Abstract
Purpose
The purpose of this study was to investigate the safety and efficacy of the combination of robot‐assisted percutaneous screw placement and pelvic internal fixator (INFIX) for minimally invasive treatment of unstable anterior and posterior pelvic ring injuries.
Methods
From September 2016 to June 2017, twenty‐four patients with unstable anterior and posterior pelvic ring injuries were treated with TiRobot‐assisted percutaneous sacroiliac cannulated screw fixation on the posterior pelvic ring combined with robot‐assisted pedicle screw placement in the anterior inferior iliac spine along with INFIX on the anterior pelvic ring. The results of the treatment, including surgery duration, fluoroscopy frequency, total drilling, amount of blood loss, fracture healing time, and postoperative functional outcomes were recorded and compared with another 21 similar patients who underwent conventional manual positioning surgery.
Results
The TiRobot group incurred significantly shorter duration of surgery; less fluoroscopy frequency, intraoperative bleeding, and total drilling than in the conventional group (P < 0.05). Postoperative radiological follow‐up showed that all screws were in the safe area and no screw penetrated the cortex. All wounds healed by primary intention and no iatrogenic damage to the blood vessels, nerves, and organs occurred. Patients showed good tolerance to INFIX and reported no discomfort. The mean follow‐up duration was 5.4 months; the fractures were all healed, no loss of reduction occurred, and the mean Majeed score at the last follow‐up did not show any difference.
Conclusion
TiRobot‐assisted percutaneous screw placement combined with INFIX for the anterior and posterior pelvic ring injuries is accurate, safe, less invasive, and shows satisfactory efficacy, suggesting it is a better method for minimally invasive treatment of unstable pelvic ring fractures.
Keywords: fracture fixation, internal, minimally invasive surgery, pelvis, robotics
1. INTRODUCTION
Unstable pelvic ring fractures often require simultaneous fixation of both the anterior and posterior pelvic rings.1, 2 Traditional fixation methods include external fixation, open reduction internal fixation with plates from the anterior and posterior pathways, and minimally invasive percutaneous screw fixation.3, 4 In recent years, computer navigation or robot‐assisted minimally invasive internal fixation has been increasingly applied in orthopedic surgeries.5, 6 This method shows significantly better accuracy in positioning and less invasiveness, as well as shorter operation time and less radiation damage7, 8, 9 compared with the conventional nonnavigated method. Thus, it has been accepted by an increasing number of orthopedic doctors and promoted in clinical practice.
In this study, the third generation of Chinese manufactured orthopedic robot, the TiRobot system, was introduced in our hospital in September 2016. A total of 24 patients with unstable anterior and posterior pelvic ring injuries underwent TiRobot‐assisted percutaneous internal fixation of both the anterior and posterior pelvic rings with sacroiliac cannulated screw and anterior pelvic internal fixator (INFIX), and satisfactory clinical results were achieved compared with a conventional manual method. The purpose of this study was to investigate the safety and efficacy of this method for minimally invasive treatment of unstable anterior and posterior pelvic ring injuries.
2. MATERIALS AND METHODS
2.1. Patients
Between September 2016 and June 2017, 45 consecutive patients with unstable pelvic injuries were included in a cohort study at the traumatic orthopedics department, the Third People's Hospital of Jinan (P.R. China). They had closed anterior and posterior pelvic ring injuries with or without displacement that could be reduced with closed reduction. The patients comprised 28 males and 17 females aged 22 to 76 years (mean 38.5 years). The body mass index (BMI) of the patients ranged from 21 to 38.7 kg/m2 (mean, 29.4 kg/m2). Injury causes included high‐level fall in 15 cases, car accident in 21 cases, and crush in the remaining 9 cases. Among these patients, 9 had rib fractures, 6 had thoracolumbar fractures, and 5 had urethral ruptures. After admission, patients were monitored for vital signs and venous access was established. Patients were also given urethral catheterization and blood volume expansion therapy (either rehydration or blood transfusion). Patients with unstable hemodynamics were initially treated with temporary pelvic external fixation and admitted to the intensive care unit. Nine patients with sacroiliac joint dislocation were treated with skeletal traction (10–20 kg). All patients routinely received X‐ray, CT scan, and 3D reconstruction. According to the Tile classification, there were 31 type B and 14 type C fractures. In general, 48 h after the injury, when hemodynamic stability was achieved, X‐ray examination was performed to examine the effects of reduction and surgery was conducted from days 3 to 12.
All the patients underwent percutaneous cannulated screw fixation of the sacroiliac joint and INFIX fixation of the anterior pelvic ring. Twenty‐four patients (TiRobot group) treated with robot‐assisted fixation were compared with 21 patients (control group) treated with conventional manual positioning. The groups were similar in age, demographics, and fracture configuration and there was no statistical significance (Table 1).
Table 1.
Patient characteristics of the two groups
| Patient characteristics | TiRobot group (n = 24) | Control group (n = 21) | P |
|---|---|---|---|
| Age (years, ± s) | 37.4 ± 6.6 | 39.8 ± 7.1 | 0.270 |
| Gender (no.) | 0.967 | ||
| Male | 15 | 13 | |
| Female | 9 | 8 | |
| BMI (kg/m2, ± s) | 29.8 ± 2.4 | 28.9 ± 2.7 | 0.174 |
| Injury mechanism (no.) | 0.632 | ||
| Fall | 8 | 7 | |
| Motor | 10 | 11 | |
| Crush | 6 | 3 | |
| Tile classification (no.) | 0.763 | ||
| Type B | 17 | 14 | |
| Type C | 7 | 7 | |
| The duration from injury to operation (days, ± s) | 5.2 ± 2.1 | 5.7 ± 2.3 | 0.371 |
2.2. Surgical equipment
The TiRobot system (TINAVI Medical Technologies Co. Ltd, China), the third generation of the TIANJI™ orthopedic robot, is composed of a robot, spatial calibration components, surgical planning and robot control software, optical tracking system, main control station, and matching tools (Figure 1). A C‐arm X‐ray system (Siemens, Germany) with a 7.3 mm diameter cannulated screw and a rod system (Synthes, Switzerland) with a 6.5 mm diameter pedicle screw were used.
Figure 1.

Overall view of the TiRobot system
The working principle is as follows: the system first imports a few intraoperative 3D images (spine) or 2D images (trauma) into the computer for orthogonal images acquisition. Next, using virtual images generated from fluoroscopic images, the surgeon plans the fixation by placing a virtual guidewire in the appropriate location using a virtual guide sleeve to establish the desired guidewire trajectory. While viewing virtual images with the planned location of the guidewire and the surgical drill, the computer interface finally guides the surgeon during placement of the guidewire in the planned location. Optoelectronic navigation offers advantages for guidewire insertion as both surgical position and guidewire can be viewed in real time without added fluoroscopy use.
2.3. Surgical procedure (TiRobot group)
Patients received general anesthesia with tracheal intubation, and supine position was adopted. The surgical plan was to initially use robot‐assisted percutaneous placement of cannulated screws into the sacroiliac joint for fixation of the posterior pelvic ring and then robot‐assisted percutaneous placement of pedicle screws into the anterior inferior iliac spine along with INFIX for fixation of the anterior pelvic ring. The patient with a left sacral fracture combined with bilateral pubic ramus fracture (Figure 2) is used to exemplify the surgical procedure. The procedure is described as follows:
Figure 2.
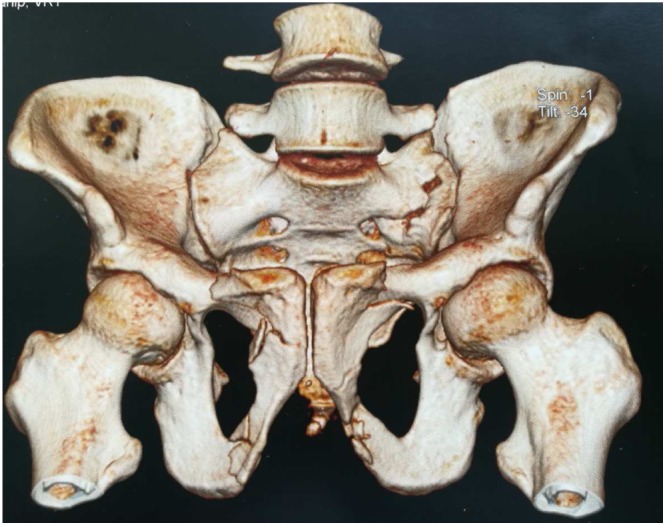
Preoperative CT 3D reconstruction showed bilateral ramus of pubis fractures and left sacrum fracture
(1) Robot‐assisted percutaneous placement of cannulated screws in the left sacroiliac joint for fixation of the posterior pelvic ring: according to the TiRobot system operation process, inlet, outlet, and lateral views were captured for positioning, and the sacroiliac screw placement path was planned according to the patient's anatomical features and fracture status (Figure 3(a)). The S1 of the patient is wide; thus, two screws would be placed in S1. The system automatically calculated and controlled the robotic arm to move to the planned area entering the point next to the posterior superior iliac spine. The drill sleeve was installed, and then moved close to the skin. A 1.5 cm stab incision was made, and the drill sleeve was inserted until the tip was pushed tightly on the bone surface where the screw would be placed. A 2.8 mm guiding needle was inserted through the drill sleeve, and the needle path was confirmed through X‐ray. The same method was used to insert a second guiding needle, and the path was again confirmed through X‐ray (Figure 3(b)). Following confirmation of the right path, a core drill was used to expand the hole. Through each guiding needle, a cannulated screw with a diameter of 7.3 mm and length of 95 mm was screwed in (Figure 3(c)). The position of the screws was again verified through X‐ray. The guiding needles were then retracted, and the skin and subcutaneous tissues were closed.
Figure 3.
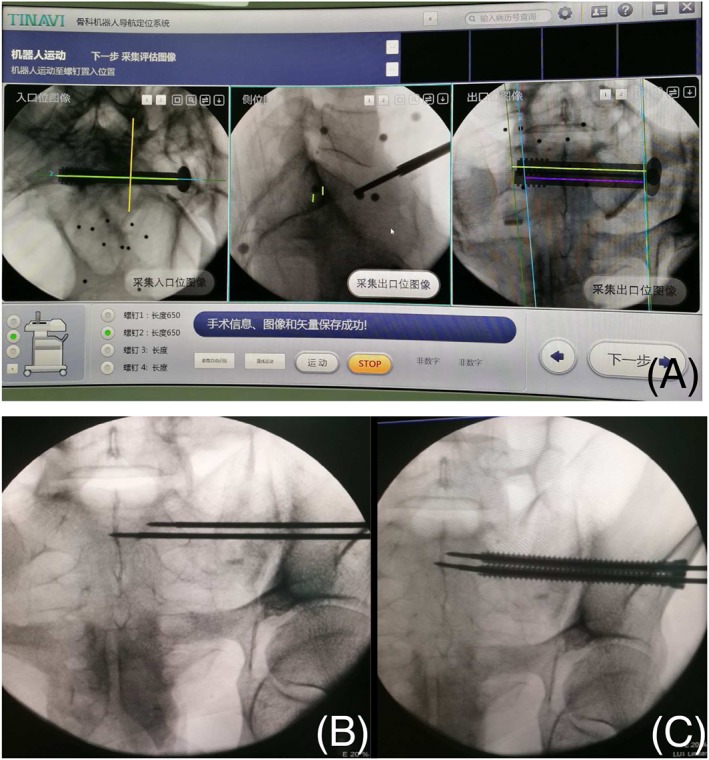
(A) Robot‐assisted path planning of sacroiliac screw placement in S1; (B) guiding needle placement; (C) screw placement along the guiding needle
(2) Robot‐assisted percutaneous placement of pedicle screws in the anterior inferior iliac spine combined with INFIX for fixation of the anterior pelvic ring (left side first, then the right side): the left teardrop (LC‐2 front view) and iliac oblique views were captured for positioning. The placement path for the left pedicle screw was planned according to the anatomical features of the patient (Figure 4(a)). The robot was moved to the predetermined screw placement position, and the drill sleeve was installed. After a stab incision was made, the drill sleeve was inserted until the tip was pushed tightly on the bone surface of the anterior inferior iliac spine. A guiding needle was then inserted, and the X‐ray of the teardrop image was used to confirm the correct needle path. Subsequently, a pedicle screw with a diameter of 6.5 mm and length of 60 mm was screwed in along the guiding needle (Figure 4(b)). X‐ray was again used to verify the screw position. The same method was used for placement of the screw on the right side. When a satisfactory screw position was achieved, a subcutaneous tunnel was established on the planes of pedicle screws of both sides; the connecting rod was then shaped according to the patient's abdomen and placed subcutaneously. The rod was opened properly and fixed in the U‐shaped slots at the end of the screws of both sides. Excess rod length was trimmed in situ with a rod cutter. The wound was then rinsed, and the skin and subcutaneous tissues were sutured. The surgical procedure was complete.
Figure 4.
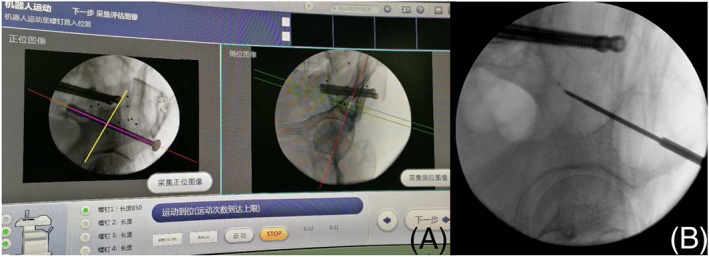
(A) Robot‐assisted path planning of left pedicle screw placement. (B) Screw placement in the anterior inferior iliac spine
2.4. Surgical procedure (control group)
The anesthetic method and surgical sequence in the control group was the same as that in the TiRobot group. The sacroiliac cannulated screws and pedicle screws were inserted and guided using conventional fluoroscopic imaging. The surgeon used a C‐arm fluoroscope in conventional 2D mode. The guiding needles were repeated and adjusted according to the insert location and angle, and were gradually advanced under repeated optimal image intensification in two planes until the optimal anatomical location was reached. After manually measuring the length, a cannulated drill bit was used to make the appropriate canal. The sacroiliac cannulated screws and pedicle screws were then inserted along the guiding needles, following which, the guiding needles were removed and INFIX was placed, and the skin and subcutaneous tissues were sutured.
2.5. Postoperative treatments and follow‐up
The postoperative regimens were similar between groups. Prophylactic anti‐infection treatment was used for 48 hours after the surgery. Meanwhile, the treatment for the prevention of deep vein thrombosis was maintained for 4 weeks. Seventy‐two hours after the surgery, inlet, outlet, and anteroposterior pelvic radiographs, as well as three‐dimensional CT, were repeated. The patients were allowed to turn in bed one week after the surgery. Meanwhile, the patients practiced active contraction of muscles in both the lower limbs and active hip and knee bending. The patients could sit up in 2–3 weeks and perform protected or partial weight‐bearing movements with the help of a walker in 6–8 weeks. At 12–18 weeks, patients could attempt full weight‐bearing walking. The patients were followed up at 4, 8, and 12 weeks for repeated X‐ray, 3D CT examination of the pelvis, and evaluation of screw position and accuracy. Information about patients' daily life activities, including lumbosacral pain, gait, walking distance with a walker, standing, tolerance to INFIX, and presence or absence of nerve damage, was obtained. At the last follow‐up, the Majeed score10 was used to evaluate the functional outcomes.
2.6. Statistical analysis
Quantitative data were expressed as mean ± standard deviation (SD) and were compared using the Student t‐test. Categoric variables were compared using the Pearson X2 test. The P‐value was set <0.05 for significance.
3. RESULTS
Between one and four sacroiliac cannulated screws and two anterior inferior iliac spine pedicle screws were placed in each patient. A total of 86 sacroiliac screws were placed, with an average of 1.9 screws per patient. The number of screw path plannings in the TiRobot group was 3–6 times per patient. The duration of surgery in the TiRobot group was significantly lower than in the control group (50–120 min (mean, 65.4 min) vs 65–160 min (mean, 86.7 min); P < 0.01). Five to eight incisions were made in the TiRobot group with a mean length of 2 cm, which was significantly smaller than the length of the incision in the control group (median 2.5 cm). The robot group incurred significantly less intraoperative bleeding (35.0 ± 7.2 mL versus 46.2 ± 9.3 mL) and lower fluoroscopy frequency (29.2 ± 7.6 times versus 52.3 ± 12.4 times) than the control group (P < 0.01).
In the robot group, all screw placements were successful on the first try, and no symptoms of nerve injury were found after recovery. All wounds healed by primary intention and postoperative X‐ray and CT 3D reconstruction revealed good morphology of pelvic rings (Figure 5). CT scan multiplanar reformation (MPR) showed satisfactory location of the sacroiliac joint screws in the sacroiliac and pedicle screws in the anterior inferior iliac spine (Figure 6); none penetrated the cortex. The Lonstein grade11 on the position of the sacroiliac joint screws was 0. Iatrogenic damage to the blood vessels, nerves, and organs was not detected. No sacroiliac arthritis and loosening, displacement, and fractures of screws were found, and the movement of lower limbs was normal.
Figure 5.
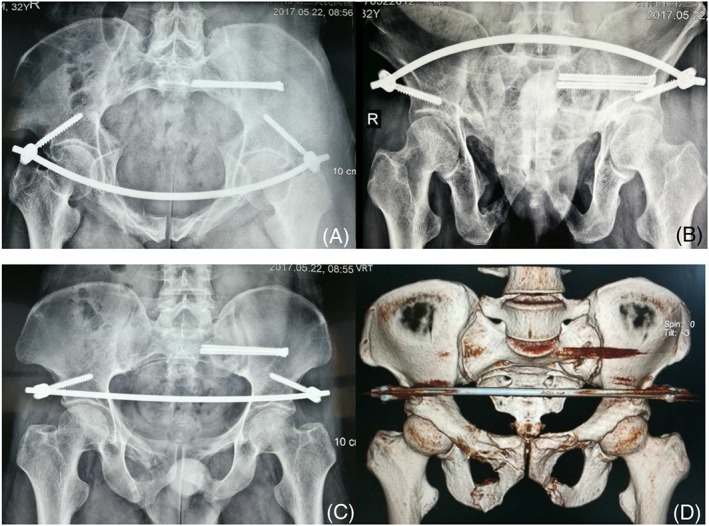
Postoperative X‐ray (A) inlet view, (B) outlet view, (C) anteroposterior view, and (D) CT 3D reconstruction showing good morphology of pelvic rings
Figure 6.
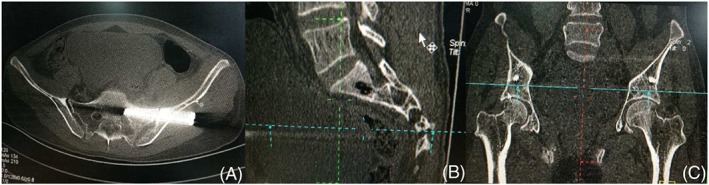
Postoperative CT MPR: (A) transverse view; (B) sagittal view; and (C) coronal view showed the sacroiliac joint screws and the pedicle screws were in the safe area and no screw penetrated bone cortex
In the control group, each screw placement took up to 1 to 6 tries, especially for the placement of sacroiliac screws. The total drilling times were more significant than in the robot group (14.5 ± 6.2 times versus 4.0 ± 0 times, P < 0.01). The screws penetrated the sacroiliac cortex in five patients and three patients incurred sacral nerve injuries, and two patients incurred lateral femoral nerve injuries after recovery. However, the imaging results and the functional outcomes at the last follow‐up were satisfactory.
As for INFIX, the subcutaneous connecting rod and screw cap could be felt by the patients. Patients' tolerance to INFIX was good, and no discomfort was reported. INFIX was removed upon full weight‐bearing movement at 16–18 weeks after the surgery when the pelvic ring fractures were considered healed.
All patients were followed up for 4–12 months, with an average of 5.4 months. Fractures were healed within 3 months after the surgery, and no loss of reduction was found. There was no significant difference between the two groups in fracture healing time (4.3 ± 0.7 months versus 4.5 ± 1.1 months) and Majeed scores at the last follow‐up (86.4 ± 7.2 points versus 84.3 ± 10.3 points). Comparison of the results for the two groups is shown in Table 2.
Table 2.
Results comparison between the two groups
| Results | TiRobot group (n = 24) | Control group (n = 21) | P |
|---|---|---|---|
| Surgery duration (min) | 65.4 ± 10.9 | 86.7 ± 14.7 | < 0.001 |
| Fluoroscopy frequency (no.) | 29.2 ± 7.6 | 52.3 ± 12.4 | < 0.001 |
| Total drilling times (no.) | 4.0 ± 0 | 14.5 ± 6.2 | < 0.001 |
| Intraoperative bleeding (mL) | 35.0 ± 7.2 | 46.2 ± 9.3 | < 0.001 |
| Fracture healing time (month) | 4.3 ± 0.7 | 4.5 ± 1.1 | 0.450 |
| Majeed score (point) | 86.4 ± 7.2 | 84.3 ± 10.3 | 0.430 |
4. DISCUSSION
Unstable pelvic fractures are often caused by injuries of both the anterior and posterior pelvic rings. Ward et al.12 proposed that internal fixation on both the anterior and posterior pelvic rings can stabilize the pelvic ring to a certain degree, and the biomechanical properties are similar to those of the normal pelvis.
Traditional fixation methods for posterior pelvic ring injuries include external fixation, posterior internal fixation with a plate, and minimally invasive percutaneous sacroiliac screw fixation.3, 5 Traditional surgery achieves the best anatomic reduction and provides strong fixation. However, its drawbacks include severe surgical trauma, more bleeding, and common damage to critical vessels and nerves, which will influence postoperative recovery. For complex anterior and posterior pelvic ring injuries, surgery with combined anterior and posterior path causes great trauma, and intraoperative body turning can influence the operation. Performing early functional exercises is difficult for patients; thus, it does not meet the new trend of minimal invasiveness.
X‐ray‐guided percutaneous sacroiliac screw fixation is a minimally invasive treatment for posterior pelvic ring injures. Biomechanical studies have shown that the sacroiliac screw fixation of the posterior pelvic ring exhibits reliable mechanical strength and can provide consistent pelvic stability.13, 14 However, under X‐ray monitoring, ensuring the best position of each screw is difficult through manual operation and the accuracy varies because of individual differences and inconsistenies. The failure rate of sacroiliac screw placement is 2–13%.5 For patients with dysmorphic sacrum, fluoroscopical guidance alone cannot guarantee that the screws will remain in the bone channel and cannot ensure safe operation. Moreover, repeated X‐ray exposures increase radioactive damage to the patient and medical personnel. 3D fluoroscopy‐based navigation is undoubtedly the best choice for percutaneous sacroiliac screw fixation.15, 16
In recent years, the application of computer‐assisted 3D navigation and medical robots in orthopedic surgery has greatly increased.5, 6 https://www.ncbi.nlm.nih.gov/pubmed/25683211). The TiRobot, which was independently developed in China, is the latest advanced orthopedic robotic system. This robotic system uses a modular, small, and universal design. It achieves a breakthrough in surgical platform technology and extends indications to the spine, traumatic orthopedic internal fixation with cannulated screws, and the positioning accuracy reaches 0.6–0.8 mm. In this study, TiRobot‐assisted sacroiliac screw fixation for the posterior pelvic ring showed satisfactory results. It has four main features. The first feature is accurate positioning. The robot provides precise spatial positioning and a stable path of insertion. Through movement of the robotic arm, screws were placed accurately, safely, and stably in the corresponding anatomical sites. None of the screws penetrated the cortex. The second feature is shorter operation time. The real‐time optical tracking technology makes repetition of X‐ray unnecessary during the operation, increasing the flexibility and fluency of the operation, shortening the operation time, and improving the operation efficiency. The third feature is reduced radiation damage. Compared with manual screw placement, robotic navigation significantly reduced the number of intraoperative X‐ray perspective examinations, thus significantly reducing the intraoperative cumulative radiation dosage. The final feature is programmed surgical procedures. During surgery, operation planning and path positioning are completed with a reminder system, which guides the doctor to complete the operation efficiently and safely.
For the anterior pelvic ring injury, traditional fixation methods include external fixation, open reduction and internal fixation with a plate, and X‐ray‐guided pubic ramus screw fixation.4 For complex fractures of the anterior ring (bilateral pubic and ischial rami fractures), maintaining reduction and stability of the anterior pelvic ring is difficult during screw placement. In addition to open surgery (such as the Stoppa approach), external fixation is still the major approach in these fractures. Pelvic external fixation is the earliest approach used for the treatment of pelvic injuries and is often used in patients in an emergency as a temporary fixation. It is easy to operate and causes less trauma; however, it has risks including needle path infection, loosening, and fixation failure. It also causes inconvenience for patients when changing clothes and performing other daily activities. The INFIX, which was described and named by Validya et al.9 in 2011, is a new minimally invasive internal fixation method for treating unstable pelvic fractures. It causes less trauma, has only a slight influence on the patients' daily life, and is particularly appropriate for obese patients.9, 17 Moreover, with this method, a small incision is made, and the pedicle screw is manually inserted between the inner and outer cortices of ilium and directed from the anterior inferior iliac spine toward the posterior superior iliac spine based on experience. The iliac internal and external bone lamellae in this area are thick; the screw will not usually penetrate the iliac cortex. Thus the technical requirements for this method are not high. However, for obese patients, blunt dissection of the subcutaneous fascia may cause large trauma and damage to the lateral femoral cutaneous nerve. Vaidya18, 19, 20 proposed its indications including anterior pelvic injury with high, low, or bilateral rami fractures. All 45 patients in this study all had complex bilateral anterior pelvic ring fracture and received INFIX. We used TiRobot in 24 patients for the first time to assist the placement of pedicle screws into the anterior inferior iliac spine; TiRobot accurately guided the surgeon to the pre‐planned location; the operation is simpler and more accurate, and results in less trauma. No complications, such as lateral femoral nerve injury, occurred. Moreover, care for INFIX placement is simple, and complications, such as needle path infection, loosening, and fixation failure, are avoidable. Patients feel more comfortable, their daily activities are not influenced,9, 19, 20, 21 and the efficacy is satisfactory.
Surgical indications and precautions: Closed anterior and posterior pelvic ring injuries but without severe visceral injury and without fracture displacement or with fracture displacement that can be easily treated with closed reduction are all indications for operation. Patients with severe visceral injuries, such as bladder rupture, intestinal perforation, and urethral rupture, require acute laparotomy, and obvious wound contamination is its contraindication. Five patients in this group had urethral rupture. After successful catheterization, the patients were included in the study. If catheterization is difficult and open urethra realignment with traction or a first‐phase repair is necessary, INFIX should not be placed. The surgical order is fixation of the posterior ring first, followed by fixation of the anterior ring. For patients with vertical instability, skeletal traction with heavy weight can usually correct the vertical displacement of fractures. For patients with no significant improvement after traction (sacral fracture displacement >10 mm), posterior lumbo‐iliac screws and rod can be used during the surgery to assist sacral fracture reduction. External fixation can be used in patients with rotational instability for temporary reduction and fixation. In cases of lateral compression injuries with rotational instability and pubic rami fracture displacement >10 mm, the internal fixator is applied and the lateral compression component of injury is distracted to reestablish the configuration of the pelvis after the posterior injury is fixed.
Robot defects and study limitation: First, the path planning of screw placement still relies on the experience of surgeons, and there may be subjective errors. Second, a drill sleeve that is too long with high lateral stress may lead to deviation of the tip of the guiding needle. Third, the cost of equipment ($2 million) is relatively high and needs special personnel training. Finally, we performed this operation for a short time and in a relatively small number of patients. Further research is needed with prospective randomized controlled studies with a large number of patients and long follow‐up to highlight its benefits.
5. CONCLUSIONS
Percutaneous sacroiliac screw fixation combined with INFIX is a good method of stabilizing the pelvic ring. TiRobot‐assisted percutaneous screw placement at the sacroiliac joint and placement of anterior superior iliac pedicle screws are accurate and minimally invasive. This method can also avoid injury and result in less radiation damage. The minimally invasive fixation combined with sacroiliac screw fixation of the posterior pelvic ring and the INFIX of the anterior pelvic ring effectively maintains the stability of the pelvic ring, obtains satisfactory clinical results, and greatly reduces the incidence of complications of open surgery. We believe that the combined application of TiRobot and INFIX is a potential minimally invasive approach to treat complex unstable anterior and posterior pelvic ring injuries.
FUNDING
This study has no funding sources to declare.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
ETHICAL APPROVAL
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
INFORMED CONSENT
Informed consent was obtained from all individual participants included in the study.
Liu H, Duan S, Liu S, Jia F, Zhu L, Liu M. Robot‐assisted percutaneous screw placement combined with pelvic internal fixator for minimally invasive treatment of unstable pelvic ring fractures. Int J Med Robotics Comput Assist Surg. 2018;14:e1927 10.1002/rcs.1927
REFERENCES
- 1. Tile M. The management of unstable injuries of the pelvic ring. J Bone Joint Surg Br. 1999;81(6):941‐943. [DOI] [PubMed] [Google Scholar]
- 2. Van den Bosch EW, Van der Kleyn R, Hogervorst M, Van Vugt AB. Functional outcome of internal fixation for pelvic ring fractures. J Trauma. 1999;47(2):365‐371. [DOI] [PubMed] [Google Scholar]
- 3. Stevenson AJ, Swartman B, Bucknill AT. Percutaneous internal fixation of pelvic fractures. German version. Unfallchirurg. 2016;119(10):825‐834. [DOI] [PubMed] [Google Scholar]
- 4. Zhou KH, Luo CF, Chen N, Hu CF, Pan FG. Minimally invasive surgery under fluoro‐navigation for anterior pelvic ring fractures. Indian J Orthop. 2016;50(3):250‐255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gautier E, Bächler R, Heini PF, Nolte LP. Accuracy of computer‐guided screw fixation of the sacroiliac joint. Clin Orthop Relat Res. 2001;393:310‐317. [DOI] [PubMed] [Google Scholar]
- 6. Zheng G, Nolte LP. Computer‐assisted orthopedic surgery: current state and future perspective. Front Surg. 2015;23:2‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Stöckle U, Schaser K, König B. Image guidance in pelvic and acetabular surgery‐expectations, success and limitations. Injury. 2007;38(4):450‐462. [DOI] [PubMed] [Google Scholar]
- 8. Zwingmann J, Konrad G, Kotter E, Südkamp NP, Oberst M. Computer‐navigated iliosacral screw insertion reduces malposition rate and radiation exposure. Clin Orthop Relat Res. 2009;467(7):1833‐1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wong JM, Bewsher S, Yew J, Bucknill A, de Steiger R. Fluoroscopically assisted computer navigation enables accurate percutaneous screw placement for pelvic and acetabular fracture fixation. Injury. 2015;46(6):1064‐1068. [DOI] [PubMed] [Google Scholar]
- 10. Majeed SA. Grading the outcome of pelvic fractures. J Bone Joint Surg Br. 1989;71(2):304‐306. [DOI] [PubMed] [Google Scholar]
- 11. Lonstein JE, Denis F, Perra JH, Pinto MR, Smith MD, Winter RB. Complications associated with pedicle screws. J Bone Joint Surg Am. 1999;81(11):1519‐1528. [DOI] [PubMed] [Google Scholar]
- 12. Ward EF, Tomasin J, Vander Griend RA. Open reduction and internal fixation of vertical shear pelvic fractures. J Trauma. 1987;27(3):291295. [DOI] [PubMed] [Google Scholar]
- 13. Giráldez‐Sánchez MA, Lázaro‐Gonzálvez Á, Martínez‐Reina J, et al. Percutaneous iliosacral fixation in external rotational pelvic fractures. A biomechanical analysis. Injury. 2015;46(2):327‐232. [DOI] [PubMed] [Google Scholar]
- 14. Zhang L, Peng Y, Du C, Tang P. Biomechanical study of four kinds of percutaneous screw fixation in in two types of unilateral sacroiliac joint dislocation: a finite element analysis. Injury. 2014;45(12):2055‐2059. [DOI] [PubMed] [Google Scholar]
- 15. Thakkar SC, Thakkar RS, Sirisreetreerux N, Carrino JA, Shafiq B, Hasenboehler EA. 2D versus 3D fluoroscopy‐based navigation in posterior pelvic fixation: review of the literature on current technology. Int J Comput Assist Radiol Surg. 2017;12(1):69‐76. [DOI] [PubMed] [Google Scholar]
- 16. Matityahu A, Kahler D, Krettek C, et al. Three‐dimensional navigation is more accurate than two‐dimensional navigation or conventional fluoroscopy for percutaneous sacroiliac screw fixation in the dysmorphic sacrum: a randomized multicenter study. J Orthop Trauma. 2014;28(12):707‐710. [DOI] [PubMed] [Google Scholar]
- 17. Vaidya R, Martin AJ, Roth M, Nasr K, Gheraibeh P, Tonnos F. INFIX versus plating for pelvic fractures with disruption of the symphysis pubis. Int Orthop. 2017;41(8):1671‐1678. [DOI] [PubMed] [Google Scholar]
- 18. Vaidya R, Kubiak EN, Bergin PF, et al. Complications of anterior subcutaneous internal fixation for unstable pelvis fractures: a multicenter study. Clin Orthop Relat Res. 2012;470(8):2124‐2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Vaidya R, Onwudiwe N, Roth M, Sethi A. Monoaxial pedicle screws are superior to polyaxial pedicle screws and the two pin external fixator for subcutaneous anterior pelvic fixation in a biomechanical analysis. Adv Orthop. 2013;2013(411):683120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Eagan M, Kim H, Manson TT, et al. Internal anterior fixators for pelvic ring injuries: do monaxial pedicle screws provide more stiffness than polyaxial pedicle screws? Injury. 2015;46(6):996‐1000. [DOI] [PubMed] [Google Scholar]
- 21. Vigdorchik JM, Esquivel AO, Jin X, Yang KH, Vaidya R. Anterior internal fixator verses a femoral distractor and external fixation for sacroiliac joint compression and single stance gait testing: a mechanical study in synthetic bone. Int Orthop. 2013;37(7):1341‐1346. [DOI] [PMC free article] [PubMed] [Google Scholar]


