Abstract
We aimed to assess the cervical cancer burden and performance of screening programme over the last decade in Apulia, Italy. Data from Hospital Discharge, Causes of Death and of Outpatient Services registries were analysed to estimate the disease burden, and data collected by the screening information system were used to evaluate the performance of the programme. We computed annual hospitalisation, incidence and mortality rates and number of outpatient services prescriptions for the follow‐up of preneoplastic/neoplastic lesions. Indicators as proposed by the National Centre for Screening Monitoring were computed to describe the screening performance. Hospitalisation rates declined from 47 in 2001 to 28 per 100,000 in 2014, incidence from 10.3 in 2004 to 6.0 per 100,000 in 2014 and mortality from 1.4 in 2001 to 1.0 per 100,000 in 2010. Prescriptions increased from 3,333 in 2006 to 4,968 in 2010, then decreased to 3,634/year in 2012–2014. Actual extension of screening increased from 10.8% in 2007 to 62% in 2014; compliance with the invitation was 32%/year. In the last decade, we observed a reduction in the cervical cancer burden as early effect of screening implementation.
Keywords: cervical cancer, cervical cancer screening, HPV test, HPV vaccination, Italy
1. INTRODUCTION
Cervical cancer (CC) is the first malignant neoplasm recognised by the World Health Organization (WHO) as totally due to a viral infection. Human papillomaviruses (HPVs) are responsible for about 99% of CC cases with two high‐risk HPV types (16 and 18) causing about 70% of all these tumours (Bosch & de Sanjose, 2003).
Worldwide, CC is the fourth most common cancer among women and the second leading cause of death in women aged 15–44 years, with an estimated 527,624 new cases and 265,653 deaths in 2012 (Bruni et al., March 24, 2015). In Europe, estimations for 2012 indicated that every year 58,373 new CC cases are diagnosed and 24,385 deaths occur. Approximately 58% of cases and 63% of deaths were reported in Eastern Europe, with the highest incidence in Romania (age‐standardised rate of 28.6 per 100,000 women per year) and Lithuania (26.1 per 100,000) and the lowest in Malta (3.8 per 100,000) and Switzerland (3.6 per 100,000) (Bruni et al., April 8, 2015). In Italy, about 2,918 new CC cases are diagnosed and about 1,016 deaths occur annually (Bruni et al., March 20, 2015). The standardised incidence rate decreased from 13.7 per 100,000 women in 1980 to 6.2 per 100,000 in 2002 and to 4.2 per 100,000 in 2012; the standardised mortality rate declined from 7 per 100,000 women in 1980 to 1.6 per 100,000 in 2012 (Bruni et al., March 20, 2015; De Angelis et al., 2010; ISS, 2013).
Organised screening programmes are generally considered the milestone in CC prevention: The long latent period between detectable preneoplastic lesions and the development of an invasive cancer (about 15–20 years) allows early diagnosis and treatment (Italian Ministry of Health, January 13, 2013; WHO, 2016). In Italy, the implementation of organised cervical screening programmes within each region has been recommended since 1996 (Ronco et al., 2015) and included in the Ministry of Health's list of “Essential Health Interventions” since 2001 (Grazzini & Zappa, 2008). Recommendations, largely based on European guidelines, include personal invitations to women aged 25–64 years for a Pap test every 3 years, a monitoring system and quality assurance for each phase of the programme. In 2012, the target population of these programmes amounted to 14,497,207 women, corresponding to 87.3% of Italian women aged 25–64 years; compliance with invitation was 40.8%, with a strong decreasing north–south trend; of all screened women, 2.4% were referred to colposcopy; the unadjusted detection rate of CIN2 or more severe histology was 3.4 per 1,000 screened women (Ronco et al., 2015).
In 2013, the Italian Ministry of Health included HPV test every 5 years as an option for screening programmes for women ≥30 years. The National Prevention Plan 2014–2018 put as an objective the full implementation of HPV‐based screening by 2018. In October 2015, also the EU guidelines have been updated including HPV testing (Italian Ministry of Health, 2015; von Karsa et al., 2015).
Since 2006, two safe and effective vaccines against HPV were licensed to prevent CC caused by vaccine genotypes (WHO, 2014). In Italy, a national HPV vaccination programme has been implemented since 2008 for females aged 12 years (starting from birth cohorts 1996 and 1997). Some regions also extended free catch‐up vaccination of one or more older cohorts (girls aged 16 years, 18 years or women aged 25 years), and almost all regions offered the vaccine at a reduced price to women younger than 26 years (ISS, 2015; Italian Ministry of Health, 2007). The nationwide coverage for the 2001 birth cohort as of 31 December 2014 was 67.1% for the full three‐dose schedule, with wide variability between regions (range, 30.2%–80.4%) (ISS, 2016, 2016).
In most of the Southern regions, including Apulia, CC prevention has long been based on spontaneous screening. In July 2007, an organised screening programme was started in the province of Bari and progressively extended to the rest of Apulia region between 2008 and 2010 (Assessorato alle Politiche della salute, Apulia Region, Italy, 2011). Universal HPV vaccination is delivered free of charge to girls aged 12 years and to a second cohort of females (aged 18 years from 2010 to 2013 and aged 25 years from 2014), with direct invitation by letter. Since 2014, vaccination is also offered free of charge to boys aged 12 (Commissione tecnico‐scientifica regionale vaccini, Apulia Region, Italy, 2014). As of December 31, 2014, the region‐wide coverage with three doses was 75% among girls born in 2001 and 55% among women born in 1995 (ISS, 2016, 2016).
As pointed out in the European quality assurance guidelines (von Karsa et al., 2015), the most effective and appropriate way for reducing cervical cancer incidence and mortality is through implementation of population‐based screening programmes. The implementation of HPV vaccination programmes will also reduce the burden of cervical cancer in the coming decades.
This study aimed to assess the cervical cancer burden and performance of screening programme over the last decade in Apulia, Italy, using routine data and predefined indicators.
2. MATERIAL AND METHODS
2.1. Burden of cervical cancer
In Apulia, three data sources are routinely available for estimating the burden of cervical cancer:
Hospital Discharge Registry (HDR), that collects data on discharge diagnoses (one main and up to five secondary diagnoses) and procedures of all patients admitted to hospitals in the region. Discharge diagnosis and procedures are coded using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD9‐CM). From this source, we extracted records of women with discharge diagnosis of CC (ICD9‐CM code: 180.x “Malignant neoplasm of cervix uteri”) as either main or secondary diagnosis for the period 2001–2014.
Causes of Death Registry, that stores death certificates coded in accordance with the International Classification of Diseases, Ninth (ICD9) and Tenth Revision (ICD10). From this source, we selected records of women with ICD9 code 180.x as main cause of death for the period 2001–2010. Moreover, as a high proportion of deaths for CC was misclassified and incorrectly attributed to “not otherwise specified uterine cancer” (Capocaccia et al., 2009; Mancuso, Sacchettini, Vicentini, Caroli, & Giorgi Rossi, 2016), we included records coded 179.x “Malignant neoplasm of uterus, part unspecified.”
Database of Outpatient Services, that collects prescriptions for specialist outpatient services coded according to the Italian tariff (Italian Ministry of Health, 2012). For the period from 2006 to 2014, we extracted prescriptions for management and follow‐up of cervical preneoplastic and neoplastic lesions: endocervical or portio biopsy (codes: 67.12 and 67.19.1), cauterisation and cryosurgery of the cervix (codes: 67.32 and 67.33), histopathological examination of cervical single biopsy (codes: 91.44.3 and 91.44.4) or multiple cervical biopsies (code: 91.46.3).
Crude and age‐specific annual hospitalisation rates were calculated by dividing the number of discharges by the number of residents in Apulia (data from Italy's National Census Bureau estimate, years 2001–2014). In order to estimate incident CC cases, we performed hospitalisation data cleansing using pseudonymised personal ID number to identify readmissions; prevalent cases in the first years of the studied period were excluded from the analysis and crude and age‐specific annual incidence rates for 2004–2014 were calculated. Crude, age‐specific and standardised annual mortality rates for CC from 2001 to 2010 were also calculated. The annual number of outpatient services prescriptions for preneoplastic and neoplastic lesions management and follow‐up was described for 2006–2014.
2.2. Performance of cervical cancer screening
Using records collected by the regional screening information system, the performance of organised cervical screening programme during 2007–2014 was described by computing process indicators as proposed by the National Centre for Screening Monitoring (Ronco et al., 2015):
Nominal extension: percentage of women involved in a screening programme out of the total female population in the 25–64 age range resident in the area covered by an organised screening programme.
Actual extension: percentage of women involved in a screening programme out of the total female population in the 25–64 age range who actually received an invitation to screening during the analysed period.
Compliance with invitation: percentage of women attending screening out of invited women.
Referral rate: percentage of women referred to colposcopy (for any reason) out of the total number of screened women.
Compliance with colposcopy for ASCUS+: percentage of women who underwent colposcopy out of women referred to colposcopy because of ASCUS or more severe cytology.
Recommendation to repeat cytology: percentage of women recommended to repeat cytology out of the total number of screened women.
Compliance with recommendation to repeat cytology: percentage of women who actually repeated cytology among those who were recommended to do so.
Detection rate (DR) CIN2+ unadjusted: number of women who had a CIN2+ detected out of 1,000 screened women.
For each year, women invited during that year and screened within the first 4 months of the subsequent year were considered (Ronco et al., 2015).
2.3. Early impact of cervical cancer screening
To assess the early impact of cervical cancer screening implementation in Apulia, the burden of CC before and after the introduction of screening was estimated. Crude and age‐specific hospitalisation rates in the “prescreening period,” calculated as the average annual rates between 2001 and 2006, were compared to the average annual rates between 2007 and 2010 (the “screening start‐up period”) and to the average annual rates within 2011–2014 (the “screening period”). Crude and age‐specific average annual incidence rates within 2004–2006 (prescreening period) were compared to the average annual incidence within 2007–2010 (start‐up period) and to the average annual incidence within 2011–2014 (screening period). Crude and age‐specific average annual mortality rates within 2001–2006 (prescreening period) were compared to the average annual rates within 2007–2010 (start‐up period) (mortality data for the screening period were provisional). Rates in the pre‐ and in the screening period and the hospitalisation (HRRs), incidence (IRRs) and mortality (MRRs) risk ratios with 95% CIs were computed using outcome‐specific Poisson regression models. Analyses were performed using Stata MP 12 for Mac OS.
2.4. Ethics
The study protocol was approved by the Institutional Review Board at the Apulian Regional Observatory for Epidemiology. The study was conducted according to the principles expressed in the Declaration of Helsinki. Informed consent was not obtained from participants because data from different sources were provided and analysed anonymously.
3. RESULTS
3.1. Burden of cervical cancer
In Apulia region, the annual hospitalisation rate for CC decreased from 47 per 100,000 women in 2001 (N = 972) to 28 per 100,000 in 2014 (N = 587 ‐ Figure 1a). The average number of admissions per patient was 5 ± 5.6, with a mean length of hospital stay of 11 ± 28 days. Hospital admission for CC was more common among 45–64 years old (46% of all hospitalisations in the studied period), with a median age at discharge of 56 years ±14.4 years.
Figure 1.
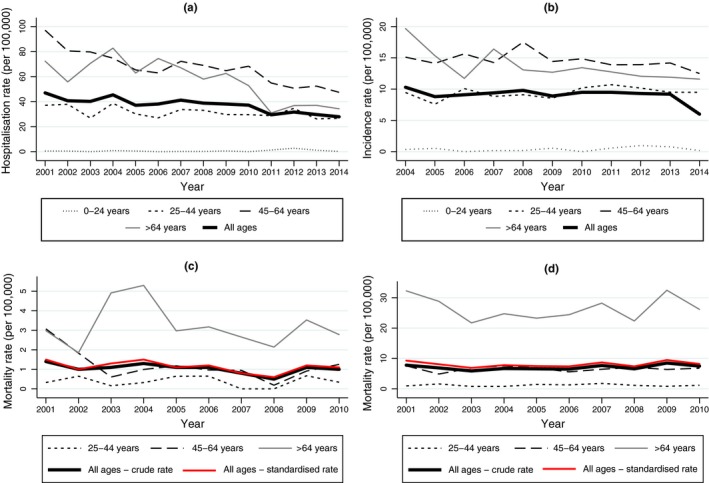
Hospitalisation rates (a), estimated incidence (b), crude and standardised mortality rates for cervical cancer (c) and for other malignant neoplasms of uterus by age group (d). Apulia, Italy, 2001–2014
After cleansing data and removing readmissions process, a total of 2,095 women discharged with a primary diagnosis of probable CC were identified between 2004 and 2014 (191 new cases/year, estimated annual rate = 9.1 per 100,000). The incidence rate declined from 10.3 per 100,000 in 2004 to 9.2 per 100,000 in 2013 and to 6.0 per 100,000 in 2014 (Figure 1b).
From 2001 to 2010, 1,695 women died for CC or other malignant neoplasms of uterus (170 deaths/year, overall annual mortality rate = 8.1 per 100,000). In particular, the crude and standardised mortality rates of CC decreased from 1.4 and 1.5 per 100,000 in 2001 to 1.0 and 1.1 per 100,000 in 2010 respectively (Figures 1c and d). More than 70% of deaths occurred among women ≥65 years old (average age at death = 70.9 ± 14.0).
The annual number of outpatient services prescriptions for the follow‐up of preneoplastic and neoplastic lesions considerably increased from 3,333 in 2006 to 4,968 in 2010, then decreased to 3,634/year in 2012–2014. The largest number of prescriptions was registered for histopathological examination of cervical single biopsy (N = 1,879/year), followed by endocervical or portio biopsy (N = 1,357/year), histopathological examination of cervical and/or multiple cervical biopsies (N = 347/year), cauterisation and cryosurgery of the cervix (N = 281/year) (Figure 2).
Figure 2.
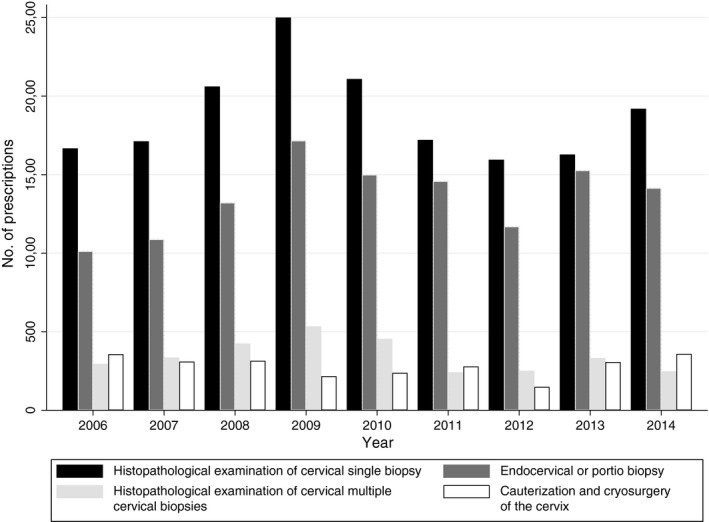
Annual number of outpatient services prescriptions for preneoplastic and neoplastic lesions follow‐up. Apulia, Italy, 2006–2014
3.2. Performance of cervical cancer screening
During the period 2007–2014, the organised screening programme in Apulia had a mean target population of 1,136,988 women aged 25–64 years. Nominal extension reached 100% since 2011. Actual extension progressively increased from 10.8% in 2007 to 62% in 2014, while compliance with invitation remained substantially stable at 32%/year (the highest rate 36.2% was recorded in 2008, the lowest 25% in 2010). The average referral rate to colposcopy was 1.7%/year and the average compliance with colposcopy for ASCUS+ was 62%/year, progressively higher in the study period. Detection rate of CIN2 or more severe histology was 0.95 per 1,000 women screened in 2014 (Table 1).
Table 1.
Value of process indicators of organised cervical screening programme. Apulia, Italy, 2007–2014
| Year of activity | ||||||||
|---|---|---|---|---|---|---|---|---|
| 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
| Population 25–64 years | 1,137,312 | 1,140,676 | 1,144,542 | 1,146,671 | 1,131,054 | 1,128,192 | 1,135,168 | 1,132,288 |
| Nominal extension (%) | 46.5 | 93.2 | 93.1 | 95.6 | 100.0 | 100.0 | 100.0 | 100.0 |
| Actual extension (%) | 10.8 | 27.8 | 53.8 | 52.3 | 41.9 | 54.9 | 46.4 | 62.0 |
| Compliance with invitation (%) | 35.7 | 36.2 | 29.3 | 25.0 | 31.0 | 29.9 | 33.5 | 32.0 |
| Referral rate (%) | 1.9 | 1.2 | 1.3 | 1.7 | 2.4 | 2.0 | 1.7 | 1.5 |
| Compliance with colposcopy for ASCUS+ (%) | N/A | 60.1 | 40.7 | 57.2 | 74.9 | 56.6 | 73.7 | 73.8 |
| Detection rate (per 1,000) | 0.14 | 0.52 | 0.76 | 1.32 | 0.4 | 0.6 | 1.2 | 0.95 |
3.3. Early impact of cervical cancer screening
Comparing the pre‐ and the screening period, hospitalisation rate decreased from 41.4 per 100,000 (N = 863/year) in 2001–2006 to 38.8 per 100,000 (N = 816/year; HRR = 0.94, 95% CI = 0.85–1.03) in 2007–2010 and significantly declined to 29.7 per 100,000 (N = 596/year; HRR = 0.72, 95% CI = 0.64–0.79) in 2011–2014. In the screening period, hospitalisation rates significantly declined in the age group 45–64 years (HRR = 0.67, 95% CI = 0.58–0.78) and ≥65 years (HRR = 0.49, 95% CI = 0.41–0.61 – Table 2a). A decrease in incidence was observed in the screening period, although not statistically significant (IRR = 0.91, 95% CI = 0.74–1.11 – Table 2b). Mortality of CC decreased during the start‐up period without statistical significance (MRR = 0.74, 95% CI = 0.40–1.36 – Tables 2c–d).
Table 2.
Hospitalisation rates and HRRs with 95% CIs (a), incidence rates and IRRs with 95% CIs (b), mortality rates and MRRs with 95% CIs for cervical cancer (c) and for other malignant neoplasms of uterus (d) in the “prescreening,” the “screening start‐up” and the “screening period.” Apulia, Italy, 2001–2014
| (a) | Prescreening period | Screening start‐up period | Screening period | |||||
|---|---|---|---|---|---|---|---|---|
| 2001–2006 | 2007–2010 | 2011–2014 | ||||||
| No. | Rate per 100,000 | No. | Rate per 100,000 | HRR (95% CI) | No. | Rate per 100,000 | HRR (95% CI) | |
| 0–24 years | 2 | 0.4 | 1 | 0.2 | 0.57 (0.06–5.02) | 7 | 1.4 | 3.37 (0.77–14.84) |
| 25–44 years | 204 | 33.0 | 189 | 31.5 | 0.96 (0.78–1.17) | 163 | 29.1 | 0.88 (0.72–1.08) |
| 45–64 years | 384 | 76.5 | 372 | 68.5 | 0.89 (0.78–1.03) | 294 | 51.3 | 0.67 (0.58–0.78) |
| ≥65 years | 273 | 69.9 | 254 | 60.0 | 0.86 (0.72–1.02) | 159 | 34.8 | 0.49 (0.41–0.61) |
| All ages | 863 | 41.4 | 816 | 38.8 | 0.94 (0.85–1.03) | 596 | 29.7 | 0.72 (0.64–0.79) |
| (b) | Prescreening period | Screening start‐up period | Screening period | |||||
|---|---|---|---|---|---|---|---|---|
| 2004–2006 | 2007–2010 | 2011–2014 | ||||||
| No. | Rate per 100,000 | No. | Rate per 100,000 | IRR (95% CI) | No. | Rate per 100,000 | IRR (95% CI) | |
| 0–24 years | 1.7 | 0.3 | 1.3 | 0.2 | 0.78 (0.08–7.97) | 3.3 | 0.6 | 2.14 (0.33–13.88) |
| 25–44 years | 56.0 | 9.0 | 55.0 | 9.2 | 1.01 (0.70–1.47) | 55.8 | 10.0 | 1.10 (0.76–1.60) |
| 45–64 years | 76.3 | 15.0 | 82.8 | 15.3 | 1.02 (0.75–1.39) | 78.0 | 13.6 | 0.91 (0.66–1.25) |
| ≥65 years | 62.7 | 15.5 | 58.8 | 13.9 | 0.89 (0.63–1.27) | 55.0 | 12.1 | 0.77 (0.54–1.12) |
| All ages | 196.7 | 9.4 | 197.8 | 9.4 | 1.00 (0.82–1.22) | 178.5 | 8.5 | 0.91 (0.74–1.11) |
| (c) | Prescreening period | Screening start‐up period | ||||||
|---|---|---|---|---|---|---|---|---|
| 2001–2006 | 2007–2010 | |||||||
| No. | Rate per 100,000 | No. | Rate per 100,000 | MRR (95% CI) | ||||
| 0–24 years | 0 | – | 0 | – | – | |||
| 25–44 years | 2.8 | 0.5 | 1.5 | 0.3 | 0.54 (0.07–3.95) | |||
| 45–64 years | 7.2 | 1.4 | 4.5 | 0.8 | 0.58 (0.18–1.89) | |||
| ≥65 years | 13.8 | 3.5 | 11.8 | 2.8 | 0.78 (0.36–1.71) | |||
| All ages | 23.8 | 1.1 | 17.8 | 0.8 | 0.74 (0.40–1.36) | |||
| (d) | Prescreening period | Screening start‐up period | ||||||
|---|---|---|---|---|---|---|---|---|
| 2001–2006 | 2007–2010 | |||||||
| No. | Rate per 100,000 | No. | Rate per 100,000 | MRR (95% CI) | ||||
| 0–24 years | 0 | – | 0 | – | 1.08 (0.39–3.00) | |||
| 25–44 years | 7.2 | 1.2 | 7.5 | 1.3 | 1.02 (0.64–1.63) | |||
| 45–64 years | 32.8 | 6.6 | 36.3 | 6.7 | 1.06 (0.81–1.38) | |||
| ≥65 years | 100.7 | 25.8 | 115.5 | 27.3 | 1.12 (0.89–1.41) | |||
| All ages | 140.7 | 6.8 | 159.3 | 7.6 | 1.08 (0.39–3.00) | |||
4. DISCUSSION
At the launch of the national HPV vaccination programme in 2008, the Italian Ministry of Health issued recommendations on how vaccine introduction should interact with the existing screening programmes. Data collected and analysed in this study derive from all the available information about cervical cancer trend.
Estimates from the Italian Network of Cancer Registries have shown that the age‐standardised incidence and mortality rates for cervical cancer were expected to decline markedly during the period 1980–2015, reaching the lowest figures (3.5 and 1.3 per 100,000, respectively) in 2015. The prevalence is also expected to decrease down to about 50 per 100,000 in 2015 (Rossi, Crocetti, Capocaccia, & Gatta, 2013). We obtained similar trends in Apulia, with incidence and mortality figures for CC declining over the observed periods. In Apulia, a regional population‐based cancer registry has been implemented in 2009 and only since 2012 the entire regional population has been covered by registration. By applying a statistical back‐calculation approach to derive incidence and prevalence figures starting from mortality and relative survival data, a study from Galise et al. (2013) estimated that in Apulia the cervical cancer incidence and mortality rates were expected to decrease from 14.5 and 8.1 per 100,000 in 1980 to 3.5 and 1.6 in 2015 respectively.
In recent years, in Italy, many diagnostic and therapeutic procedures have been moved from the hospital to the ambulatory setting (Rosano et al., 2013). So, a substantial decrease in hospitalisation rates for CC has been documented in Apulia in the period 2011–2014, especially among women >44 years (Figure 1a, Table 2a); accordingly, outpatient services prescriptions arose and more than 300 prescriptions for cauterisation and cryosurgery of the cervix were registered in the last years examined (Figure 2).
Organised cancer screening using evidence‐based tests has considerable potential to improve the health of the target population, provided that programmes are implemented cost‐effectively and with high quality (Veerus, Arbyn, Amati, & Paolo, 2010). A recent study on the impact of organised screening in Italy showed that, in line with other international experiences, invasive cervical cancer incidence rates have been decreasing since its full activation, especially among women aged 45–74 years (Serraino et al., 2015). A similar trend was observed also in Apulia since 2011. Compared to national data (Ronco et al., 2015), the performance of the regional screening programme is still low, although the actual extension progressively increased up to 62% in 2014 and compliance with invitation was 32%/year. These figures did not mean that only 20% of the target population underwent cervical cancer screening. Data from the PASSI survey, a national telephone surveillance system that continuously collects information about behavioural health risk factors and the diffusion of preventive healthcare services, showed that in Apulia, during the period 2011–2014, about 70% of women aged 25–64 years underwent Pap smear or HPV test in the 3 years before the interview (79% nationwide pooled data). Nearly 29% of women underwent a test within the screening programme (42% nationwide) and 41% spontaneously and paying (37% nationwide). Both these proportions have been increasing over the 4‐year period (ISS, December 1, 2016; Passi Puglia, anni 2011‐2014, 2016), showing that the organised screening improves coverage rates of cervical cancer prevention programmes. Organised screening programmes using standard validated tests have been shown to be more effective than opportunistic or nonorganised screening, also because opportunistic screening tends to miss the women at the greatest risk (Anttila et al., 2004; Hakama, Coleman, Alexe, & Auvinen, 2008); its population‐based approach ensures that screening also reaches the less fortunate who may be in greatest need of secondary prevention of cancer (Veerus et al., 2010).
Our study has some limitations. Some of the presented data are shortly accurate for monitoring the trend of the disease, for example: mortality in Italy is dramatically misclassified; outpatient data could include procedures not related at all with CIN or invasive CC; screening data probably missing many histological results, etc. Despite these limitations, our findings provide estimates of cervical cancer burden and performance indicators of screening that can contribute to anticipate the future benefits of prevention programmes. Further planned studies will validate our data by applying more complex algorithms to make indicators more reliable (i.e., incidence‐based mortality, record linkage between screening and hospital discharges).
Paradigms for cervical cancer screening are changing in high‐resource settings, including Italy, from cytology‐based screening to adoption of molecular screening (von Karsa et al., 2015; Pimple, Mishra, & Shastri, 2016). Shifting towards HPV‐based cervical screening have recently implemented in Italy, according to the Ministry of Health recommendations and guidelines for its application (stand‐alone HPV testing by validated methods, cytological triage of HPV positives, beginning at age 30–35, 5‐year intervals) (Italian Ministry of Health, 2013). A future challenge for the organisation of cervical screening is to link it to this new context of efforts to vaccinate young people against HPV infection (Williams, Carter, & Rychetnik, 2014). By linking vaccination, cervical screening and HPV testing data, we will be able to estimate the decline in high‐risk HPV vaccine types and nonvaccine types closely related to HPV16/18 (for cross‐protection), herd immunity among nonvaccinated females and sustained effectiveness of the vaccines on virologic outcomes at the population level (Cameron et al., 2016).
Cappelli MG, Fortunato F, Tafuri S, et al. Cervical cancer prevention: An Italian scenario between organised screening and human papillomaviruses vaccination. Eur J Cancer Care. 2018;27:e12905 10.1111/ecc.12905
Funding information
The project, “Strategies for cervical cancer prevention: a middle and long‐term prediction in Italy,” is funded by the Italian Ministry of Education, University and Research (Future in Research 2013 projects, Grant No. RBFR13TS5J). The publication of this manuscript was supported by a contribution from the University of Foggia research fund (5 x 1,000 IRPEF) in memory of Gianluca Montel.
REFERENCES
- Anttila, A. , Ronco, G. , Clifford, G. , Bray, F. , Hakama, M. , Arbyn, M. , & Weiderpass, E. (2004). Cervical cancer screening programmes and policies in 18 European countries. British Journal of Cancer, 91, 935–941. 10.1038/sj.bjc.6602069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assessorato alle Politiche della salute, Apulia Region, Italy . (2011). Atto di programmazione. Intesa Stato Regione del 29 aprile 2010. Piano Regionale della Prevenzione 2010‐2012. Approvazione. Deliberazione della Giunta Regionale 28 dicembre 2010, n. 2994. Bollettino Ufficiale della Regione Puglia ‐ n. 13 del 25‐01‐2011 Retrieved from http://www.regione.puglia.it/www/web/files/sanita/piano%20prevenzione.pdf
- Bosch, F. X. , & de Sanjose, S. (2003). Chapter 1: Human papillomavirus and cervical cancer ‐ Burden and assessment of causality. Journal of the National Cancer Institute, 31, 3–13. [DOI] [PubMed] [Google Scholar]
- Bruni, L. , Barrionuevo‐Rosas, L. , Albero, G. , Serrano, B. , Mena, M. , Gómez, D. , … de Sanjosé, S. (March 20, 2015). ICO Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in Italy. Summary Report 2015‐03‐20. Retrieved from http://www.hpvcentre.net/statistics/reports/ITA.pdf
- Bruni, L. , Barrionuevo‐Rosas, L. , Albero, G. , Serrano, B. , Mena, M. , Gómez, D. , … de Sanjosé, S. (March 24, 2015). ICO Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in the World. Summary Report 2015‐03‐24. Retrieved from http://www.hpvcentre.net/statistics/reports/XWX.pdf
- Bruni, L. , Barrionuevo‐Rosas, L. , Albero, G. , Serrano, B. , Mena, M. , Gómez, D. , … de Sanjosé, S. (April 8, 2015). ICO Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in Europe. Summary Report 2015‐04‐08. Retrieved from http://www.hpvcentre.net/statistics/reports/XEX.pdf
- Cameron, R. L. , Kavanagh, K. , Pan, J. , Love, J. , Cuschieri, K. , Robertson, C. , … Pollock, K. G. J. . (2016). Human Papillomavirus Prevalence and Herd Immunity after Introduction of Vaccination Program, Scotland, 2009‐2013. Emerging Infectious Diseases journal, 22(1), 56–64. 10.3201/eid2201.150736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capocaccia, R. , Martina, L. , Inghelmann, R. , Crocetti, C. , De Lisi, V. , Falcini, F. , … De Angelis, R. (2009). A method to estimate mortality trends when death certificates are imprecisely coded: An application to cervical cancer in Italy. International Journal of Cancer, 124(5), 1200–1205. 10.1002/ijc.24033 [DOI] [PubMed] [Google Scholar]
- Commissione tecnico‐scientifica regionale vaccini, Apulia Region, Italy (2014). Modifica Calendario Regionale per la vita 2012 ‐ DGR 241/2013. Approvazione nuovo Calendario Vaccinale per la vita 2014. Deliberazione della Giunta Regionale 20 maggio 2014, n. 958. Bollettino Ufficiale della Regione Puglia n. 74 del 11‐06‐2014. pp: 19468‐19486”. Retrieved from http://www.regione.puglia.it/index.php?page=burp&opz=getfile&file=N74_11_06_14.pdf
- De Angelis, R. , Rossi, S. , Martina, L. , Meduri, C. , Galati, F. , & Capocaccia, R. (2010). Stime di incidenza e mortalità per cervico‐carcinoma in Italia In Giambi C. & De Santis S. (Eds). Workshop. La prevenzione dell'infezione da papilloma virus umano in Italia. Roma, 28 settembre 2009. Atti. Rome, Italy: Istituto Superiore di Sanità. [Google Scholar]
- Galise, I. , Rashid, I. , Cuccaro, F. , Bisceglia, L. , Coviello, V. , Melcarne, A. , … Gatta, G. (2013). Estimates of cancer burden in Puglia. Tumori, 99(3), 382–389. 10.1177/030089161309900314 [DOI] [PubMed] [Google Scholar]
- Grazzini, G. , & Zappa, M. (2008). Attendance in cancer screening programmes in Italy. Italian Journal of Public Health, 5(2), 117–124. [Google Scholar]
- Hakama, M. , Coleman, M. P. , Alexe, D. M. , & Auvinen, A. (2008). Cancer screening: Evidence and practice in Europe 2008. European Journal of Cancer, 44(10), 1404–1413. 10.1016/j.ejca.2008.02.013 [DOI] [PubMed] [Google Scholar]
- Istituto Superiore di Sanità (ISS) (2013). Andamenti di incidenza e mortalità per cervicocarcinoma in Italia. Retrieved from http://www.epicentro.iss.it/approfondimenti/2013/8marzoTumori.asp
- Istituto Superiore di Sanità (ISS) (2015). Infezioni da hpv e cervicocarcinoma. Strategie vaccinali per Hpv. Retrieved from http://www.epicentro.iss.it/problemi/hpv/StrategieVaccini.asp.
- Istituto Superiore di Sanità (ISS) (2016). Le vaccinazioni in Italia. Copertura vaccinale anti Hpv. Retrieved from http://www.epicentro.iss.it/temi/vaccinazioni/dati_Ita.asp?tab-container-1=tab 113
- Istituto Superiore di Sanità (ISS) (December 1, 2016). La Sorveglianza Passi. Screening cervicale. Retrieved from http://www.epicentro.iss.it/passi/dati/ScreeningCervicale.asp
- Italian Ministry of Health (2012). Decree October 18, 2012. Remunerazione prestazioni di assistenza ospedaliera per acuti, assistenza ospedaliera di riabilitazione e di lungodegenza post acuzie e di assistenza specialistica ambulatoriale. Retrieved from http://www.gazzettaufficiale.it/eli/id/2013/01/28/13A00528/sg
- Italian Ministry of Health (2013). Piano Nazionale della Prevenzione 2010‐2012. Azione centrale prioritaria concernente la definizione di documenti tecnici di sintesi delle evidenze scientifiche a supporto della programmazione, monitoraggio e valutazione degli interventi di prevenzione oncologica nella popolazione a rischio. Documento di indirizzo sull'utilizzo dell'HPV‐DNA come test primario per lo screening del cancro del collo dell'utero. Retrieved from http://www.osservatorionazionalescreening.it/sites/default/files/allegati/Screening.pdf
- Italian Ministry of Health (January 13, 2013). Screening per il cancro del collo dell'utero. Retrieved from http://www.salute.gov.it/portale/salute/p1_5.jsp?id=27&area=Screening
- Italian Ministry of Health. Conferenza permanente per i rapporti tra lo Stato, le Regioni e le Province Autonome di Trento e Bolzano (2007). Intesa ai sensi dell'articolo 8, comma 6, della legge 5 giugno 2003, n. 131, del 20 dicembre 2007 concernente “Strategie per la vaccinazione anti‐HPV in Italia”. Retrieved from http://www.statoregioni.it/Documenti/DOC_016696_264%20csr.pdf
- Italian Ministry of Health. Conferenza Permanente per i rapporti tra lo Stato, le Regioni e le Province Autonome di Trento e Bolzano (2014). Intesa, ai sensi dell'articolo 8, comma 6 della legge 5 giugno 2003, n. 131, del 13 novembre 2014 sulla proposta del Ministero della salute concernente il Piano nazionale per la prevenzione per gli anni 2014‐2018. Retrieved from http://www.salute.gov.it/imgs/C_17_pubblicazioni_2285_allegato.pdf
- von Karsa, L. , Arbyn, A. , & De Vuyst, H. , et al. (2015). Executive summary In Arbyn A. A. & De Vuyst H., et al. (Eds.), European guidelines for quality assurance in cervical cancer screening. Second edition, Supplements. Luxembourg: Office for Official Publications of the European Union. [Google Scholar]
- Mancuso, P. , Sacchettini, C. , Vicentini, M. , Caroli, S. , & Giorgi Rossi, P. (2016). The accuracy of the causes of death and the estimated trend: The case of cervix uteri. Epidemiologia and Prevenzione, 40(3–4), 157–163. [DOI] [PubMed] [Google Scholar]
- Passi Puglia, anni 2011‐2014 . (July 7, 2016). Dalla sorveglianza degli stili di vita alle buone pratiche per la salute I PROGRESSI DELLE AZIENDE SANITARIE PUGLIESI NEGLI ANNI 2011/2014. Retrieved from https://www.sanita.puglia.it/web/oer/studio-passi
- Pimple, S. , Mishra, G. , & Shastri, S. (2016). Global strategies for cervical cancer prevention. Current Opinion in Obstetrics and Gynecology, 28(1), 4–10. 10.1097/GCO.0000000000000241 [DOI] [PubMed] [Google Scholar]
- Ronco, G. , Giubilato, P. , Carozzi, F. , Maia, G. , Giorgi Rossi, P. , Zappa, M. , … Italian cervical cancer screening survey group. (2015). Extension of organized cervical cancer screening programmes in Italy and their process indicators, 2011‐2012 activity. Epidemiologia and Prevenzione, 39(3 Suppl 1), 61–76. [PubMed] [Google Scholar]
- Rosano, A. , de Belvis, A. G. , Sferrazza, A. , Burgio, A. , Ricciardi, W. , van der Zee, J. (2013). Trends in avoidable hospitalization rates in Italy, 2001‐2008. Epidemiology Biostatistics and Public Health, 10(4), e88171–e88178. [Google Scholar]
- Rossi, S. , Crocetti, E. , Capocaccia, R. , Gatta, G. , & AIRTUM Working Group (2013). Estimates of cancer burden in Italy. Tumori 99(3): 416–424. 10.1177/030089161309900318 [DOI] [PubMed] [Google Scholar]
- Serraino, D. , Gini, A. , Taborelli, M. , Ronco, G. , Giorgi‐Rossi, P. , Zappa, M. , … Members of ‘IMPATTO‐CERVICE’ working group; Members of ‘IMPATTO‐CERVICE’ working group . (2015). Changes in cervical cancer incidence following the introduction of organized screening in Italy. Preventive Medicine, 75, 56–63. 10.1016/j.ypmed.2015.01.034 [DOI] [PubMed] [Google Scholar]
- Veerus, P. , Arbyn, M. , Amati, C. , Paolo, B. , & EUROCHIP Working Group . (2010). Impact of implementing a nationwide cervical cancer screening program on female population coverage by Pap‐tests in Estonia. Tumori 96(4): 524–528. [DOI] [PubMed] [Google Scholar]
- Williams, J. H. , Carter, S. M. , & Rychetnik, L. (2014). Organised cervical screening 45 years on: How consistent are organised screening practices? European Journal of Cancer, 50(17), 3029–3038. 10.1016/j.ejca.2014.09.005 [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) (2014). Human papillomavirus vaccines: WHO position paper, October 2014. Weekly epidemiological record, 89(43), 465–491. [PubMed] [Google Scholar]
- World Health Organization (WHO) (2016). Human papillomavirus (HPV) and cervical cancer. Fact sheet N°380. Retrieved from http://www.who.int/mediacentre/factsheets/fs380/en/


