Abstract
There is a critical need to develop supports for older adults who have a wide range of abilities, including those aging with long-term impairments. Without appropriate support, many individuals will be functioning below optimal levels and will face participation barriers. Technology holds great promise to provide individualized support for a wide range of abilities and for a variety of domains. To ensure technology interventions are designed well and meet research-documented user requirements, we need more specific, actionable models to provide guidance for those developing and designing interventions. In this paper, we present the TechSAge Aging and Disability Model to bridge models from the aging and disability literatures and to disambiguate the population of individuals aging into disability from those aging with disability (i.e., pre-existing impairments). We also present the TechSAge Technology Intervention Model to support aging with pre-existing impairments, which provides direction and touch points for technology interventions. These models reflect the complex and dynamic interaction between age-related changes and an individual’s prior capabilities and limitations. We describe the need for these models with respect to filling a gap in the disability and aging literature by highlighting the importance of differentiating between age-related changes and long-term impairments when designing interventions. We also show the need for quantitative and qualitative data to refine the models given complexities of the current state of the literature and survey data. The TechSAge Technology Intervention Model can be used to drive and inform technology redesign and development.
Keywords: Age-related declines, Disabilities, Intervention, Successful aging, Technology
Translational Significance: The models presented in this paper provide direction for researchers and designers to consider the dynamic between capacity, context, technology characteristics, and functional ability and how these constructs impact the likelihood of successful performance outcomes for those aging with and without a pre-existing impairment.
Background and Objectives
While there are many interventions to address the support needs of individuals who are experiencing normal aging, the needs of people who are aging with impairments have generally been neglected (e.g., Beer, Mitzner, Stuck, & Rogers, 2015; Campbell & Putnam, 2017; Harrington et al., 2015). These needs include supports for managing chronic diseases and engaging in physical exercise to optimize health (Beer, Mitzner, Stuck, & Rogers, 2015; Mitzner, McBride, Barg-Walkow, & Rogers, 2013); performing daily activities (e.g., Beer, Mitzner, Stuck, & Rogers, 2015; Luo, Hawkley, & Waite, Cacioppo, 2012; U.S. Administration on Aging, 2016); and participating in community activities (e.g., Yang & Sanford, 2012). Despite the lack of attention to this population, technology interventions hold much promise for providing the necessary supports to maximize older adults’ functional abilities and enable them to participate as fully as possible in society, for as long as possible.
The Capacity and Ability Gap
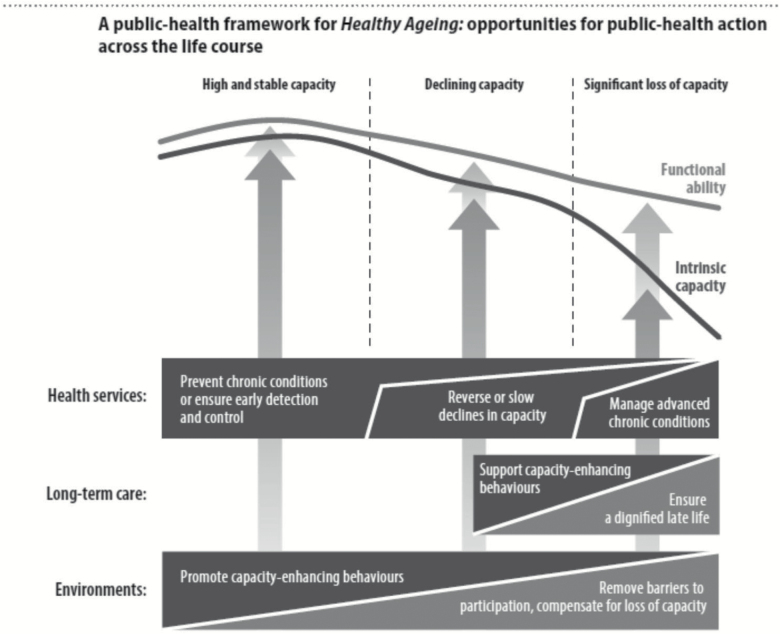
In 2015, the World Health Organization (WHO, 2015) issued a call to action highlighting the critical and urgent need to bridge the gap between intrinsic capacity (physical and mental potential of an individual based on his/her body structures and functions; WHO, 2001) and functional ability (health-related characteristics that enable activity performance and participation) of older adults (see Figure 1). The WHO report presents a public health framework to spark action for improvements in public heath for older people of all capabilities and levels of health by optimizing older adults’ trajectory of ability with the ultimate goal of maximizing functional ability despite losses in intrinsic capacity.
Figure 1.
The World Health Organization’s Public Health Framework for Healthy Ageing (WHO, 2015).
In contrast to intrinsic capacity, which resides wholly within the individual, functional ability reflects the interaction between the intrinsic capacity of the individual and the degree to which his/her context (i.e., environmental and personal factors) poses barriers or facilitators to activity and participation. In other words, functional ability represents the difference between what an individual can do and what that individual actually does do. Figure 1 depicts trajectories of decline in both intrinsic capacity and functional ability. Also shown in the model are touch points for provision of health care services, long-term care, and supportive environments. With such supports, an individual’s functional ability has a less steep decline as compared to their intrinsic capacity.
Aging and Disability
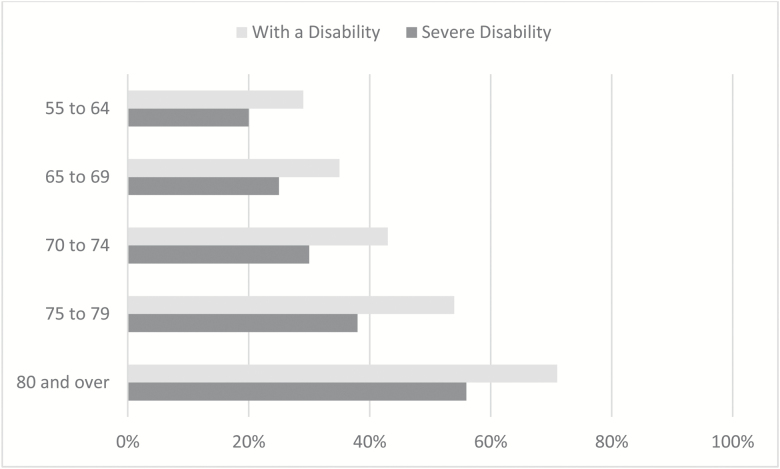
The prevalence and severity of disability increases with age. As depicted in Figure 2, almost 30% of the U.S. population 55–64 years of age reports experiencing disability, with 20% reporting severe disability. For individuals 80 years of age and older, the prevalence goes up to 71% for those reporting any disability, and 56% for those reporting severe disability (Brault, 2012).
Figure 2.
Disability by age. Disability measured by self-report on six functional limitation questions regarding difficulties with hearing, seeing, cognitive activities, ambulatory activities, self-care activities, and independent living activities. Severe disability was defined as inability to engage in these activities (e.g., Deaf or unable to hear a normal conversation, blind or unable to see words and letters; Brault, 2012).
Intrinsic capacity varies from person to person and typically declines over time, as individuals age. Some individuals’ intrinsic capacity is reduced in older adulthood due to normal age-related changes in body structures and functions (e.g., yellowing of the lens of the eye and loss of color sensitivity, respectively). Other individuals have capacity deficits due to impairments that occurred prior to older adulthood (e.g., loss of a vision) and then experience further declines in intrinsic capacity due to normal age-related declines in those (e.g., further decline in vision) or other (e.g., hearing or memory loss) body functions and structures.
Aging Into Disability
For some individuals, disability is the result of age-related declines in sensory (e.g., vision, hearing, tactile), physical (e.g., strength; dexterity), mobility (e.g., balance; coordination), and/or cognitive (e.g., working memory, executive function) functions (Birren, & Shaie, 2006). In addition to these normative age-related changes, prevalence of chronic conditions and multiple chronic diseases (Department of Health and Human Services, 2010) and dementia (Karel, Gatz, & Smyer, 2012) also increase with age. These age-related decrements and conditions typically reduce intrinsic capacity, which when acting in an unsupportive environment leads to barriers to perform everyday activities (Rogers et al., 1998) and results in diminished functional ability and often, disability.
Aging With Disability
Individuals may also experience disability due to the additive effects of age-related declines and pre-existing impairments. For the purpose of this discussion, we will define people aging with a pre-existing impairment as those who experienced impairment before the age of 50. Although many individuals who are aging with a pre-existing impairment may have been able to use contextual supports, including technologies, tools, and resources, throughout their lives to enhance functional ability and fully engage in life activities (and avoid disability), age-related declines often decrease intrinsic capacity to the point of putting these individuals at risk of disability. Moreover, those older adults who were already experiencing disability associated with impairments earlier in life may experience greater disability as the result of additional age-related declines.
Consider these scenarios of individuals who are aging AND have a pre-existing impairment:
In the first scenario, an individual with pre-existing impairments or limitations in body functions did not experience disability prior to age 65 due to minimal declines in intrinsic capacity that did not negatively affect activity and participation. However, that individual now experiences disability due to the addition of age-related declines in the same body structures and functions. Example: An individual who has had a lower-body mobility impairment for most of her life that did not negatively affect her activity and participation. However, with the addition of age-related arthritis in her knees and hips she now uses a wheelchair and encounters barriers due to lack of universal wheelchair accessibility.
In the second scenario, an individual with pre-existing impairments has experienced disability prior to age 65 due to declines in intrinsic capacity coupled with the inability or lack of supportive compensatory strategies to improve functional ability to overcome barriers to activity and participation. However, that individual now experiences greater disability due to the onset of additional age-related declines in intrinsic capacity that heighten or create new barriers to activity and participation. Example: An individual who has been blind most of his life and has experienced disability as a result (e.g., not able to walk to certain locations because of a lack of accessible pedestrian signals, such as those that provide auditory information). With the addition of age-related hearing loss, he now experiences even greater disability (e.g., now he may not be able to cross streets alone even if they do provide auditory information).
In the third scenario, an individual with pre-existing impairments and declines in intrinsic capacity who has avoided disability prior to age 65 due to supportive compensatory strategies to enhance functional ability to overcome barriers to activity and participation. However, that individual now experiences disability due to age-related declines in the same body structures and functions that further reduce intrinsic capacities and negate existing compensatory strategies. Example: An individual who has had a hearing impairment in one ear most of her life. She has been able to avoid disability by turning her body to compensate with her nonimpaired ear. With the addition of age-related hearing loss in her previously nonimpaired ear, she now experiences disability.
Note that the above scenarios represent populations that are typically not differentiated from each other or from the population of adults who experience disability as a result of aging alone (e.g., no differentiation between these populations in the data presented in Figure 2). In the first scenario an individual’s experience may be more similar to a person without an impairment who ages into disability, however individuals from the second and third scenarios likely have much more quantitatively and qualitatively different experiences. Given that these populations are typically combined in the aging and disability literatures, it is likely that fundamental differences in their needs will be overlooked. Furthermore, these examples highlight that disability, defined in the International Classification of Functioning, Disability and Health (ICF, 2001) as activity limitation and/or participation restriction (WHO, 2001), is not a given consequence of having a reduction in intrinsic capacity due to impairment in body structures or limitation in body functions. Whereas impairments in body functions and structures are preconditions for disability, the interaction of intrinsic capacity with the presence or absence of contextual barriers (e.g., low contrast/small text) and facilitators (e.g., high contrast/large text) determines whether performance outcomes result in disability.
TechSAge Aging and Disability Model
Consider the following example of the interaction between a pre-existing impairment and age-related changes leading to disability or greater disability. Arthritis is an age-related degenerative joint inflammation condition that causes pain, stiffness, and damage to joint cartilage, and surrounding structures. The damage can lead to joint weakness, instability, loss of tactile sensation, and limited joint movement. Imagine an individual who has a pre-existing lower body mobility impairment and then, with age, develops arthritis in her hands. Before she developed arthritis, she may have had a high degree of functional ability because of the use of a manual wheelchair. Her arthritis, however, reduced her ability to use her wheelchair and in turn triggered disability.
Enhancing activity and participation of individuals experiencing disability due to age-related changes alone has been a primary focus of geriatrics/gerontology. The rehabilitation fields have focused primarily on understanding the consequences of impairment-related disability throughout the lifespan. The interaction between pre-existing impairment and decline in intrinsic capacity due to age-related losses is underrepresented in the corpus of research in either domain (Campbell & Putnam, 2017). The expected activity and participation outcomes resulting from the effects of age-related limitations in addition to pre-existing impairment is captured in the TechSAge (Rehabilitation Engineering Research Center on Technologies to Support Successful Aging with Disability) Aging and Disability Model.
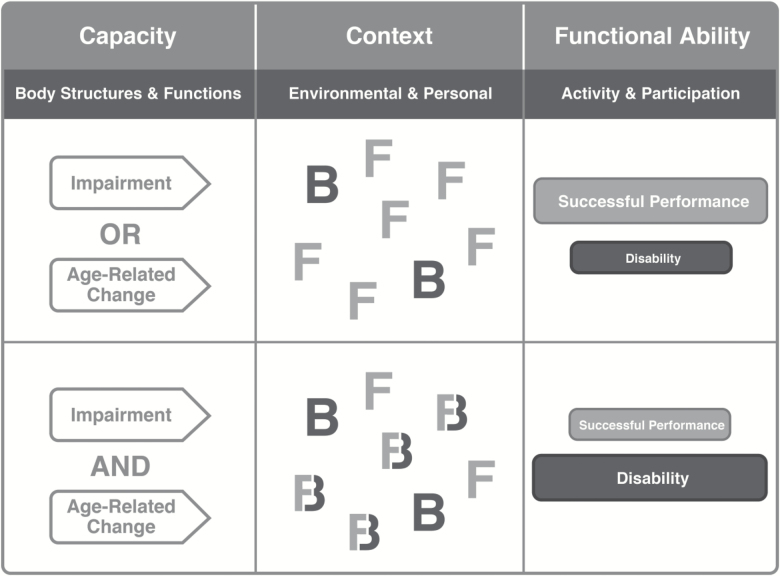
Building on an earlier version of the model (Sanford & Gonzalez, 2016), which integrated models from the WHO (2001, 2005) with Lawton’s Ecological Model of Person-Environment Fit (Lawton & Nahemow, 1973), the TechSAge Aging and Disability Model (Figure 3) describes both the conceptual similarities between traditional geriatric and rehabilitation approaches to aging or disability, respectively, and their differences from a perspective of aging with disability regarding the understanding of user needs, the impact of contextual factors, and the expected performance outcomes given contextual supports.
Figure 3.
The TechSAge Aging and Disability Model. The top row represents individuals who have a pre-existing impairment OR age-related changes. They have a certain Capacity that, when paired with a specific environmental or personal Context (Facilitators or Barriers), leads to more successful performance than disability in terms of their Functional Ability for activity and participation. The bottom row represents individuals who are aging AND have a pre-existing impairment. Their reduced capacity results in contextual facilitators becoming barriers (symbolized by Fs transitioning to Bs in figure) which leads to more disability than successful performance.
Columns
The columns in Figure 3 represent the key interactive constructs that impact performance outcomes. The first column, labeled Capacity, reflects intrinsic capacity (body structures and functions) due to an impairment or age-related changes or both. The Context (environmental and personal) column represents contextual facilitators (F) and barriers (B) that an individual may encounter in performing an activity, including physical and social environmental factors, technological interventions, and caregiving supports. Note that the social environment includes formal and informal caregivers, as many older individuals rely on caregivers (Janus & Doty, 2017). The personal context includes characteristics such as age, gender, educational level, and technology experience. The Functional Ability (activity and participation) column represents the outcome in terms of performance, either successful performance or disability (i.e., not able to perform activity/participate).
Rows
The rows in Figure 3 represent the expected impacts and performance outcomes of contextual factors on individuals with different levels of intrinsic capacity. The first row represents individuals who have age-related changes or impairments. Within a context, these individuals encounter facilitators that lead to successful performance and barriers that lead to disability. The greater the number of facilitators the greater the likelihood of successful performance outcomes in activity and participation. Conversely, barriers can result in disability as represented by activity limitations and participation restrictions. The second row represents individuals who have a pre-existing impairment and age-related changes. What is critical to note is that declines in intrinsic factors due to aging added to a long-term impairment may not only reduce the number of potential facilitators, but may also turn contextual factors that previously acted as facilitators when an individual was younger into barriers (as represented by the “Fs” changing into “Bs”) when one gets older. As a result, there is a greater likelihood of disability.
Closing the Gap: TechSAge Technology Intervention Model
Whereas impairments in body functions and structures are preconditions for disability, interventions that increase intrinsic capacity by mitigating the effects of impairment (e.g., eyeglasses, hearing aids, surgery) would eliminate or decrease disability. Similarly, increasing functional ability by maximizing facilitators and minimizing barriers (e.g., large text, high contrast) would theoretically, and ideally, result in an outcome of successful performance rather than one of disability. Theoretically, with proper contextual supports functional ability can be maximized and disability minimized or avoided. Conversely, without proper contextual supports, a loss in functional ability can result in disability. Contextual supports can range from informal or formal caregivers, to services, to tools and technologies.
Technology has great potential to provide the requisite contextual support for individuals as they age (Garcon et al., 2016; White House Conference on Aging, 2015). Supportive technologies may be higher-tech, advanced technologies such as robotics or lower-tech technologies such as grabbers and reachers. A distinction can also be made between traditional assistive technologies (AT) and off-the-shelf consumer technologies, sometimes referred to as everyday technologies (Harrington et al., 2015). The potential of technology as a solution for the growing aging population has been a focus in the United States as well as internationally (Kohlbacher & Herstatt, 2011; Rogers & Fisk, 2010). However, while more and more technologies are being developed to support the senior market, many are not based on older adults’ needs and capabilities, let alone the consideration of adults aging with a pre-existing impairment. There is a clear need for more targeted and better technology solutions. However, the development of effective technological supports for adults aging with pre-existing impairments is dependent on an understanding how contextual technological supports can be introduced to increase functional ability based on the activity and participation needs of these individuals.
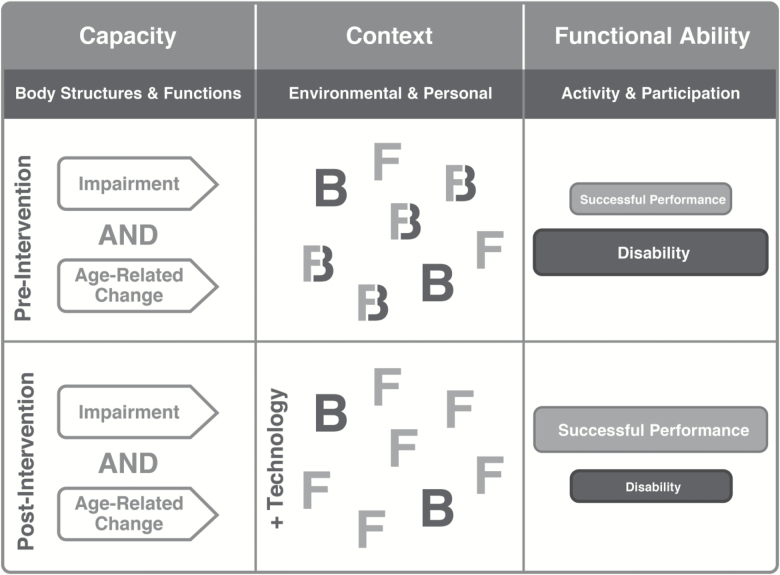
The TechSAge Technology Intervention Model (Figure 4) replicates the organization of the TechSAge Aging and Disability Model to provide a structure for describing how technological supports can act as contextual interventions to enhance activity and participation outcomes for people aging with pre-existing impairments.
Figure 4.
The TechSAge Technology Intervention Model illustrates the value of a technology intervention. The top row replicates the bottom row of Figure 3 wherein individuals are aging AND have a pre-existing impairment. Their reduced capacity results in contextual facilitators becoming barriers (symbolized by Fs transitioning to Bs in figure) and hence more disability. The bottom row illustrates how a technology intervention can turn the barriers (Bs) back into facilitators (Fs), which yields more successful performance.
The top row of Figure 4 repeats the bottom row of Figure 3, which represents individuals aging with pre-existing impairments in their everyday context prior to intervention. In contrast, the bottom row introduces technology as a contextual support (i.e., facilitator), such as the implementation of design improvements for an existing technology or the development of a new technology that is more robust in the context of age-related changes. The addition of technology facilitators has the potential to reduce the likelihood that facilitators will become barriers as well as enabling barriers (“Bs”) to be turned back into facilitators (“Fs”). This strategy increases functional ability and increases successful activity and participation performance outcomes (and decreases disability).
By identifying the interaction between intrinsic capacity and contextual factors, the TechSAge Technology Intervention Model can provide guidance for technology interventions that act as facilitators as individuals age with pre-existing impairments. Several examples of these scenarios are illustrated below.
Ms. S has been Deaf since birth and primarily communicates via American Sign Language within the Deaf community. Ms. S has always used television captioning to watch the news and movies. Therefore, closed captioning has been a facilitator for her – it enabled her successful performance for engaging in an activity. However, imagine the impact of age-related visual changes on captioning (i.e., farsightedness due to presbyopia, reduced contrast sensitivity, increased sensitivity to glare). With these age-related declines, the closed captioning text became too small, too low in contrast, and had too much glare for Ms. S to read it well. Closed-captioning became a barrier leading to disability for this activity. By improving the design of the existing technology with more robust visual output, adding user control that would enable Ms. S to modify the captioning text to meet her needs, or using a remote captioning device that Ms. S could hold close to her, captioning could become a facilitator again.
Mr. H has used a manual wheelchair since he suffered a spinal cord injury at the age of 35. His wheelchair has been a facilitator, allowing him to participate in activities inside and outside of his home. However, wheelchair use relies heavily on upper body strength and he is now experiencing age-related muscle loss and arthritis. Mr. H is having difficulty pushing his wheelchair, especially longer distances outside of his home. His manual wheelchair has become a barrier leading to disability for community participation. Mr. H’s wheelchair could become a facilitator again by the development of a wheelchair constructed of lighter materials, a different type of propulsion system, or a device that makes his pushes more efficient.
Ms. M has been blind since birth, relying on sound cues for moving around the environment. These sound cues, including pedestrian walk signals and the sound of her cane tap, have been facilitators, enabling her to walk around her community. Ms. M is now experiencing hearing loss due to presbycusis. Sound cues have become difficult for her to hear so they are now barriers causing mobility disability. Wearable or in-ear technologies that amplify meaningful sounds and mask ambient noise or present haptic or tactile information could enhance Ms. M’s mobility.
Discussion
WHO’s 2015 call to action to bridge the gap between intrinsic capacity and functional ability highlighted the need to develop tools and interventions to maximize older adults’ activity and participation. To be inclusive and have the most impact these tools and interventions must take into consideration the variability within the older adult population, including those with pre-existing impairments who have less intrinsic capacity. Older adults who are aging with pre-existing impairments may have the largest gap between capacity and functional ability, and therefore have the most to gain from interventions.
The TechSAge Aging and Disability Model furthers the WHO call to action by adding specific direction for understanding the needs of older adults with and without impairments. In the WHO (2015) model, only aging into disability is reflected without explicit acknowledgment of those aging with disability. The TechSAge Aging and Disability model integrates models from the disability and aging literatures addressing those aging into disability and those aging with disability. By doing so, it overtly differentiates between these populations bringing attention to their unique characteristics and environments. The TechSAge Aging and Disability Model highlights the need for research in this area to disambiguate characteristics such as capacity, functional ability, and disability for those aging with disability to identify needs and appropriate technology interventions. However, better metrics are required (WHO, 2015), including large-scale surveys that differentiate between the causes/etiology of difficulties and the types of difficulties individuals experience as they age. There is also need to identify standard metrics to assess functional ability outcomes (i.e., activity and participation) for evaluating interventions. Qualitative research is needed, as well, particularly research focused on understanding the details of the difficulties that adults aging with pre-existing impairments have regarding activity and participation. Lastly, there is a need for evidence-based practices for health promotion and chronic condition management that are developed or translated for adults aging with a disability (Campbell & Putnam, 2017).
The TechSAge Technology Intervention Model illustrates that technology interventions can be provided to an individual’s personal or environmental context to bridge the gap between capacity and functional ability and maximize activity and participation. These interventions may be in the form of existing technologies (AT and everyday technologies), technology redesign, or new technology development. To design technology that is useful and truly meets the needs of older adults who are aging with and without pre-existing impairments, the individuals’ characteristics need to be understood, including the nature of the challenges they have. There is a real need for understanding these characteristics, particularly those of adults aging with pre-existing impairments, as this is an understudied population. Multiple large-scale surveys have been conducted to collect descriptive data about the disability population (e.g., the National Health and Aging Trends Study; Montaquila, Freedman, Spillman, & Kasper, 2012; the National Long-Term Care Survey; Manton, 2004; and the American Community Survey; U.S. Census Bureau, 2014a). However, given the varying operationalization of the definition of disability in these surveys it is difficult to assess the underlying functional limitations (Harrington et al., 2015). It is also impossible to disentangle activity and participation difficulties caused by a pre-existing impairment versus those caused by age-related changes.
In addition to the varying definitions of disability, there are also cultural issues that make understanding the characteristics of adults aging with an impairment challenging. For one, individuals identify with one group more so than the other (disability or aging). In fact, a recent RESNA blog discussed the debate about whether disability is an outdated term in an aging world (Grott, 2015). Points made included the strong identification some individuals have with one (or the other label). The Deaf culture is another example of individuals who have a strong cultural identification that likely supersedes or at least runs in parallel with the label or identification of being part of the aging demographic. These cultural issues likely affect self-report based measures of disability and/or functional limitations, in particular, because they have implications for whether an individual self-identifies as having an impairment or disability. Future measures must be sensitive to these cultural issues to ensure the target population is fully included.
Furthermore, there is a need for research regarding the context in which an individual is functioning. For example, it is important to assess an individual’s environmental and personal context as he/she ages as well as to determine whether existing tools and supports (e.g., AT, caregivers) have become barriers with age. In the case of an aging couple, a spouse may have been able to provide support for transfers in the past, but can no longer do so safely due to age-related declines in his/her own strength and balance.
The TechSAge Technology Intervention Model also demonstrates that to understand the impact of technology one must also consider the multifaceted interaction between the technology, an individual’s capacity, and the context (see also Fisk, Rogers, Charness, Czaja, & Sharit, 2009; Rogers & Fisk, 2010). Functional ability likely varies at different points in time. Very little is known about how the interaction of aging and pre-existing impairments (and the impact of technology) affects activity and participation over time. The TechSAge Technology Intervention Model, therefore, provides direction and sets an agenda for designing technology to prevent contextual facilitators from becoming barriers as one ages and for turning barriers back into facilitators. Future research is needed to provide greater details regarding the interaction between the context and capacity for those aging with pre-existing impairments.
The TechSAge Aging and Disability Model and the TechSAge Technology Intervention Model highlight the need to take advantage of knowledge gained from both the aging and disability fields regarding technology support and design for people aging with pre-existing impairments. There is substantial research in both fields. We need to bridge the gap between these bodies of knowledge. This effort must also consider priority of needs and be supported on a policy level. Our models provide direction for this effort by encouraging researchers and designers to think about use cases and the various factors (e.g., capacity, context, technology characteristics, functional ability) that should be considered in the design process, with the ultimate goal of improving the lives of all older adults.
Funding
This research was supported in part by a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) (Department of Health & Human Services, Administration for Community Living) Grant 90RE5016-01-00 under the auspices of the Rehabilitation and Engineering Research Center on Technologies to Support Successful Aging with Disability (TechSAge; www.techsage.gatech.edu). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this publication do not necessarily represent the policy of NIDILRR, ACL, or HHS, and you should not assume endorsement by the Federal Government.
Acknowledgments
We appreciate the insights of Elena Gonzalez and other members of the TechSAge team during discussions of these models.
Conflict of Interest
None reported.
References
- Americans with Disabilities Act of 1990, Pub. L. No. 101–336 § 104, 328 Stat (1990). Retrieved from https://www.congress.gov/bill/101st-congress/senate-bill/933.
- Beer J. M., Mitzner T. L., Stuck R. E., & Rogers W. A (2015). Design considerations for technology interventions to support social and physical wellness for older adults with disability. International Journal of Automation and Smart Technology (AUSMT), 5, 249–264. doi:10.5875/ausmt.v5i4.959 [Google Scholar]
- Birren J. E., & Schaie K. W (2006). Handbook of the psychology of aging (5th ed). San Diego, CA: Academic Press. [Google Scholar]
- Brault M. W. (2012). Americans with Disabilities: 2010- Household Economic Studies Washington DC: U.S. Census Bureau; Retrieved from www.census.gov/prod/2012pubs/p70-131.pdf [Google Scholar]
- Campbell M. L., & Putnam M (2017). Reducing the shared burden of chronic conditions among persons aging with disability and older adults in the United States through bridging Aging and Disability. Healthcare, 5, 56. doi:10.3390/healthcare5030056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cumming R. G. Thomas M. Szonyi G. Salkeld G. O’Neill E. Westbury C. & Frampton G (1999). Home visits by an occupational therapist for assessment and modification of environmental hazards: A randomized trial of falls prevention. Journal of the American Geriatrics Society, 47, 1397–1402. doi:10.1111/j.1532–5415.1999.tb01556.x [DOI] [PubMed] [Google Scholar]
- Fisk A. D., Rogers W. A., Charness N., Czaja S. J., & Sharit J (2009). Designing for older adults: Principles and creative human factors approaches (2nd ed). Boca Raton, FL: CRC Press. doi:10.1201/9781420080681 [Google Scholar]
- Freedman V. A. Crimmins E. Schoeni R. F. Spillman B. C. Aykan H. Kramarow E.…Waidmann T (2004). Resolving inconsistencies in trends in old-age disability: Report from a technical working group. Demography, 41, 417–441. doi:10.1353/dem.2004.0022 [DOI] [PubMed] [Google Scholar]
- Garçon L., Khasnabis C., Walker L., Nakatani Y., Lapitan J., Borg J.,…, Velazquez Berumen A. (2016). Medical and assistive health techno logy: Meeting the needs of aging populations. The Gerontologist, 56 (Suppl 2), S293–S302. doi:10.1093/geront/gnw005 [DOI] [PubMed] [Google Scholar]
- Grott R. (2015). Is disability an outdated term in an aging world? Retrieved from http://www.resna.org/blog/disability-outdated- term-aging-world.
- Gonzalez E., Fausset C. B., Foster A., Cha G. & Fain W. B (2015). Moving in, out and around the home: Solutions from older adults with long-term mobility impairment. In Rehabilitation Engineering Society of North America (RESNA) Annual Conference 2015, Denver, Co, June 2015 Retrieved from https://www.resna.org/sites/default/files/conference/2015/wheeled_mobility/gonzalez.html [Google Scholar]
- Harrington C. N., Mitzner T. L., & Rogers W. A (2015). Understanding the role of technology for meeting the support needs of older adults in the USA with functional limitations. Gerontechnology, 14, 21–31. doi:10.4017/gt.2015.14.1.004.00 [Google Scholar]
- Holt-Lunstad J. Smith T. B. & Layton J. B (2010). Social relationships and mortality risk: A meta-analytic review. Plos Medicine, 7, e1000316. doi:10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janus A. L., & Doty P (2017). Trends in informal care for disabled older americans, 1982–2012. Gerontologist. Advance online publication. doi:10.1093/geront/gnx076 [DOI] [PubMed] [Google Scholar]
- Karel M. J., Gatz M. & Smyer M. A (2012). Aging and mental health in the decade ahead: What psychologists need to know. The American Psychologist, 67, 184–198. doi:10.1037/a0025393 [DOI] [PubMed] [Google Scholar]
- Kitchener M. Ng T. Lee H. Y. & Harrington C (2008). Assistive technology in medicaid home- and community-based waiver programs. The Gerontologist, 48, 181–189. doi:10.1093/geront/48.2.181 [DOI] [PubMed] [Google Scholar]
- Kohlbacher F., & Herstatt C (2011). The silver market phenomenon: Marketing and innovation in the aging society. (2nd ed). Berlin, Germany: Springer-Verlag. [Google Scholar]
- Lawton M. P. (1980). Environment and aging. Los Angeles, CA: Brooks/Cole. [Google Scholar]
- Lawton M. P., & Nahemow L. (1973). Ecology and the aging process. In: Eisoderofer C. & Lawton M. P. (Eds.), Psychology of adult development and aging, (pp. 619–674). Washington, DC: American Psychological Association. [Google Scholar]
- Luo Y. Hawkley L. C. Waite L. J. & Cacioppo J. T (2012). Loneliness, health, and mortality in old age: A national longitudinal study. Social Science & Medicine (1982), 74, 907–914. doi:10.1016/j.socscimed.2011.11.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manton K. G. (2004). National Long-Term Care Survey: 1982, 1984, 1989, 1994, 1999, and 2004. ICPSR09681-v5. Ann Arbor, MI: Inter-university Consortium for Political and Social Research, 2010-06-21. [Google Scholar]
- Mitzner T. L., McBride S. E., Barg-Walkow L. H., & Rogers W. A (2013). Self-management of wellness and illness for an aging population. In Morrow D. G. (Ed.), Reviews of human factors and ergonomics (Vol. 8, pp. 278–333). Santa Monica: HFES. doi:10.1177/1557234X13492979 [Google Scholar]
- Montaquila J., Freedman V. A., Spillman B., & Kasper J. D (2012). National Health and Aging Trends Study development of round 1 survey weights. NHATS Technical Paper #2. Baltimore: Johns Hopkins; Retrieved from https://www.nhats.org/scripts/documents/NHATS_Round1_WeightingDescription_Nov2012.pdf. [Google Scholar]
- National Center for Health Statistics (2010). Data File Documentation, National Health Interview Survey, 2009. Hyattsville, Maryland: National Center for Health Statistics, Centers for Disease Control and Prevention; Retrieved from ftp://ftp.cdc.gov/pub/health_statistics/nchs/dataset_documentation/nhis/2009/srvydesc.pdf. [Google Scholar]
- Rogers W. A. & Fisk A. D (2010). Toward a psychological science of advanced technology design for older adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 65, 645–653. doi:10.1093/geronb/gbq065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers W. A., Meyer B., Walker N., & Fisk A. D (1998). Functional limitations to daily living tasks in the aged: A focus group analysis. Human Factors, 40, 111–125. doi:10.1518/001872098779480613 [DOI] [PubMed] [Google Scholar]
- Sanford J. A., Gonzalez E. T (2016)RERC TechSAge: Making a difference to the lives of older adults with disability through design and technology. In Zhou J. & Salvendy G. (Eds.), Human Aspects of IT for the Aged Population. Design for Aging. ITAP 2016. Lecture Notes in Computer Science (Vol. 9754). Switzerland: Springer International Publishing. doi:10.1007/978-3-319-39943-0 [Google Scholar]
- Spector W. D. & Fleishman J. A (1998). Combining activities of daily living with instrumental activities of daily living to measure functional disability. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 53, S46–S57. doi:10.1093/geronb/53B.1.S46 [DOI] [PubMed] [Google Scholar]
- U.S. Administration on Aging (2007). A Profile of Older Americans: 2006 Retrieved from http://www.aoa.gov/PROF/Statistics/profile/2006/2006profile.pdf.
- U.S. Administration on Aging (2016). A Profile of Older Americans: 2016 Retrieved from file //cyclone.ad.gatech.edu/home/tm154/Downloads/2016-Profile.pdf.
- U.S. Census Bureau (2014a). American Community Survey. A Profile of Older Americans: 2012 Retrieved from http://aoa.gov/AoARoot/Aging_Statistics/Profile/2012/16.aspx.
- U.S. Department of Health and Human Services (2010). Multiple Chronic Conditions—A Strategic Framework: Optimum Health and Quality of Life for Individuals with Multiple Chronic Conditions. Washington, DC: US Dept. of Health and Human Services: Retrieved from https://www.hhs.gov/sites/default/files/ash/initiatives/mcc/mcc_framework.pdf [Google Scholar]
- White House Conference on Aging (2015). Final report Retrieved from https://whitehouseconferenceonaging.gov/2015-WHCOA-Final-Report.pdf
- World Health Organization (2001). International classification of functioning, disability and health. Geneva, Switzerland: World Health Organization; Retrieved from http://www.who.int/classifications/icf/en/ [Google Scholar]
- World Health Organization (2015). World report on ageing and health. Geneva, Switzerland: World Health Organization; Retrieved from http://apps.who.int/iris/bitstream/10665/186463/ 1/9789240694811_eng.pdf?ua=1 [Google Scholar]
- Yang H. Y. & Sanford J. A (2012). Home and community environmental features, activity performance, and community participation among older adults with functional limitations. Journal of Aging Research, 2012, 625758. doi:10.1155/2012/625758 [DOI] [PMC free article] [PubMed] [Google Scholar]