Abstract
AIMS
Magnetic resonance image-guided radiotherapy (MRIgRT) has been clinically implemented since 2014. This technology offers improved soft-tissue visualisation, daily imaging, and intra-fraction real-time imaging without added radiation exposure, and the opportunity for adaptive radiotherapy (ART) to adjust for anatomical changes. Here we share the longest single-institution experience with MRIgRT, focusing on trends and changes in use over the past 4.5 years.
MATERIALS AND METHODS
We analysed clinical information, including patient demographics, treatment dates, disease sites, dose/fractionation, and clinical trial enrolment for all patients treated at our institution using MRIgRT on a commercially available, integrated 0.35 T MRI, tricobalt-60 device from 2014 to 2018. For each patient, factors including disease site, clinical rationale for MRIgRT use, use of ART, and proportion of fractions adapted were summated and compared between individual years of use (2014–2018) to identify shifts in institutional practice patterns.
RESULTS
Six hundred and forty-two patients were treated with 666 unique treatment courses using MRIgRT at our institution between 2014 and 2018. Breast cancer was the most common disease, with use of cine MRI gating being a particularly important indication, followed by abdominal sites, where the need for cine gating and use of ART drove MRIgRT use. One hundred and ninety patients were treated using ART in 1,550 fractions, 67.6% (1,050) of which were adapted. ART was primarily used in cancers of the abdomen. Over time, breast and gastrointestinal cancers became increasingly dominant for MRIgRT use, hypofractionated treatment courses became more popular, and gastrointestinal cancers became the principal focus of ART.
DISCUSSION
MRIgRT is widely applicable within the field of radiation oncology and new clinical uses continue to emerge. At our institution to date, applications such as ART for gastrointestinal cancers and accelerated partial breast irradiation (APBI) for breast cancer have become dominant indications, although this is likely to continue to evolve.
Keywords: MRIgRT, online-adaptive radiation therapy, ART, MRI-guided radiation therapy, SMART
INTRODUCTION
Magnetic resonance image-guided radiotherapy (MRIgRT) has long been sought within the field of radiation oncology. MRIgRT offers superior daily visualisation of soft-tissue disease sites for improved set-up accuracy, daily imaging of sufficient quality for online adaptive radiotherapy (ART), and the potential for real-time target-based cine MRI (cMRI) gating for intra-fraction motion management without additional radiation exposure to patients [1–4] Over the past two decades, advances in the integration of MRI and radiotherapy devices culminated in the clinical implementation of MRIgRT at our clinic in 2014 [5].
Since its initial implementation, MRIgRT use has expanded to multiple centres and countries. In our clinic, it has quickly become an integral treatment modality, and has been the focus of several prospective clinical trials and multi-institutional studies [4,6,7]. As the field acclimatises to the availability of MRIgRT, clinical use of this technology matures and new applications continuously emerge.
Previously, we described our early institutional experience with MRIgRT [8]; however, as familiarity with the technology is gained, use is honed to derive maximal therapeutic benefit. In this work, we present the longest single-institution clinical experience using MRIgRT. The goal of this paper is to describe our 4.5 years of use, including shifts in our practice patterns over time, to guide best clinical practice as MRIgRT gains traction in the global clinic.
MATERIALS AND METHODS
Setting and Patients
The Radiation Oncology department at Washington University in St Louis includes 21 disease-site-specific attending radiation oncologists who cover our main site as well as five satellite facilities. Our main facility is equipped with eight linear accelerators (linacs) including the Edge radiosurgery system, an MRI-guided linac (completing commissioning), and the Halcyon, in addition to a Leksell Gamma Knife ICON, a cobalt-60-based MRIgRT system, a single-gantry proton therapy system, and a full brachytherapy suite. All patients included in this study were treated with MRIgRT between 2014–2018 and were either part of prospective clinical protocols (institutional protocol nos. 201410002, 201401160, 201311081, 201611018, 201510101, 201412038), a prospective MRIgRT patient registry (registry no. 2013111222), or an institutional retrospective registry (registry no. 201301149). The dataset was interrogated to obtain clinical information, including demographic information, dates of treatment, disease site treated, dose and fractionation, and clinical trial enrolment. For each patient, the primary clinical rationale for the use of MRIgRT was evaluated (adaptive treatment, cine gating, daily MRI for improved setup accuracy). For patients receiving ART, we also examined the proportion of fractions adapted. These factors were then summated and compared between individual years of use (2014–2018) to identify shifts in institutional practice patterns.
Three clinical MRIgRT systems are commercially available and have been clinically used including a 0.35 T MRI-linac, an integrated 0.35 T-tri-Co-60 device, and a 1.5 T MRI-linac system [5,9,10]. The patients included in this experience were treated using the 0.35 T-tri-Co-60 system, although our clinic is commissioning its counterpart, the 0.35 T MRI-linac device. Detailed descriptions of the 0.35 T MRIgRT system, commissioning, quality assurance, and the imaging unit have been published [5,11,12]. In summary, the MRIgRT system is comprised of a tri-cobalt-60 radiation delivery device straddled by an open split-solenoid low-field (0.35 T) magnetic resonance imaging (MRI) device with a nominal dose rate of 550 cGy/min from three 27.3× 27.3 cm2 fields to the 105 cm isocentre [5].
Simulation, Planning, and Treatment Delivery
All patients treated with MRIgRT underwent computed tomography (CT) simulation and an MR simulation; details for multiple simulation and treatment techniques have been described [4,8,13]. Patient positioning during CT simulation was determined by the treating physician and emulated the position used during MRIgRT. Following simulation, CT and MR simulation images are transferred to an independent treatment planning system (TPS) for volume delineation. These images are then transferred to the MRIgRT dedicated TPS for plan creation. The dedicated TPS uses a Monte Carlo dose calculation algorithm and is capable of creating both conformal and intensity modulated radiation therapy (IMRT) plans [14]. Details on plan delivery including cine gating and ART planning and delivery workflows have been reported previously [2–4].
Statistical Analysis
Data analyses were performed using Excel 2013 (Microsoft Corporation, Redmond, WA, USA).
RESULTS
Patient Characteristics and Disease Sites
Between January 2014 and March 2018, 642 patients with a median age of 64 years (range 64–90 years) were treated with 666 unique courses of MRIgRT. This included 240 IMRT, 266 stereotactic body radiation therapy (SBRT), and 160 three-dimensional (3D) conformal plans delivered over a total of 7,884 fractions. The median number of fractions per patient was 10 (mean 12; range 1–44) with a median dose per fraction of 450 cGy (range 115–2,000 cGy). Disease sites included the abdomen in 41.2%, breast in 31.4%, thorax in 11.6%, head and neck/central nervous system (CNS) in 2.6%, and pelvis in 13.2% of cases (Table 1, Figure 1). Of the abdominal malignancies treated, pancreatic and hepatobiliary primaries comprised the majority of patients (15.2% and 13%, respectively). Breast cancer treatment courses included accelerated partial breast irradiation (APBI; 30.5%) and whole-breast radiation (1%).
Table 1.
Disease sites treated between 2014–2018.
| Disease sites treated | N | % |
|---|---|---|
| Abdomen | ||
| Oligometastases | 59 | 8.9 |
| Pancreas/duodenum | 101 | 15.2 |
| Hepatobiliary | 87 | 13.1 |
| Gastric | 15 | 2.3 |
| Sarcoma | 7 | 1.1 |
| Other | 6 | 0.9 |
| Pelvis and lower extremity | ||
| Lower gastrointestinal | 12 | 1.8 |
| Prostate | 35 | 5.3 |
| Bladder | 22 | 3.3 |
| Oligometastases | 17 | 2.6 |
| Extremity | 2 | 0.3 |
| H&N and brain | ||
| H&N | 14 | 2.1 |
| CNS | 3 | 0.5 |
| Thorax | ||
| Lung and mediastinum | 67 | 10.1 |
| Oesophagus | 3 | 0.5 |
| Oligometastases | 3 | 0.5 |
| Bone | 4 | 0.6 |
| Breast | ||
| APBI | 203 | 30.5 |
| WBRT | 6 | 0.9 |
| Patient volume by year | ||
| 2014 | 86 | 12.9 |
| 2015 | 163 | 24.5 |
| 2016 | 166 | 24.9 |
| 2017 | 211 | 31.7 |
H&N, head and neck; APBI, accelerated partial breast irradiation; WBRT, whole-brain radiotherapy
Figure 1.
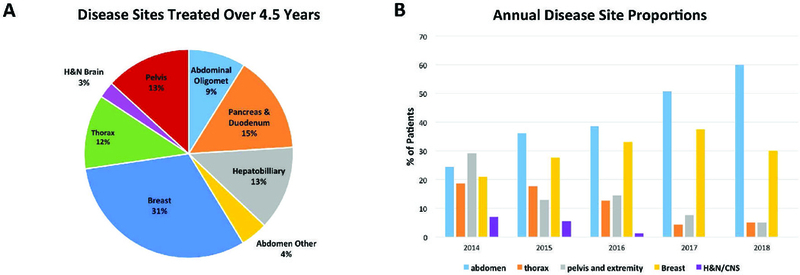
Distribution of disease sites treated over 4.5 years based on anatomical sites (a), and annual treatment trends from 2014 to 2018, with the y-axis representing the percentage of patients by year (b).
Rationale for MRIgRT
Physician rationale for use of MRIgRT was variable, but could be stratified into three principal reasons: (1) improved soft-tissue visualisation for set-up accuracy in 93 patients (14%); (2) cMRI gating for intra-fraction motion management in 383 patients (57.5%); and (3) online and offline ART in 190 patients (28.5%). Figure 2 provides a visual summary of these rationales. MRI visualisation and set-up was primarily used in the treatment of pelvic malignancies (65 patients), including prostate and bladder malignancies. Breast cancer was the most common disease treated over the total 4.5 years due to the advantage of cMRI gating, comprising the majority of treatment courses delivered (206 patients), followed by abdominal (98 patients) and thoracic (66 patients) malignancies. For APBI patients in particular, MRIgRT was selected for the advantage of planning target volume (PTV) reduction enabled by MRI localisation and cine gating upon the lumpectomy cavity [13]. Of the 190 patients who received ART, the vast majority (169/190) had abdominal malignancies (Figure 3). This included 91 pancreas and 39 hepatobiliary patients. A large proportion of patients were treated as part of prospective clinical protocols (XX%). Table 2 provides a summary of key institutional protocols completed or currently accruing at our institution, as well as the clinical rationale or study hypothesis for benefit of MRIgRT for each protocol.
Figure 2.
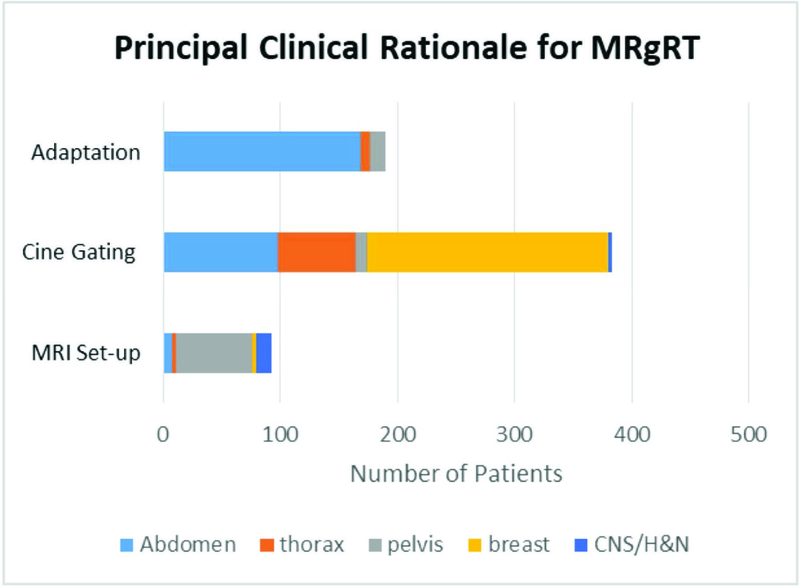
Physician rationale for the use of MRIgRT with distribution of disease sites treated.
Figure 3.

Percentage of fractions adapted for patients treated with ART.
Table 2.
Selection of key institutional clinical protocols evaluating indications for and advantages of magnetic resonance image-guided radiotherapy (MRIgRT).
| Study name | Investigational question | Hypothesised advantage of MRIgRT |
Status | Primary result |
|---|---|---|---|---|
| MRIgRT for External Beam Accelerated Partial Breast Irradiation: Evaluation of Delivered Dose and Intrafractional Cavity motion |
To determine the intrafractional motion of the breast surgical cavity and evaluate delivered versus planned dose |
MRIgRT will demonstrate minimal intra-fraction motion with good tracking such that PTV margins can be reduced |
Completed and published (Acharya and Fischer-Valuck et al., IJROBP 2016) |
Median PTV volume could be reduced by 52% and dosimetric uncertainty was less than 1% |
| Phase I Trial of Stereotactic MR-guided Online Adaptive Therapy (SMART) for the Treatment of Oligometastatic or Unresectable Malignancies of the Abdomen |
To evaluation the feasibility and safety of SMART for delivery of ablative radiation therapy to the abdomen |
Online adaptive SBRT will be feasible and increase the therapeutic index of SMART |
Completed and published (Henke et al., IJROBP 2017) |
SMART was clinically deliverable, resulted in zero grade 3 or greater CTCAE v.4 acute toxicities, and increased the dosimetric therapeutic index in a majority of cases |
| Prospective Phase I study of Nab-Paclitaxel Plus Gemcitabine with Concurrent MR-guided IMRT in Patients with Locally Advanced or borderline resectable pancreatic cancer |
Determination of the maximum tolerated dose level of hypofractionated (15 fx) with secondary end points of conversion to resectable disease and survival metrics |
MRIgRT will improve the therapeutic index of radiation, such that it can be safely delivered concurrently with full-dose systemic therapy |
Accruing at highest dose level of 67.5 Gy/15 fx + gemcitabine 1,000 mg/m2 and nab- paclitaxel100 mg/m2 |
Pending accrual completion |
| Evaluation of Single Fraction High-gradient Partial Breast Irradiation as the Sole Method of Radiation Therapy for Low To risk Stage 0 and I Breast Carcinoma |
To quantify the tolerance by estimating rates of acute and late CTCAE v4 grade 3+ toxicities and estimate the ipsilateral breast recurrence rate 5 years post-treatment |
Single fraction APBI will result in dosimetrically acceptable plans to deliver single fraction treatment for minimal impact of therapy on quality of life, low toxicity, and good cosmetic outcomes |
Accrual completed. | Preliminary toxicity results reported at ASTRO 2017 (Zoberi et al.), with zero CTCAE v. 4 Grade 2+ acute toxicities observed; preliminary cosmetic results to be presented at ASTRO 2018 |
| Prospective phase II study of Stereotactic (daily) Adapted MR-guided Radiation Therapy (SMART) for Patients with Borderline or Inoperable Locally Advanced Pancreatic Cancer |
To determine the 90-day rates of CTCAE v.4 Grade 3 or higher gastrointestinal toxicity and to evaluate long- term survival metrics |
MRIgRT will permit escalated dose and result in reduced acute GI toxicity compared to historical controls. MRIgRT will result in improved survival outcomes compared to historical controls |
Not yet open to accrual |
Pending accrual completion |
PTV, planning target volume; IMRT, intensity modulated radiotherapy; IROBP, International Journal of Radiation Oncology, Biology, and Physics; ASTRO, American Society for Radiation Oncology; APBI, accelerated partial breast irradiation; fx, fraction; CTCAE v4, Common Terminology Criteria for Adverse Events version 4.
Treatment Trends
Between 2014 and 2018, the proportion of abdominal patients increased steadily from 24.4% to 60%. An increase in the proportion of breast malignancies treated was also observed over this time frame (21% in 2014 versus 30% in 2018). Concomitantly, we observed a decrease in the annual proportion of treated patients who had thoracic or pelvic malignancies. Figure 1b illustrates the proportion of treatments that each disease site contributed, per year. We also noted that the average number of fractions used per treatment course decreased steadily over time, from 17.2 fractions in 2014 to 7.2 fractions per course in 2018 (average 14 in 2015, 11.7 in 2016, and 9.4 in 2017).
With regards to adaptation, 190/666 total treatment courses were delivered using ART. Of 1,550 fractions delivered to these 190 patients, 67.7% (1,050) of fractions were adapted. Use of ART increased by year, with nine patients undergoing adaptation in 2014, 41 in 2015, 50 in 2016, and 75 in 2017. Abdominal malignancies comprised the largest proportion of ART, and this proportion increased over time (23.3% in 2014 versus 74.8% in 2018; Figure 3). Notably, in patients receiving ART, the average proportion of treatment fractions that were adapted also increased over time, from 0.34 in 2014 to 0.79 in 2018 (0.64 in 2015, 0.72 in 2016, 0.77 in 2017), indicating improved physician selection of cases likely to require daily adaptation (Figure 3).
Of note, our institution has recently installed a 0.35 T MRI-linac. Although we have not initiated patient treatments on this device at the time of submission of this work, commissioning is nearing completion, and we have begun evaluation of plan qualities between our two MRIgRT devices. In several sites, we have observed increased sharpness of dose gradients as anticipated with a linac compared to a tri-cobalt-60 source (unpublished work), which may increase future use of MRIgRT in disease sites that demand especially steep dose fall-off.
Treatment Outcomes
Although prospective outcomes of treatment using MRIgRT have been and will continue to be reported separately by our institution for the prospective studies conducted (see Table 2), our reported outcomes using this technology have been positive thus far. In the abdomen, we found in a prospective Phase I trial that SMART permits achievement of ablative dose levels (BED = 100 or greater) with zero observed acute or late Grade 3 or higher gastrointestinal (GI) toxicities and no detriment to quality of life [4]. Multi-institutional retrospective data (manuscript in press) for use of MRIgART in locally advanced pancreatic cancer indicates that use of this technique to achieve similarly escalated BED correlates with improved overall survival [7]. For APBI, use of MRIgRT has allowed achievement of reduced PTV margins due to improved visualisation of the lumpectomy cavity and monitoring of intra-fraction motion [13]. A Phase I trial of single-fraction high-gradient partial breast irradiation has been completed on the basis of this observation, and zero Grade 2 or higher acute toxicities were observed in the preliminary report of outcomes [15]. Early results also indicate zero failures in the treated quadrant and that this technique achieves excellent-to-good cosmetic outcomes (data to be presented at ASTRO 2018), although these long-term outcome results are not fully mature at this time. In summary, MRIgRT has resulted in reduction in toxicity and potential improvements in outcomes in our clinic, consistent with the apparent improvement in the therapeutic index achieved with this technology.
DISCUSSION
Here we present the longest implementation of MRIgRT in the radiation oncology clinic. Our dataset comprises over 650 treatment courses for 642 patients across 4.5 years of use. Specifically, we report changes in patterns of our use of this technology over the past 4.5 years to highlight its key applications and share our experience with an expanding field.
First, we observed that the relative use of MRIgRT across disease sites shifted prominently over the past 4.5 years in our clinic. Initially, our department chose to emphasise smooth integration of the device into our clinic, with broad use across numerous disease sites. Initial use often mimicked standard linear accelerator treatment planning, including use of the device for typical, conventionally fractionated, non-adaptive plans, in order to uncover potential device advantages. Over the last 4.5 years, MRIgRT use for treatment of breast and GI cancers expanded dramatically. For breast, novel applications such as APBI with MR set-up for improved visualisation and cine MR gating on the lumpectomy cavity allowed for reduction of treatment margins from the standard 2–2.5 cm GTV to PTV expansion using conventional EBRT to a total 1 cm expansion with MRIgRT, which matches our brachytherapy APBI margin [13,15]. For GI cancers, the ability to perform online and offline adaptation based on changes in daily tumour and OAR anatomy, as well as cMRI gating to mitigate the effects of respiratory motion, resulted in substantial increase in use. cMRI gating has particularly affected the workflow for liver SBRT at our institution and others, as SBRT can now be performed without fiducial placement, using gadoxetic acid (Eovist, Bayer HealthCare Pharmaceuticals, USA) contrast medium as needed, and with gating on the tumour volume itself [16].
With regards to adaptive radiotherapy, our use has also shifted over the past 4.5 years. In 2018, as compared with 2014, we adapt more for GI tumours than for any other disease site. As our adaptive use shifted toward a larger proportion of GI cancers, the proportion of fractions adapted per treatment course also shifted closer to 100%, indicating that GI disease sites are the highest yield application for daily adaptation based on inter-fraction changes in tumour and organ-at-risk geometry. In fact, the first ever, prospective clinical trial of stereotactic, MRI-guided adaptive radiotherapy (SMART) focused on GI malignancies [4]. In the midst of our 4.5 year use, we also adopted an institutional guideline that abdominal cases to be considered for adaptation should comprise tumours located within 2 cm of the viscous GI tract, to maximally select patients likely to benefit. Pelvic disease sites, although they were not treated as frequently at our institution in the last 4.5 years, could similarly benefit from adaptation, and are the subject of two prospective trials (one for SMART to ovarian oligometastases and one for prostate SMART) that have recently completed accrual at our site and others [6,17]. In general, online ART addresses a major shortcoming of prior treatment modalities: the ability to ablate lesions safely in the setting of rapidly shifting and unpredictable daily anatomy. As anticipated, adaptation increases the therapeutic index of ART in such settings [4,18], permitting dose escalation that correlates with improved progression-free and overall survival for disease such as locally advanced pancreatic cancer (LAPC) that have historically not clearly benefited from RT [7]. Indeed, the first multi-institutional clinical trial using MRIgRT will focus on LAPC and ask this question prospectively [19]. We also noted an increase in use of hypofractionated treatment courses over the time-frame examined, which may make best use of applications such as ART that are more time-intensive.
Although use of MRIgRT in some sites became less prominent over the past 4.5 years at our institution, such trends may not necessarily imply lack of benefit, but rather need for further technology advancement and more nuanced use. Although analyses have demonstrated that IMRT plans created for the tri-cobalt-60 source are acceptable [14], lung plans for small target volumes such as for SBRT are less conformal using a cobalt-60 device compared to a linac [20]; however, our early institutional analysis indicates that plan quality with the MRI-linac is (as expected) equivalent to CT-based linac plans. Thus, we anticipate that clinical availability of MRI-linac devices will open further use for ART to sites such as the central thorax, where sharp dose gradients are most critical, based on both tumour response and OAR motion [21,22]. Prostate SBRT, which has been implemented with MRIgRT at other institutions with success, will also benefit from sharper dose gradients and is also likely to expand as an indication for MRIgRT [6].
It is critical to note that our experience is not exhaustive; we acknowledge that other centres have developed additional specialised applications and that new treatment and research possibilities continuously emerge. In particular, sarcomas, gastric cancers, and CNS malignancies are of developing interest, as is use of MRIgRT for unique applications in radiomics [23–26]. Applications for MRIgRT for rectal cancers and head and neck cancers have been explored and are also underway at our institution [27,28]. The unique emergence of SBRT for successful ablation of ventricular tachycardia at our institution also presents an fascinating potential non-malignant MRIgRT application, given the need to precisely account for the motion of the heart from both the cardiac and respiratory cycles [29].
We acknowledge several study limitations. First, all treatments reported were performed using a 0.35 T imaging device, which may impact image quality; however, images are known to be sufficient for ART and are an improvement upon prior cone-beam CT technologies. Although the commercially available 1.5 T system may ultimately produce improved-quality images, it has yet to be widely used clinically. At present, the available 1.5 T device also does not permit cMRI gating, limiting some MRIgRT applications until this technological obstacle is solved. Of note, current 0.35 T devices limit cMRI gating to a single sagittal plane, restricting some intrafraction motion monitoring, but this is sufficient for key applications such as the respiratory cycle. Although new images sequences for the 0.35 T devices, including T1-weighted and T2-weighted pulse and diffusion-weighted imaging (DWI) are under development by the manufacturer, sequence development beyond the standard balanced steady state free precession (bSSFP) sequence was previously institution dependent. This may have slowed implementation and collaborative research in disease sites that are not best imaged with the primary sequence, leading to their under-representation here. Additionally, while we highlight our emerging patterns of best use, prominence of disease types may vary by country and degree of device use in particular disease sites may also be impacted by physician preference. It is plausible that our GI and breast radiation oncologists have pursued use of the device more than other disease sites, resulting in disproportionate use that may be less generalisable to other institutions. Finally, accurate point-dose accumulation, autocontouring, and workflow improvements are areas of active research that may benefit applications such as SMART and reduce demands of cost and time [30,31].
In summary, MRIgRT has a broad range of applications within the field of radiation oncology and new clinical indications continue to emerge. At our institution to date, applications such as ART for GI cancers and APBI for breast cancer have become dominant indications that may best showcase the benefits of available MRIgRT technologies; however, as technology advances and clinical use matures, these trends are likely to continue to evolve.
Highlights.
Here we report single-institution clinical use patterns of magnetic resonance image-guided radiotherapy (MRIgRT), which has been implemented at our institution since 2014.
In 4.5 years, 642 patients were treated with 666 unique treatment courses, including 1550 fractions of adaptive radiotherapy (ART).
Physician rationale for MRIgRT could be stratified into three principle reasons: 1. Improved visualization for setup 2. Cine MR gating 3. Online and offline ART
Over time, breast and gastrointestinal cancers became the dominant indications for MRIgRT and treatment regimens became increasingly hypofractionated (≤12 fractions)
Over 4.5 years of use, gastrointestinal cancers became the principle indication for online ART
The changes in patterns of use observed here may help guide best clinical use for other institutions beginning implementation of MRIgRT
ACKNOWLEDGEMENTS
This publication was supported by the Washington University Institute of Clinical and Translational Sciences grant UL1T2000448 from the National Center for Advancing Translational Sciences (NCATS). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- [1].Noel CE, Parikh PJ, Spencer CR, Green OL, Hu Y, Mutic S, et al. Comparison of onboard low-field magnetic resonance imaging versus onboard computed tomography for anatomy visualization in radiotherapy. Acta Oncol 2015:1–9. doi: 10.3109/0284186X.2015.1062541. [DOI] [PubMed] [Google Scholar]
- [2].Acharya S, Fischer-Valuck BW, Kashani R, Parikh P, Yang D, Zhao T, et al. Online magnetic resonance image guided adaptive radiation therapy: first clinical applications. Int J Radiat Oncol Biol Phys 2016;94:394–403. doi: 10.1016/j.ijrobp.2015.10.015. [DOI] [PubMed] [Google Scholar]
- [3].Green OL, Rankine L, Cai B, Curcuru A, Kashani R, et al. First clinical implementation of real-time, real-anatomy tracking and radiation beam control. Med Phys 2018; In press. [DOI] [PubMed]
- [4].Henke L, Kashani R, Robinson CG, Curcuru A, DeWees T, Bradley JD, et al. Phase I trial of stereotactic MR-guided online adaptive radiation therapy (SMART) for the treatment of oligometastatic or unresectable primary malignancies of the abdomen. Radiother Oncol 2017. doi: 10.1016/j.radonc.2017.11.032. [DOI] [PubMed] [Google Scholar]
- [5].Mutic S, Dempsey JF. The ViewRay system: magnetic resonance-guided and controlled radiotherapy. Semin Radiat Oncol 2014;24:196–9. doi: 10.1016/j.semradonc.2014.02.008. [DOI] [PubMed] [Google Scholar]
- [6].Lagerwaard F, Bruynzeel A, Tetar S, Oei SS, Haasbeek C, Slotman BJ, et al. Stereotactic MR-guided adaptive radiation therapy (SMART) for prostate cancer. Int J Radiat Oncol Biol Phys 2017;99:E681–2. doi: 10.1016/j.ijrobp.2017.06.2246. [DOI] [Google Scholar]
- [7].Rudra S, Jiang N, Rosenberg SA, Olsen JR, Parikh PJ, Bassetti MF, et al. High dose adaptive MRI guided radiation therapy improves overall survival of inoperable pancreatic cancer. Int J Radiat Oncol Biol Phys 2017;99:E184. doi: 10.1016/j.ijrobp.2017.06.1042. [DOI] [Google Scholar]
- [8].Fischer-Valuck BW, Henke L, Green O, Kashani R, Acharya S, Bradley JD, et al. Two-and-a-half-year clinical experience with the world’s first magnetic resonance image guided radiation therapy system. Adv Radiat Oncol 2017;2:485–93. doi: 10.1016/j.adro.2017.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Mutic S, Low D, Chmielewski T, Fought G, Gerganov G, Hernandez M, et al. The design and implementation of a novel compact linear accelerator-based magnetic resonance imaging-guided radiation therapy (MR-IGRT) system. Int J Radiat Oncol Biol Phys 2016;96:E641. doi: 10.1016/j.ijrobp.2016.06.2234. [DOI] [Google Scholar]
- [10].Raaymakers BW, Jürgenliemk-Schulz IM, Bol GH, Glitzner M, Kotte ANTJ, van Asselen B, et al. First patients treated with a 1.5 T MRI-Linac: clinical proof of concept of a high-precision, high-field MRI guided radiotherapy treatment. Phys Med Biol 2017;62:L41–L50. doi: 10.1088/1361-6560/aa9517. [DOI] [PubMed] [Google Scholar]
- [11].Hu Y, Rankine L, Green OL, Kashani R, Li HH, Li H, et al. Characterization of the onboard imaging unit for the first clinical magnetic resonance image guided radiation therapy system. Med Phys 2015;42:5828–37. doi: 10.1118/1.4930249. [DOI] [PubMed] [Google Scholar]
- [12].Yang D, Wooten HO, Green O, Li HH, Liu S, Li X, et al. A software tool to automatically assure and report daily treatment deliveries by a cobalt-60 radiation therapy device. J Appl Clin Med Phys 2016;17:492–501. doi: 10.1120/jacmp.v17i3.6001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Acharya S, Fischer-Valuck BW, Mazur TR, Curcuru A, Sona K, Kashani R, et al. Magnetic resonance image guided radiation therapy for external beam accelerated partial-breast irradiation: evaluation of delivered dose and intrafractional cavity motion. Int J Radiat Oncol Biol Phys 2016;96:785–92. doi: 10.1016/j.ijrobp.2016.08.006. [DOI] [PubMed] [Google Scholar]
- [14].Wooten HO, Green O, Yang M, DeWees T, Kashani R, Olsen J, et al. Quality of intensity modulated radiation therapy treatment plans using a Co magnetic resonance image guidance radiation therapy system. Int J Radiat Oncol Biol Phys 2015;92:771–8. doi: 10.1016/j.ijrobp.2015.02.057. [DOI] [PubMed] [Google Scholar]
- [15].Zoberi I, Thomas MA, Ochoa LL. Evaluation of single fraction high-gradient partial breast irradiation as the sole method of radiation therapy for low-risk Stage 0 and I breast cancer: early results of a single institution prospective clinical trial. Int J Radiat Oncol Biol Phys 2017;99:E61. [Google Scholar]
- [16].Hepel JT, Tokita M, MacAusland SG, Evans SB, Hiatt JR, Price LL, et al. Toxicity of three-dimensional conformal radiotherapy for accelerated partial breast irradiation. Int J Radiat Oncol Biol Phys 2009;75:1290–6. doi: 10.1016/j.ijrobp.2009.01.009. [DOI] [PubMed] [Google Scholar]
- [17].Wojcieszynski AP, Rosenberg SA, Brower JV, Hullett CR, Geurts MW, Labby ZE, et al. Gadoxetate for direct tumour therapy and tracking with real-time MRI-guided stereotactic body radiation therapy of the liver. Radiother Oncol 2016;118:416–8. doi: 10.1016/j.radonc.2015.10.024. [DOI] [PubMed] [Google Scholar]
- [18].Robinson CG. MRI-guided stereotactic body radiation therapy (SBRT) for ovarian cancer Available at: https://clinicaltrials.gov/ct2/show/NCT02582931 (accessed ?????). [Google Scholar]
- [19].Henke L, Kashani R, Yang D, PhD TZ, PhD OG, PhD LO, et al. Simulated online adaptive magnetic resonance-guided stereotactic body radiation therapy for the treatment of oligometastatic disease of the abdomen and central thorax: characterization of potential advantages. Int J Radiat Oncol Biol Phys 2016;96:1078–86. doi: 10.1016/j.ijrobp.2016.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].ViewRay, Inc. NewsRoom. ViewRay launches clinical trial following compelling early pancreatic cancer data with MRIdian System. Available at: http://investors.viewray.com/news-releases/news-release-details/viewray-launchesclinical-trial-following-compelling-early2018 (accessed: ?????) [Google Scholar]
- [21].Park JM, Park SY, Kim HJ, Wu H-G, Carlson J, Kim J-I. A comparative planning study for lung SABR between tri-Co-60 magnetic resonance image guided radiation therapy system and volumetric modulated arc therapy. Radiother Oncol 2016;120:279–85. doi: 10.1016/j.radonc.2016.06.013. [DOI] [PubMed] [Google Scholar]
- [22].Henke L, Kashani R, Hilliard J, DeWees TD, Curcuru A, et al. In silico trial of MR-guided mid-treatment adaptive planning for hypofractionated stereotactic radiotherapy in centrally located thoracic tumors. Int J Radiat Oncol Biol Phys, 2018. in press. [DOI] [PubMed]
- [23].Henke L, Olsen JR, Contreras J, Curcuru A, DeWees TD, et al. Stereotactic MR-guided online adaptive radiation therapy (SMART) for ultra-central thorax malignancies: results of a Phase I trial. Adv Radiat Oncol, 2018. submitted. [DOI] [PMC free article] [PubMed]
- [24].Kishan AU, Cao M, Mikaeilian AG, Low DA, Kupelian PA, Steinberg ML, et al. Dosimetric feasibility of magnetic resonance imaging-guided tri-cobalt 60 preoperative intensity modulated radiation therapy for soft tissue sarcomas of the extremity. Pract Radiat Oncol 2015;5:350–6. doi: 10.1016/j.prro.2015.01.007. [DOI] [PubMed] [Google Scholar]
- [25].Mehta S, Gajjar SR, Padgett KR, Asher D, Stoyanova R, Ford JC, et al. Daily tracking of glioblastoma resection cavity, cerebral edema, and tumor volume with MRI-guided radiation therapy. Cureus 2018;10:1–9. doi: 10.7759/cureus.2346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Chun S-J, Jeon SH, Chie EK. A case report of salvage radiotherapy for a patient with recurrent gastric cancer and multiple comorbidities using real-time MRI-guided adaptive treatment system. Cureus 2018;10:1–10. doi: 10.7759/cureus.2471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Padgett K, Mihaylov I. Radiomics feature variability on 0.35T MR guided-RT system. Med Phys 2018:1.29091280
- [28].Shaverdian N, Yang Y, Hu P, Hart S, Sheng K, Lamb J, et al. Feasibility evaluation of diffusion-weighted imaging using an integrated MRI-radiotherapy system for response assessment to neoadjuvant therapy in rectal cancer. Br J Radiol 2017;90:20160739. doi: 10.1259/bjr.20160739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Chen AM, Cao M, Hsu S, Lamb J, Mikaeilian A, Yang Y, et al. Magnetic resonance imaging guided reirradiation of recurrent and second primary head and neck cancer. Adv Radiat Oncol 2017;2:167–75. doi: 10.1016/j.adro.2017.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Cuculich PS, Schill MR, Kashani R, Mutic S, Lang A, Cooper D, et al. Noninvasive cardiac radiation for ablation of ventricular tachycardia. N Engl J Med 2017;377:2325–36. doi: 10.1056/NEJMoa1613773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Bohoudi O, Bruynzeel AME, Senan S, Cuijpers JP, Slotman BJ, Lagerwaard FJ, et al. Fast and robust online adaptive planning in stereotactic MR-guided adaptive radiation therapy (SMART) for pancreatic cancer. Radiother Oncol 2017;125:439–44. doi: 10.1016/j.radonc.2017.07.028. [DOI] [PubMed] [Google Scholar]
- [32].Wardman K, Prestwich RJD, Gooding MJ, Speight RJ. The feasibility of atlas-based automatic segmentation of MRI for H&N radiotherapy planning. J Appl Clin Med Phys 2016;17:146–54. doi: 10.1120/jacmp.v17i4.6051. [DOI] [PMC free article] [PubMed] [Google Scholar]


