the prevalence and severity of these psychopathologies cannot be fully explained by the severity of the traumatic stress itself. Studies have therefore looked for other factors that might influence the trauma–mental health relationship. Daily stressors have been found to increase in the aftermath of trauma (Miller, Fernando, & Berger, 2009; Miller, Omidian, Rasmussen, Yaqubi, & Daudzai, 2008). Authors of studies involving people exposed to war or natural disasters have found that daily stressors have direct effects on mental health problems. For example, stressors such as family abuse and neglect that child soldiers experienced in postconflict settings were associated with more severe posttraumatic stress symptoms (PTSS; Betancourt, Newnham, McBain, & Brennan, 2013). In adult war refugees, postmigration stressors accounted for significant variation in PTSS, anxiety, and mood disorders (Bogic et al., 2012). In a previous study of tsunami‐exposed Sri Lankan adolescents, individuals who reported stress due to peer problems and rumors after the disaster had more serious emotional and behavioral problems than those with fewer stressors (Agampodi, Agampodi, & Fonseka, 2011). In addition to exacerbating psychological symptoms in trauma victims, daily stressors have been found to interfere with daily functioning (Cerda et al., 2013).
Recent studies have investigated the possibility that daily stressors are also involved in an indirect pathway from trauma exposure to mental health problems. According to this hypothesis, trauma can indirectly heighten the risk of psychological impairment by increasing sources of chronic daily stress. Support comes from studies in both young and adult trauma survivors. In Sri Lankan youth exposed to war and tsunami, for example, part of the effect of trauma in increasing symptoms of posttraumatic stress disorder (PTSD), depression, and anxiety could be explained by heightened current deprivation, abuse, and interparental conflict (Fernando, Miller, & Berger, 2010). In adult war refugees, daily stressors secondary to displacement contributed to the psychological distress and functional impairment associated with war‐related traumatic events (Rasmussen et al., 2010). Importantly, the extent to which daily stressors play a role appears to vary according to the specific mental health outcome. In former child soldiers in Northern Uganda, 44% of the total effect of war experiences on depression and anxiety was indirect, via postwar hardships, whereas for conduct problems, 89% of the effect of war trauma was transmitted via subsequent daily stressors (Amone‐P'Olak et al., 2014). There is some evidence that indirect pathways via daily stressors are less prominent in trauma‐specific psychopathologies, such as PTSD, than in trauma‐nonspecific psychopathologies, such as depression and anxiety. For example, in young survivors of war, the pathway from trauma exposure to PTSD was partially indirect, with 79% of the total effect related to postconflict stressors, whereas the entire effect of trauma on depressive symptoms was explained by these stressors (Newnham, Pearson, Stein, & Betancourt, 2015). Results reported to date strongly support the involvement of daily stressors in the pathway from trauma to disorder, but research has focused almost exclusively on victims of war, conflict, or displacement; moreover, in many studies, the inventory of daily stressors was also specific to the local context. By broadening the scope of the investigation to assess a wider range of traumatic experiences and more generic sources of daily stress in a population of adolescents with varying degrees of trauma exposure, we hoped to extend the generalizability of previous results. In addition, the current study examined several different aspects of adolescent psychopathology: PTSD symptoms, emotional and behavioral problems, and daily functional impairment.
Knowledge about the relative contributions of traumatic events and daily stressors to the development of psychopathology is important for understanding and addressing the impact of trauma on mental health problems. In some studies, daily stressors have appeared to be at least as pathogenic, if not more so, than the initial traumatic event. In adolescents exposed to war and tsunami in Sri Lanka, for example, daily stressors such as abuse and deprivation were stronger predictors of PTSD than the initial traumatic event (Miller et al., 2009). In managing adolescent posttraumatic mental health problems, addressing daily stressors may therefore be just as important as addressing prior trauma (Miller & Rasmussen, 2010; Newnham et al., 2015).
In adults, social support directly decreases the risk of developing mental illness and can also buffer the effects of stress on adverse outcomes (Cohen & Wills, 1985). In their meta‐analysis of PTSD risk factors in children and adolescents, Trickey, Siddaway, Meiser‐Stedman, Serpell, and Field (2012) found that low social support in the aftermath of trauma had a large direct impact on the development of PTSD; however, this analysis was based on only a handful of studies with adequate social support measures and did not address whether social support might moderate the effects of trauma or ongoing adversity on PTSD in this age group. La Greca, Silverman, Lai, and Jaccard (2010) tested a model in which a complex network of direct, moderational, and mediational processes were hypothesized to link social support to the development and persistence of PTSD symptoms following a disaster. Their prospective study in young hurricane‐exposed children showed that the impact of the disaster and subsequent life stressors on the development of PTSS depended on perceived social support, which was in line with their buffering hypothesis (La Greca et al., 2010). To our knowledge, research has not yet considered whether social support might moderate the indirect pathway, via stressors, from trauma to psychopathology.
To address some gaps in current knowledge, the present study thus investigated the nature of daily stressors and their effects on PTSD symptoms, other emotional and behavioral problems, and daily functioning in Sri Lankan adolescents exposed in varying degrees to the 2004 tsunami as well as to other traumatic experiences. We focused on four main issues; first, we examined the types, frequency, and severity of daily stressors reported by adolescents in this specific sociocultural context. Second, we assessed the role of daily stressors in the association between trauma exposure and mental health problems. We hypothesized that adolescents with more daily stressors would have more PTSS, emotional and behavioral problems (EBP), and impaired daily functioning, even after controlling for potential risk factors such as age, gender, and cumulative trauma exposure. In addition, we hypothesized that a significant part of the effect of trauma on each outcome would be transmitted indirectly via daily stressors. Given the cross‐sectional design of this part of the study and the close temporal association between daily stressors and mental health problems, we also explored an alternative model in which posttrauma psychopathology might increase the occurrence or perception of daily stressors. Third, we examined the role of social support in the processes underlying the effects of trauma and daily stressors on adolescent mental health problems. We hypothesized that perceived social support from family and friends would be directly associated with lower PTSS and EBP and less impairment. We also expected that social support would buffer the effects of cumulative trauma exposure and daily stressors on these mental health outcomes. Additionally, building on the conceptual model that conceives the total negative effect of trauma on mental health problems as having indirect as well as direct components, we hypothesized that the indirect pathways might also be moderated by social support: Trauma would thus be less strongly associated with subsequent daily stressors when adolescents feel supported by family and friends, and the association between current daily stressors and symptoms might also be attenuated. Finally, we focused on the stability of daily stressors and their associations with psychopathology over time. We compared checklist scores available for a subset of participants at both baseline (T1) and at a follow‐up assessment 16 months later (T2). These prospective data also provided the opportunity to test the association between daily stressors and mental health problems at T2 while controlling for problems at T1, to strengthen support for causal interpretations.
Method
Participants and Procedure
Participants were 753 Sinhalese‐speaking adolescents attending secondary school in Sri Lanka. Data for the main study (T1) were collected between January and March 2008 in Galle District, a region in which 4,000 people were killed and 35,000 displaced by the December 2004 tsunami. We selected two semiurban study locations with different degrees of tsunami impact: Hikkaduwa area, in the severely affected coastal belt; and Bope‐Poddala area, 6 km inland from the coast, with less tsunami impact. According to government assessments, 9 of the 40 secondary schools in Hikkaduwa but none of the 18 schools in Bope‐Poddala were directly affected by the tsunami. We chose five schools from each of the two areas such that participating schools in each area represented the three categories of secondary education in Sri Lanka. The study was approved by the ethics committee of the Faculty of Medicine, University of Ruhuna, and the school principals. All children in Grades 8 and 10 were informed about the study a few days prior to data collection; informed consent was obtained from more than 99% of the eligible adolescents and their parents. On the day of the study, fewer than 5% of the participants were absent; the remaining participants completed questionnaires in a separate classroom with the help of Sinhalese research assistants as needed.
The follow‐up study took place 16 months later, in July 2009 (T2), with the main goal of investigating cortisol secretion in relation to trauma and PTSS. The sample was drawn from 5 of the original 11 schools—3 in the high‐impact and 2 in the low‐impact tsunami locations. Based on T1 trauma and psychological symptoms, 286 adolescents were identified as belonging to one of the following three groups: trauma‐exposed meeting criteria for full or partial PTSD (n = 63), trauma‐exposed with no clinically significant PTSS or EBP (n = 61), and trauma‐free with no significant mental health symptoms (n = 162). From each school, 20 adolescents were invited to participate in the T2 follow‐up study, with care taken that all three groups were represented within a school and had similar age and gender distributions.
The T1 sample comprised 753 adolescents (53.9% girls), aged 12–16 years (M = 13.60 years, SD = 1.11). The T2 follow‐up sample included 89 participants (57.3% girls), aged 13–18 years (M = 14.39 years, SD = 1.10). Compared to the nonselected group (n = 664), the T2 subsample at T1 was slightly younger (13.25 vs. 13.69 years, respectively), t(751) = 3.52, p < .001, and had less severe emotional and behavioral problems (mean scores on the Strengths and Difficulties Questionnaire [SDQ] Total Problems scale of 8.91 vs. 10.24, respectively), t(127) = 2.68, p = .008. The groups did not differ significantly on gender, total trauma, daily stressors, PTSS, impairment, or social support.
Measures
All questionnaires were administered in Sinhalese, the local language. The two instruments) not already available in Sinhalese (i.e., measures of daily stressors and social support) were translated and back‐translated according to standard procedure and pretested in a separate group of adolescents. With the exception of the daily stressors checklist, all measures have been validated in adolescents in a range of Western and non‐Western populations.
Daily stressors
We used the Long‐Term Difficulties Questionnaire for Youth (LDQ‐Y), which we adapted from the 17‐item version (van Eck et al., 1998) of the original adult LDQ (Hendriks, Ormel, & van de Willige, 1990). The LDQ is a self‐report checklist that measures the rated severity of recent stressors in domains including work, school, finances, housing, health, social issues, and relationships with family and friends. Psychometric analyses indicated satisfactory convergence between stressor assessment via this questionnaire and semistructured interview (Hendriks et al., 1990). To date, neither the original LDQ nor its derivatives have been used to measure stressors in youth. Therefore, we first removed items deemed inappropriate for young adolescents (e.g., difficulties with work, own children, or sexual or marital relations); the 8 retained items concerned problems with school, financial situation, living situation in the neighborhood, leisure activities, peer relations, family relations, relations with other people, and health. A new item assessed worries about family members (e.g., chronic illness of parent). Adolescents rated difficulties they had experienced in each domain during the last 4 weeks on a scale ranging from 0 (no difficulties) to 3 (severe difficulties). The nine responses were summed as an index of cumulative daily stress. Although there is no a priori reason why stressors in one domain should be correlated with stressors in another domain, the LTD‐Y scale showed good reliability, Cronbach's α = .79. For each domain with a score greater than 0, respondents were asked to write a brief description of the stressor on blank lines provided for this purpose.
Traumatic events
We used the adolescent form of the UCLA PTSD Reaction Index for DSM‐IV (PTSD‐RI; Sinhalese version provided by Dr. F. Neuner) to assess lifetime exposure to 13 categories of potentially traumatic events (Steinberg, Brymer, Decker, & Pynoos, 2004). We replaced the original category “being in an earthquake that badly damaged the building you were in” with “being in the tsunami.” A cumulative trauma score was calculated as the number of different event types endorsed.
Posttraumatic stress symptoms
In participants reporting any trauma, the PTSD‐RI was also used to assess PTSD symptoms and diagnostic criteria (Steinberg et al., 2004). Of the 22 symptoms listed on the PTSD‐RI, 20 are associated with DSM‐IV‐TR clusters B (reexperiencing), C (avoidance), or D (arousal). Participants rated symptom frequency in the past month on 4‐point scales ranging from 0 (never) to 4 (most of the time). Scores on the 20 relevant items were summed as an index of PTSS. The reliability of this scale from the PTSD‐RI was high (Cronbach's α = .89). Individuals categorized as having full PTSD met DSM‐IV criteria for all three symptom clusters; those with partial PTSD met criteria for two of the three clusters. The PTSD‐RI has been validated and has shown good psychometric properties in previous studies of Sri Lankan adolescents (Neuner, Schauer, Catani, Ruf, & Elbert, 2006).
Emotional and behavioral problems
We used the Sinhalese self‐report version (Youthinmind Ltd., n.d.) of the extended SDQ (Goodman, 2001) for adolescents aged 11–17 years, validated in Sri Lanka (Perera, 2004). The SDQ has five subscales, each containing five items rated from 0 (not true) to 2 (certainly true). The summed ratings for the Emotional Problems, Conduct Problems, Hyperactivity, and Peer Problems subscales form the SDQ Total Problems scale (Cronbach's α = .76). Total scores of 15 or less are categorized as normal, 16–19 as borderline, and 20 or above as abnormal (Youthinmind Ltd., n.d.).
Daily impairment
The 5‐item SDQ Impact Supplement asks participants to rate, on a scale of 0 (not at all or only a little) to 2 (a great deal), how much their emotional and/or behavioral problems cause distress and interfere with four aspects of daily functioning: home life, friendships, classroom learning, and leisure activities. Responses are summed as an index of functional impairment. The reliability of this scale was high (Cronbach's α = .73). Total scores of 0 are categorized as normal, 1 as borderline, and 2 or more as abnormal (Youthinmind Ltd., n.d.).
Social support
The Multidimensional Scale of Perceived Social Support (MSPS; Zimet, Dahlem, Zimet, & Farley, 1988) measures perceived support from friends, family, and a significant other (“special person”). Scores for each four‐item subscale are calculated from ratings on 7‐point scales (1 = strongly disagree to 7 = strongly agree). This scale has been validated and has shown good psychometric properties in diverse ethnocultural contexts, although the factor structure may vary (Wilson, Yendork, & Somhlaba, 2017). As adolescents in our sample found it difficult to identify a “special person,” we used the sum of the eight items in the Family and Friends subscales in our analyses. This scale demonstrated good reliability (Cronbach's α = .78). The mean item score (5.09) was similar to that reported in previous studies.
Data Analysis
We completed analyses using SPSS (Version 24) with two‐tailed p values < .05 considered significant. Two participants from the baseline study and one participant from the follow‐up study were excluded because they did not complete the daily stressors scale. Missing values (3.5% of the SDQ items, 3.4% of the PTSS items, and 1.2% of the social support items at T1) were imputed with the SPSS multiple imputation procedure before scale scores were calculated.
To address hypotheses concerning the relative contributions of trauma and daily stressors to mental health problems, we first conducted three separate hierarchical regression analyses, taking PTSS, EBP, and daily impairment scores as dependent variables. Age, gender (0 = male, 1 = female), and an Age × Gender interaction were entered as covariates in the first step. The model for impaired daily functioning also controlled for EBP. Total trauma exposure and daily stressors were entered in subsequent steps. Next, to investigate indirect effects of trauma via daily stressors, we used the SPSS macro PROCESS (Version 2.16.3) with bias‐corrected bootstrap 95% confidence intervals (5,000 samples; Hayes, 2013a). Previous studies have characterized the indirect effect as a percentage of the total effect. This effect size measure (PM) has shortcomings but performs adequately when sample size is at least 500 and the total effect is larger than and in the same direction as the indirect effect (Hayes, 2013b), as was true in our case. As each mental health outcome had a different scale and distribution, we also present partially standardized indirect effects (with effects expressed relative to the standard deviation of the dependent variable) to aid model comparison. Finally, we repeated these analyses with outcome and mediator variables reversed to explore the possibility that mental health problems induced daily stressors rather than vice versa.
To examine main and buffering effects of social support on symptom measures, we repeated the hierarchical regression analyses, adding social support, Social Support × Trauma, and Social Support × Daily Stressor interactions as independent variables. We then tested whether indirect paths linking trauma to mental health outcomes (path a from trauma to daily stressors or path b from daily stressors to symptoms; PROCESS Models 7 and 14, respectively) were moderated by social support. The PROCESS macro generates an “index of moderated mediation” and a bootstrap confidence interval to infer whether the indirect effect of X on Y through mediator M is significantly moderated by another variable (for details, see Hayes, 2013a, 2013b, and 2015).
To explore the causal association between stressors and EBP, we performed multiple regression with (a) T2 EBP as the dependent variable and daily stressors at T1 and T2 as independent variables, controlling for T1 EBP, and (b) T2 stressors as the dependent variable and T1 EBP as independent variable, controlling for T1 daily stressors. Because initial models showed no significant effects of age, gender, or Age × Gender interactions on T2 outcome measures, these variables were excluded.
Results
Lifetime Trauma
A majority (60.3%) of the participants had been exposed to at least one category of traumatic event; 41.4% of participants reported multiple traumatic experiences, with a mean of 1.79 (SD = 1.98) different event types (range: 0–10). In most cases, the worst event had occurred relatively recently, with 73.1% reporting occurrence in the past 3 years and only 1.0% reporting occurrence in the interval 5–12 years prior to the study. Boys reported significantly more total trauma types than girls (M = 1.86 vs. M = 1.54, respectively), t(751) = 2.27, p = .023. Cumulative trauma score was unrelated to age, r(753) = −.02, p = .532. Figure 1 shows the reported frequency of different categories of events among the trauma‐exposed subset. Reflecting the sampling framework, the tsunami was the most common event, reported by 19.0% of all participants. In the directly affected area compared to the less‐affected area, adolescents were more likely to report tsunami exposure (43.8% vs. 7.9%, respectively), X 2 (2, N = 753) = 122.17, p < .001, and had higher total trauma scores (2.14 vs. 1.17 different event categories, respectively), t(751) = 6.92 , p < .001.
Figure 1.
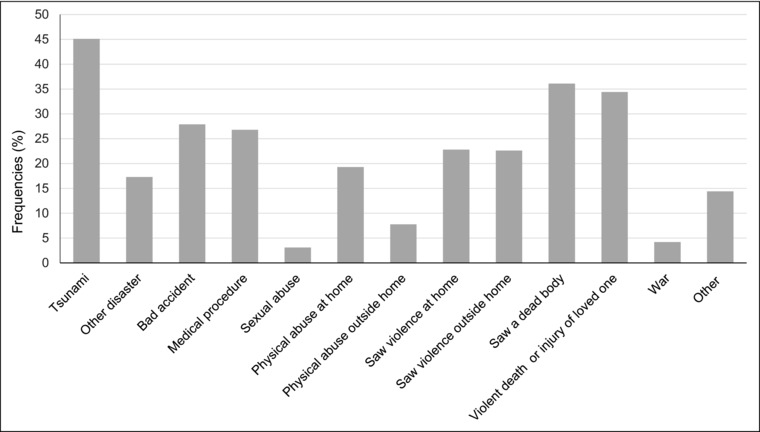
Percentage of trauma‐exposed participants (n = 451) who reported each category of traumatic event.
Daily Stressors
Of the total sample, 474 adolescents (62.9%) reported having experienced difficulties during the last 4 weeks in at least one of the nine domains; 466 participants provided short descriptions in addition to severity ratings. Table 1 shows frequencies, severity ratings, and examples of daily stressors as described for each domain. The most frequently reported daily stressors were financial problems, health problems, and problems in peer relations. Total LDQ‐Y scores ranged from 0 to 24.
Table 1.
Frequency and Severity of Daily Stressors During the Past Month
| % Reporting | Severity | ||||
|---|---|---|---|---|---|
| Stressor domain | Any Problem | Severe Problem | Mean | SD | Examples of Stressors Rated as Severe |
| Financial | 29.8 | 4.5 | 0.48 | 0.82 | Parents have debts, father is unemployed, house was robbed |
| Health | 23.3 | 3.1 | 0.34 | 0.71 | Headache, abdominal pain, asthma, always falling, got pregnant |
| Interactions with friends | 18.8 | 2.4 | 0.29 | 0.67 | Get angry very quickly, misunderstanding with friend |
| School | 17.6 | 2.1 | 0.27 | 0.66 | Learning difficulties, punished by teachers |
| Contacts with others | 15.6 | 2.0 | 0.23 | 0.59 | Others not very nice to me; if I talk with boys, others misunderstand |
| Free time activities | 15.2 | 1.5 | 0.21 | 0.57 | No money to buy cricket bat, can't play because homework isn't done |
| In the neighborhood | 14.8 | 2.4 | 0.24 | 0.65 | Fighting with the neighbor, neighbors’ loud music disturbs us |
| Worries about family | 13.9 | 2.8 | 0.23 | 0.64 | Father's alcoholism, brother is disobedient, father left mother |
| Family interactions | 7.6 | 1.0 | 0.11 | 0.44 | Parents fight, fights with siblings, family members scold and hit me |
Note. Adolescents rated recent difficulties on a scale from 0 = no difficulties to 3 = severe difficulties.
Categorization of Mental Health Problems
Diagnostic and Statistical Manual of Mental Diseases (4th ed.; DSM‐IV) criteria for full or partial PTSD, as determined following PTSD‐RI algorithms (Steinberg et al. 2004), were met by 106 adolescents (14.0% of the total sample; 23.5% of the trauma‐exposed subsample), of whom 36 (4.8%) met criteria for full PTSD and 70 (9.3%) for partial PTSD. Based on SDQ cutoffs, levels of EBP were abnormal in 37 (4.9%) of the 753 participants and borderline in 64 (8.5%).
Daily Stressors as Predictors of Mental Health Problems and Daily Impairment
As expected, daily stressors were positively correlated with total trauma exposure, PTSS, EBP, and impairment, and negatively correlated with social support (see Table 2). Results of hierarchical linear regression models are summarized in Table 3. Demographic variables age and gender had small but significant main or interaction effects for all outcomes and were thus retained in subsequent models. As expected, EBP significantly predicted greater daily impairment and was therefore retained as a possible confounder in models of this outcome variable. At Step 2, total trauma was positively associated with all dependent measures. Daily stressors, added at Step 3, were independently associated with more severe symptoms and impairment, reducing the predictive strength of prior trauma. This was true for all three outcomes; in the case of impairment, trauma exposure was no longer a significant predictor in this final step.
Table 2.
Descriptive Statistics and Intercorrelations for Key Variables
| Pearson Correlation (r) | ||||||
|---|---|---|---|---|---|---|
| Variables | 1. | 2. | 3. | 4. | 5. | 6. |
| 1. Daily stressors | – | .40 | .43 | .35 | .44 | −.28 |
| 2. Cumulative trauma | – | .39 | .27 | .24 | −.13 | |
| 3. PTSS | – | .35 | .33 | −.22 | ||
| 4. EBP | – | .30 | −.32 | |||
| 5. Daily impairment | – | −.28 | ||||
| 6. Social support | – | |||||
| n | 753 | 753 | 451 | 753 | 753 | 753 |
| M | 2.41 | 1.69 | 17.13 | 10.08 | 0.46 | 40.69 |
| SD | 3.40 | 1.98 | 12.81 | 5.15 | 1.31 | 7.00 |
Table 3.
Hierarchical Regression Estimates of Effects of Trauma Exposure and Daily Stressors on Current Symptoms and Daily Impairment
| Outcome Variable | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| PTSS | EBP | Daily Impairment | |||||||
| Predictora | B | SE Β | β | B | SE Β | β | B | SE Β | β |
| Step 1b | |||||||||
| Age | −1.63 | 0.80 | −0.14* | −1.17 | 0.24 | −0.26*** | −0.07 | 0.06 | −0.06 |
| Gender | −29.07 | 14.79 | −1.13* | −16.13 | 4.51 | −1.56*** | −2.88 | 1.12 | −1.10** |
| Gender × Age | 2.34 | 1.08 | 1.26* | 1.14 | 0.33 | 1.51*** | 0.20 | 0.08 | 1.06* |
| EBP | 0.07 | 0.01 | 0.29*** | ||||||
| Step 2c | |||||||||
| Total trauma | 2.84 | 0.30 | 0.41*** | 0.66 | 0.09 | 0.26*** | 0.10 | 0.02 | 0.16*** |
| Step 3d | |||||||||
| Total trauma | 2.10 | 0.30 | 0.30*** | 0.38 | 0.10 | 0.15*** | 0.03 | 0.02 | 0.04 |
| Daily stressors | 1.07 | 0.14 | 0.33*** | 0.42 | 0.06 | 0.28*** | 0.14 | 0.01 | 0.36*** |
| Model summary | R2 = .28, F(5, 445) = 34.22*** | R2 = .16, F(5, 747) = 28.93*** | R2 = .22, F(6, 746) = 35.59*** | ||||||
Note. PTSS = posttraumatic stress symptoms; EBP = emotional and behavioral problems; gender coded female = 1.
aControl variables from Step 1 were retained in subsequent steps (not shown in table). bChanges in explained variance: ∆R 2 PTSS = .02*, ∆R 2 EBP = .03***, ∆R 2 impairment = .10***. cChanges in explained variance: ∆R 2 PTSS = .16***, ∆R2 EBP = .06***, ∆R 2 impairment =.02***. dChanges in explained variance: ∆R 2 PTSS = .09***, ∆R 2 EBP = .07***, ∆R 2 impairment = .10***.
* p < .05, ** p < .01, *** p < .001
We next tested the extent to which daily stressors indirectly transmitted the effects of trauma on PTSS, EBP, and impaired daily functioning. Figure 2 depicts unstandardized coefficients obtained for direct and indirect pathways linking trauma to each of the three outcome variables (Models i, ii, and iii). As before, greater trauma exposure was associated with more severe symptoms (total effect, Path c). Cumulative trauma exposure was also associated with higher levels of current daily stress (Path a), and daily stressors were in turn associated with mental health problems (Path b). For PTSS (Model i), 24.3% of the total effect of trauma was indirect, through daily stressors (Path c ‐ c’), partially standardized indirect effect abps = 0.055, 95% CI [0.034, 0.082], model R 2 = .278, F(5, 445) = 34.22, p < .001. For EBP (Model ii), 42.8% of the total effect of trauma was indirectly transmitted via daily stressors, abps = 0.059, 95% CI [0.039, 0.082], R 2 = .162, F(5, 747) = 28.43, p < .001. In contrast, the pathway from trauma exposure to impaired daily functioning (Model iii) was predominantly indirect, representing 73.6% of the total effect, abps = 0.064, 95% CI [0.040, 0.091]), R 2 = .223, F(6, 746) = 35.59, p < .001. Here, the direct effect of trauma c' was not statistically significant, p = .227. Taken together, these results support the hypothesis that daily stressors were involved in indirect pathways linking trauma exposure to psychopathology, with effect sizes dependent on the specific mental health outcome.
Figure 2.
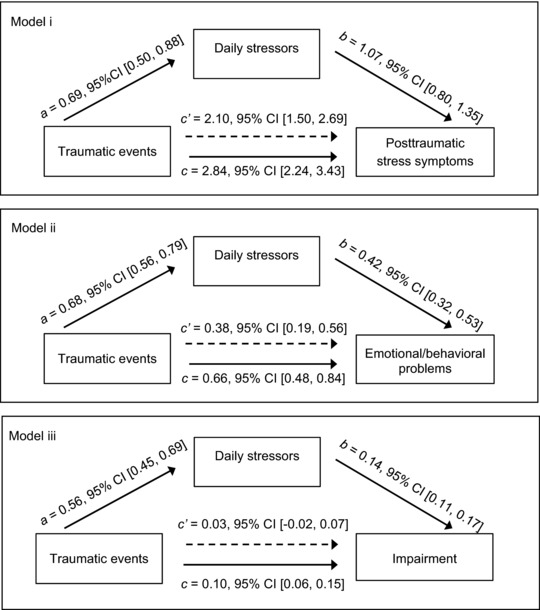
Unstandardized path coefficients for models in which daily stressors were hypothesized to transmit indirect effects of cumulative trauma on mental health outcomes. Models i, ii, and iii controlled for age, gender, and age by gender interaction; Model iii also controlled for EBP score. Coefficient a represents the effect of trauma on daily stressors, b is the effect of daily stressors on a given mental health outcome, c represents the total effect of prior trauma, c’ is the direct effect of trauma after controlling for daily stressors. Indirect effect (via daily stressors) = c ‐ c' = ab
These findings do not rule out the alternative explanation that adolescents with mental health problems generated more daily stressors or appraised their environment as more difficult or threatening. Trauma would then lead not only directly to more daily stressors, but also indirectly, via psychopathology. Results of additional analyses also lent some support to this model. With PTSS as putative mediator, 46.2% of the total effect of trauma on stressors was indirect, unstandardized indirect effect ab = 0.307, SE = 0.072, 95% CI [0.187, 0.475], abps = 0.079. It appeared that EBP played a smaller indirect role in transmitting the effect of trauma exposure on stressors, accounting for 16.6% of the total effect of trauma, ab = 0.116, SE = 0.027, 95% CI [0.072, 0.179], abps = 0.035. Similarly, the pathway from trauma to daily stressors via impairment was predominantly direct, with only 15.0% of the total effect indirect, ab = 0.087, SE = 0.037, 95% CI [0.030, 0.178], abps = 0.028. For EBP and impairment, comparison of partially standardized indirect effects for alternative models also yielded stronger support for a causal pathway from daily stressors to mental health outcomes than vice versa, whereas for PTSS, the primary causal relationship appeared to be reversed. Although mediation cannot be established in these cross‐sectional data, the patterns suggest that pathways between daily stressors and mental health problems are likely bidirectional, with their relative strength depending on the specific symptoms.
The Role of Social Support
We extended the hierarchical regression models presented in Table 3 to investigate whether social support reduced the negative impact of trauma and daily stressors directly or by buffering their effects. As shown in Table 4 (main effects model), a higher level of social support was associated with better mental health outcomes even after controlling for total trauma and daily stressors; the addition of social support as a predictor resulted in a significant increase in explained variance R 2, particularly for EBP and impairment (see Table 4 footnote). In a final step (Table 4, moderation model), results indicated that social support buffered effects of trauma and daily stressors on daily impairment but not on PTSS or EBP.
Table 4.
Hierarchical Regression Estimates of Effects of Social Support on Current Symptoms and Daily Impairment
| Dependent Variable | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| PTSS | EBP | Daily Impairment | |||||||
| Model | B | SE Β | β | B | SE Β | β | B | SE Β | β |
| Main effects modela | |||||||||
| Social support | −0.16 | 0.08 | −0.09* | −0.18 | 0.03 | −0.24*** | −0.03 | 0.01 | −0.14*** |
| Total trauma | 2.06 | 0.30 | 0.29*** | 0.37 | 0.09 | 0.14*** | 0.03 | 0.02 | 0.04 |
| Daily stressors | 0.10 | 0.15 | 0.30*** | 0.32 | 0.06 | 0.21*** | 0.13 | 0.01 | 0.33*** |
| Model summary | R2 = .29, F(6, 444) = 29.43*** | R2 = .21, F(6, 746) = 33.87*** | R2 = .24, F(7, 745) = 33.35*** | ||||||
| Moderation modelb | |||||||||
| SS × Trauma | 0.01 | 0.04 | 0.03 | 0.01 | 0.01 | 0.12 | −0.01 | 0.00 | −0.48** |
| SS × Stressors | −0.01 | 0.02 | −0.14 | 0.00 | 0.01 | 0.03 | −0.01 | 0.00 | −0.62*** |
| Model summary | R2 = .29, F(8, 442) = 22.05*** | R2 = .22, F(8, 744) = 25.43*** | R2 = .28, F(9, 743) = 31.25*** | ||||||
Note. PTSS = posttraumatic stress symptoms; EBP = emotional and behavioral problems; SS = social support. All models controlled in Step 1 for age, gender, and age by gender interaction; models for daily impairment also controlled for EBP. In Steps 2 and 3, independent variables total trauma and daily stressors were added, respectively (see Table 3 for results of these previous models). aChanges in explained variance after addition of SS and interaction variables: ∆R 2 PTSS = .01*, ∆R 2 EBP = .05***, ∆R 2 impairment = .02***. bChanges in explained variance after addition of SS and interaction variables: ∆R 2 PTSS = .00, ∆R 2 EBP = .00, ∆R 2 impairment = .04***.
* p < .05. ** p < .01. *** p < .001.
Next, we tested whether social support moderated the indirect pathways between trauma exposure and mental health outcomes. Results of models in which social support moderated path a, from trauma to daily stressors (PROCESS Model 7), depended again on the outcome measure. For PTSS and EBP, the obtained index of moderated mediation (IMM) was nonsignificant, IMMPTSS = −0.028, 95% CI [−0.064, 0.008] and IMMEBP = −0.008, 95% CI [−0.192, 0.001]; for impairment, however, the indirect effect of trauma via daily stressors was weaker when perceived social support was high, IMMimpairment = −0.003, 95% CI [−0.002, −0.000]. Thus, at high levels of social support (1 standard deviation above the mean), 10.0% of the total effect of trauma on daily impairment was indirect compared to 17.8% at low levels (1 standard deviation below the mean). Similarly, models in which social support moderated Path b, from daily stressors to mental health outcomes (PROCESS Model 14), yielded nonsignificant results for PTSS and EBP outcomes. Only in the case of daily impairment was there evidence that a low to average level of social support not only influenced Path a, from trauma to stressors, but also attenuated the association between stressors and outcome (Path b), IMM = −0.005, 95% CI [−0.010, −0.001].
Prospective Follow‐Up Findings
In the follow‐up sample of 89 adolescents, 55.1% reported daily stressors, with an average of 1.37 (SD = 1.81; range: 0–8) stressor domains per participant. The three most common daily stressors were the same as those reported at baseline: financial problems (29.2%), health problems (22.6%), and problems in relations with friends (19.1%). Total daily stressor scores at the two time points were positively correlated, r(89) = .44, p < .001, and showed no significant change over the 16‐month interval (M T1 = 1.90, SD = 2.89 and M T2 = 1.87, SD = 2.54), t(88) = 0.11, p = .913.
Results after controlling for EBP at T1, β = .19, p = .059, indicated that T2 daily stressors predicted concurrent symptoms, β = .36, p < .001. This model explained 19.9% of the variance in T2 EBP, F(2, 86) = 10.70, p < .001. Prior daily stressors at T1, in contrast, did not significantly predict T2 symptoms, β = 0.16, p = .131, nor did their addition as predictor increase explained variance compared to the previous model, ΔF(1, 85) = 0.01. Results are consistent with a causal interpretation in which recent but not past daily stressors exacerbate symptoms. We repeated the regression analysis to explore whether preexisting EBP at T1 contributed to an increase in daily stressors from T1 to T2 as would be expected if EBP generated chronic stressors. Although EBP at T1 was significantly correlated with T2 daily stressors, r(89) = .23, p = .034, this association became nonsignificant after controlling for T1 daily stressors, β = 0.16, p = .119.
Discussion
This study examined traumatic events and daily stressors and their implications for mental health and daily functioning in Sri Lankan adolescents. Our first goal was to obtain quantitative and qualitative information about daily stressors. At both baseline and follow‐up, the majority of participants reported stressors in one or more daily life domains. Participants endorsed the financial problems domain most frequently, and this source of stress also appeared to carry over into other domains. The pervasive influence of poverty was reflected, for example, in descriptions of stressors related to school (“not enough money to buy school supplies”) and leisure activities (“can't play cricket with friends because there is no money to buy a bat”). Some respondents mentioned financial problems as a cause of worries about and tension among family members, negatively influencing these relationships. Stress associated with low socioeconomic status increases the risk of developing mental health problems (Johnson, Cohen, Dohrenwend, Link, & Brook, 1999). War and disasters, with associated material loss, displacement, and economic collapse, further increase children's vulnerability to mental health problems. Studies of children exposed to tsunamis or war provide evidence that these traumas increased economic stressors, such as unemployment and lack of basic necessities, in youth (Fernando et al., 2010; Newnham et al., 2015). Addressing poverty and thus reducing the burden of daily stressors can thereby alleviate mental health problems; a program offering business skills training, subsidies, and follow‐up support to former female child soldiers exemplifies this approach (Annan, Green, & Brier, 2013).
With regard to our approach to measuring daily stressors, we note both strengths and limitations. One advantage of the LTD‐Y is its compact checklist format; such instruments are generally easy to understand and simple to administer in large samples (Compas, Davis, Forsythe, & Wagner, 1987). Despite its brevity, the LTD‐Y provides qualitative descriptions as well as quantitative information. Its focus on common, generic categories of stressors makes the LTD‐Y suitable for use in diverse populations, thus facilitating comparisons across studies and improving the generalizability of findings, in contrast to more context‐specific checklists. As examples of tailored scales, the Post‐War Adversities Index was adapted to measure postwar stressors in Sierra Leonean youth (Newnham et al., 2015) whereas the Children's Daily Stressor Scale, with content developed in focus groups, identified stressors in postwar and post‐tsunami contexts in Sri Lanka (Miller et al., 2009). The latter scale found “snakes in house or environment” to be the most frequently endorsed stressor of 29 possibilities—an unimaginable situation for Western adolescents. Among general instruments, on the other hand, research has been hampered by the lack of a standardized taxonomy of stressors for youth (Grant et al., 2004). Depending on study goals, there may be a trade‐off between sociocultural specificity and generalizability of results across settings. Miller and Rasmussen (2010) argued that daily adversity measures that differentiate ongoing traumas from minor stressors are needed; this would seem essential for research on the relative contributions both make to psychopathology. Thus, another strength of the LTD‐Y is its deliberate focus on recently occurring, mild‐to‐moderate daily stressors, uncontaminated by life events. Although the format does not preclude that respondents will report recent traumatic events in addition to daily hassles, the 4‐week time frame limits the probability of this. In contrast, other stressor scales measure adversities ranging from minor daily hassles to traumatic experiences; retrospective time frames vary from weeks to lifetime. As a weakness of the LTD‐Y, we have noted that the stressor categories were, in practice, not mutually exclusive; thus, problems related to poverty were reported not only under the financial problems domain but also in other domains. Another limitation—shared with other daily hassles checklists—is the inability to differentiate dependent from independent stressors, which potentially clouds the distinction between stressors and psychopathology (Grant et al., 2004). For example, the adolescent who described his recent difficulties with peers as “I get angry very quickly” is likely to generate new daily stressors, perhaps in other domains as well. Based on participants' brief written descriptions, the majority of daily stressors appeared to be independent, fitting the definition “environmental events or chronic conditions that objectively threaten the physical and/or psychological wellbeing of individuals...” (Grant et al., 2004, p. 413), but we had insufficient information to filter out exceptions. Lastly, while comparisons with interview data (the gold standard) support the validity of the LTD in adults, no comparable information is available for adolescents; moreover, the LTD‐Y has not been validated in the Sinhalese language. This means that results should be interpreted with caution, pending replication with validated measures of daily stressors.
Our second goal was to clarify the role of daily stressors in relation to posttrauma mental health problems and impaired daily functioning. Results were consistent with our hypotheses: Adolescents with a history of traumatic events experienced more daily stressors, and stressors were associated with more severe symptoms and impairment. Although there were significant indirect pathways from trauma via daily stressors to all three mental health outcomes, both the total effect of trauma and the relative roles of trauma versus current stress varied. Thus, in predicting PTSS, cumulative trauma had a relatively large direct effect, with daily stressors transmitting only one‐quarter of the total effect. In contrast, daily stressors were not only better predictors of EBP than prior trauma, but close to half of the total effect of trauma was transmitted via stressors. For impaired functioning, daily stressors appeared to play an even larger role, with three‐quarters of the total effect of trauma transmitted through stressors. By examining the role of daily stressors with respect to three different mental health outcomes, the current study extended knowledge about the types of problems that might be reduced by addressing such stressors in posttrauma settings. Although previous research has called attention to the importance of daily stressors in maintaining PTSS, depression, and anxiety (Fernando et al., 2010; Newnham et al., 2015), the current findings suggest that interventions aimed at reducing daily stressors (or enhancing ways of coping with them) would have an even larger positive impact on daily functioning than on symptoms alone. The burden of impairment in youth is great: In the initial psychometric study, high SDQ impact scores (top 10%) were associated with a substantial increase in prevalence of DSM‐IV disorders (odds ratio [OR] = 9.5 compared to OR = 6.6 for high EBP scores; Goodman, 2001). However, some caution is warranted in generalizing our results. Compared to studies conducted in Sri Lanka shortly after the tsunami (Agampodi et al., 2011; Neuner et al., 2006), we observed fewer participants with clinically significant symptoms (PTSS or EBP), most likely reflecting lower cumulative trauma levels as well as differences in sociodemographic characteristics. Because different instruments were used to assess key variables, direct comparisons with other Sri Lankan studies (e.g., Fernando et al., 2010) are not possible.
The pitfalls of mediation analyses with cross‐sectional data are well known (Fairchild & McDaniel, 2017), and they limit the conclusions that can be drawn about indirect effects. To support a causal interpretation, the temporal order of the variables must be clear. The hypothesis that daily stressors mediate the association between lifetime trauma and current psychopathology thus rests on the assumption that trauma preceded daily stressors as well as symptoms, which seems reasonable in our case. Defending the assumption that daily stressors precede symptoms or, more specifically, cause symptoms to increase, is less straightforward. On theoretical grounds, the temporal association between the two variables is posited to be close, with proximal stressors having more impact than distal ones. If so, even longitudinal studies may be inadequate to clarify exactly how and when daily stressors exert their influence on mental health. Acknowledging these problems, we conducted new analyses to explore the alternative hypothesis that recent symptoms may have induced stressors. Results from the large initial sample, although still correlational, point to stronger indirect processes in the trauma to symptoms via stressors model than in the alternative trauma to daily stressors via symptoms model. Some bidirectionality of the path linking stressors and symptoms did appear likely, but true mediation effects can only be teased apart longitudinally. The prospective data we collected showed that frequency, types, and severity of daily stressors were relatively stable during midadolescence in this sample. Although limited by a smaller sample, analyses confirmed that the association between stressors and EBP at T2 was not attributable to prior mental health problems. Admittedly, this falls short of proving that changes in symptoms over time were due to daily stressors. Progress in this area may depend not only on well‐designed prospective studies but also on the development of daily stressor measures with better temporal differentiation.
Results confirmed the protective role of social support in adolescent mental health outcomes. As expected, perceived social support was directly associated with lower PTSS, EBP, and daily impairment. With respect to the buffering hypothesis, however, only in the case of impairment did social support significantly modulate the direct effects of past trauma or current stress. Partly in line with our conceptual model, support from family and friends appeared to weaken the links between trauma and daily stressors as well as between stressors and symptoms; again, however, only in the case of impairment as an outcome. Although the MSPSS has been validated as a measure of social support in diverse languages and cultures, we note as a limitation that this scale has not been validated in the Sinhalese language. Although the role of social support in buffering the effects of trauma on children and adolescents remains underexplored, such knowledge can have important implications. Traumatic events that affect whole families and communities cause particularly large disruptions of social networks, underscoring the need for such interventions and effective ways to implement them.
As summarized in a recent review by Miller and Jordans (2016), progress has been made in translating research on daily stressors into practical interventions. Youth experience harsh discipline by parents and teachers and violence observed at home as highly stressful, and these all‐too‐frequent behaviors are even more common in traumatized families and communities. Going beyond traditional child‐focused interventions, programs addressing threats in children's everyday environments may, in addition to reducing family‐ and school‐related stressors, help increase perceived social support from parents and teachers.
In conclusion, daily stressors appeared to be an important transmitter of the impact of trauma on adolescents’ mental health problems. That social support moderated direct and indirect pathways from trauma to daily impairment is a novel finding that warrants further investigation. Although longitudinal studies are needed in order to develop evidence‐based interventions that address both indirect and direct pathways to various mental health outcomes following trauma, the current results reinforce the argument that research and interventions for trauma victims should focus on ongoing stressors as well as the total burden of trauma, also taking protective factors into account. In this regard, future studies would do well to consider a broader range of potential moderators or mediators, including quality of parenting, socioeconomic status, coping skills, and personality (Grant et al., 2004). Because proximal environmental circumstances not only have a strong impact on mental health following trauma but may also be modifiable, targeted interventions may play a vital role in recovery.
This research was supported in part by a grant from Cordaid, the Netherlands, to N. A. Nicolson.
References
- Agampodi, T. C. , Agampodi, S. B. , & Fonseka, P. (2011). Prevalence of mental health problems in adolescent schoolchildren in Galle District, Sri Lanka: Eight months after tsunami. Asia‐Pacific Journal of Public Health, 23, 588–600. 10.1177/1010539509349866 [DOI] [PubMed] [Google Scholar]
- Amone‐P'Olak, K. , Stochl, J. , Ovuga, E. , Abbott, R. , Meiser‐Stedman, R. , Croudace, T. J. , & Jones, P. B. (2014). Postwar environment and long‐term mental health problems in former child soldiers in Northern Uganda: The WAYS study. Journal of Epidemiology and Community Health, 68, 425–430. 10.1136/jech-2013-203042 [DOI] [PubMed] [Google Scholar]
- Annan, J. , Green, E. P. , & Brier, M. (2013). Promoting recovery after war in Northern Uganda: Reducing daily stressors by alleviating poverty. Journal of Aggression, Maltreatment & Trauma, 22, 849–868. 10.1080/10926771.2013.823636 [DOI] [Google Scholar]
- Betancourt, T. S. , Newnham, E. A. , McBain, R. , & Brennan, R. T. (2013). Posttraumatic stress symptoms among former child soldiers in Sierra Leone: Follow‐up study. The British Journal of Psychiatry, 203, 196–202. 10.1192/bjp.bp.112.113514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogic, M. , Ajdukovic, D. , Bremner, S. , Franciskovic, T. , Galeazzi, G. M. , Kucukalic, A. , . . . Priebe, S. (2012). Factors associated with mental disorders in long‐settled war refugees: Refugees from the former Yugoslavia in Germany, Italy and the UK. The British Journal of Psychiatry, 200, 216–223. 10.1192/bjp.bp.110.084764 [DOI] [PubMed] [Google Scholar]
- Cerda, M. , Bordelois, P. M. , Galea, S. , Norris, F. , Tracy, M. , & Koenen, K. C. (2013). The course of posttraumatic stress symptoms and functional impairment following a disaster: What is the lasting influence of acute versus ongoing traumatic events and stressors? Social Psychiatry and Psychiatric Epidemiology, 48, 385–395. 10.1007/s00127-012-0560-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, S. , & Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98, 310–357. 10.1037/0033-2909.98.2.310 [DOI] [PubMed] [Google Scholar]
- Compas, B. E. , Davis, G. E. , Forsythe, C. J. , & Wagner, B. M. (1987). Assessment of major and daily stressful events during adolescence: The Adolescent Perceived Events Scale. Journal of Consulting and Clinical Psychology, 55, 534–541. 10.1037/0022-006X.55.4.534 [DOI] [PubMed] [Google Scholar]
- Fairchild, A. J. , & McDaniel, H. L. (2017). Best (but oft‐forgotten) practices: Mediation analysis. The American Journal of Clinical Nutrition, 105, 1259‐1271. 10.3945/ajcn.117.152546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernando, G. A. , Miller, K. E. , & Berger, D. E. (2010). Growing pains: The impact of disaster‐related and daily stressors on the psychological and psychosocial functioning of youth in Sri Lanka. Child Development, 81, 1192–1210. 10.1111/j.1467-8624.2010.01462.x [DOI] [PubMed] [Google Scholar]
- Goodman, R. (2001). Psychometric properties of the Strengths and Difficulties Questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 1337–1345. 10.1097/00004583-200111000-00015 [DOI] [PubMed] [Google Scholar]
- Grant, K. E. , Compas, B. E. , Thurm, A. E. , McMahon, S. D. , & Gipson, P. Y. (2004). Stressors and child and adolescent psychopathology: Measurement issues and prospective effects. Journal of Clinical Child and Adolescent Psychology, 33, 412–425. 10.1207/s15374424jccp3302_23 [DOI] [PubMed] [Google Scholar]
- Hayes, A. F. (2013a). The PROCESS macro for SPSS and SAS (Version 2.16.3). Retrieved from http://www.processmacro.org/
- Hayes, A. F. (2013b). Introduction to mediation, moderation, and conditional process analysis. New York, NY: The Guilford Press. [Google Scholar]
- Hayes, A. F. (2015). An index and test of linear moderated mediation. Multivariate Behavioral Research, 50, 1–22. 10.1080/00273171.2014.962683 [DOI] [PubMed] [Google Scholar]
- Hendriks, A. A. J. , Ormel, J. , & van de Willige, G. (1990). Langdurige moeilijkheden gemeten volgens zelfbeoordelingsvragenlijst en semi‐gestructureerd interview [Long‐term difficultuies as measured by self‐report questionnaire and semistructured interview]. Gedrag en Gezondheid, 18, 273–283. [Google Scholar]
- Johnson, J. G. , Cohen, P. , Dohrenwend, B. P. , Link, B. G. , & Brook, J. S. (1999). A longitudinal investigation of social causation and social selection processes involved in the association between socioeconomic status and psychiatric disorders. Journal of Abnormal Psychology, 108, 490–499. 10.1037/0021-843X.108.3.490 [DOI] [PubMed] [Google Scholar]
- Greca La, M. A., Silverman, W. K. , Lai, B. , & Jaccard, J. (2010). Hurricane‐related exposure experiences and stressors, other life events, and social support: Concurrent and prospective impact on children's persistent posttraumatic stress symptoms. Journal of Consulting and Clinical Psychology, 78, 794–805. 10.1037/a0020775 [DOI] [PubMed] [Google Scholar]
- Miller, K. E. , Fernando, G. A. , & Berger, D. E. (2009). Daily stressors in the lives of Sri Lankan youth: A mixed methods approach to assessment in a context of war and natural disaster. Intervention, 7, 187–203. 10.1097/WTF.0b013e3283346344 [DOI] [Google Scholar]
- Miller, K. E. , & Jordans, M. J. (2016). Determinants of children's mental health in war‐torn settings: Translating research into action. Current Psychiatry Reports, 18, 58 10.1007/s11920-016-0692-3 [DOI] [PubMed] [Google Scholar]
- Miller, K. E. , Omidian, P. , Rasmussen, A. , Yaqubi, A. , & Daudzai, H. (2008). Daily stressors, war experiences, and mental health in Afghanistan. Transcultural Psychiatry, 45, 611–638. 10.1177/1363461508100785 [DOI] [PubMed] [Google Scholar]
- Miller, K. E. , & Rasmussen, A. (2010). War exposure, daily stressors, and mental health in conflict and post‐conflict settings: Bridging the divide between trauma‐focused and psychosocial frameworks. Social Science & Medicine, 70, 7–16. 10.1016/j.socscimed.2009.09.029 [DOI] [PubMed] [Google Scholar]
- Neuner, F. , Schauer, E. , Catani, C. , Ruf, M. , & Elbert, T. (2006). Post‐tsunami stress: A study of posttraumatic stress disorder in children living in three severely affected regions in Sri Lanka. Journal of Traumatic Stress, 19, 339–347. 10.1002/jts.20121 [DOI] [PubMed] [Google Scholar]
- Newnham, E. A. , Pearson, R. M. , Stein, A. , & Betancourt, T. S. (2015). Youth mental health after civil war: The importance of daily stressors. The British Journal of Psychiatry, 206, 116–121. 10.1192/bjp.bp.114.146324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perera, H. (2009). Mental health of adolescent school children in Sri Lanka: A national survey. Sri Lanka Journal of Child Health, 33, 78–81. 10.4038/sljch.v33i3.642 [DOI] [Google Scholar]
- Rasmussen, A. , Nguyen, L. , Wilkinson, J. , Vundla, S. , Raghavan, S. , Miller, K. E. , & Keller, A. S. (2010). Rates and impact of trauma and current stressors among Darfuri refugees in Eastern Chad. American Journal of Orthopsychiatry, 80, 227–236. 10.1111/j.1939-0025.2010.01026.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg, A. M. , Brymer, M. J. , Decker, K. B. , & Pynoos, R. S. (2004). The University of California at Los Angeles Posttraumatic Stress Disorder Reaction Index. Current Psychiatry Reports, 6, 96–100. 10.1007/s11920-004-0048-2 [DOI] [PubMed] [Google Scholar]
- Trickey, D. , Siddaway, A. P. , Meiser‐Stedman, R. , Serpell, L. , & Field, A. P. (2012). A meta‐analysis of risk factors for post‐traumatic stress disorder in children and adolescents. Clinical Psychology Review, 32, 122–138. 10.1016/j.cpr.2011.12.001 [DOI] [PubMed] [Google Scholar]
- van Eck, M. , Nicolson, N. A. , & Berkhof, J. (1998). Effects of stressful daily events on mood states: Relationship to global perceived stress. Journal of Personality and Social Psychology, 75, 1572–1585. 10.1037/0022-3514.75.6.1572 [DOI] [PubMed] [Google Scholar]
- Wilson, A. , Yendork, J. S. , & Somhlaba, N. Z. (2017). Psychometric properties of Multidimensional Scale of Perceived Social Support among Ghanaian adolescents. Child Indicators Research, 10, 101–115. 10.1007/s12187-016-9367-1 [DOI] [Google Scholar]
- Youthinmind Ltd. (n.d.). SDQ: Information for researchers and professionals about the Strengths & Difficulties Questionnaires. Retrieved from http://www.sdqinfo.org. [DOI] [PubMed]
- Zimet, G. D. , Dahlem, N. W. , Zimet, S. G. , & Farley, G. K. (1988). Multidimensional Scale of Perceived Social Support. Journal of Personality Assessment, 52, 30–41. 10.1207/s15327752jpa5201_2 [DOI] [PubMed] [Google Scholar]


