Abstract
Study Objectives:
The aim of this study was to evaluate the accuracy of the Watch-PAT 200 (WP200) for diagnosing obstructive sleep apnea (OSA) in adolescents compared with polysomnography (PSG) according to the respiratory rules for children (RRC) and adults (RRA).
Methods:
A total of 38 adolescents (mean age 15.1 ± 1.4 years; male 28 [73.7%]; body mass index [BMI] 23.1 ± 5.5 kg/m2) with suspected OSA were assessed with the WP200 and standard PSG simultaneously between July 2014 and September 2015 at a tertiary university hospital. All WP200 data were assessed according to the automatic algorithm, and PSG data were scored according to the RRC and RRA. We examined the correlation, agreement, and concordance in the apnea-hypopnea index (AHI) and minimum arterial oxygen saturation (mSaO2) between the WP200 and PSG-RRC or PSG-RRA.
Results:
There were high correlations (r = .945, P < .001 [AHI-WP200 versus AHI-PSG-RRC]; r = .945, P < .001 [AHI-WP200 versus AHI-PSG-RRA]; r = .921, P < .001 [mSaO2-WP versus mSaO2-PSG]) and good agreements in AHI and mSaO2 between the WP200 and PSG. In addition, there were high concordances in AHI severity (Kendall tau-b = .848, P < .001 [AHI-WP200 versus AHI-PSG-RRC]; Kendall tau-b = .944, P < .001 [AHI-WP200 versus AHI-PSG-RRA]) between the WP200 and PSG.
Conclusions:
The WP200 may be a clinically reliable tool for diagnosing OSA in adolescents.
Citation:
Choi JH, Lee B, Lee JY, Kim HJ. Validating the Watch-PAT for diagnosing obstructive sleep apnea in adolescents. J Clin Sleep Med. 2018;14(10):1741–1747.
Keywords: adolescent, obstructive sleep apnea, polysomnography
BRIEF SUMMARY
Current Knowledge/Study Rationale: Many Watch-PAT validation studies compared to polysomnography have shown that the Watch-PAT may be useful in the diagnosis of adult obstructive sleep apnea (OSA). However, there have been few validation studies of the Watch-PAT for diagnosing OSA in adolescents.
Study Impact: The results of this prospective feasibility study suggest that the Watch-PAT may be a clinically reliable diagnostic test for OSA in adolescents.
INTRODUCTION
Obstructive sleep apnea (OSA) is a chronic sleep disorder characterized by recurrent episodes of partial or complete collapse of the upper airway during sleep.1 It can cause various symptoms and signs such as habitual snoring, restless sleep, sleepiness, behavioral problems, and adaptive functioning difficulties such as attention deficit and reduced adaptive skills.1–3 Undetected or untreated childhood OSA may lead to serious complications including metabolic and cardiovascular consequences.4 Therefore, prompt and accurate diagnosis is required in patients with suspected OSA.
Traditionally, overnight full polysomnography (PSG; level 1) has been performed as a gold standard for diagnosing OSA.1,5 However, PSG has some drawbacks such as long waiting time, unfamiliar laboratory environment, and high cost.6,7 Consequently, out-of-center sleep testing using diverse home or portable monitoring devices has been developed to overcome these problems.7
Among varied home or portable monitoring devices, Watch-PAT 200 (WP200; Itamar Medical Ltd., Caesarea, Israel) has a unique feature without conventional assessments such as airflow and respiratory effort.8 In particular, this device measures respiratory events (eg, apnea, hypopnea) using a distinct mechanism. Terminating respiratory disturbances induces decreased oxygen level, increased heart rate, and digital arterial vasoconstriction. Vasoconstriction of fingertip causes reduced peripheral arterial tonometry (PAT) signal.9 The WP200 analyzes these parameter changes and reports the apnea-hypopnea index (AHI) based on the PAT signal.
Numerous validation studies for diagnosing OSA in adults using the WP200 have been performed, and these studies have shown that the device has high concordance in AHI severity, high correlation, and good agreement of AHI with attended, in-laboratory PSG (level 1).10–14 However, there have been few validation studies of a wrist-worn device such as WP200 for the diagnosis of OSA in adolescents. We hypothesized that the device would be a useful alternative diagnostic method for OSA in adolescents. Therefore, the purpose of the study was to investigate the accuracy of the WP200 for identifying OSA in adolescents against standard PSG based on the respiratory rules for children (RRC) and adults (RRA).
METHODS
Participants
This prospective study protocol was approved by the Institutional Review Board at the Ajou University Hospital (AJIRBDEV-DE2-13-324). We enrolled adolescents aged 13 to 17 years with suspicious symptoms and/or signs of OSA (eg, habitual snoring, daytime sleepiness, witnessed apnea, etc.) between July 2014 and September 2015 at a tertiary university hospital. The exclusion criteria were as follows: (1) medical histories that could have interfered with test reliability (eg, autonomic nervous system dysfunction, peripheral neuropathy or vasculopathy, cardiac or lung disease, etc.) or medications that could have affected peripheral arterial tone (eg, alpha-adrenergic receptor-blocking agents, etc.); and (2) finger problems associated with unsuitable PAT probe application.
PSG and WP200
All adolescents underwent standard full PSG (Embla N7000; Natus Medical Inc., San Carlos, California, United States) and the WP200 simultaneously in hospital-based sleep laboratories.
The standard PSG examination consisted of six-channel electroencephalogram, two-channel electrooculogram, sub-mental and leg electromyogram, airflow (thermistor and pressure transducer), respiratory effort (chest and abdominal movement), oxygen saturation, snoring, electrocardiogram, and body position. A sleep technician monitored behavior changes or sleep positions of the adolescents during sleep and manually scored all PSG data including airflow and respiratory effort based on The AASM Manual for the Scoring of Sleep and Associated Events15; a physician finally confirmed the data. Pediatric and adult respiratory events including apnea and hypopnea were scored according to the “recommended” rule. Apnea in children (adults) was defined as the cessation of the respiratory airflow for the duration of at least two breaths (10 seconds). Obstructive apnea was defined as the cessation of airflow with continued respiratory effort (chest and abdominal movement) for the same duration. Hypopnea in children (adults) was defined as a decrease in respiratory airflow of ≥ 30% for the duration of at least two breaths (10 seconds), associated with oxygen desaturation of ≥ 3% or an arousal. All PSG data were manually scored twice based on both rules. Pediatric rules were used and then adult rules were applied.
The WP200 measurements consisted of PAT signal, oxygen saturation, heart rate, wrist activity (actigraphy), snoring, and body position; the WP200 calculate these data using an automatic computerized algorithm.
After we completed interpreting the PSG and WP200 findings, we diagnosed OSA according to the International Classification of Sleep Disorders, Third Edition (ICSD-3).1 The diagnostic criteria for pediatric OSA were respiratory events ≥ 1 per hour of sleep with signs and/or symptoms suggestive of OSA (eg, snoring, witnessed apnea, sleepiness, behavioral problems, etc.). The diagnostic criteria for adult OSA were (1) respiratory events ≥ 5 per hour of sleep with signs and/ or symptoms suggestive of OSA (eg, snoring, witnessed apnea, sleepiness, comorbidities such as cardiovascular diseases, etc.) or (2) respiratory events ≥ 15 per hour of sleep regardless of signs and/or symptoms suggestive of OSA.
Statistical Analysis
All data in the study are presented as frequency (percent) for categorical variables and as mean ± standard deviation for continuous variables. To assess the diagnostic performance of the WP200 measurements, we used typical clinical criteria of 5, 10, and 15 events per hour for pediatric OSA and 5, 15, and 30 events per hour for adult OSA to calculate the diagnostic sensitivity, specificity, accuracy, and positive and negative likelihood ratio (LR; LR+, LR−) values with 95% confidence interval. The Spearman correlation coefficient and Bland-Altman plots were applied to evaluate the correlation and agreement of AHI and minimum arterial oxygen saturation (mSaO2) between PSG and WP200. Kendall tau-b was applied to investigate the concordance of AHI between PSG and WP200. We performed all statistical analyses using R (version 3.3.2; The R Foundation for Statistical Computing, Vienna, Austria). All values of P < .05 were considered to indicate statistical significance.
RESULTS
Participants
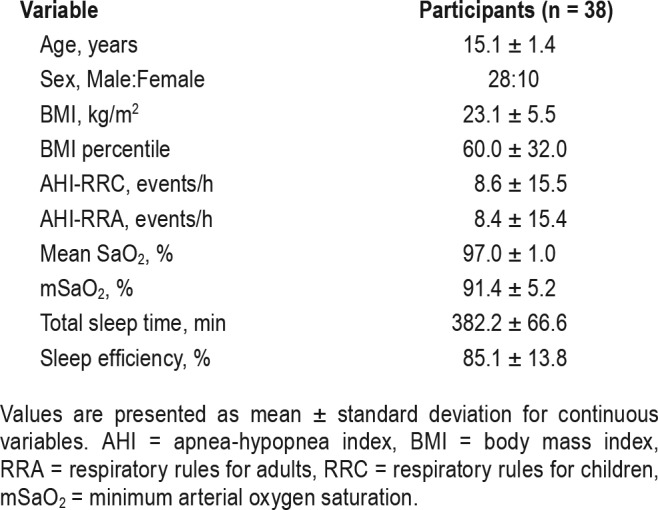
We enrolled 40 adolescents in this study, and 39 participants underwent the WP200 testing. One participant opted out of testing and data from one adolescent were not available due to a test failure. Thus, we ultimately enrolled a total of 38 adolescents of mean age 15.1 ± 1.4 years (range 13–17 years). Characteristics of the study population are presented in Table 1. The study participants consisted of 28 males and 10 females and body mass index (BMI) was 23.1 ± 5.5 kg/m2. BMI percentile for age and sex was 60.0 ± 32.0. AHI according to the RRC was 8.6 ± 15.5 events/h and AHI according to the RRA was 8.4 ± 15.4 events/h. Mean SaO2 (%) and mSaO2 (%) in PSG were 97.0 ± 1.0 and 91.4 ± 5.2, respectively. Total sleep time (minutes) and sleep efficiency (%) in PSG were 382.2 ± 66.6 and 85.1 ± 13.8, respectively.
Table 1.
Characteristics of all adolescent participants (n = 38).
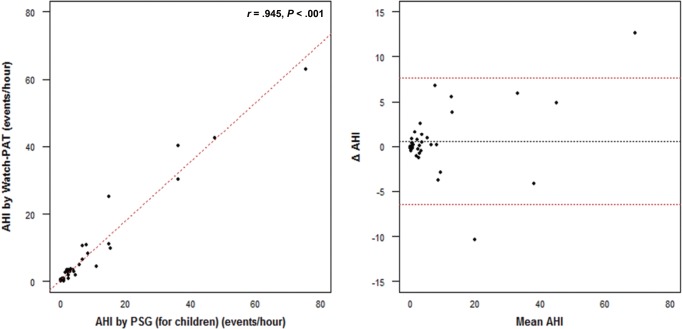
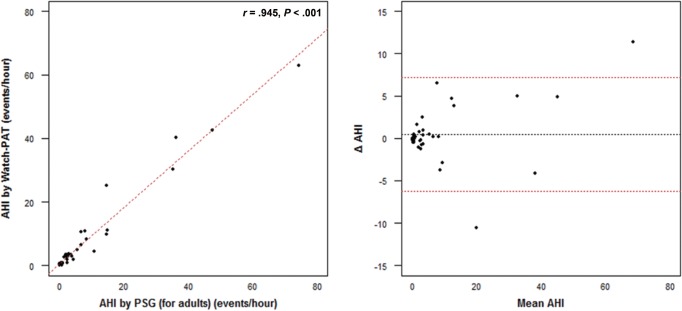
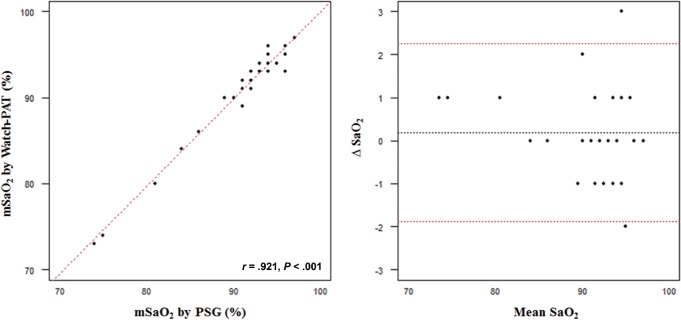
Correlation and Agreement of AHI
Figure 1 and Figure 2 show the comparisons of AHI correlation (scatterplot) and agreement (Bland-Altman plot) measured by the WP200 and PSG according to the RRC and RRA. There were no significant differences between the mean AHI measured by the WP200 and the mean AHI according to the RRC (8.0 ± 14.0 versus 8.6 ± 15.5, P = .255) and the RRA (8.0 ± 14.0 versus 8.4 ± 15.4, P = .471). We also observed no significant differences in average mSaO2 between the WP200 and PSG (91.2 ± 5.4 versus 91.4 ± 5.2, P = .31). There was a high correlation (r = .945, P < .001) and good agreement in mean AHI between the WP200 and PSG according to the RRC and RRA. In addition, a high correlation (r = .921, P < .001) and good agreement was found in average mSaO2 between the two OSA evaluation techniques (Figure 3).
Figure 1. Comparison of AHI correlation and agreement measured by the Watch-PAT 200 and PSG according to the respiratory rules for children in adolescents (n = 38).
AHI = apnea-hypopnea index, PSG = polysomnography, r = Spearman correlation coefficient.
Figure 2. Comparison of AHI correlation and agreement measured by the Watch-PAT 200 and PSG according to the respiratory rules for adults in adolescents (n = 38).
AHI = apnea-hypopnea index, PSG = polysomnography, r = Spearman correlation coefficient.
Figure 3. Comparison of mSaO2 correlation and agreement measured by the Watch-PAT 200 and PSG in adolescents (n = 38).
mSaO2 = minimum arterial oxygen saturation, PSG = polysomnography, r = Spearman correlation coefficient, SaO2 = arterial oxygen saturation.
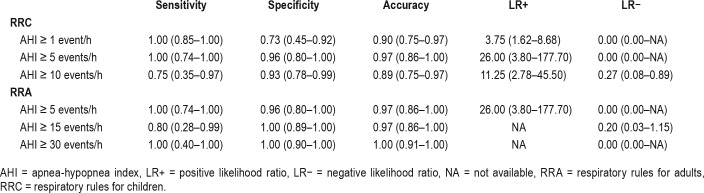
Diagnostic Performance of the WP200 With PSG
Table 2 summarizes the sensitivity, specificity, accuracy, LR+ and LR− of the WP200 with PSG according to the RRC and RRA. When AHI-RRC was used as the gold standard for diagnosis of adolescent OSA, the sensitivity, specificity, accuracy, and LR+ and LR− of different cutoffs of AHI by the WP200 were as follows: at cutoff of ≥ 1, AHI by WP200 had sensitivity of 100%, specificity of 73%, and accuracy of 90% (LR+ 3.75, LR− 0.00); at cutoff of ≥ 5, sensitivity of 100%, specificity of 96%, and accuracy of 97% (LR+ 26.00, LR− 0.00); and at cutoff of ≥ 10, sensitivity of 75%, specificity of 93%, and accuracy of 89% (LR+ 11.25, LR− 0.27). When we used AHI-RRA as the gold standard for diagnosis of adolescent OSA, the sensitivity, specificity, accuracy, and LR+ and LR− of different AHI cutoffs by the WP200 were as follows: at cutoff of ≥ 5, AHI by WP200 had sensitivity of 100%, specificity of 96%, and accuracy of 97% (LR+ 26.00, LR− 0.00); at cutoff of ≥ 15, sensitivity of 80%, specificity of 100%, and accuracy of 97% (LR+ NA, LR− 0.20); and at cutoff of ≥ 30, sensitivity of 100%, specificity of 100%, and accuracy of 100% (LR+ NA, LR− 0.00).
Table 2.
Sensitivity, specificity, accuracy, LR+, and LR- of the Watch-PAT 200 with polysomnography in adolescents (n = 38).
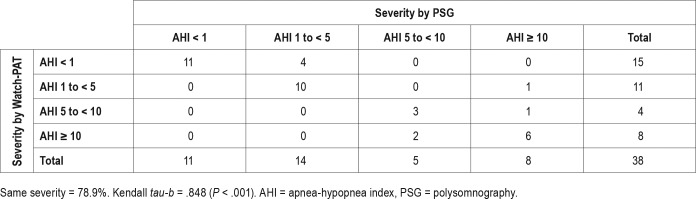
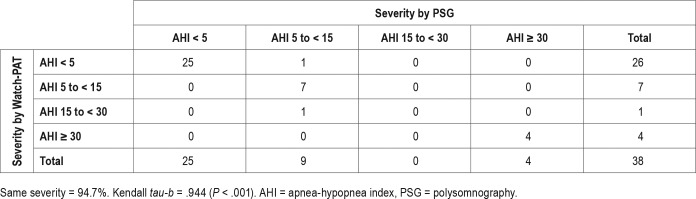
Concordance of AHI Severity
Table 3 and Table 4 show the concordance of AHI severity measured by the WP200 and PSG according to the RRC and RRA. We found significant high concordance in AHI severity between the WP200 and PSG according to the RRC (Kendall tau-b = .848, P < .001) and RRA (Kendall tau-b = .944, P < .001).
Table 3.
Concordance of AHI severity measured by the Watch-PAT 200 and PSG according to the respiratory rules for children in adolescents (n = 38).
Table 4.
Concordance of AHI severity measured by the Watch-PAT 200 and PSG according to the respiratory rules for adults in adolescents (n = 38).
DISCUSSION
The current study attempted to validate the WP200 for diagnosing OSA in adolescents against attended overnight PSG. In addition, we performed tests to determine optimal respiratory scoring rules for children and adults in the diagnosis of adolescent OSA using the WP200 because an individual sleep specialist can adopt RRC or RRA to score respiratory events in adolescents (13 to 17 years) at his or her discretion. The results of the study showed that the WP200 not only had significant concordances of AHI severity but also high correlation and good agreement in AHI and mSaO2 compared with in-laboratory PSG based on both respiratory rules. To the best of our knowledge, this is the first study to determine the reliability and clinical efficacy of the WP200 to diagnose OSA compared with PSG in adolescents according to the RRC and RRA.
Since the Watch-PAT wrist-worn device using peripheral arterial tone measurements was developed in the late 1990s, there has been much clinical research to assess the accuracy and feasibility of the Watch-PAT for identifying OSA.9–14 Yalamanchali et al.16 performed a review and meta-analysis of 14 clinical papers to estimate the correlation in respiratory parameters such as AHI between full PSG and the Watch-PAT. They detected a relatively high degree of correlation in respiratory parameters between PSG and Watch-PAT and concluded that the latter device provides valuable data for adequate diagnosis of OSA in adults. To identify the effects of older age and aging on the diagnostic precision of the Watch-PAT, Onder et al.17 analyzed sleep and respiratory variables including AHI between younger (age ranges 20 to 35 years, n = 27) and older (age ranges 50 to 65 years, n = 29) adults. They found that there was high correlation and good agreement in AHI in each group between standard PSG and the Watch-PAT and demonstrated that older age did not exert negative effects on the diagnostic accuracy of the Watch-PAT.
Although the Watch-PAT has some benefits including easy-to-use, automatic analysis of data, few adverse effects, low discomfort, and lower cost against in-laboratory PSG, it has a few clinical restrictions for use. For example, Watch-PAT is not indicated for a number of conditions such as use of several medications (eg, alpha blockers, short-acting nitrates, etc.), permanent pacemaker, sustained nonsinus cardiac arrhythmias, and age younger than 17 years. Considering the operating principle of a wrist-worn device using peripheral arterial tone measurements, most clinical limitations for application except age restrictions are easy to understand. In brief, the operating mechanism of the Watch-PAT related to identifying sleep-disordered breathing such as apnea and hypopnea is as follows: (1) abruptly elevated sympathetic activation by the termination of respiratory events causes digital arterial vasoconstriction; (2) peripheral arterial vasoconstriction by mediated alpha-receptors leads to decreased PAT signal amplitude; and (3) attenuated PAT signal amplitude, reduced oxygen saturation, elevated pulse rate, and actigraphy are used to conduct comprehensive analysis by the automatic computerized algorithm for sleep reports including AHI.9 However, it is thought that age limitations for use may be associated with the absence or deficiency of validation or feasibility studies in childhood and adolescence. The results of this study support the evidence that the WP200 may be useful for detecting respiratory disturbances such as sleep apnea and hypopnea and helpful for diagnosing OSA appropriately in adolescents.
Childhood OSA has several distinct differences from adulthood OSA such as clinical manifestations (eg, adenotonsillar hypertrophy, uncommon daytime sleepiness, etc.) and PSG findings (eg, respiratory events mainly occurred during rapid eye movement sleep, well-preserved slow-wave sleep, etc.).18 On the contrary, adult OSA has some clinical features (eg, obesity, small adenoid and tonsils, common daytime sleepiness, etc.) and PSG findings (eg, respiratory events regardless of sleep stages in most moderate to severe cases, disturbed slow-wave sleep, etc.) compared with children with OSA.18 Adolescence can be defined as the transitional period between childhood and adulthood in the human growth process. Similarly, it is presumed that adolescent OSA exhibits clinical and PSG characteristics of both childhood and adulthood OSA. However, there is still a lack of information on adolescent OSA regardless of fields such as clinical features, diagnoses, or treatment. To evaluate the anatomical or structural risk factors for OSA in adolescents, Schwab et al.19 used magnetic resonance imaging to compare three groups of adolescents: (1) teens with obesity and OSA (n = 49); (2) teens with obesity in a control group (n = 38); and (3) lean teens in a control group (n = 50). The authors reported a number of main outcomes as follows: (1) adolescents with obesity and OSA had enlarged adenoids and tonsils compared with other groups; (2) adolescents with obesity and OSA had narrower nasopharyngeal airways than other groups; and (3) there were no differences in the volume of other upper airway soft tissue anatomies between adolescents with obesity and OSA and the control group with obesity.19 To elucidate the differences in adolescents between RRC and RRA, Tapia et al.20 measured respiratory disturbances in asymptomatic adolescents (age range 13 to 18 years, n = 32) according to the RRC and RRA. They concluded that there was no clinical rationale for scoring respiratory disturbances with RRC or RRA in adolescents, although AHI (median = 0 [0–0.9] events/h) scored by RRC was significantly different from AHI (median = 0 [0–0.5] events/h) scored by RRA (P = .043).20 Accardo et al. investigated the differences between RRC and RRA (hypopnea rule A, defined by ≥ 4% desaturation, and B, defined by ≥ 3% desaturation or arousal) in adolescents referred for OSA. There was a signifi-cant concordance in OSA classification comparing RRC and RRA (hypopnea rule B) whereas a significant discordance in classification was observed comparing RRC and RRA (hypopnea rule A). They found that either RRC or RRA (hypopnea rule B) can be applied for adolescents with suspected OSA.21
This study has several limitations. First, there were relative few study participants. In the study, WP200 had a relatively high sensitivity and specificity at different cutoffs of the AHI regardless of scoring criteria. However, the sensitivity at cutoff ≥ 10 of the AHI-RRC was 75% (6/8). Only 2 of 8 adolescents in whom OSA was diagnosed (AHI ≥ 10) by the PSG had less than 10 of the AHI by the WP. Further study needs to be carried out in a large number of participants. Second, the WP200 does not provide sleep apnea results that distinguish it as central, obstructive, or mixed type. In this study, no adolescents received a diagnosis of central sleep apnea syndrome. Third, there is a possibility of failure during the WP200 testing. The failure rate of WP200 was 2.6% (1/39) in the study. One adolescent complained of finger pain during the testing, and the examination could not proceed any further. We could find no cause in the other adolescent. Fourth, overnight PSG did not include monitoring of CO2 in this study. Currently, CO2 monitoring is recommended for the detection of pediatric obstructive hypoventilation. However, WP200 cannot monitor CO2 levels natively. Therefore, CO2 levels were not measured in the study and our results of the validation of WP200 did not contain any data related with pediatric obstructive hypoventilation. These inherent limitations should be considered before using the WP200. Fifth, WP200 was not tested in the home environment where it is intended to be used. Future clinical researches are required considering these limitations.
CONCLUSIONS
In adolescents, the WP200 not only has significant concordances in AHI severity but also high correlation and good agreement in AHI and mSaO2 compared with attended in-laboratory PSG according to the RRC and RRA. The WP200 may be a clinically accurate diagnostic method for OSA in adolescents whether we used the respiratory scoring rules for children or adults. Additional WP200 feasibility studies are needed with more adolescents.
DISCLOSURE STATEMENT
This study was supported by a grant of the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HC15C3415). The authors report no conflicts of interest.
ABBREVIATIONS
- WP200
Watch-PAT 200
- OSA
obstructive sleep apnea
- PSG
polysomnography
- AHI
apnea-hypopnea index
- RRC
respiratory rules for children
- RRA
respiratory rules for adults
- mSaO2
minimum arterial oxygen saturation
REFERENCES
- 1.American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 2.Strollo PJ, Jr., Rogers RM. Obstructive sleep apnea. N Engl J Med. 1996;334(2):99–104. doi: 10.1056/NEJM199601113340207. [DOI] [PubMed] [Google Scholar]
- 3.Perfect MM, Archbold K, Goodwin JL, Levine-Donnerstein D, Quan SF. Risk of behavioral and adaptive functioning difficulties in youth with previous and current sleep disordered breathing. Sleep. 2013;36(4):517–525B. doi: 10.5665/sleep.2536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blechner M, Williamson AA. Consequences of obstructive sleep apnea in children. Curr Probl Pediatr Adolesc Health Care. 2016;46(1):19–26. doi: 10.1016/j.cppeds.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 5.Epstein LJ, Kristo D, Strollo PJ, Jr, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263–276. [PMC free article] [PubMed] [Google Scholar]
- 6.Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep. 1997;20(9):705–706. doi: 10.1093/sleep/20.9.705. [DOI] [PubMed] [Google Scholar]
- 7.Collop NA, Anderson WM, Boehlecke B, et al. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable Monitoring Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2007;3(7):737–747. [PMC free article] [PubMed] [Google Scholar]
- 8.Yuceege M, Firat H, Demir A, Ardic S. Reliability of the Watch-PAT 200 in detecting sleep apnea in highway bus drivers. J Clin Sleep Med. 2013;9(4):339–344. doi: 10.5664/jcsm.2584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schnall RP, Shlitner A, Sheffy J, Kedar R, Lavie P. Periodic, profound peripheral vasoconstriction--a new marker of obstructive sleep apnea. Sleep. 1999;22(7):939–946. [PubMed] [Google Scholar]
- 10.Bar A, Pillar G, Dvir I, Sheffy J, Schnall RP, Lavie P. Evaluation of a portable device based on peripheral arterial tone for unattended home sleep studies. Chest. 2003;123(3):695–703. doi: 10.1378/chest.123.3.695. [DOI] [PubMed] [Google Scholar]
- 11.Pittman SD, Ayas NT, MacDonald MM, Malhotra A, Fogel RB, White DP. Using a wrist-worn device based on peripheral arterial tonometry to diagnose obstructive sleep apnea: in-laboratory and ambulatory validation. Sleep. 2004;27(5):923–933. doi: 10.1093/sleep/27.5.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zou D, Grote L, Peker Y, Lindblad U, Hedner J. Validation a portable monitoring device for sleep apnea diagnosis in a population based cohort using synchronized home polysomnography. Sleep. 2006;29(3):367–374. doi: 10.1093/sleep/29.3.367. [DOI] [PubMed] [Google Scholar]
- 13.Pang KP, Gourin CG, Terris DJ. A comparison of polysomnography and the WatchPAT in the diagnosis of obstructive sleep apnea. Otolaryngol Head Neck Surg. 2007;137(4):665–668. doi: 10.1016/j.otohns.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 14.Choi JH, Kim EJ, Kim YS, et al. Validation study of portable device for the diagnosis of obstructive sleep apnea according to the new AASM scoring criteria: Watch-PAT 100. Acta Otolaryngol. 2010;130(7):838–843. doi: 10.3109/00016480903431139. [DOI] [PubMed] [Google Scholar]
- 15.Berry RB, Brooks R, Gamaldo CE, et al. for the American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Darien, IL: American Academy of Sleep Medicine; 2012. Version 2.0. [Google Scholar]
- 16.Yalamanchali S, Farajian V, Hamilton C, Pott TR, Samuelson CG, Friedman M. Diagnosis of obstructive sleep apnea by peripheral arterial tonometry: meta-analysis. JAMA Otolaryngol Head Neck Surg. 2013;139(12):1343–1350. doi: 10.1001/jamaoto.2013.5338. [DOI] [PubMed] [Google Scholar]
- 17.Onder NS, Akpinar ME, Yigit O, Gor AP. Watch peripheral arterial tonometry in the diagnosis of obstructive sleep apnea: influence of aging. Laryngoscope. 2012;122(6):1409–1414. doi: 10.1002/lary.23233. [DOI] [PubMed] [Google Scholar]
- 18.Choi JH, Kim EJ, Choi J, et al. Obstructive sleep apnea syndrome: a child is not just a small adult. Ann Otol Rhinol Laryngol. 2010;119(10):656–661. doi: 10.1177/000348941011901002. [DOI] [PubMed] [Google Scholar]
- 19.Schwab RJ, Kim C, Bagchi S, et al. Understanding the anatomic basis for obstructive sleep apnea syndrome in adolescents. Am J Respir Crit Care Med. 2015;191(11):1295–1309. doi: 10.1164/rccm.201501-0169OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tapia IE, Karamessinis L, Bandla P, et al. Polysomnographic values in children undergoing puberty: pediatric vs. adult respiratory rules in adolescents. Sleep. 2008;31(12):1737–1744. doi: 10.1093/sleep/31.12.1737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Accardo JA, Shults J, Leonard MB, Traylor J, Marcus CL. Differences in overnight polysomnography scores using the adult and pediatric criteria for respiratory events in adolescents. Sleep. 2010;33(10):1333–1339. doi: 10.1093/sleep/33.10.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]