Abstract
Introduction
Limited attention has been paid to the use of contraception in relation to women's family planning intentions. The aim of this study was to investigate the use of contraception during the most recent intercourse as well as the reproductive intentions of Swedish‐speaking women requesting contraceptive counseling.
MATERIAL AND METHODS
A cross‐sectional baseline survey in a randomized controlled trial regarding reproductive life planning (before randomization). Women requesting contraceptive counseling answered questions about contraception and whether they wanted to have children/more children in the future.
Results
In total, 1946 women participated: 33.7% (n = 656) parous and 65.7% (n = 1279) nulliparous. The majority, 87.1% (n = 1682), had used contraception during their latest intercourse; 64.6% (n = 1239) used short‐acting reversible contraception, 22.8% (n = 443) used long‐acting reversible contraception (LARC), and 12.9% (n = 251) had not used any contraception. A combined oral contraceptive was more common among nulliparous and LARC among parous. Among all women, 64.8% (n = 1253) intended to have children/more children in the future, among parous women 35.7% (n = 220) and among nulliparous 80.0% (n = 1033). Among women who did not intend to have children/more children, 22.6% (n = 60) of parous and 10% (n = 8) of nulliparous had not used contraceptives during their most recent intercourse.
Conclusions
Women did not always use contraceptives that were suitable for their reproductive intentions. Questioning women who request contraceptive counseling about their pregnancy intention can give healthcare providers better opportunities for individualized counseling.
Keywords: contraception, counseling, long‐acting reversible contraception, preconception care, reproductive health, unintended pregnancy, unplanned pregnancy
Abbreviations
- COC
combined oral contraceptive pills
- LARC
long‐acting reversible contraception
- RNM
registered nurse midwives
Key Message.
Women often do not use contraceptives that are suitable for their reproductive intentions. Women's reproductive intentions need to be understood by their counselor.
1. INTRODUCTION
Oral contraceptives have been available as a highly effective method to prevent unwanted pregnancies for more than half a century. Currently, women have a choice between different types of contraceptive methods, but in 2012, 40% of all pregnancies worldwide were still unintended. It is estimated that of these pregnancies, 50% ended in an abortion, 13% in a miscarriage, and 38% in an unplanned birth.1 Women with unintended pregnancies were less likely to take the recommended amount of preconception folic acid and to breastfeed for 8 weeks or more, but were more likely to smoke prenatally and postpartum,2 and to suffer from postpartum depression.3 Low birthweight and preterm births were also more common with unintended pregnancies.4
Many countries issue evidence‐based recommendations for healthcare providers for up‐to‐date contraceptive counseling.5, 6, 7 The Swedish national guidelines were revised in the spring of 2014. These revised guidelines indicate that maintaining women's fertility is as important as preventing unplanned pregnancies. Long‐acting reversible contraceptive methods (LARC), such as intrauterine devices and implants, fulfill these goals for nulliparous young women by providing high compliance and resulting in effective contraception for several years.7, 8 Trussel et al9 noted the difference in effectiveness between “perfect use” (= high compliance) and “typical use,” where pregnancy rates are higher for “typical users” of most contraceptives, except for LARC.9
In Sweden, registered nurse midwives (RNM) are licenced to prescribe contraceptives to healthy women.7 However, as women with risk factors also seek midwives for contraceptive counseling, the midwife is supposed to contact or refer these women to gynecologists or general practitioners. Approximately 80% of contraceptive counseling is performed by RNMs, 1% by gynecologists, and 5% by general practitioners.10 Family planning services are free of charge, and contraceptives are subsidized for young women; however, unintended pregnancies continue to be at a constant high level. The rate of induced abortions in Sweden fluctuates around approximately 20 of 1000 women aged 15‐45 years old.11 Women's use of contraception has been studied in a Swedish nationwide telephone survey, showing that 70% currently used contraception and 22% had experienced unintended pregnancies, of which 40% ended in an induced abortion.12 Another Swedish survey on female university students engaging in contraceptive counseling showed that 95% used contraception during their most recent intercourse, and 7% had experienced an induced abortion. In this group, 9 of 10 women intended to have children in the future.13 Studies that have investigated women's use of contraception in relation to their future reproductive intentions have involved other populations and have usually examined selected groups.14, 15, 16
It is unknown whether or how contraceptive counseling can be further improved by identifying groups that might benefit from adapted counseling. The aim of this study was to investigate women's use of contraception and reproductive intentions among Swedish‐speaking women visiting nurse midwives for contraceptive counseling.
2. MATERIAL and METHODS
The present cross‐sectional study is part of a baseline survey before a randomized controlled trial about reproductive life planning (RLP). Recruitment was carried out between February 2015 and March 2016 at 28 clinics for contraceptive counseling in one county in central Sweden. The county has one university town, small cities, and rural areas. The female population in the county has an economic and educational level similar to that of Sweden's overall female population. Smoking among women is akin to that of the whole of Sweden (http://www.scb.se/en). In total, 86 RNMs were employed at these clinics and assisted in the data collection. Women were informed about the survey when they booked an appointment for contraception counseling. Inclusion criteria were: being 20‐40 years old, and being able to read and understand Swedish. Initially, youth centers were not included in the study because their age group was limited to 20 years. As the centers became open to ages up to 23, after half of the study period, we also included the youth centers; however, only a few women aged 20‐23 visited these clinics during the study period.
Women received written information about the study in the waiting room. If they had any questions, the RNMs provided further information about the study. An informed consent form was signed prior to participation in the study. Before the counseling, the participants were instructed to take an envelope containing a baseline questionnaire, complete it, and put it in a sealed envelope, which was to be given to the RNM.
The baseline questionnaire consisted of 41 questions that were mainly multiple choice. The bulk of the questions had previously been used in a study on female university students’ RLP by Stern et al.16 Before our final version, we conducted a pilot study using the questionnaire on women attending contraceptive counseling; as a result, a few questions were modified.
In this study, we present the results of questions posed to women regarding their current use of contraception and reproductive intentions.
2.1. Demographics and background
The first part of the survey covered questions about age, height, weight, country of birth, education, employment, relationship stability, sexual orientation, smoking and snuff habits, sexually transmitted infections, and previous pregnancies.
2.2. Contraception and reproductive intentions
The second part consisted of questions about the use of contraception during their most recent intercourse, and reproductive intentions. The questions about reproductive intentions were as follows:
“Do you want to have children/more children in the future?” (yes/no/do not know). An affirmative response was followed by three questions with an open‐ended response format: “How many children do you want?” “At what age would you like to/did you have your first child?” and “At what age would you like to have your last child?,” followed by “What is the probability that you will have an unintended pregnancy at some point?” (Very likely, quite likely, quite unlikely, very unlikely). The questions were inspired by those used by Jack et al16 in their article about clinical content of preconception care17 and was also used in a previous study about RLP. 16
2.3. Power estimation
Power (80% power and type I error 0.05 and assuming a dropout rate of 20%) was calculated for both short‐term outcomes and for a future follow up of the randomized controlled trial. With the assumption that the intervention would increase knowledge of the importance of folic acid use prior to pregnancy, 100 individuals would be needed in each arm. According to the assumption, the intervention would decrease the hazardous use of alcohol by 50% in a future pregnancy. It was determined that 1000 women were needed in both the intervention and control groups. To be able to follow up these women subsequently, with adequate power for outcomes, the latest power calculation was chosen.
2.4. Statistical analyses
Information about participants’ demographics and responses to the questions were presented using the mean and standard deviation (SD) for normally distributed continuous variables, the median and interquartile range for continuous variables with a skewed distribution, and frequencies with corresponding percentages for categorical variables. Differences between the different subgroups were compared using Mann‐Whitney U or Kruskal‐Wallis test for continuous variables, and chi‐square test or Fisher's exact test for categorical variables. All statistical analyses were performed using SPSS Statistics version 20.0 (IBM Corp., Armonk, NY, USA). A two‐sided P‐value < 0.05 was considered statistically significant.
2.5. Ethical approval
The Regional Ethical Review Board in Uppsala, Sweden approved the study (D.nr 2012/101). The study was registered in ISRCTN 32 759.
3. RESULTS
A flowchart of the patient recruitment is shown in Figure 1. Of 3056 eligible women, 1946 (64%) participated in the study. Most of the questions in the survey were carefully filled in, with an internal response rate of 99.3‐99.8%.
Figure 1.
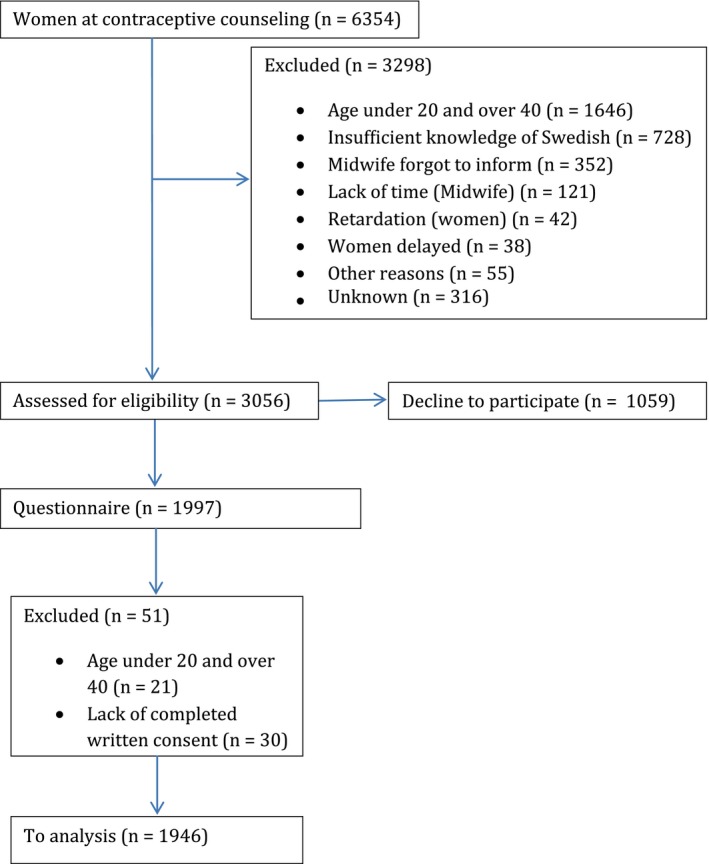
Flowchart of patient recruitment [Color figure can be viewed at http://www.wileyonlinelibrary.com
The midwives noted the reasons for lack of participation if the women spontaneously gave an explanation for this. Reasons for nonparticipation were spontaneously reported by 313 women (28%) and included: lack of time, having small children accompanying them, disliking investigations or not being interested.
3.1. Background of the study population
Background characteristics are described in Table 1. The median age of all women was 25 years; 32 years for parous vs 23 years for nulliparous (P < 0.001).
Table 1.
Demographic background in study population (women attending contraceptive counseling)
| Total n = 1946 | ||
|---|---|---|
| n | % | |
| Education | ||
| Non‐completed education | 14 | 0.7 |
| Elementary school (9 years) | 82 | 4.2 |
| High school (12 years) | 1145 | 58.8 |
| Higher professional education | 159 | 8.2 |
| College/university | 543 | 27.9 |
| Missing | 3 | 0.2 |
| Main occupation | ||
| Working | 1105 | 56.8 |
| Student | 535 | 27.5 |
| Parental leave | 171 | 8.8 |
| Unemployed | 66 | 3.4 |
| Sick leave | 52 | 2.7 |
| Other | 14 | 0.7 |
| Missing | 3 | 0.2 |
| Country of birth | ||
| Sweden | 1798 | 92.4 |
| Other Nordic country | 14 | 0.7 |
| Other European country | 50 | 2.6 |
| Outside Europe | 74 | 3.8 |
| Missing | 10 | 0.5 |
| Sexual orientation | ||
| Heterosexual | 1823 | 93.7 |
| Bisexual | 80 | 4.1 |
| Homosexual | 1 | 0.1 |
| Don't know/unsure | 21 | 1.1 |
| Other | 7 | 0.4 |
| Missing | 14 | 0.7 |
| Incidence of sexually transmitted diseases (STI) | ||
| No STI | 1333 | 68.5 |
| Chlamydia | 432 | 22.2 |
| Condyloma | 151 | 7.8 |
| Herpes | 93 | 4.8 |
| Gonorrhea | 6 | 0.3 |
| Other | 21 | 1.1 |
| Missing | 11 | 0.6 |
| Reproduction | ||
| Had tried to get pregnant | 652 | 33.5 |
| Had been pregnant | 881 | 45.3 |
| Had given birth | 656 | 33.7 |
| Experience of abortion | 280 | 14.4 |
| Experience of miscarriage | 112 | 5.8 |
| Smoking | ||
| Smoking daily | 199 | 10.2 |
| Smoking, but not daily | 221 | 11.4 |
| Former smokers | 429 | 22 |
| Never smoked | 1077 | 55.3 |
| Missing | 20 | 1 |
| Swedish snuff | ||
| Snuff daily | 126 | 6.5 |
| Use snuff but not daily | 81 | 4.2 |
| Former user of snuff | 157 | 8.1 |
| Never used snuff | 1563 | 80.3 |
| Missing | 19 | 1 |
| Drinking alcohol, 4 standard glasses or more at the same timea | ||
| Never | 360 | 18.5 |
| Less than once/month | 972 | 49.9 |
| Once/month | 495 | 25.4 |
| Once/week | 94 | 4.8 |
| Daily | 1 | 0.1 |
| Missing | 24 | 1.2 |
| BMI | ||
| Underweight | 267 | 13.7 |
| Normal weight | 1042 | 53.5 |
| Overweight | 430 | 22.1 |
| Obesity | 152 | 7.8 |
| Missing | 55 | 2.8 |
One standard glass is: Beer (≤3.5%) 50 cL, beer (>3.5%) 33 cL, wine (8‐15%) 12‐15 cL, wine (15‐22%) 8 cL or liquor (4 cL).
Almost half of the women (n = 881) had been pregnant. Of these, 74.5% had given birth, 32.9% had experienced an induced abortion, and 12.9% had experienced a miscarriage. The women did not have the opportunity to choose “ectopic pregnancy” in the questionnaire. One woman had written “ectopic pregnancy” as free text. Three of four women (75.8%, n = 1476) were in a stable relationship. The experience of sexually transmitted infections was more common among daily smokers (45.7%) than nonsmokers (29.2%) (P < 0.001).
3.2. Reproductive intentions
Two‐thirds of the women (64%, n = 1253) wanted to have children/more children, 17.8% (n = 347) stated that they did not want to have children/more children, and 17.2% (n = 335) were unsure. In Table 2, the reproductive intentions of parous and nulliparous women are described. Of the nulliparous women, 2 of 10 were uncertain or did not want to have children.
Table 2.
Reproductive intentions by women attending contraceptive counseling
| Nulliparous | Parous | P | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Want to have children/more children | |||||
| Yes | 1033 | 80.7 | 220 | 33.5 | |
| No | 81 | 6.3 | 266 | 40.4 | |
| Don't know | 165 | 12.9 | 170 | 25.9 | <0.000 |
| Desired age for having the last child | |||||
| ≤25 | 4.9 | 48 | 8.5 | 20 | |
| 26–30 | 21.6 | 213 | 32.9 | 77 | |
| 31–35 | 54.9 | 541 | 40.2 | 94 | |
| 36–40 | 17.8 | 176 | 17.5 | 41 | |
| >40 | 0.8 | 8 | 0.9 | 2 | <0.000 |
The nulliparous women wished to have their first child at a median age of 28 years (25th percentile = 26 and 75th percentile = 30) compared with the actual age of 25 years for parous women. The median age desired for having the last child was 34 years (25th percentile = 30 and 75th percentile = 35). Nulliparous women wanted to have 2.4 children (SD 0.6) and parous women 2.6 children (SD 0.7).
3.3. Contraception during their most recent intercourse
The use of contraception among women was also calculated based on parity (nulliparous women and parous women), as described in Table 3 (n = 706). Of all women, 36.3% (n = 706) used combined hormonal contraceptive pills (COC), and 22.8% (n = 443) used LARC. The nulliparous women used COC more frequently, and the parous women used LARC more frequently. Almost 2 of 10 women (18.1%) used condoms, either in combination with other contraceptives or as the only contraception (14.0%). The use of condoms was more common among women who were not in a stable relationship (27.2%, n = 123) than among women in a stable relationship (15.2%, n = 224, P < 0.001).
Table 3.
Women's reported contraception use during their most recent intercourse by parity
| Nulliparous | Parous | P | |||
|---|---|---|---|---|---|
| Total n = 1278 | Total n = 655 | ||||
| n | % | n | % | ||
| No method | 122 | 9.5 | 129 | 19.7 | <0.001 |
| LARC | 215 | 16.7 | 228 | 34.8 | <0.001 |
| Hormonal intrauterine device | 42 | 3.3 | 93 | 14.2 | <0.001 |
| Copper intrauterine device | 42 | 3.3 | 91 | 13.9 | <0.001 |
| Progestin implant contraception | 131 | 10.3 | 44 | 6.7 | 0.01 |
| Combined hormonal contraceptive pill | 565 | 44.2 | 141 | 21.5 | <0.001 |
| Combined hormonal contraceptive ring | 94 | 7.4 | 23 | 3.5 | <0.001 |
| Progestin‐only pill | 68 | 5.3 | 35 | 5.3 | 0.983 |
| Progestin‐only injection | 8 | 0.6 | 10 | 1.5 | 0.051 |
| Condom | 252 | 19.7 | 97 | 14.8 | 0.008 |
| Other | 21 | 1.6 | 10 | 1.5 | 0.983 |
LARC, long‐acting reversible contraception.
Nonuse of contraception during their most recent intercourse was reported by 12.9% (n = 251) of all women and by 20.1% (n = 91) women without a stable relationship compared with 10.8% (n = 159) in a stable relationship (P < 0.001). Nonuse of contraceptives was also more common among parous women (19.7%, n = 129) than among nulliparous women (9.5%, (n = 122) (P < 0.001).
Table 4 shows contraceptive use during the most recent intercourse for nulliparous and parous women by reproductive intentions. There was no difference in LARC use among parous women who did or did not want more children. However, the parous women who intended to have more children or were unsure were more likely to use copper intrauterine devices (16.9%) and progestin implant (8.5%) and less likely to use hormonal intrauterine devices (11.8%) than were parous women who did not want more children (9.4%, 4.2%, and 17.7%, respectively).
Table 4.
Nulliparous and parous women's reported contraception use during their latest intercourse by reproductive intentions
| Nulliparous (n = 1269) | Parous (n = 656) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Want children/don't know | Do not want children | P | Want more children/don't know | Do not want more children | P | |||||
| Total n = 1026 | Total n = 80 | Total n = 220 | Total n = 265 | |||||||
| n | % | n | % | n | % | n | % | |||
| No method | 112 | 9.4 | 8 | 10.0 | 0.864 | 69 | 17.7 | 60 | 22.6 | 0.118 |
| LARC | 197 | 16.4 | 17 | 21.0 | 0.289 | 145 | 37.2 | 83 | 31.2 | 0.115 |
| Hormonal intrauterine device | 34 | 2.9 | 8 | 10.0 | 0.001 | 46 | 11.8 | 47 | 17.7 | 0.033 |
| Copper intrauterine device | 39 | 3.3 | 3 | 3.8 | 1.000a | 66 | 16.9 | 25 | 9.4 | 0.007 |
| Progestin implant contraception | 124 | 10.4 | 6 | 7.5 | 0.536a | 33 | 8.5 | 11 | 4.2 | 0.031 |
| Combined hormonal contraceptive pill | 536 | 45.1 | 27 | 33.8 | 0.048a | 82 | 21.0 | 59 | 22.3 | 0.705 |
| Combined hormonal contraceptive ring | 88 | 7.4 | 6 | 7.5 | 1.000a | 17 | 4.4 | 6 | 2.3 | 0.222a |
| Progestin only pill | 60 | 5.0 | 8 | 10.0 | 0.057 | 26 | 6.7 | 9 | 3.4 | 0.068 |
| Progestin only injection | 4 | 0.3 | 4 | 5.0 | 0.002a | 3 | 0.8 | 7 | 2.6 | 1.000a |
| Condom | 234 | 19.7 | 14 | 17.5 | 0.634 | 53 | 13.6 | 44 | 16.6 | 0.286 |
| Other | 18 | 1.5 | 2 | 2.5 | 0.726a | 8 | 2.1 | 2 | 0.8 | 0.316a |
LARC, long‐acting reversible contraception.
Doubled one‐sided P‐value of Fisher's exact test.
Among women with an experience of abortion, 33.9% (n = 95) used LARC and 21.8% COC, and 14.3% (n = 40) did not use any contraceptive method.
Among women who were daily smokers, an implant was twice as common as in nonsmokers (15.4% vs 7.8%; P < 0.001). Daily smokers used COC less frequently than nonsmokers (27.0% vs 38.4%; P < 0.001).
3.4. Women's thoughts about the probability of future unplanned pregnancies
Overall, 15% of the women believed that an unplanned pregnancy was very likely or quite likely sometime in their future. This was more common among women who did not use contraceptives during their most recent intercourse and women with experience of an induced abortion. The proportions for different groups are presented in Table 5.
Table 5.
Women's thoughts about the probability of an unplanned pregnancy in the future
| Very probable | Quite likely | Quite unlikely | Very unlikely | P | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Nulliparous | 25 | 2.0 | 140 | 11.0 | 791 | 62 | 320 | 25.1 | |
| Parous | 31 | 4.8 | 86 | 13.3 | 294 | 45.4 | 236 | 36.5 | <0.001 |
| Women without any use of contraceptives during their recent intercourse | 12 | 4.8 | 65 | 26.2 | 127 | 51.2 | 44 | 17.7 | |
| Women who used contraceptives during their recent intercourse | 43 | 2.6 | 161 | 9.7 | 950 | 57.1 | 510 | 30.6 | <0.001 |
| Women with experience of an abortion | 9 | 3.3 | 54 | 19.9 | 145 | 53.3 | 64 | 23.5 | |
| Women without experience of an abortion | 29 | 5.0 | 77 | 13.2 | 260 | 44.7 | 216 | 37.1 | <0.001 |
| Women who want children/more children in the future | 36 | 2.9 | 161 | 13.0 | 775 | 62.6 | 267 | 21.5 | |
| Women who do not want children/more children in the future | 13 | 3.8 | 29 | 8.4 | 129 | 37.4 | 174 | 50.4 | <0.001 |
| Age 20‐25 | 24 | 2.4 | 121 | 12.3 | 626 | 63.6 | 213 | 21.6 | |
| Age 26‐30 | 16 | 3.8 | 59 | 13.9 | 239 | 56.2 | 111 | 26.1 | |
| Age 31‐40 | 14 | 3.0 | 42 | 9.0 | 190 | 40.5 | 223 | 47.5 | <0.001 |
| Elementary school (9 years) | 10 | 10.8 | 13 | 14.0 | 40 | 43.0 | 30 | 32.3 | |
| High school (12 years) | 27 | 2.4 | 143 | 12.6 | 677 | 59.8 | 285 | 25.2 | |
| College/university | 19 | 2.7 | 70 | 10.0 | 367 | 52.7 | 241 | 34.6 | <0.001 |
4. DISCUSSION
The main finding in this study is that 13% of women attending contraceptive counseling did not use any form of contraception during their most recent intercourse, whereas one‐third used COC (36.3%), followed by LARC (22%) and condoms (18%). COC were most commonly used by nulliparous women and LARC by parous women.
Furthermore, 2 of 10 women who were not in a stable relationship did not use contraceptives during their most recent intercourse, and a similar figure was noted for parous women. This indicates an unmet need for contraception prior to the visit for contraceptive counseling.
In total, 15% of the women thought that they might have an unintended pregnancy sometime in their future; however, the proportion was twice as high among women who had not used any contraception during their most recent intercourse. Women with an experience of abortion believed that they would have another unintended pregnancy in the future, to a greater extent (23%). Despite the fact that these women showed up for contraceptive counseling, they still believed that they had a future risk for an unplanned pregnancy.
In this population, the use of LARC was twice as common among parous women (35%) than nulliparous women (17%), which was expected based on our clinical experiences. One of ten nulliparous women who did not want to have children, one of 10 used LARC during their most recent intercourse, indicating that LARC could be used to a greater extent. In a US study that promoted LARC, 68% chose LARC and 11% COC. The compliance after 12 months was 86% of those who chose LARC compared with 55% of those who used COC, indicating a higher satisfaction rate within the LARC users.18 Some explanations for the lower than expected use of LARC in our study may be that some women do not want to have LARC for such reasons as fear of pain related to the insertion19 or that they have experienced side effects with previous use of LARC.20, 21 Another aspect may be that some counselors are not fully implementing the national guidelines into their counseling. Therefore, it seems prudent for healthcare providers to ask women who attend contraceptive counseling about their intentions to become pregnant and to address the pros and cons of all kinds of contraceptives, especially LARC, for those who need a method offering high compliance and long‐term protection. This recommendation is in line with the national guidelines that advocate LARC, mainly due to their high compliance; however, one must bear in mind that COC is more suitable for some women.
Other highly effective methods are tubal ligation and vasectomy; however, these alternatives should mainly be recommended to women and men who cannot use reversible contraceptives.7
One of the strengths of this study is that it is a large population‐based study among women attending contraceptive counseling. All clinics in the region participated, minimizing the risk of selection bias. Women with different educational levels and occupations participated, as well as both parous and nulliparous women. An additional strength is that the level of education in the different age groups was almost the same as that in all pregnant women in Sweden in 2015.22 The region where the present study took place is similar to many regions in Sweden. The women's economy, education, and smoking rates are similar to those of women in other regions. We therefore believe that our results are representative of other regions in Sweden.
A weakness in this study is that we included only Swedish‐speaking women. A previous study found that it was very difficult to recruit women who did not speak Swedish, despite great efforts, for example, using translated questionnaires and interpreters.23 The study design also made this difficult, as the participants were supposed to take part in an intervention after having filled in the questionnaire. Women under 20 and over 40 were excluded because we wanted to include women in the ages when pregnancies are most common. Furthermore, since midwives are only licenced to prescribe contraceptives for healthy women, women with chronic diseases may be underrepresented in the study. However, it is possible for women with chronic diseases to make an appointment with the midwife and, if necessary, the midwife can contact a gynecologist or general practitioner after the counseling. Thus, this study may include women with chronic diseases or other health problems.
The participation rate (64%) was seen as satisfactory, as it has gradually become more difficult to recruit people for survey studies. The response rate in the annual Swedish public health survey, for instance, has decreased from 60.8% in 2004 to 47% in 2016, and the response rate is especially low among young adults.24 In the nationwide study on the use of contraception by Kopp Kallner et al (2015), 1001 (25.3%) of 3950 women participated.12
Men's reproductive intentions are also important; however, in this study we investigated women only. Two recent studies in Sweden found a strong coherence between men and women concerning their pregnancy planning.23, 25
Our study showed similar results concerning the use of LARC as reported by Kopp Kallner et al.12 Additionally, the desired mean age for having the first and last child was almost the same in the present study, as reported by Stenhammar et al.13 Reports from many countries have shown that women tend to postpone their childbearing.26 In Sweden, the mean age for the first child was 24 years in the 1970s and close to 29 years in 2015.22
In this study, women wanted to have their first child at a mean age of 28 years and the last child at 34 years, indicating no further postponing of their childbearing. On the other hand, many women were still young and had not yet finished their education. They may change their minds in the future, but their intentions were not to postpone their childbearing.
The discrepancy between contraception use and intentions of reproduction is important information for prescribers. It is also important to know whether the women exposed themselves to an unplanned pregnancy earlier. We found that women who have failed to use contraceptives earlier and women with an experience of induced abortion have the highest risk of a future unplanned pregnancy. We believe it is challenging to have a dialogue with women about their reproductive intentions to offer contraception that is suitable for specific stages of their life. A method for this type of dialogue could be the RLP, a tool for helping women arrive at a personal plan for when they want to get pregnant, how to protect against unintended pregnancies, and how to achieve a healthy future pregnancy.27
5. CONCLUSION
In this study, a large group of women did not use contraceptives that are most suitable for their reproductive intentions, and some exposed themselves to unplanned pregnancies by not using contraceptives at all. Questioning women who request contraceptive counseling about their pregnancy intention can give healthcare providers better opportunities for individualized counseling. Future research on methods for personalized counseling would be valuable.
CONFLICT OF INTEREST
Professor Tanja Tydén became a member of Bayer's Advisory Board in Sweden in 2017. Yvonne Skogsdal was a speaker at the Bayer Winter conference for Nordic employees in 2018, without receiving any payment. There are no other conflicts of interest.
ACKNOWLEDGMENTS
We thank all the midwives of the Region Örebro County for helping us with recruitment, and Wilma Rutfjäll, Jennifer Drevin, Jenny Stern, Marie Lidén, and Elina Backman for their assistance with data entry.
Skogsdal YRE, Karlsson JÅ, Cao Y, Fadl HE, Tydén TA. Contraceptive use and reproductive intentions among women requesting contraceptive counseling. Acta Obstet Gynecol Scand. 2018;97:1349‐1357. 10.1111/aogs.13426
Funding information
ALF founding Region Örebro län and the Research Council of Örebro Region County have provided grants for research time for the authors. Bayer AB has sponsored the production costs for information leaflets and questionnaires used in the study.
REFERENCES
- 1. Sedgh G, Singh S, Hussain R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud Fam Plann. 2014;45:301‐314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cheng D, Schwarz EB, Douglas E, Horon I. Unintended pregnancy and associated maternal preconception, prenatal and postpartum behaviors. Contraception. 2009;79:194‐198. [DOI] [PubMed] [Google Scholar]
- 3. Mercier RJ, Garrett J, Thorp J, Siega‐Riz AM. Pregnancy intention and postpartum depression: secondary data analysis from a prospective cohort. BJOG. 2013;120:1116‐1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shah PS, Balkhair T, Ohlsson A, Beyene J, Scott F, Frick C. Intention to become pregnant and low birth weight and preterm birth: a systematic review. Matern Child Health J. 2011;15:205‐216. [DOI] [PubMed] [Google Scholar]
- 5. Black A, Guilbert E, Co A, et al. Canadian contraception consensus (Part 1 of 4). J Obstet Gynaecol Can. 2015;37:936‐942. [DOI] [PubMed] [Google Scholar]
- 6. FSRH . UK Medical Eligibility Criteria for Contraceptive Use (UKMEC). 2016. http://ukmec.pagelizard.com/2016#sectiona/cover. Accessed December 18, 2017.
- 7. Antikonception ‐ behandlingsrekommendation. Information från läkemedelsverket. [Contraception ‐ Treatment Recommendation. Information from the Swedish Medical Products Agency] In Swedish. Swedish Medical Products Agency 2014;25:14‐28. [Google Scholar]
- 8. Winner B, Peipert JF, Zhao Q, et al. Effectiveness of long‐acting reversible contraception. N Engl J Med. 2012;366:1998‐2007. [DOI] [PubMed] [Google Scholar]
- 9. Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397‐404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lindh I, Skjeldestad FE, Gemzell‐Danielsson K, et al. Contraceptive use in the Nordic countries. Acta Obstet Gynecol Scand. 2017;96:19‐28. [DOI] [PubMed] [Google Scholar]
- 11. Hognert H, Skjeldestad FE, Gemzell‐Danielsson K, et al. High birth rates despite easy access to contraception and abortion: a cross‐sectional study. Acta Obstet Gynecol Scand. 2017;96:1414‐1422. [DOI] [PubMed] [Google Scholar]
- 12. Kopp Kallner H, Thunell L, Brynhildsen J, Lindeberg M, Danielsson KG. Use of contraception and attitudes towards contraceptive use in Swedish women—a nationwide survey. PLoS ONE. 2015;10:e0125990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Stenhammar C, Ehrsson YT, Akerud H, Larsson M, Tyden T. Sexual and contraceptive behavior among female university students in Sweden—repeated surveys over a 25‐year period. Acta Obstet Gynecol Scand. 2015;94:253‐259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kennedy S, Grewal M, Roberts EM, Steinauer J, Dehlendorf C. A qualitative study of pregnancy intention and the use of contraception among homeless women with children. J Health Care Poor Underserved. 2014;25:757‐770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Coombe J, Harris ML, Wigginton B, Lucke J, Loxton D. Contraceptive use at the time of unintended pregnancy: findings from the Contraceptive Use, Pregnancy Intention and Decisions study. Aust Fam Physician. 2016;45:842‐848. [PubMed] [Google Scholar]
- 16. Stern J, Larsson M, Kristiansson P, Tyden T. Introducing reproductive life plan‐based information in contraceptive counselling: an RCT. Hum Reprod. 2013;28:2450‐2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jack BW, Atrash H, Coonrod DV, Moos MK, O'Donnell J, Johnson K. The clinical content of preconception care: an overview and preparation of this supplement. Am J Obstet Gynecol. 2008;199:S266‐S279. [DOI] [PubMed] [Google Scholar]
- 18. Peipert JF, Zhao Q, Allsworth JE, et al. Continuation and satisfaction of reversible contraception. Obstet Gynecol. 2011;117:1105‐1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Asker C, Stokes‐Lampard H, Beavan J, Wilson S. What is it about intrauterine devices that women find unacceptable? Factors that make women non‐users: a qualitative study. J Fam Plann Reprod Health Care. 2006;32:89‐94. [DOI] [PubMed] [Google Scholar]
- 20. Flore M, Chen XL, Bonney A, et al. Patients’ perspectives about why they have their contraceptive Implanon NXT device removed early. Aust Fam Physician. 2016;45:740‐744. [PubMed] [Google Scholar]
- 21. Dickerson LM, Diaz VA, Jordon J, et al. Satisfaction, early removal, and side effects associated with long‐acting reversible contraception. Fam Med. 2013;45:701‐707. [PubMed] [Google Scholar]
- 22. Socialstyrelsen . Graviditet, Förlossning och Födda Barn 2015. [Pregnancy, Childbirth and Children Born 2015.] Stockholm, Sweden: Swedish National Board of Health and Welfare; 2015. http://www.socialstyrelsen.se/publikationer2017/2017-3-3. Accessed January 5, 2018. [Google Scholar]
- 23. Stern J, Salih Joelsson L, Tyden T, et al. Is pregnancy planning associated with background characteristics and pregnancy‐planning behavior? Acta Obstet Gynecol Scand. 2016;95:182‐189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Folkhälsomyndigheten . Nationella Folkhälsoenkäten—Hälsa på Lika Vilkor? [National Public Health Survey – Health on Equal Terms?]. Solna: The Public Health Agency of Sweden; 2016. https://www.folkhalsomyndigheten.se/globalassets/statistik-uppfoljning/enkater-undersokningar/nationella-folkhalsoenkaten/fakta-nationella-folkhalsoenkaten-2016.pdf. Accessed January 5, 2017. [Google Scholar]
- 25. Bodin M, Stern J, Kall LF, Tyden T, Larsson M. Coherence of pregnancy planning within couples expecting a child. Midwifery. 2015;31:973‐978. [DOI] [PubMed] [Google Scholar]
- 26. Johnson JA, Tough S. No‐271‐delayed child‐bearing. J Obstet Gynaecol Can. 2017;39:e500‐e515. [DOI] [PubMed] [Google Scholar]
- 27. American College of Obstetricians and Gynecologists’ Committee on Health Care for Underserved Women . Committee opinion No. 654: reproductive life planning to reduce unintended pregnancy. Obstet Gynecol. 2016;127:e66‐e69. [DOI] [PubMed] [Google Scholar]


