Abstract
Background
Chronic and treatment‐resistant depressions pose serious problems in mental health care. Mindfulness‐based cognitive therapy (MBCT) is an effective treatment for remitted and currently depressed patients. It is, however, unknown whether MBCT is effective for chronic, treatment‐resistant depressed patients.
Method
A pragmatic, multicenter, randomized‐controlled trial was conducted comparing treatment‐as‐usual (TAU) with MBCT + TAU in 106 chronically depressed outpatients who previously received pharmacotherapy (≥4 weeks) and psychological treatment (≥10 sessions).
Results
Based on the intention‐to‐treat (ITT) analysis, participants in the MBCT + TAU condition did not have significantly fewer depressive symptoms than those in the TAU condition (–3.23 [–6.99 to 0.54], d = 0.35, P = 0.09) at posttreatment. However, compared to TAU, the MBCT + TAU group reported significantly higher remission rates (χ 2(2) = 4.25, φ = 0.22, P = 0.04), lower levels of rumination (–3.85 [–7.55 to –0.15], d = 0.39, P = 0.04), a higher quality of life (4.42 [0.03–8.81], d = 0.42, P = 0.048), more mindfulness skills (11.25 [6.09–16.40], d = 0.73, P < 0.001), and more self‐compassion (2.91 [1.17–4.65], d = 0.64, P = 0.001). The percentage of non‐completers in the MBCT + TAU condition was relatively high (n = 12, 24.5%). Per‐protocol analyses revealed that those who completed MBCT + TAU had significantly fewer depressive symptoms at posttreatment compared to participants receiving TAU (–4.24 [–8.38 to –0.11], d = 0.45, P = 0.04).
Conclusion
Although the ITT analysis did not reveal a significant reduction in depressive symptoms of MBCT + TAU over TAU, MBCT + TAU seems to have beneficial effects for chronic, treatment‐resistant depressed patients in terms of remission rates, rumination, quality of life, mindfulness skills, and self‐compassion. Additionally, patients who completed MBCT showed significant reductions in depressive symptoms. Reasons for non‐completion should be further investigated.
Keywords: depressive disorder, mindfulness, quality of life, randomized controlled trial, treatment‐resistant depression
1. INTRODUCTION
Major depressive disorder is one of the leading causes of disability worldwide (Lopez, Mathers, Ezzati, Jamison, & Murray, 2006). Despite evidence‐based treatments, about 20% of all depressed patients develop a chronic course (Kessler et al., 2003), typically defined as a period of 2 years or longer of depressive symptoms (DSM‐IV‐TR, 2000). Chronic depression not only affects the personal life of a patient, but is also associated with high costs for society in terms of health care costs and workplace losses (Pincus, 2001). Unfortunately, a large number of chronically depressed patients do not respond to treatment (Torpey & Klein, 2008). Therefore, novel treatment strategies for this severely ill population are much needed (Cuijpers, Huibers, & Furukawa, 2017).
Surprisingly, no unified definition of treatment‐resistant depression exists. Staging methods to measure treatment resistance mostly focus on the number of biological treatment steps (Trevino, McClintock, Fischer, Vora, & Husain, 2014). In line with these staging methods, most clinical trials define a depressive episode as treatment‐resistant if two or more trials with antidepressant medication were unsuccessful (Rush, Thase, & Dubé, 2003; Trevino et al., 2014). However, this definition conflicts with multidisciplinary treatment guidelines (NICE, 2009), which state that depressed patients with moderate to severe symptoms should receive a combination of psychological and pharmacological treatments. Therefore, a new staging method to measure treatment resistance was developed, which is termed as the “Dutch Measure for quantification of Treatment Resistance in Depression” (DM‐TRD) (Peeters et al., 2016). In contrast to previous staging methods (Fekadu, Wooderson, Donaldson, et al., 2009; Fekadu, Wooderson, Markopoulou, & Cleare, 2009; Petersen et al., 2005; Souery et al., 1999; Thase & Rush, 1997), the DM‐TRD not only focuses on biological treatments but also includes evidence‐based psychological treatments. For these reasons, we have chosen to apply the criteria of the DM‐TRD for treatment resistance in the current study.
Mindfulness‐based cognitive therapy (MBCT) is an 8‐week group training that combines mindfulness meditation techniques with elements of cognitive‐behavioral therapy (Segal, Williams, & Teasdale, 2012). MBCT teaches participants to recognize and disengage from maladaptive automatic cognitive patterns, and to develop a nonjudgmental and compassionate attitude toward their own cognitions and feelings. MBCT has been demonstrated to be effective in reducing relapse (Kuyken et al., 2016). In addition, it has been shown that MBCT reduces depressive symptoms in currently depressed patients (Strauss, Cavanagh, Oliver, & Pettman, 2014). Preliminary studies (Barnhofer Crane, Hargus, Amarasinghe, Winder, & Williams, 2009; Eisendrath et al., 2008; Kenny & Williams, 2007) have even found beneficial effects of MBCT for patients with chronic or treatment‐resistant depression. In line with these findings, in a recent randomized controlled trial (RCT) of Eisendrath et al. (2016) in treatment‐resistant depressed patients, MBCT was demonstrated to be superior to an active control group matched on treatment intensity. However, partly contrasting results were found by Michalak, Probst, Heidenreich, Bissantz, and Schramm (2016) in an RCT comparing MBCT with Cognitive Behavioural Analysis System of Psychotherapy (CBASP) and treatment‐as‐usual (TAU) in chronically depressed patients. CBASP is a psychological treatment with a strong interpersonal orientation that focuses on overcoming the learned helplessness of the patient by teaching patients that their own behavior affects others and themselves (McCullough, 2003). Michalak et al. (2016) concluded that MBCT was inferior to CBASP, and MBCT was superior to TAU only at one treatment site.
Importantly, all available controlled studies about MBCT for treatment‐resistant depression focused on pharmacoresistant depressed patients (Eisendrath et al., 2008, 2016). It therefore remains unclear whether MBCT is effective in chronically depressed patients who have been treated according to treatment guidelines (i.e., received evidence‐based psychological treatment and pharmacotherapy) but have not responded.
The aim of the current study was to investigate the effectiveness of MBCT + TAU versus TAU only for chronically depressed patients with current moderate to severe depressive symptoms who have not responded to previous pharmacotherapy and evidenced‐based psychological treatments, that is, cognitive behavioral therapy (CBT) or interpersonal therapy (IPT). The primary outcome measure was the level of depressive symptoms. Secondary outcome measures were remission rates, rumination, quality of life, mindfulness skills, and self‐compassion. Additionally, we examined the following variables as potential moderators of treatment effect gender, age, childhood trauma, number of previous episodes, duration of current depressive episode, treatment resistance, baseline levels of depressive symptoms, rumination, mindfulness skills, and self‐compassion.
2. METHOD
2.1. Design
This trial was an open‐labeled, multicenter RCT comparing two groups: MBCT + TAU and TAU. Methods and procedures are fully described in the published protocol (Cladder‐Micus et al., 2015) and are summarized below. All participants gave written informed consent and the study was approved by the Medical Ethical Committee Arnhem‐Nijmegen (number 2012/339).
2.2. Participants
Participants (N = 106) were recruited at different locations of a local mental health institute (Pro Persona) and a university medical center (Radboud University Medical Center, Centre for Mindfulness). Participants were referred by mental health care professionals or recruited via flyers, posters, and websites. Clinicians were also explicitly asked to screen their caseload for potentially eligible participants. A depressive episode was defined as “chronic” if symptoms persisted for ≥12 months, because research has shown that chances of recovery decrease substantially after this period (Spijker et al., 2002). Inclusion criteria were (a) age ≥ 18, (b) current depressive episode according to DSM‐IV criteria with a duration of ≥12 months, (c) moderate to high levels of depressive symptoms (Inventory of Depressive Symptomatology‐Self‐Report [IDS‐SR] ≥ 21), (d) at least one adequate trial of antidepressant medication during the current episode (defined as appropriate doses of antidepressant medication for ≥4 weeks or patient's refusal to use medication contrary to the advice of a psychiatrist), and (e) previous psychological treatment during the current episode (defined as ≥10 sessions of CBT or IPT or < 10 sessions if discontinued because of patient's withdrawal). Exclusion criteria were as follows: (a) current psychotic symptoms; (b) lifetime bipolar disorder; (c) current alcohol or drug dependence; (d) recent electro convulsive therapy (< 3 months ago); (e) current somatic disorder partly explaining depressive symptoms; (f) physical, linguistic, cognitive, or intellectual impairments, which might interfere with participation in MBCT or assessments; and (g) previous MBCT training. Baseline characteristics can be found in Table 1.
Table 1.
Demographic characteristics, clinical characteristics, and baseline levels of symptoms in both conditions displayed as number (percentage) unless otherwise specifieda
| Whole sample | TAU | MBCT + TAU | |
|---|---|---|---|
| n = 106 | n = 57 | n = 49 | |
| Demographic characteristics | |||
| Female | 66 (62) | 34 (60) | 32 (65) |
| Age, M (SD), years | 47.1 (10.25) | 47.33 (10.9) | 46.86 (9.53) |
| Education | |||
| Low | 34 (32) | 18 (32) | 16 (32) |
| Medium | 29 (27) | 20 (35) | 9 (18) |
| High | 35 (33) | 18 (32) | 17 (35) |
| Marital status | |||
| Single/widowed/divorced | 45 (43) | 28 (49) | 17 (35) |
| Married/cohabitating | 44 (42) | 24 (42) | 20 (41) |
| Employment | |||
| Full time | 10 (9.4) | 7 (12.3) | 3 (6.1) |
| Part time | 19 (17.9) | 7 (12.3) | 12 (24.5) |
| Unemployed | 67 (63.2) | 40 (70.2) | 27 (55.1) |
| Retired | 3 (2.8) | 1 (1.8) | 1 (2) |
| Clinical characteristics | |||
| n = 104 | n = 56 | n = 48 | |
| Previous episodes, M (SD) | 2.69 (3.37) | 2.68 (3.96) | 2.71 (2.56) |
| Age of onset, M (SD), years | 29.84 (13.16) | 31.75 (12.70) | 27.61 (13.48) |
| n = 103 | n = 56 | n = 47 | |
| Duration episodeb, M (SD), months | 63.59 (70.74) | 60.54 (65.42) | 67.23 (77.76) |
| Current episode ≥ 2 years | 85 (80) | 45 (79) | 40 (82) |
| Anxiety disorderc | 50 (47) | 30 (53) | 20 (41) |
| n = 97 | n = 53 | n = 44 | |
| Psychological treatment sessions (CBT/IPT)b, M (SD) | 36.29 (49.69) | 32.94 (36.27) | 40.32 (62.38) |
| Previous inpatient treatment b | |||
| Inpatient | 20 (19) | 13 (23) | 7 (14) |
| Day‐hospital | 15 (14) | 8 (14) | 7 (14) |
| > 2 AD's current episode (%) | 38.7 | 36.8 | 40.8 |
| Medication level at baseline | |||
| No AD | 23 (22) | 14 (25) | 9 (18) |
| 1 SSRI | 20 (19) | 12 (21) | 8 (16) |
| 1 TCA/SNRI/other AD | 24 (23) | 13 (23) | 11 (22) |
| 1 MAOI | 3 (3) | 1 (2) | 2 (4) |
| 2 AD's | 4 (4) | 1 (2) | 3 (6) |
| 1 AD + antipsychotic | 21 (20) | 11 (19) | 10 (20) |
| 1 AD + lithium | 7 (7) | 4 (7) | 3 (6) |
| n = 106 | n = 57 | n = 49 | |
| Treatment‐resistance (DM‐TRD), M (SD) | 13.92 (2.73) | 14.08 (2.71) | 13.74 (2.77) |
| n = 89 | n = 52 | n = 37 | |
| Childhood trauma (CTQ), M (SD) | 49.22 (19.48) | 48.77 (17.80) | 49.86 (21.64) |
| Baseline assessment, M (SD) | |||
| n = 106 | n = 57 | n = 49 | |
| Depression (IDS‐SR) | 41.11 (9.37) | 42.21 (9.12) | 39.83 (9.59) |
| n = 100 | n = 57 | n = 43 | |
| Rumination (RRS) | 56.82 (9.89) | 56,89 (10.12) | 56.75 (9.69) |
| Brooding | 13.54 (2.94) | 13,57 (3.08) | 13.51 (2.77) |
| Reflective | 10.79 (3.09) | 10,80 (3.37) | 10.79 (2.71) |
| Quality of life (WHOQoL‐BREF) | 71.92 (10.24) | 70,97 (8.97) | 73.18 (11.72) |
| Physical | 18.87 (4.07) | 18,59 (3.28) | 19.23 (4.94) |
| Psychological | 13.67 (3.07) | 13,50 (2.95) | 13.88 (3.23) |
| Social | 8.67 (2.34) | 8,52 (2.23) | 8.86 (2.49) |
| Environment | 26.15 (4.03) | 25,82 (3.90) | 26.60 (4.22) |
| n = 99 | n = 56 | n = 43 | |
| Mindfulness (FFMQ) | 101.21 (15.27) | 100.92 (15.34) | 101.60 (15.35) |
| Observing | 21.37 (5.67) | 21.27 (5.73) | 21.51 (5.66) |
| Describing | 22.50 (6.57) | 22.24 (5.64) | 22.86 (7.69) |
| Acting/awareness | 19.23 (4.86) | 19.18 (4.79) | 19.30 (5.04) |
| Nonjudging | 21.37 (6.40) | 21.65 (6.78) | 21.01 (5.92) |
| Nonreacting | 16.92 (3.91) | 16.94 (4.24) | 16.31 (3.50) |
| n = 98 | n = 56 | n = 42 | |
| Self‐compassion (SCS) | 17.59 (4.61) | 17.63 (5.16) | 17.55 (3.88) |
| Self‐kindness | 2.67 (1.11) | 2.68 (1.14) | 2.67 (1.09) |
| Self‐judging | 2.99 (1.26) | 2.98 (1.28) | 3.01 (1.27) |
| Common humanity | 3.01 (1.09) | 2.99 (1.13) | 3.05 (1.06) |
| Isolation | 2.73 (1.07) | 2.79 (1.23) | 2.64 (0.81) |
| Mindfulness | 3.17 (1.15) | 3.05 (1.45) | 3.33 (1.15) |
| Overidentification | 3.03 (1.23) | 3.18 (1.34) | 2.83 (1.10) |
Note. AD, antidepressant; CBT, cognitive behavioral therapy; IPT, interpersonal therapy; MAOI, monoamine‐oxidase inhibitor; SNRI, serotonin–norepinephrine reuptake inhibitor; SSRI, serotonin; TCA, tricyclic antidepressant; IDS‐SR, Inventory of Depressive Symptomatology‐Self Report; WHOQoL‐BREF, World Health Organisation Quality of Life Questionnaire; FFMQ, Five Facets Mindfulness Questionnaire; SCS, Self‐Compassion Scale.
There were no significant differences between the MBCT + TAU and TAU condition.
Current depressive episode.
At baseline, according to DSM‐IV criteria.
2.3. Procedure
Interested patients received an information letter and were contacted via telephone. During a subsequent research interview, the Mini International Neuropsychiatric Interview (MINI, Sheehan et al., 1998) was administered to diagnose depressive, anxiety, psychotic, and addictive disorders according to DSM‐IV criteria. In addition, sociodemographic and clinical characteristics were assessed, including treatment resistance (DM‐TRD, Peeters et al., 2016) and childhood trauma (Childhood Trauma Questionnaire; Bernstein et al., 2003). The DM‐TRD includes domains such as duration and severity of symptoms, comorbid anxiety disorders, functional impairments, previous biological treatments, and previous psychological treatments. After completion of the baseline measures, participants were randomized to MBCT + TAU or TAU only by means of a web‐based application that was specifically designed for this study by an independent statistician. Randomization was 1:1 to MBCT + TAU or TAU only, stratified for treatment center, and minimized for the severity of depressive symptoms (IDS‐SR: 21–31; 32–39; > 40) and chronicity (1–2 years, ≥2 years), without using block randomization. If due to scheduling constraints the time between baseline assessment and start of MBCT exceeded 4 weeks, a second baseline assessment was conducted before MBCT started. Participants assigned to the TAU condition were offered MBCT after completion of posttreatment measures. Follow‐up data were collected at 3 and 6 months after completing MBCT. Additionally, a subsample (N = 86) was invited to participate in experimental tasks during baseline and posttreatment to assess biased information processing. These data focus on different research questions and will be presented separately. Data presented here were collected between January 2013 and April 2016.
2.4. Interventions
2.4.1. MBCT + TAU
MBCT was based on the manual by Segal, Williams, and Teasdale (2002) and consisted of 8 weekly 2.5‐hr sessions and 1 day of practice (day of silence). Participants were enrolled in MBCT courses that were part of the regular treatment program for patients with depressive disorders. The average number of study participants was 2.41 (SD = 1.55) per MBCT group of 8–12 patients. Mindfulness trainers were informed about enrollment of participants in the study, but were pressed to adopt an identical approach and procedure for all patients. Group members were not informed about study participation of individual fellow members, but participants were of course allowed to share this information at will. All mindfulness trainers were highly experienced in working with depressed patients and had completed a postgraduate 2‐year mindfulness teacher training. Thereby they met the advanced criteria of good practice guidelines of the UK Network for Mindfulness‐Based Teachers (Network, 2011). Teacher competence and adherence was assessed with the Mindfulness‐Based Interventions‐Teaching Assessment Criteria (Crane et al., 2012) based on two video recorded sessions per trainer. Two independent mindfulness trainers rated the trainers. Mutually agreed ratings of the trainers were “proficient” (n = 2), “proficient/competent” (n = 1), “competent” (n = 2), and “advanced beginner” (n = 1). Videos of two trainers (who trained, respectively, two and three participants) were unavailable. Participants received TAU in conjunction with MBCT.
2.4.2. TAU
Treatment‐as‐usualTAU was a naturalistic condition consisting of mental health care for depression, including antidepressant medication, psychological treatment, support by a psychiatric nurse, or day‐hospital treatment. There were no significant differences between conditions in the mean number of treatment sessions or in the number of patients who received these treatments (see Table 2). Medication levels at baseline can be found in Table 1. A minority of participants changed in medication level. This information is summarized in Table 2 and additional information can be found in the Supporting Information Table 1.
Table 2.
Total number of participants and mean amount of therapy sessions received as treatment‐as‐usual (TAU) and changes in antidepressant medication from baseline to posttreatment
| MBCT + TAU | TAU | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | M | SD | N | % | M | SD | Test | |
| Therapy sessions | |||||||||
| Psychologist | 23 | 46.9 | 4.84 | 6.59 | 30 | 52.6 | 3.86 | 4.37 | χ2(1) = 0.256, P = 0.61 |
| t(92) = –0.859, P = 0.39 | |||||||||
| Psychiatrist | 15 | 30.6 | 0.73 | 1.33 | 20 | 35.1 | 0.72 | 1.09 | χ2(1) = 0.178, P = 0.67 |
| t(92) = –0.092, P = 0.97 | |||||||||
| Occupational therapist/ nurse specialist | 8 | 16.3 | 1.04 | 3.12 | 13 | 22.8 | 1.28 | 2.63 | χ2(1) = 0.626, P = 0.43 |
| t(92) = 0.395, P = 0.69 | |||||||||
| Day care treatment | 4 | 9.7 | 14.5b | 11.21 | 1 | 1.75 | 12b | 0 | Fisher's exact: P = 0.174 |
| t(3) = –0.199, P = 0.855 | |||||||||
| Medication | |||||||||
| Discontinueda | 4 | 8.2 | 2 | 3.5 | |||||
| Decrease in medication level | 3 | 6.1 | 1 | 1.8 | |||||
| Increase in medication level | 0 | 0 | 4 | 7.0 | |||||
Note. Psychologist sessions include therapy sessions lead by a registered psychologist (e.g., CBT, IPT, neuropsychological tests, schema therapy). Sessions by a psychiatrist include check‐up and advice concerning medications. Therapy sessions given by an occupational therapist/nurse specialist include therapies such as running therapy, rehabilitation modules, and psychomotor therapy. Day care includes outpatient care provided by a mental health care institution such as day treatment.
All antidepressant medication tapered to zero.
In days; only including participants with ≥1 day of day care treatment.
2.5. Outcome measures
2.5.1. Primary outcome measure
The primary outcome was the level of depressive symptoms assessed with IDS‐SR (Rush, Gullion, Basco, Jarrett, & Trivedi, 1996). The IDS‐SR has good psychometric properties (Rush et al., 1996). The IDS‐SR has previously been used in research on MBCT and is sensitive to change (Geschwind, Peeters, Huibers, van Os, & Wichers, 2012). In the current sample, the internal consistency was α = 0.74.
2.5.2. Secondary outcome measures
Remission was assessed with the depression module of the MINI, which investigates depressive symptoms according to DSM‐IV criteria. Remission was defined as the absence of depressive symptoms during the last 2 weeks. Participants reporting some symptoms but not fulfilling DSM‐IV criteria according to the MINI were classified as being in partial remission. The interviews were administered by trained research psychologists supervised by an experienced psychiatrist (AS) and were audio recorded. For logistical reasons, it was not possible to keep the research psychologists blind to treatment allocation. A random sample (n = 25) of the recorded MINI depression modules was scored by an independent psychologist blind to condition, who was extensively trained in the administration of the MINI. This yielded a high interrater reliability (Cohen's kappa 0.88).
Rumination was assessed with the Ruminative Response Scale (RRS‐EXT; Raes & Hermans, 2007; Schoofs, Hermans, & Raes, 2010). Quality of life was assessed with the World Health Organization Quality of Life scale (Skevington, Lotfy, & O'Connell, 2004). Mindfulness skills and self‐compassion were assessed with the Five Facet Mindfulness Questionnaire (Baer et al., 2008) and the Self‐Compassion Scale (Neff, 2003), respectively. More information about these secondary outcome measures can be found in the published study protocol (Cladder‐Micus et al., 2015, pp. 5–6).
2.6. Statistical analysis
The power calculation was based on a Cohen's d effect size of 0.53 for currently depressed patients as reported in a previous study (van Aalderen et al., 2011). Based on an α of 0.05 and power of 80%, estimating the correlation between baseline and posttreatment scores to be 0.5, and expecting a drop‐out of 8 participants, a required sample size of 94 participants emerged (Cladder‐Micus et al., 2015). For the main analysis, posttreatment scores of depressive symptoms were compared between the two conditions in an analysis of covariance (ANCOVA), controlling for baseline scores of depression, chronicity (1–2 years; ≥2 years), and treatment site. Similar analyses were conducted for the secondary outcome measures, controlling for baseline scores of the respective variable, chronicity (1–2 years; ≥2 years), and treatment site. A Cohen's d effect size was calculated based on the total group's (n = 106) standard deviation on the IDS‐SR at baseline. A statistical significance level of 0.05 was adhered to for all analyses. Moderating effects of gender, age, childhood trauma, number of previous episodes, duration of current depressive episode treatment resistance, baseline levels of depressive symptoms, rumination, mindfulness skills, and self‐compassion were explored in the intention‐to‐treat (ITT) sample by incorporating interaction effects in the models. Posttreatment IDS‐SR scores were missing for 10 participants (9.4%, TAU: n = 5, MBCT + TAU: n = 5). There were no differences in clinical or baseline characteristics between patients with and without posttreatment IDS‐SR scores, except that the patients with missing scores reported a higher number of previous depressive episodes (M = 5.00, SD = 8.90, t (102) = –2.32, P = 0.02) than complete cases (M = 2.45, SD = 2.07). For two patients without posttreatment scores, follow‐up scores were used. Analyses were based on an ITT approach including all available data. Next, analyses were repeated in the per‐protocol (PP) sample, including participants of MBCT + TAU who attended ≥4 sessions and participants of TAU. Sensitivity analyses were performed by imputing missing data according to the last observation carried forward (LOCF) technique. IBM SPSS statistics 22 was used to analyze the data.
3. RESULTS
3.1. Patient flow
Of the 213 patients who were assessed for eligibility, 111 were interviewed and 106 were randomized over MBCT + TAU (n = 49) and TAU (n = 57) (see Figure 1). There were no significant differences in clinical characteristics or baseline scores between the conditions (see Table 1). Before entering the study, 102 participants had received > 10 sessions of psychological treatment during the current episode, one participant completed nine sessions during the current depressive episode and > 10 during the previous episode, and three participants refused psychological treatment because they received > 10 sessions during the previous depressive episode. Five participants refused to use antidepressant medication during the current depressive episode against the advice of their psychiatrist. All other participants (n = 101) had been using adequate levels of antidepressant medication for at least 4 weeks. Twenty‐six (53.0%) MBCT + TAU participants completed a second baseline because time from randomization to MBCT exceeded 4 weeks and no significant changes in depressive symptoms between the first and second baseline were observed (M baseline1 = 41.15, SD baseline1 = 7.86, M baseline2 = 40.38, SD baseline2 = 9.99; t (25) = 0.47, P = 0.64). None of the participants of the TAU condition took part in MBCT or other mindfulness‐based training. Twelve participants of the MBCT + TAU condition (24.5%) attended fewer than four sessions of MBCT and were classified as non‐completers. The other participants (completers) attended on average 7.09 (SD = 1.15) out of the eight MBCT sessions. The most prevalent reason for drop‐out was the occurrence or deterioration of physical problems (see Figure 1). Non‐completers reported a shorter duration of the current depressive episode (M = 60.05 months, SD = 71.72) than completers (M = 93.18 months, SD = 56.22; U = 246.5, P = 0.005) and they were more often unemployed (χ 2 (5) = 8.60, P = 0.04). There were no other significant differences in sociodemographic or clinical characteristics between non‐completers and completers (see Table 2 in the Supporting Information). No serious adverse events occurred.
Figure 1.
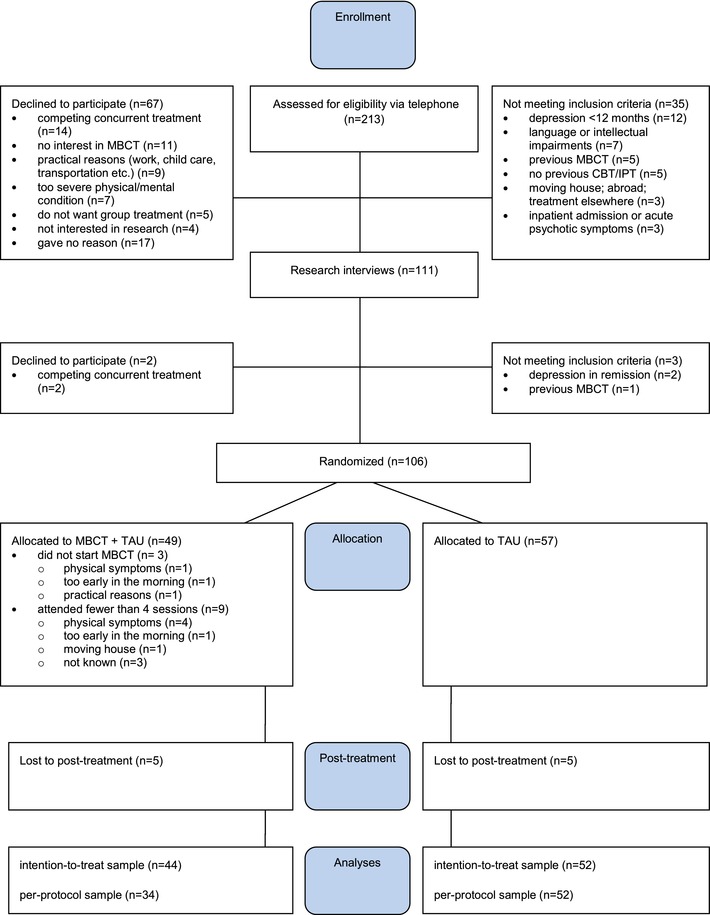
Consort flow diagram
3.2. Primary outcome
Depression scores were analyzed separately for the ITT sample and the PP sample. In both analyses, the MBCT + TAU condition showed lower levels of depressive symptoms than TAU, with small to medium effect sizes. However, the difference was only significant in the PP sample (–4.24, 95% CI [–8.38 to –0.11], d = 0.45, P = 0.04) and not in the ITT sample (–3.23, 95% CI [–7.02 to 0.56], d = 0.35, P = 0.09) (see Table 3). Sensitivity analyses using the LOCF sample led to similar findings. When participants who refused to take antidepressant medication (n = 5) were excluded from the analyses, results of the ITT sample (–3.01, 95% CI [–6.8, 0.78], d = 0.31, P = 0.12) and the PP sample (–4.59, 95% CI [–8.8, –0.38], d = 0.51, P = 0.03) were comparable to the main analyses.
Table 3.
Depressive symptoms, rumination, quality of life, mindfulness skills, and self‐compassions at postmeasurement of mindfulness‐based cognitive therapy (MBCT) and treatment‐as‐usual (TAU) for intention‐to‐treat (ITT) and per‐protocol (PP) analyses
| ITT | PP | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Postmeasurement results, unadjusted mean (SD) | MBCT + TAU n = 44 | TAU n = 52 | Group difference (95% CI) | F | P | d | MBCT + TAU n = 34 | TAU n = 52 | Group difference (95% CI) | F | P | d |
| Depression (IDS‐SR) | 35.27 (12.66) | 40.52 (11.83) | –3.23 (–7.02 to 0.56) | 2.86 | 0.092 | 0.35 | 33.50 (11.13) | 40.52 (11.83) | –4.24 (–8.38 to –0.11) | 4.17 | 0.044 | 0.45 |
| n = 39 | n = 51 | n = 31 | n = 51 | |||||||||
| Rumination (RRS) | 50.51 (11.06) | 54.47 (9.99) | –3.85 (–7.55 to –0.15) | 4.28 | 0.042 | 0.39 | 50.67 (10.00) | 54.47 (9.99) | –3.36 (–6.92 to 0.21) | 3.51 | 0.065 | 0.33 |
| Brooding | 11.72 (2.85) | 13.08 (3.38) | –1.37 (–2.48 to –0.26) | 6.03 | 0.016 | 0.47 | 11.64 (2.75) | 13.08 (3.38) | –1.38 (–2.51 to –0.26) | 6.04 | 0.016 | 0.47 |
| Reflective pondering | 10.13 (2.94) | 10.16 (2.88) | 0.084 (–0.85 to 1.01) | 0.32 | 0.859 | 0.03 | 10.49 (2.75) | 10.16 (2.88) | 0.38 (–0.57 to 1.34) | 0.64 | 0.425 | 0.13 |
| Quality of life (WHOQoL‐BREF) | 77.31 (16.00) | 71.13 (11.29) | 4.42 (0.03 to 8.81) | 4.01 | 0.048 | 0.42 | 78.37 (12.72) | 71.13 (11.29) | 5.13 (0.81 to 9.45) | 5.59 | 0.021 | 0.49 |
| Physical health | 19.74 (5.43) | 18.63 (3.78) | 0.65 (–0.86 to 2.16) | 0.76 | 0.394 | 0.15 | 20.26 (4.64) | 18.62 (3.78) | 0.71 (–0.86 to 2.28) | 0.82 | 0.368 | 0.17 |
| Psychological | 15.92 (3.89) | 13.86 (3.29) | 1.82 (0.56 to 3.08) | 8.20 | 0.005 | 0.59 | 16.05 (3.42) | 13.85 (3.29) | 1.74 (0.48 to 3.00) | 7.59 | 0.007 | 0.56 |
| Social relationships | 8.87 (3.18) | 8.72 (2.48) | 0.14 (–0.83 to 1.11) | 0.9 | 0.770 | 0.06 | 8.71 (2.95) | 8.72 (2.48) | 0.28 (–0.75 to 1.31) | 0.29 | 0.595 | 0.12 |
| Environment | 27.41 (4.69) | 25.61 (4.79) | 1.01 (–0.45 to 2.47) | 1.88 | 0.174 | 0.25 | 27.77 (4.06) | 25.61 (4.79) | 1.56 (0.12 to 2.99) | 4.67 | 0.034 | 0.38 |
| n = 39 | n = 50 | n = 31 | n = 51 | |||||||||
| Mindfulness skills (FFMQ) | 113.56 (20.11) | 101.95 (14.55) | 11.25 (6.09 to 16.40) | 18.85 | <0.001 | 0.73 | 114.54 (17.94) | 101.94 (14.55) | 11.67 (6.65 to 16.69) | 21.46 | <0.001 | 0.76 |
| Observe | 24.59 (6.56) | 21.26 (6.11) | 3.04 (1.30 to 4.77) | 12.01 | 0.001 | 0.53 | 25.87 (5.37) | 21.26 (6.11) | 4.05 (2.33 to 5.77) | 22.01 | <0.001 | 0.71 |
| Describe | 24.66 (7.69) | 22.15 (6.12) | 1.67 (–0.17 to 3.52) | 3.23 | 0.076 | 0.25 | 24.89 (7.79) | 22.15 (6.12) | 1.38 (–0.59 to 3.35) | 1.95 | 0.167 | 0.21 |
| Act with awareness | 21.77 (5.81) | 19.89 (5.26) | 1.76 (0.02 to 3.50) | 4.04 | 0.048 | 0.35 | 21.90 (4.71) | 19.89 (5.26) | 1.89 (0.08 to 3.70) | 4.34 | 0.041 | 0.39 |
| Nonjudging | 23.53 (4.77) | 22.04 (6.63) | 2.04 (0.02 to 4.06) | 4.02 | 0.048 | 0.32 | 22.38 (3.86) | 22.04 (6.63) | 0.90 (–1.13 to 2.92) | 0.78 | 0.381 | 0.14 |
| Nonreactivity | 19.00 (4.45) | 16.93 (4.15) | 2.41 (0.81 to 4.02) | 8.99 | 0.004 | 0.49 | 19.48 (3.63) | 16.93 (4.15) | 3.05 (1.52 to 4.59) | 15.73 | <0.001 | 0.59 |
| n = 38 | n = 50 | n = 31 | n = 50 | |||||||||
| Self‐Compassion Scale (SCS) | 20.54 (4.64) | 17.93 (5.22) | 2.91 (1.17 to 4.65) | 11.05 | 0.001 | 0.64 | 20.51 (4.30) | 17.92 (5.22) | 3.08 (1.36 to 4.80) | 12.76 | 0.001 | 0.68 |
| Self‐kindness | 3.19 (1.07) | 2.73 (1.06) | 0.51 (0.11 to 0.91) | 6.52 | 0.013 | 0.46 | 3.29 (1.07) | 2.73 (1.06) | 0.67 (0.27 to 1.08) | 10.92 | 0.001 | 0.61 |
| Self‐judgment | 3.38 (1.16) | 3.29 (1.36) | 0.07 (–0.39 to 0.54) | 0.10 | 0.753 | 0.06 | 3.31 (1.12) | 3.29 (1.36) | –0.05 (–0.51 to .42) | 0.40 | 0.843 | 0.04 |
| Common humanity | 3.09 (.98) | 2.81 (1.21) | 0.31 (–0.12 to 0.73) | 2.06 | 0.155 | 0.28 | 3.07 (1.07) | 2.81 (1.21) | 0.31 (–0.16 to .78) | 1.71 | 0.195 | 0.28 |
| Isolation | 3.52 (1.27) | 2.92 (1.30) | 0.74 (0.29 to 1.19) | 10.64 | 0.002 | 0.72 | 3.46 (1.19) | 2.92 (1.30) | 0.69 (0.25 to 1.14) | 9.53 | 0.003 | 0.67 |
| Mindfulness | 3.66 (1.03) | 3.12 (1.20) | 0.47 (0.02 to 0.93) | 4.27 | 0.042 | 0.42 | 3.73 (.93) | 3.12 (1.20) | 0.62 (0.15 to 1.09) | 6.96 | 0.010 | 0.54 |
| Overidentification | 3.70 (1.31) | 3.15 (1.16) | 0.78 (0.31 to 1.23) | 11.30 | 0.001 | 0.70 | 3.63 (1.16) | 3.15 (1.16) | 0.73 (0.30 to 1.17) | 11.07 | 0.001 | 0.66 |
Note. FFMQ, Five Facets Mindfulness Questionnaire; IDS‐SR, Inventory of Depressive Symptomatology‐Self Report; SCS, Self‐Compassion Scale; WHOQoL, World Health Organisation Quality of Life Questionnaire.
3.3. Secondary outcomes
Compared to TAU, a significantly larger proportion of MBCT + TAU participants reached remission (MBCT + TAU: 41.5%; TAU: 21.6%, Table 4). However, most cases were classified as partial remission (MBCT + TAU: 39.0%; TAU: 17.65%) and a minority as full remission (MBCT + TAU: 2.44%; TAU: 3.92%). Compared to TAU, the MBCT + TAU condition showed significantly less rumination (d = 0.39, P = 0.04) and significantly higher quality of life (d = 0.42, P = 0.048) at posttreatment, controlling for baseline scores. Additionally, participants with MBCT + TAU showed significantly more mindfulness skills (d = 0.73, P < 0.001) and significantly more self‐compassion (d = 0.64, P = 0.001) than participants with TAU only. Analyses in the PP sample yielded comparable results (see Tables 3 and 4).
Table 4.
Number (and percentages) of depression status at posttreatment according to DSM‐IV criteria
| ITT | PP | |||||
|---|---|---|---|---|---|---|
| MBCT + TAU | TAU | MBCT + TAU | TAU | |||
| n = 41 | n = 51 | χ2 test | n = 34 | n = 51 | χ2 test | |
| Major depression | 24 (58.5) | 40 (78.4) | χ 2(2) = 4.25, P = 0.039, φ = 0.22 | 19 (55.9) | 40 (78.4) | χ 2(2) = 4.89, P = 0.027, φ = 0.24 |
| Remission | 17 (41.5) | 11 (21.6) | 15 (44.1) | 11 (21.6) | ||
| Full remission | 1 (2.44) | 2 (3.92) | 0 (0) | 2 (3.92) | ||
| Partial remission | 16 (39.0) | 9 (17.65) | 15 (44.14) | 9 (17.65) | ||
Note. Remission is defined as reporting no DSM‐IV symptoms of depression during the last 2 weeks based on the MINI. Partial remission is defined as reporting some symptoms but not fulfilling DSM‐IV criteria for a major depressive disorder. Depression is defined as fulfilling the DSM‐IV criteria for major depression on the MINI.
3.4. Moderation analyses
There were no significant moderators for the effect of condition on depressive symptoms in the ITT sample, apart from baseline levels of rumination (F (1, 84) = 5.44, P = 0.02). Participants with higher baseline rumination showed a significantly larger decrease in depressive symptoms in the MBCT + TAU condition compared to TAU, while controlling for depressive symptoms on baseline. In an exploratory analysis, participants were grouped based on a previously published clinical mean of the RRS‐EXT (Raes et al., 2009). In the group of participants scoring above the clinical mean for rumination, participants assigned to MBCT + TAU showed significantly lower depressive symptoms compared to TAU (–10.79, 95% CI [–15.72 to –5.85], d = 1.64, P < 0.001; MBCT + TAU n = 17, TAU n = 22) posttreatment while controlling for baseline depressive symptoms, whereas no difference between MBCT + TAU and TAU was observed in the group of participants scoring below the clinical mean (1.47, 95% CI [–4.38 to 7.33], d = 0.24, P = 0.62; MBCT + TAU n = 22, TAU n = 30). Patients of the MBCT + TAU condition who scored high on treatment resistance (DM‐TRD) tended to report higher levels of depressive symptoms posttreatment, however this difference was not significant (F (1, 89) = 3.05, P = 0.084).
4. DISCUSSION
The aim of the current study was to investigate the effectiveness of MBCT + TAU for chronic, treatment‐resistant depressed patients, who had not improved during not only previous pharmacotherapy but also psychological treatment. The results of the ITT analysis did not confirm the expected reduction in depressive symptoms. However, completers of the MBCT + TAU did show a significant decrease in depressive symptoms compared to TAU. Further, according to the ITT analyses, more participants in the MBCT + TAU condition reached partial remission and MBCT + TAU participants reported less rumination and increased quality of life, mindfulness skills, and self‐compassion compared to participants receiving TAU only.
The finding that the decrease in depressive symptoms was significant only in the PP analysis and not in the ITT analysis can be partially explained by the relatively high proportion of patients not completing MBCT (n = 12, 24.5%). This percentage is comparable to other studies on MBCT in chronic (27.8%; Michalak, Schultze, Heidenreich, & Schramm, 2015) or pharmacoresistant depressed patients (22.98%; Eisendrath et al., 2016), but seems to be higher than in studies focusing on patients with recurrent depression (8.8%; van Aalderen et al., 2011). Compared to completers, non‐completers reported a shorter duration of the current depressive episode and were more often unemployed. This could indicate that a longer duration might increase psychological burden and thereby motivates patients to acquire new skills. Additionally, a daily routine could be helpful in incorporating mindfulness skills into daily life. However, the sample of non‐completers is too small to draw firm conclusions here. Although one might expect that the most severely depressed patients drop out of treatment, non‐completers and completers did not differ in the severity of depressive symptoms, number of previous episodes, or age of onset. By contrast, a noticeable number of non‐completers reported that physical problems (see Figure 1) interfered with participation and were the reason for discontinuing MBCT.
MBCT + TAU had significant effects on rumination, quality of life, mindfulness skills, and self‐compassion. Following the course, MBCT + TAU participants reported less rumination and a higher quality of life. The increase in mindfulness skills and self‐compassion might indicate that chronic, treatment‐resistant depressed patients are able to learn mindfulness meditation techniques and develop a more compassionate and friendlier attitude toward themselves. Although results of these secondary outcomes should be interpreted as preliminary, as the power analysis was focused on changes in depressive symptoms, this may indicate that MBCT + TAU has effects that could be valuable for chronic, treatment‐resistant depressed patients, even if no or only small changes in depressive symptoms are evoked.
This study is the first to investigate the effectiveness of MBCT + TAU for chronic, treatment‐resistant depressed patients who did not benefit from pharmacotherapy and psychological treatment. The current study has high ecological validity because of its pragmatic design. Participants were moderately to severely depressed outpatients and were enrolled in MBCT trainings provided regularly at their local mental health care institution. Thereby this study provides much‐needed insight into the effectiveness rather than efficacy of MBCT, which was formulated as an important research goal in a recent review paper of MBCT (Dimidjian & Segal, 2015). However, the effect sizes found in this study (ITT: d = 0.35; PP: d = 0.45) are smaller than in previous preliminary studies of chronic or treatment‐resistant depressed patients (Barnhofer et al., 2009; Eisendrath et al., 2008; Kenny & Williams, 2007), as well as smaller than the effect size found in previous research on currently depressed patients (d = 0.53; van Aalderen et al., 2011), which was used for our power analysis. Both the relatively small effect size and the high drop‐out rate from MBCT can likely be explained by the higher severity of symptoms in the current study sample compared to previous research (van Aalderen et al., 2011). As only completers showed a significant decrease in depressive symptoms, obstacles to completing treatment should be investigated in future research, for example, by conducting qualitative interviews.
In addition to the effectiveness of MBCT, we also investigated possible moderators of treatment effect. Importantly, levels of rumination moderated the effect of MBCT + TAU compared to TAU on depressive symptoms. Participants with high levels of rumination benefitted more from MBCT + TAU than TAU. According to the underlying theoretical model, rumination is an important working mechanism of MBCT (Segal et al., 2002) and previous work has indicated that rumination might mediate the effect of MBCT on depressive symptoms (Shahar, Britton, Sbarra, Figueredo, & Bootzin, 2010; van der Velden et al., 2015). The current study indicates that MBCT could be particularly helpful for chronic, treatment‐resistant depressed patients with high levels of rumination. However, because of the explorative nature of the moderation analysis, this finding should be interpreted as preliminary and requires replication and further investigation. In addition, the results of the current study showed no moderating effects of childhood trauma, baseline severity of depression, chronicity, or treatment resistance. Moderating effects of childhood trauma and severity of baseline symptoms were previously found in recurrent depressed patients (Ma & Teasdale, 2004; Williams et al., 2014). However, recent studies on MBCT in chronic or pharmacoresistant depression found no moderating effect of these variables (Eisendrath et al., 2016; Michalak et al., 2016), which is in line with our findings. Taken together, these results indicate that rumination might be an important moderator in chronic, treatment‐resistant depression, while levels of childhood trauma and severity of depressive symptoms at baseline appear to be of less influence.
A limitation of the current study is that MBCT was implemented as an add‐on to TAU. The results in the MBCT + TAU condition could therefore be partially due to nonspecific therapy effects, such as peer support, hope, and attention received from the therapist. Additionally, patients and investigators were not blind to treatment allocation, which might have been a potential source of bias. Future studies should compare MBCT to active treatments matched on treatment intensity and should also investigate long‐term effects and cost effectiveness. Furthermore, due to the pragmatic design of the study, MBCT trainings were not in all cases immediately available after randomization. Participants who had to wait more than 4 weeks until the start of MBCT received a second baseline assessment. This means that the total duration of the study is not identical for the conditions. However, one should note that we found no difference in depressive symptoms between the first and second baseline assessment. In addition, research designs investigating potential mediators such as rumination, mindfulness skills, and self‐compassion by including multiple assessments during the course of MBCT would give further insight into mechanisms of change.
The current study provides several clinical and research implications. Even though effects on depressive symptoms were not significant in the ITT analysis, results of the secondary outcome measures indicated that MBCT might have beneficial effects for chronic, treatment‐resistant patients on important factors other than depressive symptoms. In addition, the results of the PP analyses indicated that completers of MBCT + TAU did show a significantly greater reduction in depressive symptoms compared to TAU alone. Keeping in mind that the study sample represents a seriously ill population, small effects on depressive symptoms accompanied by effects on rumination, quality of life, mindfulness, and self‐compassion may be valuable for an individual patient. In addition, the relatively low costs and rare side effects of MBCT compared with other treatment options for this population, for example, intensive pharmacological treatment or electroconvulsive therapy, should be taken into account in treatment choice. However, it seems to be important to further investigate reasons why patients do not complete MBCT. Additionally, future research should further focus on rumination and other possible working mechanisms in order to provide researchers and clinicians with more information about the working mechanisms of MBCT and predictors of treatment success.
CONFLICT OF INTEREST
A.E.M. Speckens is founder and clinical director of the Radboudumc Centre for Mindfulness. She is a mindfulness trainer and occasionally receives payment for training workshops and presentations related to mindfulness‐based cognitive therapy. She also donates all such fees to Radboud University Medical Center. M.B. Cladder‐Micus, J. Spijker, E.S. Becker, J.N. Vrijsen, and A.R.T. Donders declare they have no potential conflict of interest.
Supporting information
Tables
ACKNOWLEDGMENTS
This research was partly funded by a grant from Fonds Psychische Gezondheid, the Netherlands Foundation for Mental Health (number 2011 6630). The funder had no role in the conduct of the study, data collection, analysis, interpretation of results, or preparation of the manuscript. The authors would like to thank the participants for their willingness to take part in the trial. We would also like to thank the mindfulness trainers for providing the training, and Hiske van Ravesteijn, Melanie Schellekens, and Lotte School for independent ratings of the data. In addition, we would like to acknowledge and thank Mark Mepschen, Renske Olearnik, Peter Delsink, Veroniek Vugts, Rosalie van Woezik, Denise te Paste, Anja Calaminus, Peter Janssen, Tessa Heijnen, Charlotte van den Beuken, Sophie Bekmann, and Nadera Aga for helping with recruitment and data collection. We would like to thank Julie Krans for helpful comments on a previous version of the manuscript.
Cladder‐Micus MB, Speckens AEM, Vrijsen JN, Donders ART, Becker ES, Spijker J. Mindfulness‐based cognitive therapy for patients with chronic, treatment‐resistant depression: A pragmatic randomized controlled trial. Depress Anxiety. 2018;35:914–924. 10.1002/da.22788
REFERENCES
- Baer, R. A. , Smith, G. T. , Lykins, E. , Button, D. , Krietemeyer, J. , Sauer, S. , … Williams, J. M. G. (2008). Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment, 15(3)329–342. [DOI] [PubMed] [Google Scholar]
- Barnhofer, T. , Crane, C. , Hargus, E. , Amarasinghe, M. , Winder, R. , & Williams, J. M. G. (2009). Mindfulness‐based cognitive therapy as a treatment for chronic depression: A preliminary study. Behaviour Research and Therapy, 47(5), 366–373. 10.1016/j.brat.2009.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein, D. P. , Stein, J. A. , Newcomb, M. D. , Walker, E. , Pogge, D. , Ahluvalia, T. , … Zule, W. (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse and Neglect, 27(2), 169–190. 10.1016/s0145-2134(02)00541-0 [DOI] [PubMed] [Google Scholar]
- Cladder‐Micus, M. B. , Vrijsen, J. N. , Becker, E. S. , Donders, R. , Spijker, J. , & Speckens, A. E. (2015). A randomized controlled trial of mindfulness‐based cognitive therapy (MBCT) versus treatment‐as‐usual (TAU) for chronic, treatment‐resistant depression: Study protocol. BMC Psychiatry, 15(1), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane, R. S. , Kuyken, W. , Williams, J. M. G. , Hastings, R. P. , Cooper, L. , & Fennell, M. J. V. (2012). Competence in teaching mindfulness‐based courses: Concepts, development and assessment. Mindfulness, 3(1), 76–84. 10.1007/s12671-011-0073-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers, P. , Huibers, M. J. , & Furukawa, T. A. (2017). The need for research on treatments of chronic depression. JAMA Psychiatry, 74, 242–243. [DOI] [PubMed] [Google Scholar]
- Dimidjian, S. , & Segal, Z. V. (2015). Prospects for a clinical science of mindfulness‐based intervention. American Psychologist, 70(7), 593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DSM‐IV‐TR, A. (2000). Diagnostic and statistical manual of mental disorders‐text revision. Washington, DC: American Psychiatric Association. [Google Scholar]
- Eisendrath, S. J. , Delucchi, K. , Bitner, R. , Fenimore, P. , Smit, M. , & McLane, M. (2008). Mindfulness‐based cognitive therapy for treatment‐resistant depression: A pilot study. Psychotherapy and Psychosomatics, 77(5), 319–320. 10.1159/000142525 [DOI] [PubMed] [Google Scholar]
- Eisendrath, S. J. , Gillung, E. , Delucchi, K. L. , Segal, Z. V. , Nelson, J. C. , McInnes, L. A. , … Feldman, M. D. (2016). A randomized controlled trial of mindfulness‐based cognitive therapy for treatment‐resistant depression. Psychotherapy and Psychosomatics, 85(2), 99–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fekadu, A. , Wooderson, S. , Donaldson, C. , Markopoulou, K. , Masterson, B. , Poon, L. , & Cleare, A. J. (2009). A multidimensional tool to quantify treatment resistance in depression: The Maudsley staging method. The Journal of Clinical Psychiatry, 70(2), 177–184. [DOI] [PubMed] [Google Scholar]
- Fekadu, A. , Wooderson, S. C. , Markopoulou, K. , & Cleare, A. J. (2009). The Maudsley staging method for treatment‐resistant depression: Prediction of longer‐term outcome and persistence of symptoms. The Journal of Clinical Psychiatry, 70(7), 952–957. [DOI] [PubMed] [Google Scholar]
- Geschwind, Peeters, Huibers, van Os, & Wichers (2012). Efficacy of mindfulness‐based cognitive therapy in relation to prior history of depression: Randomised controlled trial. The British Journal of Psychiatry, 201(4), 320–325. 10.1192/bjp.bp.111.104851 [DOI] [PubMed] [Google Scholar]
- Kenny, M. A. , & Williams, J. M. G. (2007). Treatment‐resistant depressed patients show a good response to mindfulness‐based cognitive therapy. Behaviour Research and Therapy, 45(3), 617–625. 10.1016/j.brat.2006.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R. C. , Berglund, P. , Demler, O. , Jin, R. , Koretz, D. , Merikangas, K. R. , … Wang, P. S. (2003). The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS‐R). Jama, 289(23), 3095–3105. [DOI] [PubMed] [Google Scholar]
- Kuyken, W. , Warren, F. C. , Taylor, R. S. , Whalley, B. , Crane, C. , Bondolfi, G. , … Dalgleish, T. (2016). Efficacy of mindfulness‐based cognitive therapy in prevention of depressive relapse: An individual patient data meta‐analysis from randomized trials. JAMA Psychiatry, 10.1001/jamapsychiatry.2016.0076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez, A. D. , Mathers, C. D. , Ezzati, M. , Jamison, D. T. , & Murray, C. J. (2006). Global and regional burden of disease and risk factors, 2001: Systematic analysis of population health data. The Lancet, 367(9524), 1747–1757. [DOI] [PubMed] [Google Scholar]
- Ma, S. H. , & Teasdale, J. D. (2004). Mindfulness‐based cognitive therapy for depression: Replication and exploration of differential relapse prevention effects. Journal of Consulting and Clinical Psychology, 72(1), 31–40. 10.1037/0022-006x.72.1.31 [DOI] [PubMed] [Google Scholar]
- McCullough, J. P. (2003). Treatment for chronic depression using cognitive behavioral analysis system of psychotherapy (CBASP). Journal of Clinical Psychology, 59(8), 833–846. [DOI] [PubMed] [Google Scholar]
- Michalak, J. , Probst, T. , Heidenreich, T. , Bissantz, N. , & Schramm, E. (2016). Mindfulness‐based cognitive therapy and a group version of the cognitive behavioral analysis system of psychotherapy for chronic depression: Follow‐up data of a randomized controlled trial and the moderating role of childhood adversities. Psychotherapy and Psychosomatics, 85(6), 378–380. [DOI] [PubMed] [Google Scholar]
- Michalak, J. , Schultze, M. , Heidenreich, T. , & Schramm, E. (2015). A randomized controlled trial on the efficacy of mindfulness‐based cognitive therapy and a group version of cognitive behavioral analysis system of psychotherapy for chronically depressed patients. Journal of Consulting and Clinical Psychology, 83(5), 951–963. 10.1037/ccp0000042 [DOI] [PubMed] [Google Scholar]
- Neff, K. D. (2003). The development and validation of a scale to measure self‐compassion. Self and Identity, 2(3), 223–250. [Google Scholar]
- Network, U. M.‐B. T. T. (2011). Good practice guidance for teachers. Retrieved from https://mindfulnessteachersuk.org.uk/pdf/teacher-guidelines.pdf
- NICE . (2009). Depression: The treatment and management of depression in adults (updated edition). Leicester, England: British Psychological Society; Retrieved from http://www.nice.org.uk/CG90 [PubMed] [Google Scholar]
- Peeters, F. P. , Ruhe, H. G. , Wichers, M. , Abidi, L. , Kaub, K. , van der Lande, H. J. , … Schene, A. H. (2016). The Dutch Measure for quantification of Treatment Resistance in Depression (DM‐TRD): An extension of the Maudsley Staging Method. Journal of Affective Disorders, 205, 365–371. [DOI] [PubMed] [Google Scholar]
- Petersen, T. , Papakostas, G. I. , Posternak, M. A. , Kant, A. , Guyker, W. M. , Iosifescu, D. V. , … Fava, M. (2005). Empirical testing of two models for staging antidepressant treatment resistance. Journal of Clinical Psychopharmacology, 25(4), 336–341. [DOI] [PubMed] [Google Scholar]
- Pincus, H. A. H. (2001). The societal costs of chronic major depression. Journal of Clinical Psychiatry, 62, 5–9. [PubMed] [Google Scholar]
- Raes, F. , & Hermans, D. (2007). The revised version of the Dutch ruminative response scale (Unpublished instrument).
- Raes, F. , Schoofs, H. , Hoes, D. , Hermans, D. , Van Den Eede, F. , & Franck, E. (2009). 'Reflection'en'brooding'als subtypes van rumineren: Een herziening van de Ruminative Response Scale. Gedragstherapie, 42(3/4), 205–214. [Google Scholar]
- Rush, A. J. , Gullion, C. M. , Basco, M. R. , Jarrett, R. B. , & Trivedi, M. H. (1996). The inventory of depressive symptomatology (IDS): Psychometric properties. Psychological Medicine, 26(3), 477–486. [DOI] [PubMed] [Google Scholar]
- Rush, A. J. , Thase, M. E. , & Dubé, S. (2003). Research issues in the study of difficult‐to‐treat depression. Biological Psychiatry, 53(8), 743–753. [DOI] [PubMed] [Google Scholar]
- Shahar, B. , Britton, W. B. , Sbarra, D. A. , Figueredo, A. J. , & Bootzin, R. R. (2010). Mechanisms of change in mindfulness‐based cognitive therapy for depression: Preliminary evidence from a randomized controlled trial. International Journal of Cognitive Therapy, 3(4), 402–418. [Google Scholar]
- Schoofs, H. , Hermans, D. , & Raes, F. (2010). Brooding and reflection as subtypes of rumination: Evidence from confirmatory factor analysis in nonclinical samples using the Dutch Ruminative Response Scale. Journal of Psychopathology and Behavioral Assessment, 32(4), 609–617. [Google Scholar]
- Segal, Z. V. , Williams, J. , & Teasdale, J. (2002). Mindfulness‐based cognitive therapy for depression: A new approach to relapse prevention. New York, NY: Guilford Press. [Google Scholar]
- Segal, Z. V. , Williams, J. M. G. , & Teasdale (2012). Mindfulness‐based cognitive therapy for depression. New York, NY: Guilford Press. [Google Scholar]
- Sheehan, D. V. , Lecrubier, Y. , Sheehan, K. H. , Amorim, P. , Janavs, J. , Weiller, E. , … Dunbar, G. C. (1998). The Mini‐International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM‐IV and ICD‐10. Journal of Clinical Psychiatry, 59, 22–33. [PubMed] [Google Scholar]
- Skevington, S. M. , Lotfy, M. , & O'Connell, K. A. (2004). The World Health Organization's WHOQOL‐BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Quality of Life Research, 13(2), 299–310. [DOI] [PubMed] [Google Scholar]
- Souery, D. , Amsterdam, J. , De Montigny, C. , Lecrubier, Y. , Montgomery, S. , Lipp, O. , … Mendlewicz, J. (1999). Treatment resistant depression: Methodological overview and operational criteria. European Neuropsychopharmacology, 9(1), 83–91. [DOI] [PubMed] [Google Scholar]
- Spijker, J. , De Graaf, R. , Bijl, R. V. , Beekman, A. T. , Ormel, J. , & Nolen, W. A. (2002). Duration of major depressive episodes in the general population: Results from The Netherlands Mental Health Survey and Incidence Study (NEMESIS). The British Journal of Psychiatry, 181(3), 208–213. [DOI] [PubMed] [Google Scholar]
- Strauss, C. , Cavanagh, K. , Oliver, A. , & Pettman, D. (2014). Mindfulness‐based interventions for people diagnosed with a current episode of an anxiety or depressive disorder: A meta‐analysis of randomised controlled trials. PLoS One, 9(4), e96110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thase, M. E. , & Rush, A. J. (1997). When at first you don't succeed: Sequential strategies for antidepressant nonresponders. The Journal of Clinical Psychiatry, 58, 23–29. [PubMed] [Google Scholar]
- Torpey, D. C. , & Klein, D. N. (2008). Chronic depression: Update on classification and treatment. Current Psychiatry Reports, 10(6), 458–464. [DOI] [PubMed] [Google Scholar]
- Trevino, K. , McClintock, S. M. , Fischer, N. M. , Vora, A. , & Husain, M. M. (2014). Defining treatment‐resistant depression: A comprehensive review of the literature. Annals of Clinical Psychiatry, 26(3), 222–232. [PubMed] [Google Scholar]
- van der Velden, A. M. , Kuyken, W. , Wattar, U. , Crane, C. , Pallesen, K. J. , Dahlgaard, J. , … Piet, J. (2015). A systematic review of mechanisms of change in mindfulness‐based cognitive therapy in the treatment of recurrent major depressive disorder. Clinical psychology review, 37, 26–39. [DOI] [PubMed] [Google Scholar]
- van Aalderen, J. R. , Donders, A. R. T. , Giommi, F. , Spinhoven, P. , Barendregt, H. P. , & Speckens, A. E. M. (2011). The efficacy of mindfulness‐based cognitive therapy in recurrent depressed patients with and without a current depressive episode: A randomized controlled trial. Psychological Medicine, 42(05), 989–1001. 10.1017/s0033291711002054 [DOI] [PubMed] [Google Scholar]
- Williams, J. M. G. , Crane, C. , Barnhofer, T. , Brennan, K. , Duggan, D. S. , Fennell, M. J. V. , … Russell, I. T. (2014). Mindfulness‐based cognitive therapy for preventing relapse in recurrent depression: A randomized dismantling trial. Journal of Consulting and Clinical Psychology, 82, 275–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables


