Abstract
Evidence from Sierra Leone reveals the significant limitations of big data in disease detection and containment efforts. Early in the 2014–2016 Ebola epidemic in West Africa, media heralded HealthMap's ability to detect the outbreak from newsfeeds. Later, big data—specifically, call detail record data collected from millions of cell phones—was hyped as useful for stopping the disease by tracking contagious people. It did not work. In this article, I trace the causes of big data's containment failures. During epidemics, big data experiments can have opportunity costs: namely, forestalling urgent response. Finally, what counts as data during epidemics must include that coming from anthropological technologies because they are so useful for detection and containment.
Keywords: global health, technology, big data, Ebola, cell phones, digital humanitarianism
At the center of big data approaches to Ebola containment in West Africa is a curious, yet oddly essential question: What is it about a cell phone—as thing and social artifact—that has any meaningful correlation to the containment of the often‐fatal hemorrhagic disease? To answer this, we must return to how cell phones became part of the effort to contain the largest known outbreak of Ebola. In 2014, global public health epidemiologists theorized that cell phones could provide the data necessary to stop Ebola's spread. They counted on the signals cell phones send and receive from cellular towers to leave a trail and thus create digital data sets for tracking people who might be spreading Ebola. Cell phones would serve, according to this logic, as beacons of contagion, signalling the mobility patterns of people with the disease. In this article, I show that this proposition was flawed largely because of what Harvard‐based computational epidemiologists1 did not know. They did not know that cell phones and people's selves are related in ways that are not universally shared across nations, cultures, and peoples. These experts did not recognize what might be called the “thing‐self” problem of cell phones. Focusing on a particular zone of global public health engagement in Sierra Leone2 in 2014, I describe here how, in a race against time, big data enthusiasts—who understood neither the social lives of cell phones nor the geographies of Ebola—oversold advantages of big data technologies.
To explain the mistakes surrounding Ebola‐containment‐by‐phone ambitions, I take up the cell phone's thing‐ness. Throughout the world, the centrality of the cell phone in people's lives originate in its “thing‐power,” what Jane Bennett has called the condition of a thing that “commands attention as vital and alive in its own right” (Bennett 2004, 350). Cell phones are powerful black boxes that house mechanisms that can appear omniscient but in fact can be broken out and examined. Moreover, the thing‐power of cell phones is shaped by its grouping, its assemblage with other things and subjectivities. The power of the particular public health assemblage deployed here, connecting cell phones to big data to Ebola, was based on an assumption that things and people exchange properties (Bennett 2004, 355). Computational epidemiologists faithfully believed that things—cell phones—would work as if they were interchangeable with the people who owned them: Tracking a cell phone would mean following a person. This was the first of several ways that the cell phones’ thing‐self problem entered. Mistaking the cell phone for a person, and vice versa, was where the public health assemblage first went off‐track. Unfortunately, this mistake became fixed in later calculations and conceits, as I will explain.
Relative to their big data–Ebola aspirations, computational epidemiologists misunderstood the self. Anthropologists have long noted how conceptions of the self vary from place to place (e.g., Hallowell 1955; Piot 2010; Rosaldo 1980; Stathern 1988; Stoller 1999). In the cell phone–big data–Ebola conjunction, though, it was assumed that a West African and her or his cell phone would be synonymous, operating as one, with an identity that is singular and stable. In short, computational epidemiologists presumed universal phone‐self subjectivities that followed North American proclivities. As Lesley Alderman observed: “[We Americans] have an intimate relationship with our phones. We sleep with them, eat with them and carry them in our pockets. We check them, on average 47 times a day—82 times if you're between 18 and 24 years old” (Alderman 2017, also citing Deloitte 2016). In Sierra Leone, there is a far looser link between cell phone ownership and identity, and certainly no one‐to‐one synecdoche of self and phone.
The attempt to use big data in 2014 during the initial West African Ebola humanitarian response is part of a larger global humanitarian aid movement. Big data is both a technology and a foundation for other technologies, and has been heralded as a new organizational necessity for crisis response and management (Qadir et al. 2016; Watson et al. 2016). “Digital humanitarians” (Conneally 2011; Meier 2015; PLoS 2012) aim to apply big data analytics to humanitarian relief via, for example, participatory mapping, crowdsourcing translation, and real time social media communications. As a former international development worker and unapologetic pragmatist, I must disclose that I lean heavily toward endorsing these approaches. I believe that intensely localized needs‐based humanitarian problem‐solving technologies involving big data analytics for in‐the‐moment mapping, language translation, and online emergency dispatch can work. But big data applications to humanitarian aid are not uniform and universal in their utility.
In what follows, I analyze two cases: HealthMap's claim of Ebola detection and Harvard‐based computational epidemiologists’ claim for Ebola containment, neither of which worked in Sierra Leone as advertised. Big data outputs were intended to be deployed at a distance (from Boston), in a dismissal of the actual (e.g., Ebola transmission from caring for the sick and funeral preparations in Sierra Leone) in favor of the speculative and anticipatory (Adams et al. 2009, 247). In calculative acts of computer reckoning rather than on‐the‐ground human engagement, big data experts championed “mode[s] of anticipation [that did] not need actual objects or events” (Adams et al. 2009, 257) to justify experimenting with technologies mid‐epidemic.
To show how all this worked in Sierra Leone I draw from research done over 2013–2014 on data use in humanitarian aid, funded by the Social Sciences and Humanities Research Council of Canada. In that project, I explored global health as an interactive global social field where humanitarian activities by state and non‐state actors at all levels of income were included. I relied on and received help from three graduate students studying health statistics in various capacities. We conducted participant observation for three months or more each, lived in the capital city of Sierra Leone, Freetown, and made several trips to smaller cities and towns. All team members spoke Krio, the local lingua franca, and some Mende, and one member spoke both languages fluently. More than 70 one‐on‐one interviews were conducted, and all were transcribed and coded. Data for this article emerged from the primary data collected. The study was approved by the Simon Fraser University Research Ethics Board, study number 2012s0643.
In what follows, I first take up how HealthMap's Ebola detection algorithm was represented in North American media in ways that hyped big data as a break‐through technology and shortchanged what Sierra Leoneans knew and when they knew it. I then turn to how a prototype Harvard study that modeled malaria exposures using cell phone data became a de facto exemplar for Ebola. I show the ways the model did not translate well to Ebola, citing ethnographic descriptions of how Sierra Leoneans actually use their cell phones; the problem of estimates; and the lack of network coverage. I then turn to the opportunity costs of mid‐epidemic experimentation and concerns about health surveillance by phone and drone. I conclude with discussion of the value of ethnographic data and narrative knowledge in effective disease containment.
Background: Ebola Outbreak in Sierra Leone
The first West African case of Ebola occurred in December 2013 (Baize et al. 2014) in Guéckédou district, Guinea, an area bordering Liberia and known as the “parrot's beak,” for its shape and the way it dips into the far eastern part of Sierra Leone near Kailahun. By July 2016, when Ebola was finally contained in the three countries most impacted by the disease—Guinea, Liberia, and Sierra Leone—a total of 28,616 people had had Ebola, 11,310 of whom had died. Sierra Leone, a country of 6 million people, had almost half the cases in the region, 14,122, and about a third of the deaths, 3,955 (WHO 2016a) (see Figure 1).
Figure 1.
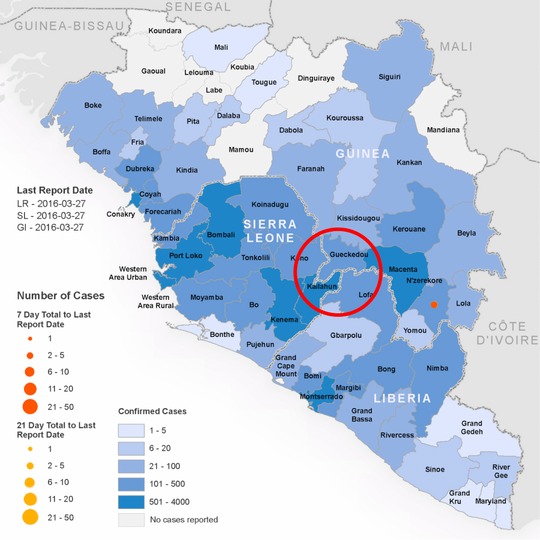
Geographical distribution of new and total confirmed cases in Guinea, Liberia, and Sierra Leone, as of March 27, 2016 (WHO 2016b), at the end of the epidemic. Author added red circle indicating the originating city, Gueckedou, and the environs at the borderlands of Sierra Leone, Liberia, and Guinea. [This figure appears in color in the online issue]
The same region had been pummeled during decade‐long wars in Liberia and Sierra Leone. I lived in the eastern province for two years prior to the war in Sierra Leone, and when I visited this area again in 2008, the region was drastically different, war‐torn. Alluding to that area, a teacher told me, “We don't have a wild west, we have a wild east.” Sierra Leoneans often talk about the region as loosely organized politically and beyond the reach of Freetown governance. The region retained the highest number of weapons after the war, despite a nation‐wide UN disarmament project. Just before Ebola hit, the region was not actively inundated by violence, but there were more annual isolated events involving firearms than in other parts of the county. In terms of infrastructure, this area was the most devastated by the wars in Sierra Leone and Liberia, and economically it was the least recovered area a decade after the war in Sierra Leone ended in 2002. Historically, this region where Sierra Leone, Liberia, and Guinea meet was divvied up by colonial powers without regard for extant family, village, and regional ties; there is a long history of cross‐border traffic, relationships, and market exchange (see Silberfein and Conteh 2006). Cross‐border porousness contributed not only to Ebola's spread, but also complicated disease containment efforts.
Big Data as an Anticipatory Technology
Big data is much talked about but often not clearly defined. By big data I mean those overly large digital data sets coming from many sources and that require computational software to make some kind of meaning. In the health sector, digital data can be extracted from any mix of electronic health records, diagnostic images, lab tests, biometric scans, patient phone calls, insurance claims, and population health databases. Big data collection in health care is a grab‐bag of collection‐sites—what Gerrie (in Webster 2014) has called “total patient data capture” and what Cukier and Mayer‐Schönberger (2013, 31) hail as N = all.
The aim is to have massive data stores at the ready for any future question or hypothesis. Governments and corporations alike now keep and curate such databases in which data are collected, aggregated, and analyzed in relation to a question or need. This method of analysis, some argue, is the opposite of the scientific method, since it does not establish a research question first and collect data second. In a spirited and seminal promotion of big data in 2008, Chris Anderson, the editor‐in‐chief of Wired at the time, summed up this new world ordering by arguing that big data would make the scientific method obsolete (2008, 1). With big data, no one has to decide ahead of time what constitutes the exact data that will answer a question, they just need massive volumes of collected data, computer hardware, and software from which to “source” the answer. Or so the thinking goes.
Big data problem‐solving capacities can appear infinite and evoke a pleasing sense of what Taussig et al. (2013, S3) have called the affective potentiality “to imagine particular human futures, and to warn against undesirable outcomes.” Big data is believed to be advantageous and profitable in some societal sectors (Mayer‐Schönberger and Cukier 2013), but questions remain about the degree to which health is one of those sectors. Some public health academics and practitioners (Anema et al. 2014; Salathé et al. 2012) laud the potential of big data health applications; others are more circumspect (e.g., Letouzé and Vinck 2015; McDonald 2016).
In Sierra Leone, I heard expatriate international development workers working with large data sets talk about how “the big numbers take care of the independent variables,” as one NGO consultant put it. “We don't have to sample any more,” said another, “because now we've got it all beforehand.” He explained that data from many sources means that everyone is taken into account at the start and that a lot of data means (sui generis) that problematic contextual and situational variabilities will disappear. Sampling biases are assumed to become nonexistent because data samples include entire populations; that there can be no bias if everyone is counted. Cukier and Mayer‐Schönberger (2013, 31) have characterized this historical shift like this:
[W]e might have to give up on clean, carefully curated data and tolerate some messiness. This idea runs counter to how people have tried to work with data for centuries. Yet the obsession with accuracy and precision is in some ways an artifact of an information‐constrained environment. When there was not that much data around, researchers had to make sure that the figures they bothered to collect were as exact as possible. Tapping vastly more data means that we can now allow some inaccuracies to slip in (provided the data set is not completely incorrect), in return for benefiting from the insights that a massive body of data provides.
This move in the field of statistics from “some to all and from clean to messy” has meant that correlations (Cukier and Mayer‐Schönberger 2013, 31–32)—i.e., the way enumerated variables appear to affect one another—take on greater significance. This has prompted some big data‐influenced sectors in global health to move away from deeper “why” explanations of health phenomena; big data analytics can only find simple associations between phenomena, not answer how or why questions. It was this low threshold of association that Harvard computational epidemiologists used when they strategized the application of a big data model for malaria migration to Ebola containment. First, though, I explore the limitations of big data when it comes to disease detection. Unlike disease containment, big data detection does not require cell phone data, just large data sets from online newsfeed chatter.
Specious Claims of Early Ebola Detection by Big Data
In late summer–early fall of 2014, when the world began to take seriously the Ebola epidemic in West Africa, news magazines (Schlanger 2014), blogs (Public Health Watch 2014), and e‐news (Ngowi 2014) were prolific with praise about the good uses to which big data had been put at the start of the crisis. Fast Company headlined “How This Algorithm Detected the Ebola Outbreak before Humans Could” (Titlow 2014). This article, like many others, describes how HealthMap (2014a), an online global disease monitoring platform, picked up on Ebola nine days before the World Health Organization (WHO) announced its presence on March 23, 2014 (see Figure 2). In the vast majority of accounts, HealthMap was prominently featured, and the Associated Press went so far as crediting HealthMap as the “online tool [that] nailed Ebola” (Associated Press 2014). Similarly, HealthMap co‐founder John Brownstein was widely credited with the early detection and surveillance of Ebola (i.e., Wikipedia 2018).
Figure 2.

Typical media hype about big data detecting Ebola: “Machines saw the outbreak coming a week before the world knew about it” (Titlow 2014). [This figure appears in color in the online issue]
In 2014, HealthMap (2014b) described its disease detection process this way:
HealthMap brings together disparate data sources, including online news aggregators, eyewitness reports, expert‐curated discussions and validated official reports, to achieve a unified and comprehensive view of the current global state of infectious diseases and their effect on human and animal health. Through an automated process, updating 24/7/365, the system monitors, organizes, integrates, filters, visualizes and disseminates online information about emerging diseases in nine languages, facilitating early detection of global public health threats. … HealthMap's content is aggregated from freely available information from the following sources: ProMED Mail, World Health Organization, GeoSentinel, World Organisation for Animal Health, Food and Agriculture Organization, EuroSurveillance, Google News, Moreover, Wildlife Data Integration Network, Baidu News, SOSO Info. … HealthMap is a Linux/Apache/MySQL/PHP application and relies on the following open products: Google Maps, GoogleMapAPI for PHP, Google Translate API, xajax PHP AJAX library, Fisher‐Robinson Bayesian filtering.
To make sense of this amalgam of sources, HealthMap uses an algorithm widely credited to a single software developer and the other HealthMap co‐founder, Clark Freifeld. It is not open source, meaning that the algorithm is not publicly published. But this is known: The code instructs HealthMap computers about which newsfeed words to find and which news accounts to flag for inclusion3 in HealthMap visuals (world maps with red dots representing disease outbreaks). Interns then scour (clean) the flagged data for repetitions and relevance. Decisions about data selection, weightedness, and sequence (choosing which accounts count, in what order, and by how much) as well as the translations of these decisions to computer code are made by HealthMap's two co‐founders. In news reports, the subjective dimensions of HealthMap processes, particularly the choices made by the two men and a handful of interns, are obscured and minimized. While this is not reason to dismiss HealthMap outright, knowing how it works allows us to raise the spectre of unexamined biases, unselfconscious omissions, and special interests, and bring into question HealthMap's reported objectivity and omniscience.
Retrospectively, it is fair to say that the hype about big data's genius, particularly for early detection of Ebola, was misplaced. HealthMap's algorithm missed some of the very first notifications about “patients with Ebola‐like symptoms” because they were published in French and the algorithm was coded for English. Additionally, “[b]y the time HealthMap monitored its very first report, the Guinean government had actually already announced the outbreak and notified the WHO” (Leetaru 2014), making its work as a detection tool seem redundant at best. But the biggest blow to claims of HealthMap's algorithmic supremacy is the simple fact that a disease outbreak must first be reported—thus already detected—for the HealthMap algorithm to pick it up.
In early March 2014, I was in Freetown, which is about 250 miles from the Guinean site of the first confirmed death from Ebola. I read about a “strange hemorrhagic fever presenting like Ebola” for the first time on February 27, 2014 from an online newsfeed. I am sure I was not the first person in Freetown to learn of the case; Sierra Leoneans in the Ministry of Health and Sanitation were talking about Ebola in eastern Sierra Leone from early March 2014 onward. During the first two weeks of March, public health workers were anxious and began planning a response. They were just waiting, they said, for laboratory confirmation of Ebola cases in Sierra Leone before they initiated official interventions (positive lab results were delayed and were not officially announced until May 2014). In the meantime, there was intragovernmental push back against public health prevention campaigns. Ministries overseeing both the economy and finance were concerned about what closing the borders would mean to the post‐conflict improvements in Sierra Leone's economic outlook, which in early 2014 were significant and promising. Then, because there was so little reaction in March on the part of the WHO and the international NGOs, panic eased and then quieted almost completely, only to resurge in force in May 2014 when Ebola case numbers in Sierra Leone soared and deaths multiplied.
Big data could not capture or predict the kinds of things that were being said, done, and thought on the ground, seen by anthropologists but ignored by WHO officials, that led to the epidemic levels of Ebola during the 2014–2016 West African outbreak. HealthMap's ability to simply note disease incidence did not help anyone predict that Ebola would spread from its originating Guinean site to its pandemic proportions. HealthMap, after all, identifies disease outbreaks every day that do not become pandemics. Arguably, community health workers and anthropologists working in the area would have been able to predict the likely social factors that would lead to disease spread, had they been consulted in March 2014.
HealthMap is an interesting and valuable platform for visualizing disease. But the heralded links between its algorithm, early detection, and improved health outcomes were not evident for the Ebola epidemic. Ultimately, the hype about big data's capability for containment, the topic to which I now turn, was eclipsed by the hype about HealthMap's detection proficiency. But the unmet promises and lost opportunity costs of the containment hype were graver.
First Principles of Containment, or How to Use a Cell Phone to Locate a Person
Early in the 2014–2016 Ebola outbreak, headlines like “How Big Data Could Help Stop the Spread of Ebola” (Public Radio International 2014) (Figure 3) appeared, championing big data as a tool for tracking people contagious with Ebola in real‐time. How? Broadly speaking, the process relies not so much on people being tracked as the cell phones they carry being tracked. There are three ways to accomplish this: via global positioning system (GPS), cell phone tower triangulation, and/or with a phone's call detail record (CDR).
Figure 3.

Typical media hype about big data containing Ebola: “How ‘big data’ could help stop the spread of Ebola” (Public Radio International 2014). [This figure appears in color in the online issue]
With GPS, a chip in a cell phone sends and receives intermittent signals from a constellation of about 30 satellites orbiting earth, the vast majority of which are owned and operated by the U.S. Department of Defense.4 Cell phone companies buy or rent software to operate location services using these satellites. Three to four GPS satellites are typically involved in locating a cell phone, calculating its location based on the length of time a cell phone signal takes to travel to the satellites. In Sierra Leone, where older and refurbished cell phones are commonplace and GPS chips far less likely, GPS location finding has considerable limitations. One young Sierra Leonean, Abu, was quick to point out to me that cell phone sellers in Freetown markets regularly modify cell phones, taking out a chip from one cell phone to add to another, and then pricing each accordingly.
Cell phone triangulation, a separate method, relies on three towers communicating with a single cell phone. Signals, called pings, are regularly sent and received by cell phones each time a cell phone passes a cell phone telecommunications tower. People could be carrying the cell phone and pass on foot, with a car, or while on public transportation. A cell phone's digital footprint is the result of a cell phone sending time‐coded signals to the cell phone towers in its area. The distance in time from the three footprints and their concentric overlap helps to calculate where the cell phone is located, within a half mile or so (see Figure 4).
Figure 4.

Finding location with cell phone triangulation. Illustration by Nichola Henne. [This figure appears in color in the online issue]
During the Ebola epidemic, computational epidemiologists were intent on employing a third method—using the CDR data collected and stored by West African cell phone companies. CDR are digitally warehoused by cell phone company servers and can show where cell phones have been. They show the calling history, times of calls, duration, the phone tower or towers used for calls, and more. Using CDR logs, computational epidemiologists can estimate callers’ longitude and latitude coordinates (though there is the same delay as with Google traffic maps, which shows the traffic that recently happened, not the traffic we find en route). It was the estimates of callers’ longitude and latitude coordinates that empowered the epidemiologists to think that by following a cell phone through space and time, from cell phone tower to cell phone tower, CDR data would show where Ebola‐sick people go. In theory at least, CDR data roll disease ecology and cell phone triangulation information into one public health “disease disaster management” technology believed to be capable of delivering populations ready for any necessary humanitarian health interventions (e.g., Cinnamon et al. 2016).
In the Harvard prototype model, computational epidemiologists used CDR data in an algorithm that calculated how far people travel from the geographic point considered their base, usually their home. Their algorithm used an equation called “the radius of gyration,” which calculated human travel, such as regular travel between work and home, for millions of Kenyans (see Figure 5). The radius of gyration was calculated for each call record (Wesolowski et al. 2013, 5), and collectively, the calculations show population density shifts.
Figure 5.
Equation for radius of gyration used in human mobility studies (Wesolowski et al. 2013, 5).
Processing big data sets like millions of CDRs requires algorithms (i.e., step by step instructions, including factors like the radius of gyration equation). The algorithm then needs to be written as computer code. Computer coders “create this world on a machine that can understand and execute only simple commands. You do this solely by writing precise instructions, often many hundreds of thousands of lines long” (Derman 2004, 107). The aim is to make up an instructional computer code that matches the desired result—in this case, estimating where a person has traveled and, with the intent of trying to predict, where they are likely to go next.
Harvard computational epidemiologists had worked out the CDR big data mechanics for malaria migration, as described in a later section, and in 2014, they were eager to use CDRs in West Africa to apply their malaria model to Ebola. Not only did they face opposition to their use of CDRs on human rights, privacy, and consent grounds (see also McDonald 2016), but, as I show next, the black‐boxed big data calculations were scaffolded onto a false first principle that cell phones are people.
Containment Counterfactual: The Phone Is Not Self in Sierra Leone
In this section, I explain why Ebola‐containment‐by‐cell‐phone could not work. Despite the fact that cell phone use5 in Sierra Leone is reported for 94% of the population (BuddeComm 2017),6 cell phones do not work well as beacons of individual identity and precise whereabouts because they are not synonymous with individual people. Many Sierra Leoneans possess cell phones, but this possession is often temporary, even fleeting. Cell phones are loaned, traded, and passed around among family and friends, like clothes, books, and bicycles. A single phone can be shared by an extended family or, in rural areas, a neighborhood or a village. Cell phones are fluid, exchangeable, and relational. Abdul, a 17‐year‐old high school student living in a neighborhood in Freetown, told me he'd had six cell phones in five years: One was from his aunt “who brought it in for him from the diaspora”; two had been “stolen,” but he knew who had them; and one he gave to a friend who “needed it more.” Abdul described his favorite Nokia cell phone as a “pink laptop,” meaning it was a pink cell phone with a slide‐out keyboard. At the moment of our interview, Abdul had three cell phones and numerous SIM cards. For many cell phone users in Freetown, having more than one phone was common.
Outside of larger cities, fewer Sierra Leoneans have cell phones. But in Freetown and Kenema, the capital city of the Eastern Province, I met many people who had more than one. They used several different phone networks, because “out‐of‐network calls cost too much,” Emmanuel, one of Abdul's workmates, explained. Almost all of the Sierra Leonean physicians I met had more than one cell phone, but “you don't have to be rich to have a lot,” Emmanuel said. An HIV/AIDS counselor, Fatmata, had four cell phones, one for each primary phone network, because calling outside of a network was more expensive than having four separate cell phones. Abdul pointed out to me that network access could be accomplished by having multiple SIM cards, rather than many cell phones. But Fatmata told me she liked separating the networks by phone to help her manage her various roles—as a health care worker, as a mother, as a friend, and as a small business owner. The networks did not fall neatly along these groupings, she admitted, but “aw foh du” (“it doesn't matter”). Another reason to have many cell phones, Fatmata pointed out, is how much time it takes to charge the battery. Electricity in her Freetown neighborhood is irregular, so one or two cell phones charge while she uses the others.
Few people had cell phone plans; buying topup (credit) from a general store kiosk was preferred, but topup availability can be a hit or miss proposition, especially when moving about. Cell phone plans, with their regular payments each month, do not make much economic sense in an environment that experiences high degrees of economic precarity, as is the case in Sierra Leone. Fatmata, for example, despite her high status salaried job as an HIV/AIDS counselor, has gone for months at a time without being paid her salary because of donor funding delays, withholdings, and departures.
When I started the 2014 research work in Sierra Leone, I was at Lungi, the Freetown airport, when I bought a SIM card for a low‐end, no‐flip, not‐smart, two‐band Nokia 1208 “candybar” cell phone (because it is shaped like a mid‐sized candybar). (The phone is nearly indestructible; when I drop it, it bounces. I bought it in Freetown in 2008 and continue to use it regularly to this day in Sierra Leone and Germany, another two‐band country.) At the airport, I bought the SIM card, which instantaneously gave me a phone number and free minutes, from a vendor who pulled it from a rubber‐banded stack of the plastic cards with embedded break‐away SIMs he kept in the breast pocket of his cotton button‐down shirt. We made the transaction through a shuttle bus window in the airport parking lot at dawn. I paid 30,000 Leone or about $6 USD. The exchange was completely transactional; no name or address was asked for, none was given. Unlocked phones using credit loaded to the SIM card, not pay‐monthly phone plans, are the norm in Sierra Leone.
Later, when I inquired about buying genuine Apple, Samsung, and Nokia products, I was sent by several people to a store owner who was well stocked with the latest iPhones and iPads, as well as the latest Samsung Galaxy cell phones. She asked me to call one month in advance of needing them; she brought merchandise about twice a month in her luggage into Freetown from Dubai. Alternatively, cheap cell phones are sold in the central downtown Freetown market (Figure 6). Usman, one of about 10 young men in Freetown's Aberdeen neighborhood who regularly traded information and expertise about the latest cell phone apps and cheap downloads, was a discerning consumer when it came to buying cell phones from the market. He showed me how to check a cell phone's serial number: Press (*#06#) to tell if it was a genuine product. Start with the cell phone's weight, he said. “When you hold it … well, the light ones we call ‘duplicates’ and they have nothing inside … you want to see when you open it [that] it is made in Korea or Finland.” Be sure to write down your serial number, Usman coached. That way, I could keep track of it. Even if I lost my phone or someone “borrowed” it, he said, “you can still lock it so the thief cannot use it.” He had an app for that. Best to keep some additional phones, just in case.
Figure 6.

Cell phones at Freetown market. Photo by Sam Eglin. [This figure appears in color in the online issue]
Calling within networks, sharing a cellphone, tasking a phone per role, or juggling the precarities of electricity and the local economy are reasons to have more than one cell phone and SIM card in Sierra Leone. What computational epidemiologists missed is that one cell phone does not equal an individualized, unique self. Studying cell phone data sheds no light on actual identity and social attachments. Next, I elaborate on the several remaining reasons why the public health model linking cell phones to containment of the Ebola virus was flawed from its start.
Modeling Ebola Transmission with Malaria Disease Exemplars
One of the reasons cell phones were conscripted in the fight to contain Ebola was that they were previously used to track malaria. Before Ebola, cell phone data were championed for revealing links between human migration and malaria parasite travel. In a 2012 Harvard study, CDR data from 14,816,521 cell phones users in Kenya who traveled from home to work in 2008 and 2009 (Wesolowski et al. 2012, 268) showed that human migration patterns contribute to the spread of malaria. In the study, Carolyn Buckee and her colleagues found that East African labor migration was a factor in malarial disease ecologies. In short, they reported that when people carrying malarial parasites in their bloodstream (which is common even when people do not feel sick) traveled from home to new areas for work, there was an uptick in malarial incidence in areas where they went. More people in malaria endemic environments means higher concentrations of malarial parasites in a population and increased probability for higher malaria prevalence7 rates. The computational epidemiologists confirmed this by correlating: (1) cell phone data movement records and (2) Kenyan malaria prevalence estimates before and after labor migration. This knowledge, of course, does not come exclusively from cell phone data; many would argue that this knowledge is common sense, widespread, and not new. But confirming the correlations with cell phone data was new, and the research methodology was distinguished as a “breakthrough technology of 2013” (Talbot 2013).
When Ebola began to spread in West Africa in early 2014, Buckee and colleagues at Sweden's Karolinska Institute were eager to apply the same technology to a new disease. They intended to use CDR data to construct maps to show where Ebola‐infected people were, “where they were traveling to, and the effects of government health warnings and travel advisories on the public's movements” (The Economist 2014). They forged confidently ahead with the conviction that the “benefits of [using] CDRs in the context of the current Ebola outbreak are clear” and uncontestable (Wesolowski et al. 2014b). They were mistaken on both counts. Their third mistake was to assume that Ebola transmission was driven by human mobility (Wesolowski et al. 2014b, 2), rather than by activities that proved to be the primary transmission vectors: the social intimacies of caring for the sick and funeral preparations (see also Richards et al. 2015).
In disease containment, correlations alone are very weak points of departure for education and eradication campaigns. Statistical correlations simply do not provide enough useful information to bring about meaningful and improved outcomes in and of themselves; they must be accompanied by smart, granular public health interventions in malaria‐endemic areas. There is a vast anthropological literature on the interventions that lead to improved health outcomes (see also Chandler and Beisel 2017; Kamat 2013; Kelly and Beisel 2011; Packard and Brown 1997).
The computational epidemiologists’ gravest mistake was presuming that the model of an endemic problem (malaria) would apply to an epidemic (Ebola). The approximate ecologies of the Harvard study model could not be translated to Ebola containment for specific reasons. The contact tracing that brought an end to Ebola depended on knowing the exact person in an exact location with the disease. CDR data could not identify an individual cell phone user or if a cell phone user was sick with Ebola. CDR data only gave the Harvard researchers information about where millions of cell phones had gone, not where a person infected with malaria was.
Further, the 2012 malaria model used location and prevalence estimates. It analyzed 2008 and 2009 CDR data long after the fact, to estimate the locations of the nearly 15 million Kenyan cell phone subscribers. And, rather than actual cases of malaria, the study used 2009 estimates of malaria prevalence in targeted areas (Wesolowski et al. 2012, 268). Estimated location and prevalence—rather than specific people and incidence—are at the core of the Harvard study. In a revealing disclosure, at a 2012 digital disease detection conference at Harvard Medical School, the lead author of the Harvard study confidently stated: “You don't have to worry too much about face‐to‐face contact” (Buckee 2012) for the model to be valid. (Because the vector of contagion is the mosquito, malaria containment does not depend on fact‐to‐face contact with sick people. Control the mosquito, contain the disease.) With Ebola, contact tracing and care require fact‐to‐face contact. To assume that Ebola could be tracked in the same way malaria was tracked was to misunderstand the weaknesses of the correlative model itself as well as the modes of containment that could halt Ebola's spread.
Face‐to‐face contact tracing is largely responsible for bringing an end to the Ebola epidemic in Sierra Leone. Hundreds of Sierra Leoneans participated in contact tracing in Operation Os‐to‐Os (Operation House‐to‐House). Contact tracing is a labor intensive, low‐tech approach to containment, one that requires house‐to‐house visitations and face‐to‐face meetings with people who may be sick with Ebola or who have had direct contact with sick people. It is fair to say that CDR data had nothing to do with how the 2014–2016 Ebola containment campaigns actually worked.
Finally, the promise of Ebola containment by way of cell‐phone big data is easily undone by another simple fact: Using cell phones to detect human mobility requires network coverage. Network coverage outside of Freetown is spotty, even though cell phone towers have sprung up across Sierra Leone over the last 15 years in remote rural locations. In the parrot's beak area of Sierra Leone bordering Guinea and Liberia, as well as north and south of it—the site of the first outbreak and an area that experienced high Ebola mortality rates—thousands of people are regularly un‐ and underserved by cell phone coverage. Figure 7 shows the lack of reception in October 2014, mid‐epidemic.
Figure 7.
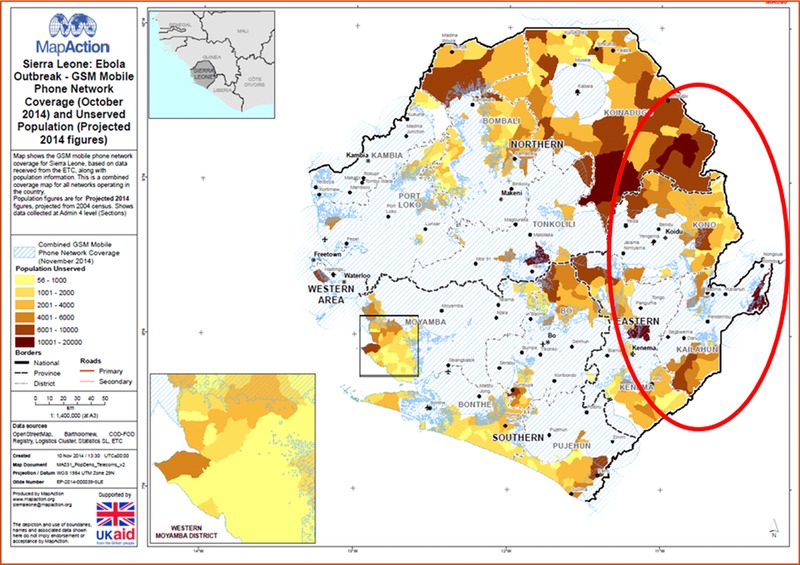
Mobile phone network coverage in Sierra Leone (MapAction 2014). Author added red oval indicating network coverage and non‐coverage near the initial Ebola outbreak areas at the borderlands of Sierra Leone, Liberia, and Guinea. [This figure appears in color in the online issue]
Pesky Issues of Data Access and Health Systems Yearnings
By the end of 2014, the Harvard study model was bedeviled by an earlier assumption that telecommunications companies would freely turn over CDR cell phone data during the Ebola crisis. West African telecommunications companies—Orange, Safaricom, Digicel, and others—have engaged a few times in what Robert Kirkpatrick has called “data philanthropy” (2011) for other public health ends (Wesolowski et al. 2014a). The computational epidemiologists assumed that telecommunications corporations would be philanthropic with their call record data during the epidemic (even though it is more commonly for sale). During the West African epidemic, soon after the WHO's August 2014 declaration that Ebola as an emergency of international concern, the computational epidemiologists pushed hard for CDR cell phone data access. UN and Sierra Leone government agencies were directly involved in discussions. But talks broke down and CDR data were not made available to the researchers. This overall failure of the containment plan in Sierra Leone has not prevented bragging about CDR data “break‐through[s]” during the Ebola epidemic in U.S. government reports (e.g., Fast and Waugaman 2016, 35).
The rise of big data solution‐making has been coincidental with the global ceding of meaningful commitment to the slow hard slog of building health care infrastructure in the places that need it most, as in Sierra Leone. During the Ebola crisis, the distracting buzz around big data followed decades of nation‐state withdrawal of public spending, mandated as a condition for Sierra Leone to get loan money for nation‐building from international development banks after its 1961 independence from British colonialism. Since the 1980s, conditional caps have been placed on salaries and payments for doctors, nurses, and other health care professionals. NGOs have filled health services voids since, but unevenly. Rural regions, like the area where Ebola first emerged, have the lowest levels of both health care practitioners and facilities.
When models promising public health miracles come out of academic domains like the Harvard School of Public Health, they are taken seriously and exert disproportionate influence in global public health decision‐making. The models tend to come with a certainty and clarity that feels hopeful amidst the chaos of emergency. Harvard models are given the benefit of the doubt, even when they lack basic implementation logic, as in this case. They are often uncritically enabled further by other global health leaders. Cell phone health technologies, for example, are promoted for use in humanitarian aid response by the WHO as a priority investment because it is “capable of target[ing] almost any disease—from haemorrhagic fevers to the common cold” (WHO 2014b).
Technologies, though, need local health infrastructure to plug in to in times of crisis and epidemic. “[E]conomies of fear, hope, salvation, and precariousness” (Adams et al. 2009, 260) can fuel the overselling of health futures that require massive hardware and software investments. Importantly, prioritizing experimental technology like big data for Ebola containment was at odds with what many interlocutors concerned with health care in Sierra Leone consistently say they want. They want primary health care infrastructure first. That would have been the best defense against Ebola, they say. Despite being well intentioned and prodigiously hyped, the big data technologies for detecting and containing Ebola had no demonstrable affect on Ebola containment or improved health outcomes. Technology troubles started with thing–self problems and only amplified with dependence on newsfeeds and networks that could not deliver respite in places where too few investments in health infrastructures have been made. Successful health technologies, at their most basic, are tools that get a job done to improve health outcomes. Successful health technologies, at their most basic, are tools that get a job done to improve health outcomes. Big data–Ebola containment tools did not meet this measure.
Troubling Data Technologies of Anticipatory Capture
Seared into my mind in a way I cannot unsee is the image a U.S. military officer composed as he imagined out loud a drone following a person presumed to be contagious or pre‐contagious with Ebola. We were sharing a meal at an international conference when he said that sick people would be identified and traced by their cell phone up to the point when a drone would take over the job. As he and his colleagues imagined it, the person would be living in a ubiquitous African village, and she or he would require surveillance because “they were a vector of contagion.” He anticipated capture literally. From his vivid description, my mind's eye saw a running man on the ground, pursued by a dark flying object—a drone—chased toward the open side door of a van, security forces ready to whisk him away. This is a chilling image in a place where South African mercenaries were hired by the Sierra Leonean government on the advice of expatriate global security advisors to shoot villagers presumed to be rebels from helicopters during a war not so long ago (Rubin 1997). In 2003, two years after the war's end, MI24 helicopter gunships and MI8 armed observation helicopters were a part of Operation Blue Vigilance, a UN peacekeeping mission (Silberfein and Conteh 2006) that regularly flew in the airspace over the same West African border region where Ebola first emerged. There is little question that any future public health surveillance by military drone would be a socially fraught intervention, as was the militarization of the Ebola epidemic more generally (see Benton 2014, 2017; Sandvik 2014).
The military officer I spoke with imagined the literal capture of people sick with Ebola. My use of anticipatory capture in this last section, however, is meant as a closing comment and prompt to think critically about data capture8 and epidemic problem‐solving. Global public health leadership—like the WHO, the World Bank, the Gates Foundation, and the UN—have pushed hard in the last two decades to build databases to bank health data from every country in the world. Now is a good time to ask broader and harder questions about data technology and its uses.
During an epidemic, what counts as essential data? What data will solve an emergency health crisis? What kind of data matter? For the West African Ebola case, containment solutions did not lie in being able to count how many people were infected and had died, though this was important for showing the world the magnitude and spread of the crisis. Even further removed from solving containment challenges was the CDR data that epidemiologists imagined would be collected from cell phones. Actual solutions, instead, were found in what West Africans and anthropologists already knew and could talk and write about. Epidemic solution‐making started in earnest with descriptive, narrative, and ethnographic data.
In September 2014, about the same time that computational epidemiologists were pushing the West African telecommunications companies to give them the CDR data and anthropologists were waving their hands for attention like keeners with an answer in class (e.g., Abramowitz 2014), the WHO issued a news brief titled, “Ebola Situation in Liberia: Non‐conventional Interventions Needed” (WHO 2014a). “Conventional Ebola control interventions are not having an adequate impact,” the brief said. A door opened; anthropologists and their work were about to be taken seriously. In a well‐told debrief by members of the UK's Ebola response anthropology platform, Fred Martineau and colleagues (2017) recall how U.K. humanitarian crisis policy makers began to turn to anthropologists for their expertise in September 2014. Anthropologists entered the conversations by noting that Ebola transmission was as much an attack on the social body as it was a deadly viral pathogen. They were able to explain that people were primarily getting sick from taking care of sick loved ones, a social obligation few could abandon. And people were getting sick when they prepared the dead for a dignified burial. West Africans and anthropologists were essential for explaining to the world how people were getting sick and what respectful disease containment could look like.
We live in a time when reasonable people feel righteous enough during an emergency of Ebola's magnitude to insist that local telecommunications companies devote energies and fixed resources to getting customer cell phone data to computer science labs in Boston rather than setting up and facilitating additional communication networks and satellite servers for medical responders in Ebola hot spots.9 In medical humanitarian crises, there is always the chance that new technologies will forestall more fundamental and essential steps and strategies of health crisis management. Even if the model had worked as the computational epidemiologists imagined, it would only have been capable of identifying vague geographies for additional interventions. The big data technology itself was not life‐saving; it could not do contact tracing, provide treatment, enable safe supported homecare, or engage in the dialog necessary to reimagine how safe and dignified burials could be conducted.
During the Ebola outbreak, did West Africans and anthropologists understand the nature of the health crisis better without big data? Yes, there is plenty of evidence that is true (e.g., AAA 2014; Abramowitz 2014; Lipton 2015; Moran 2017; Moran and Hoffman 2014; Spencer 2015; Wilkinson and Leach 2014). Computational epidemiologists may continue to play with what they believe is big data's unrealized potential during epidemics, but the world is better served when what counts as data in global health draws first from what people in affected communities and anthropologists already know. Like basic laboratory scientists, anthropologists mostly labor in relative obscurity until the granularity of knowledge they already have meets up with a course‐altering event or a problem that needs fixing. This mix can prompt spontaneous and indispensable problem‐solving insights. Disease containment strategies and policies have the best chance of working when they include field‐based engagement with in‐the‐moment social practices. Based on what actually worked to contain the 2014–2016 West African Ebola epidemic, when we are faced with the challenges of epidemic containment in the future, it is sensible to herald anthropological theory, method, data, and knowledge as anticipatory technologies of the first instance.
Acknowledgments
I am grateful for the opportunities I had to think about big data interventions with Claudia Derichs, Stephen Brown, Mubnii Morshed, Sylvanus Spencer, Baindu Kosia, Rayna Rapp, Linda Hogle, Duana Fullwiley, Stacy Pigg, Elizabeth Dunn, and Kirsten Bell. Special thanks to Richard Rottenburg, Songi Park, and colleagues of the Law, Organization, Science and Technology Network at the University of Halle. Thanks also to Iveoma Udevi‐Aruevoru, Puneet Grewal, Lukas Henne, Andrew Carpenter, and Stanford's 2017 Spring Department of Anthropology Workshop participants. The initial space to think about this article was during a sabbatical fellowship from the Centre for Global Cooperation Research, Käte Hamburger Kolleg, University of Duisburg/Essen, Duisburg, Germany. The Social Science and Humanities Research Council of Canada funded the 2013 and 2014 fieldwork research in Sierra Leone, Grant No. 430‐2012‐0128.
Notes
For ease of reference throughout this article, I use the term computational epidemiologists to categorize a group of big data academic researchers with far‐ranging, often hybrid disciplinary expertise, including computer science, mathematics, epidemiology, medicine, and demography, from the Harvard School of Public Health in the United States, the Karolinska Institute in Sweden, the National University of Defense Technology in China, and the University of Southampton in the United Kingdom, who worked together on the malaria mobility model and/or its applications to Ebola.
Expatriate humanitarian interventions in the three countries most effected during the Ebola outbreak proceeded predominantly, though not exclusively, in keeping with historical and/or former colonial relationships: the United Kingdom focused on Sierra Leone, the United States on Liberia, and France on Guinea. My expertise is in Sierra Leone where I have worked over several decades.
Inclusion of “eyewitness reports”—which is the closest corollary to qualitative data in the HealthMap source repertoire—is extremely rare; the algorithm simply does not have the capability to process qualitative data and narrative analysis.
There are alternatives to GPS, which is a U.S.‐government‐controlled system initiated by the U.S. military and made available to civilian users. For the explanatory purposes of this article, I use the GPS satellite system as the default satellite system reference. Russia has its own system, GLONASS, and there are systems for smaller regional coverage like that of Japan's QZSS and China's Beidou. The European Union is currently developing a system called Galileo, and China is developing a global system called Compass (Bhatta 2011).
“Mobile phone penetration” is considered the number of active SIM (Subscriber Identity Module) users per 100 people. The rate is misleading because it does not account for users having more than one phone, which can bring the percentage to over 100%. A great irony for the Sierra Leone case, when we account for the number of cell phones and SIM cards people claim as their own, is that any count disproportionally overcounts owners of one or more cell phones while missing other large groups of people without cell phones, for example, in the rural areas where Ebola emerged.
The BuddeComm estimate is an example of a statistic that is kept in circulation with no real means of verification. BuddeComm derives its figures from various sources, including self‐reported statistics from most of the Sierra Leonean telecommunication companies (Sierratel, Celtel, Comium, Africell, Tigo, and others). Their data collection methodologies are not transparent (see BuddeComm 2017) and there is no means of verification by the public.
In public health parlance, prevalence and incidence are two widely used global public health metrics that aim to enumerate the concentration of a disease within human populations. Prevalence is the proportion of a population that has a disease over a given period, usually a year. Incidence refers to the number of new cases of a disease occurring during a given period.
Capture–ReCapture (CRC) is actually a public health data sampling methodology intended to estimate disease incidence rates in so‐called elusive populations. It was adapted from animal studies that captured, marked, released, and then recaptured animals. See “Use of Capture–Recapture to Estimate Underreporting of Ebola Virus Disease, Montserrado County, Liberia” (Gignoux et al. 2015).
For four months during the height of the epidemic, computational epidemiologists along with some employees of UNICEF and UN Global Pulse (a UN initiative supporting big data prediction‐making) tried to get CDR data. They tried to involve the [Sierra Leonean] National Ebola Response Committee (NERC), UNMEER (UN Mission for Ebola Emergency Response) and other branches of the Sierra Leonean Government to put pressure on telecommunications companies to release their CDR data (Fast and Waugaman 2016, 34–35).
References Cited
- Abramowitz, S. 2014. Ten Things that Anthropologists Can Do to Fight the West African Ebola Epidemic. Somatosphere September 26. http://somatosphere.net/2014/09/ten-things-that-anthropologists-can-do-to-fight-the-west-african-ebola-epidemic.html (accessed January 24, 2017). [Google Scholar]
- Adams, V. , Murphy M., and Clarke A.. 2009. Anticipation: Technoscience, Life, Affect, Temporality. Subjectivity 28: 246–65. [Google Scholar]
- Alderman, L. 2017. The Phones We Love Too Much. New York Times, May 2. https://www.nytimes.com/2017/05/02/well/mind/the-phones-we-love-too-much.html (accessed July 20, 2017). [Google Scholar]
- American Anthropological Association (AAA) . 2014. Strengthening West African Health Care Systems to Stop Ebola: Anthropologists Offer Insights. http://s3.amazonaws.com/rdcms.aaa/files/production/public/FileDownloads/pdfs/about/Governance/upload/AAA-Ebola-Report.pdf (accessed May 28, 2017).
- Anderson, C. 2008. The End of Theory: The Data Deluge Makes the Scientific Method Obsolete. Wired Magazine, June 23. https://www.wired.com/2008/06/pb-theory/ (accessed May 28, 2017). [Google Scholar]
- Anema, A. , Kluberg S., Wilson K., Hogg R. S., Khan K., Hay S. I., Tatem A. J., and Brownstein J. S.. 2014. Digital Surveillance for Enhanced Detection and Response to Outbreaks. The Lancet Infectious Diseases 14: 1035–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Press Associated. 2014. Online Tool Nailed Ebola Epidemic. Politico, August 9. http://www.politico.com/story/2014/08/healthmap-ebola-outbreak-109881 (accessed October 27, 2014). [Google Scholar]
- Baize, S. , Pannetier D., Oestereich L., Rieger T., Koivogui L., Magassouba N., Soropogui B., Sow M.S., Keïta S., De Clerck H., Tiffany A., Dominguez G., Loua M., Traoré A., Kolié M., Malano E. R., Heleze E., Bocquin A., Mély S., Raoul H., Caro V., Cadar D., Gabriel M., Pahlmann M., Tappe D., Schmidt‐Chanasit J., Impouma B., Diallo A. K., Formenty P., Van Herp M., and Günther S.. 2014. Emergence of Zaire Ebola Virus Disease in Guinea. The New England Journal of Medicine 371: 1418–25. [DOI] [PubMed] [Google Scholar]
- Bennett, J. 2004. The Force of Things: Steps toward an Ecology of Matter. Political Theory 32: 347–72. [Google Scholar]
- Benton, A. 2014. The Epidemic Will Be Militarized: Watching Outbreak as the West African Ebola Epidemic Unfolds. Hot Spots. https://culanth.org/fieldsights/599-the-epidemic-will-be-militarized-watching-outbreak-as-the-west-african-ebola-epidemic-unfolds (accessed October 27, 2014).
- Benton, A. 2017. Whose Security? Militarization and Securitization during West Africa's Ebola Outbreak In The Politics of Fear: Médicin sans Frontiéres and the West African Ebola Epidemic, edited by Hofman M. and Au S., 25–50. Oxford: Oxford University Press. [Google Scholar]
- Bhatta, B. 2011. Global Navigation Satellite Systems: Insights into GPS, GLONASS, Galileo, Compass and Others. Boca Raton, FL: CRC Press. [Google Scholar]
- Buckee, C. 2012. International Digital Disease Detection Conference, Harvard Medical School, February 16–17, 2012, video of conference proceedings DDD2012: Caroline Buckee: Mobile Devices and Disease Detection Panel (accessed July 2, 2017).
- BuddeComm . 2017. Sierra Leone: Telecoms, Mobile and Broadband—Market Insights and Statistics. BuddeComm, January 20. https://www.budde.com.au/Research/Sierra-Leone-Telecoms-Mobile-and-Broadband-Statistics-and-Analyses (accessed April 2, 2017). [Google Scholar]
- Chandler, C. , and Beisel U.. 2017. The Anthropology of Malaria: Locating the Social. Medical Anthropology 36: 411–21. [DOI] [PubMed] [Google Scholar]
- Cinnamon, J. , Jones S. K., and Adger W. N.. 2016. Evidence and Future Potential of Mobile Phone Data for Disease Disaster Management. Geoforum 75: 253–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conneally, P. 2011. How Mobile Phones Power Disaster Relief. TED Talk/ TEDxRC2, November. https://www.ted.com/talks/paul_conneally_digital_humanitarianism (accessed January 28, 2018).
- Cukier, K. , and Mayer‐Schoenberger V.. 2013. The Rise of Big Data: How It's Changing the Way We Think about the World. Foreign Affairs 92: 27–40. [Google Scholar]
- Deloitte . 2016. Global Mobile Consumer Survey: US Edition. https://www2.deloitte.com/us/en/pages/technology-media-and-telecommunications/articles/global-mobile-consumer-survey-us-edition.html (accessed July 13, 2017).
- Derman, E. 2004. My Life as a Quant: Reflections on Physics and Finance. Hoboken, NJ: Wiley. [Google Scholar]
- Economist, The . 2014. Ebola and Big Data: Waiting on Hold. October 27. https://www.economist.com/news/science-and-technology/21627557-mobile-phone-records-would-help-combat-ebola-epidemic-getting-look (accessed January 20, 2018).
- Fast, L. , and Waugaman A.. 2016. Fighting Ebola with Information: Learning from Data and Information Flows in the West Africa Ebola Response. USAID Report, Washington, DC. https://www.usaid.gov/sites/default/files/documents/15396/FightingEbolaWithInformation.pdf (accessed July 10, 2017).
- Gignoux, E. , Idowu R., Bawo L., Hurum L., Sprecher A., Bastard M., and Porten K.. 2015. Use of Capture–Recapture to Estimate Underreporting of Ebola Virus Disease, Montserrado County Liberia. Emerging Infectious Diseases 21: 2265–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallowell, A. I. 1955. Culture and Experience. New York: Schocken Books. [Google Scholar]
- HealthMap . 2014a. http://www.healthmap.org/ (accessed October 27, 2014).
- HealthMap . 2014b. http://www.healthmap.org/site/about (accessed October 27, 2014).
- Kamat, V. R. 2013. Silent Violence: Global Health, Malaria, and Child Survival in Tanzania. Tucson: University of Arizona Press. [Google Scholar]
- Kelly, A. H. , and Beisel U.. 2011. Neglected Malarias: The Frontlines and Back Alleys of Global Health. Biosocieties 6: 71–87. [Google Scholar]
- Kirkpatrick, R. 2011. Data Philanthropy Is Good for Business. Forbes. September 20. https://www.forbes.com/sites/oreillymedia/2011/09/20/data-philanthropy-is-good-for-business/#36a3c4675f70 (accessed January 18, 2018). [Google Scholar]
- Leetaru, K. 2014. Why Big Data Missed the Early Warning Signs of Ebola. Foreign Policy, September 26. http://foreignpolicy.com/2014/09/26/why-big-data-missed-the-early-warning-signs-of-ebola/ (accessed July 2, 2017). [Google Scholar]
- Letouzé, E. , and Vinck P.. 2015. The Law, Politics and Ethics of Cell Phone Data Analytics. Data‐Pop Alliance White Paper Series. World Bank Group, Harvard Humanitarian Initiative, MIT Media Lab and Overseas Development Institute. April. http://datapopalliance.org/wp-content/uploads/2015/04/WPS_LawPoliticsEthicsCellPhoneDataAnalytics.pdf (accessed July 10, 2017).
- Lipton, J. 2015. Obligations, Obstacles, and Opportunities: Performing Burials in a Time of Crisis in Freetown, Sierra Leone. Unpublished paper presented at Beyond Ebola: Knowledge Production and the Limitations of Translation workshop, October 28–30, 2015, Max Planck Institute for Social Anthropology, Halle, Germany.
- MapAction . 2014. Sierra Leone: Ebola Outbreak—GSM Mobile Phone Network Coverage in Kailahun district, Eastern Province. https://www.humanitarianresponse.info/system/files/documents/files/MA040_PopUnserved_Telecoms_v1-300dpi.pdf (accessed November 28, 2014).
- Martineau, F. , Wilkinson A., and Parker M.. 2017. Epistemologies of Ebola: Reflections on the Experience of the Ebola Response Anthropology Platform. Anthropology Quarterly 90: 475–94. [Google Scholar]
- Mayer‐Schönberger, V. , and Cukier K.. 2013. Big Data: A Revolution that Will Transform How We Live, Work and Think. London: John Murray Publishers. [Google Scholar]
- McDonald, S. M. 2016. Ebola: A Big Data Disaster Privacy, Property, and the Law of Disaster Experimentation. CIS Papers 2016.01. The Centre for Internet and Society, http://cis-india.org/papers/ebola-a-big-data-disaster (accessed July 13, 2017).
- Meier, P. 2015. Digital Humanitarians: How Big Data Is Changing the Face of Humanitarian Response. Boca Raton, FL: CRC Press. [Google Scholar]
- Moran, M. H. 2017. Missing Bodies and Secret Funerals: The Production of “Safe and Dignified Burials” in the Liberian Ebola Crisis. Anthropology Quarterly 90: 399–422. [Google Scholar]
- Moran, M. H. , and Hoffman D.. 2014. Introduction: Ebola in Perspective. Cultural Anthropology, October 7. https://culanth.org/fieldsights/586-introduction-ebola-in-perspective (accessed May 28, 2017). [Google Scholar]
- Ngowi, R. 2014. US Bots Flagged Ebola Outbreak in West Africa Days before Formal Announcement of Epidemic.” US News, August 9. https://www.usnews.com/news/technology/articles/2014/08/09/us-bots-flagged-ebola-before-outbreak-announced (May 28, 2017). [Google Scholar]
- Packard, R. M. , and Brown P. J.. 1997. Rethinking Health, Development, and Malaria: Historicizing a Cultural Model in International Health. Medical Anthropology 17: 181–94. [DOI] [PubMed] [Google Scholar]
- Piot, C. 2010. Nostalgia for the Future: West Africa after the Cold War. Chicago: University of Chicago Press. [Google Scholar]
- PLoS Medicine Editors . 2012. Digital Humanitarianism: Collective Intelligence Emerging. PLoS Medicine 9: e1001278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watch Public Health. 2014. How A Computer Algorithm Predicted West Africa's Ebola Outbreak before It Was Announced. http://publichealthwatch.wordpress.com/2014/08/10/how-a-computer-algorithm-predicted-west-africas-ebola-outbreak-before-it-was-announced/ (accessed October 27, 2014).
- Public Radio International . 2014. How “Big Data” Could Help Stop the Spread of Ebola. Public Radio International, October 24. https://www.pri.org/stories/2014-10-24/how-big-data-could-help-stop-spread-ebola (accessed May 28, 2017). [Google Scholar]
- Qadir, J. , Ali A., ur Rasool R., Zwitter A., Sathiaseelan A., and Crowcroft J.. 2016. Crisis Analytics: Big Data‐driven Crisis Response. Journal of International Humanitarian Action 1: 1–21. [Google Scholar]
- Richards, P. , Mara J., Ferme M. C., Kamara P., Mokuwa E., Sheriff A. I., Suluku R., and Voors M. 2015. Social Pathways for Ebola Virus Disease in Rural Sierra Leone, and Some Implications for Containment. PLoS Neglected Tropical Diseases 9: e0003567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosaldo, M. 1980. Knowledge and Passion: Ilongot Notions of Self and Social Life. Cambridge: Cambridge University Press. [Google Scholar]
- Rubin, E. 1997. An Army of One's Own. Harper's Magazine Feb., 44–55. [Google Scholar]
- Salathé, M. , Bengtsson L., Bodnar T. J., Brewer D. D., Brownstein J. S., Buckee C., Campbell E. M., Cattuto C., Khandelwal S., Mabry P. L., and Vespignani A.. 2012. Digital Epidemiology. PLoS Computational Biology 8: e1002616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandvik, K. B. 2014. Fighting the War with the Ebola Drone. Norwegian Centre for Humanitarian Studies Blog, December 3. http://www.humanitarianstudies.no/2014/12/03/fighting-the-war-with-the-ebola-drone/ (accessed May 28, 2017). [Google Scholar]
- Schlanger, Z. 2014. An Algorithm Spotted the Ebola Outbreak Nine Days before WHO Announced It. Newsweek, August 11. http://www.newsweek.com/algorithm-spotted-ebola-outbreak-9-days-who-announced-it-263875 (accessed May 28, 2017). [Google Scholar]
- Silberfein, M. , and Conteh Al‐H.. 2006. Boundaries and Conflict in the Mano River Region of West Africa. Conflict Management and Peace Science 23: 343–361. [Google Scholar]
- Spencer, S. 2015. “Invisible Enemy”: Translating Ebola Prevention and Control Measures in Sierra Leone. Working Papers Series No. 13, Priority Programme 1448 of the German Research Foundation. Edited by U. Engel and R. Rottenburg.
- Stathern, M. 1988. The Gender of the Gift. Berkeley: University of California Press. [Google Scholar]
- Stoller, P. 1999. Jaguar: A Story of Africans in America. Chicago: The University of Chicago Press. [Google Scholar]
- Talbot, D. 2013. Big Data from Cheap Phones. MIT Technology Review. https://www.technologyreview.com/s/513721/big-data-from-cheap-phones/ (accessed May 28, 2017). [Google Scholar]
- Taussig, K.‐S. , Hoeyer K., and Helmreich S.. 2013. The Anthropology of Potentiality in Biomedicine: An Introduction. Current Anthropology 54: S3–S14. [Google Scholar]
- Titlow, J. P. 2014. How This Algorithm Detected the Ebola Outbreak before Humans Could. Fast Company. August 13. https://www.fastcompany.com/3034346/how-this-algorithm-detected-the-ebola-outbreak-before-humans-could (accessed May 28, 2017). [Google Scholar]
- Watson, H. , Finn R. L., and Wadhwa K.. 2016. Organizational and Societal Impacts of Big Data in Crisis Management. Journal of Contingencies and Crisis Management 25: 15–22. [Google Scholar]
- Webster, P. 2014. Reality Mining: Big Data and the Future of Risk Factor Surveillance. CARRFS eNews, January 19. http://www.carrfsenews.ca/feature/2014/1/19/reality-mining-big-data-and-the-future-of-risk-factor-surveillance (accessed May 28, 2017). [Google Scholar]
- Wesolowski, A. , Bengtsson L., Buckee C. O., Lu X., Wetter E., and Tatem A. J.. 2014a. Flowminder Foundation West Africa Human Mobility Models: Version 1.0. http://www.worldpop.org.uk/ebola/Flowminder-Mobility-Data-21.08.14.pdf (accessed September 10, 2014).
- Wesolowski A., Buckee C. O., Bengtsson L., Wetter E., Lu X., and Tatem A. J.. 2014b. Commentary: Containing the Ebola Outbreak—the Potential and Challenge of Mobile Network Data. PLOS Currents Outbreaks. Edition 1. http://currents.plos.org/outbreaks/article/containing-the-ebola-outbreak-the-potential-and-challenge-of-mobile-network-data/#ref5 (July 13, 2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesolowski, A. , Eagle N., Noor A. M., Snow R. W., and Buckee C. O.. 2013. The Impact of Biases in Mobile Phone Ownership on Estimates of Human Mobility. Journal of the Royal Society Interface 10: 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesolowski, A. , Eagle N., Tatem A. J., Smith D. L., Noor A. M., Snow R. W., and Buckee C.. 2012. Quantifying the Impact of Human Mobility on Malaria. Science 338: 267–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wikipedia . 2018. John Brownstein. https://en.wikipedia.org/wiki/John_Brownstein (accessed February 17, 2018).
- Wilkinson, A. , and Leach M.. 2014. Briefing: Ebola—Myths, Realities, and Structural Violence. African Affairs 114: 136–248. [Google Scholar]
- World Health Organization (WHO) . 2014a. Ebola Situation in Liberia: Non‐conventional Interventions Needed. http://www.who.int/mediacentre/news/ebola/8-september-2014/en/ (accessed January 18, 2018).
- World Health Organization (WHO) . 2014b. Government of Senegal Boosts Ebola Awareness through SMS Campaign. http://www.who.int/features/2014/senegal-ebola-sms/en/ (accessed July 2, 2017).
- World Health Organization (WHO) . 2016a. Ebola Data and Statistics. http://apps.who.int/gho/data/view.ebola-sitrep.ebola-summary-latest?lang=en (accessed May 28, 2017).
- World Health Organization (WHO) . 2016b. Ebola Situation Report: 30 March 2016. http://apps.who.int/ebola/current-situation/ebola-situation-report-30-march-2016 (accessed July 2, 2017).


