Abstract
Background
This study aimed to evaluate anxiety and pain following perioperative music interventions compared with control conditions in adult patients.
Methods
Eleven electronic databases were searched for full‐text publications of RCTs investigating the effect of music interventions on anxiety and pain during invasive surgery published between 1 January 1980 and 20 October 2016. Results and data were double‐screened and extracted independently. Random‐effects meta‐analysis was used to calculate effect sizes as standardized mean differences (MDs). Heterogeneity was investigated in subgroup analyses and metaregression analyses. The review was registered in the PROSPERO database as CRD42016024921.
Results
Ninety‐two RCTs (7385 patients) were included in the systematic review, of which 81 were included in the meta‐analysis. Music interventions significantly decreased anxiety (MD –0·69, 95 per cent c.i. –0·88 to –0·50; P < 0·001) and pain (MD –0·50, –0·66 to –0·34; P < 0·001) compared with controls, equivalent to a decrease of 21 mm for anxiety and 10 mm for pain on a 100‐mm visual analogue scale. Changes in outcome corrected for baseline were even larger: MD –1·41 (–1·89 to –0·94; P < 0·001) for anxiety and –0·54 (–0·93 to –0·15; P = 0·006) for pain. Music interventions provided during general anaesthesia significantly decreased pain compared with that in controls (MD –0·41, –0·64 to –0·18; P < 0·001). Metaregression analysis found no significant association between the effect of music interventions and age, sex, choice and timing of music, and type of anaesthesia. Risk of bias in the studies was moderate to high.
Conclusion
Music interventions significantly reduce anxiety and pain in adult surgical patients.
Short abstract
Effective
Introduction
Worldwide, an estimated 266–360 million surgical procedures are undertaken annually according to the WHO1. Surgical patients often suffer from preoperative anxiety and postoperative pain; recent data suggest that 75 per cent of patients facing surgery are anxious, despite anxiety‐decreasing measures2, 3. Preoperative anxiety can increase the level of postoperative pain4 and, despite interventions to reduce postoperative pain, approximately 40–65 per cent of patients experience moderate to severe pain after surgery5, 6.
As the use of analgesics has inherent side‐effects6, music interventions have been suggested as a way to reduce perioperative anxiety7, 8 and postoperative pain6, 9. Despite a large number of studies, perioperative music interventions are still not used widely. Two recently published meta‐analyses9, 10 on the effect of music interventions in different hospital procedures, and of different forms of perioperative art therapy, reported small to moderate beneficial effects on anxiety and pain in surgical, but also in non‐surgical, patients. Research on music interventions in healthcare often identifies heterogeneity in study populations and lack of negative studies possibly owing to publication bias. These factors may be the reason why perioperative music interventions are not often applied in clinical practice.
The purpose of the present study therefore was to perform a systematic review and meta‐analysis of all RCTs evaluating the effects of music interventions on patients' anxiety and pain before, during and after exclusively invasive surgical procedures.
Methods
This systematic review and meta‐analysis was conducted according to the PRISMA statement11. The review was registered in the PROSPERO database (https://www.crd.york.ac.uk/PROSPERO) as record number CRD42016024921.
Search strategy
A dedicated biomedical information specialist helped define the search strategy. The electronic databases Embase, MEDLINE, OvidSP, Web of Science, Scopus, PsycINFO, OvidSP, CINAHL, Cochrane Central Register of Controlled Trials, PubMed publisher and Google Scholar were searched for publications on the effect of music interventions before, during and after surgery published between 1 January 1980 and 20 October 2016 (Appendix S1, supporting information).
Study selection
Titles and abstracts of articles identified by the search, and full texts of those deemed potentially eligible, were double‐screened for relevance by four investigators independently. Inclusion criteria for the systematic review were: full‐text article of an RCT; investigating effects of music interventions on anxiety and/or pain; mean age of participants at least 18 years; written in English; invasive surgical procedures, either open or laparoscopic, such as abdominal surgery or total knee surgery; use of general anaesthesia, regional anaesthesia or both; use of any recorded or live music intervention having melody, harmony and rhythm; intervention offered by a researcher or a music therapist; and intervention performed in a hospital or outpatient clinic. Studies involving non‐invasive procedures such as endoscopy were excluded, as were those using quasi‐ or pseudo‐randomization. Nature sounds were considered only when they were used in addition to music. If populations overlapped between studies, only the most recent or most complete study was included. Studies were included in the meta‐analysis only if they included measures of dispersion of a particular outcome. A fifth investigator was consulted in the event of disagreement about inclusion of an article.
Data extraction
Data were extracted and checked by three authors independently. The following study characteristics were recorded: author, year of publication, journal, number of patients, sex ratio, mean age, inclusion period, mean follow‐up, ethical approval, outcome scale used, type of surgery, type of anaesthesia, timing of the music intervention (before, during or after surgery), recorded versus live music intervention and description of intervention, and type of control group. Primary outcomes were mean anxiety scores and mean pain scores (including measures of dispersion) in the intervention and control groups measured at baseline and at the end of the study or within 7 days after operation. When available, outcome data on change from baseline, including measures of dispersion for both intervention and control groups, were also extracted. If a study used multiple time points, only the first and final time points were considered (at most 7 days after surgery).
Statistical analysis
Data were analysed using Review Manager version 5.3.5 (The Nordic Cochrane Centre, Copenhagen, Denmark). Outcome measures were pooled using the inverse‐variance method in a random‐effects model. Standardized mean differences (MDs) were calculated with Hedges' adjusted g using pooled weighted standard deviations. Effect sizes were summarized with 95 per cent confidence intervals. In five studies only an i.q.r. or range was provided; the i.q.r. was divided by 1·3512 and the range by 4 to produce approximations of the standard deviation. Data were summarized and presented visually in forest plots. Funnel plots were constructed to investigate publication bias. Heterogeneity among included studies was analysed with both the Cochran Q statistic and the I 2 index. Risk of bias among studies was assessed by three reviewers using the Cochrane Collaboration risk‐of‐bias assessment tool13. Two‐sided statistical significance was inferred at P < 0·050.
A metaregression analysis was conducted in Stata® release 14 (StataCorp, College Station, Texas, USA) to investigate possible associations between study characteristics and the effect of music. The following subgroups were chosen a priori for subgroup analyses: timing of intervention (before, during or after surgery); type of anaesthesia (general or regional); type of music intervention (chosen by investigator, chosen by patient from a list provided, or patient's own music). During data collection, other variables that could potentially influence the intervention effect were added: single (only 1 intervention during the course of the study) or multiple (several music interventions during the course of the study) music interventions; sex; and age. Multivariable metaregression analyses were carried out first with all variables, and subsequently based on the results of the subgroup analyses and univariable metaregression analyses, including only variables that were either statistically significant or had a β‐coefficient larger than the corresponding standard error.
Back‐transformations were calculated in Microsoft Excel® (Microsoft Corporation, Redmond, Washington, USA) by multiplying the MD of both State–Trait Anxiety Inventory (STAI)14 and visual analogue scale (VAS) scores for anxiety and VAS scores for pain with the typical among‐person standard deviation, which was derived from pooling baseline standard deviations of control arms from studies that reported these.
Results
The literature search resulted in the inclusion of 92 RCTs8, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101, 102, 103, 104, 105 in the systematic review (7385 patients). Eighty‐one of these were included in the meta‐analysis (Fig. 1). Details of study characteristics are presented in Table S1 (supporting information).
Figure 1.
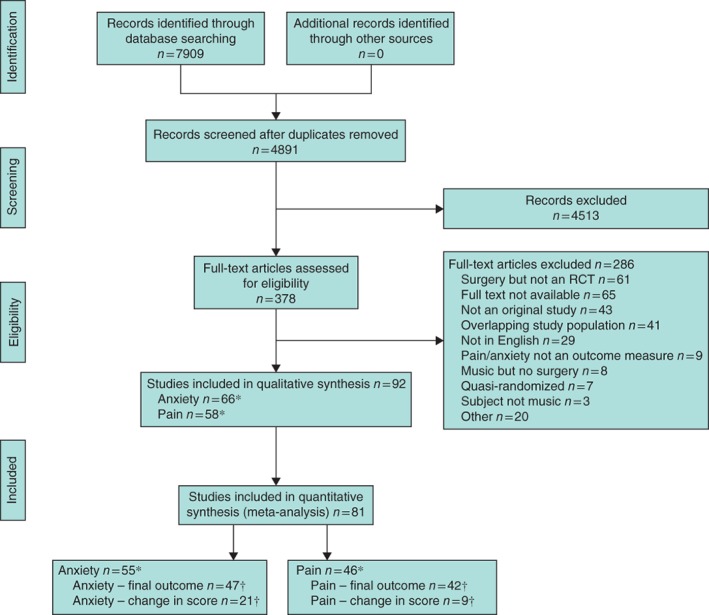
Flow chart showing selection of studies for review. *Some studies reported both anxiety and pain outcomes. †Some studies reported both final outcome and change in scores
The studies investigated music interventions in many types of surgery and in different patient populations, with a mean(s.d.) age of 51·7(10·4) years and predominance of women (57 per cent). Most studies evaluating anxiety outcomes used the STAI (55 per cent) and/or a VAS (43 per cent); the studies evaluating pain outcomes used a VAS (79 per cent) and/or a numerical rating scale (21 per cent). In the majority of studies (67 per cent on anxiety, 64 per cent on pain) the effects of single interventions were investigated. Music interventions were offered before operation (anxiety: 17, 26 per cent; pain: 3, 5 per cent), during surgery (anxiety: 13, 20 per cent; pain: 13, 22 per cent), after operation (anxiety: 13, 20 per cent; pain: 21, 36 per cent), at multiple times (anxiety: 22, 33 per cent; pain: 21, 36 per cent) or not specified (anxiety: 1, 2 per cent). Four studies (4 per cent) investigated anxiety and/or pain‐reducing effects of live music therapy provided by a music therapist, whereas all other studies used recorded music interventions. Control arms of studies provided standard medical care without (28, 30 per cent) or with (11, 12 per cent) a resting period, reported no music (13, 14 per cent), reported no intervention (17, 18 per cent), used a device with sham sounds (8, 9 per cent), provided headphones without music (6, 7 per cent) or with noise‐blocking features (2, 2 per cent), used midazolam (1, 1 per cent) or had an unclear description (5, 5 per cent). Eleven RCTs15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25 (12 per cent) did not report on quantitative data and could not therefore be included in the quantitative analyses (Table S1, supporting information).
Risk‐of‐bias assessment
The included studies had a moderate to high risk of bias (Fig. S1, supporting information). As blinding of patients to music interventions during surgery is only feasible under general anaesthesia, the assessment was limited to blinding of personnel involved in patient care. All included studies reported the use of randomization, but studies that did not report specific methods of sequence generation or allocation concealment were assessed as having an unclear risk of selection bias. Few studies reported on attrition bias (43, 47 per cent), blinding of data collectors (33, 36 per cent), reporting bias (16, 17 per cent) and other bias (4, 4 per cent); in most studies, therefore, a majority of bias regarding these variables was unclear. Inspection of funnel plots for the presence of publication bias revealed a tendency towards asymmetry in the funnel plot for anxiety, but not in that for pain (Figs S2 and S3, supporting information).
Effect of music interventions on anxiety and pain
Pooling data on the different outcome measures of anxiety from the intervention and control groups resulted in a moderate to large statistically significant MD of –0·69 (95 per cent c.i. –0·88 to –0·50; P < 0·001). Pooling of the data on mean change in anxiety scores between postoperative outcomes and preoperative baseline measurements from the 21 studies that reported this revealed a large effect of music interventions in reducing anxiety, with a MD of –1·41 (–1·89 to –0·94; P < 0·001) (Table 1 and Fig. 2; Fig. S4, supporting information).
Table 1.
Results of meta‐analyses for the outcome anxiety (55 studies) and pain (46 studies)
| No. of studies | Mean difference* | P | I 2 (%) | |
|---|---|---|---|---|
| Anxiety | ||||
| Final anxiety score | 47 | –0·69 (–0·88, –0·50) | < 0·001 | 87 |
| Change in anxiety score* | 21 | –1·41 (–1·89, –0·94) | < 0·001 | 95 |
| Subgroup analyses | ||||
| Selection of music | ||||
| Chosen by patient from list provided | 23 | –0·71 (–0·99, –0·43) | < 0·001 | 88 |
| Chosen by investigator | 19 | –0·67 (–0·97, –0·36) | < 0·001 | 87 |
| Patient's own | 4 | –0·45 (–0·82, –0·07) | 0·020 | 75 |
| Timing† | ||||
| Preoperative | 13 | –1·10 (–1·53, –0·66) | < 0·001 | 89 |
| Perioperative | 10 | –0·57 (–1·06, –0·09) | 0·020 | 92 |
| Postoperative | 10 | –0·66 (–1·07, –0·25) | 0·002 | 87 |
| No. of interventions | ||||
| Single | 34 | –0·76 (–1·02, –0·50) | < 0·001 | 91 |
| Multiple | 13 | –0·51 (–0·64, –0·38) | < 0·001 | 0 |
| Type of anaesthesia‡ | ||||
| General | 13 | –0·47 (–0·71, –0·23) | < 0·001 | 69 |
| General, only perioperative music | 1 | –0·23 (–0·62, 0·17) | – | |
| Regional | 14 | –0·88 (–1·34, –0·42) | < 0·001 | 92 |
| Pain | ||||
| Final pain score | 42 | –0·50 (–0·66, –0·34) | < 0·001 | 78 |
| Change in pain score* | 9 | –0·54 (–0·93, –0·15) | 0·006 | 84 |
| Subgroup analyses | ||||
| Selection of music | ||||
| Chosen by patient from list provided | 21 | –0·55 (–0·81, –0·28) | < 0·001 | 84 |
| Chosen by investigator | 16 | –0·47 (–0·67, –0·26) | < 0·001 | 65 |
| Patient's own | 5 | –0·26 (–0·56, 0·04) | 0·090 | 61 |
| Timing† | ||||
| Preoperative | 3 | –0·73 (–1·54, 0·08) | 0·080 | 84 |
| Perioperative | 10 | –0·18 (–0·36, 0·00) | 0·050 | 44 |
| Postoperative | 19 | –0·53 (–0·79, –0·28) | < 0·001 | 82 |
| No. of interventions | ||||
| Single | 32 | –0·47 (–0·65, –0·29) | < 0·001 | 80 |
| Multiple | 10 | –0·62 (–0·93, –0·30) | < 0·001 | 72 |
| Type of anaesthesia‡ | ||||
| General | 23 | –0·55 (–0·72, –0·39) | < 0·001 | 55 |
| General, only perioperative music | 5 | –0·41 (–0·64, –0·18) | < 0·001 | 9 |
| Regional | 8 | –0·41 (–0·80, –0·03) | 0·040 | 84 |
Values in parentheses are 95 per cent confidence intervals.
Some studies reported on the primary outcome and change in score.
Studies included in analysis used either preoperative, perioperative or postoperative interventions, not multiple.
Studies included in analysis used either general or regional anaesthesia, not both.
Figure 2.
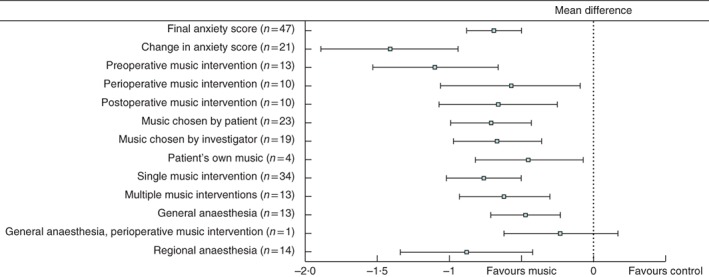
Summary forest plot for anxiety. Mean differences between music intervention and control groups are shown with 95 per cent confidence intervals. The number of studies in each subgroup analysis is indicated
Pooling of the different outcome measures of pain resulted in a statistically significant MD of –0·50 (–0·66 to –0·34; P < 0·001), indicating a moderate effect of music interventions in reducing pain. Pooling of the data on mean change between postoperative outcomes and preoperative baseline measurements in pain scores (9 studies) yielded a MD of –0·54 (–0·93 to –0·15; P = 0·006) (Table 1 and Fig. 3; Fig. S4, supporting information).
Figure 3.
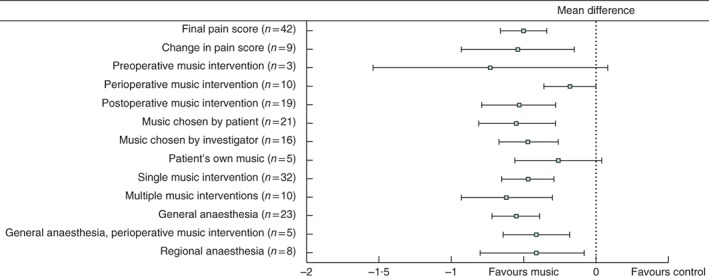
Summary forest plot for pain. Mean differences between music intervention and control groups are shown with 95 per cent confidence intervals. The number of studies in each subgroup analysis is indicated
To facilitate clinical interpretation, effect sizes from the main analyses were back‐transformed, demonstrating that music interventions led to a mean 6·3‐point decrease on the 20–80‐scale of the STAI and a mean 21‐mm decrease on a 100‐mm VAS for anxiety, and to a mean 10‐mm decrease on a 100‐mm VAS for pain.
Subgroup analyses
Subgroup meta‐analyses showed that music interventions before, during and after surgery all led to a reduction in anxiety, with the largest effect seen when offered before surgery (Table 1 and Fig. 2). Postoperative interventions had the largest effect in decreasing pain (Table 1 and Fig. 3). Pooled analysis of the five studies75, 81, 84, 88, 105 that investigated the effects of music interventions solely during general anaesthesia showed a statistically significant decrease in pain. Only one study81 investigated the effect of music interventions during general anaesthesia on anxiety, and demonstrated no significant difference between the music and control groups. Fourteen studies28, 33, 37, 47, 51, 53, 55, 58, 61, 66, 77, 80, 93, 96 investigating music interventions during regional anaesthesia showed a large statistically significant anxiety‐reducing effect. A moderate statistically significant pain‐reducing effect was found for the eight47, 51, 58, 60, 61, 66, 77, 96 studies that investigated music interventions during regional anaesthesia. Pain reduction was enhanced by offering multiple interventions rather than a single music intervention29, 32, 34, 35, 38, 46, 52, 76, 77, 101. An opposite trend was seen for anxiety, where a single intervention had a larger effect8, 27, 28, 30, 36, 37, 39, 40, 42, 45, 47, 49, 51, 55, 58, 61, 63, 66, 67, 70, 72, 73, 74, 78, 80, 81, 86, 87, 94, 95, 96, 97, 100, 102. The largest beneficial effect on both anxiety and pain was seen when patients selected music from a list provided. The smallest benefit was found when patients had freely chosen the music themselves39, 58, 60, 89, 92, 93, 95.
Studies that had at least three items with low risk of bias were also analysed separately, resulting in a smaller but statistically significant MD of –0·61 (95 per cent c.i. –0·94 to –0·29; P < 0·001) for anxiety and of –0·34 (–0·55 to –0·13; P = 0·002) for pain (Figs S5 and S6, supporting information).
Metaregression
Overall, heterogeneity was high among studies (Table 1). Results of univariable and multivariable metaregression analysis are shown in Tables S2 and S3 (supporting information) respectively. These results were consistent with those of the subgroup meta‐analyses. A statistically significant association between preoperative music interventions and pain was found in the data‐driven multivariable regression analysis of this outcome. None of the other explanatory variables were significant, and no evidence was found for an association between any of the other variables and anxiety or pain.
Discussion
This meta‐analysis found a statistically significant decrease in both anxiety and pain in adults receiving music interventions before, during or after surgery. The effect on anxiety seemed largest when the music intervention was offered before operation; however, music interventions offered during and after surgery also significantly reduced anxiety. Postoperative music interventions were most likely to reduce pain; a significant pain‐reducing effect of preoperative music was also seen in the data‐driven multivariable regression analysis. As preoperative anxiety is associated with postoperative pain4, pain reduction noted after preoperative music interventions might be the result of decreased anxiety. In the present meta‐analysis, the mean changes in anxiety and pain from baseline values showed even larger anxiety‐ and pain‐reducing effects of music than did the direct comparison of postintervention outcomes. Previous meta‐analyses that investigated music interventions also included other interventions10, or other procedures that did not involve surgery9. Moreover, they included fewer RCTs. The results presented here underline and reinforce the findings of other studies7, 9, 10, 106. The more specific inclusion criteria in the present meta‐analysis, which investigated music interventions alone in exclusively surgical populations, emphasize the effect of the intervention, and make it more applicable in practice. The analysis of mean changes in scores between intervention and control situations, with outcome scores corrected for baseline values, reveals the true effect of the intervention more than previous studies have shown, and should encourage its implementation in surgery.
An important finding is that many different music interventions each have positive effects. Although most of the music interventions used in the studies were bound by restrictions, such as slow, soft, relaxing music (Table S1, supporting information), the effect does not seem to be related to one specific type of music. Moreover, it has been suggested that individual music preference is important to the effect of a music intervention54. Effect sizes in the present study were slightly higher when patients chose music from a list provided. The small number of studies that investigated freely chosen music compared with music selected by the investigator and preselected music makes it hard to draw definite conclusions about the importance of individual preferences. Besides individual music preference, specific features of the music intervention such as rhythm and harmony, and the use of specific instruments like string instruments, also seem important features in anxiety and pain reduction107. A placebo effect cannot be ruled out as the studies relied on self‐reporting. It could be argued that a placebo effect is beneficial anyway108, in this instance reducing anxiety and pain. However, the subgroup analysis of perioperative music interventions during general anaesthesia did show a statistically significant pain‐reducing effect. Factors such as distraction strategies and interference from personnel and observers do not play a role when patients are under general anaesthesia75, 81, 84, nor do the psychological effects of listening to music. These considerations militate against a mere placebo effect.
Overall, risk of bias in the included studies was moderate to high. Many studies did not adequately address methodological considerations (randomization techniques and power) and risk of bias, and were therefore scored as having an unclear risk. In randomized trials of non‐pharmacological treatments, it may be difficult to blind the relevant parties and to exclude the influence of the provider's expertise109. Although the nature of music interventions makes it hard to perform double‐blinded studies, suitable randomization and reporting following the CONSORT checklist for non‐pharmacological trials110 could help minimize the risk of bias in future trials. No clear association was found for any explanatory variable in either subgroup analyses or univariable metaregression analyses. A statistically significant association was found between preoperative music interventions and pain in the data‐driven multivariable regression analysis. However, the absence of this effect in the subgroup meta‐analysis, the small number of studies investigating the effect of preoperative music interventions on pain, and the possible issue of multiple testing make the reproducibility of this result questionable.
This study has strengths and limitations. A dedicated biomedical information specialist was consulted to identify all publications on this subject in the scientific literature. Bias was limited by excluding studies that generated randomization sequences inadequately. The present review is, however, limited by the overall high level of heterogeneity. Even though the search was limited to surgical patients, there is a wide variety of surgical procedures in the study population, with diverse methods of anaesthesia. These issues in part explain the large degree of heterogeneity. Moreover, the diverse control conditions also create variety in study populations. Publications might have been missed as a result of the language restriction (Fig. 1). The funnel plot for anxiety raises the possibility of publication bias. Previous publications of mainly favourable results might affect the conclusion of this review.
This review provides evidence for the implementation of music interventions before, during and after surgery. Preoperative anxiety and postoperative pain are clinically relevant issues that may determine morbidity, duration of hospital stay and even mortality2. Alleviating these factors may improve clinical outcomes and quality of life, may also lead to earlier discharge from hospital, and thus may help to reduce healthcare costs111. Pain relief after surgery continues to be an important medical challenge112 and it has been shown that a minimum 12 (95 per cent c.i. 9 to 15)‐mm reduction in VAS pain score signifies clinical relevance113. Based on this, at least some of the patients in the music intervention groups included in this meta‐analysis experienced a clinically relevant reduction in pain. Defining minimally important differences to determine clinically relevant effects is challenging114. No clear minimally important differences for anxiety have been defined; however, minimally important differences for depression have previously been inferred at an MD of 0·50, and an MD of 0·24 has also been reported114. The pooled MD of –0·69 for anxiety reported in the present analysis therefore appears clinically relevant. Some of the included studies have also investigated other parameters to evaluate the efficacy of music interventions. Music has, for instance, been shown to reduce the use of analgesics after surgery24, 35, 39, 60, 76, 82, and was more effective in reducing preoperative anxiety than orally administered midazolam8. More foot movement and a reduction in the rate of delirium was found following music interventions after hip and knee surgery in elderly patients69. Furthermore, duration of hospital stay after mastectomy was shorter for patients receiving music interventions compared with controls102.
Supporting information
Appendix S1 Literature search
Table S1 Study characteristics
Table S2 Results of univariable meta‐regression analysis
Table S3 Results of data driven multivariable meta‐regression analysis
Fig. S1 Summary Risk of Bias
Fig. S2 Funnel plot anxiety
Fig. S3 Funnel plot pain
Fig. S4 Summary forest plots meta‐analyses anxiety and meta‐analyses pain
Fig. S5 Subgroup analysis of anxiety based on studies with Low Risk of Bias, that is those scoring at least three items with Low Risk of Bias
Fig. S6 Subgroup analysis of pain based on studies with Low Risk of Bias, that is those scoring at least three items with Low Risk of Bias
Acknowledgements
The authors thank W. Bramer, biomedical information specialist at the Erasmus University Medical Centre Medical Library, for his expertise with the literature search; J. van der Pijl, medical student, for help with the title and abstract screening; J. van Rosmalen, biostatistician, for advice on metaregression results; and K. Hagoort for critically reviewing the manuscript. The data sets generated during the study and/or analysed here are available from the corresponding author on reasonable request.
This work was funded by Stichting Coolsingel (Rotterdam, The Netherlands) and Stichting Swart‐van Essen (Rotterdam, The Netherlands). The funders of the study had no role in the study design, data collection, data analysis, manuscript preparation and publication decision. All authors had complete access to the study data that support the publication. M.G.M.H. was supported by ZonMw, the European Institute for Biomedical Imaging Research, European Society of Radiology and Cambridge University Press outside of the submitted work.
Disclosure: The authors declare no other conflict of interest.
References
- 1. Weiser TG, Haynes AB, Molina G, Lipsitz SR, Esquivel MM, Uribe‐Leitz T et al Size and distribution of the global volume of surgery in 2012. Bull World Health Organ 2016; 94: 201F–209F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. De Oliveira GS Jr, Holl JL, McCarthy RJ, Butt ZA, Nouriel J, McCaffery K et al Overestimation of mortality risk and preoperative anxiety in patients undergoing elective general surgery procedures: a propensity matched analysis. Int J Surg 2014; 12: 1473–1477. [DOI] [PubMed] [Google Scholar]
- 3. Robleda G, Sillero‐Sillero A, Puig T, Gich I, Baños JE. Influence of preoperative emotional state on postoperative pain following orthopedic and trauma surgery. Rev Lat Am Enfermagem 2014; 22: 785–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ip HY, Abrishami A, Peng PW, Wong J, Chung F. Predictors of postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology 2009; 111: 657–677. [DOI] [PubMed] [Google Scholar]
- 5. Sommer M, de Rijke JM, van Kleef M, Kessels AG, Peters ML, Geurts JW et al The prevalence of postoperative pain in a sample of 1490 surgical inpatients. Eur J Anaesthesiol 2008; 25: 267–274. [DOI] [PubMed] [Google Scholar]
- 6. Cao X, Elvir‐Lazo OL, White PF, Yumul R, Tang J. An update on pain management for elderly patients undergoing ambulatory surgery. Curr Opin Anaesthesiol 2016; 29: 674–682. [DOI] [PubMed] [Google Scholar]
- 7. Bradt J, Dileo C, Shim M. Music interventions for preoperative anxiety. Cochrane Database Syst Rev 2013; (6) CD006908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bringman H, Giesecke K, Thörne A, Bringman S. Relaxing music as pre‐medication before surgery: a randomised controlled trial. Acta Anaesthesiol Scand 2009; 53: 759–764. [DOI] [PubMed] [Google Scholar]
- 9. Hole J, Hirsch M, Ball E, Meads C. Music as an aid for postoperative recovery in adults: a systematic review and meta‐analysis. Lancet 2015; 386: 1659–1671. [DOI] [PubMed] [Google Scholar]
- 10. Vetter D, Barth J, Uyulmaz S, Uyulmaz S, Vonlanthen R, Belli G et al Effects of art on surgical patients: a systematic review and meta‐analysis. Ann Surg 2015; 262: 704–713. [DOI] [PubMed] [Google Scholar]
- 11. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. BMJ 2009; 339: b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Higgins JPT, Green S. (eds). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. http://www.handbook.cochrane.org [accessed 30 November 2017]. [Google Scholar]
- 13. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD et al; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011; d5928: 343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Spielberger CD, Gorsuch RL. Manual for the State–Trait Anxiety Inventory (Form Y): (‘Self‐Evaluation Questionnaire’). Consulting Psychologists Press: Palo Alto, 1983. [Google Scholar]
- 15. Bellan L, Gooi A, Rehsia S. The Misericordia Health Centre cataract comfort study. Can J Ophthalmol 2002; 37: 155–160. [DOI] [PubMed] [Google Scholar]
- 16. Easter B, DeBoer L, Settlemyre G, Starnes C, Marlowe V, Tart RC. The impact of music on the PACU patient's perception of discomfort. J Perianesth Nurs 2010; 25: 79–87. [DOI] [PubMed] [Google Scholar]
- 17. Finlay KA, Wilson JA, Gaston P, Al‐Dujaili EAS, Power I. Post‐operative pain management through audio‐analgesia: investigating musical constructs. Psychol Music 2016; 44: 493–513. [Google Scholar]
- 18. Gaberson KB. The effect of humorous distraction on preoperative anxiety. A pilot study. AORN J 1991; 54: 1258–1264. [DOI] [PubMed] [Google Scholar]
- 19. Heiser RM, Chiles K, Fudge M, Gray SE. The use of music during the immediate postoperative recovery period. AORN J 1997; 65: 777–778, 781–785. [DOI] [PubMed] [Google Scholar]
- 20. Heitz L, Symreng T, Scamman FL. Effect of music therapy in the postanesthesia care unit: a nursing intervention. J Post Anesth Nurs 1992; 7: 22–31. [PubMed] [Google Scholar]
- 21. Kang JG, Lee JJ, Kim DM, Kim JA, Kim CS, Hahm TS et al Blocking noise but not music lowers bispectral index scores during sedation in noisy operating rooms. J Clin Anesth 2008; 20: 12–16. [DOI] [PubMed] [Google Scholar]
- 22. Sen H, Ates F, Sizlan A, Yanarates O, Dere K, Teksoz E et al Effect of music on sedation during local urological surgeries. Anatolian J Clin Invest 2009; 3: 131–135. [Google Scholar]
- 23. Walworth D, Rumana CS, Nguyen J, Jarred J. Effects of live music therapy sessions on quality of life indicators, medications administered and hospital length of stay for patients undergoing elective surgical procedures for brain. J Music Ther 2008; 45: 349–359. [DOI] [PubMed] [Google Scholar]
- 24. Wang Y, Tang H, Guo Q, Liu J, Liu X, Luo J et al Effects of intravenous patient‐controlled sufentanil analgesia and music therapy on pain and hemodynamics after surgery for lung cancer: a randomized parallel study. J Altern Complement Med 2015; 21: 667–672. [DOI] [PubMed] [Google Scholar]
- 25. Wu J, Chaplin W, Amico J, Butler M, Ojie MJ, Hennedy D et al Music for surgical abortion care study: a randomized controlled pilot study. Contraception 2012; 85: 496–502. [DOI] [PubMed] [Google Scholar]
- 26. Alam M, Roongpisuthipong W, Kim NA, Goyal A, Swary JH, Brindise RT et al Utility of recorded guided imagery and relaxing music in reducing patient pain and anxiety, and surgeon anxiety, during cutaneous surgical procedures: a single‐blinded randomized controlled trial. J Am Acad Dermatol 2016; 75: 585–589. [DOI] [PubMed] [Google Scholar]
- 27. Allred KD, Byers JF, Sole ML. The effect of music on postoperative pain and anxiety. Pain Manag Nurs 2010; 11: 15–25. [DOI] [PubMed] [Google Scholar]
- 28. Bae I, Lim HM, Hur MH, Lee M. Intra‐operative music listening for anxiety, the BIS index, and the vital signs of patients undergoing regional anesthesia. Complement Ther Med 2014; 22: 251–257. [DOI] [PubMed] [Google Scholar]
- 29. Bally K, Campbell D, Chesnick K, Tranmer JE. Effects of patient‐controlled music therapy during coronary angiography on procedural pain and anxiety distress syndrome. Crit Care Nurse 2003; 23: 50–58. [PubMed] [Google Scholar]
- 30. Barnason S, Zimmerman L, Nieveen J. The effects of music interventions on anxiety in the patient after coronary artery bypass grafting. Heart Lung 1995; 24: 124–132. [DOI] [PubMed] [Google Scholar]
- 31. Bauer BA, Cutshall SA, Anderson PG, Prinsen SK, Wentworth LJ, Olney TJ et al Effect of the combination of music and nature sounds on pain and anxiety in cardiac surgical patients: a randomized study. Altern Ther Health Med 2011; 17: 16–23. [PubMed] [Google Scholar]
- 32. Binns‐Turner PG, Wilson LL, Pryor ER, Boyd GL, Prickett CA. Perioperative music and its effects on anxiety, hemodynamics, and pain in women undergoing mastectomy. AANA J 2011; 79(Suppl): S21–S27. [PubMed] [Google Scholar]
- 33. Chang SC, Chen CH. Effects of music therapy on women's physiologic measures, anxiety, and satisfaction during cesarean delivery. Res Nurs Health 2005; 28: 453–461. [DOI] [PubMed] [Google Scholar]
- 34. Chen HJ, Chen TY, Huang CY, Hsieh YM, Lai HL. Effects of music on psychophysiological responses and opioid dosage in patients undergoing total knee replacement surgery. Jpn J Nurs Sci 2015; 12: 309–319. [DOI] [PubMed] [Google Scholar]
- 35. Ciğerci Y, Özbayir T. The effects of music therapy on anxiety, pain and the amount of analgesics following coronary artery surgery. Turk Gogus Kalp Dama 2016; 24: 44–50. [Google Scholar]
- 36. Cooke M, Chaboyer W, Schluter P, Hiratos M. The effect of music on preoperative anxiety in day surgery. J Adv Nurs 2005; 52: 47–55. [DOI] [PubMed] [Google Scholar]
- 37. Cruise CJ, Chung F, Yogendran S, Little D. Music increases satisfaction in elderly outpatients undergoing cataract surgery. Can J Anaesth 1997; 44: 43–48. [DOI] [PubMed] [Google Scholar]
- 38. Dabu‐Bondoc S, Vadivelu N, Benson J, Perret D, Kain ZN. Hemispheric synchronized sounds and perioperative analgesic requirements. Anesth Analg 2010; 110: 208–210. [DOI] [PubMed] [Google Scholar]
- 39. Ebneshahidi A, Mohseni M. The effect of patient‐selected music on early postoperative pain, anxiety, and hemodynamic profile in cesarean section surgery. J Altern Complement Med 2008; 14: 827–831. [DOI] [PubMed] [Google Scholar]
- 40. Gaberson KB. The effect of humorous and musical distraction on preoperative anxiety. AORN J 1995; 62: 784–788, 790–791. [DOI] [PubMed] [Google Scholar]
- 41. Ghetti CM. Active music engagement with emotional‐approach coping to improve well‐being in liver and kidney transplant recipients. J Music Ther 2011; 48: 463–485. [DOI] [PubMed] [Google Scholar]
- 42. Good M. A comparison of the effects of jaw relaxation and music on postoperative pain. Nurs Res 1995; 44: 52–57. [PubMed] [Google Scholar]
- 43. Good M, Albert JM, Anderson GC, Wotman S, Cong X, Lane D et al Supplementing relaxation and music for pain after surgery. Nurs Res 2010; 59: 259–269. [DOI] [PubMed] [Google Scholar]
- 44. Good M, Chin CC. The effects of Western music on postoperative pain in Taiwan. Kaohsiung J Med Sci 1998; 14: 94–103. [PubMed] [Google Scholar]
- 45. Good M, Stanton‐Hicks M, Grass JA, Cranston Anderson G, Choi C, Schoolmeesters LJ et al Relief of postoperative pain with jaw relaxation, music and their combination. Pain 1999; 81: 163–172. [DOI] [PubMed] [Google Scholar]
- 46. Graversen M, Sommer T. Perioperative music may reduce pain and fatigue in patients undergoing laparoscopic cholecystectomy. Acta Anaesthesiol Scand 2013; 57: 1010–1016. [DOI] [PubMed] [Google Scholar]
- 47. Guerrero JM, Castaño PM, Schmidt EO, Rosario L, Westhoff CL. Music as an auxiliary analgesic during first trimester surgical abortion: a randomized controlled trial. Contraception 2012; 86: 157–162. [DOI] [PubMed] [Google Scholar]
- 48. Hansen MM. A feasibility pilot study on the use of complementary therapies delivered via mobile technologies on Icelandic surgical patients' reports of anxiety, pain, and self‐efficacy in healing. BMC Complement Altern Med 2015; 15: 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Heidari S, Babaii A, Abbasinia M, Shamali M, Abbasi M, Rezaei M. The effect of music on anxiety and cardiovascular indices in patients undergoing coronary artery bypass graft: a randomized controlled trial. Nurs Midwifery Stud 2015; 4: e31157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hook L, Sonwathana P, Petpichetchian W. Music therapy with female surgical patients: effect on anxiety and pain. Thai J Nurs Res 2008; 12: 259–271. [Google Scholar]
- 51. Hudson B, Ogden J, Whiteley M. Randomized controlled trial to compare the effect of simple distraction interventions on pain and anxiety experienced during conscious surgery. Eur J Pain 2015; 19: 1447–1455. [DOI] [PubMed] [Google Scholar]
- 52. Ikonomidou E, Rehnström A, Naesh O. Effect of music on vital signs and postoperative pain. AORN J 2004; 80: 269–274, 277–278. [DOI] [PubMed] [Google Scholar]
- 53. Ilkkaya NK, Ustun FE, Sener EB, Kaya C, Ustun YB, Koksal E et al The effects of music, white noise, and ambient noise on sedation and anxiety in patients under spinal anesthesia during surgery. J Perianesth Nurs 2014; 29: 418–426. [DOI] [PubMed] [Google Scholar]
- 54. Jafari H, Emami Zeydi A, Khani S, Esmaeili R, Soleimani A. The effects of listening to preferred music on pain intensity after open heart surgery. Iran J Nurs Midwifery Res 2012; 17: 1–6. [PMC free article] [PubMed] [Google Scholar]
- 55. Jiménez‐Jiménez M, García‐Escalona A, Martín‐López A, De Vera‐Vera R, De Haro J. Intraoperative stress and anxiety reduction with music therapy: a controlled randomized clinical trial of efficacy and safety. J Vasc Nurs 2013; 31: 101–106. [DOI] [PubMed] [Google Scholar]
- 56. Johnson B, Raymond S, Goss J. Perioperative music or headsets to decrease anxiety. J Perianesth Nurs 2012; 27: 146–154. [DOI] [PubMed] [Google Scholar]
- 57. Kaempf G, Amodei ME. The effect of music on anxiety. A research study. AORN J 1989; 50: 112–118. [DOI] [PubMed] [Google Scholar]
- 58. Kim YK, Kim SM, Myoung H. Musical intervention reduces patients' anxiety in surgical extraction of an impacted mandibular third molar. J Oral Maxillofac Surg 2011; 69: 1036–1045. [DOI] [PubMed] [Google Scholar]
- 59. Kipnis G, Tabak N, Koton S. Background music playback in the preoperative setting: does it reduce the level of preoperative anxiety among candidates for elective surgery? J Perianesth Nurs 2016; 31: 209–216. [DOI] [PubMed] [Google Scholar]
- 60. Koch ME, Kain ZN, Ayoub C, Rosenbaum SH. The sedative and analgesic sparing effect of music. Anesthesiology 1998; 89: 300–306. [DOI] [PubMed] [Google Scholar]
- 61. Kongsawatvorakul C, Charakorn C, Paiwattananupant K, Lekskul N, Rattanasiri S, Lertkhachonsuk AA. Limited impact of music therapy on patient anxiety with the large loop excision of transformation zone procedure – a randomized controlled trial. Asian Pac J Cancer Prev 2016; 17: 2853–2856. [PubMed] [Google Scholar]
- 62. Laurion S, Fetzer SJ. The effect of two nursing interventions on the postoperative outcomes of gynecologic laparoscopic patients. J Perianesth Nurs 2003; 18: 254–261. [DOI] [PubMed] [Google Scholar]
- 63. Lee KC, Chao YH, Yiin JJ, Chiang PY, Chao YF. Effectiveness of different music‐playing devices for reducing preoperative anxiety: a clinical control study. Int J Nurs Stud 2011; 48: 1180–1187. [DOI] [PubMed] [Google Scholar]
- 64. Lepage C, Drolet P, Girard M, Grenier Y, DeGagné R. Music decreases sedative requirements during spinal anesthesia. Anesth Analg 2001; 93: 912–916. [DOI] [PubMed] [Google Scholar]
- 65. Li XM, Yan H, Zhou KN, Dang SN, Wang DL, Zhang YP. Effects of music therapy on pain among female breast cancer patients after radical mastectomy: results from a randomized controlled trial. Breast Cancer Res Treat 2011; 128: 411–419. [DOI] [PubMed] [Google Scholar]
- 66. Li Y, Dong Y. Preoperative music intervention for patients undergoing cesarean delivery. Int J Gynaecol Obstet 2012; 119: 81–83. [DOI] [PubMed] [Google Scholar]
- 67. Liu Y, Petrini MA. Effects of music therapy on pain, anxiety, and vital signs in patients after thoracic surgery. Complement Ther Med 2015; 23: 714–718. [DOI] [PubMed] [Google Scholar]
- 68. Masuda T, Miyamoto K, Shimizu K. Effects of music listening on elderly orthopaedic patients during postoperative bed rest. Nord J Music Ther 2005; 14: 4–14. [Google Scholar]
- 69. McCaffrey R, Locsin R. The effect of music on pain and acute confusion in older adults undergoing hip and knee surgery. Holist Nurs Pract 2006; 20: 218–224. [DOI] [PubMed] [Google Scholar]
- 70. McClurkin SL, Smith CD. The duration of self‐selected music needed to reduce preoperative anxiety. J Perianesth Nurs 2016; 31: 196–208. [DOI] [PubMed] [Google Scholar]
- 71. Mirbagher Ajorpaz N, Mohammadi A, Najaran H, Khazaei S. Effect of music on postoperative pain in patients under open heart surgery. Nurs Midwifery Stud 2014; 3: e20213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Mullooly VM, Levin RF, Feldman HR. Music for postoperative pain and anxiety. J N Y State Nurses Assoc 1988; 19: 4–7. [PubMed] [Google Scholar]
- 73. Nilsson U. The effect of music intervention in stress response to cardiac surgery in a randomized clinical trial. Heart Lung 2009; 38: 201–207. [DOI] [PubMed] [Google Scholar]
- 74. Nilsson U, Rawal N, Enqvist B, Unosson M. Analgesia following music and therapeutic suggestions in the PACU in ambulatory surgery; a randomized controlled trial. Acta Anaesthesiol Scand 2003; 47: 278–283. [DOI] [PubMed] [Google Scholar]
- 75. Nilsson U, Rawal N, Unosson M. A comparison of intra‐operative or postoperative exposure to music – a controlled trial of the effects on postoperative pain. Anaesthesia 2003; 58: 699–703. [DOI] [PubMed] [Google Scholar]
- 76. Nilsson U, Unosson M, Rawal N. Stress reduction and analgesia in patients exposed to calming music postoperatively: a randomized controlled trial. Eur J Anaesthesiol 2005; 22: 96–102. [DOI] [PubMed] [Google Scholar]
- 77. Ottaviani S, Jean‐Luc B, Thomas B, Pascal R. Effect of music on anxiety and pain during joint lavage for knee osteoarthritis. Clin Rheumatol 2012; 31: 531–534. [DOI] [PubMed] [Google Scholar]
- 78. Padmanabhan R, Hildreth AJ, Laws D. A prospective, randomised, controlled study examining binaural beat audio and pre‐operative anxiety in patients undergoing general anaesthesia for day case surgery. Anaesthesia 2005; 60: 874–877. [DOI] [PubMed] [Google Scholar]
- 79. Palmer JB, Lane D, Mayo D, Schluchter M, Leeming R. Effects of music therapy on anesthesia requirements and anxiety in women undergoing ambulatory breast surgery for cancer diagnosis and treatment: a randomized controlled trial. J Clin Oncol 2015; 33: 3162–3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Pongraweewan O, Lertakyamanee J, Luangnateethep U, Pooviboonsuk P, Nanthaniran M, Sathanasaowapak P et al The efficiency of different adjunct techniques for regional anesthesia. J Med Assoc Thai 2005; 88: 371–376. [PubMed] [Google Scholar]
- 81. Reza N, Ali SM, Saeed K, Abul‐Qasim A, Reza TH. The impact of music on postoperative pain and anxiety following cesarean section. Middle East J Anaesthesiol 2007; 19: 573–586. [PubMed] [Google Scholar]
- 82. Sen H, Yanarateş O, Sızlan A, Kılıç E, Ozkan S, Dağlı G. The efficiency and duration of the analgesic effects of musical therapy on postoperative pain. Agri 2010; 22: 145–150. [PubMed] [Google Scholar]
- 83. Sendelbach SE, Halm MA, Doran KA, Miller EH, Gaillard P. Effects of music therapy on physiological and psychological outcomes for patients undergoing cardiac surgery. J Cardiovasc Nurs 2006; 21: 194–200. [DOI] [PubMed] [Google Scholar]
- 84. Simcock XC, Yoon RS, Chalmers P, Geller JA, Kiernan HA, Macaulay W. Intraoperative music reduces perceived pain after total knee arthroplasty: a blinded, prospective, randomized, placebo‐controlled clinical trial. J Knee Surg 2008; 21: 275–278. [DOI] [PubMed] [Google Scholar]
- 85. Steelman VM. Intraoperative music therapy. Effects on anxiety, blood pressure. AORN J 1990; 52: 1026–1034. [DOI] [PubMed] [Google Scholar]
- 86. Stein TR, Olivo EL, Grand SH, Namerow PB, Costa J, Oz MC. A pilot study to assess the effects of a guided imagery audiotape intervention on psychological outcomes in patients undergoing coronary artery bypass graft surgery. Holist Nurs Pract 2010; 24: 213–222. [DOI] [PubMed] [Google Scholar]
- 87. Szeto CK, Yung PM. Introducing a music programme to reduce preoperative anxiety. Br J Theatre Nurs 1999; 9: 455–459. [DOI] [PubMed] [Google Scholar]
- 88. Szmuk P, Aroyo N, Ezri T, Muzikant G, Weisenberg M, Sessler DI. Listening to music during anesthesia does not reduce the sevoflurane concentration needed to maintain a constant bispectral index. Anesth Analg 2008; 107: 77–80. [DOI] [PubMed] [Google Scholar]
- 89. Taylor LK, Kuttler KL, Parks TA, Milton D. The effect of music in the postanesthesia care unit on pain levels in women who have had abdominal hysterectomies. J Perianesth Nurs 1998; 13: 88–94. [DOI] [PubMed] [Google Scholar]
- 90. Téllez A, Sánchez‐Jáuregui T, Juárez‐García DM, García‐Solís M. Breast biopsy: the effects of hypnosis and music. Int J Clin Exp Hypn 2016; 64: 456–469. [DOI] [PubMed] [Google Scholar]
- 91. Twiss E, Seaver J, McCaffrey R. The effect of music listening on older adults undergoing cardiovascular surgery. Nurs Crit Care 2006; 11: 224–231. [DOI] [PubMed] [Google Scholar]
- 92. Vaajoki A, Pietilä AM, Kankkunen P, Vehviläinen‐Julkunen K. Effects of listening to music on pain intensity and pain distress after surgery: an intervention. J Clin Nurs 2012; 21: 708–717. [DOI] [PubMed] [Google Scholar]
- 93. Vachiramon V, Sobanko JF, Rattanaumpawan P, Miller CJ. Music reduces patient anxiety during Mohs surgery: an open‐label randomized controlled trial. Dermatol Surg 2013; 39: 298–305. [DOI] [PubMed] [Google Scholar]
- 94. Voss JA, Good M, Yates B, Baun MM, Thompson A, Hertzog M. Sedative music reduces anxiety and pain during chair rest after open‐heart surgery. Pain 2004; 112: 197–203. [DOI] [PubMed] [Google Scholar]
- 95. Wang SM, Kulkarni L, Dolev J, Kain ZN. Music and preoperative anxiety: a randomized, controlled study. Anesth Analg 2002; 94: 1489–1494. [DOI] [PubMed] [Google Scholar]
- 96. Wang Y, Dong Y, Li Y. Perioperative psychological and music interventions in elderly patients undergoing spinal anesthesia: effect on anxiety, heart rate variability, and postoperative pain. Yonsei Med J 2014; 55: 1101–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Winter MJ, Paskin S, Baker T. Music reduces stress and anxiety of patients in the surgical holding area. J Post Anesth Nurs 1994; 9: 340–343. [PubMed] [Google Scholar]
- 98. Wiwatwongwana D, Vichitvejpaisal P, Thaikruea L, Klaphajone J, Tantong A, Wiwatwongwana A. Medscape. The effect of music with and without binaural beat audio on operative anxiety in patients undergoing cataract surgery: a randomized controlled trial. Eye (Lond) 2016; 30: 1407–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Yates GJ, Silverman MJ. Immediate effects of single‐session music therapy on affective state in patients on a post‐surgical oncology unit: a randomized effectiveness study. Arts Psychother 2015; 44: 57–61. [Google Scholar]
- 100. Yung PM, Chui‐Kam S, French P, Chan TM. A controlled trial of music and pre‐operative anxiety in Chinese men undergoing transurethral resection of the prostate. J Adv Nurs 2002; 39: 352–359. [DOI] [PubMed] [Google Scholar]
- 101. Zengin S, Kabul S, Al B, Sarcan E, Doğan M, Yildirim C. Effects of music therapy on pain and anxiety in patients undergoing port catheter placement procedure. Complement Ther Med 2013; 21: 689–696. [DOI] [PubMed] [Google Scholar]
- 102. Zhou K, Li X, Li J, Liu M, Dang S, Wang D et al A clinical randomized controlled trial of music therapy and progressive muscle relaxation training in female breast cancer patients after radical mastectomy: results on depression, anxiety and length of hospital stay. Eur J Oncol Nurs 2015; 19: 54–59. [DOI] [PubMed] [Google Scholar]
- 103. Zimmerman L, Nieveen J, Barnason S, Schmaderer M. The effects of music interventions on postoperative pain and sleep in coronary artery bypass graft (CABG) patients. Sch Inq Nurs Pract 1996; 10: 153–170. [PubMed] [Google Scholar]
- 104. Ni CH, Tsai WH, Lee LM, Kao CC, Chen YC. Minimising preoperative anxiety with music for day surgery patients – a randomised clinical trial. J Clin Nurs 2012; 21: 620–625. [DOI] [PubMed] [Google Scholar]
- 105. Nilsson U, Rawal N, Uneståhl LE, Zetterberg C, Unosson M. Improved recovery after music and therapeutic suggestions during general anaesthesia: a double‐blind randomised controlled trial. Acta Anaesthesiol Scand 2001; 45: 812–817. [DOI] [PubMed] [Google Scholar]
- 106. Lee JH. The effects of music on pain: a meta‐analysis. J Music Ther 2016; 53: 430–477. [DOI] [PubMed] [Google Scholar]
- 107. Nilsson U. The anxiety‐ and pain‐reducing effects of music interventions: a systematic review. AORN J 2008; 87: 780–807. [DOI] [PubMed] [Google Scholar]
- 108. Colagiuri B, Schenk LA, Kessler MD, Dorsey SG, Colloca L. The placebo effect: from concepts to genes. Neuroscience 2015; 307: 171–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P; CONSORT Group . Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med 2008; 148: 295–309. [DOI] [PubMed] [Google Scholar]
- 110. Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P; CONSORT Group . Methods and processes of the CONSORT Group: example of an extension for trials assessing nonpharmacologic treatments. Ann Intern Med 2008; 148: W60–W66. [DOI] [PubMed] [Google Scholar]
- 111. van der Meij E, Huirne JA, Bouwsma EV, van Dongen JM, Terwee CB, van de Ven PM et al Substitution of usual perioperative care by eHealth to enhance postoperative recovery in patients undergoing general surgical or gynecological procedures: study protocol of a randomized controlled trial. JMIR Res Protoc 2016; 5: e245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Rawal N. Current issues in postoperative pain management. Eur J Anaesthesiol 2016; 33: 160–171. [DOI] [PubMed] [Google Scholar]
- 113. Kelly AM. The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J 2001; 18: 205–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Cuijpers P, Turner EH, Koole SL, van Dijke A, Smit F. What is the threshold for a clinically relevant effect? The case of major depressive disorders. Depress Anxiety 2014; 31: 374–378. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Literature search
Table S1 Study characteristics
Table S2 Results of univariable meta‐regression analysis
Table S3 Results of data driven multivariable meta‐regression analysis
Fig. S1 Summary Risk of Bias
Fig. S2 Funnel plot anxiety
Fig. S3 Funnel plot pain
Fig. S4 Summary forest plots meta‐analyses anxiety and meta‐analyses pain
Fig. S5 Subgroup analysis of anxiety based on studies with Low Risk of Bias, that is those scoring at least three items with Low Risk of Bias
Fig. S6 Subgroup analysis of pain based on studies with Low Risk of Bias, that is those scoring at least three items with Low Risk of Bias


