Abstract
Double strand breaks induced by genotoxic agents, if inappropriately repaired, will cause cell death or induce cancer. Poly(ADP-ribose) polymerase-3 (PARP-3) serves a role in double strand break repair, and may be involved in tumorigenesis. To the best of our knowledge, the role of PARP-3 in breast cancer has not yet been examined. In the present study, the expression of PARP-3 was investigated in 493 breast cancer samples and 54 tumor-adjacent control samples using tissue-microarray-based immunohistochemistry. PARP-3 expression was higher in breast cancer samples compared with control samples. PARP-3 overexpression was significantly associated with histological grade II–III (P=0.012). In addition, PARP-3 overexpression was significantly associated with shorter disease-free survival (DFS; P=0.027) time and exhibited a tendency toward shorter overall survival (OS; P=0.183) time in patients with breast cancer compared with patients with lower PARP-3 expression, particularly in BRCA1-positive patients (P=0.004 for disease-free survival and P=0.095 for OS). Multivariate Cox regression analysis indicated that PARP-3 was an independent prognostic factor in patients with breast cancer. Furthermore, it was revealed that PARP-3 overexpression was associated with shorter survival time in patients with cyclophosphamide/doxorubicin or epirubicin/5-fluorouracil (CAF/CEF) chemotherapy compared with low PARP-3 expression, but not in patients with CAF/CEF + docetaxel chemotherapy. The present study suggested that PARP-3 may be used as a biomarker for predicting the clinical outcome of patients receiving chemotherapy, and targeting PARP-3 may be a potential therapeutic strategy for the treatment of breast cancer.
Keywords: breast cancer, poly(ADP-ribose) polymerase, breast cancer gene 1, chemotherapy, survival
Introduction
Breast cancer is a group of heterogeneous diseases with different clinical and histological forms (1). The molecular and clinical heterogeneity of breast cancer renders it necessary to identify biomarkers of clinical outcomes so that patients can be treated with the most appropriate chemotherapeutic protocols (2). Therefore, identification of biomarkers that will predict breast cancer to chemotherapeutic drugs is important for the future development of individualized treatment for patients with breast cancer.
Poly(ADP-ribose) polymerases (PARPs) constitute a family of enzymes that catalyze poly(ADP-ribosylation) of DNA-binding proteins and perform a key role in the regulation of transcription, genome stability, energy metabolism, tumorigenesis and cellular responses to DNA damage (3,4). The PARP superfamily is composed of 17 members, of which PARP-1, PARP-2 and PARP-3 are activated by DNA strand breaks and serve an important role in the repair of single strand breaks and/or double strand breaks (DSBs) (5–7). PARP-1, the most studied member of the PARP superfamily, has been reported to be overexpressed in numerous malignant tumors, including breast cancer, and is associated with invasiveness and poor clinical outcomes (8–13). In addition, it is well-known that the a combination of PARP inhibitors and DNA damaging chemotherapy, can increase tumor responses and improve the survival of triple-negative patients with breast cancer compared with chemotherapy alone (14). Most importantly, PARP inhibitors are particularly efficient against tumors with defects in DNA repair mechanisms, including tumors with breast cancer gene (BRCA) mutations (15,16).
Despite having similar functions in the regulation of cellular responses to DNA damage, PARP-3 exhibits structural and functional differences from PARP-1 (17). Although PARP-3 shares a conserved C-terminal region with PARP-1, it has a shorter N-terminal region than PARP-1. PARP-3 also exhibits different N-terminal functions, including DNA binding or DNA-dependent activation (18). In addition, it has been reported that knockdown of PARP3, but not PARP1, results in an increase in the production of DSB induced by ionizing radiation (19). However, unlike PARP-1, less is known about the role of PARP-3 in breast cancer. Bieche et al (20) reported that the mRNA expression of PARP-3 was under-expressed in 10.4% of patients with breast cancer and this PARP-3 under-expression was mutually exclusive with overexpression of PARP-1. To date, the protein expression of PARP-3 in patients with breast cancer has not yet been investigated. It remains to be determined whether the protein level of PARP-3 is consistent with its mRNA level in breast cancer.
In the present study, the expression of PARP-3 was investigated in 493 breast cancer samples and 54 tumor-adjacent control samples using immunohistochemistry. The present study aimed to analyze the association of PARP-3 expression with clinicopathological features, chemotherapeutic responses and prognosis of patients with breast cancer.
Patients and methods
Ethics statement
The present study was approved by the Medical Ethics Committee of China Medical University (Shenyang, China). Due to the retrospective nature of the study, the Medical Ethics Committee waived the requirement of written informed consents by the patients.
Patients
The present study included human breast tissues from 493 female patients with breast cancer, who underwent surgery at the First Affiliated Hospital of China Medical University between January 2005 and October 2010. A total of 54 samples adjacent to the tumors outside the cancer loci were collected as controls. The diagnosis of breast cancer was confirmed by pathological staining. Histological evaluation of 54 samples adjacent to tumors exhibited no histological tumor-associated features.
The average age of patients with breast cancer was 51.3±10.6 years (range, 20–82 years). The histological grade of the cancer was determined according to the World Health Organization grading system (21,22). The stage of the cancer was evaluated according to the tumor-node-metastasis (TNM) staging system (22). Clinicopathological data, including patient age, menopausal status, tumor size, lymph node metastasis, p53 status and BRCA1 status were retrospectively retrieved from medical records.
All patients did not undergo radiation therapy and chemotherapy prior to surgery. Following surgery, 291 patients received cyclophosphamide/doxorubicin or epirubicin/5-fluorouracil (CAF/CEF) and 95 patients received CAF/CEF and docetaxel (CAF/CEF and D). The remaining 107 patients received other chemotherapeutic regimens containing docetaxel or cisplatin alone or in combination.
Immunohistochemistry
Tissue sections (4 µm) were fixed with 4% formalin at room temperature for 48 h and paraffin-embedded tissue blocks for immunohistochemical staining. Sections were deparaffinized with xylene, rehydrated in a graded alcohol series of 100 and 95% (Sinopharm Chemical reagent Co., Ltd., Shanghei, China) at a concentration of 100, 95, 85, 75, 65% and H2O and sections were put into 3% citric acid-sodium citrate buffer (pH=6.0) and heated in a microwave oven at 100°C for 10 min to retrieve the antigen. Endogenous peroxidase activity was blocked by incubating the sections in 3% H2O2 at 37°C for 20 min. Sections were subsequently blocked to avoid nonspecific binding with 10% normal goat serum (Boster Biological Technology, Pleasanton, CA, USA) at 37°C for 30 min and incubated at 4°C overnight with the polyclonal antibody against PARP-3 (dilution, 1:100; cat. no. 96601; rabbit anti-human polyclonal antibodies; Abcam, Cambridge, UK), followed by incubation with biotinylated secondary antibodies (secondary antibody A in the kit-0305; dilution, 1:200; cat. no. kit-0305; Maxim Biotechnologies, Fuzhou, China) for 30 min at 37°C. Sections were then incubated with streptavidin horseradish peroxidase (secondary antibody B in the kit-0305; dilution, 1:200; cat. no. kit-0305; Maxim Biotechnologies) for an additional 20 min at 37°C and stained with 3,3-diaminobenzidine at room temperature for 1 min (dilution, 1:200; cat. no. LI-9032; OriGene Technologies, Inc, Beijing, China). Sections were counterstained with hematoxylin, dehydrated and mounted. For negative controls, the sections were not incubated with primary antibodies.
Evaluation of immunohistochemistry
The immunostained sections were examined under the light microscope (magnification, ×200; select 3 fields/view) by two pathologists blinded to the experimental conditions. The intensity of immunoreactivity was scored as follows: 0, no staining; 1, weak staining; 2, moderate staining and 3, strong staining. A percentage scoring system was used to assess the number of stained cells and the scores were assigned by using 5% increments as previously reported (23,24). The final scores were used to determine the cutoff value for discriminating tumors with the high expression of PARP-3 from tumors with the low expression, using receiver operating characteristic (ROC) curves. The sensitivity and specificity for the survival of patients with breast cancer was plotted to generate ROC curves.
Statistical analysis
Analyses were performed using SPSS 16.0 (SPSS, Inc., Chicago, IL, USA). Pearson's χ2 or Fisher's exact probability tests were used to evaluate the association between PARP-3 expression and clinicopathological characteristics of patients with breast cancer. Survival probabilities were estimated by the Kaplan-Meier method and assessed by a log-rank test. Univariate and multivariate Cox proportional hazards regression models were used for assessing the association between potential confounding variables and prognosis [overall survival (OS) or disease-free survival (DFS)]. OS was calculated as the time between the first day of diagnosis and disease-associated mortality or last known follow-up. The disease-free survival (DFS) was calculated as the time between the first day of diagnosis and the occurrence of local recurrence or distant metastasis. P<0.05 was considered to indicate a statistically significant difference.
Results
Clinicopathological characteristics of patients with breast cancer
Table I summarizes clinicopathological characteristics of 493 patients with breast cancer. Of the 493 patients, age, menopausal status, tumor size, tumor type, histological grade, TNM stage and lymph node metastasis were recorded in 493, 493, 493, 492, 492, 493 and 493 patients, respectively. The majority of these patients had a tumor with invasive ductal carcinoma (92.5%), <2 cm in size (65.9%), histological grade II (74.6%) or TNM stage I–II (73.8%). Lymph node metastasis occurred in 225 (45.6%) of 493 patients.
Table I.
Clinicopathological characteristics of patients with breast cancer.
| Parameters | Total, n | Patients, n (%) |
|---|---|---|
| Age at diagnosis | 493 | |
| ≤51 years | 279 (56.6) | |
| >51 years | 214 (43.4) | |
| Menopausal status | 493 | |
| Pre-menopause | 268 (54.4) | |
| Post-menopause | 225 (45.6) | |
| Tumor size | 493 | |
| ≤2.0 cm | 325 (65.9) | |
| >2.0, <5.0 cm | 146 (29.6) | |
| ≥5.0 cm | 22 (4.5) | |
| Tumor type | 492 | |
| Ductal carcinoma | 455 (92.5) | |
| Lobular carcinoma | 11 (2.2) | |
| Mucinous carcinoma | 9 (1.8) | |
| Others | 17 (3.5) | |
| Histological grade | 492 | |
| G1 | 83 (16.9) | |
| G2 | 367 (74.6) | |
| G3 | 42 (8.5) | |
| TNM stage | 493 | |
| I–II | 364 (73.8) | |
| III–IV | 129 (26.2) | |
| Lymph node metastasis | 493 | |
| No | 268 (54.4) | |
| Yes | 225 (45.6) | |
| p53 | 397 | |
| Negative | 166 (41.8) | |
| Positive | 231 (58.2) | |
| BRCA1 | 396 | |
| Negative | 102 (25.8) | |
| Positive | 294 (74.2) | |
| Chemotherapy regimen | 386 | |
| CAF/CEF | 291 (75.4) | |
| CAF/CEF+T | 95 (24.6) |
CAF/CEF, cyclophosphamide/doxorubicin or epirubicin/5-fluorouracil; CAF/CEF + T, CAF/CEF+ docetaxel; TNM, tumor-node-metastasis; BRCA1, breast cancer susceptibility gene 1.
Follow-up information was available for 493 patients with breast cancer. During the follow-up period of 9–118 months, relapses occurred in 85 cases and cancer-associated mortalities were identified in 55 cases. The 5-year survival rate was 88.0%. The mean OS and DFS times were 66.3 and 63.7 months, respectively.
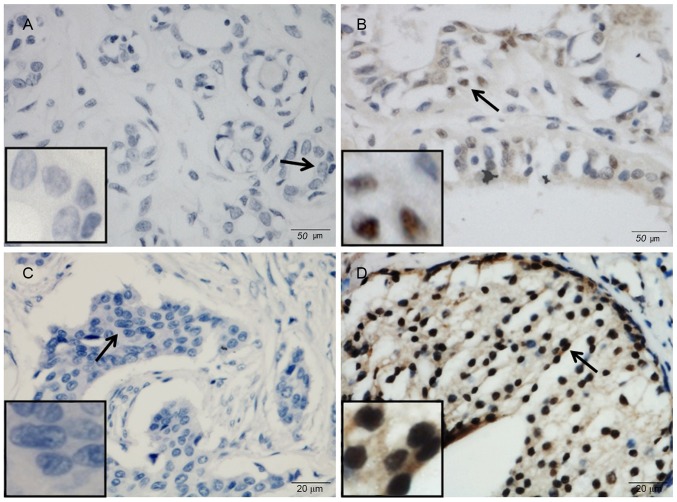
PARP-3 overexpression in breast cancer
The expression of PARP-3 was studied in 493 breast cancer samples and 54 tumor-adjacent control samples using immunohistochemistry (Fig. 1). PARP-3 was mainly expressed in the nucleus. Nuclear expression of PARP-3 was observed in 234 (47.5%) of 493 breast cancer samples and 9 (16.7%) of 54 control samples. PARP-3 immunoreactivity occurred significantly more frequently in breast cancer samples compared with control samples (P<0.001).
Figure 1.
Representative micrographs showing (A and C) negative and (B and D) positive immunohistochemical staining of poly(ADP-ribose) polymerase-3 in (A and B) tumor-adjacent tissues and (C and D) breast cancer tissues. Arrows indicate the magnified regions in the insert. Magnification, ×400. Scale bar, 50 µm.
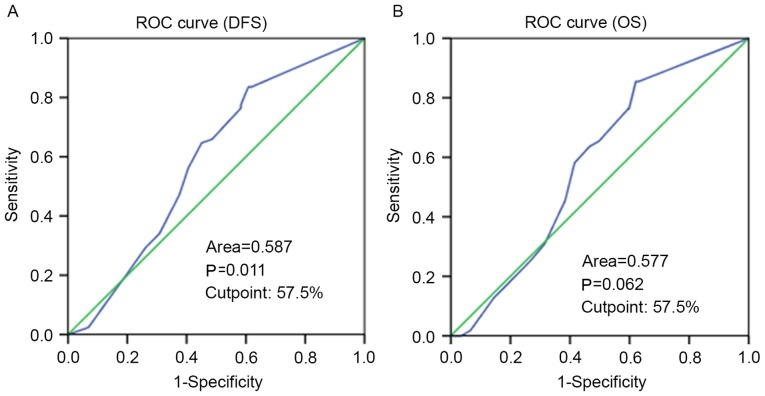
Selection of the cutoff value for PARP-3 expression
ROC curve analysis was performed to determine an optimal cutoff score for PARP-3 expression in breast cancer samples. Based on DFS time data, a cutoff score of 57.5% was selected for PARP-3 expression (Fig. 2). Tumors with immunohistological scores ≥57.5 and <57.5% were defined as tumors with high and low PARP-3 expression, respectively. A total of 234 (47.5%) tumors exhibited high expression and 259 (52.5%) tumors showed low expression.
Figure 2.
ROC curves were used to determine the cutoff score for poly(ADP-ribose) polymerase-3 overexpression in breast cancer, based on the DFS of patients with breast cancer. Values for sensitivity and specificity for (A) DFS and (B) OS were plotted. The areas under the curve and P-value are indicated in the figure. ROC, receiver operating characteristic; DFS, disease-free survival; OS, overall survival.
Association of PARP-3 expression with clinicopathological characteristics of patients with breast cancer
The association between PARP-3 expression and clinicopathological characteristics of patients with breast cancer was investigated (Table II). Age, menopausal status, tumor size, tumor type, TNM stage, lymph node metastasis, p53 status and BRCA1 status were not significantly associated with the expression of PARP-3. High PARP-3 expression level was associated with histological grade II–III (P=0.012) when compared with PARP-3 low expression level.
Table II.
Association between PARP-3 expression and clinicopathological features of patients with breast cancer.
| PARP-3 expression, n (%) | |||
|---|---|---|---|
| Characteristics | High | Low | P-valuea |
| Age at diagnosis | |||
| ≤51 years | 138 (49.5) | 141 (50.5) | 0.310 |
| >51 years | 96 (44.9) | 118 (55.1) | |
| Menopausal status | |||
| Pre-menopause | 133 (49.6) | 135 (50.4) | 0.294 |
| Post-menopause | 101 (44.9) | 124 (55.1) | |
| Tumor size | |||
| ≤2.0 cm | 156 (48.0) | 169 (52.0) | 0.942 |
| >2.0, <5.0 cm | 68 (46.6) | 78 (53.4) | |
| ≥5.0 cm | 10 (45.5) | 12 (54.5) | |
| Lymph node metastasis | |||
| No | 122 (45.5) | 146 (54.5) | 0.346 |
| Yes | 112 (49.8) | 113 (50.2) | |
| TNM stage | |||
| I–II | 175 (48.1) | 189 (51.9) | 0.647 |
| III–IV | 70 (54.3) | 59 (45.7) | |
| Histological grade | |||
| G1 | 29 (34.9) | 54 (65.1) | 0.012 |
| G2 | 178 (48.5) | 189 (51.5) | |
| G3 | 26 (61.9) | 16 (38.1) | |
| Histological type | |||
| Ductal carcinoma | 216 (47.5) | 239 (52.5) | 0.196 |
| Lobular carcinoma | 7 (63.6) | 4 (36.4) | |
| Mucinous carcinoma | 6 (66.7) | 3 (33.3) | |
| Other | 5 (29.4) | 12 (70.6) | |
| p53 status | |||
| Negative | 80 (48.2) | 86 (51.8) | 0.650 |
| Positive | 106 (45.9) | 125 (54.1) | |
| BRCA1 status | |||
| Negative | 52 (51.0) | 50 (49.0) | 0.289 |
| Positive | 132 (44.9) | 162 (55.1) | |
P-value calculated using χ2 or Fisher's exact. PARP-3, poly(ADP-ribose). polymerase-3; TNM, tumor-node-metastasis; BRCA1, breast cancer susceptibility gene 1.
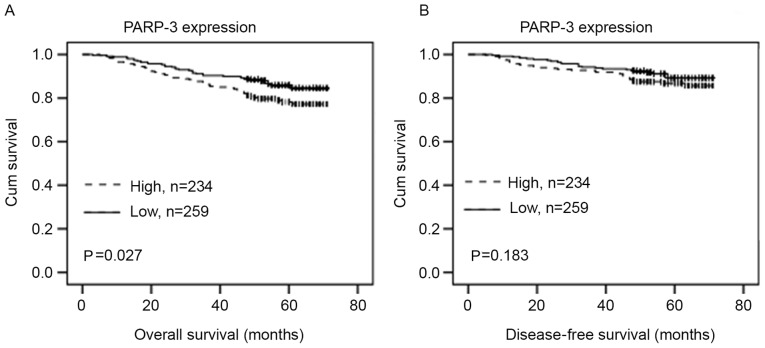
Association of PARP-3 expression with the survival of patients with breast cancer
The association of the PARP-3 expression with the OS or DFS in patients with breast cancer was evaluated using Kaplan-Meier analysis and log-rank test. PARP-3 overexpression was significantly associated with shorter DFS time (P=0.027) (Fig. 3A). Although PARP-3 expression exhibited a tendency toward shorter OS, no statistically significant difference was observed (P=0.183) (Fig. 3B).
Figure 3.
Kaplan-Meier survival analysis of PARP-3 expression in patients with breast cancer. The log-rank test was performed to test statistical significance. Survival curves show the association between PARP-3 expression and (A) DFS or (B) OS in 493 patients with breast cancer with PARP-3 expression. PARP-3, poly(ADP-ribose) polymerase-3; DFS, disease-free survival; OS, overall survival; Cum, cumulative.
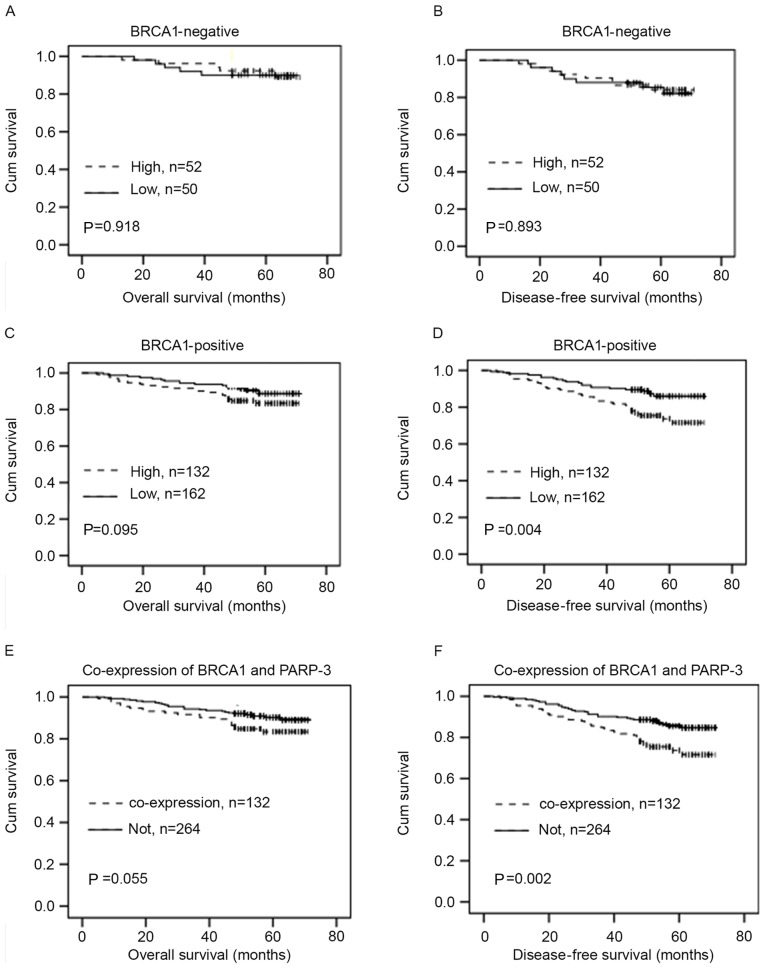
The association of PARP-3 expression with the OS or DFS in breast cancer patients with different BRCA1 statuses was then investigated. In BRCA1-negative patients, PARP-3 expression was not significantly associated with the OS or DFS (P>0.05) (Fig. 4A and B). However, in BRCA1-positive patients, PARP-3 expression exhibited a tendency toward shorter OS, but this association was not statistically significant (P=0.095) (Fig. 4C). PARP-3 overexpression was significantly associated with shorter DFS time (P=0.004) (Fig. 4D). Furthermore, there was a greater association between the combination of high PARP3 and BRCA1 expression and shorter OS (P=0.055) (Fig. 4E) and DFS time (P=0.002) (Fig. 4F) compared with non-combination of PARP3 and BRCA1.
Figure 4.
Kaplan-Meier survival analysis of PARP-3 expression in patients with breast cancer with different BRCA1 status. The log-rank test was performed to test statistical significance. (A-D) Survival curves show the association between PARP-3 expression and DFS or OS in patients with BRCA1-negative andBRCA1-positive breast cancer. (E and F) Survival curves show the association of the combined expression of PARP-3 and BRCA1 with OS or DFS in patients with breast cancer. PARP-3, poly(ADP-ribose) polymerase-3; DFS, disease-free survival; OS, overall-survival; BRCA1, breast cancer susceptibility gene 1; Cum, cumulative.
Univariate Cox regression analysis was performed to estimate the impact of each clinicopathological variable on OS and DFS in patients with breast cancer. The univariate analysis identified that menopausal status [hazard ratio (HR)=1.527; P=0.044], histological grade (HR=2.674; P=0.012), TNM stage (HR=4.20; P<0.001) and lymph node metastasis (HR=2.513; P<0.001) were significantly associated with the OS and DFS of patients with breast cancer (Table III). Age (P=0.041) and tumor size (P=0.042) were also identified to be significantly associated with the OS of patients with breast cancer. In addition, PARP-3 overexpression was significantly associated with shorter DFS time of patients with breast cancer (P=0.029; Table III). Furthermore, multivariate Cox regression analysis (Table IV) indicated that TNM stage (RR=5.665; P<0.001), menopausal status (RR=2.535; P=0.045) and PARP-3 (RR=1.944; P=0.008) were independent prognostic factors for shorter DFS time. TNM stage (HR=9.75; P<0.001) and histological grade (HR=2.592; P=0.004) were independent prognostic factors for shorter OS in patients with breast cancer.
Table III.
Univariate Cox regression analysis of overall survival and disease-free survival in patients with breast cancer.
| DFS | OS | |||
|---|---|---|---|---|
| Parameters | HR (95% CI) | P-valuea | HR (95% CI) | P-valuea |
| Age (>51/≤51 years) | 1.352 (0.90–2.04) | 0.148 | 1.702 (1.02–2.84) | 0.041 |
| Menopausal status (post/pre) | 1.527 (1.01–2.30) | 0.044 | 1.846 (1.10–3.09) | 0.020 |
| Tumor size (>2.0/≤2.0 cm) | 1.272 (0.83–1.95) | 0.271 | 1.714 (1.02–2.88) | 0.042 |
| Histological grade (III/II/I) | 2.674 (1.24–5.78) | 0.012 | 6.350 (1.55–25.99) | 0.010 |
| Histological type (ductal/lobular) | 0.804 (0.53–1.21) | 0.296 | 0.569 (0.26–1.23) | 0.153 |
| TNM stage (V/IV/III/II/I) | 4.200 (2.78–6.34) | <0.001 | 9.084 (5.12–16.11) | <0.001 |
| Lymph node status (yes/no) | 2.513 (1.63–3.87) | <0.001 | 4.572 (2.47–8.45) | <0.001 |
| BRCA1 status (positive/negative) | 1.365 (0.79–2.38) | 0.271 | 1.431 (0.71–2.87) | 0.312 |
| p53 status (positive/negative) | 1.063 (0.67–1.68) | 0.792 | 1.027 (0.59–1.79) | 0.927 |
| PARP-3 (positive/negative) | 1.619 (1.05–2.49) | 0.029 | 1.434 (0.84–2.44) | 0.186 |
P-value obtained from Univariate Cox regression analysis. DFS, disease-free survival; OS, overall survival; PARP-3, poly(ADP-ribose) polymerase-3; TNM, tumor-node-metastasis; BRCA1, breast cancer susceptibility gene 1; HR, hazard ratio; 95% CI, 95% confidence interval.
Table IV.
Multivariate Cox regression analysis of overall survival and disease-free survival in breast in patients with breast cancer.
| Disease-free survival | Overall survival | |||
|---|---|---|---|---|
| Category | RR (95% CI) | P-valuea | RR (95% CI) | P-valuea |
| Age (>51/≤51 years) | 0.740 (0.30~1.82) | 0.513 | 0.77 (0.215~2.76) | 0.689 |
| Menopausal status (post/pre) | 2.535 (1.02~6.30) | 0.045 | 3.156 (0.85~11.70) | 0.086 |
| Tumor size (≥5/ 2–5/≤2.0 cm) | 1.163 (0.77~1.77) | 0.481 | 1.543 (0.95~2.51) | 0.081 |
| Histological grade (III/II/I) | 1.681 (0.98~2.90) | 0.062 | 2.592 (1.35~4.97) | 0.004 |
| Histological type (ductal/ lobular/mucinous/other) | 0.952 (0.52–1.76) | 0.875 | 0.591 (0.14–2.52) | 0.477 |
| TNM stage (V/IV/III/II/I) | 5.665 (2.56~12.5) | <0.001 | 9.75 (3.12~30.51) | <0.001 |
| Lymph node status (≥10/4~9/1~3/0) | 0.720 (0.31~1.65) | 0.439 | 0.934 (0.26~3.35) | 0.917 |
| PARP-3 (positive/negative) | 1.944 (1.19~3.19) | 0.008 | 1.716 (0.93~3.15) | 0.082 |
| BRCA1 status (positive/negative) | 1.167 (0.64~2.12) | 0.612 | 1.078 (0.51~2.29) | 0.846 |
| p53 status (positive/negative) | 1.130 (0.69~1.87) | 0.632 | 1.116 (0.60~2.08) | 0.730 |
P-value obtained from Multivariate Cox regression. DFS, disease-free survival; OS, overall survival; PARP-3, poly(ADP-ribose) polymerase-3; TNM, tumor-node-metastasis; RR, relative risk; 95% CI, 95% confidence interval.
Association of PARP-3 expression with therapeutic responses in patients with breast cancer
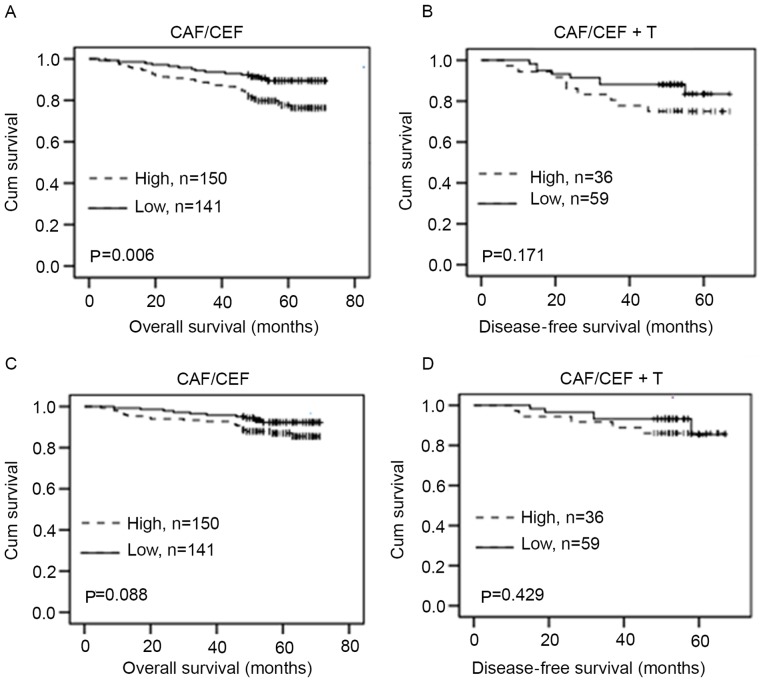
The association between the level of PARP-3 expression and therapeutic responses in patients with breast cancer receiving chemotherapy was examined. PARP-3 overexpression was significantly associated with shorter DFS time in patients with breast cancer with CAF/CEF treatment (P=0.006) (Fig. 5A), but not significantly associated with DFS (P=0.171) (Fig. 5B) in patients with CAF/CEF+T treatment. Although PARP-3 overexpression exhibited a tendency toward shorter OS in patients with breast cancer with CAF/CEF treatment, no statistically significant difference was observed (P=0.088) (Fig. 5C). In addition, PARP-3 expression was not significantly associated with OS (P=0.420) (Fig. 5D) in patients with CAF/CEF+T treatment.
Figure 5.
Kaplan-Meier survival analysis of PARP-3 expression in patients with breast cancer with chemotherapy. (A-D) Survival curves show the association between PARP-3 expression and disease-free survival oroverall survival in patients with breast cancer receiving CAF/CEF treatment or CAF/CEF + T treatment. PARP-3, poly(ADP-ribose) polymerase-3; CAF/CEF, cyclophosphamide/doxorubicin or epirubicin/5-fluorouracil; CAF/CEF + T, CAF/CEF + docetaxel.
Discussion
It is well known that DNA damage, if not repaired properly, can lead to genetic instability, which may increase the development of cancer (25). Previous studies have shown that PARP-3 serves an important role in DSB repair (7,19). However, the role of PARP-3 in breast cancer tumorigenesis remains to be determined. In the present study, tissue-microarray-based immunohistochemistry was performed to examine PARP-3 expression in 493 patients with breast cancer and 54 tumor-adjacent control samples. It was revealed that PARP-3 immunoreactivity occurred more frequently in breast cancer samples compared with control samples, indicating that PARP-3 overexpression may contribute to the development of breast cancer malignancy. Similarly, several studies have shown that PARP-1, the most studied member of PARP superfamily that is also involved in DNA damage repair, is upregulated in numerous tumors, including breast cancer (8–13). These findings indicated that the DNA damage repair function of PARP-1 and PARP-3 may be important for cancer development. However, Bieche et al (20) reported that the mRNA expression of PARP-3 was under-expressed in 10.4% of patients with breast cancer. The difference between the study by Bieche et al and the present study may be due to different methods, since the mRNA levels of PARP-3 detected by Bieche et al may not reflect the protein level of PARP-3 examined by the present study.
The association between PARP-3 expression and clinicopathological features in patients with breast cancer was analyzed in the present study. It was revealed that PARP-3 overexpression was associated with more differentiated (histological grade I–II) tumors. It is likely that PARP-3 is upregulated in response to an increase in DNA breaks during tumor cell differentiation, and PARP-3 upregulation may promote repair of DNA damage in tumors, thereby increasing cancer progression and development. Consistent with this hypothesis, PARP-3 overexpression was also found to be significantly associated with shorter DFS time and exhibited a tendency toward shorter OS in patients with breast cancer. Similarly, PARP-1 overexpression has been reported to be associated with poor prognosis in patients with breast cancer (12,26). Furthermore, it was found that PARP-3 overexpression is an independent prognostic factor for shorter DFS and OS in patients with breast cancer. Therefore, PARP-3 may be used as a potential biomarker for clinical outcomes of patients with breast cancer.
Eukaryotic cells have two repair pathways to repair DSB: Homologous recombination and non-homologous end joining (NHEJ) (27). PARP-3 in combination with aprataxin and PNKP-like factor accelerates NHEJ (28,29), and BRCA1 is known to be a central component in homologous recombination (30–32). Furthermore, Beck et al reported that PARP-3 performs a key role in determining the choice between homologous recombination and NHEJ pathways in the repair of DSB (33). In the present study, it was indicated that PARP-3 overexpression was significantly associated with shorter DFS time and exhibited a tendency toward shorter OS in BRCA1-positive patients with breast cancer. Additionally, the combined high expression of BRCA1 and PARP-3 was associated with shorter DFS and OS in patients with breast cancer compared with non-combined BRCA1 and PARP-3 expression. Therefore, for tumor cells with high expression of BRCA1, PARP-3-overexpressing cells may able to repair DNA damage more efficiently compared with PARP-3 deficient cells, thus leading to prolonged survival of the tumor and poor prognosis of the patients with cancer. However, it was found that PARP-3 expression was not significantly associated with the OS or DFS in BRCA1-negative patients with breast cancer. The findings that PARP-3 overexpression was significantly associated with the shorter survival time in BRCA1-positive, but not BRCA1-negative, breast cancer patients suggest that the role of PARP-3 in breast cancer may depend on BRCA1 status. Therefore, PARP-3 inhibitor may be a novel strategy for the treatment of BRAC1-positive breast cancer patients with PARP-3 overexpression.
It is known that chemotherapeutic drugs can induce DNA damage, and DNA damage repair may affect the outcome of therapy (34). In the present study, the association of PARP-3 expression with therapeutic responses in patients with breast cancer receiving CAF/CEF chemotherapy was examined. It was revealed that PARP-3 overexpression was significantly associated with shorter DFS time, and exhibited a tendency toward shorter OS in patients with breast cancer who received CAF/CEF treatment. The present findings suggested that tumors with PARP-3 overexpression exhibited resistance to chemotherapy, possibly by an increased ability of DNA repair. Furthermore, PARP-3 overexpression was not significantly associated with DFS and OS in patients with CAF/CEF+T treatment. It appears that addition of docetaxel inhibited PARP-3-induced drug resistance in patients with breast cancer. It has been reported that docetaxel can cause cleavage of PARP in breast cancer cells, melanoma cells and ovarian cancer cells (35–37). Taken together, the present results suggested that docetaxel may induce cleavage of PARP-3, thereby reducing PARP-3-induced drug resistance and improving the survival of patients with breast cancer with PARP-3 overexpression.
In summary, PARP-3 expression was investigated in 493 patients with breast cancer, and the association of PARP-3 expression with the clinicopathological feature, therapeutic responses and prognosis of patients with breast cancer was analyzed. It was found that PARP-3 expression was significantly increased in breast cancer tissues compared with tumor-adjacent tissues. PARP-3 overexpression was associated with poor outcome of patients with breast cancer, particularly in BRCA1-positive patients. Furthermore, it was found that PARP-3 overexpression was associated with shorter survival time in patients with CAF/CEF chemotherapy, but not in patients with CAF/CEF+T chemotherapy, indicating that inhibition of PARP-3 by docetaxel may increase the survival of patients with breast cancer. PARP-3 may be used as a biomarker for predicting the clinical outcome of patients receiving chemotherapy, and targeting PARP-3 may be a potential therapeutic strategy for the treatment of breast cancer with PARP-3 overexpression.
Acknowledgements
The authors would like to acknowledge Xuefeng Bai for providing technical help and Xiaosong Yu for assisting in writing the manuscript.
Funding
The present study was supported by grants from the National Natural Science Foundation of the People's Republic of China (grant no. 71273279; Beijing China), Program for Liaoning Innovative Research Team in University, (grant no. LT2014016; Shenyang, China) and Shenyang Science and Technology Projects (grant no. F14-232-6-05; Shenyang, China).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contribution
MW, ZS, LZ and HW assisted in the design and conception of the present study. ZS, YW, QX, MS and ZY analyzed and interpreted the data of patients with breast cancer. ZS, WL and XG performed the histological examination of the breast cancer tissues. LZ, HW, MS contributed in drafting the manuscript. QX and MW were major contributor in revising the manuscript. ZC, PH collected the patients' clinical data and performed the follow-up study. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The Institute Research Medical Ethics Committee of China Medical University approved the consent procedure.
Patient consent for publication
The patient, or parent, guardian or next of kin (if patient is deceased) provided verbal informed consent for the publication of any associated data and accompanying images.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Bertucci F, Birnbaum D. Reasons for breast cancer heterogeneity. J Biol. 2008;7:6. doi: 10.1186/jbiol67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patani N, Martin LA, Dowsett M. Biomarkers for the clinical management of breast cancer: International perspective. Int J Cancer. 2013;133:1–13. doi: 10.1002/ijc.27997. [DOI] [PubMed] [Google Scholar]
- 3.Hakmé A, Wong HK, Dantzer F, Schreiber V. The expanding field of poly(ADP-ribosyl)ation reactions. ‘Protein modifications: Beyond the usual suspects’ review series. EMBO Rep. 2008;9:1094–1100. doi: 10.1038/embor.2008.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hottiger MO, Hassa PO, Lüscher B, Schüler H, Koch-Nolte F. Toward a unified nomenclature for mammalian ADP-ribosyltransferases. Trends Biochem Sci. 2010;35:208–219. doi: 10.1016/j.tibs.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Megnin-Chanet F, Bollet MA, Hall J. Targeting poly(ADP-ribose) polymerase activity for cancer therapy. Cell Mol Life Sci. 2010;67:3649–3662. doi: 10.1007/s00018-010-0490-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cepeda V, Fuertes MA, Castilla J, Alonso C, Quevedo C, Soto M, Pérez JM. Poly(ADP-ribose) polymerase-1 (PARP-1) inhibitors in cancer chemotherapy. Recent Pat Anticancer Drug Discov. 2006;1:39–53. doi: 10.2174/157489206775246430. [DOI] [PubMed] [Google Scholar]
- 7.Boehler C, Dantzer F. PARP-3, a DNA-dependent PARP with emerging roles in double-strand break repair and mitotic progression. Cell Cycle. 2011;10:1023–1024. doi: 10.4161/cc.10.7.15169. [DOI] [PubMed] [Google Scholar]
- 8.Miwa M, Masutani M. PolyADP-ribosylation and cancer. Cancer Sci. 2007;98:1528–1535. doi: 10.1111/j.1349-7006.2007.00567.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shimizu S, Nomura F, Tomonaga T, Sunaga M, Noda M, Ebara M, Saisho H. Expression of poly(ADP-ribose) polymerase in human hepatocellular carcinoma and analysis of biopsy specimens obtained under sonographic guidance. Oncol Rep. 2004;12:821–825. [PubMed] [Google Scholar]
- 10.Staibano S, Pepe S, Lo Muzio L, Somma P, Mascolo M, Argenziano G, Scalvenzi M, Salvatore G, Fabbrocini G, Molea G, et al. Poly(adenosine diphosphate-ribose) polymerase 1 expression in malignant melanomas from photoexposed areas of the head and neck region. Hum Pathol. 2005;36:724–731. doi: 10.1016/j.humpath.2005.04.017. [DOI] [PubMed] [Google Scholar]
- 11.Brustmann H. Poly(adenosine diphosphate-ribose) polymerase expression in serous ovarian carcinoma: Correlation with p53, MIB-1, and outcome. Int J Gynecol Pathol. 2007;26:147–153. doi: 10.1097/01.pgp.0000235064.93182.ec. [DOI] [PubMed] [Google Scholar]
- 12.Rojo F, García-Parra J, Zazo S, Tusquets I, Ferrer-Lozano J, Menendez S, Eroles P, Chamizo C, Servitja S, Ramírez-Merino N, et al. Nuclear PARP-1 protein overexpression is associated with poor overall survival in early breast cancer. Ann Oncol. 2012;23:1156–1164. doi: 10.1093/annonc/mdr361. [DOI] [PubMed] [Google Scholar]
- 13.Ossovskaya V, Koo IC, Kaldjian EP, Alvares C, Sherman BM. Upregulation of Poly(ADP-Ribose) Polymerase-1 (PARP1) in triple-negative breast cancer and other primary human tumor types. Genes Cancer. 2010;1:812–821. doi: 10.1177/1947601910383418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Shaughnessy J, Osborne C, Pippen JE, Yoffe M, Patt D, Rocha C, Koo IC, Sherman BM, Bradley C. Iniparib plus chemotherapy in metastatic triple-negative breast cancer. N Engl J Med. 2011;364:205–214. doi: 10.1056/NEJMoa1011418. [DOI] [PubMed] [Google Scholar]
- 15.Fong PC, Boss DS, Yap TA, Tutt A, Wu P, Mergui-Roelvink M, Mortimer P, Swaisland H, Lau A, O'Connor MJ, et al. Inhibition of poly(ADP-ribose) polymerase in tumors from BRCA mutation carriers. N Engl J Med. 2009;361:123–134. doi: 10.1056/NEJMoa0900212. [DOI] [PubMed] [Google Scholar]
- 16.Tutt A, Robson M, Garber JE, Domchek SM, Audeh MW, Weitzel JN, Friedlander M, Arun B, Loman N, Schmutzler RK, et al. Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and advanced breast cancer: A proof-of-concept trial. Lancet. 2010;376:235–244. doi: 10.1016/S0140-6736(10)60892-6. [DOI] [PubMed] [Google Scholar]
- 17.De Vos M, Schreiber V, Dantzer F. The diverse roles and clinical relevance of PARPs in DNA damage repair: Current state of the art. Biochem Pharmacol. 2012;84:137–146. doi: 10.1016/j.bcp.2012.03.018. [DOI] [PubMed] [Google Scholar]
- 18.Langelier MF, Riccio AA, Pascal JM. PARP-2 and PARP-3 are selectively activated by 5′ phosphorylated DNA breaks through an allosteric regulatory mechanism shared with PARP-1. Nucleic Acids Res. 2014;42:7762–7775. doi: 10.1093/nar/gku474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boehler C, Gauthier LR, Mortusewicz O, Biard DS, Saliou JM, Bresson A, Sanglier-Cianferani S, Smith S, Schreiber V, Boussin F, Dantzer F. Poly(ADP-ribose) polymerase 3 (PARP3), a newcomer in cellular response to DNA damage and mitotic progression. Proc Natl Acad Sci USA. 2011;108:2783–2788. doi: 10.1073/pnas.1016574108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bieche I, Pennaneach V, Driouch K, Vacher S, Zaremba T, Susini A, Lidereau R, Hall J. Variations in the mRNA expression of poly(ADP-ribose) polymerases, poly(ADP-ribose) glycohydrolase and ADP-ribosylhydrolase 3 in breast tumors and impact on clinical outcome. Int J Cancer. 2013;133:2791–2800. doi: 10.1002/ijc.28304. [DOI] [PubMed] [Google Scholar]
- 21.Bansal C, Pujani M, Sharma KL, Srivastava AN, Singh US. Grading systems in the cytological diagnosis of breast cancer: A review. J Cancer Res Ther. 2014;10:839–845. doi: 10.4103/0973-1482.140979. [DOI] [PubMed] [Google Scholar]
- 22.Cowherd SM. Tumor staging and grading: A primer. Methods Mol Biol. 2012;823:1–18. doi: 10.1007/978-1-60327-216-2_1. [DOI] [PubMed] [Google Scholar]
- 23.Fang Y, Wei J, Cao J, Zhao H, Liao B, Qiu S, Wang D, Luo J, Chen W. Protein expression of ZEB2 in renal cell carcinoma and its prognostic significance in patient survival. PLoS One. 2013;8:e62558. doi: 10.1371/journal.pone.0062558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhu W, Cai MY, Tong ZT, Dong SS, Mai SJ, Liao YJ, Bian XW, Lin MC, Kung HF, Zeng YX, et al. Overexpression of EIF5A2 promotes colorectal carcinoma cell aggressiveness by upregulating MTA1 through C-myc to induce epithelial-mesenchymaltransition. Gut. 2012;61:562–575. doi: 10.1136/gutjnl-2011-300207. [DOI] [PubMed] [Google Scholar]
- 25.Khanna KK, Jackson SP. DNA double-strand breaks: Signaling, repair and the cancer connection. Nat Genet. 2001;27:247–254. doi: 10.1038/85798. [DOI] [PubMed] [Google Scholar]
- 26.Goncalves A, Finetti P, Sabatier R, Gilabert M, Adelaide J, Borg JP, Chaffanet M, Viens P, Birnbaum D, Bertucci F. Poly(ADP-ribose) polymerase-1 mRNA expression in human breast cancer: A meta-analysis. Breast Cancer Res Treat. 2011;127:273–281. doi: 10.1007/s10549-010-1199-y. [DOI] [PubMed] [Google Scholar]
- 27.Chapman JR, Taylor MR, Boulton SJ. Playing the end game: DNA double-strand break repair pathway choice. Mol Cell. 2012;47:497–510. doi: 10.1016/j.molcel.2012.07.029. [DOI] [PubMed] [Google Scholar]
- 28.Rulten SL, Fisher AE, Robert I, Zuma MC, Rouleau M, Ju L, Poirier G, Reina-San-Martin B, Caldecott KW. PARP-3 and APLF function together to accelerate nonhomologous end-joining. Mol Cell. 2011;41:33–45. doi: 10.1016/j.molcel.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 29.Fenton AL, Shirodkar P, Macrae CJ, Meng L, Koch CA. The PARP3- and ATM-dependent phosphorylation of APLF facilitates DNA double-strand break repair. Nucleic Acids Res. 2013;41:4080–4092. doi: 10.1093/nar/gkt134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang J. The role of BRCA1 in homologous recombination repair in response to replication stress: Significance in tumorigenesis and cancer therapy. Cell Biosci. 2013;3:11. doi: 10.1186/2045-3701-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Prakash R, Zhang Y, Feng W, Jasin M. Homologous recombination and human health: The roles of BRCA1, BRCA2, and associated proteins. Cold Spring Harb Perspect Biol. 2015;7:a016600. doi: 10.1101/cshperspect.a016600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Willis NA, Chandramouly G, Huang B, Kwok A, Follonier C, Deng C, Scully R. BRCA1 controls homologous recombination at Tus/Ter-stalled mammalian replication forks. Nature. 2014;510:556–559. doi: 10.1038/nature13295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Beck C, Boehler C, Barbat Guirouilh J, Bonnet ME, Illuzzi G, Ronde P, Gauthier LR, Magroun N, Rajendran A, Lopez BS, et al. PARP3 affects the relative contribution of homologous recombination and nonhomologous end-joining pathways. Nucleic Acids Res. 2014;42:5616–5632. doi: 10.1093/nar/gku174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Casorelli I, Bossa C, Bignami M. DNA damage and repair in human cancer: Molecular mechanisms and contribution to therapy-related leukemias. Int J Environ Res Public Health. 2012;9:2636–2657. doi: 10.3390/ijerph9082636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang Q, Wieder R. All-trans retinoic acid potentiates Taxotere-induced cell death mediated by Jun N-terminal kinase in breast cancer cells. Oncogene. 2004;23:426–433. doi: 10.1038/sj.onc.1207040. [DOI] [PubMed] [Google Scholar]
- 36.Mhaidat NM, Wang Y, Kiejda KA, Zhang XD, Hersey P. Docetaxel-induced apoptosis in melanoma cells is dependent on activation of caspase-2. Mol Cancer Ther. 2007;6:752–761. doi: 10.1158/1535-7163.MCT-06-0564. [DOI] [PubMed] [Google Scholar]
- 37.Kolfschoten GM, Hulscher TM, Duyndam MC, Pinedo HM, Boven E. Variation in the kinetics of caspase-3 activation, Bcl-2 phosphorylation and apoptotic morphology in unselected human ovarian cancer cell lines as a response to docetaxel. Biochem Pharmacol. 2002;63:733–743. doi: 10.1016/S0006-2952(01)00895-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.