Abstract
Background
Sustained retention in HIV care (RIC) and viral suppression (VS) are central to US national HIV prevention strategies, but have not been comprehensively assessed in criminal justice (CJ) populations with known health disparities. The purpose of this study is to identify predictors of RIC and VS following release from prison or jail.
Methods and findings
This is a retrospective cohort study of all adult people living with HIV (PLWH) incarcerated in Connecticut, US, during the period January 1, 2007, to December 31, 2011, and observed through December 31, 2014 (n = 1,094). Most cohort participants were unmarried (83.7%) men (77.0%) who were black or Hispanic (78.1%) and acquired HIV from injection drug use (72.6%). Prison-based pharmacy and custody databases were linked with community HIV surveillance monitoring and case management databases. Post-release RIC declined steadily over 3 years of follow-up (67.2% retained for year 1, 51.3% retained for years 1–2, and 42.5% retained for years 1–3). Compared with individuals who were not re-incarcerated, individuals who were re-incarcerated were more likely to meet RIC criteria (48% versus 34%; p < 0.001) but less likely to have VS (72% versus 81%; p = 0.048). Using multivariable logistic regression models (individual-level analysis for 1,001 individuals after excluding 93 deaths), both sustained RIC and VS at 3 years post-release were independently associated with older age (RIC: adjusted odds ratio [AOR] = 1.61, 95% CI = 1.22–2.12; VS: AOR = 1.37, 95% CI = 1.06–1.78), having health insurance (RIC: AOR = 2.15, 95% CI = 1.60–2.89; VS: AOR = 2.01, 95% CI = 1.53–2.64), and receiving an increased number of transitional case management visits. The same factors were significant when we assessed RIC and VS outcomes in each 6-month period using generalized estimating equations (for 1,094 individuals contributing 6,227 6-month periods prior to death or censoring). Additionally, receipt of antiretroviral therapy during incarceration (RIC: AOR = 1.33, 95% CI 1.07–1.65; VS: AOR = 1.91, 95% CI = 1.56–2.34), early linkage to care post-release (RIC: AOR = 2.64, 95% CI = 2.03–3.43; VS: AOR = 1.79; 95% CI = 1.45–2.21), and absolute time and proportion of follow-up time spent re-incarcerated were highly correlated with better treatment outcomes. Limited data were available on changes over time in injection drug use or other substance use disorders, psychiatric disorders, or housing status.
Conclusions
In a large cohort of CJ-involved PLWH with a 3-year post-release evaluation, RIC diminished significantly over time, but was associated with HIV care during incarceration, health insurance, case management services, and early linkage to care post-release. While re-incarceration and conditional release provide opportunities to engage in care, reducing recidivism and supporting community-based RIC efforts are key to improving longitudinal treatment outcomes among CJ-involved PLWH.
In a cohort study from the United States, Jaimie P. Meyer and colleagues identify predictors of retention in HIV care and viral suppression following release from prison or jail.
Author summary
Why was this study done?
HIV prevention and treatment strategies aim to reduce HIV-related morbidity, mortality, and transmission by retaining people with HIV in care and sustaining them on antiretroviral treatment to achieve viral suppression (VS).
Few prior studies had described long-term retention in HIV care (RIC) or VS for people incarcerated in prisons or jails and transitioning to communities. In fact, incarceration periods are often excluded from studies of RIC. This is an important knowledge gap because HIV and incarceration are overlapping epidemics that disproportionately affect people who are already marginalized by homelessness, substance use and psychiatric disorders, and socioeconomic status.
What did the researchers do and find?
We merged statewide databases from the Connecticut Department of Correction and Connecticut Department of Public Health on all people living with HIV who were released from prisons or jails in Connecticut, US, between 2007 and 2011. We followed each individual in this cohort for 3 years after release from prison/jail to examine RIC and VS.
Among 1,094 individuals included in the study, continuous RIC declined over time (67.2% retained during year 1, 51.3% retained during years 1–2, and 42.5% retained during all 3 years). Compared with individuals who were not re-incarcerated, individuals who were re-incarcerated were more likely to meet RIC criteria (48% versus 34%; p < 0.001) but less likely to have VS (72% versus 81%; p = 0.048).
Successful RIC and achievement of VS was associated with older age (RIC: adjusted odds ratio [AOR] = 1.61; VS: AOR = 1.37), having health insurance (RIC: AOR = 2.15; VS: AOR = 2.01), being treated for HIV while in prison (RIC: AOR = 1.33; VS: AOR = 1.91), receiving case management services during follow-up (RIC: AOR = 1.79; VS: AOR = 1.31), and early linkage to care in the community following release (RIC: AOR = 2.64; VS: AOR = 1.79). In addition, receiving an increased number of case management visits after release and spending an increased proportion of follow-up time re-incarcerated were correlated with better RIC and VS outcomes.
What do these findings mean?
Dedicated resources are needed to optimize people’s HIV care while they are in prison and to link them to care following release. Although prior studies suggest that prison provides a temporary window of opportunity to reconnect people to care, sustained retention in care and continuity of care ultimately require keeping people in the community longer and avoiding incarceration.
Introduction
Along the HIV care continuum, retention in HIV care (RIC) is necessary for providing antiretroviral therapy (ART) and achieving viral suppression (VS), which reduces individual morbidity, mortality, and forward transmission [1–4]. Most incident HIV infections in the US are acquired from people living with HIV (PLWH) who are either undiagnosed or diagnosed but not retained in HIV care [5–7]. Poor RIC is associated with minority race/ethnicity, younger age, substance use disorders, and incarceration [8–12], although few studies have assessed longitudinal RIC beyond 6- or 12-month follow-up periods [13–16].
The US has the highest incarceration rate globally (910 per 100,000 adults) [17,18], with one-sixth of the country’s 1.2 million PLWH cycling through prisons or jails annually [19]. Yet incarcerated PLWH are frequently censored or excluded altogether from RIC studies [20]. For PLWH engaged in community-based care, frequent brief incarcerations disrupt care, and undermine ART adherence and VS [21–25]. When healthcare is optimized during incarceration, the highly structured environment can be an opportunity to reengage PLWH in care, initiate ART, and achieve VS, though this is often unsustained after release [26–28].
While several recent studies have elucidated challenges with linkage to community care post-release [29–32], the longitudinal impact of incarceration on continuity of HIV care remains poorly understood. Prior studies of RIC that have included criminal justice (CJ)–involved PLWH have been limited by short follow-up [33–35], exclusion of PLWH re-incarcerated during follow-up [34], recall biases in self-reported incarceration and ART use [9,21,24], reliance on ART prescription refill data [25], and inability to comprehensively link community and CJ data [26,28]. Because RIC is currently defined as having a clinic visit with viral load (VL) assessment at least every 6 months, a window of observation beyond 1 year is needed to better understand RIC [36]. Furthermore, a more nuanced understanding of longitudinal RIC among incarcerated PLWH is important for the development of future policies and interventions to address deficiencies within both CJ and community systems of care.
We therefore assessed 3-year RIC and VS in a large retrospective cohort of incarcerated PLWH. We had hypothesized that having health insurance and successfully linking to care would predict sustained RIC, but did not presuppose how recidivism would impact outcomes. Because we linked all community and CJ data within an integrated CJ system, we were able to examine “real world” outcomes in CJ-involved PLWH, accounting for re-incarcerations during follow-up and HIV-1 RNA levels obtained in both CJ and community settings.
Methods
Setting
The Connecticut Department of Correction (CTDOC) has been described previously [32]. Healthcare within CTDOC is guided by federally monitored clinical protocols requiring VL assessment within 96 hours of arrival, with continued monitoring every 3 months during incarceration. ART is prescribed according to national guidelines, which, at the time of observation, used CD4-based criteria.
Data sources
As previously published [32], we combined comprehensive custody and pharmacy data from the CTDOC with the Connecticut Department of Public Health (CTDPH) Enhanced HIV/AIDS Reporting System (eHARS) surveillance and CAREWare service utilization databases. The eHARS surveillance system is maintained by CTDPH to be >95% complete. In the original data analysis plan, we prespecified linkage to and retention in care as major outcomes of interest (S1 Text).
Study population
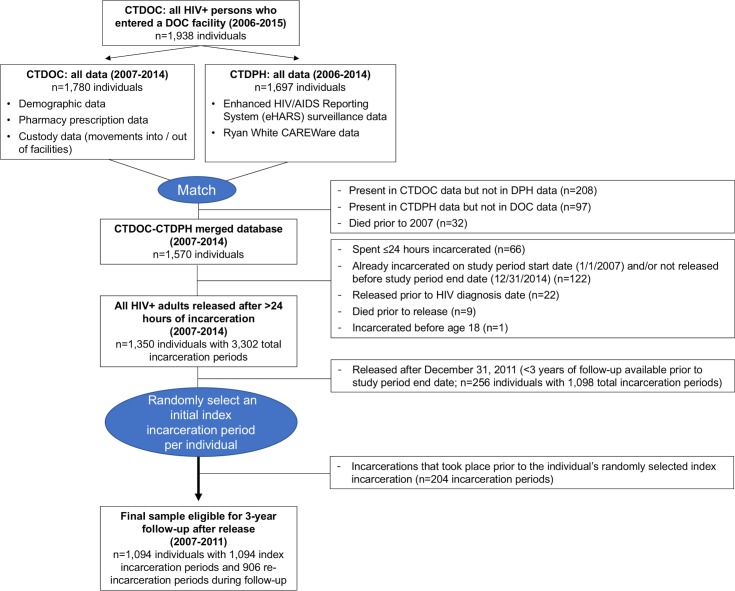
There were 1,094 individuals who met the following inclusion criteria (Fig 1): (1) were ≥18 years old with confirmed HIV before release from CTDOC; (2) were included in CTDOC and CTDPH databases; (3) were incarcerated at least once for >24 hours between January 1, 2007, and December 31, 2011; and (4) had ≥3 years of observation data after release (through December 31, 2014). For individuals never re-incarcerated, their only incarceration period was analyzed as their index incarceration. For participants with multiple eligible incarcerations (n = 538), we randomly selected 1 incarceration period to treat as each individual’s index incarceration/release to avoid differentially biasing the sample toward earlier incarceration periods (when fewer resources were available for HIV treatment and care) or later incarceration periods (with less time to observe outcomes or re-incarcerations). Random selection of index incarceration periods is consistent with an approach justified in prior studies of hospital readmissions and avoids inflating the association between re-incarceration during follow-up and the RIC and VS outcomes [37,38]. Subsequent re-incarcerations were recorded as covariates. Individuals entered the cohort starting on the day of index release from a CTDOC facility and were followed for 3 years or until death. For logistic regression models assessing outcomes after 3 years of follow-up, 1,001 PLWH were included, after excluding 93 deaths. For models using generalized estimating equations (GEEs), the full cohort of 1,094 PLWH contributed 6,227 complete 6-month follow-up periods (prior to death).
Fig 1. Participant flow diagram.
CTDOC, Connecticut Department of Correction; CTDPH, Connecticut Department of Public Health; DOC, Department of Correction; DPH, Department of Public Health.
Data merging
CTDOC databases were securely transferred to the CTDPH, where on-site data managers matched individuals to eHARS and CAREWare databases [32]. CTDOC inmate numbers are routinely reported to the CTDPH by facility nursing supervisors when a new HIV case is diagnosed in prison or by eHARS managers as part of routine data management. Inmate numbers were thus available for a majority of individuals in CTDPH databases. Rather than solely relying on inmate number, the match was done using the Link Plus probabilistic record linkage program developed by the Centers for Disease Control and Prevention (https://www.cdc.gov/cancer/npcr/tools/registryplus/lp.htm), with confirmatory data points including name, date of birth, race, and sex. The merged dataset was further restricted to PLWH currently living in Connecticut (excluding 97 individuals), then de-identified and securely provided to investigators for analysis (Fig 1).
Measures
Recorded HIV-1 RNA VLs served as the proxy for routine HIV care clinic visits (both in prison/jail and in the community), which has demonstrated validity in multiple other settings and is consistent with core indicators for national HIV surveillance [39,40]. Using national RIC guidelines, we defined “sustained 3-year RIC” as having ≥1 VL measured during every 6-month period during the 3-year follow-up period, with ≥60 days between VLs in adjacent periods [36]. Because RIC does not necessarily predict VS and because VL was measured at different frequencies during follow-up, we created a “terminal VS” outcome, defined as having VL < 400 copies/ml measured within the last 6-month period of the 3-year follow-up [1,26]. Using time period as the unit of analysis, additional major outcomes were (1) “RIC over time” (defined as having ≥1 VL measured during a 6-month period) and (2) “VS over time” (defined as having ≥1 VL measured during a 6-month period with the last measured VL being <400 copies/ml). We concluded that the use of a binary outcome in accordance with the standard definitions of RIC would be more appropriate than a survival analysis strategy (which examines time to an event) and would thus provide more clinically meaningful results. PLWH without VL assessments at least every 6 months were defined as being out of care; missing VLs were conservatively assigned VL ≥ 400 copies/ml (non-suppression) by convention [41], which applied to 24.5% (245/1,001) of the individuals and 23.0% (1,432/6,227) of the analyzed 6-month periods in the final multivariable models [42]. VLs were not missing at random, and therefore multiple imputation was not performed. For example, compared to the 756 people with VLs recorded during the last 6-month period of observation, the 245 people with missing VLs were significantly more likely to be uninsured, to have been recently diagnosed with HIV, to have been diagnosed with HIV during index incarceration, to have had fewer re-incarcerations or less time spent re-incarcerated, and to have had fewer case management visits. There were no significant differences between individuals missing and not missing VLs in terms of age, race/ethnicity, or sex. Using the Behavioral Model for Vulnerable Populations framework [43], adapted for CJ populations [44], we examined a broad range of predisposing, enabling/disabling, and need severity factors as potential predictors of RIC and VS over time. Continuous variables that were not normally distributed were categorized or calculated as described below.
Predisposing factors
Predisposing factors included demographic characteristics (sex, race/ethnicity, education level, and marital status), source of HIV transmission, and time since HIV diagnosis. Sex was dichotomized as male/female based on available data; there was no consistent information available on the number of individuals who were transgender, intersex, or gender-nonconforming. Age was dichotomized at the sample median of 45 years. CTDPH databases assessed prior injection drug use (IDU) based on the original HIV risk, and time since HIV diagnosis was calculated by subtracting release date from HIV diagnosis date.
Enabling/Disabling factors
Enabling/disabling factors included year of release, whether HIV was diagnosed during the index incarceration, and health insurance coverage (dichotomous; time-varying in GEE models), which was assessed every 6–12 months in the CAREWare database and dichotomized as yes (public or private insurance) or no (“none”, “unknown”, or “not reported”); if healthcare or social service resources were used without having formal health insurance, persons were designated as uninsured. Using previous criteria, early linkage to care was defined as VL assessment within 14 days after index release [32]. Length of incarceration was calculated using dates and types of movements into and out of facilities and analyzed categorically. Generally, shorter incarcerations (≤30 days) corresponded to jail detentions, whereas longer incarcerations (≥365 days) involved prison sentences. Conditions of release were categorized as unsupervised, conditional release (e.g., parole or transitional housing), or release on bond. Because length of incarceration and conditions of release are closely associated, we created 1 multilevel categorical variable. Re-incarceration (recidivism) was defined as spending >24 hours in a CTDOC facility after initial release. To fully explore the potential effect of re-incarceration, we examined it in 4 ways: dichotomous (re-incarcerated during follow-up or not; time-varying in GEE models), categorical (number of times re-incarcerated during follow-up), total number of days spent in a CTDOC facility during the 3-year follow-up, and percentage of each 6-month period spent in a CTDOC facility (time-varying). Case management visit dates were used to create a dichotomous variable for receipt of case management services during each 6-month period (time-varying) and total number of case management visits over the 3-year follow-up period. CTDOC provides additional psychiatric case management services for those with serious mental illness, but these are not consistently recorded in CAREWare.
Need severity factors
The last VL measured during the index incarceration (within 90 days of release) was used to determine VS status prior to release. ART prescription during incarceration was extracted from pharmacy data and coded dichotomously. Prescribed medications to treat psychiatric disorders (i.e., antipsychotics, antidepressants, or other neuropsychiatric medications), treatment for an opioid use disorder (i.e., medication-assisted therapy with methadone, buprenorphine, or naltrexone as brief supervised withdrawal or maintenance therapy), and treatment of other medical comorbidities were each coded dichotomously. The number of medical conditions other than HIV treated during the incarceration period was summed [44]. As previously described [32], inmates are assigned psychiatric need and addiction severity scores on intake (5-point scale) to determine service programming, with 1–2 (no or low severity), 3 (moderate, requiring treatment), and 4–5 (severe, needing residential or intensive outpatient treatment). Increased psychiatric need was further assessed by combining psychiatric severity score and psychiatric disease treatment to create a 4-category psychiatric need variable (lower severity [score 1–2], untreated; lower severity, treated; higher severity [score 3–5], untreated; higher severity, treated) [32]. Additional information on psychiatric and substance use diagnoses was unavailable.
Statistical analysis
To examine RIC and VS over time, Cochrane–Armitage tests for trend were used to compare the proportion of PLWH with RIC or with VS during year 1, years 1–2, and years 1–3. Chi-squared tests were used to compare RIC for re-incarcerated individuals and those who were not re-incarcerated. Among PLWH with RIC, we assessed the proportion with terminal VS using chi-squared tests. Logistic regression was used to model predictors of 3-year sustained RIC and terminal VS. Then, we examined each 6-month period of the 3-year follow-up period for RIC and VS over time using a logit GEE, assuming an autoregressive correlation structure to account for intra-individual correlation. Observations on the same individual were not assumed to be independent; rather, the GEE model allowed us to account for correlated release periods for the same individual and to calculate appropriate standard errors when performing statistical inference. Individuals who died during follow-up were excluded from logistic regression models but could contribute any complete 6-month time periods before death to the GEE models; including the incomplete periods during which PLWH died did not change effect estimates nor model fit.
For model building, relevant variables within the Behavioral Model for Vulnerable Populations with clinical significance or bivariate associations significant at p < 0.20 were included in full multivariable models. To minimize the Akaike information criterion and maximize the area under the receiver operating characteristic curve, backward selection was used to generate final parsimonious models, including variables with p < 0.05. Sex, race/ethnicity, and recidivism were assessed for significance in parsimonious models a priori. Final logistic regression models were also assessed for fit using Hosmer–Lemeshow goodness-of-fit tests (p > 0.05). Based on tolerance, variance inflation factor, and eigenvalue diagnostics, final models did not have significant multicollinearity. Interactions between race/ethnicity, sex, and recidivism were not found to be statistically significant. Due to small numbers of individuals treated for opioid withdrawal, this variable was only assessed in GEE models. All analyses were performed using SAS version 9.4 (SAS Institute).
Ethics approval
The CTDOC Research Advisory Committee and institutional review boards at Yale University and CTDPH approved all procedures. Participant consent was waived because all data were previously collected and de-identified for analysis.
Results
Sample description
Table 1 summarizes selected characteristics of the included 1,094 PLWH. Half (52.3%) were >45 years old, and most were male (77.0%) and of racial/ethnic minorities (81.8%). Most HIV infections were related to IDU (72.6%) and were not recently diagnosed (96.1%).
Table 1. Description of the full sample of 1,094 individuals initially released from prison or jail during 2007–2011.
| Variable | Full sample n (%)* (n = 1,094 individuals) |
|---|---|
| Predisposing factors | |
| Age at time of release | |
| ≤45 years | 422 (47.7%) |
| >45 years | 572 (52.3%) |
| Sex† | |
| Female | 252 (23.0%) |
| Male | 842 (77.0%) |
| Race/ethnicity | |
| White | 198 (18.1%) |
| Black | 452 (41.2%) |
| Hispanic | 404 (36.9%) |
| Other | 41 (3.8%) |
| Education level | |
| <High school | 508 (46.4%) |
| ≥High school | 586 (53.6%) |
| Marital status‡ | |
| Not married | 887 (83.7%) |
| Married | 173 (16.3%) |
| Injection-drug-use-related source of HIV transmission | |
| No | 300 (27.4%) |
| Yes | 794 (72.6%) |
| Time since HIV diagnosis | |
| ≤1 year | 43 (3.9%) |
| >1 year | 1,051 (96.1%) |
| Enabling or disabling factors | |
| Any health insurance | |
| No insurance/none reported | 478 (43.7%) |
| Yes | 616 (56.3%) |
| HIV diagnosed during index incarceration | |
| No | 1,072 (98.0%) |
| Yes | 22 (2.0%) |
| Year of release | |
| 2007–2008 | 430 (39.3%) |
| 2009–2010 | 469 (42.8%) |
| 2011 | 195 (17.8%) |
| Length of incarceration and conditions of release | |
| Incarcerated ≤30 days, release without conditions | 199 (18.2%) |
| Incarcerated ≤30 days, conditional or bonded release | 144 (13.2%) |
| Incarcerated 31–364 days, release without conditions | 383 (35.0%) |
| Incarcerated 31–364 days, conditional or bonded release | 206 (18.8%) |
| Incarcerated ≥365 days, release without conditions | 71 (6.5%) |
| Incarcerated ≥365 days, conditional release (none were released on bond) | 91 (8.3%) |
| Number of re-incarcerations | |
| 0 | 556 (50.8%) |
| 1 | 274 (25.1%) |
| 2 | 153 (14.0%) |
| ≥3 | 111 (10.2%) |
| Days spent re-incarcerated | |
| 0–6 (<1 week) | 567 (51.8%) |
| 7–30 | 52 (4.8%) |
| 31–90 | 96 (8.8%) |
| 91–180 | 171 (15.6%) |
| 181–365 | 162 (14.8%) |
| >365 | 46 (4.2%) |
| Number of transitional case management visits | |
| 0 | 599 (54.8%) |
| 1–5 | 116 (10.6%) |
| 6–14 | 162 (14.8%) |
| 15–30 | 115 (10.5%) |
| >30 | 102 (9.3%) |
| Early linkage to care (within 14 days of index release) | |
| No | 836 (76.4%) |
| Yes | 230 (21.0%) |
| Re-incarcerated within 14 days | 28 (2.6%) |
| Need severity factors | |
| Prescribed ART during incarceration | |
| No | 458 (41.9%) |
| Yes | 636 (58.1%) |
| Virally suppressed prior to release§ | |
| No | 487 (44.5%) |
| Yes | 357 (32.6%) |
| Viral load not drawn prior to release | 250 (22.9%) |
| Number of medical comorbidities|| | |
| 0 | 677 (61.9%) |
| 1 | 232 (21.2%) |
| ≥2 | 185 (16.9%) |
| Psychiatric need | |
| Lower severity score, untreated | 505 (46.2%) |
| Lower severity score, treated | 53 (4.8%) |
| Higher severity score, untreated | 205 (18.7%) |
| Higher severity score, treated | 331 (30.3%) |
| Addiction severity score¶ | |
| 1–2 | 163 (15.2%) |
| 3 | 708 (66.0%) |
| 4–5 | 201 (18.8%) |
| Treated for an opioid use disorder during index incarceration | |
| No | 1,091 (99.7%) |
| Yes | 3 (0.3%) |
*Numbers listed are n (%) out of the total number of individuals who were initially eligible for analysis (n = 1,094), including those who were found to have died during follow-up (n = 93). Percentages may not sum to 100% due to rounding.
†Transgender males (n = 1) were included the male category, and transgender females (n = 2) were included in the female category.
‡There were n = 34 individuals with a missing or unreported marital status during their index incarceration.
§In 4% of cases, a viral load was drawn within 90 days prior to release, but the viral load value itself was not reported. These cases were included in the “no” viral suppression category because viral suppression could not be confirmed.
||Medical comorbidities broadly included gastrointestinal disease, cardiovascular disease, hyperlipidemia, diabetes, other endocrine disease, viral hepatitis C, hematologic disorders, hypercoagulable states, hypertension, immunological and autoimmune conditions, neurological conditions, pregnancy, pulmonary disease, renal failure, and urological conditions including benign prostatic hypertrophy.
¶There were n = 22 individuals whose addiction severity scores were never assessed during their index incarceration.
Description of retention in care and viral suppression over 3 years
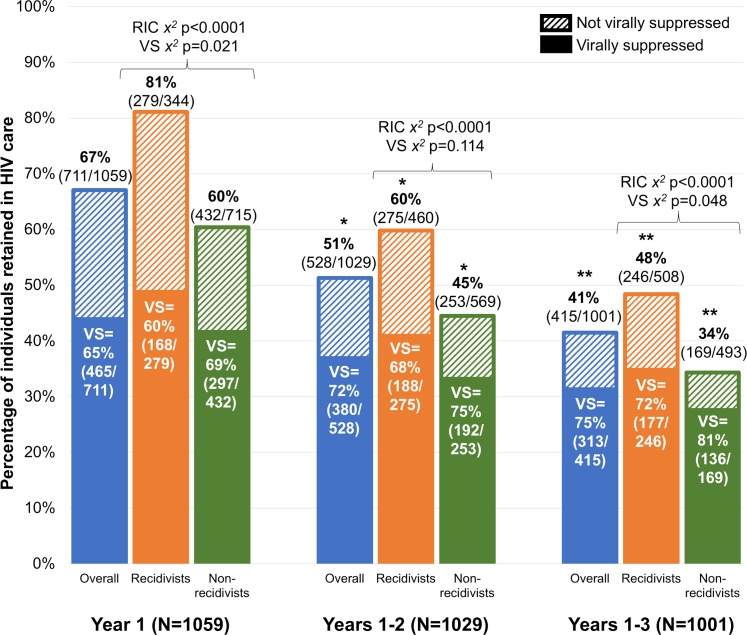
Continuous post-release RIC (i.e., having ≥1 VL measured during every 6-month period, with ≥60 days between VLs in adjacent periods) [36] and VS significantly declined with each additional year of follow-up (Figs 2 and 3, respectively). Excluding deaths (n = 35 in year 1, n = 30 in year 2, and n = 28 in year 3), RIC rates were significantly higher among individuals who were re-incarcerated compared with those who were not within each time frame (Fig 2). Among those retained, however, re-incarcerated individuals were less likely to be virally suppressed than individuals who were not re-incarcerated; this pattern was consistent across all 3 years but statistically significant in year 1 and years 1–3 only.
Fig 2. Longitudinal sustained retention in HIV care (RIC), based on frequency of HIV-1 RNA viral testing, and percentage with viral suppression (VS) at 1, 2, and 3 years post-release, stratified by whether individuals were re-incarcerated (recidivist) at some point during the follow-up period.
There was a statistically significant difference in RIC rates between individuals were re-incarcerated and individuals who were not re-incarcerated across all time points (χ2 p < 0.001). Among those retained, individuals who were not re-incarcerated had higher VS rates compared to re-incarcerated individuals at end of year 1 (χ2 p = 0.021) and year 3 (χ2 p = 0.048). *Statistically significant decline in RIC compared with initial 1-year rates (McNemar’s test p < 0.001). **Statistically significant decline in RIC compared with sustained 2-year rates (McNemar’s test p < 0.001).
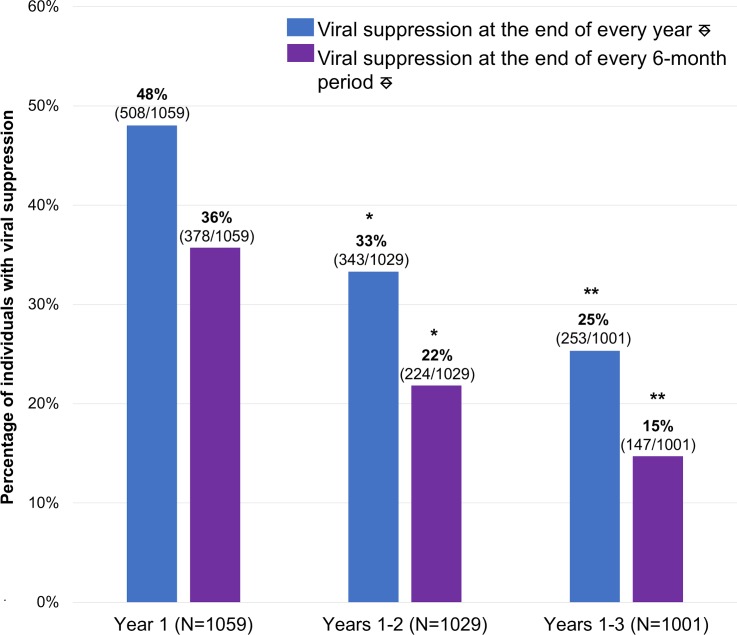
Fig 3. Longitudinal HIV viral suppression (VS) at 1, 2, and 3 years post-release.
⎑Individuals with detectable viral loads during these time frames were considered virally suppressed if their last viral load within the time frame of interest was <400 copies/ml. *Statistically significant decline in VS compared with initial 1-year rates (McNemar’s test p < 0.001). **Statistically significant decline in VS compared with sustained 2-year rates (McNemar’s test p < 0.001).
For all individuals, only re-incarcerated individuals, and only individuals who were not re-incarcerated, there was a statistically significant decline in RIC over time (Cochran–Armitage test 1-way p < 0.001). There was a statistically significant difference in RIC rate between individuals who were re-incarcerated and those who were not across all time points (χ2 p < 0.001). Among those retained, individuals who were not re-incarcerated had higher VS rates compared to re-incarcerated individuals at the end of year 1 (χ2 p = 0.021) and year 3 (χ2 p = 0.048).
Individuals with detectable viral levels during these time frames were considered virally suppressed if their last viral level within the time frame of interest was <400 copies/ml. For both definitions of VS (i.e., VS at the end of every year and at the end of every 6-month period), there was a statistically significant decline in sustained VS over time (Cochran–Armitage test 1-way p < 0.001).
Factors predicting sustained retention in care and VS after 3 years
The 1,001 PLWH who were alive 3 years after release (n = 93 died) were demographically similar to the overall sample, and 41.5% of PLWH met criteria for sustained RIC (Table 2). In the final model, sustained RIC was independently associated with older age (>45 years), having health insurance, being re-incarcerated for >90 days during follow-up, receiving >30 case management visits, and being linked to care or re-incarcerated within 14 days after initial release. VS prior to release was not independently associated with RIC, although not having a VL measured prior to release was negatively associated with RIC.
Table 2. Logistic regression model of sustained retention in care and HIV viral suppression.*.
| Variable | Total n (%)† (n = 1,001 individuals) | Sustained 3-year retention in care | Terminal viral suppression | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Row n (%)‡ with retention | Unadjusted model OR (95% CI) | p-Value | Parsimonious adjusted model OR (95% CI) | p-Value | Row n (%)§ with viral suppression | Unadjusted model OR (95% CI) | p-Value | Parsimonious adjusted model OR (95% CI) | p-Value | ||
| Predisposing factors | |||||||||||
| Age at time of release | |||||||||||
| ≤45 years | 495 (49.5%) | 179 (36.2%) | Referent | Referent | 243 (49.1%) | Referent | Referent | ||||
| >45 years | 506 (50.6%) | 236 (46.6%) | 1.54 (1.20–1.99) | <0.001 | 1.61 (1.22–2.12) | <0.001 | 302 (59.7%) | 1.54 (1.20–1.97) | <0.001 | 1.37 (1.06–1.78) | 0.018 |
| Sex|| | |||||||||||
| Female | 237 (23.7%) | 87 (36.7%) | Referent | 123 (51.9%) | Referent | ||||||
| Male | 764 (76.3%) | 328 (42.9%) | 1.30 (0.96–1.75) | 0.090 | 422 (55.2%) | 1.14 (0.85–1.53) | 0.368 | ||||
| Race/ethnicity | |||||||||||
| White | 177 (17.7%) | 69 (39.0%) | Referent | 102 (57.6%) | Referent | ||||||
| Black | 416 (41.6%) | 175 (42.1%) | 1.14 (0.79–1.63) | 0.485 | 230 (55.3%) | 0.91 (0.64–1.30) | 0.600 | ||||
| Hispanic | 371 (36.1%) | 154 (41.5%) | 1.11 (0.77–1.60) | 0.574 | 194 (52.3%) | 0.81 (0.56–1.16) | 0.242 | ||||
| Other | 37 (3.7%) | 17 (46.0%) | 1.33 (0.65–2.72) | 0.433 | 19 (51.4%) | 0.78 (0.38–1.58) | 0.484 | ||||
| Education level | |||||||||||
| <High school | 456 (45.6%) | 187 (41.0%) | Referent | 236 (51.8%) | Referent | ||||||
| ≥High school | 545 (54.5%) | 228 (41.8%) | 1.04 (0.80–1.33) | 0.792 | 309 (56.7%) | 1.22 (0.95–1.57) | 0.118 | ||||
| Marital status¶ | |||||||||||
| Not married | 814 (84.2%) | 344 (42.3%) | Referent | 442 (54.3%) | Referent | ||||||
| Married | 153 (15.8%) | 62 (40.5%) | 0.93 (0.66–1.32) | 0.691 | 87 (56.9%) | 1.11 (0.78–1.57) | 0.561 | ||||
| Injection drug use | |||||||||||
| No | 281 (28.1%) | 107 (38.1%) | Referent | 148 (52.7%) | Referent | ||||||
| Yes | 720 (71.9%) | 308 (42.8%) | 1.22 (0.92–1.61) | 0.175 | 397 (55.1%) | 1.11 (0.84–1.46) | 0.480 | ||||
| Time since HIV diagnosis | |||||||||||
| ≤1 year | 42 (4.2%) | 11 (26.2%) | Referent | 16 (38.1%) | Referent | ||||||
| >1 year | 959 (95.8%) | 404 (42.1%) | 2.05 (1.02–4.13) | 0.044 | 529 (55.2%) | 2.00 (1.06–3.78) | 0.033 | ||||
| Enabling or disabling factors | |||||||||||
| Any health insurance | |||||||||||
| No insurance/none reported | 419 (41.9%) | 122 (29.1%) | Referent | Referent | 175 (41.8%) | Referent | Referent | ||||
| Yes | 582 (58.1%) | 293 (50.3%) | 2.47 (1.89–3.22) | <0.001 | 2.15 (1.60–2.89) | <0.001 | 370 (63.6%) | 2.43 (1.88–3.15) | <0.001 | 2.01 (1.53–2.64) | <0.001 |
| HIV diagnosed during index incarceration | |||||||||||
| No | 979 (97.8%) | 410 (41.9%) | Referent | 537 (54.9%) | Referent | ||||||
| Yes | 22 (2.2%) | 5 (22.7%) | 2.45 (0.90–6.69) | 0.081 | 8 (36.4%) | 2.13 (0.88–5.11) | 0.092 | ||||
| Year of release | |||||||||||
| 2007–2008 | 382 (38.2%) | 136 (35.6%) | Referent | 181 (47.4%) | Referent | ||||||
| 2009–2010 | 432 (43.2%) | 185 (42.8%) | 1.36 (1.02–1.80) | 0.036 | 241 (55.8%) | 1.40 (1.06–1.85) | 0.017 | ||||
| 2011 | 187 (18.7%) | 94 (50.3%) | 1.83 (1.28–2.61) | <0.001 | 123 (65.8%) | 2.13 (1.49–3.07) | <0.001 | ||||
| Length of incarceration and conditions of release | |||||||||||
| Incarcerated ≤30 days, release without conditions | 175 (17.5%) | 71 (40.6%) | Referent | 88 (50.3%) | Referent | ||||||
| Incarcerated ≤30 days, conditional or bonded release | 125 (12.5%) | 61 (48.8%) | 1.40 (0.88–2.22) | 0.157 | 74 (59.2%) | 1.43 (0.90–2.28) | 0.127 | ||||
| Incarcerated 31–364 days, release without conditions | 353 (35.3%) | 138 (39.1%) | 0.94 (0.65–1.36) | 0.744 | 185 (52.4%) | 1.09 (0.76–1.56) | 0.646 | ||||
| Incarcerated 31–364 days, conditional or bonded release | 190 (19.0%) | 76 (40.0%) | 0.98 (0.64–1.48) | 0.912 | 107 (56.3%) | 1.28 (0.84–1.93) | 0.249 | ||||
| Incarcerated ≥365 days, release without conditions | 70 (7.0%) | 26 (37.1%) | 0.87 (0.49–1.53) | 0.620 | 41 (58.6%) | 1.40 (0.80–2.45) | 0.242 | ||||
| Incarcerated ≥365 days, conditional release (none were released on bond) | 88 (8.8%) | 43 (48.9%) | 1.40 (0.84–2.34) | 0.201 | 50 (56.8%) | 1.30 (0.78–2.18) | 0.317 | ||||
| Number of re-incarcerations | |||||||||||
| 0 | 493 (49.3%) | 169 (34.3%) | Referent | 251 (50.9%) | Referent | ||||||
| 1 | 250 (25.0%) | 101 (40.4%) | 1.30 (0.95–1.78) | 0.102 | 142 (56.8%) | 1.27 (0.93–1.72) | 0.129 | ||||
| 2 | 147 (14.7%) | 82 (55.8%) | 2.42 (1.66–3.52) | <0.001 | 86 (58.5%) | 1.36 (0.94–1.97) | 0.106 | ||||
| ≥3 | 111 (11.1%) | 63 (56.8%) | 2.52 (1.66–3.83) | <0.001 | 66 (59.5%) | 1.41 (0.93–2.15) | 0.104 | ||||
| Days spent re-incarcerated | |||||||||||
| 0–6 (<1 week) | 502 (50.2%) | 171 (34.1%) | Referent | Referent | 254 (50.6%) | Referent | |||||
| 7–30 | 46 (4.6%) | 17 (37.0%) | 1.14 (0.61–2.12) | 0.693 | 1.29 (0.66–2.51) | 0.456 | 26 (56.5%) | 1.27 (0.69–2.33) | 0.443 | ||
| 31–90 | 89 (8.9%) | 37 (41.6%) | 1.38 (0.87–2.18) | 0.173 | 1.47 (0.90–2.41) | 0.122 | 49 (55.1%) | 1.20 (0.76–1.88) | 0.438 | ||
| 91–180 | 163 (16.3%) | 77 (47.3%) | 1.73 (1.21–2.48) | 0.003 | 1.92 (1.29–2.84) | 0.001 | 95 (58.3%) | 1.36 (0.95–1.95) | 0.088 | ||
| 181–365 | 155 (15.5%) | 80 (51.6%) | 2.07 (1.43–2.98) | <0.001 | 2.36 (1.51–3.66) | <0.001 | 89 (57.4%) | 1.32 (0.92–1.89) | 0.138 | ||
| >365 | 46 (4.6%) | 33 (71.7%) | 4.91 (2.52–9.58) | <0.001 | 5.82 (2.80–12.11) | <0.001 | 32 (69.6%) | 2.23 (1.16–4.28) | 0.016 | ||
| Number of transitional case management visits | |||||||||||
| 0 | 532 (53.2%) | 183 (34.4%) | Referent | Referent | 254 (47.7%) | Referent | Referent | ||||
| 1–5 | 110 (11.0%) | 40 (36.4%) | 1.09 (0.71–1.67) | 0.694 | 0.75 (0.47–1.19) | 0.224 | 72 (65.5%) | 2.07 (1.35–3.18) | <0.001 | 1.69 (1.09–2.63) | 0.020 |
| 6–14 | 150 (15.0%) | 73 (48.7%) | 1.81 (1.25–2.61) | 0.002 | 1.12 (0.74–1.68) | 0.604 | 87 (58.0%) | 1.51 (1.05–2.18) | 0.027 | 1.23 (0.84–1.79) | 0.295 |
| 15–30 | 111 (11.1%) | 54 (48.7%) | 1.81 (1.20–2.73) | 0.005 | 0.83 (0.51–1.36) | 0.462 | 61 (55.0%) | 1.34 (0.89–2.01) | 0.168 | 1.08 (0.70–1.65) | 0.731 |
| >30 | 98 (9.8%) | 65 (66.3%) | 3.76 (2.38–5.92) | <0.001 | 1.84 (1.11–3.03) | 0.017 | 71 (72.5%) | 2.88 (1.79–4.63) | <0.001 | 2.04 (1.25–3.34) | 0.005 |
| Early linkage to care (within 14 days of index release) | |||||||||||
| No | 774 (77.3%) | 281 (36.3%) | Referent | Referent | 408 (52.7%) | Referent | |||||
| Yes | 205 (20.5%) | 120 (58.5%) | 2.48 (1.81–3.39) | <0.001 | 2.31 (1.65–3.24) | <0.001 | 125 (61.0%) | 1.40 (1.02–1.92) | 0.035 | ||
| Re-incarcerated within 14 days | 22 (2.2%) | 14 (63.6%) | 3.07 (1.27–7.41) | 0.013 | 2.63 (1.03–6.74) | 0.044 | 12 (54.6%) | 1.08 (0.46–2.52) | 0.865 | ||
| Need severity factors | |||||||||||
| Prescribed ART during incarceration | |||||||||||
| No | 415 (41.5%) | 147 (35.4%) | Referent | 191 (46.0%) | Referent | Referent | |||||
| Yes | 586 (58.5%) | 268 (45.7%) | 1.54 (1.19–1.99) | 0.001 | 354 (60.4%) | 1.79 (1.39–2.31) | <0.001 | 1.39 (1.06–1.82) | 0.016 | ||
| Virally suppressed prior to release | |||||||||||
| No | 439 (43.9%) | 186 (42.4%) | Referent | Referent | 220 (50.1%) | Referent | |||||
| Yes | 333 (33.3%) | 150 (45.1%) | 1.12 (0.84–1.49) | 0.458 | 0.92 (0.67–1.26) | 0.616 | 209 (62.8%) | 1.68 (1.26–2.24) | <0.001 | ||
| Viral load not drawn prior to release | 229 (22.9%) | 79 (34.5%) | 0.72 (0.51–1.00) | 0.049 | 0.65 (0.45–0.93) | 0.020 | 116 (50.7%) | 1.02 (0.74–1.41) | 0.894 | ||
| Number of medical comorbidities | |||||||||||
| 0 | 626 (62.5%) | 237 (37.9%) | Referent | 320 (51.1%) | Referent | ||||||
| 1 | 215 (21.5%) | 97 (45.1%) | 1.35 (0.99–1.85) | 0.061 | 132 (61.4%) | 1.52 (1.11–2.09) | 0.009 | ||||
| ≥2 | 160 (16.0%) | 81 (50.6%) | 1.68 (1.19–2.39) | 0.004 | 93 (58.1%) | 1.33 (0.93–1.89) | 0.114 | ||||
| Psychiatric need | |||||||||||
| Lower severity score, untreated | 457 (45.7%) | 181 (39.6%) | Referent | 234 (51.2%) | Referent | ||||||
| Lower severity score, treated | 50 (5.0%) | 21 (42.0%) | 1.10 (0.61–2.00) | 0.743 | 35 (70.0%) | 2.22 (1.18–4.18) | 0.371 | ||||
| Higher severity score, untreated | 187 (18.7%) | 75 (40.1%) | 1.02 (0.72–1.45) | 0.906 | 103 (55.1%) | 1.17 (0.83–1.64) | 0.013 | ||||
| Higher severity score, treated | 307 (30.7%) | 138 (45.0%) | 1.25 (0.93–1.67) | 0.142 | 173 (56.4%) | 1.23 (0.92–1.65) | 0.162 | ||||
| Addiction severity score** | |||||||||||
| 1–2 | 158 (16.1% | 52 (32.9%) | Referent | 78 (49.4%) | Referent | ||||||
| 3 | 644 (66.7% | 274 (42.6%) | 1.51 (1.05–2.18) | 0.028 | 359 (55.8%) | 1.29 (0.91–1.83) | 0.150 | ||||
| 4–5 | 179 (18.3%) | 78 (43.6%) | 1.57 (1.01–2.46) | 0.045 | 96 (53.6%) | 1.19 (0.77–1.82) | 0.435 | ||||
p-Values in bold are statistically significant (< 0.05).
*Sample is restricted to individuals who were alive at the end of the 3-year follow-up period; there were 93 deaths, resulting in 1,001 individuals eligible for analysis, among whom 41.5% (415/1,001) were retained in care continuously for 3 years and 54.4% (545/1,001) had a viral load < 400 copies/ml at the end of the 3 years.
†Numbers listed are n (%) out of the total number of individuals (n = 1,001). Percentages may not sum to 100% due to rounding.
‡Numbers listed are the row n (%) of individuals who experienced the outcome of sustained retention in care. Percentages should not be expected to sum to 100%.
§Numbers listed are the row n (%) of individuals who experienced the outcome of viral suppression after 3 years of follow-up. Percentages should not be expected to sum to 100%.
||Transgender males (n = 1) were included the male category, and transgender females (n = 2) were included in the female category.
¶Incarceration periods for individuals with missing/unreported marital status (n = 34) were excluded from the bivariate analysis, such that the total n = 1,025.
**Incarceration periods where the addiction severity score was never assessed (n = 20) were excluded from the bivariate analysis, such that the total n = 1,039.
OR, odds ratio.
Overall, 54.4% of individuals demonstrated terminal VS after 3 years of follow-up (Table 2), which was independently associated with age > 45 years, having health insurance, and receiving increased numbers of case management visits. Unlike RIC, VS was not independently associated with the percentage of overall follow-up time spent re-incarcerated. In addition, although VS before release and early linkage to care were not significantly correlated with terminal VS, ART prescribed during incarceration was positively associated with terminal VS.
Factors predicting retention in care and VS over time
The full cohort of 1,094 PLWH contributed 6,227 6-month follow-up periods, with 77.0% of periods meeting the criteria for RIC (Table 3). Independent correlates of RIC per 6-month period were age > 45 years, being diagnosed with HIV >1 year prior to release, having health insurance, having a short (≤30 days) initial incarceration period followed by conditional or bonded release, re-incarceration, increased proportion of follow-up time spent re-incarcerated, receipt of case management services, and early linkage to care post-release. Compared with having a short index incarceration with unconditional release (i.e., “time served”), being incarcerated for ≥1 year with unconditional release was associated with significantly poorer RIC. RIC was also significantly less likely during the final 6-month follow-up period after the index release. Regarding need severity factors, receiving ART and being treated for a medical comorbidity during incarceration were positively associated with RIC, while no VL obtained before release was negatively associated with RIC.
Table 3. Binomial generalized estimating equations of retention in care and viral suppression per 6-month follow-up period.*.
| Variable | Total n (%)† (n = 6,227 6-month periods) | Retention in care over time | Viral suppression over time | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Row n (%)‡ with retention | Unadjusted model OR (95% CI) | p-Value | Parsimonious adjusted model OR (95% CI) | p-Value | Row n (%)§ with viral suppression | Unadjusted model OR (95% CI) | p-Value | Parsimonious adjusted model OR (95% CI) | p-Value | ||
| Predisposing factors | |||||||||||
| Age at time of index release | |||||||||||
| ≤45 years | 3,020 (48.5%) | 2,226 (73.7%) | Referent | Referent | 1,331 (44.1%) | Referent | Referent | ||||
| >45 years | 3,207 (51.5%) | 2,569 (80.1%) | 1.45 (1.20–1.76) | <0.001 | 1.30 (1.07–1.57) | 0.008 | 1,836 (57.3%) | 1.70 (1.44–2.00) | <0.001 | 1.44 (1.22–1.71) | <0.001 |
| Sex|| | |||||||||||
| Female | 1,454 (23.4%) | 1,125 (77.4%) | Referent | 693 (47.7%) | Referent | ||||||
| Male | 4,773 (76.7%) | 3,670 (76.9%) | 0.98 (0.79–1.21) | 0.855 | 2,474 (51.8%) | 1.17 (0.97–1.41) | 0.102 | ||||
| Race/ethnicity | |||||||||||
| White | 1,111 (17.8%) | 849 (76.4%) | Referent | 594 (53.5%) | Referent | ||||||
| Black | 2,584 (41.5%) | 2,028 (78.5%) | 1.13 (0.87–1.45) | 0.369 | 1,315 (50.9%) | 0.90 (0.71–1.13) | 0.356 | ||||
| Hispanic | 2,299 (36.9%) | 1,735 (75.5%) | 0.94 (0.72–1.22) | 0.617 | 1,127 (49.0%) | 0.82 (0.65–1.04) | 0.100 | ||||
| Other | 233 (3.7%) | 183 (78.5%) | 1.12 (0.65–1.92) | 0.680 | 131 (56.2%) | 1.11 (0.72–1.69) | 0.644 | ||||
| Education level | |||||||||||
| <High school | 2,850 (45.8%) | 2,174 (76.3%) | Referent | 1,433 (50.3%) | Referent | ||||||
| ≥High school | 3,377 (54.2%) | 2,621 (77.6%) | 1.10 (0.91–1.33) | 0.325 | 1,734 (51.4%) | 1.07 (0.91–1.27) | 0.411 | ||||
| Marital status | |||||||||||
| Not married | 5,048 (83.8%) | 3,906 (77.4%) | Referent | 2,533 (50.2%) | Referent | ||||||
| Married | 975 (16.2%) | 738 (75.7%) | 0.89 (0.69–1.16) | 0.401 | 516 (52.9%) | 1.10 (0.87–1.39) | 0.420 | ||||
| Injection drug use | |||||||||||
| No | 1,733 (27.8%) | 1,280 (73.9%) | Referent | 751 (43.3%) | Referent | Referent | |||||
| Yes | 4,494 (72.2%) | 3,515 (78.2%) | 1.27 (1.03–1.56) | 0.025 | 2,416 (53.8%) | 1.49 (1.23–1.81) | <0.001 | 1.31 (1.07–1.60) | 0.009 | ||
| Time since HIV diagnosis | |||||||||||
| ≤1 year | 253 (4.1%) | 155 (61.3%) | Referent | Referent | 86 (34.0%) | Referent | |||||
| >1 year | 5,974 (95.9%) | 4,640 (77.7%) | 2.22 (1.40–3.53) | <0.001 | 1.66 (1.05–2.62) | 0.029 | 3,081 (51.6%) | 2.13 (1.33–3.42) | 0.002 | ||
| Enabling or disabling factors | |||||||||||
| Health insurance** | |||||||||||
| No insurance/none reported | 4,267 (68.5%) | 3,128 (73.3%) | Referent | Referent | 1,966 (46.1%) | Referent | Referent | ||||
| Yes | 1,960 (31.5%) | 1,667 (85.1%) | 1.60 (1.36–1.88) | <0.001 | 1.61 (1.34–1.94) | <0.001 | 1,201 (61.3%) | 1.41 (1.25–1.60) | <0.001 | 1.18 (1.02–1.38) | 0.028 |
| Length of index incarceration and conditions of index release | |||||||||||
| Incarcerated ≤30 days, release without conditions | 1,106 (17.8%) | 834 (75.4%) | Referent | Referent | 519 (46.9%) | Referent | Referent | ||||
| Incarcerated ≤30 days, conditional release | 78 (1.3%) | 67 (85.9%) | 2.22 (0.97–5.05) | 0.058 | 2.29 (1.00–5.27) | 0.050 | 52 (66.7%) | 2.20 (0.96–5.02) | 0.061 | 2.38 (1.08–5.28) | 0.033 |
| Incarcerated ≤30 days, bonded release | 712 (11.4%) | 573 (80.5%) | 1.39 (0.96–2.02) | 0.077 | 1.66 (1.14–2.40) | 0.008 | 384 (53.9%) | 1.33 (0.97–1.82) | 0.072 | 1.58 (1.16–2.17) | 0.004 |
| Incarcerated 31–364 days, release without conditions | 2,201 (35.4%) | 1,652 (75.1%) | 1.00 (0.75–1.32) | 0.979 | 0.77 (0.58–1.02) | 0.068 | 1,028 (46.7%) | 1.03 (0.80–1.31) | 0.840 | 0.76 (0.59–0.97) | 0.029 |
| Incarcerated 31–364 days, conditional release | 1,062 (17.1%) | 825 (77.7%) | 1.19 (0.87–1.62) | 0.282 | 0.80 (0.58–1.10) | 0.169 | 572 (53.9%) | 1.38 (1.04–1.82) | 0.025 | 0.86 (0.65–1.14) | 0.299 |
| Incarcerated 31–364 days, bonded release | 116 (1.9%) | 92 (79.3%) | 1.28 (0.64–2.58) | 0.487 | 0.99 (0.52–1.89) | 0.986 | 50 (43.1%) | 0.85 (0.45–1.60) | 0.620 | 0.67 (0.37–1.22) | 0.193 |
| Incarcerated ≥365 days, release without conditions | 420 (6.7%) | 312 (74.3%) | 0.95 (0.62–1.44) | 0.799 | 0.55 (0.36–0.84) | 0.006 | 228 (54.3%) | 1.38 (0.94–2.01) | 0.099 | 0.69 (0.47–1.02) | 0.060 |
| Incarcerated ≥365 days, conditional release (none released on bond) | 532 (8.5%) | 440 (82.7%) | 1.64 (1.09–2.46) | 0.018 | 0.96 (0.62–1.48) | 0.863 | 334 (62.8%) | 2.03 (1.43–2.87) | <0.001 | 1.16 (0.82–1.63) | 0.397 |
| Re-incarcerated** | |||||||||||
| No | 5,325 (85.5%) | 3,931 (73.8%) | Referent | Referent | 2,696 (50.6%) | Referent | Referent | ||||
| Yes | 902 (14.5%) | 864 (95.8%) | 5.24 (4.04–6.79) | <0.001 | 2.27 (1.44–3.58) | <0.001 | 471 (52.2%) | 0.99 (0.86–1.13) | 0.836 | 0.65 (0.51–0.81) | <0.001 |
| Percent time spent re-incarcerated** | |||||||||||
| 0% | 5,019 (80.6%) | 3,653 (72.8%) | Referent | Referent | 2,494 (49.7%) | Referent | Referent | ||||
| 1%–50% | 749 (12.0%) | 698 (93.2%) | 4.35 (3.31–5.71) | <0.001 | 2.56 (1.67–3.91) | <0.001 | 367 (49.0%) | 0.98 (0.85–1.14) | 0.812 | 1.38 (1.08–1.76) | 0.010 |
| 51%–100% | 459 (7.4%) | 444 (96.7%) | 8.69 (5.34–14.16) | <0.001 | 5.39 (3.15–9.22) | <0.001 | 306 (66.7%) | 1.72 (1.40–2.11) | <0.001 | 2.52 (1.91–3.32) | <0.001 |
| Year of index release | |||||||||||
| 2007–2008 | 2,405 (38.6%) | 1,777 (73.9%) | Referent | 1,049 (43.6%) | Referent | Referent | |||||
| 2009–2010 | 2,677 (43.0%) | 2,074 (77.5%) | 1.24 (1.00–1.52) | 0.046 | 1,418 (53.0%) | 1.49 (1.24–1.80) | <0.001 | 1.04 (0.85–1.27) | 0.712 | ||
| 2011 | 1,145 (18.4%) | 944 (82.5%) | 1.65 (1.25–2.16) | <0.001 | 700 (61.1%) | 2.02 (1.60–2.56) | <0.001 | 1.60 (1.24–2.06) | 0.003 | ||
| Transitional case management services** | |||||||||||
| No | 5,126 (82.3%) | 3,803 (74.2%) | Referent | Referent | 2,489 (48.6%) | Referent | Referent | ||||
| Yes | 1,101 (17.7%) | 992 (90.1%) | 2.32 (1.91–2.82) | <0.001 | 1.79 (1.44–2.22) | <0.001 | 678 (61.6%) | 1.48 (1.28–1.70) | <0.001 | 1.31 (1.12–1.53) | <0.001 |
| Early linkage to care | |||||||||||
| No | 4,798 (77.1%) | 3,541 (73.8%) | Referent | Referent | 2,277 (47.5%) | Referent | Referent | ||||
| Yes | 1,296 (20.8%) | 1,142 (88.1%) | 2.77 (2.15–3.57) | <0.001 | 2.64 (2.03–3.43) | <0.001 | 824 (63.6%) | 1.95 (1.59–2.39) | <0.001 | 1.79 (1.45–2.21) | <0.001 |
| Re-incarcerated within 14 days without any community viral load | 133 (2.1%) | 112 (84.2%) | 1.91 (0.82–4.47) | 0.135 | 1.57 (0.68–3.63) | 0.295 | 66 (49.6%) | 1.07 (0.60–1.91) | 0.811 | 1.05 (0.56–1.98) | 0.874 |
| Time since index release†† | |||||||||||
| 0 to <6 months | 1,080 (17.3%) | 853 (79.0%) | Referent | Referent | 522 (48.3%) | Referent | Referent | ||||
| 6 to <12 months | 1,059 (17.0%) | 826 (78.0%) | 0.95 (0.80–1.12) | 0.519 | 1.02 (0.85–1.23) | 0.802 | 511 (48.3%) | 1.00 (0.89–1.12) | 0.978 | 1.00 (0.87–1.15) | 1.000 |
| 12 to <18 months | 1,039 (16.7%) | 796 (76.6%) | 0.87 (0.73–1.04) | 0.123 | 0.86 (0.71–1.05) | 0.132 | 519 (50.0%) | 1.06 (0.93–1.22) | 0.357 | 1.04 (0.89–1.22) | 0.607 |
| 18 to <24 months | 1,029 (16.5%) | 789 (76.7%) | 0.87 (0.73–1.05) | 0.139 | 0.88 (0.72–1.08) | 0.228 | 535 (52.0%) | 1.15 (1.00–1.33) | 0.058 | 1.14 (0.96–1.35) | 0.137 |
| 24 to <30 months | 1,019 (16.4%) | 775 (76.1%) | 0.84 (0.70–1.01) | 0.071 | 0.84 (0.68–1.04) | 0.104 | 535 (52.5%) | 1.18 (1.01–1.36) | 0.032 | 1.14 (0.96–1.36) | 0.133 |
| 30 to 36 months | 1,001 (16.1%) | 756 (75.5%) | 0.83 (0.69–0.99) | 0.038 | 0.81 (0.65–0.99) | 0.041 | 545 (54.5%) | 1.28 (1.10–1.48) | 0.001 | 1.26 (1.06–1.49) | 0.010 |
| Need severity factors | |||||||||||
| Prescribed ART during index incarceration | |||||||||||
| No | 2,577 (41.4%) | 1,855 (72.0%) | Referent | Referent | 994 (38.6%) | Referent | Referent | ||||
| Yes | 3,650 (58.6%) | 2,940 (80.6%) | 1.63 (1.35–1.97) | <0.001 | 1.33 (1.07–1.65) | 0.011 | 2,173 (59.5%) | 2.46 (2.07–2.91) | <0.001 | 1.91 (1.56–2.34) | <0.001 |
| Virally suppressed prior to index releas | |||||||||||
| No | 2,744 (44.1%) | 2,112 (77.0%) | Referent | Referent | 1,190 (43.4%) | Referent | Referent | ||||
| Yes | 2,059 (33.1%) | 1,653 (80.3%) | 1.23 (0.98–1.54) | 0.068 | 1.06 (0.84–1.33) | 0.620 | 1,302 (63.2%) | 2.37 (1.96–2.87) | <0.001 | 1.94 (1.59–2.37) | <0.001 |
| Viral load not drawn prior to release | 1,424 (22.9%) | 1,030 (72.3%) | 0.77 (0.61–0.97) | 0.029 | 0.71 (0.56–0.91) | 0.006 | 675 (47.4%) | 1.19 (0.96–1.47) | 0.117 | 1.18 (0.95–1.47) | 0.130 |
| Number of medical comorbidities | |||||||||||
| 0 | 3,874 (62.2%) | 2,872 (74.1%) | Referent | Referent | 1,818 (46.9%) | Referent | |||||
| 1 | 1,334 (21.4%) | 1,079 (80.9%) | 1.49 (1.17–1.90) | 0.001 | 1.29 (1.01–1.66) | 0.046 | 750 (56.2%) | 1.48 (1.21–1.83) | <0.001 | ||
| ≥2 | 1,019 (16.4%) | 844 (82.8%) | 1.73 (1.33–2.24) | <0.001 | 1.29 (0.96–1.74) | 0.096 | 599 (58.8%) | 1.64 (1.31–2.07) | <0.001 | ||
| Psychiatric need | |||||||||||
| Lower severity score, untreated | 2,853 (45.8%) | 2,146 (75.2%) | Referent | 1,353 (47.4%) | Referent | Referent | |||||
| Lower severity score, treated | 312 (5.0%) | 255 (81.7%) | 1.47 (0.97–2.23) | 0.069 | 199 (63.8%) | 2.06 (1.38–3.09) | <0.001 | 1.47 (0.97–2.21) | 0.068 | ||
| Higher severity score, untreated | 1,166 (18.7%) | 889 (76.2%) | 1.04 (0.80–1.34) | 0.772 | 598 (51.3%) | 1.15 (0.91–1.45) | 0.233 | 1.36 (1.07–1.72) | 0.011 | ||
| Higher severity score, treated | 1,896 (30.5%) | 1,505 (79.4%) | 1.28 (1.02–1.60) | 0.035 | 1,017 (53.6%) | 1.31 (1.08–1.59) | 0.006 | 1.07 (0.87–1.31) | 0.510 | ||
| Addiction severity score during index incarceration‡‡ | |||||||||||
| 1–2 | 957 (15.7%) | 685 (71.6%) | Referent | 425 (44.4%) | Referent | ||||||
| 3 | 4,030 (66.0%) | 3,129 (77.6%) | 1.38 (1.07–1.79) | 0.013 | 2,110 (52.4%) | 1.38 (1.09–1.75) | 0.008 | ||||
| 4–5 | 1,118 (18.3%) | 874 (78.2%) | 1.44 (1.05–1.97) | 0.024 | 561 (50.2%) | 1.29 (0.96–1.73) | 0.091 | ||||
| Treated for an opioid use disorder during index incarceration | |||||||||||
| No | 6,209 (99.7%) | 4,779 (77.0%) | Referent | 3,152 (50.8%) | Referent | ||||||
| Yes | 18 (0.3%) | 16 (88.9%) | 2.17 (0.35–13.42) | 0.405 | 15 (83.3%) | 4.84 (0.71–33.10) | 0.108 | ||||
p-Values in bold are statistically significant (< 0.05).
*Sample is restricted to 6-month follow-up periods where individuals were alive at the end of the 6-month period. There were 6,227 6-month post-release periods (1,080 individual-based clusters) eligible for analysis, of which there were 4,795 (77.0%) 6-month post-release periods during which at least 1 viral load was drawn (retained in care) and 3,167 (50.9%) 6-month post-release periods in which the last viral level obtained was <400 copies/ml (virally suppressed).
†Numbers listed are n (%) out of the total number of 6-month time periods (n = 6,227). Percentages may not sum to 100% due to rounding.
‡Numbers listed are the row n (%) of 6-month time periods during which the individual experienced the outcome of retention in care. Percentages should not be expected to sum to 100%.
§Numbers listed are the row n (%) of 6-month time periods during which the individual experienced the outcome of viral suppression. Percentages should not be expected to sum to 100%.
||Transgender males (n = 1) were included the male category, and transgender females (n = 2) were included in the female category.
¶Follow-up periods for individuals with missing/unreported marital status (n = 204) were excluded from the bivariate analysis, such that the total n = 6,023.
**Variable refers to the 6-month interval rather than the individual or index incarceration.
††In a sensitivity analysis of probability of viral suppression over time (by Cochran–Armitage test), there was a significant trend toward higher probability of viral suppression with increased time since initial release.
‡‡Follow-up periods where the addiction severity score was never assessed (n = 122) were excluded from the bivariate analysis, such that the total n = 6,105.
OR, odds ratio.
VS was reported in 50.9% of the eligible 6-month periods (Table 3). In GEE models, independent correlates of VS per 6-month period were age > 45 years, IDU-related transmission risk, having health insurance, having a short index incarceration period (≤30 days) followed by conditional or bonded release, increased percentage of follow-up time spent re-incarcerated, receipt of case management services, and early linkage to care. Unlike for RIC, disabling factors for VS were re-incarceration and a medium length of incarceration (31–364 days) followed by unconditional release. VS was also significantly better for more contemporary releases and during the final 6-month follow-up period after the index release. Receipt of ART, VS, and untreated high psychiatric need during incarceration were need severity factors each positively associated with VS over time.
Discussion
To our knowledge, this is one of the longest assessments of RIC and VS in a large cohort of individuals with HIV released from prison or jail. Despite HIV being a chronic condition that requires lifelong treatment, prior longitudinal RIC studies in the general population have not accounted for the complex impact of incarceration and the unique vulnerabilities it represents for many PLWH [8,11,14–16]. By comprehensively linking multiple CJ and community-based data sources, we were able to follow all CJ-involved PLWH statewide, including those re-incarcerated. We identified major correlates of optimal HIV treatment outcomes and found that the impact of re-incarceration is complex and dependent on time spent in facilities and conditions of release. These findings offer new insights into potential strategies to improve RIC and VS in CJ-involved PLWH.
Rates of sustained RIC and VS significantly declined over time, with re-incarcerated individuals demonstrating higher RIC rates than individuals who were not re-incarcerated, across all 3 years. Re-incarceration likely represents “forced” reengagement in care, but was not necessarily associated with VS itself. Rather, the length of time one spent in correctional facilities was associated with RIC and VS per 6-month interval and over the 3 years of observation. These findings speak not only to the potential for incarceration to facilitate reengagement in HIV care within a structured setting that can provide appropriate care and resources [21,25,26], but also to the potential for re-incarceration to interrupt HIV care. Re-incarceration itself was associated with worse VS outcomes, which is consistent with literature showing an association between incarceration, ART non-adherence, and virological failure [21,24,25]. Short-term benefits gained during incarceration appear to be outweighed by the long-term harm incarceration inflicts on physical and mental health, especially after release [45].
Individuals who were not re-incarcerated and who demonstrated RIC in the community had significantly higher VS rates compared with re-incarcerated individuals, underscoring the importance of better supporting community-based RIC through expanded enabling resources like case management and health insurance and minimizing recidivism, which is disruptive both medically and socially [46,47]. This finding is consistent with that from a recent study in North Carolina and Rhode Island showing that PLWH released from prison and retained in community care (without being re-incarcerated) had similar VS rates to PLWH continuously engaged in community care [48]. Sentencing policies, particularly for drug-related or nonviolent offenses, should be modified to encourage community-based CJ rehabilitation and engagement in community-based healthcare and to facilitate access to post-release resources like psychiatric and addiction treatment, both of which improve RIC and reduce recidivism [49–54].
Engaging PLWH in the HIV care continuum during and immediately after release significantly impacts longitudinal RIC. PLWH whose VLs were adequately monitored, who were prescribed ART, or who achieved VS before release had better RIC over time. Also, early linkage to care (within 2 weeks) post-release was associated with sustained 3-year RIC as well as RIC and VS over time. Paradoxically, prisons/jails influence longitudinal HIV treatment outcomes, especially when community-based resources are inadequate. Many PLWH likely benefit from CJ-based services as a safety net as long as these services are integrated, continuous, and align health and justice priorities. If jail/prison services are comprehensive and coordinated, jails and prisons can serve as highly effective “patient-centered medical homes” [55]. Despite these opportunities, the uneven and often disjointed care provided in CJ settings and the detrimental medical and social consequences alongside the excessive financial burden associated with mass incarceration in the US favor supporting less costly, integrated community healthcare systems to improve care for PLWH [45,54,56–59].
Having a short index incarceration with subsequent supervised release was associated with increased RIC and VS over time relative to both short and longer incarcerations with unconditional release. PLWH with brief incarcerations may not lose their social and medical community-based ties [60] and consequently, with post-release support from CJ supervision, may better reintegrate back into the community [58]. Conditional release may also facilitate RIC by providing an access point for PLWH to engage in social and medical services, whereas PLWH released on bond may represent a population with greater financial resources or social support that improves their ability to navigate the healthcare system [29].
In randomized trials, transitional case management services for incarcerated PLWH are no better than pre-release discharge planning at improving post-release linkage to care and retention [32,33,61]. Within an integrated prison/jail system, and when targeted to those most in need, case management may require a differentiated service delivery model that caters to PLWH at highest risk for recidivism. Differentiated service delivery is a client-centered approach that simplifies and targets key services (e.g., health insurance and treatment for addiction and psychiatric disorders) needed along the HIV continuum to reduce unnecessary burdens on the health system [33,34,62]. In the absence of such services, multiple stressors and barriers to care can lead to substance use relapse, high-risk behaviors, and suboptimal healthcare engagement, such as defaulting from ART, which undermine VS [63–65]. Unlike prior studies, findings here demonstrate that transitional case management is a key enabling factor that is strongly associated with RIC and VS. Despite the important role of case management to facilitate health insurance and community services to improve RIC and VS [32,65], most PLWH (54.8%) did not receive these services, and health insurance coverage remained low (56.3%) over 3 years of follow-up. This indicates an urgent need to expand the provision of case management services both during and after the transition to the community.
When RIC and VS did not significantly improve despite numerous case management visits, it is likely that those PLWH had multiple severe medical and social needs. Thus, the positive effect of case management may be masked by the higher baseline need of those who received these services compared with those who were not targeted to receive case management. Unlike in Connecticut, most states terminate insurance benefits during incarceration [62], with findings here supporting the need to reexamine policies that promote continuation of, reactivation of, or potentially new enrollment into insurance before release.
Unlike previous studies [20,56], IDU transmission risk and high psychiatric need correlated with VS over time. While IDU and psychiatric need were not associated with frequency of transitional case management utilization, such individuals may have received additional psychiatric case management to link and retain them in treatment for psychiatric or substance use disorders, which could have improved VS. Also, some PLWH with an IDU history died early during follow-up, including from drug overdose [66], which limited our ability to clearly assess the role of current or past IDU on longitudinal HIV treatment outcomes.
Other limitations of the study included limited data regarding post-release housing status and psychiatric and substance use disorders. Addiction and psychiatric severity scores were our best indicators for comorbidities that potentially impact RIC in the community. We also could not fully measure brief fluctuations in insurance status.
Strengths of the study included the ability to follow both individuals who were re-incarcerated and those who were not, for an extended period of time, and to account for many factors that changed over time, including health insurance status. Instead of using prescription refill or clinic visit data to approximate RIC and VS, our outcomes were constructed using reliably and systematically reported biological data and used standardized, generalizable, and clinically justifiable definitions of RIC and VS. Defining missing VL data as indicating being out of care and not having VS may have biased findings, but is a standardized analytic convention that provides conservative estimates [40,41,67], given that a very small proportion of PLWH may have moved out of state and not been fully measured despite extensive efforts by CTDPH to cross-check interstate databases. Finally, we minimized typical database linkage challenges through the use of complete databases (aside from psychiatric case management data), reliable variables for individual matching, and CTDPH database managers with considerable experience linking data.
Despite some limitations, this study is, to our knowledge, one of the first to extensively identify correlates of longitudinal RIC and VS for all PLWH in a CJ setting, while simultaneously describing and accounting for the complex impact of incarceration. RIC decreases markedly after release from prison/jail, but several key factors correlate with improved RIC and VS after release, including provision of HIV care during incarceration, health insurance, case management, and early linkage to care post-release. While re-incarceration and conditional release facilitate engagement in care for some PLWH, our findings strongly indicate that strategies that reduce recidivism and support community-based RIC will yield better treatment outcomes than using re-incarceration as a mechanism to promote RIC in this population. Improving RIC and VS will, however, require policy changes, including expanding health insurance through new enrollments and avoiding suspension; expanding and targeting transitional case management to those at risk for recidivism and poor health outcomes; aligning community supervision (i.e., probation and parole) with healthcare by promoting continued care for HIV, psychiatric disorders, and addiction (which often requires health insurance) to avoid recidivism; and screening for and treating psychiatric and substance use disorders, and continuing these treatments post-release. Such changes in policy will likely positively influence HIV treatment outcomes while diminishing the negative consequences of mass incarceration, especially for racial/ethnic minorities in the US.
Supporting information
(DOC)
(DOCX)
(PDF)
Acknowledgments
This research was conducted in collaboration with CTDOC and CTDPH. We thank Kathleen Maurer, Patrick Hynes, Cheryl Cepelak, and Heidi Jenkins for assisting with study design, guiding the interpretation of our findings, and fostering the inter-institutional collaborations that made this study possible. We also thank Kirsten Shea, Suzanne Speers, Michael Ostapoff, and Melanie Alvarez for their invaluable assistance with data collection, extraction, and linkage; no compensation was received for these contributions. Finally, we sincerely thank Paula Dellamura for her crucial administrative support.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations
- AOR
adjusted odds ratio
- ART
antiretroviral therapy
- CJ
criminal justice
- CTDOC
Connecticut Department of Correction
- CTDPH
Connecticut Department of Public Health
- eHARS
Enhanced HIV/AIDS Reporting System
- GEE
generalized estimating equation
- IDU
injection drug use
- PLWH
people living with HIV
- RIC
retention in HIV care
- VL
viral load
- VS
viral suppression
Data Availability
Because of the highly confidential nature of the data (related to people's HIV status and incarcerations), access to data is highly regulated by the Connecticut Departments of Correction and Public Health. Data are available to researchers who receive permission from these organizations and meet criteria for access to confidential data. Interested researchers should contact Suzanne Speers (suzanne.speers@ct.gov) or Kirsten Shea (kshea@uchc.edu).
Funding Statement
The National Institute on Drug Abuse (NIDA) provided funding for this project through grants F30DA041247 (KBL), K23DA033858 (JPM), K24DA017072 (FLA), R01DA030768 (FLA), and R01DA030762. The project was also supported by the Yale University Medical Scientist Training Program under the National Institute of General Medical Sciences (NIGMS) T32GM007205 and the Yale Center for Interdisciplinary Research in AIDS (CIRA) under the National Institute of Mental Health (NIMH) P30MH062294. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.AIDSinfo. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents Washington (DC): US Department of Health and Human Services; 2018. [cited 2018 Feb 28]. Available from: https://aidsinfo.nih.gov/contentfiles/lvguidelines/glchunk/glchunk_458.pdf. [Google Scholar]
- 2.Crawford TN. Poor retention in care one-year after viral suppression: a significant predictor of viral rebound. AIDS Care. 2014;26(11):1393–9. 10.1080/09540121.2014.920076 [DOI] [PubMed] [Google Scholar]
- 3.Mugavero MJ, Westfall AO, Cole SR, Geng EH, Crane HM, Kitahata MM, et al. Beyond core indicators of retention in HIV care: missed clinic visits are independently associated with all-cause mortality. Clin Infect Dis. 2014;59(10):1471–9. 10.1093/cid/ciu603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tripathi A, Youmans E, Gibson JJ, Duffus WA. The impact of retention in early HIV medical care on viro-immunological parameters and survival: a statewide study. AIDS Res Hum Retroviruses. 2011;27(7):751–8. 10.1089/AID.2010.0268 [DOI] [PubMed] [Google Scholar]
- 5.Shah M, Perry A, Risher K, Kapoor S, Grey J, Sharma A, et al. Effect of the US National HIV/AIDS Strategy targets for improved HIV care engagement: a modelling study. Lancet HIV. 2016;3(3):e140–6. 10.1016/S2352-3018(16)00007-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Skarbinski J, Rosenberg E, Paz-Bailey G, Hall HI, Rose CE, Viall AH, et al. Human immunodeficiency virus transmission at each step of the care continuum in the United States. JAMA Intern Med. 2015;175(4):588–96. 10.1001/jamainternmed.2014.8180 [DOI] [PubMed] [Google Scholar]
- 7.amfAR. Curbing the HIV epidemic by supporting effective engagement in HIV care New York: amfAR; 2016. [cited 2018 Sep 7]. Available from: http://www.amfar.org/uploadedFiles/_amfarorg/Articles/On_The_Hill/2016/DC-2016-Engagement-Policy-Report_081916-October.pdf. [Google Scholar]
- 8.Ulett KB, Willig JH, Lin HY, Routman JS, Abroms S, Allison J, et al. The therapeutic implications of timely linkage and early retention in HIV care. AIDS Patient Care STDS. 2009;23(1):41–9. 10.1089/apc.2008.0132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Westergaard RP, Hess T, Astemborski J, Mehta SH, Kirk GD. Longitudinal changes in engagement in care and viral suppression for HIV-infected injection drug users. AIDS. 2013;27(16):2559–66. 10.1097/QAD.0b013e328363bff2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yehia BR, Rebeiro P, Althoff KN, Agwu AL, Horberg MA, Samji H, et al. Impact of age on retention in care and viral suppression. J Acquir Immune Defic Syndr. 2015;68(4):413–9. 10.1097/QAI.0000000000000489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rebeiro P, Althoff KN, Buchacz K, Gill J, Horberg M, Krentz H, et al. Retention among North American HIV-infected persons in clinical care, 2000–2008. J Acquir Immune Defic Syndr. 2013;62(3):356–62. 10.1097/QAI.0b013e31827f578a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giordano TP, Hartman C, Gifford AL, Backus LI, Morgan RO. Predictors of retention in HIV care among a national cohort of US veterans. HIV Clin Trials. 2009;10(5):299–305. 10.1310/hct1005-299 [DOI] [PubMed] [Google Scholar]
- 13.Rowan SE, Burman WJ, Johnson SC, Connick E, Reirden D, Daniloff E, et al. Engagement-in-care during the first 5 years after HIV diagnosis: data from a cohort of newly HIV-diagnosed individuals in a large US city. AIDS Patient Care STDS. 2014;28(9):475–82. 10.1089/apc.2013.0340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Colasanti J, Kelly J, Pennisi E, Hu YJ, Root C, Hughes D, et al. Continuous retention and viral suppression provide further insights into the HIV care continuum compared to the cross-sectional HIV care cascade. Clin Infect Dis. 2016;62(5):648–54. 10.1093/cid/civ941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fleishman JA, Yehia BR, Moore RD, Korthuis PT, Gebo KA. Establishment, retention, and loss to follow-up in outpatient HIV care. J Acquir Immune Defic Syndr. 2012;60(3):249–59. 10.1097/QAI.0b013e318258c696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crepaz N, Tang T, Marks G, Mugavero MJ, Espinoza L, Hall HI. Durable viral suppression and transmission risk potential among persons with diagnosed HIV infection: United States, 2012–2013. Clin Infect Dis. 2016;63(7):976–83. 10.1093/cid/ciw418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glaze LE, Kaeble D. Correctional populations in the United States, 2013 Washington (DC): Bureau of Justice Statistics; 2014. [cited 2018 Sep7]. Available from: https://www.bjs.gov/content/pub/pdf/cpus13.pdf. [Google Scholar]
- 18.Dolan K, Wirtz AL, Moazen B, Ndeffo-Mbah M, Galvani A, Kinner SA, et al. Global burden of HIV, viral hepatitis, and tuberculosis in prisoners and detainees. Lancet. 2016;388(10049):1089–102. 10.1016/S0140-6736(16)30466-4 [DOI] [PubMed] [Google Scholar]
- 19.Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006: declining share of epidemic but persistent public health opportunity. PLoS ONE. 2009;4(11):e7558 10.1371/journal.pone.0007558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bulsara SM, Wainberg ML, Newton-John TRO. Predictors of adult retention in HIV care: a systematic review. AIDS Behav. 2018;22(3):752–64. 10.1007/s10461-016-1644-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Westergaard RP, Kirk GD, Richesson DR, Galai N, Mehta SH. Incarceration predicts virologic failure for HIV-infected injection drug users receiving antiretroviral therapy. Clin Infect Dis. 2011;53(7):725–31. 10.1093/cid/cir491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lim S, Harris TG, Nash D, Lennon MC, Thorpe LE. All-cause, drug-related, and HIV-related mortality risk by trajectories of jail incarceration and homelessness among adults in New York City. Am J Epidemiol. 2015;181(4):261–70. 10.1093/aje/kwu313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pai NP, Estes M, Moodie EE, Reingold AL, Tulsky JP. The impact of antiretroviral therapy in a cohort of HIV infected patients going in and out of the San Francisco county jail. PLoS ONE. 2009;4(9):e7115 10.1371/journal.pone.0007115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Milloy MJ, Kerr T, Buxton J, Rhodes T, Guillemi S, Hogg R, et al. Dose-response effect of incarceration events on nonadherence to HIV antiretroviral therapy among injection drug users. J Infect Dis. 2011;203(9):1215–21. 10.1093/infdis/jir032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Palepu A, Tyndall MW, Chan K, Wood E, Montaner JS, Hogg RS. Initiating highly active antiretroviral therapy and continuity of HIV care: the impact of incarceration and prison release on adherence and HIV treatment outcomes. Antivir Ther. 2004;9(5):713–9. [PubMed] [Google Scholar]
- 26.Meyer JP, Cepeda J, Wu J, Trestman RL, Altice FL, Springer SA. Optimization of human immunodeficiency virus treatment during incarceration: viral suppression at the prison gate. JAMA Intern Med. 2014;174(5):721–9. 10.1001/jamainternmed.2014.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Milloy MJ, Montaner JS, Wood E. Incarceration of people living with HIV/AIDS: implications for treatment-as-prevention. Curr HIV/AIDS Rep. 2014;11(3):308–16. 10.1007/s11904-014-0214-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meyer JP, Cepeda J, Springer SA, Wu J, Trestman RL, Altice FL. HIV in people reincarcerated in Connecticut prisons and jails: an observational cohort study. Lancet HIV. 2014;1(2):e77–84. 10.1016/S2352-3018(14)70022-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baillargeon J, Giordano TP, Rich JD, Wu ZH, Wells K, Pollock BH, et al. Accessing antiretroviral therapy following release from prison. JAMA. 2009;301(8):848–57. 10.1001/jama.2009.202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baillargeon JG, Giordano TP, Harzke AJ, Baillargeon G, Rich JD, Paar DP. Enrollment in outpatient care among newly released prison inmates with HIV infection. Public Health Rep. 2010;125(Suppl 1):64–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Montague BT, Rosen DL, Sammartino C, Costa M, Gutman R, Solomon L, et al. Systematic assessment of linkage to care for persons with HIV released from corrections facilities using existing datasets. AIDS Patient Care STDS. 2016;30(2):84–91. 10.1089/apc.2015.0258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Loeliger KB, Altice FL, Desai MM, Ciarleglio MM, Gallagher C, Meyer JP. Predictors of linkage to HIV care and viral suppression after release from jails and prisons: a retrospective cohort study. Lancet HIV. 2018;5(2):e96–106. 10.1016/S2352-3018(17)30209-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Althoff AL, Zelenev A, Meyer JP, Fu J, Brown SE, Vagenas P, et al. Correlates of retention in HIV care after release from jail: results from a multi-site study. AIDS Behav. 2013;17(Suppl 2):S156–70. 10.1007/s10461-012-0372-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spaulding AC, Messina LC, Kim BI, Chung KW, Lincoln T, Teixeira P, et al. Planning for success predicts virus suppressed: results of a non-controlled, observational study of factors associated with viral suppression among HIV-positive persons following jail release. AIDS Behav. 2013;17(Suppl 2):S203–11. 10.1007/s10461-012-0341-8 [DOI] [PubMed] [Google Scholar]
- 35.Subramanian Y, Khan MN, Berger S, Foisy M, Singh A, Woods D, et al. HIV outcomes at a Canadian remand centre. Int J Prison Health. 2016;12(3):145–56. 10.1108/IJPH-12-2015-0041 [DOI] [PubMed] [Google Scholar]
- 36.Health Resources and Services Administration. HIV/AIDS Bureau performance measures Rockville (MD): Health Resources and Services Administration; 2015. [cited 2018 Sep 7]. Available from: https://hab.hrsa.gov/sites/default/files/hab/About/clinical-quality-management/coremeasures.pdf. [Google Scholar]
- 37.Bratzler DW, Normand SL, Wang Y, O’Donnell WJ, Metersky M, Han LF, et al. An administrative claims model for profiling hospital 30-day mortality rates for pneumonia patients. PLoS ONE. 2011;6(4):e17401 10.1371/journal.pone.0017401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lindenauer PK, Bernheim SM, Grady JN, Lin Z, Wang Y, Wang Y, et al. The performance of US hospitals as reflected in risk-standardized 30-day mortality and readmission rates for medicare beneficiaries with pneumonia. J Hosp Med. 2010;5(6):E12–8. 10.1002/jhm.822 [DOI] [PubMed] [Google Scholar]
- 39.Hu YW, Kinsler JJ, Sheng Z, Kang T, Bingham T, Frye DM. Using laboratory surveillance data to estimate engagement in care among persons living with HIV in Los Angeles County, 2009. AIDS Patient Care STDS. 2012;26(8):471–8. 10.1089/apc.2011.0371 [DOI] [PubMed] [Google Scholar]
- 40.Cohen SM, Hu X, Sweeney P, Johnson AS, Hall HI. HIV viral suppression among persons with varying levels of engagement in HIV medical care, 19 US jurisdictions. J Acquir Immune Defic Syndr. 2014;67(5):519–27. 10.1097/QAI.0000000000000349 [DOI] [PubMed] [Google Scholar]
- 41.Centers for Disease Control and Prevention. Guidance on community viral load: a family of measures, definitions, and method for calculation Atlanta: Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 42.Committee for Medicinal Products for Human Use. Guideline on missing data in confirmatory clinical trials London: European Medicines Agency; 2010. [Google Scholar]
- 43.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–302. [PMC free article] [PubMed] [Google Scholar]
- 44.Chen NE, Meyer JP, Avery AK, Draine J, Flanigan TP, Lincoln T, et al. Adherence to HIV treatment and care among previously homeless jail detainees. AIDS Behav. 2013;17(8):2654–66. 10.1007/s10461-011-0080-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wildeman C, Wang EA. Mass incarceration, public health, and widening inequality in the USA. Lancet. 2017;389(10077):1464–74. 10.1016/S0140-6736(17)30259-3 [DOI] [PubMed] [Google Scholar]
- 46.Morenoff JD, Harding DJ. Incarceration, prisoner reentry, and communities. Annu Rev Sociol. 2014;40:411–29. 10.1146/annurev-soc-071811-145511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McNeil R, Kerr T, Coleman B, Maher L, Milloy MJ, Small W. Antiretroviral therapy interruption among HIV postive people who use drugs in a setting with a community-wide HIV treatment-as-prevention initiative. AIDS Behav. 2017;21(2):402–9. 10.1007/s10461-016-1470-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Costa M, Montague BT, Solomon L, Sammartino C, Gutman R, Zibman C, et al. Assessing the effect of recent incarceration in prison on hiv care retention and viral suppression in two states. J Urban Health. 2018;95(4):499–507. 10.1007/s11524-018-0255-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wilton G, Stewart LA. Outcomes of offenders with co-occurring substance use disorders and mental disorders. Psychiatr Serv. 2017;68(7):704–9. 10.1176/appi.ps.201500391 [DOI] [PubMed] [Google Scholar]
- 50.Kesten KL, Leavitt-Smith E, Rau DR, Shelton D, Zhang W, Wagner J, et al. Recidivism rates among mentally ill inmates: impact of the Connecticut Offender Reentry Program. J Correct Health Care. 2012;18(1):20–8. 10.1177/1078345811421117 [DOI] [PubMed] [Google Scholar]
- 51.Tracy K, Burton M, Nich C, Rounsaville B. Utilizing peer mentorship to engage high recidivism substance-abusing patients in treatment. Am J Drug Alcohol Abuse. 2011;37(6):525–31. 10.3109/00952990.2011.600385 [DOI] [PubMed] [Google Scholar]
- 52.Colins O, Vermeiren R, Vahl P, Markus M, Broekaert E, Doreleijers T. Psychiatric disorder in detained male adolescents as risk factor for serious recidivism. Can J Psychiatry. 2011;56(1):44–50. 10.1177/070674371105600108 [DOI] [PubMed] [Google Scholar]
- 53.Wilson AB, Draine J, Hadley T, Metraux S, Evans A. Examining the impact of mental illness and substance use on recidivism in a county jail. Int J Law Psychiatry. 2011;34(4):264–8. 10.1016/j.ijlp.2011.07.004 [DOI] [PubMed] [Google Scholar]
- 54.Schmitt J, Warner K, Gupta S. The high budgetary cost of incarceration Washington (DC): Center for Economic and Policy Research; 2010. [cited 2018 Sep 7]. Available from: http://cepr.net/documents/publications/incarceration-2010-06.pdf. [Google Scholar]
- 55.Miller WL. Patient-centered medical home (PCMH) recognition: a time for promoting innovation, not measuring standards. J Am Board Fam Med. 2014;27(3):309–11. 10.3122/jabfm.2014.03.140079 [DOI] [PubMed] [Google Scholar]
- 56.Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376(9738):367–87. 10.1016/S0140-6736(10)60829-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Springer SA, Spaulding AC, Meyer JP, Altice FL. Public health implications for adequate transitional care for HIV-infected prisoners: five essential components. Clin Infect Dis. 2011;53(5):469–79. 10.1093/cid/cir446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Haney C. The psychological impact of incarceration: implications for post-prison adjustment Washington (DC): US Department of Health and Human Services; 2001. [Google Scholar]
- 59.McVay D, Schiraldi V, Ziedenberg J. Treatment or incarceration. National and state findings on the efficacy and cost savings of drug treatment versus imprisonment Washington (DC): Justice Policy Institute; 2004. [cited 2018 Sep 7]. Available from: http://www.justicepolicy.org/uploads/justicepolicy/documents/04-01_rep_mdtreatmentorincarceration_ac-dp.pdf. [Google Scholar]
- 60.Desmond M. Disposable ties and the urban poor. Am J Sociol. 2012;117(5):1295–335. 10.1086/663574 [DOI] [Google Scholar]
- 61.Booker CA, Flygare CT, Solomon L, Ball SW, Pustell MR, Bazerman LB, et al. Linkage to HIV care for jail detainees: findings from detention to the first 30 days after release. AIDS Behav. 2013;17(Suppl 2):S128–36. 10.1007/s10461-012-0354-3 [DOI] [PubMed] [Google Scholar]
- 62.FamiliesUSA. Medicaid eligibility for people leaving incarceration is smart policy Washington (DC): FamiliesUSA; 2016. July 12 [cited 2017 Aug 6]. Available from: http://familiesusa.org/sites/default/files/product_documents/ENR_Suspension%20v.%20Termination%20Map%20Infographic_07-12-16.pdf. [Google Scholar]
- 63.Luther JB, Reichert ES, Holloway ED, Roth AM, Aalsma MC. An exploration of community reentry needs and services for prisoners: a focus on care to limit return to high-risk behavior. AIDS Patient Care STDS. 2011;25(8):475–81. 10.1089/apc.2010.0372 [DOI] [PubMed] [Google Scholar]
- 64.Haley DF, Golin CE, Farel CE, Wohl DA, Scheyett AM, Garrett JJ, et al. Multilevel challenges to engagement in HIV care after prison release: a theory-informed qualitative study comparing prisoners’ perspectives before and after community reentry. BMC Public Health. 2014;14:1253 10.1186/1471-2458-14-1253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yehia BR, Stephens-Shields AJ, Fleishman JA, Berry SA, Agwu AL, Metlay JP, et al. The HIV care continuum: changes over time in retention in care and viral suppression. PLoS ONE. 2015;10(6):e0129376 10.1371/journal.pone.0129376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Loeliger KB, Altice FL, Ciarleglio MM, Rich KM, Chandra DK, Gallagher C, et al. All-cause mortality among people with HIV released from an integrated system of jails and prisons in Connecticut, USA, 2007-14: a retrospective observational cohort study. Lancet HIV. 2018. September 6 pii: S2352-3018(18)30175-9. 10.1016/S2352-3018(18)30175-9 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Edelman EJ, Tate JP, Fiellin DA, Brown ST, Bryant K, Gandhi N, et al. Impact of defined clinical population and missing data on temporal trends in HIV viral load estimation within a health care system. HIV Med. 2015;16(6):346–54. 10.1111/hiv.12219 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOCX)
(PDF)
Data Availability Statement
Because of the highly confidential nature of the data (related to people's HIV status and incarcerations), access to data is highly regulated by the Connecticut Departments of Correction and Public Health. Data are available to researchers who receive permission from these organizations and meet criteria for access to confidential data. Interested researchers should contact Suzanne Speers (suzanne.speers@ct.gov) or Kirsten Shea (kshea@uchc.edu).