Abstract
Abstract—As more low- and middle-income countries (LMICs) commit to universal health coverage (UHC), there is a growing need for rational priority setting using health technology assessment (HTA) and other policy tools. We describe an approach for rapidly mapping LMICs' capacity and needs for rational priority setting, aimed at identifying candidate countries where technical assistance would be most viable, and present our findings from applying this approach to three continents.
Drawing on the multiple streams theory and a conceptual model of HTA in health systems, we developed qualitative and quantitative indicators for political commitment, current position along UHC journey, institutional and technical capacity, health system financing characteristics, and potential economies of scale in rational priority setting and associated data collection tools. We additionally defined criteria for shortlisting countries, emphasizing feasibility of technical assistance. We purposively sampled 17 countries and gathered data up to May 2014 from various sources and applied the shortlisting criteria to these countries.
The four shortlisted countries (Indonesia, Myanmar, South Africa, Ghana) had varying capacities for rational priority setting and shared clear demand for rational priority setting as a means of achieving UHC. Indonesia was the strongest candidate for technical assistance, given the potential scale of impact on its large population and potential lessons for LMICs transitioning from aid. We conducted additional in-country scoping, and technical assistance to support HTA development in Indonesia is now underway.
Our approach is of potential value to development funders and initiatives seeking to maximize the impact of their aid investments in support of UHC.
Keywords: evidence-informed priority setting; health technology assessment, LMICs, resource allocation; universal coverage
INTRODUCTION
All health systems face the fundamental challenge of priority setting; that is, allocating finite health resources between competing purposes against infinite demand for health care.1 As more low- and middle-income countries (LMICs) commit to universal health coverage (UHC), health care budgets expand with policy makers' corresponding ambitions to maximize coverage and population health. Yet in the face of multiple priorities and lack of institutional mechanisms for setting explicit priorities in health, haphazard rationing occurs by default.1 This implicit priority setting, where it is unclear how or by whom health care spending decisions are being made, often results in low coverage of highly cost-effective interventions, overuse of cost-ineffective or inappropriate ones, inequitable coverage and access, and ultimately poor population health outcomes.1 In contrast, in rational priority setting the decision makers and the process are made explicit and transparent, and priority setting is done in a deliberative manner involving relevant stakeholders, in consideration of best available evidence about clinical and cost-effectiveness and social values. The “judicialization” of the right to health in many LMICs has arguably increased the need for rational priority-setting mechanisms, such as health technology assessment (HTA), to provide relevant guidance for courts of law.2
HTA is recognized as an essential foundation for achieving and sustaining UHC through the efficient and equitable allocation of health care resources.3,4 Global funders and development initiatives play an important role in supporting countries to strengthen their institutional capacity for establishing HTA systems.1 We define institutions not only as discrete structures but, more important, in terms of formal and informal rules, practices, and norms5 and institutional capacity as a broader “enabling environment” (potentially a network of institutions)6,7 for sustaining rational priority setting within the country. Motivated by such capacity needs, the international Decision Support Initiative (iDSI) was established in November 2013 as an international network bringing together priority-setting practitioners, academics, and think tanks, aimed at providing policy makers with demand-driven practical support1 in the shape of technical assistance to strengthen capacity through learning by doing. iDSI was asked by its funders to develop a process for prioritizing and selecting potential client countries.
There have been previous documented attempts to understand the development and use of HTA in LMICs. For example, Towse and colleagues8 put forward a model of HTA in health systems, exploring the interactions between health expenditure and the degree of its centralization as inputs and types of appraisal (for example, effectiveness versus cost-effectiveness) and breadth (for example, new technologies versus candidates for disinvestment) as outputs. This model was used to categorize HTA development in Brazil, China, and Taiwan8 and 12 other LMICs across sub-Saharan Africa (SSA), Asia Pacific (APAC), and Latin America and the Caribbean (LAC).9 Though the 12-country study identified some potentially useful forms of technical assistance in three in-depth case studies (South Africa, Kenya, and Vietnam),9 the model did not address in detail other issues of interest to iDSI, such as what institutional capacity building might look like or the potential policy impacts. Other frameworks and data collection tools that exist have also tended to focus on HTA's narrower, technical aspects,10 while relatively neglecting HTA beyond single technologies and the procedural and political aspects of rational priority setting, such as the deliberative processes that lie at its core.1 Better understanding of these broader issues could help iDSI and other development initiatives better target and maximize the impact of supporting priority-setting.
Aim and Objective
Our primary aim was to prioritize a shortlist of candidate partner countries for iDSI to provide practical strengthening for rational priority-setting capacity, where there would be the greatest likelihood of success within the two-year time frame of the iDSI grant. An intermediate objective was to develop and apply a framework for rapidly assessing LMICs' institutional and technical capacity for rational priority setting, the likely impact of practical support in the country and beyond, and the kinds of practical support that might have the most impact. In short, we shall describe a priority-setting process for iDSI itself.
METHOD
We identified three broad geographical regions in the world, LAC, SSA, and APAC, with a high concentration of LMICs. From these regions, we purposively sampled 17 countries with a broad mix of geographical representations, population sizes, and economic performance (including a mix of low-income countries [LICs] and middle-income countries [MICs]). The countries sampled were Brazil, Chile, Colombia, Mexico, Uruguay (LAC); Ghana, Kenya, Malawi, South Africa, Uganda (SSA); China, India, Indonesia, Myanmar, the Philippines, Thailand, and Vietnam (APAC).
Throughout framework development, data collection, and synthesis, we adopted a mixed-methods approach because no single set of quantitative or qualitative indicators could sufficiently capture the complexity of priority setting in any country.
Development of Conceptual Framework and Indicators
Taking Towse and colleagues'8 model of HTA as a starting point, we sought to develop a framework that would explicitly recognize priority setting as a political process,11 broaden the scope of analysis beyond HTA to include other rational priority-setting mechanisms relevant to countries on the UHC journey (including clinical guidelines and health benefits plans), and focus the analysis on potential ways of and outcomes of supporting improved priority-setting processes.
Establishing rational priority-setting processes lies in the realm of political decision making. Our approach for mapping the political context drew on Kingdon and Thurber's multiple streams theory (MST).12 MST is particularly useful in explaining how certain issues become policy issues through the opening of “policy windows.” The three streams (problem, politics, and policy) that combine to create policy windows are seen as independent and difficult to predict. The MST framework's main assumption is that policy makers can only give limited time and attention to policy issues, so particular issues will not make it on to the policy agenda, regardless of the push from policy entrepreneurs. This, in turn, has implications for the policy stream, which has been referred to as a “primeval soup” of ideas generated by policy experts. However, the MST posits that ideas must meet a number of criteria (such as technical feasibility, value acceptability, and resource adequacy) in order to make it on to the policy agenda and be potentially implementable.13 The MST framework was used in predictive models for specific health policies such as nutrition security14 and maternal health,15 as well as in retrospective policy analysis,16 and so was particularly suited for the rapid mapping of the priority-setting potential in our chosen countries.
Development of Qualitative and Quantitative Indicators
Reflecting on these frameworks within the context of iDSI's collective experience of engaging with LMICs, we proposed a range of factors that might determine whether efforts to support institutionalization of rational priority setting would be successful. After consultation with iDSI delivery partners (NICE International, Office of Health Economics, the Health Intervention and Technology Assessment Program (HITAP), Center for Global Development, University of York Centre of Health Economics, and Imperial College London), the final qualitative indicators were political commitment to rational priority setting, current position along the UHC journey, institutional and technical capacity for rational priority setting, health system financing characteristics, and potential economies of scale in rational priority setting (Table 1).
Table 1.
Factors Used for the Rapid Assessment of Priority Setting and How These Map Out onto Kingdon and Thurber's12 MST. MST, multiple streams theory; NICE, National Institute for Health and Care Excellence; HITAP, Health Intervention and Technology Assessment Program
| Politics Stream | Policy Stream | Problem Stream |
|---|---|---|
| 1. Political commitmentNational health strategyCentralization of policy-making power | 3. InstitutionsInstitutional capacity for explicit prioritysetting (policy-making and technical levels)Governance in health resources allocation | 2. Current position on UHC journeyAccess and qualityFinancial protection and distributionalissues |
| |
4. Health system financingFinancial sustainability of the health systemPresence of other donors/developmentagencies |
|
| Policy Entrepreneurs5. Economies of scale (iDSI related)Geographic scope Existing support from NICE and HITAP | ||
We also proposed a set of accompanying quantitative indicators, through deliberative discussions between the authors (RL, KHV, AT, and KC). An extensive set of indicators was initially considered, and the final selection reflected what we judged to be a sufficiently sensitive set of indicators that would allow for a manageable analysis with reasonably strong conclusions, within the time constraints (Table 2).
Table 2.
Quantitative Factors and Indicators Used in the Rapid Assessment of Priority Setting (Continued)
| Political will and influence | |
|---|---|
| National health strategy calls for rational priority setting and HTA |
Sponsor of World Health Assembly Resolution on “Health Interventions and Technology Assessment in Support of Universal Health Coverage” |
|
Potential to benefit given current position along the UHC journey | |
| Health indicators of current position along the UHC journey | Millennium Development Goals IndicatorsProportion of one-year-old children immunized against measles29,30 Proportion of births attended by skilled health personnela,23 Maternal mortality ratiob,23 NCD Indicators Prevalence of smoking in adults (females and males)c,29 Percentage of all NCD deaths occurring under age of 70 (females and males).31 Effective cervical cancer screening coverage for women32 |
| General availability of breastd/bowele cancer screening at the primary health care level33 Probability of premature death from cardiovascular disease, cancer, diabetes, and chronic respiratory diseasef,34 | |
| Financial protection and distributional issues |
Gini coefficientg,23 Out-of-pocket expenditure as percentage of total health expenditureh,23 Incidence of catastrophic health expenditure due to out-of-pocket paymentsi,35 |
|
Institutions | |
| Identified institutional capacity for priority setting at policy maker level | Presence of essential drugs lists36 Presence of national clinical guidelines: National treatment guidelines for adult and pediatric treatment of HIV (year of the first record in the AIDSTAR-One database)37 Standard treatment guidelines, national and regional osteoporosis guidelines (year of the first record in the International Osteoporosis Foundation database)38 Political stability and absence of violence/terrorism (2012)j,39 |
| Identified institutional capacity for priority setting at technical level | Researchers, headcounts/million population (2012)k,40 QS World University Rankings, average score top three (2012)l,40University/industry research collaboration (2012)m,40 Statistical capacity scientific and technical journal articles (per 100,000 people) (2009)n,41Scientific and technical journal articles (per 100,000 people) (2009)o,23 |
| Governance in health resource allocation | Corruption perception indexp,42Government effectiveness (2012)q,39Performance of grants by component: tuberculosis, malaria, and HIVr |
|
Health system financing | |
| Financial sustainability of the health system, considering projected growth and government spending | Growth in health expenditure per capita (estimation based on the World Bank data regarding health expenditure per capita23)Public expenditure as percentage of total health expenditures,23 |
| Significant presence of other donors/development agencies in health care | Disbursements to recipient countries for health (per capita, constant 2009 USD)t,43 External resources as percentage of total health expenditure (2011)u,44 |
HTA = health technology assessment, UHC = universal health coverage, NCDs = noncommunicable diseases.
Percentage of deliveries attended by personnel trained to give the necessary supervision, care, and advice to women during pregnancy, labor, and the postpartum period; to conduct deliveries on their own; and to care for newborns.23
Maternal mortality ratio is the number of women who die during pregnancy and childbirth, per 100,000 live births. The data are estimated with a regression model using information on fertility, birth attendants, and HIV prevalence.23
Prevalence of smoking any tobacco product among adults aged ≥15 years (%): Smoking of any form of tobacco, including cigarettes, cigars, pipes, bidis, etc., and excluding smokeless tobacco. Age-standardized prevalence rates for smoking tobacco.29
Whether the country has breast cancer screening (by palpation or mammogram) generally available at the primary health care level.33
Whether the country has bowel cancer screening (by digital exam or colonoscopy) generally available at the primary health care level.33
Percentage of 30-year-old people who would die before their 70th birthday from any of cardiovascular disease, cancer, diabetes, or chronic respiratory disease, assuming that she or he would experience current mortality rates at every age and she or he would not die from any other cause of death (e.g., injuries or HIV/AIDS).34
The Gini index measures the extent to which the distribution of income or consumption expenditure among individuals or households within an economy deviates from a perfectly equal distribution. A Gini index of 0 represents perfect equality, and an index of 100 represents perfect inequality.23
Any direct outlay by households, including gratuities and in-kind payments, to health practitioners and suppliers of pharmaceuticals, therapeutic appliances, and other goods and services whose primary intent is to contribute to the restoration or enhancement of the health status of individuals or population groups23
The measure of financial burden and catastrophic health expenditure from out-of-pocket expenditure is based on the concept of health spending relative to household nonsubsistence expenditure (or household capacity to pay). The latter was defined on the basis on food expenditure, whereby all household expenditure exceeding a particular food expenditure threshold was considered to be nonsubsistence expenditure. Out-of-pocket expenditure is presented as a share of household capacity to pay. Additionally, a household is defined as facing catastrophic health expenditure if its health spending exceeds 40% of its capacity to pay.35
Reflects perceptions of the likelihood that the government will be destabilized or overthrown by unconstitutional or violent means, including politically motivated violence and terrorism. Estimate of governance ranges from approximately −2.5 (weak governance performance) to +2.5 (strong governance performance).39
Researchers per million population, headcounts. Researchers in research and development are professionals engaged in the conception or creation of new knowledge, products, processes, methods, or systems and in the management of the projects concerned. Postgraduate PhD students (International Standard Classification of Education, 1997, level 6) engaged in research and development are included.40
Average score of the top three universities at the QS world university ranking per country. If fewer than three universities are listed in the QS ranking of the global top 700 universities, the sum of the scores of the listed universities is divided by three, thus implying a score of zero for the nonlisted universities40
Average answer to the survey question: To what extent do business and universities collaborate on research and development in your country? (1 = do not collaborate at all; 7 = collaborate extensively).40
Statistical capacity indicator provides an overview of the statistical capacity of developing countries. It is based on a diagnostic framework developed with a view to assessing the capacity of statistical systems. The framework consists of three assessment areas: methodology, data sources, and periodicity and timeliness (institutional framework has not been included in score calculation).41
Scientific and technical journal articles refer to the number of scientific and engineering articles published in the following fields: physics, biology, chemistry, mathematics, clinical medicine, biomedical research, engineering and technology, and earth and space sciences.23
The Corruption Perceptions Index ranks countries and territories based on how corrupt their public sector is perceived to be. A country or territory's score indicates the perceived level of public sector corruption on a scale of 0–100, where 0 means that a country is perceived as highly corrupt and 100 means that it is perceived as very clean.42
Reflects perceptions of the quality of public services, the quality of the civil service and the degree of its independence from political pressures, the quality of policy formulation and implementation, and the credibility of the government's commitment to such policies. Ranges from approximately −2.5 (weak governance performance) to +2.5 (strong governance performance).39
Based on The Global Fund database. The grant portfolio includes more than 1,000 programs across more than 140 countries. Grants are measured and rated against country-owned targets at each periodic disbursement of funding. Only in the case of Chile are there no registered programs related to HIV, tuberculosis, and/or malaria,45
Public health expenditure consists of recurrent and capital spending from government (central and local) budgets, external borrowings and grants (including donations from international agencies and nongovernmental organizations), and social (or compulsory) health insurance funds. Total health expenditure is the sum of public and private health expenditure. It covers the provision of health services (preventive and curative), family planning activities, nutrition activities, and emergency aid designated for health but does not include provision of water and sanitation.23
The amount of disbursements of official development assistance for health, from donor(s) to recipient(s). A disbursement is the release of funds to or the purchase of goods or services for a recipient and, by extension, the amount thus spent. Disbursements record the actual international transfer of financial resources or of goods or services valued at the cost to the donor.43
External resources for health are funds or services in kind that are provided by entities not part of the country in question. The resources may come from international organizations, other countries through bilateral arrangements, or foreign nongovernmental organizations. These resources are part of total health expenditure.45
We neither set out to weight the indicators nor to consider factors in isolation. Rather, taken together, the qualitative and quantitative indicators were hoped to reveal a richer overview of what a policy window for supporting rational priority setting might look like in each country.
Political Commitment
Pertaining to the politics stream, political commitment could provide clear entry points through which rational priority setting can add value. Institutional commitment 14,17 clearly articulated in high-level policy documents was sought, specifically whether the national health strategy calls for rational priority setting and HTA. The existence of a centralized HTA institution would be an even stronger signal of institutional and budgetary commitment to rational priority setting.14,17
It was equally important to understand the existing rules of political decision making in the national context, particularly referring to governance structures (unitary, federal) and processes (pluralist, corporatist, statist).18 Rational priority setting should be easier to implement in countries with a robust central government and with a centralization of policy-making power, and this might be closely correlated with centralization of health care budget allocation.8
Current Position on the UHC Journey
The problem stream level constituted relevant indicators that shed light on the size of the policy problem. In this case, the stream refers to the health system and the stage of its development toward UHC: health indicators of current position along the UHC journey—for example, access and quality of health services—on the one hand and financial protection and redistribution of wealth on the other. Health systems more advanced on the road toward UHC are more likely to have identified the need for rational priority setting, and each system's progress from predominantly out-of-pocket financing mechanisms toward UHC tends to coincide with the development of HTA systems.8 On the flip side, health systems at earlier stages might be expected to have an even greater need for HTA, being relatively underresourced and highly inequitable. Those with a high incidence of catastrophic payments might be expected particularly to benefit from rational priority-setting processes.
Institutional Capacity
Pertaining to the policy stream level, institutional capacity at the policy-maker level refers to the acceptability of rational priority setting as a policy solution among high-level policy makers, in countries where rational priority setting and HTA was not yet formalized. Both personal and architectural capacity is needed, as is political stability; factors that influence the politics stream, such as general elections or other reasons for expected turnover of policy makers, could disrupt efforts to make priority-setting processes more rational.
The policy stream also refers to technical feasibility and resources adequacy. Here, institutional capacity at the technical level refers to advisory bodies and academic and research institutions that support technical aspects of rational priority setting (for example, health economics analyses, education, and training). Although resource adequacy was difficult to estimate for an institutional process such as priority setting, we approached the issue by linking it with governance in resource allocation. The assumption for doing so was that perceived corruption (from policy maker to clinician levels) and the waste in resources it causes could highlight a need to formalize priority-setting processes, thus providing rational incentive structures and ultimately improving health system governance.
Health System Financing
The fourth factor also pertained to the policy stream, specifically to resource adequacy within the health system. Firstly, the mapping would assess the financial sustainability of the health system, considering projected growth and government spending. Health systems that are primarily government funded (with highly centralized spending) are more amenable to the successful introduction of rational priority setting, because the dominant payer is incentivized to make the most efficient use of its resources for improving population health, compared to fragmented health systems, where it may be unclear who pays for priority setting.8 Rational priority-setting processes can make the health system more sustainable by either identifying opportunities for disinvestment (where health baskets include clinically suboptimal and/or financially unsustainable interventions) or by maximizing gains from investments (where increases in health expenditure are linked to commitments to UHC), again varying depending on the current level of expenditure.8
A key issue related to resource adequacy at the health system level was the presence of other donors/development agencies. We assumed a trade-off between the opportunity of donors as an entry point for rational priority setting (for example, the opportunity to influence or to coordinate donor-driven vertical health spending) and the challenge of competing with other donors or development initiatives for policy makers' attention and resources.
Economies of Scale
The policy entrepreneur stream referred to iDSI and its access, resources, and strategy in each country. The geographic scope of the project was important, given that the introduction of rational priority-setting processes could be beneficial for countries with geographical proximity and/or similar socioeconomic situations; for instance, through the sharing of methods, models, or data on disease burden, clinical effectiveness, and costing.19 Further, if the candidate country had political, economic, or cultural influence within their geographic region or otherwise sociopolitically similar countries, awareness about rational priority setting might be transferrable across countries. Finally, existing support for rational priority setting from NICE International and HITAP should be capitalized on, in terms of both technical institutional capacity and existing links with policy actors.
Development of Data Collection Tools
Standardized Questionnaire
Designed to capture some of the qualitative indicators identified in Table 1, including political commitment, potential gains and economies of scale, and capacity for development and implementation of rational priority-setting tools (Appendix 1). Questionnaire development was informed by an earlier questionnaire about HTA use in Vietnam, which was used during a technical workshop in Hanoi.10 The current questionnaire was designed for self-completion by individuals with a good understanding of the country's priority-setting landscape, though it could also be used as part of a semistructured interview. The questionnaire was field-tested with 20 delegates from various African countries during a supervised session at the African Health Economics and Policy Association conference in 201420 and then adopted in its current form.
Semistructured Interview Guide
Designed to help iDSI delivery partners capture more in-depth qualitative data on rational priority setting around the key descriptive factors set out in Table 1, through semistructured interviews with key stakeholders or opinion leaders (Appendix 2). This included guidance for the interviewer when leading an open discussion, with ten suggested questions designed to capture three main themes of supply-side, demand-side, and potential impact of rational priority setting.
Standard Reporting Template
Designed to ensure that iDSI delivery partners had consistent synthesized data for each country (Appendix 3), the template included the following headings with guidance questions: overview of the country's health system landscape, demand side of priority setting, supply side of priority setting, potential impact of rational priority setting, and conclusions (potential options for iDSI practical support activities). A completed template for India was shown to iDSI delivery partners as an example.
Development of Shortlisting Criteria
We sought exclusion criteria that would most directly address our aim of selecting a shortlist of potential client countries for iDSI practical support, emphasizing feasibility and the strategic priorities of iDSI and its funders. Through discussion with iDSI delivery partners, we agreed that the criteria should eliminate the greatest possible number of countries, given that iDSI only had sufficient resources to support one country. The agreed exclusion criteria were as follows:
The presence of an existing, centralized priority-setting institution: iDSI support should be prioritized in countries that do not already have rational priority-setting mechanisms at a national level.
No expressed political commitment to UHC: UHC is a primary motivating factor for rational priority setting and a strategic goal for one iDSI funder (Rockefeller Foundation).
No existing engagement with NICE International and HITAP or engagement unlikely to be feasible for other reasons: Given the short time frame of practical support, success would be most likely where iDSI had existing relationships with key political and technical champions and where our links and their policy influence was likely to remain stable in the short term.
Data Collection and Synthesis
We assigned each of the 17 sampled countries to an iDSI delivery partner, who gathered qualitative data for each given country following the standard reporting template (Appendix 3). iDSI partners collected and synthesized data from January through May 2014 from various sources, including selective review of published and unpublished academic and gray literature, supplemented with personal communications with key stakeholders or opinion leaders, both informal and formal (including questionnaires and semistructured interviews). We placed no other restrictions on data sources or identification of questionnaire or interview respondents. Three authors (KHV, AT, and RL) collected and synthesized the quantitative data from public data sets.
Shortlisting Process
We applied the shortlisting criteria and sought expressions of interest from relevant senior policy makers or policy advisers in the shortlisted countries. In June 2014, we presented the mapping findings to the iDSI Steering Group, who made the final decision on the partner country for iDSI practical support.
RESULTS
Complete findings of the mapping are reported in detail elsewhere.21 We present the following key findings of direct relevance to the study objectives of prioritizing iDSI practical support countries.
Descriptive Data
General characteristics of the 17 sampled countries are shown in Table 3. There were four LICs, of which three were in SSA (Kenya, Malawi, Uganda) and the fourth was in APAC (Myanmar). Two countries, both in LAC, had recently made the transition into high-income countries (Chile and Uruguay). The remaining 11 countries were all MICs.
Table 3.
General Characteristics of Sampled Countries
| Region |
Country (Classification by Income)a |
Population in Millions (2012) |
Gross Domestic Product per Capita (Current USD) (2013) |
Health Expenditure per Capita (Current USD) (2011) |
Cause of Death by Communicable Diseasesb (% of Total) (2008) |
Infant Mortality Ratec (2008) |
Life Expectancy at Birth, Female (Years) (2011) |
Life Expectancy at Birth, Male (Years) (2011) |
| Latin America and the Caribbean | Brazil (UMI) | 198.66 | 11,340 | 1,120.6 | 14 | 14 | 77 | 70 |
| Chile (HI) | 17.46 | 15,452 | 1,074.5 | 9 | 8 | 82 | 76 | |
| Colombia (UMI) | 47.70 | 7,748 | 432.0 | 13 | 15 | 77 | 70 | |
| Mexico (UMI) | 120.85 | 9,749 | 619.6 | 12 | 13 | 79 | 75 | |
| Uruguay (HI) | 3.40 | 14,703 | 1,104.9 | 8 | 9 | 80 | 73 | |
| Sub-Saharan Africa | Ghana (LMI) | 25.37 | 1,605 | 75.0 | 53 | 3 | 62 | 60 |
| Kenya (LI) | 43.18 | 943 | 36.2 | 63 | 48 | 62 | 59 | |
| Malawi (LI) | 15.91 | 268 | 30.9 | 63 | 53 | 54 | 54 | |
| South Africa (UMI) | 52.27 | 7,508 | 689.3 | 67 | 35 | 57 | 53 | |
| Uganda (LI) | 36.35 | 547 | 42.4 | 65 | 58 | 59 | 57 | |
| Asia Pacific | China (UMI) | 1,350.70 | 6,091 | 278.0 | 7 | 13 | 76 | 74 |
| India (LMI) | 1,236.69 | 1,489 | 59.1 | 37 | 47 | 68 | 64 | |
| Indonesia (LMI) | 246.86 | 3,557 | 95.0 | 28 | 25 | 72 | 68 | |
| Myanmar (LI) | 52.80 | 1,144 | 22.5 | 33 | 48 | 67 | 63 | |
| The Philippines (LMI) | 96.71 | 2,587 | 96.5 | 31 | 20 | 72 | 65 | |
| Thailand (UMI) | 66.79 | 5,480 | 201.8 | 17 | 11 | 77 | 71 | |
| Vietnam (LMI) | 88.77 | 1,755 | 94.8 | 16 | 17 | 80 | 71 |
UMI = upper-middle-income economies (4,086 USD to 12,615 USD), HI = high-income economies (12,616 USD or more), LMI = lower-middle-income economies (1,036 USD to 4,085 USD), LI = low-income economies (1,035 USD or less).
Country groups by income according with The World Bank classification24: The split is based on 2012 gross national income per capita.
Cause of death by communicable diseases and maternal, prenatal, and nutritional conditions.
Probability of dying by age one per 1,000 live births.
Source: Data extracted from data.worldbank.org.24 The gross domestic product for Myanmar was extracted from data.un.org.46
Synthesis of Quantitative and Qualitative Findings
Political Commitment
The countries could be categorized into three groups with respect to rational priority setting1: clearly established and centralized HTA institutions at different levels of maturity (Brazil, Chile, Colombia, Mexico, Uruguay, China, Thailand, the Philippines, Vietnam),2 HTA applied on an unstructured or informal basis (South Africa, India, Indonesia, Myanmar),3 and no contribution of HTA to priority setting (Ghana, Kenya, Malawi, Uganda). Countries in the second group, three of which (South Africa, Indonesia, Myanmar) had expressed commitment to rational priority setting through sponsorship of the World Health Assembly Resolution on “Health Interventions and Technology Assessment in Support of Universal Health Coverage,”4 could benefit from consolidation and institutionalization of existing priority-setting activities and technical capacity within the broader UHC context.
Current Position on UHC Journey
All 17 countries showed political commitment to UHC (with stated timelines for UHC in many national health strategies), and most SSA and APAC countries faced current challenges in at least one health indicator for Millennium Development Goals or noncommunicable diseases (NCDs). For example, all SSA countries and three APAC countries (India, Indonesia, Myanmar) had maternal mortality ratios above 200 per 100,000 live births; Ghana and Indonesia both had high proportions of NCD deaths, and both had low coverage of cancer screening. Such countries could benefit from rational priority-setting mechanisms to ensure that higher quality health care reached the most vulnerable population groups.
Health System Financing
Seven countries had experienced dramatic growth more than doubling between 2006 and 2011 in total health expenditure (Brazil, Uruguay, China, Indonesia, Myanmar, the Philippines, Vietnam) and presented clear needs for rational priority setting. External donors accounted for high proportions of expenditure in all SSA countries except South Africa and Myanmar. In Ghana, public health expenditure accounted for a high proportion (56%), due to a generous national health insurance scheme, whereas in South Africa, a relatively low proportion of out-of-pocket expenditure masked a highly unequal health system where total health expenditure was driven by private health insurance of the wealthiest quintile.
Shortlisting Process
We identified four countries for a potential iDSI practical support project: Indonesia, Myanmar, Ghana, and South Africa (Figure 1).
Figure 1.
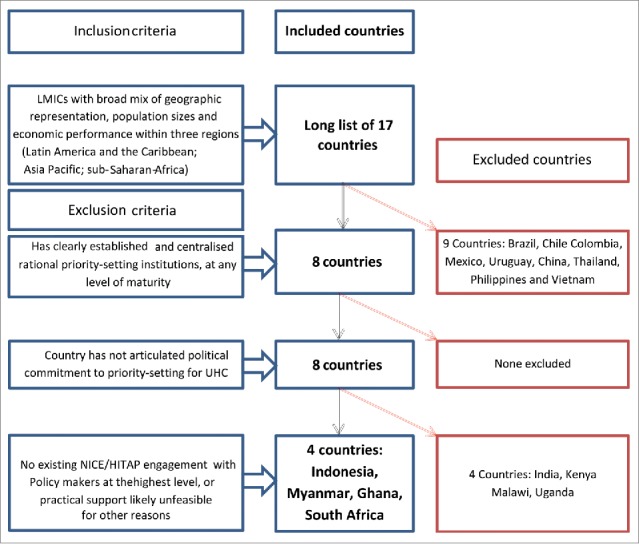
Flow of Country Shortlisting Process
From the 17 sampled countries, we excluded the nine that had already established formal HTA institutions, including all LAC countries and four Asian countries (Thailand, China, the Philippines, and Vietnam). We further excluded four countries based on low feasibility during the time frame of the iDSI practical support project, including Kenya, Malawi, and Uganda, where iDSI had no existing links with senior policy makers. India was excluded because the formation of a new central government in May 2014 meant that the existence of a policy window for iDSI was unclear at the time. In all four remaining shortlisted countries, Indonesia, Myanmar, Ghana, and South Africa, iDSI practical support was likely to succeed during the grant time frame, receive political backing, and add value in terms of within- or cross-country impact.
Indonesia
Indonesia is an MIC that has enjoyed dramatic economic growth in recent years, with a negative consequence that NCDs have now surpassed communicable diseases as major causes of death. Indonesia was concurrently transitioning from Gavi support and will eventually have to pay for its own immunization coverage. In the face of growing domestic demand for quality health care and decreasing external aid, the government of Indonesia is committed to introducing a single national health insurance program for its 250 million citizens by 2019.
iDSI has engaged in preliminary discussions with senior Ministry of Health (MoH) members and the World Health Organization Country Office since early 2012. iDSI could build on this early engagement to strengthen institutional and technical capacity for HTA, in collaboration with aforementioned stakeholders and other development partners that have been active in Indonesia, including PATH, the Australian Agency for International Development, and the United States Agency for International Development. This could generate important lessons for other upper-MICs transitioning from foreign aid and potentially other Islamic nations on the UHC journey. The MoH has expressed interest in further cooperation with NICE International and its partners: “It is the right time [for technical assistance] since we are building an HTA organization in our office” (personal communication with Professor Akmal Taher, Director General of Health Care, MoH, Indonesia, May 2014).
Myanmar
Myanmar has had the lowest per capita government spending on health in the world (less than 1.8% of gross domestic product in 2012), with high rates of impoverishment from private health care, inequitable access, and overall poor care. The MoH is committed to introducing UHC by 2035, and government expenditure in health has doubled over the past few years.22 Myanmar also had significant and increasing donor-led health care investments following recent political and economic reforms, and it was thought that the MoH could benefit greatly from introducing rational priority-setting mechanisms for coordinating and prioritizing international support alongside its own investments for sustainable UHC.
HITAP has engaged significantly in Myanmar with Gavi and the World Health Organization in maternal and child health, and the Three Millennium Development Goals Fund Coordination Group has expressed an interest in iDSI support. Practical support could include supporting the development of a rational health benefits plan using HTA and adapting evidence-based clinical guidelines in high-priority disease areas. Both components would involve learning by doing through collaboration with local policy makers, clinicians, and academics. From a low baseline, the potential positive impact on the population health of Myanmar could be substantial. The lessons could also be transferrable to other LIC settings with strong donor presence and growing political commitment toward UHC. The MoH of Myanmar recognized the considerable challenges facing evidence-based policy making, and were “looking forward to [collaboration] with HITAP and NICE International” (personal communication with Dr. San San Aye, Director (Planning), Department of Health and Planning, MoH, Myanmar, May 2014).
South Africa
South Africa has the world's highest Gini coefficient23 and a similarly inequitable fragmented health system, with 20% of the population accounting for 80% of total expenditure. South Africa also faces a quadruple burden of HIV and tuberculosis, maternal and child mortality, NCDs, and injury and violence.24 In this context, the government aims to reach a single, predominately public national health insurance scheme by 2025 with the goal of UHC. There is tremendous need for more explicit and coordinated priority-setting mechanisms, with equity and sustainability as core objectives.
Priority setting (including limited aspects of HTA) at the central government level currently occurs within three separate committees for essential medicines, pricing, and essential equipment. South Africa is relatively advanced among SSA countries, with strong academic track records in health economics-focused programs in the University of Cape Town, and PRICELESS SA, at the University of the Witwatersrand, which has provided support to the National Department of Health (NDoH). A major challenge for the NDoH will be to coordinate and integrate priority-setting efforts and capacity, driving economies of scale across both public and private sectors.25
Building on a longstanding memorandum of understanding and ministerial engagements between NDoH and NICE, future iDSI practical support could focus on a South African regional hub to convene and consolidate existing capacity, with the potential to influence neighboring SSA countries and provide learning for other UHC-committed upper-MICs grappling with inequity. The NDoH recognized “an urgent need for international collaboration both between MICs as peers as well as the more advanced economies so as to ensure that we maximise the effectiveness of our available resources” (questionnaire response from Gavin Steele, Chief Director, NDoH, April 2014).
Ghana
Since 2003, Ghana has implemented a national health insurance scheme for basic health care, now covering 36% of the population. However, a generous benefits package with no explicit positive or negative list has meant high pharmaceutical expenditures, and there are genuine concerns about national health insurance scheme affordability and sustainability. In addition, MoH-produced, stakeholder-led clinical guidelines have not been consistently implemented. There were gaps in technical capacity, with only a small number of health economists in universities, and around data availability.
Major health care reforms were now under way, including new provider payment mechanisms (moving toward capitation) and the development of clinical guidelines. iDSI could leverage this momentum through NICE International's ongoing engagement with the MoH and the National Health Insurance Agency and strong links with the UK Department for International Development (DFID) in Ghana, the Rockefeller Foundation, and the World Bank regional office. Practical support could aim at introducing rational mechanisms for listing decisions and quality standards for provider payment. This could help the MoH improve quality and contain costs, through inclusive and evidence-informed processes, and provide transferrable experiences for other SSA countries. With Ghana's strong institutions in health care purchasing and provision, “working with iDSI would complement and strengthen policy makers' existing efforts in using evidence and social values… making decisions better and more defensible” (personal communication with Patricio V. Marquez, Lead Health Specialist, World Bank Africa Region, May 2014).
Final Country Selection
In June 2014, the iDSI Steering Group reviewed the rapid mapping and chose Indonesia as iDSI's target country, subject to further detailed in-country scoping. The main reasons for choosing Indonesia were its greater population and potential generalizability, in comparison with South Africa for instance whose fragmented health system could limit the generalizability of iDSI's work. HITAP completed this scoping through a stakeholder workshop in Jakarta, in conjunction with PATH. The scoping report confirmed and expanded upon the findings from our initial mapping of Indonesia and in July 2014 the iDSI Steering Group approved the decision to initiate practical support. This has been in progress since August 2014, to convene in-country stakeholders and external donors in the HTA policy process and to develop technical capacity through three demonstration analyses.26
DISCUSSION
The current study represents the first effort to propose a comprehensive framework and practical tools and indicators (both qualitative and quantitative) for rapidly assessing countries' national landscapes of priority setting in health, incorporating all relevant considerations such as institutional and technical capacity for HTA and other priority-setting mechanisms (such as health benefits plans), in the overarching context of rational priority setting for UHC. Through applying the framework to 17 countries on three continents, we have achieved our aim of identifying strong candidate countries for and the nature of iDSI technical assistance, while providing a baseline assessment of countries' gaps and needs that could be tracked in future. The mapping was completed relatively quickly (in five months) primarily through desk-based activities and could usefully inform iDSI's ongoing priority setting, and potentially also that of other development funders and initiatives interested in supporting priority setting.
Our four shortlisted countries varied in terms of economic performance, with one LIC (Myanmar), two lower-MICs (Indonesia and Ghana), and one upper-MIC (South Africa). All four were working at UHC and at different stages of the journey, but respective policy makers shared a common vision of increasing the role of public financing and provision of health care. They also recognized rational priority setting as crucial to sustaining access to high-quality, equitable care. In all four countries, we identified significant economies of scale that could be generated from iDSI support in capacity building either regionally or across other jurisdictions with similar socioeconomic or cultural contexts.
The four countries had different levels of capacity for rational priority setting and thus different needs and potential benefits from iDSI support. Ghana had relatively strong institutions and needed to focus on strengthening technical and data capacity. South Africa had potential technical capacity that would need to be consolidated and institutionalized among different private and public sector stakeholders. Myanmar would require extensive support in building capacity, but the marginal gains from strengthened priority setting could be substantial both in this country given the “blank slate” of the health system and potential important lessons for other LICs, a group of countries that have received relatively less attention in terms of international support for rational priority setting. Finally, Indonesia has been moving rapidly in order to realize its vision of UHC by 2019 and had a pressing need to build upon existing institutional and technical capacity for rational priority setting. Indonesia was chosen as the country for iDSI practical support, and progress is being made.
Limitations
Our study did not employ systematic literature reviews or formal qualitative synthesis methods, and findings might have been subject to authors' as well as interviewees' biases. The initial selection of 17 countries was purposive rather than systematic, and this could have introduced its own biases, especially given that LICs formed a minority of our sample. We tried to minimize biases through the use of standard data collection and reporting templates, and given limited time and resources to map a large number of countries, our pragmatic approach generated findings that turned out useful for achieving our goal of identifying an iDSI partner country. The in-country scoping of Indonesia corroborated the findings of our initial mapping.
The indicators varied in their sensitivity and specificity in relation to rational priority setting. For example, the presence or absence of an essential drugs list does not in itself denote whether such lists were developed or implemented through a deliberative process that considers cost-effectiveness. Our UHC indicators were static and would not have captured progress toward UHC objectives over time. Acknowledging the trade-off between simple, easily quantifiable indicators versus rich descriptive indicators that would be harder to measure,27 we drew conclusions from quantitative indicators in conjunction with detailed qualitative findings from stakeholder interviews and relevant literature.
Despite being founded on existing models for HTA development and policy, many of our proposed indicators remain to be empirically validated, and further research is needed to develop and assess predictors of success of priority-setting institutions in countries moving toward UHC. iDSI and its partners have now begun to address some of these research questions.27,28
CONCLUSIONS
We achieved our objectives of developing and applying a framework and rapid approach to mapping priority setting in LMICs and of identifying a shortlist of strong candidate countries for iDSI technical assistance. The findings were gathered fairly quickly and strengthened by in-country scoping of the final candidate country, Indonesia, where significant progress has been made through our practical support. Our approach was useful for iDSI's own priority setting and also of potential value to other development funders and initiatives seeking to maximize the impact of their aid investments.a[a]
DISCLOSURE OF POTENTIAL CONFLICTS OF INTEREST
No potential conflict of interest was reported by the authors.
Footnotes
Please find Appendix 1 at http://www.idsihealth.org/knowledge_base/idsi-priority-setting-questionnaire-v1-0/, Appendix 2 at pp. 108–109 (Annex 3) of ref. 21, and Appendix 3 at p. 101 (Annex 1) of ref. 21.
Acknowledgments
We are grateful to the following individuals for their contributions: Paul Barnsley, Francoise Cluzeau, Derek Cutler, Lou Garrison, Ursula Gideion, Amanda Glassman, Kate McQueston, Dominic Nkhoma, Tran Thi Mai Oanh, Natalie Phaholyothin, Moriah Pollock-Hawthorne, Paul Revill, Francis Ruiz, Yot Teerawattananon, and Nattha Tritasavit.
NOTE
Funding
This study was funded by the Department for International Development, the Bill and Melinda Gates Foundation, and the Rockefeller Foundation under the international Decision Support Initiative.
REFERENCES
- [1].Glassman A, Chalkidou K. Priority-setting institutions in health. Building institutions for smarter public spending. Washington, DC: Center for Global Development; 2012. [DOI] [PubMed] [Google Scholar]
- [2].Dittrich R, Cubillos L, Gostin L, Chalkidou K, Li R. The international right to health: what does it mean in legal practice and how can it affect priority setting for universal health coverage? Health Sys Ref, this issue. [DOI] [PubMed] [Google Scholar]
- [3].Chalkidou K, Marten R, Cutler D, Culyer T, Smith R, Teerawattananon Y, Cluzeau F, Li R, Sullivan R, Huang Y, et al.. Health technology assessment in universal health coverage. Lancet 2013; 382(9910): e48-e49. [DOI] [PubMed] [Google Scholar]
- [4].World Health Organization Sixty-seventh World Health Assembly. WHA67.23. Agenda item 15.7. 24 May 2014 Health intervention and technology assessment in support of universal health coverage. Geneva: World Health Organization; 2014. Available at http://apps.who.int/gb/ebwha/pdf_files/WHA67/A67_R23-en.pdf?ua=1 [Google Scholar]
- [5].Keohane R. International institutions: two approaches. Int Stud Q 1988; 32(4): 379-396. [Google Scholar]
- [6].Forss K, Venson P. An evaluation of the capacity building efforts of United Nations operational activities in Zimbabwe: 1980–1995. Geneva: United Nations; 2002. [Google Scholar]
- [7].Willems S, Baumert K. Institutional capacity and climate actions. Paris: Organization for Economic Cooperation and Development; 2003. [Google Scholar]
- [8].Towse A, Devlin N, Hawe E, Garrison L. Consulting report. The evolution of HTA in emerging markets health care systems: analysis to support a policy response. London: Office of Health Economics; 2011. [Google Scholar]
- [9].Garrison L, Babigumira J, Bartlein R, Nguyen H. Health technology assessment in low- and middle-income countries: findings from a survey and case studies. Arlington, VA: Management Sciences for Health; 2012. [Google Scholar]
- [10].Health Interventions and Technology Assessment Program, NICE International Situation analysis of HTA Introduction at national level, version 2.0. 2013. Bangkok, Thailand: Health Interventions and Technology Assessment Program. [Google Scholar]
- [11].Hauck K, Smith P. The politics of priority setting in health: a political economy perspective. Working Paper 414. Washington, DC: Center for Global Development; 2015. [Google Scholar]
- [12].Kingdon JW, Thurber JA.. Agendas, alternatives, and public policies. Boston: Little, Brown; 1984. [Google Scholar]
- [13].Zahariadis N. Ambiguity and multiple streams In: Theories of the policy process (3rd ed.), Sabatier P, Weible C, eds. Boulder: Westview Press; 2014; 25–58. [Google Scholar]
- [14].Fox AM, Balarajan Y, Cheng C, Reich MR. Measuring political commitment and opportunities to advance food and nutrition security: piloting a rapid assessment tool. Health Policy Plan 2015; 30(5): 566-578. [DOI] [PubMed] [Google Scholar]
- [15].Shiffman J, Smith S. Generation of political priority for global health initiatives: a framework and case study of maternal mortality. Lancet 2007; 370(9595): 1370-1379. [DOI] [PubMed] [Google Scholar]
- [16].Guldbrandsson K, Fossum B. An exploration of the theoretical concepts policy windows and policy entrepreneurs at the Swedish public health arena. Health Promot Int 2009; 24(4): 434-444. [DOI] [PubMed] [Google Scholar]
- [17].Fox AM, Goldberg AB, Gore RJ, Bärnighausen T. Conceptual and methodological challenges to measuring political commitment to respond to HIV. J Int AIDS Soc 2011; 14(Suppl 2):S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Delvaux B, Mangez E. Towards a sociology of the knowledge–policy relation. Louvain-la-Neuve: Université Catholique de Louvain; 2008. [Google Scholar]
- [19].Hernandez-Villafuerte K, Li R, Hofman K. Author linkages in economic evaluations: tendencies in Southern Africa. Presentation by Adrian Towse to the World Health Organization, “Consultation on using health technology assessment in for universal health coverage and reimbursement systems,” 3 November 2015, WHO, Geneva. [Google Scholar]
- [20].Wilkinson T.Economic evaluation: a tool for priority setting in the context UHC—learning from the international experience. Presented at the African Health Economics and Policy Association Conference, 13 March 2014, Nairobi, Kenya. [Google Scholar]
- [21].Hernandez-Villafuerte K, Li R, Towse A, Chalkidou K. International decision support initiative: mapping of priority-setting in health for 17 low and middle countries across Asia, Latin America and Africa. Occasional Paper 2015/01. London: Office of Health Economics; 2015. Available at https://www.ohe.org/system/files/private/publications/413%20-%20International%20Decision%20Support%20Initiative%20Country%20selection%20report.pdf?download=1 [Google Scholar]
- [22].Grundy J.Myanmar: key issues and feasible options for accelerating progress to UHC. Bangkok, Thailand: WHO Regional Office for South-East Asia; 2012. [Google Scholar]
- [23].World Bank Open Data Free and open access to data about development in countries around the globe the world bank. Washington, DC: The World Bank; 2014. [Google Scholar]
- [24].National Department of Health (South Africa). National health insurance in South Africa : policy paper. Pretoria: National Department of Health (South Africa); 2011. [Google Scholar]
- [25].Garrison LP, Babigumira J, Bartlein R, Nguyen H. Health technology assessment in low- and middle-income countries: finding from a survey and case studies. Arlington, VA: Management Sciences for Health; 2012. [Google Scholar]
- [26].Rattanavipapong W, Luz ACG, Kumluang S, Kusumawardani N, Teerawattananon Y, Indriani D, Primastuti PA, Rivai LB, Idiani S, Adhie U, et al.. One step back, two steps forward: an economic evaluation of the PEN program in Indonesia. Health Sys Ref, this issue. [DOI] [PubMed] [Google Scholar]
- [27].Itad, NICE International Report on NICE International's engagement in India. Hove, UK: ITAD; 2015. [Google Scholar]
- [28].Chootipongchaivat S, Tritasavit N, Luz A, Teerawattananon Y, Tantivess S. Policy brief and working paper. Conducive factors to the development of health technology assessment in Asia. Bangkok, Thailand: Prince Mahidol Award Foundation; 2016. [Google Scholar]
- [29].World Health Organization World health statistics 2013. Geneva: World Health Organization; 2013. [Google Scholar]
- [30].Boerma T, Eozenou P, Evans D, Evans T, Kieny M-P, Wagstaff A. Monitoring progress towards universal health coverage at country and global levels. Geneva: World Health Organization; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].World Health Organization Global status report on noncommunicable diseases 2010. Geneva: World Health Organ ization; 2011. [Google Scholar]
- [32].Gakidou E, Nordhagen S, Obermeyer Z. Coverage of cervical cancer screening in 57 countries: low average levels and large inequalities. PLOS Med 2008; 5(6): e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].World Health Organization Health system response and capacity: NCD-related tests. Geneva: World Health Organization; 2013. [Google Scholar]
- [34].World Health Organization Mortality: risk of premature death from target NCDs. Geneva: World Health Organization; 2014. [Google Scholar]
- [35].Saksena P, Xu K, Durairaj V. The drivers of catastrophic expenditure: outpatient services, hospitalization or medicines? Geneva: World Health Organization; 2010. [Google Scholar]
- [36].World Health Organization. The selection and use of essential medicines report of the WHO Expert Committee, 2013 (including the 18th WHO model list of essential medicines and the 4th WHO model list of essential medicines for children). WHO Report Series 985. 2013. Available at http://apps.who.int/iris/bitstream/10665/112729/1/WHO_TRS_985_eng.pdf . [Google Scholar]
- [37].United States Agency International Development (USAID), U.S. President's Emergency Plan for AIDS Relief (PEPFAR) & AIDS Free. Treatment guidance database: HIV treatment guidance database. n.d. Available at https://aidsfree.usaid.gov/resources/guidance-data/treatment. [Google Scholar]
- [38].International Osteoporosis Foundation. National & regional osteoporosis guidelines. Nyon: International Osteoporosis Foundation; 2014. Available at http://www.iofbonehealth.org/national-regional-osteoporosis-guidelines [Google Scholar]
- [39].The World Bank. The Worldwide Governance Indicators (WGI) project. Washington, DC: The World Bank; 2013. Available at http://info.worldbank.org/governance/wgi/index.aspx#home [Google Scholar]
- [40].Cornell University, Institut européen d'administration des affaires, World Intellectual Property Organization Global Innovation Index 2013: the local dynamics of innovation. Geneva; Ithaca, NY; and Fontainebleau, France: Cornell University, INSEAD, and WIPO; 2013. [Google Scholar]
- [41].The World Bank. Statistical capacity indicator. Washington, DC: The World Bank; 2011. [Google Scholar]
- [42].Transparency International. Corruption Perceptions Index 2013. Berlin: Transparency International; 2014. Available at https://www.transparency.org/cpi2013 [Google Scholar]
- [43].World Health Organization. Recipient countries: commitments and disbursements to recipient countries, 2000–2010. Geneva: World Health Organization; 2013. Available at http://www.who.int/gho/governance_aid_effectiveness/country/en/ [Google Scholar]
- [44].The World Bank. World development indicators. Washington, DC: The World Bank; 2014. Available at http://data.worldbank.org/data-catalog/world-development-indicators [Google Scholar]
- [45].The Global Fund. Grant portfolio. Geneva: The Global Fund; 2013. Available at http://www.theglobalfund.org/en/portfolio/ [Google Scholar]
- [46].United Nations Statistics Division. UNdata: country profile: Myanmar. n.d. Available at http://data.un.org/CountryProfile.aspx?crName=MYANMAR. [Google Scholar]


