Abstract
Introduction
Gastropericardial fistulas are rare conditions, with less than 100 reported cases. The diagnosis is associated with significant morbidity, prolonged hospitalization and often has a fatal outcome.
Case presentation
We describe a unique case of cardiac arrest caused by pneumopericardium and cardiac tamponade as the acute presentation of a gastropericardial fistula, in a patient admitted with an infection of unknown origin. Rapid return of spontaneous circulation occurred, and a computed tomography scan revealed the diagnosis. A benign penetrating ulcer was found on gastroscopy, and surgical management with laparotomy and gastrorrhaphy was performed. The patient had no risk factors for gastric ulceration. However, he had significant comorbidity, which makes survival through a complicated postoperative course to full recovery remarkable.
Discussion
This case shows that pneumopericardium due to a penetrating benign gastric ulcer can cause cardiac tamponade, and illustrates the value of a multidisciplinary approach to management.
Keywords: Gastropericardial fistula, Pneumopericardium, Cardiac tamponade, Cardiac arrest, Case report
Learning points
This case demonstrates a multidisciplinary approach to a patient with a complex and exceptional condition.
Pneumopericardium due to a penetrating benign gastric ulcer can cause cardiac tamponade.
With prompt treatment survival is possible even in a debilitated patient.
Introduction
Pneumopericardium is most commonly traumatic or iatrogenic. Non-traumatic pneumopericardium is caused by infections and pericardial perforation of gastric ulcers or malignancies. Yet, gastropericardial fistulas are rare conditions, with less than 100 reported cases,1 of which 35 cases document radiological findings.2 The condition typically occurs as a late complication after surgery to the gastric ventricle or lower oesophagus (more than 50% of all reported cases), such as Nissen fundoplication3 and Roux-en-Y bypass for reflux4 or bariatric surgery.5 Other reported risk factors include diaphragmatic hernias6 and radiochemotherapy.7 The diagnosis is associated with significant morbidity with prolonged hospitalization, and often has a fatal outcome.
We present a unique case of survival after cardiac arrest caused by cardiac tamponade due to a gastropericardial fistula.
Timeline
| Day | Events |
|---|---|
| 8 years prior to presentation | Tetraplegic after fall accident |
| Autonomic dysreflexia | |
| Posttraumatic epilepsy | |
| Frequent infections | |
| 15 days prior to presentation | Suspected urinary tract infection |
| Cefotaxim therapy started | |
| Generalized urticaria, and antibiotic regimen changed to ciprofloxacin | |
| Acute presentation | Admission to local hospital with an infection of unknown origin |
| Dyspnea, fever, fatigue ande left shoulder pain | |
| Blood pressure 97/68mmHg, heart rate 89bpm, temperature 37.1°C | |
| ECG: 1mm ST elevation in leads I, III, aVF, V3 ande V5-6 | |
| Antibiotic therapy with cefuroxime and gentamycine, changed to clindamycin due to suspected cephalosporin allergy | |
| Transer to local hospital intensive care unit (ICU) | |
| CARDIAC ARREST! CPR for 1 minute → ROSC | |
| Chest X-ray: pneumopericardium | |
| Computer tomography: gastropericardial fistula | |
| Transfer to the Univesity Hospital of North-Norway | |
| Surgical phase | Percutaneous drainage attempted |
| Open pericardial decompression performed | |
| Gastroscopy reveled a deep ulcer | |
| Laparotomy and gastrorrhaphy performed | |
| Transfer to University Hospital ICU | |
| Postoperative day 0 | Atrial fibrillation, treated with amiodarone |
| Postoperative day 2 | Respiratory failure, ICU treatment |
| Pleural effusion, percutaneous drainage | |
| Postoperative day 7 | Relaparotomy because of wound dehiscence |
| Postoperative day 12 | Colonic pseudoobstruction: relaparotomy with construction of a coecostomy |
| Postoperative day 14 | Transfer to department of gastrointestinal surgery |
| Gradually tolerating oral intake and tapering off total parenteral nutrition | |
| Postoperative day 23 | Transfer to local hospital |
| Postoperative day 39 | Discharged to home in preadmission condition |
Case presentation
Our patient was admitted to his local hospital with a suspected urinary tract infection, after unsatisfactory response to initial antibiotic therapy with cefotaxim at a local health centre.
On admission, he was described to have an erythematous rash on the right hip and thigh. He later developed a generalized urticaria, suspected to represent an allergic reaction to cefotaxim. The regimen was changed to ciprofloxacin orally, and he recovered well on this treatment and was discharged after 5 days. He was readmitted to his local hospital 10 days later, with an infection of unknown origin, suspected to represent pneumonia.
He was described to have dyspnoea, fever, and fatigue and had deteriorated significantly over the past few days. He was also reported to have neck and left shoulder pain, which occurred a day earlier during exercise with his physiotherapist.
The patient was a 56-year-old man with C4 level tetraplegia after a fall accident 8 years earlier. He had autonomic dysreflexia with a habitual blood pressure around 90/60 mmHg. He also had post-traumatic epilepsy and a past history of alcohol abuse. He had no previous history of cardiovascular disease. He received antiepileptic therapy with gabapentin and karbamazepin, spasmolytic treatment with baklofen, metenamin to prevent urinary tract infections, and bisakordyl and natriumlaurylsulfat for constipation. He used salbutamol and nebulized acetylcystein to optimize respiration and cough. Metoclopramid, diazepam, paracetamol, and zopiclone was administered as required. Sublingual nitroglycerin was prescribed in relation to his autonomic dysreflexia for sporadic use during episodic blood pressure elevation. This had not occurred for several weeks.
Upon initial examination on readmission, he was drowsy but arousable, with blood pressure 97/68 mmHg, heart rate 89 b.p.m., temperature 37.1°C, respiratory rate 16/min, and saturation 96%. Weak heart sounds and a split S2 was described, and jugular vein distension was observed. The abdomen was soft, non-tender and had normal configuration.
Electrocardiogram showed slow septal R progression, and 1 mm ST-elevation in leads I, III, aVF, V3 and V5-6, and 1, 5 mm ST-elevation in leads II and V4. Biphasic T in leads III, aVL, aVF and V3-4. C-reactive protein (CRP) was 354 mg/L (ref. <5 mg/L), troponin I 63 ng/L (ref. <40 ng/L), sodium 129 mmol/L (ref. 137–145 mmol/L), and potassium 5, 1 mmol/L (ref. 2, 15–2, 55 mmol/L) at the time of admission. Initial antibiotic therapy was started with cefuroxime and gentamycine. He was transferred from the emergency department to the intensive care unit (ICU) after a drop in blood pressure to systolic 72 mmHg. His antibiotic regimen was changed to clindamycin due to the suspected cephalosporin allergy. A repeat troponin I after 6 hours rose to 75 ng/L, whereas the electrolytes were unchanged. He deteriorated the following night with severe hypotension and loss of consciousness. Crystalloids and noradrenaline infusion was started, with initial improvement. A few hours later he underwent cardiac arrest with asystole. Immediate treatment with cardiopulmonary resuscitation was initiated, with return of spontaneous circulation (ROSC) after one minute. A chest X-ray revealed a widened mediastinum with pneumopericardium (Figure 1).
Figure 1.
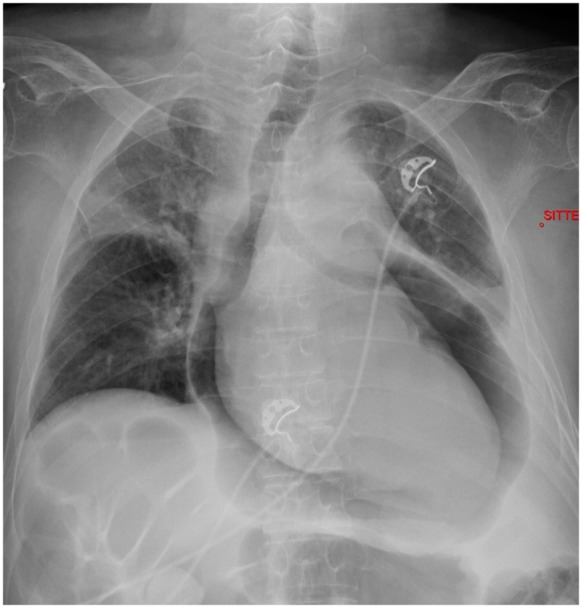
Antero-posterior (AP) chest X-ray showing pneumopericaridum.
Further investigation was performed with a thoracic computed tomography (CT) scan with intravenous contrast. There was air contained in the pericardial cavity, with normal findings in the remaining mediastinum, and no pneumothorax. Oesophageal perforation or barotrauma was therefore considered unlikely. There was no exudate in the pericardial sac or stranding in the fat around the heart as would have been expected with a bacterial pericarditis from gas producing organisms. With careful scrutiny of coronal (Figure 2) and sagittal (Figure 3) images a discontinuity was seen in the left hemidiaphragm with a connection from the superior aspect of the stomach to the posterior pericardial sac, diagnostic of a fistula.
Figure 2.
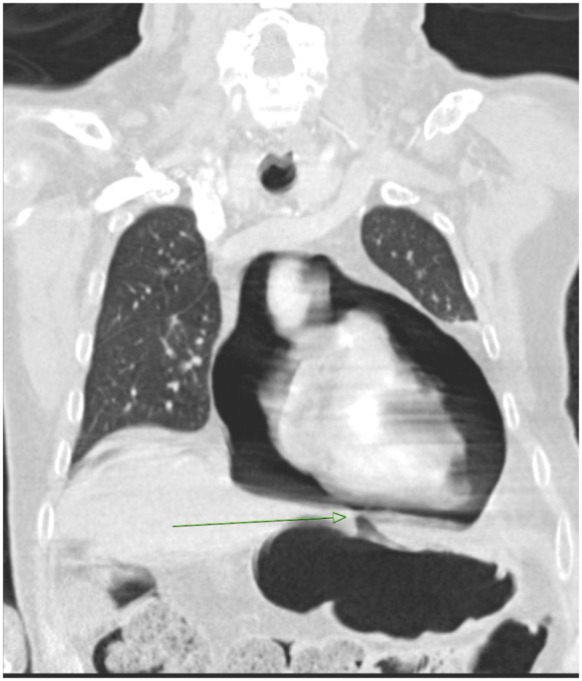
Coronal CT image demonstrating pneumopericardium and a diaphragmatic discontinuity.
Figure 3.
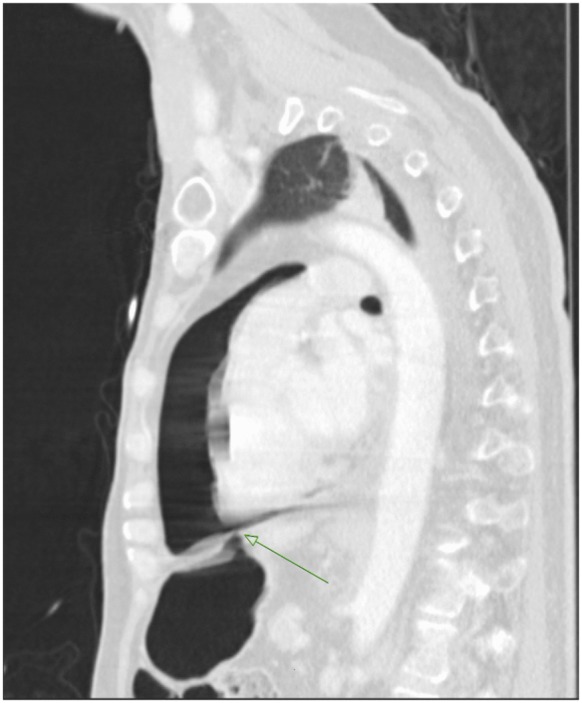
Sagittal CT image demonstrating pneumopericardium and a diaphragmatic discontinuity.
The patient was transferred by helicopter to the University Hospital, and immediately taken to the operating room.
He was met by a team of an anaesthesiologist, a cardiologist, a cardiac surgeon, and a gastrointestinal surgeon. The strategy was to drain the pericardial cavity before endoscopy, to prevent a new cardiac tamponade by air escaping through the suspected fistula. An initial attempt on subxiphoid percutaneous drainage was unsuccessful. Parasternal puncture in the left third intercostal space allowed for drainage of air from the pericardial sac. The risk of complications was considered to be too high for placement of a permanent drain in this atypical position.
General anaesthesia was administered, a subxiphoid open pericardial decompression was performed, and a pericardial drain was placed. No macroscopic gastric contamination was detected.
A gastroscopy could now safely be performed, and revealed a deep ulcer on the anterior wall of the stomach, with no other pathology, thus macroscopically compatible with a benign penetrating ulcer with no suspicion of malignancy (Figure 4).
Figure 4.

Gastroscopy revealed a macroscopically benign gastric ulcer.
A laparotomy was performed. There was no abdominal soiling, and the anterior wall of the stomach was firmly adherent to the left side of the diaphragm. This was released, and the ulceration was excised. The ventricular defect was closed in two layers, and the diaphragmatic defect closed with placement of an omental patch. An intra-abdominal drain was positioned in relation to the gastrorrhaphy. Histology confirmed a benign aetiology. Intravenous infusion with pantoprazole was started, and the nasogastric tube was kept for 24 h.
Postoperative intensive care was necessary due to respiratory failure, hypotension, and episodic atrial fibrillation for the first postoperative days. Stable sinus rhythm returned after amiodarone therapy. Clindamycine treatment was continued with addition of metronidazole. Fluconazol was added due to growth of Candida Albicans in the pericardial fluid sample. Pleural effusion occurred on day 2, and was treated with percutaneous drainage.
On day 7, he was reoperated because of wound dehiscence.
Due to persistent serous secretion from the wound he underwent a new reoperation on day 12, revealing pseudo-obstruction of the colon (Ogilvie) probably due to the background condition, the previous surgery and long-time stay in the ICU. A coecostomy was constructed.
Over the following days he gradually recovered, and was transferred from ICU to the department of gastrointestinal surgery on day 14.
Due to persistent fever, a transthoracic echocardiogram was performed on day 21. There was a small amount of remaining pericardial fluid, but no sign of tamponade, no valvular pathology and no vegetations. An increased filling pressure advocated diuretic therapy. The heart function was described to be normal. No bacterial infection was suspected, and antibiotic therapy was discontinued, whereas antifungal treatment was continued against a suspected Candida pneumonia.
He was initially depending on total parenteral nutrition, but gradually tolerating oral intake.
On transferal back to the local hospital on day 23, he was circulatory and respiratory stable with improving levels of function.
He stayed in the local hospital for an addition of 16 days, with further antifungal therapy, and treatment with drainage of bilateral pleural effusion. He was discharged to his home, mobilized to his preadmission level, with no antibiotic treatment, oral nutrition and an unchanged medical regimen.
Fourteen months after discharges, he was seen in the out patient clinic by a gastric surgeon. He has regained normal colonic function, and readmission for reversal of his coecostomy has been scheduled.
Discussion
We believe this is an extraordinary case report. We have not been able to find any previous report of gastropericardial fistula with development of pneumopericardium with concomitant cardiac arrest.
ROSC was obtained after one minute of chest compression. It is possible that the external massage forced some of the pericardial entrapped air back to the stomach, and by this relieving the acute cardiac tamponade situation.
A plain chest X-ray showed pneumopericardium, which is a non-specific finding, with differential causes as previously listed. When a gastropericardial fistula is suspected, further investigation with CT is recommended. Oral contrast before the CT scan could have demonstrated contrast in the pericardial space, or a fluoroscopy contrast study could have detected fistulas or mucosal lesions.2 However, this kind of investigation should be reserved for cases with a dubious CT scan, because the effect of contrast on the pericardium is not well studied. It is also important to limit the amount to prevent iatrogenic cardiac tamponade.
An attempt of subxiphoidal needle drainage was unsuccessful. The reason for this could be the supine position of the patient causing air to rise to the anterior aspect of the heart. Parasternal puncture easily evacuated the air allowing for safe intubation.
The finding of Candida in the pericardial fluid was a rather surprising finding, and is a pathogen described in other case reports to be a rare cause of serious and potentially life threatening pericarditis.
Intestinal pseudo-obstruction complicated the course of recovery. Causes of pseudo-obstruction of the colon include trauma, surgery, infection, myocardial infarction, heart failure, chronic obstructive pulmonary disease, metabolic diseases, medications (anticholinergics, opioids, antipsychotics, clonidine), neurological diseases (spinal cord injury, stroke, Parkinson’s disease, Alzheimer’s disease), and obstetric/gynaecological conditions (caesarean section, normal vaginal delivery, preeclampsia, normal pregnancy, pelvic surgery). The pathophysiology is not clearly understood but involvement of the sympathetic and parasympathetic nervous system leading to relaxation of the proximal colon and functional obstruction of the distal colon is suggested.8 It can be treated with endoscopic decompression, medically with neostigmine or surgically with deviation which was the chosen method in this case. Deviation is a definitive solution to the problem and worked out fine for our patient.
What caused the fistula to occur remains obscure in this case. None of the patient’s medications were known to be ulcerogenic and there was presently no alcohol abuse.9
We consider the prognosis of a gastropericardial fistula causing cardiac tamponade and heart arrest to be extremely poor, particularly due to the comorbidity in the present case. The full recovery of the patient is therefore remarkable.
Conclusion
This case demonstrates a multidisciplinary approach to a patient with a complex and exceptional condition. Pneumopericardium due to a penetrating benign gastric ulcer can cause cardiac tamponade. With prompt treatment survival is possible even in a debilitated patient.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
References
- 1. Imran Hamid U, Booth K, McManus K.. Is the way to a man's heart through his stomach? Enteropericardial fistula: case series and literature review. Dis Esophagus 2013;26:457–464. [DOI] [PubMed] [Google Scholar]
- 2. Davidson JP, Connelly TM, Libove E, Tappouni R.. Gastropericardial fistula: radiologic findings and literature review. J Surg Res 2016;203:174–182. [DOI] [PubMed] [Google Scholar]
- 3. Kakarala K, Edriss H, Nugent K.. Gastropericardial fistula as a delayed complication of a Nissen fundoplication. Proc (Bayl Univ Med Cent) 2015;28:478–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dhillon A, Eltweri AM, Shah V, Bowrey DJ.. Gastropericardial fistula after Roux-en-Y bypass for reflux disease. BMJ Case Rep 2015;2015:bcr2014206108.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rodriguez D, Heller MT.. Pneumopericardium due to gastropericardial fistula: a delayed, rare complication of gastric bypass surgery. Emerg Radiol 2013;20:333–335. [DOI] [PubMed] [Google Scholar]
- 6. Suciu BA, Opris M, Bud V, Copotoiu C, Brinzaniuc K, Muresan M.. A fatal complication of an incarcerated diaphragmatic hernia Pyo-pneumopericardium due to a gastro-pericardial fistula, case report and literature review. Ann Ital Chir 2015;86. (ePub) [PubMed] [Google Scholar]
- 7. Neri A, Lambert Y, Marrelli D, Di Mare G, Mastrogiacomo D, Corso G, Volterrani L, Roviello F.. Gastro-pleuro-pericardial fistula following combined radiation and chemotherapy for lung metastases from renal cell carcinoma: report of a case. Surg Today 2013;43:1457–1460. [DOI] [PubMed] [Google Scholar]
- 8. Wells CI, O’Grady G, Bissett IP.. Acute colonic pseudo-obstruction: a systematic review of aetiology and mechanisms. World J Gastroenterol 2017;23:5634–5644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Reicher JJ, Mindelzun R.. Case report: benign gastric ulcer erosion leading to a gastropericardial fistula in a patient with no known risk factors. Clin Imaging 2014;38:547–549. [DOI] [PubMed] [Google Scholar]


