Abstract
Background
The comorbidity of mood and anxiety disorders (MD and AD) with substance use disorders (SUD) is common. One explanation for this comorbidity is the self‐medication hypothesis, which posits that individuals with MD or AD use substances to cope with the difficult symptoms associated with the disorder. Over time, self‐medication (SM) can develop into an independent SUD. This narrative review will present the prevalence and correlates of SM with alcohol and/or drugs for MD and AD and the relationship between SM and subsequent SUD using both cross‐sectional and longitudinal epidemiological data.
Methods
Scopus and PsycINFO were searched from January 1997 to April 2018 to identify original research articles that examined the prevalence and correlates of SM and the temporal relationship between MD/AD and SUD in the general population (n = 22).
Results
The prevalence of SM with alcohol and/or drugs among those with MD or AD ranged from 21.9% to 24.1%. Male sex, younger age, being separated, divorced or widowed, and being Caucasian were characteristics associated with higher proportions of respondents endorsing SM with alcohol/drugs for MD and AD. Longitudinal data supports the temporal onset of primary MD/AD and secondary SUD among those who self‐report SM.
Conclusion
Providing and promoting alternate coping strategies for those with MD/AD may reduce SM, the development of SUD, and the comorbidity of MD/AD with SUD. The concurrent treatment of MD/AD and substance use is the current “gold standard” model of care, and the results of this review support its use.
Keywords: addiction, alcoholism/alcohol use disorders, anxiety/anxiety disorders, coping, depression, epidemiology, substance use disorders
1. INTRODUCTION
The prevalence estimates of past‐year mood and anxiety disorders (MD and AD) in the general population are 9.2 and 11.1%, respectively (Grant et al., 2004). Recent estimates of past‐year alcohol use disorder (AUD) are slightly higher than those for MD and AD at 13.9% (Grant et al., 2015), and prevalence of past‐year drug use disorders ranges between 2 and 3% (Merikangas & Mcclair, 2012). These disorders are associated with significant costs to the individual and society including: low levels of educational attainment, unstable employment, decreased work productivity, decreased health‐related quality of life, and increased primary care use (Donovan, Mattson, Cisler, Longabaugh, & Zweben, 2005; Kessler, 2012; Walley et al., 2012; Wittchen, 2002). The co‐occurrence of MD/AD and substance use disorders (SUD) has been well‐established in the literature (Conway, Compton, Stinson, & Grant, 2006; Demetrovics, 2009; Grant et al., 2004; Lai, Cleary, Sitharthan, & Hunt, 2015; Regier et al., 1990; Sareen et al., 2006), with an estimated two‐ to five‐fold increase in odds of having a MD/AD or SUD when the other condition is present (Kessler et al., 1997; Kushner, Sher, & Erickson, 1999; Sareen et al., 2006; Sareen, Chartier, Kjernisted, & Stein, 2001). Experiencing comorbid MD/AD and SUD is associated with greater symptom severity, impairment, suicidality, and help seeking (Mojtabai, Olfson, & Mechanic, 2002; Prior, Mills, Ross, & Teesson, 2017) compared to experiencing only one disorder, and as such is a major public health problem. Understanding the mechanisms by which MD/AD and SUD co‐occur is important for developing appropriate and effective prevention strategies and treatment options.
The self‐medication hypothesis (SMH) is one mechanism that can explain the comorbidity between MD/AD and SUD (Khantzian, 1985,1997). The SMH was first described in 1985 by Edward Khantzian as a psychological explanation for the comorbidity between MD/AD and substance use (Khantzian, 1985), and posits that substances are used as coping mechanisms to deal with the difficult symptoms associated with MD/AD. As substance use becomes a more frequently relied‐on coping strategy, the use can develop into an independent SUD. For the remainder of this article, self‐medication (SM) will be defined as the self‐reported use of alcohol or drugs to help cope with feelings of depression or anxiety. While the SMH is one plausible mechanism to explain the comorbidity between MD/AD and SUD, other mechanisms include: (a) the reverse causal pathway, namely, substance use leading to a psychiatric disorder; (b) shared environmental or genetic vulnerability (i.e., childhood trauma) that may increase risk for both MD/AD and SUD (no causal relationship); and (c) a gene–environment interaction that may increase risk for SUD among those with MD/AD, or vice versa, through some third variable (indirect causal relationship) (Kraemer, Stice, Kazdin, Offord, & Kupfer, 2001; Zhou et al., 2017).
Aside from potentially contributing to the development of a SUD, SM itself is associated with several other adverse outcomes, such as increased psychiatric comorbidity, suicidal behavior, treatment utilization, levels of stress and dysfunction, and lower health‐related quality of life (Bolton, Cox, Clara, & Sareen, 2006; Bolton, Robinson, & Sareen, 2009; Leeies, Pagura, Sareen, & Bolton, 2010; Robinson, Sareen, Cox, & Bolton, 2009a, 2009b). Furthermore, even after adjusting for current SUD, SM for AD or PTSD was related to a number of mood and personality disorders (Leeies et al., 2010; Robinson et al., 2009a), lifetime suicidal ideation and attempts (Bolton et al., 2006), and lower mental and physical health‐related quality of life scores (Leeies et al., 2010; Robinson et al., 2009b). These results show that SM itself is an independent risk factor for poor outcomes even after controlling for the presence of a SUD. Similar relationships were also evident with SM for MDs (Bolton et al., 2009).
The SMH has been examined using both treatment‐seeking and epidemiological samples. Strengths of treatment‐seeking samples include the ability to use more detailed measures of substance use motivation and symptom experiences to study the SMH; however, these studies are limited by small sample size and selection bias. One clinical method that is particularly powerful for assessing the SMH is the ecological momentary analysis method, which uses real‐time data to uncover the complex interplay between MD/AD symptoms and substance use. Previous work using this method has shown support for the SMH (Gorka, Hedeker, Piasecki, & Mermelstein, 2017; Possemato et al., 2015). Epidemiological studies using general population samples can overcome some of the limitations of treatment‐seeking samples, such as treatment‐seeking bias, by being representative of the general population (Alegria et al., 2010; Crum, La Flair et al., 2013; Crum, Mojtabai et.al., 2013; Farmer et al., 2017; Feingold, Weiser, Rehm, & Lev‐ran, 2015, 2016; Fergusson, Boden, & Horwood, 2009; Kessler et al., 1997; Kuo, Gardner, Kendler, & Prescott, 2006; Lazareck et al., 2012; Liang, Chikritzhs, & Lenton, 2011; Martins et al., 2012; Martins, Keyes, Storr, Zhu, & Chilcoat, 2009; Menary, Kushner, Maurer, & Thuras, 2011; Robinson, Sareen, Cox, & Bolton, 2011; Sareen et al., 2001; Swendsen et al., 1998; Wolitzky‐Taylor, Bobova, Zinbarg, Mineka, & Craske, 2012). Epidemiological samples are further strengthened by using age of onset or longitudinal designs to assess the temporal onset of MD/AD and SUD.
The literature currently lacks a synthesis of the epidemiological literature examining SM with alcohol and/or drugs for MD/AD symptoms. Including studies that examine the temporal onset of SUD and MD/AD without including self‐reported SM, in addition to those that include data of self‐reported SM will provide a comprehensive overview of the epidemiological literature examining the SMH. This is important as there is an inherent reporting bias in only considering those who self‐report SM. The aim of this review is to present: (a) the prevalence of self‐reported SM in the general population; (b) sociodemographic factors associated with SM; (c) cross‐sectional epidemiological studies that examine the comorbidity between MD/AD and SUD using age‐of‐onset data; (d) longitudinal studies that examine the relationship between MD/AD and SUD among those who self‐report SM for symptoms of MD/AD and, (e) the clinical implications resulting from the current findings.
2. METHODS
Scopus and PsycINFO were searched using combinations of the terms “self‐medication,” “substance use,” “mood OR anxiety,” “general population,” “longitudinal,” “epidemiology,” and “comorbid” from January 1997 through April 2018 to find relevant peer‐reviewed journal articles. About 178 abstracts were returned from the search and 18 individual manuscripts using longitudinal and cross‐sectional methodologies with age‐of‐onset data were included in this narrative review. An additional four manuscripts were identified to describe the prevalence and correlates of SM. Manuscripts were excluded if they did not present original research, used clinical data, focused exclusively on tobacco as the substance for SM, or did not include age of onset for MD/AD and SUD so that incidence of the disorder could be measured. See Figure 1 for a flowchart of the abstract selection.
Figure 1.
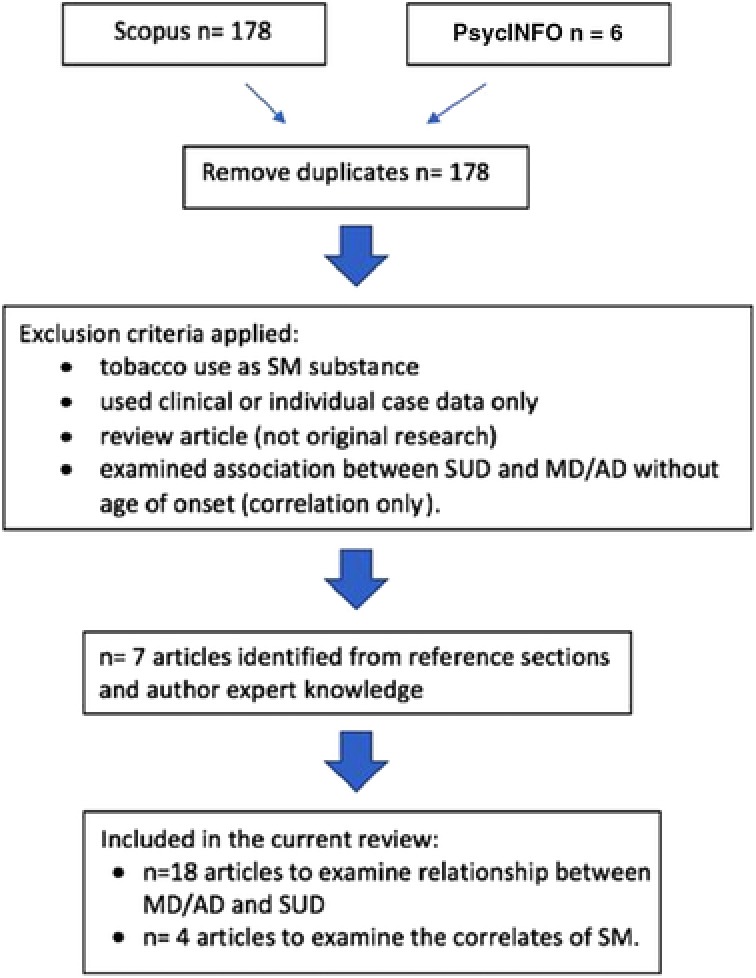
Flowchart of article selection
3. RESULTS
3.1. The prevalence of self‐mediation
Two main epidemiological surveys have been used to determine the prevalence of SM and the comorbidity of MD/AD and SUD in the general population: The National Epidemiologic Study of Alcohol and Related Conditions (NESARC) and the National Comorbidity Survey (NCS). The NESARC is a representative survey from the United States that surveyed the same respondents at two time points. Wave 1 included 43,093 respondents collected in 2001–2002 (Grant et al., 2004; Grant, Kaplan, Shepard, & Moore, 2003) and the follow‐up, wave 2, resurveyed 36,356 respondents and was collected in 2004–2005 (Grant & Kaplan, 2005). SM was assessed in the NESARC for those endorsing symptoms of MD or AD by asking respondents if they had ever used alcohol or drugs to relieve their symptoms or make them feel better. The question was asked separately for drugs and alcohol and for each MD and AD category. The NCS, is a representative survey from United States that surveyed a sample of 8,098 respondents, collected in 1990–1992 (Kessler et al., 1994). The NCS assessed SM for MD and AD by asking the respondent if they had ever drank more than usual or used drugs not prescribed (or in larger quantities than prescribed) to face the symptoms they reported experiencing. The NCS and the NESARC are the only known surveys with published data that directly assess self‐reported SM for psychiatric disorder symptoms.
In the NESARC wave 1, the prevalence of SM with alcohol only for different ADs ranged from 3.0% for panic disorder without agoraphobia to 14.9% for social phobia (Table 1) (Robinson et al., 2009a). The prevalence of SM with drugs (with or without alcohol) ranged from 0.7% for panic disorder without agoraphobia to 7.0% for GAD (Leeies et al., 2010; Robinson et al., 2009a). When considering the prevalence of any SM (alcohol and/or drugs), results from the NCS provide a prevalence range from 7.9% for social phobia speaking subtype to 35.6% for GAD (Bolton et al., 2006). The prevalence of SM with alcohol only for any AD ranged from 10.0 to 20.8% using data from the NESARC waves 1 and 2 (Menary et al., 2011; Robinson et al., 2009a); and using the NCS data, the prevalence of any SM (alcohol and/or drugs) for any AD was 21.9% (Bolton et al., 2006).
Table 1.
Prevalence of self‐medication with drugs or alcohol for anxiety disorders
| Anxiety disorder | Self‐medication with alcohol (%) | Self‐medication with drugs (%) | Any self‐medication (%) | Author | Sample |
|---|---|---|---|---|---|
| Panic disorder without agoraphobia | 3.0 | 0.7 (Both alcohol and drugs) | Robinson et al. 2009a | NESARC 1 (2001/2) | |
| Panic disorder with agoraphobia | 6.7 | 4.3 (Both alcohol and drugs) | Robinson et al. 2009a | NESARC 1 (2001/2) | |
| Panic disorder | 23.0 | Bolton et al., 2006 | NCS (1990/2) | ||
| Social phobia | 14.9 | 4.5 (Both alcohol and drugs) | Robinson et al. 2009a | NESARC 1 (2001/2) | |
| Social phobia speaking subtype | 7.9 | Bolton et al., 2006 | NCS (1990/2) | ||
| Social phobia complex subtype | 21.2 | Bolton et al., 2006 | NCS (1990/2) | ||
| Simple phobia | 12.1 | Bolton et al., 2006 | NCS (1990/2) | ||
| Agoraphobia | 15.8 | Bolton et al., 2006 | NCS (1990/2) | ||
| Specific phobia | 4.1 | 1.1 (Both alcohol and drugs) | Robinson et al. 2009a | NESARC 1 (2001/2) | |
| GAD | 14.1 | 5.1 (Both alcohol and drugs) | Robinson et al. 2009a | NESARC 1 (2001/2) | |
| 35.6 | Bolton et al., 2006 | NCS (1990/2) | |||
| PTSD | 14.4 | 7.0 (Drugs with or without alcohol) | 21.4 | Leeies et al., 2010 | NESARC 2 (2004/5) |
| Any anxiety disorder | 20.3 | Menary et al., 2011, * | NESARC 1 (2001/2) | ||
| 20.8 | Menary et al., 2011 | NESARC 2 (2004/5) | |||
| 10.0 | 3.1 (Both alcohol and drugs) | Robinson et al. 2009a, * | NESARC 1 (2001/2) | ||
| 21.9 | Bolton et al., 2006 | NCS (1990/2) |
*The discrepancy in the findings for any anxiety disorder using the NESARC wave 1 is likely due to a selection of different study samples used in each study. In Menary et al., 2011, the study sample was limited to only those who were consumers of alcohol in wave 1 and reported psychiatric symptoms for all AD except specific phobia. In Robinson et al. 2009a, the study sample was the entire population that reported psychiatric symptoms in wave 1 and did not limit to only consumers of alcohol.
GAD, generalized anxiety disorder, PTSD, post‐traumatic stress disorder
SM for MD with alcohol and/or drugs has only been examined using the NESARC wave 1 and appears to be slightly more common than SM for AD (Bolton et al., 2009). Bipolar 2 disorder had the highest prevalence of SM with alcohol only (23.9%) and dysthymia had the lowest (12.1%). Bipolar 2 disorder also had the highest prevalence of SM with drugs (with or without alcohol) at 18.9% and major depressive disorder had the lowest at 7.8%. The prevalence of any SM (alcohol and/or drugs) ranged from 22.9% for dysthymia to 41.0% for bipolar 1 disorder. The prevalence of any SM for any MD was 24.1% (Table 2).
Table 2.
Prevalence of self‐medication with drugs or alcohol for mood disorders
| Mood disorder | Self‐medication with alcohol only (%) | Self‐medication with drugs (with or without alcohol) (%) | Any self‐medication | Author | Sample |
|---|---|---|---|---|---|
| Dysthymia | 12.1 | 10.8 | 22.9 | Bolton et al., 2009 | NESARC 1 (2001/2) |
| Major depressive disorder | 15.4 | 7.8 | 23.2 | Bolton et al., 2009 | NESARC 1 (2001/2) |
| Bipolar 1 disorder | 22.1 | 18.9 | 41.0 | Bolton et al., 2009 | NESARC 1 (2001/2) |
| Bipolar 2 disorder | 23.9 | 10.8 | 34.7 | Bolton et al., 2009 | NESARC 1 (2001/2) |
| Any mood disorder | 15.7 | 8.4 | 24.1 | Bolton et al., 2009 | NESARC 1 (2001/2) |
3.2. Sociodemographic characteristics associated with SM
Studies using waves 1 and 2 of the NESARC and the NCS have shown that there are certain demographic characteristics that are associated with a significantly higher prevalence of SM with alcohol and/or drugs for MD and AD in the general population (Bolton et al., 2006, 2009; Leeies et al., 2010; Robinson et al., 2009a). In the NESARC wave 1, SM with alcohol and drugs for one or more AD was more prevalent among males (55.8% male in the SM category compared to 32.5% male in the no SM category), younger age (30.1% were aged 18–29 in the SM category compared to 20.1% aged 18–29 in the no SM category), those who are separated or divorced, or never married (30.7 and 34.6% are separated or divorced, or never married in the SM category compared to 19.5 and 18.6% in the no SM category), those with lower income (31.3% with less than $20,000 income per year in the SM category compared to 23.1% in the no SM category), those with less than a high school college education (20% with less than a high school education in the SM category compared to 14.6% with less than a high school education in the no SM category), and those who were identified as Caucasian (81.3% identified as Caucasian in the SM category compared to 71.4% in the no SM category) (Robinson et al., 2009a).
Results using the NCS data show similar associations, with the exception of education and income not being significantly related to SM with alcohol and/or drugs for ADs (Bolton et al., 2006). Another study by Leeies et al. (2010) focused on SM with alcohol or drugs for PTSD symptoms using the NESARC wave 2 and also corroborates previous findings. In this study, male sex, being never married, being in a younger age category, being Caucasian, and having some college education were associated with increased odds of any SM for PTSD symptoms (Leeies et al., 2010).
The same sociodemographic characteristics have also been found to be significantly associated with SM with alcohol and/or drugs for MD. One study using wave 1 of the NESARC examined the association between sociodemographic characteristics and SM with drugs and/or alcohol for MD. The findings mirror those found for AD, with SM being significantly associated with male sex (OR = 2.18, 95% confidence of interval [CI] = 1.90–2.49, compared to females), younger age (OR = 0.28, 95% CI = 0.20–0.39 for those 65 years and older, compared to age 18–29 years old), being widowed or divorced (OR = 1.47, 95% CI = 1.22–1.76, compared to married), and being Caucasian (OR were significantly below 1 for those who were Black (OR = 0.77, 95% CI = 0.64–0.94), Asian/Hawaiian (OR = 0.52, 95% CI = 0.30, 0.89), and Hispanic or Latino (OR = 0.58, 95% CI = 0.47–0.72) compared to those who were White) (Bolton et al., 2009). Importantly, education and income levels were not associated with SM with drugs and/or alcohol for MD.
3.3. The self‐medication hypothesis for ADs
There is a large body of evidence that tests the temporal association between AD and SUD with both cross‐sectional data using age of onset and longitudinal data. It is important to note that many studies do not include self‐reports of SM when looking at the relationship between AD and SUD, therefore limiting true assessment of the SMH (Alegria et al., 2010; Farmer et al., 2017; Kessler et al., 1997; Liang et al., 2011; Martins et al., 2009, 2012; Swendsen et al., 1998; Wolitzky‐Taylor et al., 2012). However, a review of the data that looks at the temporal onset of AD and SUD is important because data that only considers those who self‐report SM will likely underestimate the true prevalence of SM in the population. Expanding our view to consider the temporal association between AD and SUD without limiting to those who report SM will provide a more comprehensive assessment of these relationships. In the following paragraphs, data assessing the temporal relationship between AD and SUD will be presented, followed by data that examines this temporal relationship among populations who self‐report SM for AD.
Multiple epidemiological datasets with reports of age of onset of AD and SUD have been used to answer the following question: Do ADs more commonly precede SUD, or do SUD more commonly precede AD? Some studies show support for the temporal onset of AD leading to SUD while others do not (Alegria et al., 2010; Crum et al., 2013; Farmer et al., 2017; Feingold et al., 2016; Kessler et al., 1997; Liang et al., 2011; Martins et al., 2009, 2012; Menary et al., 2011; Robinson et al., 2011; Swendsen et al., 1998; Wolitzky‐Taylor et al., 2012). Data from three epidemiological studies in Europe and the United States showed that phobic disorders are more likely to precede AUD, but the pathway between panic disorders and AUD was equally strong in both directions (Swendsen et al., 1998). Using data from the NCS, phobic disorders, including agoraphobia, social and simple phobia, and PTSD more commonly occurred after the onset of alcohol abuse or dependence than before. However, panic disorder and generalized AD (GAD) more commonly occurred before the onset of alcohol abuse or dependence (Kessler et al., 1997). Data from the Ontario Health Survey showed that diagnoses of phobic disorders preceded the onset of alcohol abuse or dependence 57–90% of the time, depending on the phobic disorder (Sareen et al., 2001). Data from the Mental Health and Wellbeing Study in Australia showed that anxiety disorders predicted harmful drug use and dependence, but the opposite association between drug use and incident anxiety disorders was not examined (Liang et al., 2011). A series of studies using data from waves 1 and/or 2 of the NESARC have examined the temporal onset of AD and substance abuse or dependence (Alegria et al., 2010; Feingold et al., 2016; Martins et al., 2009, 2012). One study showed that among those who had comorbid GAD and SUD (alcohol or drugs), mean age of onset was lower for the SUD than for GAD (Alegria et al., 2010). Analyses looking specifically at opioid use and dependence and AD in the NESARC found evidence for both causal pathways; AD predicted opioid use, and opioid use also predicted AD (Martins et al., 2009, 2012). No significant findings were documented for the relationship between AD and incident cannabis abuse or dependence, aside from those with panic disorder, who were more likely to initiate cannabis use (Feingold et al., 2016). In a sample of adolescents from the United States, the presence of one or more AD was associated with later onset of SUD, with particularly strong findings for social AD predicting AUD and PTSD predicting both drug and AUD (Wolitzky‐Taylor et al., 2012). The same sample also found that primary AUD was significantly associated with later onset obsessive‐compulsive disorder, but no other significant associations in this direction existed. In a different US adolescent sample, the presence of AD had no association with new onset AUD (Farmer et al., 2017).
The analytic approach of examining the temporal onset of AD and SUD does not take into account those who actually report using alcohol or drugs for the purposes of self‐medicating anxiety symptoms. Examining the population who report SM can provide more insight into the relationship between AD and SUD, specifically for those who use substances as coping mechanisms, and is central to the validation of the SMH. Three studies using longitudinal data from the NESARC waves 1 and 2 have measured the likelihood of incident SUD among those reporting SM for AD symptoms (Crum et al., 2013; Menary et al., 2011; Robinson et al., 2011). When considering AD overall, there is strong evidence that self‐medicating AD symptoms is related to the development of new substance dependence or SUD and also to the persistence of SUD (Crum et al., 2013; Menary et al., 2011; Robinson et al., 2011). SM with alcohol for AD symptoms at wave 1 was associated with a 2.50 (95% CI = 1.26–4.97) odds increase for wave 2 onset AUD (Robinson, Sareen, Cox, & Bolton, 2011) and the persistence of alcohol dependence from wave 1 to wave 2 (AOR = 6.25, 95% CI = 3.24–12.05) (Crum et al., 2013). SM with drugs for anxiety symptoms at wave 1 was also related to wave 2 onset drug use disorders (AOR = 3.46, 95% CI = 1.26–9.49) (Robinson et al. 2011, Table 3). This relationship was also seen for those with subthreshold AD symptoms (Crum et al., 2013). In Robinson et al. (2011), the reverse relationship was tested, looking at the association between those with SUD who SM for subthreshold anxiety symptoms and incident AD. In these analyses, primary SUD at baseline was related to incident social phobia at follow‐up among those who endorsed SM for subclinical anxiety symptoms at wave one; however, this pathway was not significant for any other ADs.
Table 3.
Odds of incident and persistent AUD/ dependence and incident and persistent DUD/ dependence among those who self‐medicate for mood and anxiety symptoms
| Odds of incident AUD/dependence (AOR, 95% CI) | Odds of persistent alcohol dependence (AOR, 95% CI) | Odds of incident DUD/dependence (AOR, 95% CI) | Odds of persistent DUD (AOR, 95% CI) | Author | Sample | |
|---|---|---|---|---|---|---|
| Self‐medicate with alcohol for any anxiety symptoms | 2.50 (1.26–4.97) (AUD) | 1.46 (0.73–2.91) (DUD) | aRobinson et al., 2011 | NESARC 1 and 2 (2001/2) and (2004/5) | ||
| 6.25 (3.24–12.05) | bCrum et al., 2013 | NESARC 1 and 2 (2001/2) and (2004/5) | ||||
| 3.77 (2.58–5.51) (dependence) | cMenary et al., 2011 | NESARC 1 and 2 (2001/2) and (2004/5) | ||||
| Self‐medicate with drugs for any anxiety symptoms | 2.62 (0.94–7.32) (AUD) | 3.46 (1.26–9.49) (DUD) | aRobinson et al., 2011 | NESARC 1 and 2 (2001/2) and (2004/5) | ||
| Self‐medicate with alcohol for any mood symptoms | 3.10 (1.55–6.19) (dependence) | 3.45 (2.35–5.08) | dCrum et al., 2013 | NESARC 1 and 2 (2001/2) and (2004/5) | ||
| Self‐medicate with drugs for any mood symptoms |
4.11 (2.33–7.25) (DUD) 7.65 (3.70–15.82) (dependence) |
2.02 (1.46–2.80) | eLazareck et al., 2012 | NESARC 1 and 2 (2001/2) and (2004/5) |
Odd ratios calculated using logistic regression and adjusted for sex, age, income, marital status, education level, ethnicity, region, urban status, and any lifetime psychiatric disorder at wave 1.
Odd ratios calculated using logistic regression and propensity score matching for age, sex, race–ethnicity, education level, drinking pattern and consumption level, current history of generalized anxiety disorder, panic disorder, social phobia, specific phobia and, major depressive disorder, nonalcohol substance use disorder, nicotine dependence, personality disorder, family history of alcoholism, and lifetime treatment for anxiety.
Odds ratio calculated using logistic regression without adjustment.
Odd ratios calculated using inverse probability treatment weights and adjusted for sex, age, ethnicity, past‐month mood disorder, and lifetime treatment history for mood symptoms.
Odd ratios calculated using logistic regression and adjusted for sex, age, income, marital status, education level, ethnicity, region, urban status, and any lifetime psychiatric disorder at wave 1.
AUD, alcohol use disorder; DUD, drug use disorder.
3.4. The self‐medication hypothesis for MDs
An additional body of literature has assessed the temporal onset of MD and SUD without directly assessing SM, and found evidence for both causal pathways (Crum et al., 2013; Feingold et al., 2015; Fergusson et al., 2009; Kessler et al., 1997; Kuo et al., 2006; Lazareck et al., 2012; Liang et al., 2011; Martins et al., 2012; Wolitzky‐Taylor et al., 2012). Data from Australia showed that those with MD were at a higher risk of incident harmful or dependent drug use (Liang et al., 2011). However, the alternate hypothesis to test whether those with drug use dependence were at a higher risk of developing incident MD was not assessed. In a sample of adolescents from the United States., major depression predicted later onset of AUD, but AUD did not predicted the onset of major depression (Wolitzky‐Taylor et al., 2012). Data from the NCS showed that, in general, depression, dysthymia, and mania more commonly occurred before the onset of alcohol abuse or dependence than after (Kessler et al., 1997). Using longitudinal data from waves 1 and 2 of the NESARC, specific findings about opioid use showed support for both the pathways from MD to opioid use and the reverse (Martins et al., 2012). Using the NESARC data again, different authors found that baseline major depressive disorder predicted the initiation of cannabis use, but no significant association was found for bipolar disorder and incident cannabis use. Furthermore, daily cannabis use was not significantly associated with incident major depression or bipolar disorder (Feingold et al., 2015). A study including three different geographic communities from the USA and Puerto Rico showed that the age of onset for alcohol abuse/dependence disorders and depressive disorders was evenly distributed, with about 50% of depressive disorders occurring before and 50% occurring after the onset of alcohol abuse/dependence (Swendsen et al., 1998). Using data from young adults of age 17–25 years in New Zealand, one study concluded that the strongest pathway existed for baseline alcohol abuse and dependence followed by incident major depression (Fergusson et al., 2009). Finally, using data from a large population‐based registry in Virginia, Kuo et al., 2006, found significant evidence for the pathway of baseline major depression, followed by the onset of alcohol dependence, and no significant evidence for the reverse pathway (Kuo et al., 2006). While all of the above studies measured the temporal association between SUD and MD, none measured self‐reported SM to cope with symptoms of MD.
Again, analyses using longitudinal data from waves 1 and 2 of the NESARC have provided the strongest approach to test the SMH by measuring the relationship between MD and incident SUD among those who report SM with alcohol and/or drugs for MD symptoms (Crum et al., 2013; Lazareck et al., 2012). Individuals who reported using alcohol to self‐medicate MD symptoms had an increased odds of incident and persistent alcohol dependence (AOR = 3.10, 95% CI = 1.55–6.19 and AOR = 3.45, 95% CI = 2.35–5.08, respectively) (Table 3) (Crum et al., 2013). This trend also held for those who had subthreshold MD symptoms, namely, SM with alcohol for subthreshold MD symptoms was significantly related to incident alcohol dependence. Individuals who reported using drugs with or without alcohol to self‐medicate MD symptoms also had an increased odds of incident and persistent drug use disorders (drug abuse and/or drug dependence) (AOR = 4.11, 95% CI = 2.33–7.25 and AOR = 2.02, 95% CI = 1.46–2.80, respectively; Table 3) (Lazareck et al., 2012). In the same study by Lazareck et al. (2012), the reverse relationship was also tested among those with drug use disorders and reports of SM for subthreshold mood symptoms at baseline and incident MD at follow‐up. No significant evidence was observed for this pathway.
4. DISCUSSION
There are four main findings in the current review: (a) there are several sociodemographic factors that are related to SM; (b) SM for MD/AD affects a sizeable proportion of the population, with between 21.9% and 24.1% reporting using alcohol and/or drugs to relieve their MD/AD symptoms; (c) research examining the temporal onset of MD/AD and SUD without assessing SM provides support for both pathways, and (d) research using longitudinal data has consistently shown that those who report SM for symptoms of MD/AD are more likely to develop an incident or persistent SUD.
Four studies in the previous literature have examined the sociodemographic correlates of SM for AD and MD and have found generally consistent results (Bolton et al., 2006, 2009; Leeies et al., 2010; Robinson et al., 2009a). Male sex, younger age, being separated, divorced or widowed, and being Caucasian are factors that increase the prevalence of reporting SM for symptoms of AD and MD. Interestingly, education and income status did not consistently appear as significant correlates across studies. It may be hypothesized that more vulnerable populations would be more likely to self‐medicate with alcohol and drugs, and often low income and low education are indicators of social vulnerability. However, other contextual factors may be at play, such as the social acceptability of using alcohol as a “stress reliever” among higher income and educational groups. This hypothesis may be supported by results from Robinson et al., 2009a which found a higher prevalence of SM in the higher education and income categories.
The literature shows that a significant proportion of the population with symptoms of MD/AD report SM, with 7.9–35.6% reporting SM for various AD, and 22.9–41.0% reporting SM for various MD. There is a larger body of research on SM for AD, which is curious given that MD appear to have a higher prevalence of SM, specifically for those with bipolar disorder. It is possible that the current self‐report assessments of SM underestimate the true prevalence of SM in the population, because an individual is required to recognize their substance use as self‐medicating and be willing to report it as so for SM to be captured in the data. Additional data and research on the prevalence of SM for specific MD is needed to understand the true burden of SM in this population and its relation to incident SUD.
Results from cross‐sectional studies looking at the relationships between MD/AD and SUD without measurements of self‐reported SM show support for relationships in both directions. This identifies that SM is one possible mechanism by which MD/AD and SUD may co‐occur, but it is not the only pathway. However, the strongest approach to assessing the SMH lies in longitudinal studies that assess SM for MD/AD symptoms as a predictor of incident and persistent SUD. In the current literature, five studies were identified that assessed the relationship between MD/AD and SUD for those who report SM (Crum, La Flair et al., 2013; Crum, Mojtabai et al., 2013; Lazareck et al., 2012;Menary et al., 2011; Yaworski, Robinson, Sareen, & Bolton, 2011). The results consistently demonstrated that SM for MD/AD symptoms is a significant predictor of incident and persistent SUD. These results show that when SM is identified as a coping mechanism for MD/AD, it is consistently related to subsequent or persistent SUD.
4.1. Clinical/treatment implications
The most prominent criticism of the SMH is that it encourages under‐recognition and under‐treatment of SUD because of the belief that substance use is a consequence of psychiatric conditions (Lembke, 2012). However, the current psychiatric “gold standard” model of care is concurrent treatment of MD/AD and SUD (Kleber et al., 2006; Mclntyre et al., 2012). The presence of MD/AD has been associated with increased relapse and poorer treatment outcomes among those also being treated for an AUD (Driessen et al., 2001). Therefore, addressing both MD/AD and SUD is an important treatment goal and may lead to improved treatment outcomes overall. A recent meta‐analysis of eight randomized controlled trials on concurrent treatment of MD/AD and alcohol misuse concluded that interventions, such as CBT and motivational interviewing are effective for treating both MD/AD and alcohol disorders simultaneously (Baker, Thornton, Hiles, Hides, & Lubman, 2012). An additional consideration is the use of Dialectical Behaviour Therapy (DBT), a therapy that was developed for the treatment of borderline personality disorder, but has been suggested to be effective for the treatment of SUD as well as other psychiatric disorders (Dimeff & Linehan, 2008). DBT focuses on promoting self‐acceptance, while recognizing the need to change. Skills, such as improving motivation to change, restructuring one's environment to support change, distress tolerance, and preparing for possible relapse are practiced in DBT that could promote positive coping strategies and reduce SM.
4.2. Limitations
There are several limitations in the current literature that should be recognized. First, the assessment of SM using self‐report methods is subject to recall and response bias and may not accurately represent the true prevalence of SM. It is possible that individuals may not report their SM behavior due to desirability bias, forgetting that they engaged in the behavior, or not being aware that their substance use is related to symptoms of MD or AD. If true, this limitation would underestimate the current strength of association between MD/AD and SM. Physician‐based reporting or collateral information from family and friends could improve the validity of this data; however, implementing these methods in population‐based surveys may be challenging. Second, while some studies measure SM in response to disorder symptoms in the absence of diagnosis, others only look at symptoms among those who meet diagnostic criteria for the disorder. A more complete understanding of SM may be found in assessments of SM for those with subthreshold symptoms as well as those who meet diagnostic criteria. Third, those with externalizing psychopathology may be more likely to report SM as a way to rationalize their substance use. Among those with externalizing disorders, addressing SM may not fully resolve a SUD. Fourth, the NESARC waves 1 and 2 are the only datasets available to study SM for MD/AD and incident and persistent SUD but only include one follow‐up period that is 3 years apart. These data preclude a more nuanced examination of the association between SM for MD/AD and SUD over time. Fifth, the current review synthesizes literature from various different research groups using different methodologies; therefore, the direct comparability of statistics cannot be inferred. Sixth, among studies, the outcome variable is inconsistent, with drug/alcohol abuse, dependence or disorder being used in different studies. These differences have been specified when reporting results in this text; however, attention should be given to the clinical differences between abuse, dependence and disorder when interpreting the findings presented in this review.
5. CONCLUSIONS
The SMH was first described using data from treatment‐seeking samples, which is limited by the inability to draw conclusions about the general population. In the last two decades, epidemiological data have been used to overcome this bias by using general population samples. In studies that look specifically at those who report SM for MD/AD symptoms, strong relationships have been seen with incidence and persistence of SUD. This methodology is the strongest approach in testing the SMH and shows consistent evidence across studies. Future studies of SM should be conducted using longitudinal designs with longer follow‐up periods and more assessment points. Further, evaluation of the differential effects of treatment for those who report SM and those who do not may reveal important variations that could inform clinical practice. Not all those who have comorbid MD/AD and SUD will arrive at their comorbidity through SM; there are several other pathways including the causal pathway between SUD and MD/AD, shared environmental or genetic etiology of MD/AD and SUD, and gene–environment interaction whereby MD/AD increases this risk of SUD among those who already have a genetic vulnerability to SUD. Future research could systematically compare the evidence for these different hypotheses.
The current review shows that SM is a prevalent behavior in general population samples and those who report self‐medicating MD/AD symptoms with alcohol and/or drugs are significantly more likely to develop a comorbid SUD. It is possible that addressing SM could be targeted to prevent the development and persistence of a threshold SUD. Clinicians and healthcare providers should screen for SM among those presenting with MD/AD and provide “gold standard” concurrent treatment to address SM behavior and MD/AD simultaneously.
Turner S, Mota N, Bolton J, Sareen J. Self‐medication with alcohol or drugs for mood and anxiety disorders: A narrative review of the epidemiological literature. Depress Anxiety. 2018;35:851–860. 10.1002/da.22771
Funding Information
This research was supported by funding from a CIHR Foundations grant (Sareen).
REFERENCES
- Alegria, A. , Hasin, D. , Nunes, E. , Lui, S.‐M. , Davies, C. , Grant, B. , & Blanco, C. (2010). Comorbidity of generalized anxiety disorder and substance use disorders: Results from the National Epidemiological Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry, 71(9), 1187–1195. 10.4088/JCP.09m05328gry.Comorbidity [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker, A. L. , Thornton, L. K. , Hiles, S. , Hides, L. , & Lubman, D. I. (2012). Psychological interventions for alcohol misuse among people with co‐occurring depression or anxiety disorders: A systematic review. Journal of Affective Disorders, 139(3), 217–229. 10.1016/j.jad.2011.08.004 [DOI] [PubMed] [Google Scholar]
- Bolton, J. , Cox, B. , Clara, I. , & Sareen, J. (2006). Use of alcohol and drugs to self‐medicate anxiety disorders in a nationally representative sample. The Journal of Nervous and Mental Disease, 194(11), 818–825. 10.1097/01.nmd.0000244481.63148.98 [DOI] [PubMed] [Google Scholar]
- Bolton, J. M. , Robinson, J. , & Sareen, J. (2009). Self‐medication of mood disorders with alcohol and drugs in the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Affective Disorders, 115(3), 367–375. 10.1016/j.jad.2008.10.003 [DOI] [PubMed] [Google Scholar]
- Conway, K. P. , Compton, W. , Stinson, F. E. S. , & Grant, B. F. (2006). Lifetime comorbidity of DSM‐IV mood and anxiety disorders and specific drug use disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry, 67(2), 247–257. [DOI] [PubMed] [Google Scholar]
- Crum, R. , La Flair, L. , Storr, C. , Green, K. , Stuart, E. , Alvanzo, A. , … Mojtabai, R. (2013). Reports of drinking to self‐medicate anxiety symptoms: Longitduinal assessment for subgroups of individuals with alcohol dependence. Depression and Anxiety, 30(2), 174–183. 10.1038/jid.2014.371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crum, R. , Mojtabai, R. , Lazareck, S. , Bolton, J. M. , Robinson, J. , Sareen, J. , … Storr, C. L. (2013). A prospective assessment of reports of drinking to self‐medicate mood symptoms with the incidence and persistence of alcohol dependence. JAMA Psychiatry, 70(7), 718 10.1001/jamapsychiatry.2013.1098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demetrovics, Z. (2009). Co‐morbidity of drug addiction: An analysis of epidemiological data and possible etiological models. Addiction Research and Theory, 17(4), 420–431. 10.1080/16066350802601324 [DOI] [Google Scholar]
- Dimeff, L. A. , & Linehan, M. M. (2008). Dialectical behavior therapy for substance abusers. Addiction Science & Clinical Practice, 4(2), 39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan, D. , Mattson, M. E. , Cisler, R. A. , Longabaugh, R. , & Zweben, A. (2005). Quality of life as an outcome measure in alcoholism treatment research. Journal of Studies on Alcohol, 15, 119–139. https://doi.org/10.15288/jsas.2005.s15.119 [DOI] [PubMed] [Google Scholar]
- Driessen, M. , Meier, S. , Hill, A. , Wetterling, T. , Lange, W. , & Junghanns, K. (2001). The course of anxiety, depression and drinking behaviours after completed detoxification in alcoholics with and without comorbid anxiety and depressive disorders. Alcohol and Alcoholism, 36(3), 249–255. [DOI] [PubMed] [Google Scholar]
- Farmer, R. F. , Seeley, J. R. , Kosty, D. B. , Gau, J. M. , Duncan, S. , Sher, K. , & Lewinsohn, P. (2017). No reliable evidence that emotional disorders are proximal antecedents, concomitants, or short‐term consequences of first episode alcohol use disorders in a representative community sample. Journal of Studies on Alcohol and Drugs, 78(2), 222–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feingold, D. , Weiser, M. , Rehm, J. , & Lev‐ran, S. (2015). The association between cannabis use and mood disorders : A longitudinal study. Journal of Affective Disorders, 172, 211–218. 10.1016/j.jad.2014.10.006 [DOI] [PubMed] [Google Scholar]
- Feingold, D. , Weiser, M. , Rehm, J. , & Lev‐Ran, S. (2016). The association between cannabis use and anxiety disorders: Results from a population‐based representative sample. European Neuropsychopharmacology, 26(3), 493–505. 10.1016/j.euroneuro.2015.12.037 [DOI] [PubMed] [Google Scholar]
- Fergusson, D. M. , Boden, J. M. , & Horwood, L. J. (2009). Tests of causal links between alcohol abuse or dependence and major depression. Archives of General Psychiatry, 66(3), 260–266. 10.1001/archgenpsychiatry.2008.543 [DOI] [PubMed] [Google Scholar]
- Gorka, S. M. , Hedeker, D. , Piasecki, T. M. , & Mermelstein, R. (2017). Impact of alcohol use motives and internalizing symptoms on mood changes in response to drinking: An ecological momentary assessment investigation. Drug and Alcohol Dependence, 173, 31–38. 10.1016/j.drugalcdep.2016.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant, B. F. , Goldstein, R. B. , Saha, T. D. , Chou, S. P. , Jung, J. , Zhang, H. , … Hasin, D. S. (2015). Epidemiology of DSM‐5 Alcohol Use Disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditons III. JAMA Psychiatry, 72(8), 757–766. 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant, B. F. , & Kaplan, K. D. (2005). Source and accuracy statement for Wave 2 of the 2004–2005 National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- Grant, B. F. , Kaplan, K. D. , Shepard, J. , & Moore, T. (2003). Source and accuracy statement for Wave 1 of the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- Grant, B. F. , Stinson, F. S. , Dawson, D. A. , Chou, S. P. , Dufour, M. C. , Compton, W. , … Kaplan, K. (2004). Prevalence and co‐occurrence of substance use disorders and independent mood and anxiety disorders. Archives of General Psychiatry, 61(8), 807–816. 10.1001/archpsyc.61.8.807 [DOI] [PubMed] [Google Scholar]
- Kessler, R. C. (2012). The costs of depression. Psychiatric Clinics of North America, 35(1), 1–14. 10.1111/j.1747-0285.2012.01428.x.Identification [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R. C. , Crum, R. M. , Warner, L. A. , Nelson, C. B. , Schulenberg, J. , & Anthony, J. (1997). Lifetime co‐occurrence of DSM‐III‐R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Archives of General Psychiatry, 54, 313–321. [DOI] [PubMed] [Google Scholar]
- Kessler, R. C. , McGonagle, K. a , Zhao, S. , Nelson, C. B. , Hughes, M. , Eshleman, S. , … Kendler, K. S. (1994). Lifetime and 12‐month prevalence of DSM‐III‐R psychiatric disorders in the United States; Results from the National Comorbidity Survey. Archives of General Psychiatryeneral Psychiatry, 51(1), 8–19. 10.1001/archpsyc.1994.03950010008002 [DOI] [PubMed] [Google Scholar]
- Khantzian, E. J. (1985). The self‐medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. American Journal of Psychiatry, 142(11), 1259–1264. [DOI] [PubMed] [Google Scholar]
- Khantzian, E. J. (1997). The self‐medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry, 4(5), 231–244. [DOI] [PubMed] [Google Scholar]
- Kleber, H. , Weiss, R. , Raymond, F. , George, T. , Greenfield, S. , Kosten, T. , … Ziedonis, D. (2006). Practice guideline for the treatment of patients with substance use disorders‐second edition. American Psychiatric Association, 1–276. [PubMed] [Google Scholar]
- Kraemer, H. C. , Stice, E. , Kazdin, A. , Offord, D. , & Kupfer, D. (2001). How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry, 158(6), 848–856. 10.1176/appi.ajp.158.6.848 [DOI] [PubMed] [Google Scholar]
- Kuo, P.‐H. , Gardner, C. O. , Kendler, K. S. , & Prescott, C. A. (2006). The temporal relationship of the onsets of alcohol dependence and major depression: Using a genetically informative study design. Psychological Medicine, 36(8), 1153–1162. 10.1017/S0033291706007860 [DOI] [PubMed] [Google Scholar]
- Kushner, M. , Sher, K. J. , & Erickson, D. J. (1999). Prospective analysis of the relation between DSM‐III anxiety disorders and alcohol use disorders. The American Journal of Psychiatry, 156(5), 723–732. 10.1176/ajp.156.5.723 [DOI] [PubMed] [Google Scholar]
- Lai, H. M. X. , Cleary, M. , Sitharthan, T. , & Hunt, G. E. (2015). Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: A systematic review and meta‐analysis. Drug and Alcohol Dependence, 154, 1–13. 10.1016/j.drugalcdep.2015.05.031 [DOI] [PubMed] [Google Scholar]
- Lazareck, S. , Robinson, J. A. , Crum, R. M. , Mojtabai, R. , Sareen, J. , & Bolton, J. M. (2012). A longitudinal investigation of the role of self‐medication in the development of comorbid mood and drug use disorders: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). The Journal of Clinical Psychiatry, 73(5), e588–e593. 10.4088/JCP.11m07345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeies, M. , Pagura, J. , Sareen, J. , & Bolton, J. M. (2010). The use of alcohol and drugs to self‐medicate symptoms of posttraumatic stress disorder. Depression and Anxiety, 27(8), 731–736. 10.1002/da.20677 [DOI] [PubMed] [Google Scholar]
- Lembke, A. (2012). Time to abandon the self‐medication hypothesis in patients with psychiatric disorders. The American Journal of Drug and Alcohol Abuse, 38(6), 524–529. 10.3109/00952990.2012.694532 [DOI] [PubMed] [Google Scholar]
- Liang, W. , Chikritzhs, T. , & Lenton, S. (2011). Affective disorders and anxiety disorders predict the risk of drug harmful use and dependence. Addiction, 106(6), 1126–1134. 10.1111/j.1360-0443.2011.03362.x [DOI] [PubMed] [Google Scholar]
- Martins, S. , Fenton, M. , Keyes, K. , Blanco, C. , Zhu, H. , & Storr, C. (2012). Mood and anxiety disorders and thier association with non‐medical prescription opiois use disorder: Longitudinal evidence from the National epidemiologic study on alcohol and related conditions. Psychological Medicine, 42(6), 1261–1272. 10.1017/S0033291711002145.Mood/Anxiety [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins, S. , Keyes, K. M. , Storr, C. L. , Zhu, H. , & Chilcoat, H. (2009). Pathways between nonmedical opioid use/dependence and psychiatric disorders: Results from the National Epidemiologic Survey on alcohol and related conditions. Drug and Alcohol Dependence, 103(1–2), 16–24. 10.1016/j.drugalcdep.2009.01.019.Pathways [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mclntyre, R. S. , Rosenbluth, M. , Ramasubbu, R. , Bond, D. J. , Taylor, V. H. , Beaulieu, S. , … Schaffer, A. (2012). Managing medical and psychiatric comorbidity in individuals with major depressive disorder and bipolar disorder. Annals of Clinical Psychiatry, 24(2), 163–169. [PubMed] [Google Scholar]
- Menary, K. , Kushner, M. , Maurer, E. , & Thuras, P. (2011). The prevalence and clinical implications of self‐medication among individuals with anxiety disorders. Journal of Anxiety Disorders, 25(3), 335–339. 10.1016/j.janxdis.2010.10.006.The [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas, K. R. , & Mcclair, V. L. (2012). Epidemiology of substance use disorders. Human Genetics, 131(6), 779–789. 10.1007/s00439-012-1168-0.Epidemiology [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai, R. , Olfson, M. , & Mechanic, D. (2002). Perceived need and help‐seeking in adults with mood, anxiety, or substance use disorders. Archives of General Psychiatry, 59, 77–84. 10.1001/archpsyc.59.1.77 [DOI] [PubMed] [Google Scholar]
- Possemato, K. , Maisto, S. A. , Wade, M. , Barrie, K. , McKenzie, S. , Lantinga, L. J. , & Ouimette, P. (2015). Ecological momentary assessment of PTSD symptoms and alcohol use in combat veterans. Psychology of Addictive Behaviors : Journal of the Society of Psychologists in Addictive Behaviors, 29(4), 894–905. 10.1037/adb0000129 [DOI] [PubMed] [Google Scholar]
- Prior, K. , Mills, K. , Ross, J. , & Teesson, M. (2017). Substance use disorders comorbid with mood and anxiety disorders in the Australian general population. Drug and Alcohol Review, 36(3), 317–324. 10.1111/dar.12419 [DOI] [PubMed] [Google Scholar]
- Regier, D. A. , Farmer, M. , Rae, D. , Locke, B. , Keith, S. , Judd, L. , & Goodwin, F. (1990). Comorbidity of mental disorders with alcohol and other drug abuse: Results from the Epidemiologic Catchment Area (ECA) Study. JAMA, 264(19), 2511–2518. 10.1001/jama.1990.03450190043026 [DOI] [PubMed] [Google Scholar]
- Robinson, J. , Sareen, J. , Cox, B. J. , & Bolton, J.M. (2009a). Self‐medication of anxiety disorders with alcohol and drugs: Results from a nationally representative sample. Journal of Anxiety Disorders, 23(1), 38–45. 10.1016/j.janxdis.2008.03.013 [DOI] [PubMed] [Google Scholar]
- Robinson, J. , Sareen, J. , Cox, B. J. , & Bolton, J. M. (2009b). Correlates of self‐medication for anxiety disorders. The Journal of Nervous and Mental Disease, 197(12), 873–878. 10.1097/NMD.0b013e3181c299c2 [DOI] [PubMed] [Google Scholar]
- Robinson, J. , Sareen, J. , Cox, B. J. , & Bolton, J. M. (2011). Role of self‐medication in the development of comorbid anxiety and substance use disorders: A longitudinal investigation. Archives of General Psychiatry, 68(8), 800–807. 10.1001/archgenpsychiatry.2011.75 [DOI] [PubMed] [Google Scholar]
- Sareen, J. , Chartier, M. , Kjernisted, K. D. , & Stein, M. B. (2001). Comorbidity of phobic disorders with alcoholism in a Canadian community sample. Canadian Journal of Psychiatry, 46, 733–740. [DOI] [PubMed] [Google Scholar]
- Sareen, J. , Chartier, M. , Paulus, M. P. , Stein, M. B. , Lieb, R. , Wittchen, H.‐U. , … Kupfer, D. J. (2006). Illicit drug use and anxiety disorders: Findings from two community surveys. Psychiatry Research, 142(1), 11–17. 10.1016/j.psychres.2006.01.009 [DOI] [PubMed] [Google Scholar]
- Swendsen, J. , Merikangas, K. , Canino, G. , Kessler, R. , Rubio‐Stipec, M. , & Angst, J. (1998). The comorbidity of alcoholism with anxiety and depressive disorders in four geographic communities. Comprehensive Psychiatry, 39(4), 174–184. 10.1016/S0010-440X(98)90058-X [DOI] [PubMed] [Google Scholar]
- Walley, A. Y. , Paasche‐Orlow, M. , Lee, E. C. , Forsythe, S. , Chetty, V. K. , Mitchell, S. , & Jack, B. W. (2012). Acute care hospital utilization among medical inpatients discharged with a substance use disorder diagnosis. Journal of Addiction Medicine, 6(1), 50–56. 10.1097/ADM.0b013e318231de51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittchen, H. U. (2002). Generalized anxiety disorder: Prevalence, burden, and cost to society. Depression and Anxiety, 16(4), 162–171. 10.1002/da.10065 [DOI] [PubMed] [Google Scholar]
- Wolitzky‐Taylor, K. , Bobova, L. , Zinbarg, R. , Mineka, S. , & Craske, M. (2012). Longitudinal investigation of the impact of anxiety and mood disorders in adolescence on subsequent substance use disorder onset and vice versa. Addictive Behaviors, 37(8), 982–985. 10.1016/j.addbeh.2012.03.026.Longitudinal [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaworski, D. , Robinson, J. , Sareen, J. , & Bolton, J. M. (2011). The Relation between nicotine dependence and suicide attempts in the general population. The Canadian Journal of Psychiatry, 56(3), 161–170. 10.1177/070674371105600306 [DOI] [PubMed] [Google Scholar]
- Zhou, H. , Polimanti, R. , Yang, B.‐Z. , Wang, Q. , Han, S. , Sherva, R. , … Gelernter, J. (2017). Genetic risk variants associated with comorbid alcohol dependence and Major depression. JAMA Psychiatry, 74(12), 1234–1241. 10.1001/jamapsychiatry.2017.3275 [DOI] [PMC free article] [PubMed] [Google Scholar]


