Abstract
Background:
The European Union's Working Time Directive stipulates recovery periods as "Eleven consecutive hour daily rest periods (DRPs) between working days." In Japan, adopting this regulation has been discussed.
Objective:
To examine the association between weekday DRPs and recovery from fatigue by conducting a one-month observational study using a fatigue monitoring application (fatigue app) on a smart tablet.
Methods:
Fifty-five daytime employees working at an information technology company participated in this study. Visual analogue scales (VAS) regarding fatigue, psychological detachment from work, a psychomotor vigilance task (PVT), and sleep-wake logs were repeatedly measured using a fatigue app that we developed for this study. Sleep was measured by a wrist actigraph.
Results:
The average and SD of weekday DRPs was 13.1 ± 2.3 h. However, 54.5% of employees experienced less than the minimum 11-hour DRP at least once a month. Sleep duration was significantly changed with weekday DRPs, though no significant difference was found in sleep efficiency. Linear mixed effects models showed that sleep duration increased by approximately 15 minutes for each hour of weekday DRPs (β = 0.24, 95% CI; 0.17, 0.32, p <.001). VAS-measured fatigue and psychological detachment from work significantly improved as DRPs increased (β = −3.4, 95% CI; −4.7, −2.1, p <.001; β = 2.6, 95% CI; 1.2, 4.0, p <.001, respectively). However, PVT performance did not significantly change with weekday DRPs.
Conclusions:
Ensuring weekday DRPs plays an essential role in protecting the opportunities to sleep, with better recovery from fatigue and stress among information technology workers.
Keywords: Fatigue, Fatigue app, Overwork, Psychological detachment from work, Recovery, Sleep
Introduction
Long work hours are one of the crucial issues in Japan today. Approximately 300 Karoshi (i.e., death due to overwork) cases are compensated each year1). Consequently, there has been a great deal of interest in new work-time regulations for preventing excessive fatigue. The new regulation was inspired by the European Union's (EU) Working Time Directive, which mandates recovery periods as "11 consecutive hour daily rest periods (DRP) between working days." 2) In terms of fatigue recovery, the EU's working-time regulation would be more effective than Japan's in preventing overwork, because ensuring off-job time is very important for recovering from work-induced fatigue3). However, to our knowledge, evidence regarding the association between work-induced fatigue and appropriate recovery time is lacking for daytime workers, although data regarding shift workers has accumulated4-7). A previous systematic review suggested a link between quick-return to work (i.e., less than 11 hours between two shifts) and acute health problems (e.g., sleep, sleepiness, and fatigue), although the link with chronic health problems was not clear4).
To address these issues, we researched the associations between weekday DRPs and health parameters among information technology employees. Our previous findings suggest that insufficient weekday DRPs could be linked to higher blood pressure8) and a lower level of mental health9). Similarly, our latest study using an internet survey of 3,867 Japanese permanent employees found that a shorter weekday DRP was associated with deteriorations in sleep quantity and quality10). Thus, our data partially support a positive association between weekday DRPs and workers' health.
However, our previous studies have some limitations. First, those studies were conducted using either a cross-sectional study design9,10), or a limited number of observations during the study period8). Second, because weekday DRPs were mainly measured using a recall method (i.e., what time did you start or finish working in the previous month?), it was not possible to investigate the influences of day-to-day variations in weekday DRPs. Third, there was a lack of objectively measured data regarding the association between DRPs and fatigue recovery. To fill the gap, more research measuring objective outcomes (such as sleep actigraphy and neurobehavioral functions) for longer periods is needed. Because sleep plays an essential role in fatigue recovery11), objectively measured sleep would provide important insights for understanding the link between desirable weekday DRPs and fatigue recovery. Moreover, sleep studies are shifting from shorter to longer observation times to understand the links between sleep and fatigue recovery in real work-life settings. For instance, Åkerstedt et al. conducted an intensive longitudinal study across 42 days in order to understand day-to-day variations in sleepiness and their relationship to the period immediately preceding sleep12). Their findings suggested that daytime sleepiness could be determined by a short amount of sleep, poor sleep quality, and early rising.
However, an intensive longitudinal study design can often lead to gaps in data due to missing measurements, especially when using paper-based questionnaires. Therefore, to perform this study we designed a novel, tablet-based fatigue monitoring application (fatigue app) that can easily measure fatigue-related parameters. Our aim in this one-month observational study was to use this fatigue app to examine the association of weekday DRPs with fatigue recovery measured by carryover fatigue, psychological detachment from work, a psychomotor vigilance task (PVT), and sleep actigraphy. Furthermore, we aimed to investigate the effectiveness of using the fatigue app to detect DRP over a one-month observation period, compared with a pre-study questionnaire using the recall method8).
Methods
Participants
Sixty-eight daytime employees of an information technology company participated in this one-month observational study. Of these, 13 participants did not complete the study and their data were excluded. Thus, the data of 55 participants (26 females; mean age and SD 39.6 ± 6.3 yr) were analyzed in this study. The main characteristics of the 55 participants were as follows: mean self-reported daily working hours were 10.1 ± 1.6 h; mean one-way commute time was 51.5 ± 20.5 min; 60% (n = 33) were married; 18.2% (n = 10) had a common cold; 14.5% (n = 8) used medication (Table 1). All employees voluntarily participated in this study without a monetary reward. The Institutional Review Board of the National Institute of Occupational Safety and Health, Japan, reviewed and approved the study protocol (H26-1-02). All participants gave written informed consent.
Table 1.
Characteristics of the participants
| Mean (SD) or % (n) | |
|---|---|
| a The data were measured in the pre-study questionnaire and excluded a 1-hour break. | |
| n | 55 |
| Age (yr) | 39.6 (6.3) |
| Gender (% female) | 47.2 (26) |
| Year of continuous employment (yr) | 8.6 (5.5) |
| Marriage (%) | 60.0 (33) |
| Child/children 12 years of age or younger (%) | 32.7 (18) |
| One-way commuting time (min) | 51.5 (20.5) |
| Self-reported daily working hours (h) a | 10.1 (1.6) |
| Common cold during the study (%) | 18.2 (10) |
| Medication use during the study (%) | 14.5 (8) |
Study design
We adopted a one-month observational study design to measure day-to-day variations in fatigue-related parameters coupled with weekday DRPs. This study was conducted from October to December of 2015. Of the participants, 32 employees participated in the first period (October) and 23 employees participated in the second period (November to December). During their respective study periods, participants were required to wear sleep actigraphy monitors (Zzz-Logger; Ambulatory Monitoring Inc, Ardsley, New York) during sleep and to use a new tablet-based fatigue app that we designed (dynabook Tab S38/23M; TOSHIBA Co., Ltd., Tokyo) to measure fatigue-related parameters.
Measurements
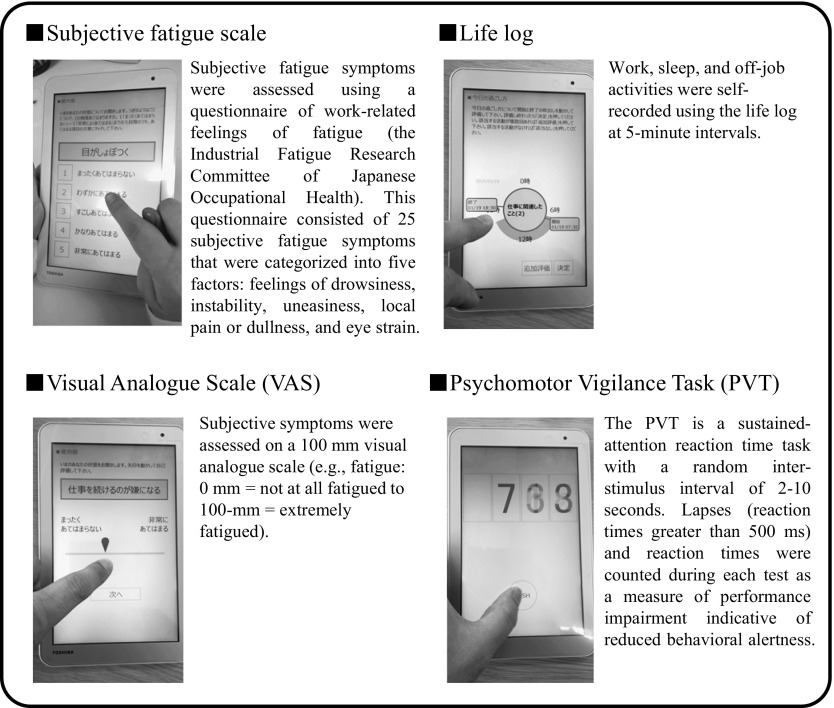
Fatigue app
As shown in Fig. 1, the novel fatigue app that we developed for this one-month observational study has functions that allow it to easily measure fatigue-related parameters. Likewise, the app can freely change the set of parameter's contents. For this study, we used a visual analogue scale (VAS), a 5-minute PVT, and daily DRP logs. Carry-over fatigue upon awakening ( "I carry-over work-induced fatigue"; 0 = not fatigued at all, 100 = extremely fatigued), and psychological detachment from work at bedtime ( "I do not think about work at all"; 0 = I think about work all the time, 100 = I do not think about work at all) were measured using the VAS method. PVT, which is a sustained-attention reaction time task, was set at 5-minutes duration with a random inter-stimulus interval of 2 to 10 seconds and measured upon waking using the app. Lapses (a response of longer than 500 ms) and reaction times were counted during each 5-minute test. Based on the daily log, weekday DRPs were calculated as the interval from the end to the start of working hours (including commute time). In this analysis, weekend DRP data were excluded because our research interest was the minimum 11-hour DRP set by the EU's standard. Additionally, we did not compare fatigue app-measured parameters with the paper-based VAS method and the original PVT test. However, given the relatively simple procedure for measuring those parameters, the data may be reliable regardless of the measurement method (i.e., paper-based or app-measured). However, testing the validity of the fatigue app using many users is an important next step. The app will be provided on our institutional website (https://www.jniosh.go.jp/).
Fig. 1.
Fatigue app
Sleep actigraphy
During the study period, sleep was measured by an actigraph unit secured to the participants' nondominant wrist. The epoch length was set at 1-minute intervals. Sleep duration and sleep efficiency (the percentage of time scored as sleep during the sleep period) were calculated to examine the quantity and quality of sleep using AW2 ver.2.6 (Ambulatory Monitoring Inc, Ardsley, New York).
Pre-study questionnaire
Participants were required to answer a questionnaire regarding their demographic data as well as their typical start and end work-times for the month preceding the study. Questionnaire-measured DRPs were calculated using this data and reported in our previous study8).
Data analysis
Weekday DRPs were categorized into five levels according to the day-to-day individual variation in DRPs: <11 hours (reference), <12 hours, <13 hours, <14 hours, and ≥14 hours. Linear mixed effects models were used to evaluate the association between weekday DRPs and our parameters. Categorized weekday DRPs were included as a fixed factor, whereas each participant was entered as a random factor, and covariates of age, gender, week (1, 2, 3, and 4 weeks), and day (from Monday to Sunday) were included. Based on the STROBE statements (especially No.11)13), the data of weekday DRPs were also set as continuous variables in addition to categorical variables. Then, the data were analyzed to examine the dose-response associations between weekday DRP per hour and the parameters. Statistical analyses were performed using Stata/CI 14.0 for Windows.
Results
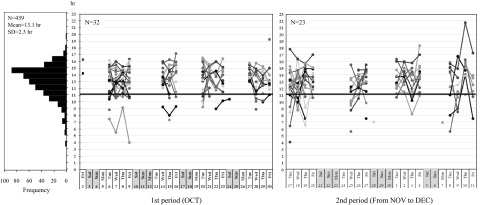
Day-to-day variations in DRPs during the one-month period
As shown in Fig. 2, data measured by the fatigue app reveal the individual day-to-day variations in weekday DRPs. The black line indicates the minimum 11-hour DRP which is set as the EU standard2). Because some employees worked during the weekends, their data were included in this analysis. The average and SD of weekday DRP data observed throughout this study period was 8.0 ± 4.1 days per participant. The maximum period of DRP data observation was 16 days per month. Thus, approximately 50% of the available data were obtained and analyzed in this study. The average and SD of DRPs was 13.1 ± 2.3 h, but 30 employees (54.5%) experienced less than the minimum 11-hour DRP at least once a month. Notably, a few employees had the shortest DRP, which was only 4 hours per day. Table 2 shows the difference between fatigue app-measured DRPs in this study and questionnaire-measured DRPs from our previous report8). Both studies observed the same employees, but one employee did not answer the questionnaire in the previous study. The average and SD of the DRPs were the same levels (12.8 ± 1.6 h vs. 13.1 ± 2.3 h). However, the percentage of employees who experienced less than the 11-hour DRP showed a large difference between the two studies (9% vs. 54.5%).
Fig. 2.
Day-to-day variations in the daily rest period (DRP) between working days during the one-month study periods. The vertical axis shows DRP length, while the horizontal axis shows the day of month. Each plotted line represents individual variations (55 participants) in DPRs. The bold horizontal line indicates the minimum 11-hour DRP length, which is set as an EU working directive standard. The histogram on the left shows the frequency of DRP lengths during the study (Total DRPs observed: N= 439).
Table 2.
The comparison of fatigue app-measured DRPs and questionnaire-measured DRPs at pre-study
| Daily rest period | |||
|---|---|---|---|
|
a The DRPs were based on the average start and end time of participant's workday for the previous month, and were reported by our previous paper (Ikeda et al. 2017) 8) b The data indicate that employees experienced less than the 11-hour DRP at least once a month. Note: Fatigue app data were based on 55 employees, while the questionnaire data was calculated from 54 employees because 1 employee did not answer the questionnaire. | |||
| Mean ± SD (h) | % of employees with <11 h DRP (n) | ||
| Pre-study questionnaire-measured DRPs a | 12.8 | 1.6 | 9% (5) |
| Fatigue app-measured DRPs during the one-month study period | 13.1 | 2.3 | 54.5% (30) b |
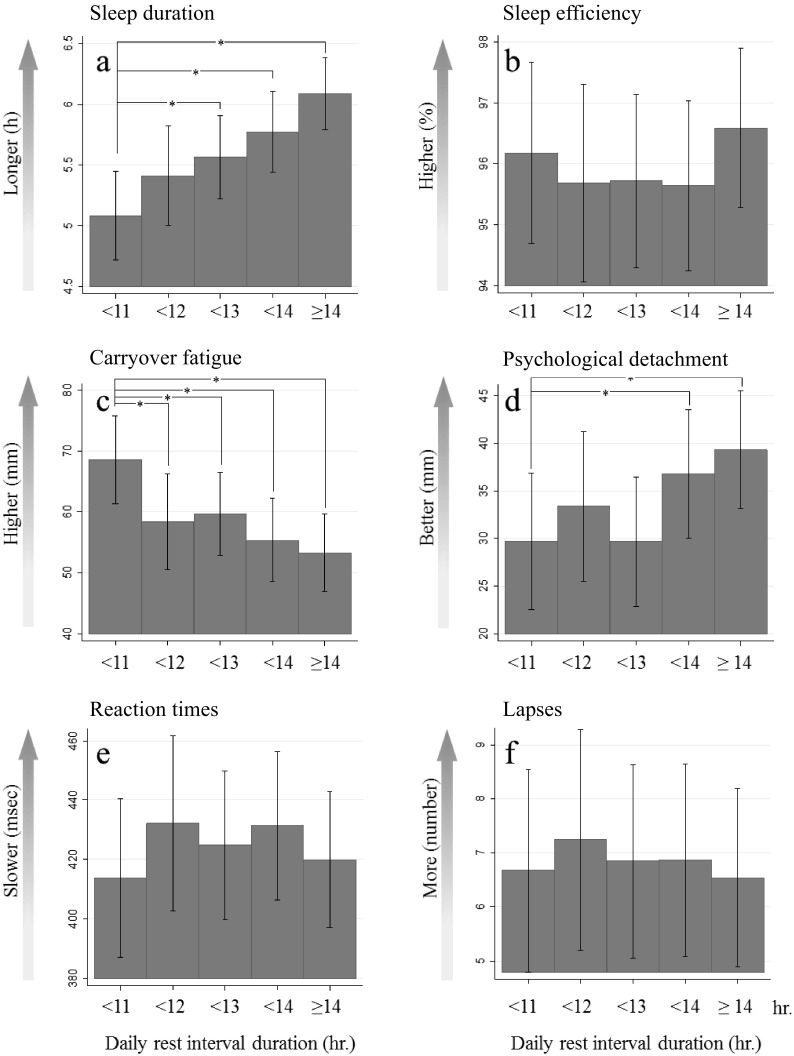
Weekday DRPs and the fatigue-related parameters
Fig. 3 and Table 3 show the relationship between weekday DRPs and the fatigue-related parameters. Actigraph data showed no significant difference in sleep efficiency, an indicator of sleep quality. However, sleep duration was significantly associated with DRPs, and an association between shorter weekday DRPs and shorter sleep duration was observed (Fig. 3A, B).
Fig. 3.
The effect of DRP length on sleep and fatigue-related parameters. Actigraphically measured sleep duration (a), efficiency (b), carryover fatigue (c), psychological detachment from work (d), and PVT performance (e, f), according to the length of DRPs between working days. Data represent estimated marginal mean and 95% CI. Covariates [age, gender, week, day]. * p < .005
Table 3.
Results from linear mixed effects models predicting parameters
| Weekday DRP length as categorical variable | Weekday DRP length as continuous variable | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| DRP | β | 95%CI | P | DRP | β | 95%CI | P | ||||
| DRP: daily rest period , 95%CI: 95 confidence interval; Weekly DRP length was included as a fixed factor, while participant was entered as a random factor, and covariates of age, gender, week, and day were included. β represents the regression coefficient for the fixed effect model and the coefficents in bold show the significant difference level. | |||||||||||
| Sleep duration (h) | < 11h | (reference) | DRP (h) | 0.24 | 0.17 | 0.32 | 0.000 | ||||
| < 12h | 0.33 | -0.08 | 0.74 | 0.119 | |||||||
| < 13h | 0.48 | 0.12 | 0.84 | 0.009 | |||||||
| < 14h | 0.69 | 0.33 | 1.05 | 0.000 | |||||||
| ≥ 14h | 1.01 | 0.67 | 1.35 | 0.000 | |||||||
| Sleep efficiency (%) | < 11h | (reference) | DRP (h) | 0.1 | -0.1 | 0.4 | 0.353 | ||||
| < 12h | -0.49 | -1.90 | 0.92 | 0.494 | |||||||
| < 13h | -0.46 | -1.69 | 0.78 | 0.470 | |||||||
| < 14h | -0.53 | -1.78 | 0.71 | 0.401 | |||||||
| ≥ 14h | 0.41 | -0.76 | 1.58 | 0.490 | |||||||
| Carry-over fatigue (0-100 mm) | < 11h | (reference) | DRP (h) | -3.4 | -4.7 | -2.1 | 0.000 | ||||
| < 12h | -10.2 | -17.1 | -3.2 | 0.004 | |||||||
| < 13h | -8.9 | -14.9 | -2.9 | 0.004 | |||||||
| < 14h | -13.2 | -19.3 | -7.1 | 0.000 | |||||||
| ≥ 14h | -15.2 | -20.9 | -9.6 | 0.000 | |||||||
| Psychological detachment from work (0-100 mm) | < 11h | (reference) | DRP (h) | 2.6 | 1.2 | 4.0 | 0.000 | ||||
| < 12h | 3.7 | -3.7 | 11.0 | 0.326 | |||||||
| < 13h | 0.0 | -6.4 | 6.3 | 0.995 | |||||||
| < 14h | 7.1 | 0.6 | 13.5 | 0.031 | |||||||
| ≥ 14h | 9.6 | 3.6 | 15.6 | 0.002 | |||||||
| PVT reaction times (msec) | < 11h | (reference) | DRP (h) | 0.8 | -4.8 | 6.3 | 0.790 | ||||
| < 12h | 18.3 | -10.6 | 47.3 | 0.214 | |||||||
| < 13h | 11.0 | -14.2 | 36.2 | 0.394 | |||||||
| < 14h | 17.5 | -8.0 | 43.1 | 0.178 | |||||||
| ≥ 14h | 6.1 | -18.0 | 30.1 | 0.621 | |||||||
| PVT lapses (number) | < 11h | (reference) | DRP (h) | -0.1 | -0.4 | 0.3 | 0.696 | ||||
| < 12h | 0.57 | -1.29 | 2.42 | 0.549 | |||||||
| < 13h | 0.18 | -1.44 | 1.79 | 0.832 | |||||||
| < 14h | 0.20 | -1.44 | 1.84 | 0.813 | |||||||
| ≥ 14h | -0.14 | -1.69 | 1.41 | 0.862 | |||||||
Compared with the less than 11-hour DRPs (reference), sleep duration (h) significantly increased in <13-hour DRPs (β = 0.48 [95% confidence interval (CI); 0.12, 0.84], p =.009), <14-hour DRPs (β = 0.69 [95% CI; 0.33, 1.05], p <.001), and ≥14-hour DRPs (β = 1.01 [95% CI; 0.67, 1.35], p <.001), while no significant difference was found in <12-hour DRPs (β = 0.33 [95% CI; −0.08, 0.74], p =.119). When the data from weekday DRPs were set as the continuous variable, the linear mixed effects models showed that sleep duration increased by approximately 15 minutes for each 1 hour of the DRP (β = 0.24 [95% CI; 0.17, 0.32], p<.001).
A similar association was found in subjective fatigue parameters (Fig. 3C and 3D), which also showed significant differences among DRPs. Carryover fatigue measured by a VAS (mm) significantly decreased in all DRPs relative to the reference, <12-hour DRPs (β = −10.2 [95% CI; −17.1, −3.2], p =.004), <13-hour DRPs (β = −8.9 [95% CI; −14.9, −2.9], p =.004), <14-hour DRPs (β = −13.2 [95% CI; −19.3, −7.1], p <.001), and ≥14-hour DRPs (β = 15.2 [95% CI; −20.9, −9.6], p <.001). On the other hand, psychological detachment from work (mm) significantly increased in <14-hour DRPs (β = 7.1 [95% CI; 0.6, 13.5], p =.031) and ≥14-hour DRPs (β = 9.6 [95% CI; 3.6, 15.6], p =.002) compared to the reference, while there was no significant difference in other DRPs. Additionally, the linear mixed effects models (with DRPs as the continuous variable) showed that carryover fatigue due to work decreased by about 3 mm for each 1 hour of DRP (β = −3.4 [95% CI; −4.7, −2.1]), while psychological detachment from work increased by about 2.6 mm for each 1 hour of DRP (β = 2.6 [95% CI; 1.2, 4.0]).
In contrast, PVT performance did not significantly change with DRP (Fig. 3E and 3F).
Discussion
To our knowledge, this is the first study describing day-to-day individual variations in weekday DRPs during a one-month period among information technology workers. As shown in Fig. 2, the average weekday DRP length was 13.1 hours per day. However, 54.5% of employees experienced less than the minimum 11-hour DRP (the EU's working directive standard) at least once a month. In our previous study based on the recall method, only 9% of employees met the minimum 11-hour DRP8). The large difference relates to the methodology. DRPs reported by Ikeda et al. (2017)8) were calculated using a questionnaire about employees' usual working time preceding the study. However, this study measured day-to-day variations in DRPs during the one-month period using the fatigue app. Our data showed that the methodology of this one-month observation study has the benefit of detecting the impact of working times on fatigue at work, compared with previous studies based on the recall method, which may underestimate the relationship. However, fatigue app-measured DRPs were based on self-reported data, even though participants continuously recorded their DRPs throughout this study period. In Finland, a series of studies using payroll data has been conducted to examine objective working hours and health outcomes14,15), and more research using objective working hour data, such as payroll data, is essential for investigating the links between working hours and health at work.
Although employees who repeatedly underwent the minimum 11-hour DRP during this study were not observed, the shortest length of weekday DRP was surprisingly only 4 hours per day. In Japan, the standard for Karoshi (death due to overwork) compensation is set as more than 100 overtime working hours in the previous month, or 80 overtime hours per month for the past 2 to 6 months1). In other words, the overtime working hours could be the same level as the Karoshi standard, even if the minimum 11-hour DRP was continuously repeated for the past one month. In this study, the average weekday DRPs would not be problematic from the perspective of health at work, but care should be taken when examining the individual day-to-day variations in weekday DRPs.
Regarding objectively measured sleep, our data showed that a shorter DRP was significantly associated with shorter sleep duration. This result is in line with the latest findings of Ikeda et al. (2017)10). However, that study showed that sleep duration was approximately 6 hours per night (5.8 hours) under the minimum 11-hour DRP, while our data indicates sleep duration of around 5 hours per night (5.1 hours) in the same conditions. The discrepancy could be related to the difference between subjective and objective assessments of sleep. According to an earlier epidemiologic study, actigraphically measured sleep was 6.1 hours, and subjectively reported sleep was 6.8 hours16). Thus, our finding regarding sleep duration is reliable. A previous study suggested that sleep duration of less than 5 hours per night can be linked to a greater risk of disease17). Furthermore, links have been suggested between shorter sleep duration and deteriorated alertness and performance18), and a decreased ability to recognize others' facial emotions19). Therefore, this study suggests that ensuring the length of weekday DRPs is important to preventing poor recovery due to lack of sleep.
Likewise, subjective assessments of carryover fatigue and psychological detachment from work also significantly deteriorate with shortened sleep duration. Because sleep is essential for recovering from fatigue and stress among workers11), these findings reinforce the importance of ensuring DRPs in order to recover from work. Perhaps more important is investigating the quality of DRP by exploring proactive ways that individuals spend their off-job time to enhance fatigue recovery, as some Japanese employees may not appropriately take advantage of their leisure time to recover from work, even if they have sufficient DRPs. Therefore, more intervention studies would be valuable for examining the positive influences of employees' leisure crafting, which is defined as the proactive pursuit of leisure activities that target goal-setting, human connection, learning, and personal development20).
No significant difference was obtained in objectively measured sleep quality (i.e., sleep efficiency). The sleep duration observed in this study was relatively short regardless of weekday DRPs, with sleep duration measured at less than 6 hours per night even when participants had 14-hour DRPs (Fig. 3A). Basically, sleep efficiency tends to be higher as sleep duration shortens, which could explain why this study did not show an association between weekday DRPs and sleep efficiency. In contrast, our previous study using a questionnaire showed that shorter weekday DRPs were associated with deteriorated sleep quality measured by the Pittsburgh Sleep Quality Index (PSQI)21). This discrepancy in sleep quality may be associated with a difference in parameter characteristics. The PSQI measures many aspects of sleep (including sleep quality, sleep duration, use of sleep-inducing medication, daytime dysfunction, etc.), while the actigraphically measured sleep efficiency is defined as the percent of time scored as sleep during the sleep period. Thus, the sleep efficiency metric used here is different than our previous study.
In this study, PVT performance did not show any significant differences when coupled with weekday DRPs. There could be at least two explanations for this. We could assume that weekday DRPs do not affect PVT performance upon waking; however, this assumption is not in line with accumulated evidence showing that PVT performance deteriorates as sleep duration shortens18). Given that this study found a significant association between weekday DRPs and sleep duration, our data should have been consistent with previous findings. The other possibility is related to the validity of the PVT performance test in real-world settings. The variability of PVT data was larger than other parameters, as seen in the error bars in Figure 3E, 3F (95% CI). It is likely that demanding that the participants perform 5-minute PVT tests every day could be a heavy burden. In addition, the participants were not observed by researchers when conducting the test. A previous study examined the validity of a 3-minute smartphone-based PVT test against a 5-minute laptop-based PVT test22). Further investigations are necessary to determine how the PVT performance test is appropriately conducted in real settings without an observer. Comparing the original PVT test and the fatigue app-based PVT test is also important to test the validity of the fatigue app. Moreover, we did not measure the light conditions during daytime or during PVT testing. A previous study suggested an effect of daytime exposure to bright light on PVT performance23). Light settings during PVT testing could also affect PVT performance24). Thus, controlling light conditions throughout the study would be preferable in future work.
The primary strength of this study is that it was based on data measuring day-to-day individual variations in weekday DRPs during the one-month period. The previous study adopted the recall method8,10) (i.e., what time did you start or finish working in the previous month?), potentially missing the influences of day-to-day weekday DRP variations on outcomes. As expected, our findings support the use of a one-month observational study compared to a questionnaire-based study (shown in Table 2). Thus, this study provides essential insights into understanding the characteristics of weekday DRP variations. Furthermore, it should be noted that showing the associations between weekday DRPs and objectively measured sleep duration in this study is meaningful in reinforcing the importance of ensuring weekday DRPs through sleep duration on protecting workers' health. In terms of methodology, the fatigue app we designed could provide more available data than paper-based questionnaires when conducting a longitudinal intensive study. Developing an original app that is suitable for various study designs would thus be necessary to performing this type of study.
Meanwhile, some limitations of this study should be addressed. First, the generalizability of these findings is limited due to the single occupation of participants as information technology workers. Further study of other occupations is required to examine the associations of weekday DRPs with fatigue recovery. Also, because commuting time varies between rural and urban areas, employees who live in urban areas may not sufficiently take advantage of DRP to recover from fatigue compared to their counterparts. Thus, examining the influence of commuting time is also important for optimizing the DRP system in Japan. Furthermore, given that the half of the participants were female, our data could be affected by the menstrual cycle. However, these influences could be controlled by adjusting gender as a covariate. Second, only about 50% (about 8 days per participant) of the potentially available DRP data was reported by the participants in this study, while the maximum period of DRP data observation was 16 days per month. This study's design required the participants to repeatedly conduct the fatigue app test during a one-month period; and we did not have any contact with the participants, who voluntarily participated without any incentives. Those factors might lead to the observed collection rate. More data could be likely collected if procedures such as sending a reminder during the study were used. However, given the situation, the observed 50% of DRP data is not particularly low. Third, the one-month observation period used in this study is relatively longer and more intensive in order to better investigate the links between working hours and fatigue at work. This design is beneficial for precisely detecting short-term effects of fatigue; however, it cannot examine the long-term effects of fatigue on health, such as absenteeism, sleep problems, and health disorders. Thus, selecting the appropriate study period and methodology is important for studying the effects of working hours on health. Fourth, this study did not examine weekend DRPs, because the minimum 11-hour DRP was our primary interest. However, the way individuals spend their weekends25,26) is closely linked to recovery from work. Further investigations are needed to examine the relationship between weekend DRPs and fatigue recovery. Fifth, our data did not fully examine the differences of sleep quality coupled with weekday DRPs. It is possible that sleep architecture might change due to psychological stress, regardless of sleep duration. More studies using polysomnography in real settings are necessary to relationship between sleep quality and weekday DRPs. Finally, information and communication technology (ICT) allows employees to easily work outside their workplace (e.g., business e-mail after working hours), even when complying fully with the minimum 11-hour weekday DRPs. Given that the right to disconnect from work was introduced in France in 2017 (NOR: ETSX1604461L27)), it will be significant to reveal how flexible work using ICT has advantages and disadvantages for health at work in further investigations.
Conclusions
This study suggests an association between weekday DRPs and longer sleep duration with better work recovery among information technology workers by using a one-month observation method. Notably, given that ensuring DRPs was linked to increased objectively-measured sleep duration, our data provide essential insights and reinforce the importance of protecting suitable DRPs on workers' health. On the other hand, our data suggested that sleep duration was approximately 5 hours per night even under the 11-hour weekday DRPs. Because a short sleep period (less than 5 hours per night) is associated with greater risks of safety and health at work, protecting the 11-hour DRP (i.e., the EU standard) could be equal to the minimum necessary for protecting recovery opportunities from work-induced fatigue risks. However, more research with other occupations is important to better clarify suitable DRPs in relation to fatigue recovery.
Acknowledgments: This study was supported by the National Institute of Occupational Safety and Health, Japan (N-P26-01).
Conflicts of interest: None declared.
References
- 1). Yamauchi T, Yoshikawa T, Takamoto M, et al. Overwork-related disorders in Japan: recent trends and development of a national policy to promote preventive measures. Ind Health 2017; 55 (3): 293-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2). EUR-Lex. . Directive 2003/88/EC of the European parliament and of the council of 4 November 2003 concerning certain aspects of the organisation of working time. Official Journal of the European Union 2003; L299: 9-19. [Google Scholar]
- 3). Sonnentag S. Psychological detachment from work during leisure time: The benefits of mentally disengaging from work. Curr Dir Psychol Sci 2012; 21 (2): 114-118. [Google Scholar]
- 4). Vedaa Ø, Harris A, Bjorvatn B, et al. Systematic review of the relationship between quick returns in rotating shift work and health-related outcomes. Ergonomics 2016; 59 (1): 1-14. [DOI] [PubMed] [Google Scholar]
- 5). Vedaa Ø, Mørland E, Larsen M, et al. Sleep detriments associated with quick returns in rotating shift work: A diary study. J Occup Environ Med 2017; 59 (6): 522-527. [DOI] [PubMed] [Google Scholar]
- 6). Flo E, Pallesen S, Moen BE, et al. Short rest periods between work shifts predict sleep and health problems in nurses at 1-year follow-up. Occup Environ Med 2014; 71 (8): 555-561. [DOI] [PubMed] [Google Scholar]
- 7). Eldevik MF, Flo E, Moen BE, et al. Insomnia, excessive sleepiness, excessive fatigue, anxiety, depression and shift work disorder in nurses having less than 11 hours in-between shifts. PLoS One 2013; 8 (8): e70882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8). Ikeda H, Kubo T, Izawa S, et al. Impact of daily rest period on resting blood pressure and fatigue: A one-month observational study of daytime employees. J Occup Environ Med 2017; 59 (4): 397-401. [DOI] [PubMed] [Google Scholar]
- 9). Tsuchiya M, Takahashi M, Miki K, et al. Cross-sectional associations between daily rest periods during weekdays and psychological distress, non-restorative sleep, fatigue, and work performance among information technology workers. Ind Health 2017; 55 (2): 173-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10). Ikeda H, Kubo T, Sasaki T, et al. Cross-sectional Internet-based survey of Japanese permanent daytime workers' sleep and daily rest periods. J Occup Health 2018; 60 (3): 229-235. (doi: 10.1539/joh.17-0165-OA). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11). Akerstedt T, Nilsson PM, Kecklund G. Sleep and recovery. In: Sonnentag S, Perrewe PL, Ganster DC, editors. Current Perspectives on Job-Stress Recovery. Bingley, UK: JAI Press; 2009. p. 205-247. [Google Scholar]
- 12). Akerstedt T, Axelsson J, Lekander M, et al. The daily variation in sleepiness and its relation to the preceding sleep episode--a prospective study across 42 days of normal living. J Sleep Res 2013; 22 (3): 258-265. [DOI] [PubMed] [Google Scholar]
- 13). Vandenbroucke JP, von Elm E, Altman DG, et al. ; STROBE Initiative.. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Epidemiology 2007; 18 (6): 805-835. [DOI] [PubMed] [Google Scholar]
- 14). Karhula K, Koskinen A, Ojajärvi A, et al. Are changes in objective working hour characteristics associated with changes in work-life conflict among hospital employees working shifts? A 7-year follow-up. Occup Environ Med 2018; 75 (6): 407-411. (doi: 10.1136/oemed-2017-104785). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15). Härmä M, Ropponen A, Hakola T, et al. Developing register-based measures for assessment of working time patterns for epidemiologic studies. Scand J Work Environ Health 2015; 41 (3): 268-279. [DOI] [PubMed] [Google Scholar]
- 16). Lauderdale DS, Knutson KL, Yan LL, et al. Self-reported and measured sleep duration: how similar are they? Epidemiology 2008; 19 (6): 838-845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17). Cappuccio FP, D'Elia L, Strazzullo P, et al. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep 2010; 33 (5): 585-592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18). Van Dongen HP, Maislin G, Mullington JM, et al. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep 2003; 26 (2): 117-126. [DOI] [PubMed] [Google Scholar]
- 19). van der Helm E, Gujar N, Walker MP. Sleep deprivation impairs the accurate recognition of human emotions. Sleep 2010; 33 (3): 335-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20). Petrou P, Bakker AB. Crafting one's leisure time in response to high job strain. Human relations 2016; 69 (2): 507-529. [Google Scholar]
- 21). Doi Y, Minowa M, Uchiyama M, et al. Psychometric assessment of subjective sleep quality using the japanese version of the pittsburgh sleep quality index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res 2000; 97 (2-3): 165-172. [DOI] [PubMed] [Google Scholar]
- 22). Grant DA, Honn KA, Layton ME, et al. 3-minute smartphone-based and tablet-based psychomotor vigilance tests for the assessment of reduced alertness due to sleep deprivation. Behav Res Methods 2017; 49 (3): 1020-1029. [DOI] [PubMed] [Google Scholar]
- 23). Phipps-Nelson J, Redman JR, Dijk DJ, et al. Daytime exposure to bright light, as compared to dim light, decreases sleepiness and improves psychomotor vigilance performance. Sleep 2003; 26 (6): 695-700. [DOI] [PubMed] [Google Scholar]
- 24). Phipps-Nelson J, Redman JR, Schlangen LJ, et al. Blue light exposure reduces objective measures of sleepiness during prolonged nighttime performance testing. Chronobiology International 2009; 26 (5): 891-912. [DOI] [PubMed] [Google Scholar]
- 25). Weigelt O, Syrek CJ. Ovsiankina's great relief: How supplemental work during the weekend may contribute to recovery in the face of unfinished tasks. Int J Environ Res Public Health 2017; 14 (12): 1606. (doi: 10.3390/ijerph14121606). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26). Binnewies C, Sonnentag S, Mojza EJ. Recovery during the weekend and fluctuations in weekly job performance: a week-level study examining intra-individual relationships. J Occup Organ Psychol 2010; 83 (2): 419-441. [Google Scholar]
- 27). Article 55 under chapter II "Adapting the labour law to the digital age" (Adaptation du droit du travail à l'ère du numérique). [Online]. 2017[cited 2018 Apr. 4]; Available from: URL: https://www.legifrance.gouv.fr/eli/loi/2016/8/8/ETSX1604461L/jo#JORFSCTA000032983228