Abstract
Background
Non-atherosclerotic spontaneous coronary artery dissection (SCAD) is a rare disease that predominantly affects women. It presents with acute chest pain, ventricular arrhythmias, and even sudden cardiac death.
Case Summary
A 33-year-old man presented to emergency department with fatigue and cold sweat. He had no complaint of chest pain at the time of admission. He experienced a retrosternal chest pain 2 days ago after lifting a 30 pounds weight in the gym. Para-clinic results such as coronary computed tomography angiography and electrocardiogram were normal. However, coronary angiography showed multiple coronary dissections. We followed the patient for 4 months. He was asymptomatic except for one episode of chest pain during Tehran earthquake, while he was carrying his child to escape the room. Follow-up myocardial perfusion scan was negative for ischaemia.
Discussion
Stressors such as intense exercise, emotional stress, and Valsalva manoeuvre may cause SCAD in otherwise healthy patient. As in our case, lifting heavy weights was the most likely reason for SCAD. Stable patients without ongoing chest pain will be followed conservatively.
Keywords: Spontaneous coronary artery dissection, Coronary angiography, Chest pain, Case report
Learning points
In a patient with acute chest pain without any cardiovascular risk factor always think about rare conditions such as spontaneous coronary artery dissection (SCAD).
Para-clinic results such as unremarkable electrocardiogram and normal multislice computed tomography angiogram does not rule out SCAD.
Introduction
Non-atherosclerotic spontaneous coronary artery dissection (SCAD) is a rare disease that predominantly affects women.1 It presents with acute chest pain, ventricular arrhythmias, and even sudden cardiac death.2 It is frequently underdiagnosed and the exact prevalence of the disease is not clear. It may happen in an atherosclerotic coronary artery, which is more often involves male population (atherosclerotic type). However, pathophysiology and progression of non-atherosclerotic types of SCAD are more challenging.3
Important differential diagnoses of acute chest pain, in a young patient with no coronary risk factor are as follows; aortic dissection, arteritis, prinzmetal angina, myocarditis, Takotsubo cardiomyopathy, pulmonary thromboemboli, aortic stenosis, and also coronary artery dissection.
Timeline
| A week before admission | Upper respiratory tract infection |
| Three days before admission | Intense isometric exercise and first episode of retrosternal burning |
| Day of admission (9 a.m.) | Fatigue and cold sweat while doing house chores |
| Initial presentation | History of fatigue and weakness without any complaint of chest pain, normal electrocardiogram, and borderline troponin level (no significant rise) |
| Three days after admission | Experiencing chest pain while holding his 2-year-old child |
| Coronary angiography (Day 3) | Multiple coronary artery dissection in left circumflex artery has been diagnosed |
| Three month after hospital discharge | One episode of similar chest pain while holding his child to escape the room because of the earthquake |
| Four months after hospital discharge | Myocardial perfusion scan with exercise test was performed, and it was negative for ischaemia |
Case presentation
A 33-year-old man came to emergency department with chief complaint of fatigue and cold sweat in the morning while doing routine house chores. He also complained from retrosternal burning sensation 2 days ago. He had upper tract respiratory infection 1 week ago. He was not a professional athlete, however, from 2 days ago he began ‘light body building and aerobic exercise’. When detailed history was taken, retrosternal chest discomfort was associated with holding a 30 pounds weight at the first time. The pain did not exacerbate with walking and did not radiate to arms or jaw. At the first day of presentation, he had no chest pain or shortness of breath. Physical examination was unremarkable and vital sign was stable. He was non-diabetic and normotensive. Past medical history was negative. He did not use any kind of drug substance and cigarette.
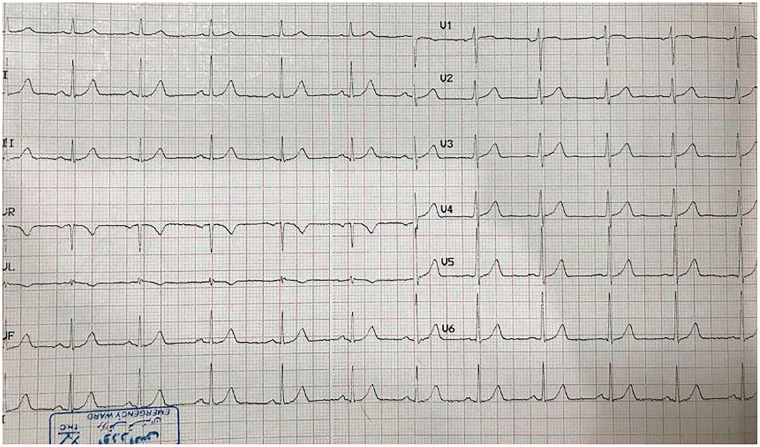
After physical examination, electrocardiogram (ECG) and routine lab test were ordered.
ECG revealed normal sinus rhythm, normal axis, and no ST-T change (except for tall R in V1) (no dynamic change in serial ECGs), Figure 1. Right and posterior ECGs were normal. High sensitivity Troponin T scores (0 and 2 h protocol) were 87 ng/dL and 84 ng/dL, respectively, with upper limit of 24 ng/dL. D-dimer was negative. Erythrocyte sedimentation rate (ESR) and C-reactive peptide (CRP) were also negative. Transthoracic echocardiography (TTE) was performed; normal left ventricle and right ventricle size left ventricular ejection fraction 55%, good right ventricular function, no evident wall motion abnormality, and no significant valvular disease.
Figure 1.
Admission electrocardiogram.
In this step, besides acute coronary syndrome (ACS), we thought about myopericarditis and also aortic dissection (AD). Physical examination, TTE, and D-dimer level were not in favour of AD. But we could not rule out myopericarditis or even ACS.
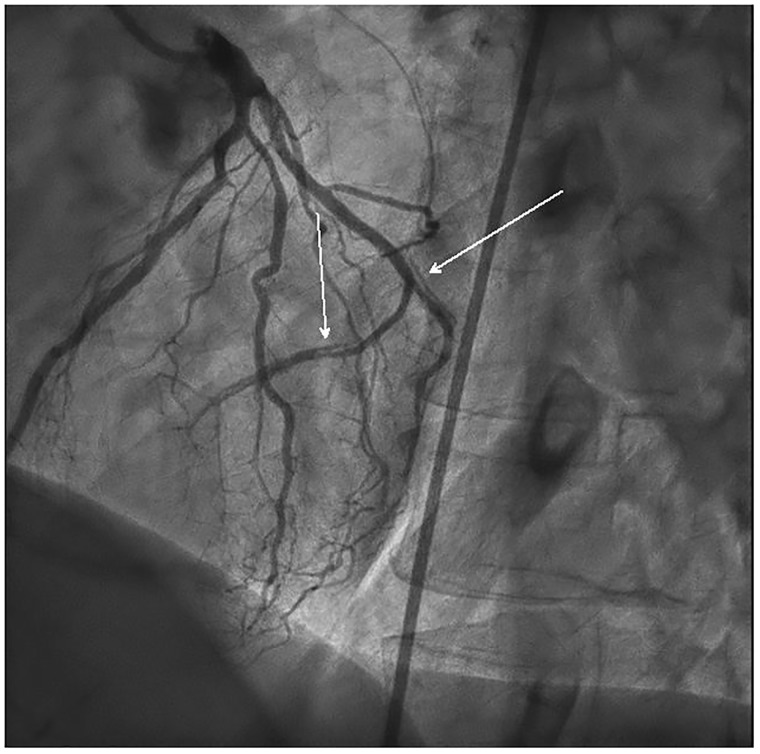
The patient received ASA 650 mg TDS, Pantoprazole 40 mg daily, Atorvastatin 40 daily, Clopidegrol 75 daily, Metoral 25 mg BD, and enoxaparin 80 mg SC BD. We decided to perform coronary multislice computed tomography angiogram (MDCT). It was done at heart rate 80 b.p.m. with prospective triggering method. Calcium score was zero, and coronary vessels were normal except mild stenosis in mid part of left anterior descending artery (LAD). The patient was asymptomatic and transmitted from coronary care unit (CCU) to the ward. He insisted on hospital discharge as soon as possible. At the day 3, we planned to discharge the patient and follow him medically. But, he complained from similar retrosternal pain while holding his 2-year-old child, which was brought to the hospital against hospital regulations to visit her father. The resident immediately visited the patient; fortunately serial ECGs and Troponin level were not remarkable. Hence, we changed the plan and scheduled him for coronary angiography (CAG). The next day, he underwent CAG, Figure 2. In addition to mild LAD lesion, multiple linear coronary dissections, and contrast dye staining within left circumflex artery (and its obtuse marginal branches) were seen. After consultation with interventionist the patient transferred to CCU again.
Figure 2.
Spontaneous coronary dissection in left circumflex artery and its branches.
Connective tissue disease may cause SCAD. Anti-nuclear antibody, anti double-stranded DNA, and rheumatic factor were ordered and were negative. Colour Doppler sonogram of renal arteries was performed to evaluate probable fibromuscular dysplasia. All para-clinic results were normal.
We observed the patient for the next 2 days and discharged him with ASA 80 daily, Clopidegrol 75 daily, Pentoprazole 40 daily, Atorvastatin 20 qHS, and Metoral 25 mg BD.
Monthly follow-up was done for about 4 months. Restriction of isometric exercises was advised. After 3 months, he was asymptomatic except one similar episode. The night of Tehran earthquake, he held his child to escape from the apartment and experienced the same symptoms. He was revisited in our clinic and myocardial perfusion scan with exercise test was performed, which was negative for ischaemia.
Discussion
Although SCAD more often affects woman, clinicians should be aware of this disease in face of a young man without any coronary risk factor presenting with indeterminate symptoms and lab data. Stressors such as intense exercise,4 emotional stress, and Valsalva manoeuvre may cause SCAD in otherwise healthy patient. As in our case, lifting heavy weights was the most likely reason for SCAD. SCAD may be idiopathic or be associated with fibromuscular dysplasia, connective tissue disease, and hormonal therapy.5
Non-invasive tests such as coronary MDCT angiography and magnetic resonance angiogram may be misleading.6 MDCT angiography of our patient was rechecked, but there was still no sign of SCAD. Limited data are available about the exact role of MDCT as the first diagnostic step for SCAD. This non-invasive method is a safe and accurate method to evaluate patients with chest pain in emergency department. However, in patients with SCAD it may be missed while relying solely on MDCT reports.7
Treatment strategy differs based on patients’ symptoms, coronary flow, and expert opinion. Stable patients without ongoing chest pain will be followed conservatively.8 ASA, clopidegrol, and beta blockers are mainstay of wait and watch strategy and improve healing process.9 Patients with ongoing chest pain, compromised haemodynamics should be considered for revascularization; percutaneous or even open surgery may be considered. Revascularization in these patients is more challenging than simple atherosclerotic plaques and also has higher rates of failure.10 Hence, since he was stable and did not have ongoing chest pain, we decided to follow him medically with triple therapy (ASA, Clopidogreal, and Metoral). His symptoms recurred just once (3 months after discharge), but he was not symptomatic at daily chores.
Vascular healing after SCAD has been reported in majority of cases, which was managed conservatively. There are many complications when the patient undergoes percutaneous coronary intervention for SCAD. Hence, in case of repeated chest pain (as in our patient with one episode of chest pain in 3 months) careful and precise decision should be made for revascularization option. He may benefit from myocardial perfusion scan to evaluate the probable ischaemia and also to assess the healing process.
Non-invasive tests will show coronary healing through time. MDCT and CAG has been suggested for follow-up evaluations.7,11
History of upper tract infection, atypical chest pain, and the high prevalence of myopericarditis in winter all caused improper diagnosis at the first place. Lack of coronary risk factor, young age, and the coronary computed tomography angiography report has also delayed CAG performance. However, detailed history taking and delayed hospital discharge finally helped us with the right diagnosis.
Conclusion
Although detailed history reveals the diagnosis most of the times, incidental findings such as history of upper tract infection in this case, may be misleading. MDCT coronary is an accurate imaging technique but may not reveal SCAD in some cases. Data about management of patients with SCAD are limited. Stable patients may be managed conservatively. Three drugs has been suggested in the literature, which improve healing process of the coronary dissection; ASA, Clopidogrel, and beta-blocker. Atorvastatin has been suggested in the case of dyslipidaemia.
Supplementary Material
Acknowledgements
We thank Dr Kimia Najafi for her great help in writing this manuscript. Our gratitude goes to Tehran Heart Centre (THC) for all the support.
Funding
All interventions and lab test were done in Tehran Heart Centre. Tehran Heart Centre provided all funding.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
References
- 1. Vavuranakis M, Latsios G, Tousoulis D, Vaina S, Triantafyllou G, Drakopoulou M, Stefanadis C.. Spontaneous coronary dissection as a cause of acute coronary syndrome: evidence for non-inflammatory underlying mechanisms. Int J Cardiol 2007;114:E24–EE6. [DOI] [PubMed] [Google Scholar]
- 2. Saw J, Aymong E, Sedlak T, Buller CE, Starovoytov A, Ricci D, Robinson S, Vuurmans T, Gao M, Humphries K, Mancini GB.. Spontaneous coronary artery dissection: association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ Cardiovasc Interv 2014;7:645–655. [DOI] [PubMed] [Google Scholar]
- 3. Saw J, Ricci D, Starovoytov A, Fox R, Buller C.. Spontaneous coronary artery dissection: prevalence of predisposing conditions including fibromuscular dysplasia in a tertiary centre cohort. JACC Cardiovasc Interv 2013;6:44–52. [DOI] [PubMed] [Google Scholar]
- 4. Hering D, Piper C, Hohmann C, Schultheiss H, Horstkotte D.. Prospective study of the incidence, pathogenesis and therapy of spontaneous, by coronary angiography diagnosed coronary artery dissection. Z Kardiol 1998;87:961–970. [DOI] [PubMed] [Google Scholar]
- 5. Michelis KC, Olin JW, Kadian-Dodov D, D’escamard V, Kovacic JC.. Coronary artery manifestations of fibromuscular dysplasia. J Am Coll Cardiol 2014;64:1033–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Saw J, Sedlak T, Ganesh SK, Isserow S, Mancini GJ.. Spontaneous coronary artery dissection (SCAD). Circulation 2015;131:e3–e5. [DOI] [PubMed] [Google Scholar]
- 7. Eleid MF, Tweet MS, Young PM, Williamson E, Hayes SN, Gulati R.. Spontaneous coronary artery dissection: challenges of coronary computed tomography angiography. Eur Heart J Acute Cardiovasc Care 2017; doi:10.1177/2048872616687098. [DOI] [PubMed] [Google Scholar]
- 8. Eddinger J, Dietz WA.. Recurrent spontaneous coronary artery dissection. Catheter Cardiovasc Interv 2005;66:566–569. [DOI] [PubMed] [Google Scholar]
- 9. Maeder M, Ammann P, Angehrn W, Rickli H.. Idiopathic spontaneous coronary artery dissection: incidence, diagnosis and treatment. Int J Cardiol 2005;101:363–369. [DOI] [PubMed] [Google Scholar]
- 10. Tweet MS, Eleid MF, Best PJ, Lennon RJ, Lerman A, Rihal CS, Holmes DR, Hayes SN, Gulati R.. Spontaneous coronary artery dissection: revascularization versus conservative therapy. Circ Cardiovasc Interv 2014;7:777–786. [DOI] [PubMed] [Google Scholar]
- 11. Alfonso F, Paulo M, Lennie V, Dutary J, Bernardo E, Jiménez-Quevedo P, Gonzalo N, Escaned J, Bañuelos C, Pérez-Vizcayno MJ, Hernández R, Macaya C.. Spontaneous coronary artery dissection: long-term follow-up of a large series of patients prospectively managed with a “conservative” therapeutic strategy. JACC Cardiovasc Interv 2012;5:1062–1070. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.