Abstract
Objective
To understand stroke risk factors, status of stroke care, and opportunities for improvement as China and India develop national strategies to address their disproportionate and growing burden of stroke.
Methods
We compared stroke risk factors, acute management, adherence to quality performance measures, and clinical outcomes among hospitalized ischemic stroke patients using data from the Indo-US Collaborative Stroke Project (IUCSP) and China National Stroke Registry-II (CNSR-II). The IUCSP included 5 academic stroke centers from different geographic regions (n = 2,066). For comparison, the CNSR-II dataset was restricted to 31 academic hospitals among 219 participating sites from 31 provinces (n = 1,973).
Results
Indian patients were significantly younger, had health insurance less often, and had significantly different risk factors (more often diabetes mellitus, dyslipidemia, and coronary heart disease; less often prior stroke, hypertension, atrial fibrillation, and smoking). Hospitalized Indian patients had greater stroke severity (median NIH Stroke Scale score 10 vs 4), higher rates of IV thrombolysis within 3 hours (7.5% vs 2.4%), greater in-hospital mortality (7.9% vs 1.2%), and worse outcome (3-month modified Rankin Scale score 0–2, 49.3% vs 78.1%) (all p < 0.001). The poorer clinical outcomes were attributable mainly to greater stroke severity in IUCSP patients. Chinese patients more often received antithrombotics, stroke education, and dysphagia screening during hospitalization.
Conclusion
These data provide insights into the status of ischemic stroke care in academic urban centers within 2 large Asian countries. Further research is needed to determine whether these patterns are representative of care across the countries, to explain differences in observed severity, and to drive improvements.
Stroke burden is increasing, especially in low- and middle-income countries.1 China and India, which account for more than one-third of the world's population,2 have a major stroke burden.3,4 In China, the age-standardized incidence and prevalence rates are 246.8 and 1,114.8 per 100,000 person-years.5 In India, the incidence and prevalence rates are estimated to be 117 to 145 and 147 to 922 per 100,000 population.4 As China and India develop national strategies to address their growing burden of stroke, it is important to compare stroke risk factors and the status of stroke care and to understand their effect on the process of stroke care and outcomes. We used the data from China National Stroke Registry-II (CNSR-II)6 and Indo-US Collaborative Stroke Project (IUCSP)7,8 to compare demographics, risk factors, stroke quality performance measures, and clinical outcomes in China and India.
Methods
Standard protocol approvals, registrations, and patient consents
This comparative project was approved by the Ethics Committee of the IUCSP participating hospitals and the Central Institutional Review Board of Beijing Tiantan Hospital. For both registries, trained research coordinators reviewed the medical records daily to identify and enroll consecutive eligible patients at each hospital. Written informed consent was obtained. Data were prospectively entered in a secure web-based electronic platform.
The IUCSP
The IUCSP was a multicenter hospital-based study conducted at 5 high-volume academic tertiary hospitals across India funded by the US NIH and the Indian government's Department of Biotechnology to study the inpatient profile of ischemic stroke, to train a core group of researchers to stimulate stroke infrastructure development, and to lay the foundation for future scientific collaborations.7,8 Patients were enrolled consecutively from January 2012 until August 2014 if they met the following criteria: ischemic stroke symptoms of <2 weeks’ duration with imaging-confirmed infarction or perfusion deficit by CT or MRI or >70% stenosis in the relevant artery for patients with transient symptoms. Data variables and definitions were consistent with the NIH Stroke Common Data Elements and American Heart Association's Get With The Guidelines (AHA-GWTG)–Stroke datasets, plus risk behaviors or variables relevant to India (e.g., beedi, paan tobacco consumption). Admission NIH Stroke Scale (NIHSS) scores were obtained by certified physicians or coinvestigators.
The CNSR-II
The CNSR-II, launched in 2012 by the Ministry of Health of China, is a nationwide database focusing on the delivery of stroke care in clinical practice. Hospitals are classified into 3 grades according to location, bed numbers, staff expertise, and facilities.9 Patients were recruited consecutively from 219 hospitals from June 2012 to January 2013 if they met the following criteria: age ≥18 years; diagnosis of ischemic stroke, TIA, spontaneous intracerebral hemorrhage, or subarachnoid hemorrhage within 1 week confirmed by CT or MRI; and direct hospital admission from a physician's clinic or emergency department. Detailed methods have been published.6
Comparison of registry data
We included all 2,066 patients from the IUCSP. The CNSR-II has a total of 19,604 patients with acute ischemic stroke admitted to 219 hospitals, including 127 (58%) academic hospitals. To allow comparison, we restricted the CNSR-II cohort to the 1,973 ischemic stroke patients admitted to 31 academic (grade III) hospitals10 (1 from each of 27 provinces and 4 municipalities in Mainland China, with convenience sampling to select target hospitals from provinces having >1 grade III hospital).
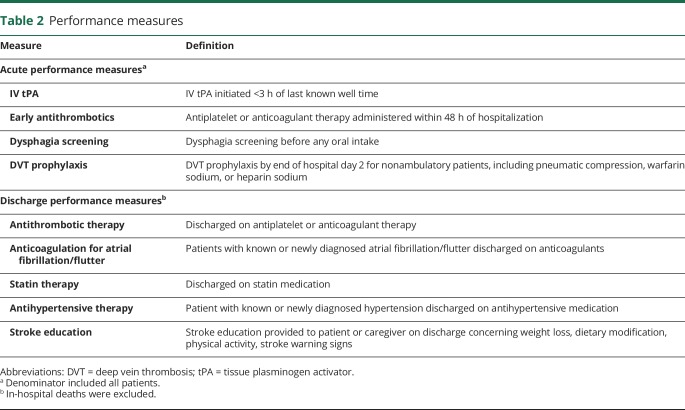
Baseline variables common to both registries are listed in table 1. Risk factors such as hypertension, diabetes mellitus, and smoking were considered present if documented in the medical chart or if supported by laboratory values or clinical assessments. In addition, 9 stroke quality performance metrics were compared (table 2): (1) IV tissue plasminogen activator (tPA) therapy; (2) antithrombotic medication by the end of hospital day 2; (3) deep vein thrombosis (DVT) prophylaxis by the end of day 2 for nonambulatory patients; (4) dysphagia screening before any oral intake; (5) antithrombotic medication on discharge; (6) anticoagulation for atrial fibrillation/flutter on discharge; (7) antihypertensive medication; (8) statin treatment; and (9) stroke education. These performance measures were similar but not identical to the AHA-GWTG performance measures because of language and cultural differences (table 2).
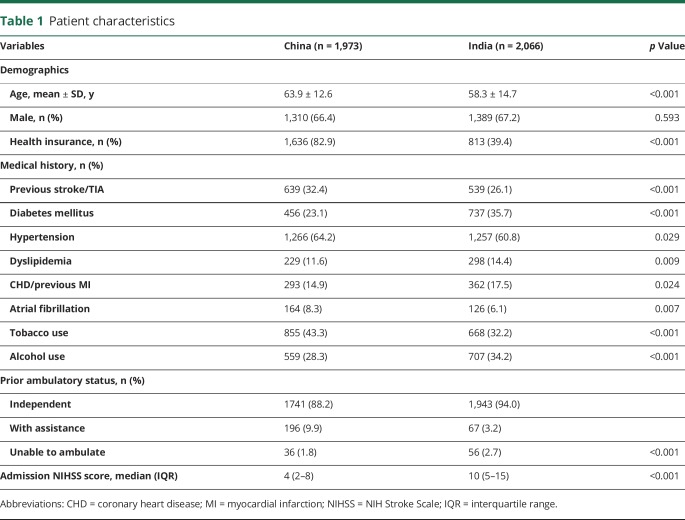
Table 1.
Patient characteristics
Table 2.
Performance measures
In-hospital outcomes included pneumonia and all-cause mortality. Pneumonia was defined as the presence of clinical/laboratory features (fever, cough, auscultatory findings, new purulent sputum, or positive sputum culture) supported by chest x-ray results. Finally, we compared 3-month modified Rankin Scale (mRS) scores, which were obtained during follow-up visits by clinicians or via telephone by trained and certified research personnel using standardized scripts.
Statistical analysis
Student t, χ2, Pearson, and Wilcoxon rank-sum tests were used as appropriate. Missing data were excluded from the denominator. Multivariable logistic regression analyses were conducted to identify predictors of favorable 3-month outcome (mRS score ≤2), including all variables significant at p < 0.10 on univariate testing. A value of p < 0.05 was considered statistically significant. Statistical analyses were performed with SAS version 9.3 (SAS Institute Inc, Cary, NC).
Data availability
All data used for analysis are presented in the tables. Data will be shared after ethics approval if requested by other investigators for purposes of replicating the results.
Results
Table 1 shows baseline characteristics. Patients in the IUCSP were significantly younger by an average of 5 years; the sex distribution was similar. The IUCSP patients had health insurance less often, although both populations were predominantly covered by government insurance. The vascular risk profile was significantly different between groups, with IUSCP patients having significantly greater rates of diabetes mellitus, dyslipidemia, coronary heart disease, and alcohol use and the CSNR-II patients having significantly higher rates of prior stroke, hypertension, atrial fibrillation, and tobacco use (in the IUSCP, tobacco use included consumption of beedi, paan, hukka, and other indigenous products).
In Indian academic centers, hospitalized patients had greater stroke severity (median NIHSS score 10 vs 4, p < 0.001). Among patients presenting to IUCSP hospitals, the rate of IV tPA administered within 3 hours was 7.5% vs 2.4% in CSNR-II (p < 0.001).
In India, tPA is approved for use up to 4.5 hours and endovascular treatment is available. An additional 84 patients received IV tPA either at the transferring hospital or between 3 and 4.5 hours (including 30 who underwent bridging with intra-arterial lysis) for an overall IV tPA rate of 11.5%; in addition, endovascular treatment alone was administered to 29 (1.4%) patients.
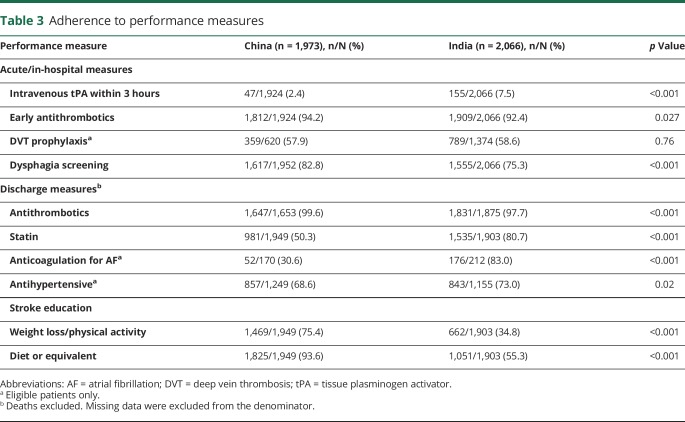
Table 3 shows performance on in-hospital and discharge quality measures. The CSNR-II data reflected greater adherence to guideline-recommended stroke quality performance, e.g., significantly higher rates of antithrombotics within 48 hours of admission, dysphagia screening, antithrombotics on discharge, and stroke education concerning weight loss, physical activity, and dietary modification on discharge. IUCSP patients received significantly more stroke preventive medications, including statins, anticoagulants for atrial fibrillation, and antihypertensives.
Table 3.
Adherence to performance measures
Outcomes
On univariate testing, CSNR-II patients had lower rates of in-hospital pneumonia (8.3% vs 12.7%, p < 0.001) and in-hospital mortality (1.2% vs 7.9%) and more favorable outcomes (78.1% vs 49.3% with mRS score 0–2, p < 0.001). After adjustment for baseline variables shown in table 1, patients in the CSNR-II showed significantly lower odds of pneumonia (odds ratio [OR] 0.50, 95% confidence interval [CI] 0.39–0.65), in-hospital mortality (OR 0.11, 95% CI 0.07–0.19), and better 3-month outcome (mRS score 0–2, OR 3.11, 95% CI 2.47–3.92).
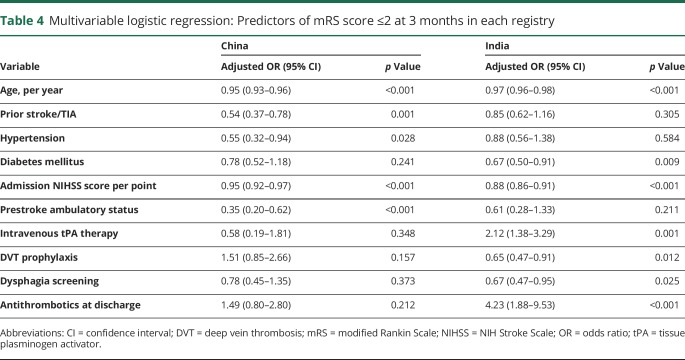
Multivariable analyses showed that younger age and lower admission NIHSS scores were associated with 3-month favorable outcome in both China and India (table 4). Prior stroke/TIA, hypertension, and independent ambulatory status were inversely associated with favorable outcome in China but not in India; diabetes mellitus was inversely associated with favorable outcome in India but not in China. Interventions such as IV recombinant tPA treatment, DVT prophylaxis, and dysphagia screening were associated with 3-month favorable outcome in India but not in China.
Table 4.
Multivariable logistic regression: Predictors of mRS score ≤2 at 3 months in each registry
Discussion
Our results provide important insights into the differences in stroke risk factors, acute and in-hospital management, and outcomes in 2 large cohorts of hospitalized patients with acute ischemic stroke in China and India. Similar to other efforts comparing stroke between countries,11,12 this first detailed comparison of stroke demographics, risk factors, and inpatient management in China and India provides data that may improve resource allocation in national stroke prevention and management strategies, evaluate their effect of over time, and foster collaboration. Furthermore, these comparative data are relevant to recent studies showing opportunities for improvement of stroke prevention guidelines in low- and middle-income countries such as China and India.13
While both groups developed stroke at younger ages compared to Western populations,14 Indian patients were significantly younger than Chinese patients. Stroke was male preponderant in both countries, likely due to a higher incidence and possible cultural biases resulting in men being evaluated and admitted more often than women. There was a relatively high burden of modifiable risk factors in both countries. The rates of hypertension, diabetes mellitus, and dyslipidemia in IUCSP were lower than previously reported in individual Indian hospital-based registries, probably reflecting the larger scope of the IUCSP. The rates in this restricted CSNR-11 sample were consistent with rates reported in the overall CSNR-II registry.1,4–6,15 The rates of diabetes mellitus and tobacco use were much higher and the rates of hypertension and atrial fibrillation were much lower in China and India compared to AHA-GWTG data from the United States.14 Strategies such as increasing tobacco taxes, reducing tobacco-product advertisements, labeling foods with sugar, cholesterol, and salt content, and promoting physical exercise are globally important, but some strategies may need greater focus in China (e.g., antitobacco efforts), and diabetes prevention may need more effort in India. Atrial fibrillation, on the other hand, does not appear to be as important in these countries compared to the West. Health insurance was relatively low, especially in India; however, the CSNR-II and IUCSP were conducted in academic government hospitals where insurance status has little or no effect on health care delivery. Nevertheless, these data may be relevant to the future of health insurance in both countries.
There were significant differences in stroke severity and rates of IV tPA administration. These results mainly reflect disparities in resource availability and the systems of care between the 2 countries. In China, all patients with ischemic stroke are admitted and offered IV tPA from 0 to 3 hours if eligible; the tPA delivery rate, however, is relatively low due to patient factors such as affordability, risk aversion, and lesser stroke severity.16 In India, as a result of limited inpatient bed availability at hospitals like those participating in the registry, patients with severe stroke and thrombolysis are preferentially admitted, and others are sent to lower-level hospitals or home. The relatively high rate of tPA in IUCSP is also attributable to the 24/7 coverage by experienced physicians in enrolling hospitals, the subsidized cost of tPA in India, and government financial support to hospitals offering tPA. These data do not reflect the national rates of tPA use in India. More efforts are still needed to improve acute stroke care, including prehospital notification, prompt access to emergency departments with urgent head CT capability, training of key personnel, and wider availability of thrombolysis in both countries.
Lower stroke severity on admission contributes to the lower rates of in-hospital pneumonia and mortality and better 3-month clinical outcome observed in Chinese patients compared with those in India. However, systems of care may be more advanced in China, contributing to better outcomes. For example, CSNR-II showed higher rates of early antithrombotics, dysphagia screening, and stroke education at discharge. Of note, the number of patients eligible for DVT prophylaxis was lower in China, presumably due to preserved ambulation and consistent with the lower stroke severity of admitted patients; however, the rate of DVT prophylaxis was similar in both countries. Statins and anticoagulant medications were less frequently prescribed at discharge in China as a result of multiple barriers to care, including the limited availability of regular international normalized ratio testing, the cost of medications, and patient and physician concerns about adverse effects. Compared to data from AHA-GWTG–Stroke,14 the rates of DVT prophylaxis, dysphagia screening, and discharge medications and education were substantially lower in China and India than in the United States, suggesting opportunities to develop national quality improvement programs. Education and training of health care personnel should be a key component of such programs, especially given the relatively low number of neurologists and stroke-trained physicians in these countries.17
Substantial differences were observed in the adjusted OR for many variables associated with good outcomes between the 2 countries. The reasons for this are not apparent, and there are no data within the registries to address this question. These differences may be due to differences in hospital- or patient-level unmeasured confounders, to differences in postdischarge care and adherence to prescribed interventions, or to patient-level factors such as stroke mechanism, genetics, or unhealthy behaviors.
Because the IUCSP and selected CSNR-II hospitals are urban tertiary centers with stroke experts, our data likely do not reflect nationwide risk factor prevalence or quality of care in China and India. Therefore, the results of our study have limited generalizability to academic hospital practice. However, these registries provide the best available and reliable evidence for tertiary stroke care in both countries, and the hospital locations were geographically diverse in both countries. The CSNR-II data presented here are consistent with the overall CSNR-II data.6 A major strength is that both projects enrolled consecutive patients and achieved a relatively high rate of data acquisition until the 90-day follow-up. Unlike the AHA-GWTG dataset, we did not capture reasons for noncompliance with quality performance measures such as patient refusal or medication contraindications, which may underestimate the quality of care. In CNSR II, 69.8% were assessed for rehabilitation, which is one of the core performance metrics in AHA-GWTG. Given the paucity of postacute rehabilitation facilities in India, the IUCSP did not collect data on assessment for rehabilitation. Differences in stroke rehabilitation may account for some of the disparity in long-term outcomes of hospitalized stroke patients and may be a target for resource use in India and China. The multivariate analysis did not include some variables that are known to be associated with outcome, e.g., stroke mechanism or infarct volume, because imaging data were not captured in CSNR-II. Lastly, requirements for informed consent may have biased the enrolled cohort to less severe strokes, and this been shown to limit generalizability in other published reports.18
Vascular risk factors, acute and inpatient management as assessed by quality performance measures, and clinical outcomes in acute ischemic stroke vary in India and China. National strategies should be tailored per regional differences to improve resource use and to ultimately reduce stroke burden in China, India, and other developing countries.
Glossary
- AHA-GWTG
American Heart Association’s Get With The Guidelines
- CI
confidence interval
- CNSR-II
China National Stroke Registry-II
- DVT
deep vein thrombosis
- IUCSP
Indo-US Collaborative Stroke Project
- mRS
modified Rankin Scale
- NIHSS
NIH Stroke Scale
- OR
odds ratio
- tPA
tissue plasminogen activator
Footnotes
Editorial page 643
Author contributions
Zixiao Li: analyzed and interpreted the data, drafted the manuscript, performed statistical analysis. Yilong Wang, Xingquan Zhao, and Liping Liu: conceived and designed the research. Chunjuan Wang: acquired the data. Yongjun Wang: conceived and designed the research. Jeyaraj Pandian, P.N. Sylaja, Dheeraj Khurana, M.V. Padma Srivastava, Subhash Kaul, and Deepti Arora: acquired the data. Lee H. Schwamm: conceived and designed the research. Aneesh B. Singhal: conceived and designed the research, analyzed and interpreted the data, and drafted the manuscript.
Study funding
This study is supported by grants from National Institute of Neurological Disorders and Stroke R21NS077442 and Department of Biotechnology India (A.B. Singhal, principal investigator: Indo-US Collaborative Stroke Registry and Infrastructure Development); MoST 2011BAI08B02, 2012ZX09303, 2013BAI09B14, 2013BAI09B03, 2015BAI12B02, 2015BAI12B04, 2017YFC1310900, and 2017YFC1310901; and the Ministry of Science and Technology (Y.J. Wang, principal investigator: CNSR-II).
Disclosure
The authors report no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
Publication history
Received by Neurology March 26, 2018. Accepted in final form June 26, 2018.
References
- 1.Feigin VL, Roth GA, Naghavi M, et al. Global burden of stroke and risk factors in 188 countries, during 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet Neurol 2016;15:913–924. [DOI] [PubMed] [Google Scholar]
- 2.Available at: statisticstimes.com/population/china-vs-india-population.php. Accessed March 20, 2018.
- 3.Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990-2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet 2016;387:251–272. [DOI] [PubMed] [Google Scholar]
- 4.Pandian JD, Sudhan P. Stroke epidemiology and stroke care services in India. J Stroke 2013;15:128–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang W, Jiang B, Sun H, et al. Prevalence, incidence and mortality of stroke in China: results from a nationwide population-based survey of 480,687 adults. Circulation 2017;135:759–771. [DOI] [PubMed] [Google Scholar]
- 6.Li Z, Wang C, Zhao X, et al. Substantial progress yet significant opportunity for improvement in stroke care in China. Stroke 2016;47:2843–2849. [DOI] [PubMed] [Google Scholar]
- 7.Khurana D, Pandian J, Sylaja PN, et al. The Indo-US Collaborative Stroke Registry and Infrastructure Development Project. Neurol India 2018;66:276–278. [DOI] [PubMed] [Google Scholar]
- 8.Sylaja PN, Pandian JD, Kaul S, et al. Ischemic stroke profile, risk factors, and outcomes in India: the Indo-US Collaborative Stroke Project. Stroke 2018;49:219–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jin H, Zhu S, Wei JW, et al. Factors associated with prehospital delays in the presentation of acute stroke in urban China. Stroke 2012;43:362–370. [DOI] [PubMed] [Google Scholar]
- 10.Minister of Health. Acts for hospital classification. Beijing: Minister of Health; 1989. [Google Scholar]
- 11.Malmivaara A, Meretoja A, Peltola M, et al. Comparing ischaemic stroke in six European countries: the EuroHOPE Register study. Eur J Neurol 2015;22:284–291, e225–286. [DOI] [PubMed] [Google Scholar]
- 12.Venketasubramanian N, Yoon BW, Pandian J, et al. Stroke epidemiology in south, east, and south-east Asia: a review. J stroke 2017;19:286–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bayona H, Owolabi M, Feng W, et al. A systematic comparison of key features of ischemic stroke prevention guidelines in low- and middle-income vs. high-income countries. J Neurol Sci 2017;375:360–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwamm LH, Fonarow GC, Reeves MJ, et al. Get With The Guidelines-Stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or transient ischemic attack. Circulation 2009;119:107–115. [DOI] [PubMed] [Google Scholar]
- 15.O'Donnell MJ, Chin SL, Rangarajan S, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet 2016;388:761–775. [DOI] [PubMed] [Google Scholar]
- 16.Wang Y, Liao X, Zhao X, et al. Using recombinant tissue plasminogen activator to treat acute ischemic stroke in China: analysis of the results from the Chinese National Stroke Registry (CNSR). Stroke 2011;42:1658–1664. [DOI] [PubMed] [Google Scholar]
- 17.Li Z, Singhal AB, Wang Y. Stroke physician training in China. Stroke 2017;48:e338–e340. [DOI] [PubMed] [Google Scholar]
- 18.Tu JV, Willison DJ, Silver FL, et al. Investigators in the Registry of the Canadian Stroke Network: impracticability of informed consent in the Registry of the Canadian Stroke Network. N Engl J Med 2004;350:1414–1421. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data used for analysis are presented in the tables. Data will be shared after ethics approval if requested by other investigators for purposes of replicating the results.