Abstract
Objective
Prescription drug monitoring programs (PDMPs) enable prescribers to review patient prescription histories, and their use is mandatory in many states. We estimated the cost of physicians retrieving PDMP patient reports compared with a model where a delegate (i.e., administrative staff) retrieves reports.
Methods
We performed a cost analysis with a one-year time horizon, from the perspective of physicians’ employers. We obtained specialty-specific estimates of controlled substance prescribing frequency from the National Ambulatory Medical Care Survey, 2012–2014. We defined three PDMP usage cases based on the frequency of queries: comprehensive (before every Schedule II–IV controlled substance prescription), selective (before new Schedule II–IV prescriptions and every six months for continuing medications), and minimal (before new Schedule II or III prescriptions and annually for continuing medications).
Results
The delegate model was less costly for all specialties in the comprehensive usage case and most specialties in the selective usage case, and it was similar to physician model costs in the minimal usage case. Estimated annual costs of the physician model to a large health care system (1,000 full-time equivalent physicians) were $1.6 million for comprehensive usage, $1.1 million for selective usage, and $645,313 for minimal usage. The delegate model was less costly in the comprehensive (savings of $907,283) and selective usage cases (savings of $156,216).
Conclusions
Relying on delegates vs physicians to retrieve reports is less costly in most cases. Automation and integration of PDMP data into electronic health records may reduce costs further. Physicians, health care systems, and states should collaborate to streamline access to PDMPs.
Keywords: Prescription Drug Monitoring Programs, Opioid Analgesics, Controlled Substances, Primary Care, Cost Analysis
Introduction
Prescription drug monitoring programs (PDMPs) are state-level registries of controlled substances dispensed to patients. By allowing prescribers to query the database for patients’ complete prescription histories, PDMPs have the potential to help prescribers recognize patterns of concerning behavior that suggest high-risk use or misuse [1]. While PDMPs have received considerable attention in the context of the opioid epidemic, most state PDMPs also receive data on other controlled substances such as stimulants, androgenic steroids, benzodiazepines, and prescription sleep medications, among others. As of December 2017, statewide PDMPs are operational in 49 of 50 states, and creation of a PDMP has been authorized in the remaining state [2,3].
Although physicians value information obtained from PDMPs, they have low rates of use in routine clinical practice [4–11]. In response, at least 39 states now mandate that physicians retrieve a PDMP patient report in certain situations, such as when prescribing chronic opioid therapy [12], a policy supported by clinical guidelines [13]. These state mandates are varied: In New York, for example, prescribers are required to retrieve a PDMP patient report prior to all Schedule II, III, and IV prescriptions, with few exceptions. Other states, like Tennessee, only require retrieval of a PDMP patient report before new prescriptions for a narrower set of medications (i.e., opioid analgesics and benzodiazepines) and annually for those receiving chronic therapy.
Despite considerable improvements to PDMP interfaces in recent years, time burden remains a frequently reported barrier to consistent PDMP use [4,5,7,8]. Simply retrieving patient reports from the PDMP system—a clerical function—can be laborious given the frequency of controlled substance prescriptions in clinical practice. The time that physicians spend retrieving PDMP patient reports may detract from other clinical activities or contribute to burnout. In the current environment, where PDMP use is shifting from voluntary to mandatory, this burden will be amplified. However, as with other administrative activities, training of delegates (e.g., administrative staff) to access PDMP patient reports could reduce physicians’ workload. Currently, 47 of 49 states with operational statewide PDMPs authorize delegates to obtain PDMP patient reports [14].
The goal of the current study was to estimate the time burden and cost of retrieving PDMP patient reports for primary care and specialty physicians. We estimated this cost for three PDMP usage cases corresponding to frequencies with which physicians check PDMPs. We created these usage cases based on clinical guidelines and existing state mandates. Further, to provide evidence for health systems, we compared whether relying on delegates to retrieve PDMP patient reports was more or less costly than relying on physicians. Finally, we estimated and compared the total cost of the physician and delegate models for a large outpatient health care system.
Methods
Time to Retrieve PDMP Patient Reports
For the purposes of this study, we focused only on the time required to retrieve PDMP patient reports and did not include the time associated with clinical functions such as reviewing and interpreting the reports. Retrieving a patient report consists of navigating to the PDMP web portal, logging in, and typing in the patient’s name and any relevant details (e.g., date of birth), submitting the query, and waiting for the results. As no studies have specifically detailed the time required for each of these steps, we directly timed a convenience sample of 29 primary care and specialist physicians from 13 states using a standardized script (Supplementary Data). We asked each physician to log in and retrieve a PDMP patient report five times each. We used the overall mean values of each step: 27 seconds to log in and 37 seconds to retrieve a report once logged in.
In addition to the time spent retrieving each PDMP patient report, we estimated that PDMP users have to periodically change their password (three minutes, twice per year) and would occasionally lose or forget their password and have to call the PDMP help desk to reset it (15 minutes, once every other year).
PDMP Usage
We considered three different PDMP usage cases, termed comprehensive, selective, and minimal. We created these usage cases to represent meaningful clinical variation and to be reflective of guideline recommendations and existing state mandates. We defined comprehensive usage as retrieving a PDMP patient report prior to prescribing any Schedule II (e.g., stimulants and opioid analgesics), Schedule III (e.g., androgenic steroids and some opioid analgesics), or Schedule IV controlled substance (e.g., benzodiazepines and nonbenzodiazepine sleep medicines). This could be either a new or continuing (renewal) prescription. We defined selective usage as retrieving a PDMP patient report prior to prescribing any new Schedule II, III, or IV controlled substance and every six months for patients taking Schedule II, III, or IV controlled substances chronically. We defined minimal usage as retrieving a PDMP patient report prior to prescribing any new Schedule II or III controlled substance and annually for any patient taking Schedule II or III controlled substances chronically.
Next, we obtained estimates of prescribing frequency. To estimate the specialty-specific proportion of visits involving a controlled substance prescription, we extracted data from the National Ambulatory Medical Care Survey (NAMCS) [15]. NAMCS is a national survey designed to collect information about the provision of ambulatory care services in the United States. Using pooled data from 2012–2014 and for each physician specialty as recorded by NAMCS, we first identified visits involving a prescription for any Schedule II, III, or IV controlled substances. As scheduling has changed recently (e.g., hydrocodone combination products were reclassified as Schedule II in 2014, and tramadol products were classified as Schedule IV in 2015), we recoded all medications, such that our results reflect current scheduling as of 2017. Next, for the comprehensive, selective, and minimal usage cases, we estimated the relevant proportion of visits that would require retrieval of a PDMP patient report. For example, for comprehensive usage, we estimated the specialty-specific proportion of visits where any Schedule II, III, or IV controlled substance was prescribed either as a new medication or as a continuation of chronic therapy. In all analyses, to make estimates nationally representative, we incorporated survey weights and variables to account for the survey’s design.
Physician and Delegate Models
For each usage case, we estimated the costs of retrieving PDMP patient reports using a model where physicians retrieve all information for their own patients and a model where a delegate (i.e., administrative staff) retrieves reports and provides them to physicians. There are no consensus protocols for these models, and so we based our parameters on the anecdotal experiences of our clinician authors and discussions with other clinicians.
For the physician model, prior to the start of each clinical day, the physician retrieves a PDMP patient report for each patient scheduled for that day who takes a controlled substance chronically. Therefore, the physician needs to log in once per day and can check all such patients at one time. As new controlled substance prescriptions are not typically predictable (i.e., due to an acute and unanticipated patient concern), physicians log in separately and retrieve a PDMP patient report for each new controlled substance that is prescribed.
For the delegate model, prior to the start of a clinical day, the physician and delegate meet for five minutes in which the physician indicates which patients are taking controlled substances chronically (i.e., will receive a continuing prescription). The delegate then obtains PDMP patient reports on these patients, prints out the reports (10 seconds per patient), and provides the reports to the physician. In addition to these time costs, the delegate model incurs additional costs of $0.05 for paper, ink, and printer wear-and-tear per printed patient report. As new controlled substance prescriptions are not typically predictable, physicians log in separately and retrieve a PDMP patient report for each new controlled substance that is prescribed (i.e., the delegate does not retrieve reports for new prescriptions).
Cost Estimation
The costs of retrieving PDMP patient reports are primarily time costs. For physicians (if self-employed) or their employers, these represent opportunity costs in that physician time spent retrieving PDMP patient reports could alternatively be spent on clinical activities such as face-to-face interactions with patients or follow-up of test results.
To estimate the total time spent retrieving PDMP patient reports over one year, we considered a full-time equivalent physician to have 4,200 patient visits per year, which is the productivity standard set by the Centers for Medicare and Medicaid Services and Health Resources and Services Administration [16]. For each usage case (i.e., comprehensive, selective, minimal) and model (i.e., physician, delegate), we summed the specialty-specific amount of time spent retrieving PDMP patient reports over a year, including logging in, submitting and receiving queries, routine password changes, lost/forgotten passwords, etc.
Time spent retrieving PDMP patient reports was valued according to physicians’ and delegates’ respective total hourly compensation. We calculated total hourly compensation by summing the specialty-specific hourly wage [17–19] and benefits (33.5%) [20]. For physicians of “other medical and surgical specialties” as defined by NAMCS, we used the hourly wage of “other physicians and surgeons” from Bureau of Labor Statistics data. For delegates, we summed the mean hourly wage and benefits (also 33.5%) for receptionists/information clerks working in offices of physicians [17]. To compare the specialty-specific physician costs of retrieving PDMP patient reports with the delegate model, we calculated the difference between the specialty-specific physician costs for each PDMP usage case and the delegate costs.
Total Cost for an Outpatient Health Care System
Finally, although costs incurred by individual providers are important, the aggregate cost over a health care system may be sizeable. To estimate the magnitude of costs for a health care system, we simulated a hypothetical large health care system with 1,000 full-time equivalent physicians. We based the composition of physician specialties in this health care system on the composition of the outpatient portion of one of our affiliated health care systems (Montefiore Medical Center). We then multiplied and summed the specialty-specific physician costs for each model and PDMP usage case.
Sensitivity Analysis
At each visit, NAMCS reports medications “continued,” defined as a renewal prescription or an explicit recommendation that the patient continue the medication (i.e., review of the patient’s medication list). Therefore, we may have overestimated the frequency of continuing prescriptions for some specialties, for example, cardiology, where 1.3% of visits resulted in a new prescription but 16.8% of visits have a continuing medication. Therefore, we conducted a sensitivity analysis limiting the percentage of continuing prescription office visits to three times the percentage of new prescription office visits (the approximate ratio for internal medicine and family medicine).
Results
For physicians, the estimated percentage of visits resulting in a new Schedule II, III, or IV controlled substance prescription is highest for orthopedic surgeons (6.3%, 95% confidence interval [CI] = 4.3–8.4), and the percentage of visits resulting in a continuing Schedule II, III, or IV controlled substance is highest for psychiatrists (36.3%, 95% CI = 32.8–39.9) (Table 1). Total hourly compensation varies between $118 (pediatrics) and $284 (orthopedic surgery), with the total compensation for delegates being $19. Psychiatrists spend the longest estimated time retrieving PDMP patient reports (21.9 hours annually), followed by neurologists (13.6), family medicine physicians (13.5), and internal medicine physicians (13.2) (Table 2).Time spent retrieving PDMP patient reports decreases substantially with selective PDMP usage and drops further with minimal usage (e.g., 8.9 and 3.3 hours, respectively, for psychiatrists).
Table 1.
Hourly total compensation and frequency of controlled substance prescriptions for physicians, by specialty, and nonphysician delegate
| Office Visits Resulting in a Schedule II, III, or IV Controlled Substance Prescription* |
|||||
|---|---|---|---|---|---|
| Category | Specialty | Hourly Total Compensation, $ | No. (unweighted) | New Prescription (95% CI), % | Continuing Prescription (95% CI), % |
| Primary care | Family medicine | 123 | 31,337 | 6.2 (5.7–6.8) | 16.5 (15.3–17.7) |
| Internal medicine | 126 | 16,950 | 5.0 (4.3–5.8) | 18.0 (16.3–19.7) | |
| Pediatrics | 118 | 21,468 | 1.2 (0.9–1.4) | 3.3 (2.8–3.9) | |
| Medical subspecialties | Cardiovascular diseases | 263 | 5,935 | 1.3 (0.6–1.8) | 16.8 (14.7–18.9) |
| Dermatology | 245 | 5,664 | 0.3 (0.2–0.5) | 2.7 (1.9–3.6) | |
| Neurology | 155 | 4,039 | 4.1 (2.5–5.7) | 20.5 (15.8–25.2) | |
| Oncology | 211 | 2,585 | 2.6 (1.7–3.6) | 14.3 (10.5–18.1) | |
| Psychiatry | 124 | 7,632 | 6.1 (4.4–7.8) | 36.3 (32.8–39.9) | |
| Surgical specialties | General surgery | 207 | 6,192 | 2.8 (1.9–3.7) | 9.9 (7.5–12.3) |
| Obstetrics and gynecology | 143 | 10,373 | 1.4 (1.1–1.7) | 4.6 (3.6–5.6) | |
| Ophthalmology | 198 | 9,814 | 0.5 (0.2–0.7) | 4.2 (3.3–5.2) | |
| Orthopedic surgery | 284 | 9,744 | 6.3 (4.3–8.4) | 14.8 (12.7–16.9) | |
| Otolaryngology | 237 | 4,400 | 1.7 (1.0–2.3) | 6.7 (4.6–8.8) | |
| Urology | 236 | 4,687 | 2.8 (2.1–3.5) | 11.3 (9.1–13.5) | |
| Other | Other medical and surgical specialties† | 127 | 29,978 | 4.2 (3.6–4.7) | 16.2 (14.5–18.0) |
| Nonphysician | Delegate‡ | 19 | — | — | — |
CI = confidence interval.
Estimates obtained from the 2012–2014 National Ambulatory Medical Care Survey.
Includes pain management, palliative care, and physical medicine/rehabilitation specialists, among others.
The delegate is a “healthcare receptionist” from Bureau of Labor Statistics wage estimates.
Table 2.
Annual time spent retrieving prescription drug monitoring program patient reports by physicians
| Usage Case Time, h |
||||
|---|---|---|---|---|
| Category | Specialty | Comprehensive | Selective | Minimal |
| Primary care | Family medicine | 13.5 | 6.7 | 3.4 |
| Internal medicine | 13.2 | 5.9 | 2.7 | |
| Pediatrics | 3.4 | 1.3 | 1.0 | |
| Medical subspecialties | Cardiovascular diseases | 9.9 | 3.0 | 0.7 |
| Dermatology | 2.3 | 0.6 | 0.3 | |
| Neurology | 13.6 | 5.6 | 2.2 | |
| Oncology | 9.8 | 3.7 | 1.6 | |
| Psychiatry | 21.9 | 8.9 | 3.3 | |
| Surgical specialties | General surgery | 8.1 | 3.3 | 2.1 |
| Obstetrics and gynecology | 4.5 | 1.6 | 0.8 | |
| Ophthalmology | 3.5 | 0.9 | 0.3 | |
| Orthopedic surgery | 12.8 | 6.5 | 4.4 | |
| Otolaryngology | 5.9 | 2.1 | 0.7 | |
| Urology | 8.7 | 3.5 | 2.2 | |
| Other | Other medical and surgical specialties | 11.8 | 5.1 | 2.8 |
| Nonphysician | Delegate (mean) | 11.8 | 3.4 | 1.7 |
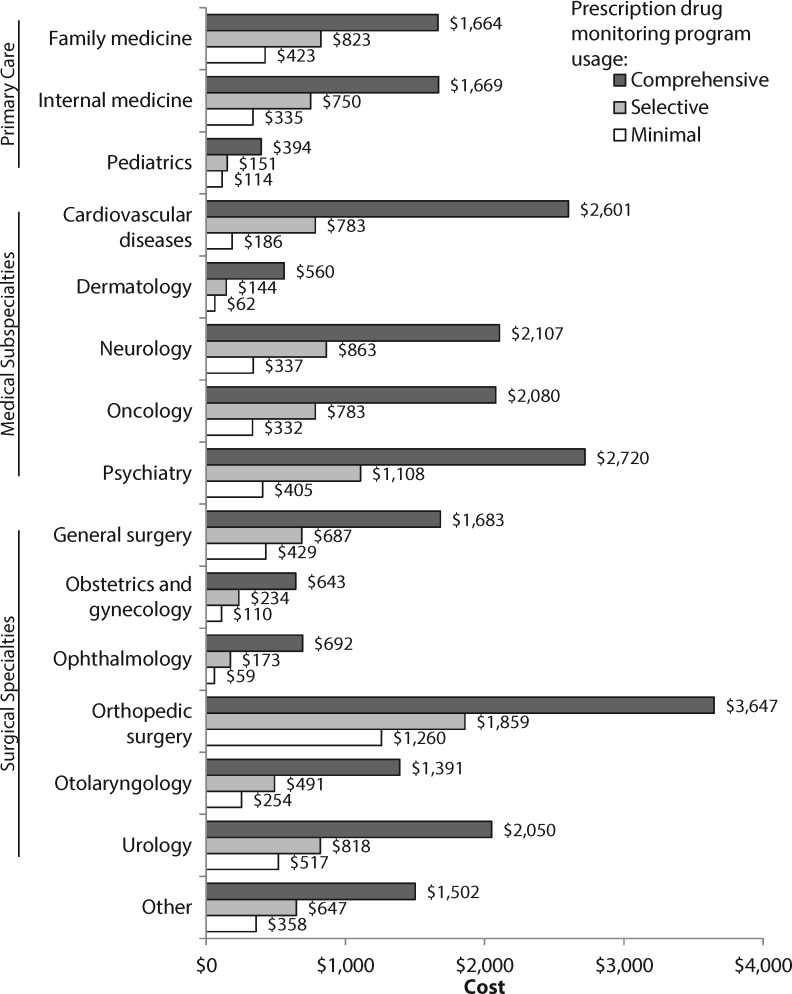
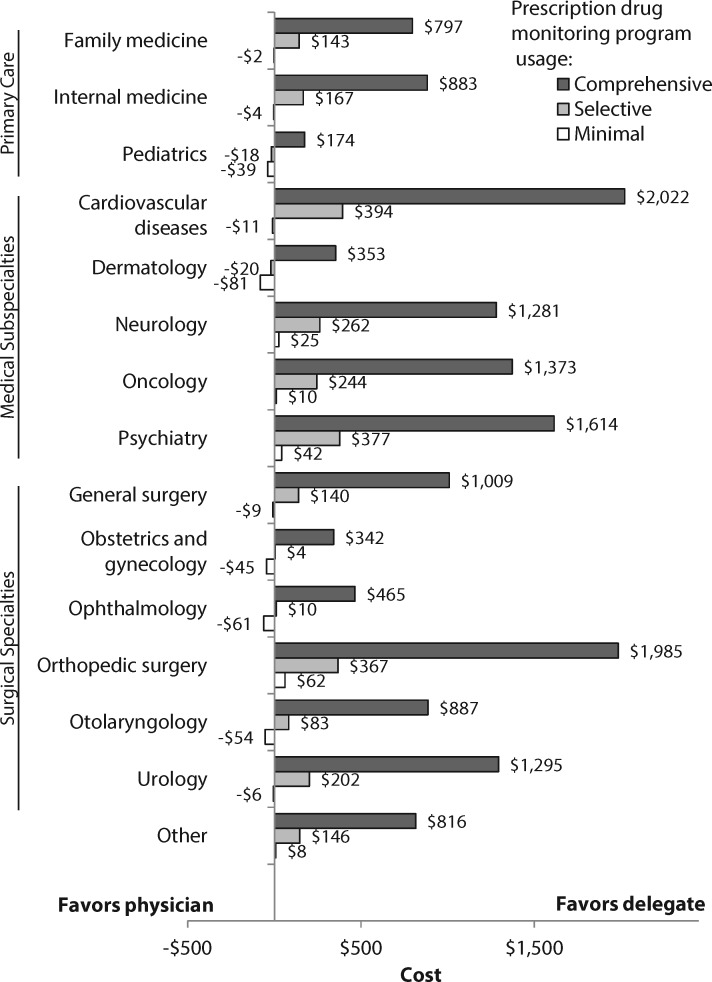
The annual time cost of retrieving PDMP patient reports varies by physician specialty (Figure 1). For comprehensive, selective, and minimal PDMP usage, orthopedic surgeons incur the highest costs ($3,647, $1,859, and $1,260, respectively), followed by psychiatrists ($2,720, $1,108, and $405, respectively) and cardiologists ($2,601, $783, and $186, respectively). Comparing the cost of the physician vs delegate model, use of the delegate model produces cost savings for all specialties in the comprehensive usage case and all specialties except for pediatrics and dermatology in the selective usage case (Figure 2). For the minimal usage case, the physician and delegate models are roughly similar in cost.
Figure 1.
Annual time cost for physician retrieval of prescription drug monitoring program patient reports by specialty. Dark gray bars show the annual time cost, by physician specialty, in the comprehensive usage case (querying before every Schedule II–IV controlled substance prescription). Medium gray bars show the cost in the selective usage case (before new Schedule II–IV prescriptions and every six months for continuing medications), and white bars show the cost in the minimal usage case (before new Schedule II or III prescriptions and annually for continuing medications).
Figure 2.
Difference between annual cost of physician versus delegate retrieval of prescription drug monitoring program patient reports, by specialty. Bars show the cost of the physician model minus the cost of the delegate model in the comprehensive usage case (querying before every Schedule II–IV controlled substance prescription), selective usage case (before new Schedule II–IV prescriptions and every six months for continuing medications), and minimal usage case (before new Schedule II or III prescriptions and annually for continuing medications). A negative number indicates that the physician model is less costly, and a positive number indicates that the delegate model is less costly.
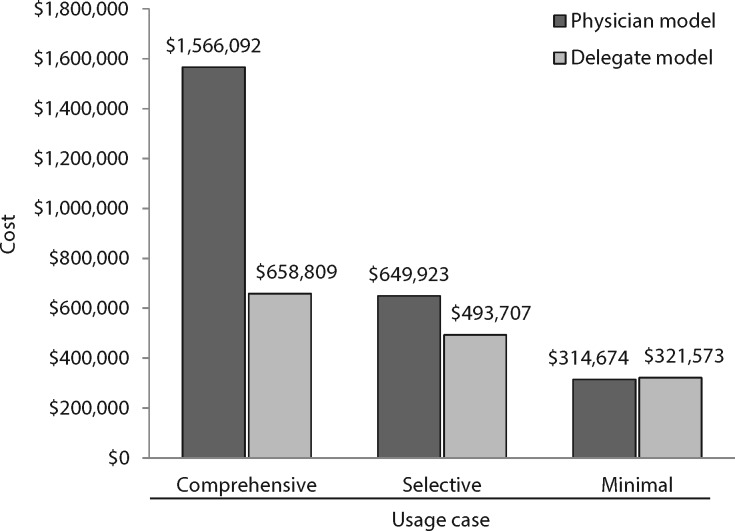
For a large outpatient health care system consisting of 1,000 full-time equivalent physicians, the aggregate cost of retrieving PDMP patient reports is shown in Figure 3. Compared with the physician model, the delegate model is less costly with comprehensive and selective PDMP usage (savings of $907,283 and $156,216, respectively). In the minimal usage case, the physician and delegate model costs are similar. In a sensitivity analysis accounting for possible overcounting of continuing prescriptions, the cost to a large health care system is approximately 20% lower than the main analysis for comprehensive PDMP usage, 13% lower for selective PDMP usage, and 5% lower for minimal PDMP usage (Supplementary Data).
Figure 3.
Total cost of physician versus delegate retrieval of prescription drug monitoring program patient reports for a 1000 full-time equivalent outpatient health care system. Dark gray bars show the total annual cost of the physician model in the comprehensive usage case (querying before every Schedule II–IV controlled substance prescription), selective usage case (before new Schedule II–IV prescriptions and every six months for continuing medications), and minimal usage case (before new Schedule II or III prescriptions and annually for continuing medications).
Discussion
Using data on controlled substance prescriptions from a national survey, combined with compensation data for physicians and delegates, we estimated the time cost of retrieving PDMP patient reports. Costs vary significantly by specialty both due to compensation and frequency of prescribing controlled substances, with orthopedic surgeons and psychiatrists incurring the highest costs. For most specialties, a model where delegates retrieve PDMP patient reports is less costly than relying on physicians to retrieve reports in the comprehensive usage case and in the selective usage case. While the cost to individual providers is relatively small as a proportion of providers’ yearly compensation, it represents potential lost opportunities for other activities such as patient care.
The rationale for PDMP mandates is intuitive, and a recent study found that mandates that prescribers register for, or both register for and use, were associated with reductions in prescribing of Schedule II opioid analgesics in Medicaid [21]. However, the optimal frequency with which physicians should check PDMP patient reports is not known. In the current study, we found large differences in the time spent retrieving PDMP patient reports by usage case, and, for many physicians, the time saved by less frequent retrieval of PDMP patient reports will be used for clinical activities. Further, physicians may retrieve PDMP patient reports during uncompensated time, and a high burden of such administrative tasks is linked with decreased satisfaction and burnout [22,23]. Future research should delineate the optimal frequency of PDMP patient report retrieval, balancing time burden and the ability to detect high-risk medication use.
While we found that the delegate model is less costly than the physician model in most cases, the ability of delegates to access PDMP systems varies by state. As of December 2017, virtually all states authorize delegates to obtain PDMP patient reports under the supervision of physicians [14]. We estimated costs for an administrative staff member delegate (i.e., without a clinical license), and this scenario is possible in 70% (33/47) of states that have a statewide PDMP and authorize delegate access; the remaining states require delegates to have a clinical license (unpublished data, Prescription Drug Monitoring Program Training and Technical Assistance Center). A requirement that the delegate be clinically licensed, and therefore have a higher compensation, could reduce or negate the cost savings we found for the delegate model. To reduce the costs of PDMP use by delegates, physicians and health care systems can advocate that unlicensed delegates have PDMP access for the purposes of retrieving patient reports for physician review. Furthermore, because delegates do not generate revenue directly, health systems may not invest in them unless it can be shown that delegates will allow for greater throughput of visits by physicians.
In addition to the physician and delegate models described here, models of retrieving PDMP patient reports that harness the electronic health record (EHR) hold promise. In collaboration with the Substance Use and Mental Health Services Administration, the Office of the National Coordinator for Health Information Technology recently embarked on an initiative to explore integration of PDMP data into EHRs [24]. Through pilot studies in several states, this initiative found that EHRs could be successfully configured to automatically retrieve PDMP patient reports, triggered by events such as patient scheduling or e-prescribing, and directly integrate that information into the EHR field containing patients’ prescription history. While these were small-scale pilot projects typically involving one clinical site, they were accomplished with budgets of between $32,500 and $111,877, suggesting that even when scaled up, EHR-PDMP integration could cost health care systems less compared with physician or delegate retrieval of PDMP patient reports.
This study has limitations. First, our estimates rely on several assumptions, but where possible, we produced conservative estimates. For example, we assumed an optimal workflow for physicians when retrieving PDMP patient reports (i.e., batching of patients receiving continuing prescriptions). Therefore, we may have underestimated physician costs. In addition, our estimates for the time spent logging in and retrieving a PDMP patient report are averages and may not be generalizable to all physicians. Second, for health care system estimates, we could not extract specific data for every specialty from NAMCS. The “other medical and surgical specialties” category contains pain management, palliative care, and physical medicine and rehabilitation specialists who tend to have a high rate of controlled substance prescribing and therefore incur considerable costs. Thus, our cost estimates may not reflect costs for a health system consisting of more or fewer of these specialists compared with the fraction represented in NAMCS. Third, the most recent NAMCS prescribing data available at the time of this analysis was 2014; therefore our estimates may not reflect current prescribing. Fourth, due to NAMCS limitations, we may have overestimated the frequency of continuing prescriptions. Our sensitivity analysis suggests that health system costs may be lower than estimates from the main analysis. Fifth, we did not estimate costs for nurse practitioners or physicians’ assistants who prescribe controlled substances because data for these clinicians were not available in NAMCS; the ability to prescribe controlled substances also varies by state. Not including the costs experienced by these providers may underestimate health care system costs. Similarly, we did not estimate costs to pharmacists who may be mandated to retrieve a report, so our estimates do not reflect costs for health care systems with integrated pharmacy services.
Conclusions
While physicians view PDMP information as important for clinical care, retrieval of PDMP patient reports—a clerical function—can detract from other clinical activities or contribute to burnout. Alternative models employing delegates to retrieve reports reduce time burden to physicians and are less costly in most circumstances. Integration of PDMP information directly into EHRs is a promising model that may be less costly than relying on physicians or delegates. Physicians find value in the information obtained from PDMPs, clinical guidelines recommend routine use, and states increasingly mandate it. Therefore, physicians, health care systems, and state governments should work together to streamline PDMP access.
Authors’ Contributions
All contributors met authorship criteria.
Supplementary Data
Supplementary Data may be found online at http://painmedicine.oxfordjournals.org.
Supplementary Material
Funding sources: The research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health (K08DA043050 and P30DA040500). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosure and conflicts of interest: MAB: no conflict; BS: no conflict; ML: no conflict; JSM: no conflict; BCM: no conflict; DP: no conflict; NS: no conflict; SMM: no conflict.
Prior presentations: This work was presented in part at the 2017 Society of General Internal Medicine Annual Meeting, Washington, DC.
References
- 1. Perrone J, Nelson LS.. Medication reconciliation for controlled substances–an “ideal” prescription-drug monitoring program. N Engl J Med 2012;36625:2341–3. [DOI] [PubMed] [Google Scholar]
- 2. Prescription Drug Monitoring Program Training and Technical Assistance Center. Status of PMP’s. Available at: http://www.pdmpassist.org/pdf/pdmpstatustable.pdf (accessed August 2017).
- 3. Governor Eric Greitens announces statewide prescription drug monitoring program. Available at: https://governor.mo.gov/news/archive/governor-eric-greitens-announces-statewide-prescription-drug-monitoring-program (accessed August 2017).
- 4. Young HW 2nd, Tyndall JA, Cottler LB.. The current utilization and perceptions of prescription drug monitoring programs among emergency medicine providers in Florida. Int J Emerg Med 2017;101:16.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lin DH, Lucas E, Murimi IB, et al. Physician attitudes and experiences with Maryland’s prescription drug monitoring program (PDMP). Addiction 2017;1122:311–9. [DOI] [PubMed] [Google Scholar]
- 6. Irvine JM, Hallvik SE, Hildebran C, et al. Who uses a prescription drug monitoring program and how? Insights from a statewide survey of Oregon clinicians. J Pain 2014;157:747–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Blum CJ, Nelson LS, Hoffman RS.. A survey of physicians’ perspectives on the New York State Mandatory Prescription Monitoring Program (ISTOP). J Subst Abuse Treat 2016;70:35–43. [DOI] [PubMed] [Google Scholar]
- 8. Poon SJ, Greenwood-Ericksen MB, Gish RE, et al. Usability of the Massachusetts Prescription Drug Monitoring Program in the Emergency Department: A mixed-methods study. Acad Emerg Med 2016;234:406–14. [DOI] [PubMed] [Google Scholar]
- 9. Deyo RA, Irvine JM, Hallvik SE, et al. Leading a horse to water: Facilitating registration and use of a prescription drug monitoring program. Clin J Pain 2015;319:782–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fleming ML, Hatfield MD, Wattana MK, Todd KH.. Exploratory study of emergency physicians’ use of a prescription monitoring program using a framework of technology acceptance. J Pain Palliat Care Pharmacother 2014;281:19–27. [DOI] [PubMed] [Google Scholar]
- 11. Green TC, Zaller N, Rich J, Bowman S, Friedmann P.. Revisiting Paulozzi et al.’s “Prescription drug monitoring programs and death rates from drug overdose.” Pain Med 2011;126:982–5. [DOI] [PubMed] [Google Scholar]
- 12. Prescription Drug Monitoring Program Training and Technical Assistance Center. PDMP mandatory query by prescribers and dispensers. Available at: http://www.pdmpassist.org/pdf/Mandatory_Query_20171114.pdf (accessed December 2017).
- 13. Dowell D, Haegerich TM, Chou R.. CDC guideline for prescribing opioids for chronic pain–United States, 2016. JAMA 2016;31515:1624–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Prescription Drug Monitoring Program Training and Technical Assistance Center. PDMPs authorized and engaged in sending solicited and unsolicited reports to health care providers and patients. Available at: http://pdmpassist.org/pdf/Health_Care_Entity_Table_3.pdf (accessed August 2017).
- 15. Centers for Disease Control and Prevention. Ambulatory health care data. Available at: https://www.cdc.gov/nchs/ahcd/about_ahcd.htm (accessed August 2017).
- 16. US Department of Health and Human Services, Centers for Medicare and Medicaid Services. Medcare Provider Reimbursement Manual. Part 2, Provider Cost Reporting Forms and Instructions. Washington, DC: Centers for Medicare and Medicaid Services; 2011.
- 17. Bureau of Labor Statistics, United States Department of Labor. May 2015 occupation profiles. Available at: https://www.bls.gov/oes/2015/may/oes_stru.htm (accessed November 2016).
- 18. Peckham C. Medscape physician compensation report 2016. Available at: https://www.medscape.com/features/slideshow/compensation/2016/public/overview (accessed August 2017).
- 19. Hamblin J. What doctors make. The Atlantic. Available at: https://www.theatlantic.com/health/archive/2015/01/physician-salaries/384846/ (accessed August 2017).
- 20. Bureau of Labor Statistics, United States Department of Labor. Employer costs for employee compensation—September 2014. Available at: https://www.bls.gov/news.release/archives/ecec_12102014.pdf (accessed November 2016).
- 21. Wen H, Schackman BR, Aden B, Bao Y.. States with prescription drug monitoring mandates saw a reduction in opioids prescribed to medicaid enrollees. Health Aff 2017;364:733–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rao SK, Kimball AB, Lehrhoff SR, et al. The impact of administrative burden on academic physicians: Results of a Hospital-Wide Physician Survey. Acad Med 2017;922:237–43. [DOI] [PubMed] [Google Scholar]
- 23. Woolhandler S, Himmelstein DU.. Administrative work consumes one-sixth of U.S. physicians’ working hours and lowers their career satisfaction. Int J Health Serv 2014;444:635–42. [DOI] [PubMed] [Google Scholar]
- 24. HealthIT.gov. Connecting for impact: Linking potential prescription drug monitoring programs (PDMPs) to patient care using health IT. Available at: https://www.healthit.gov/PDMP (accessed August 2017).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.