Abstract
The purpose of the present study was to examine the relationships of multiple factors to menopausal symptoms in different racial/ethnic groups of midlife women. This secondary analysis was conducted with the data from 980 midlife women that were collected from 2005 to 2013 using the Midlife Women’s Symptom Index. Structural equation modeling was used to analyze the data. The model had the highest fit indices for Non-Hispanic (NH) White midlife women, and prominent racial/ethnic differences were observed in the relationships of multiple factors to menopausal symptoms. In all racial/ethnic groups (except in Hispanic women), perceived health status was significantly associated positively with menopausal symptoms (β=−0.149 for NH African American; β=−0.207 for NH Asians; β=−0.162 for NH Whites). Body mass index was significantly positively associated with menopausal symptoms only in NH Asians (β=0.118) and Hispanics (β=0.210). The racial/ethnic differences in the relationships of multiple factors to menopausal symptoms could have resulted from the different cultural contexts in which women undergo during their menopausal transitions. Further cultural studies on the associations of racial/ethnic-specific factors with menopausal symptoms would help in understanding possible causes for racial/ethnic differences in the factors significantly associated with menopausal symptoms.
Keywords: race/ethnicity, menopausal symptoms, covariates, midlife women, structural equation modeling
INTRODUCTION
Menopause is a life transition that brings about drastic biological, psychological, and cultural changes in midlife women’s lives (Jones, Jurgenson, Katzenellenbogen, and Thompson 2012; Mitchell, Woods, and Mariella 2000). Midlife women frequently experience a variety of symptoms during their menopausal transitions mainly due to hormonal changes (Freeman, 2015). Women experience various types of symptoms, including vasomotor symptoms, sleep difficulties, musculoskeletal symptoms, and cognitive symptoms (Gold et al. 2007). These symptoms are associated with many background and contextual factors, lifestyle factors, and factors related to health and menopausal status (Gold et al. 2017; Pimenta, Leal, Maroco, and Ramos 2012b). However, little has been reported on whether these multiple factors are related differently to menopausal symptoms in different racial/ethnic groups of midlife women.
The knowledge of menopausal symptoms and their related factors are still mostly derived from studies conducted among non-Hispanic (NH) White women (Andrist and MacPherson 2001). However, with continuous challenge to the universality of menopausal symptoms, racial/ethnic differences in menopausal symptoms and their related factors have been increasingly reported (Gold et al 2006; Haines, Xing, Park, Holinka, and Ausmanas 2005; Im and Chee 2005; Im, Lee, Chee, Brown, and Dormire 2010; Im, Lee, Chee, Dormire, and Brown 2010; Kagawa-Singer et al. 2002; Kardia, Chu, and Sowers 2006; Kravitz and Joffe 2011; Llaneza, García-Portilla, Llaneza-Suárez, Armott, and Pérez-López 2012; Thurston et al. 2008). For instance, one of the first multi-racial/ethnic studies in the U.S. on the menopausal transition and related symptoms, the Study of Women’s Health Across the Nation (SWAN) (Avis et al. 2001; Gold et al. 2000; Gold et al 2006; Kardia et al. 2006; Kravitz and Joffe 2011; Thurston et al. 2008; Thurston et al. 2008) revealed significant racial/ethnic differences in menopausal symptoms, quality of life, and the prevalence rate of premature menopause. These publications suggested that the cause of racial/ethnic differences is multifactorial, resulting from differences in complex biological, social, economic, and cultural situations among the groups (Thurston et al. 2008). Thus, it is suspected that the associations of multiple factors to menopausal symptoms could be different in different racial/ethnic groups.
Structural equation modeling (SEM) is a statistical technique that is usually used to examine and approximate causal associations using an integration of statistical data and qualitative causal propositions (Bagozzi and Yi 2012). SEM is frequently used to decide if a specific model is valid, subsequently clarifying the relationships among the variables (Bagozzi and Yi 2012). Through SEM, the relationships among various variables can be identified, which could help in constructing the most approximate model to explain these relationships (Bagozzi and Yi 2012). In addition, because SEM uses latent variables (i.e., hypothetical constructs derived from several measurable variables), researchers can control those variables’ measurement errors (Bagozzi and Yi 2012). Hence, SEM is more reliable than multiple logistic regression models in identifying the relationships among multiple variables (Bagozzi and Yi 2012).
Until recently, however, SEM has rarely been used to identify the relationships among multiple variables related to menopausal symptoms, especially in different racial/ethnic groups. When the PUBMED database was searched using two key words, “structural equation model” and “menopausal symptoms,” only 10 articles were retrieved. Among them, eight articles were published during the last 10 years, and four articles were written by the same author (Pimenta, Leal, Maroco, and Ramos 2011, 2012a; Pimenta et al. 2012b; Pimenta, Maroco, Ramos, and Leal 2014). Also, among them, only six articles actually included the findings of associations of various variables to menopausal symptoms. For example, Seib et al.(2013) examined the relationships of background characteristics, lifestyle characteristics, and perceived physical health to perceived mental health in post-menopausal women using SEM. Using SEM, Pimenta et al. explored the associations of spirituality, life events, background factors, health- and menopause-related factors, and lifestyle factors to menopausal symptoms in general, specifically hot flashes and sweats (Pimenta et al., 2011, 2012a, 2012b, 2014). In addition, using SEM, Elavsky and Gold (2009) determined if depression and fatigue mediated the associations among physical activity, body mass index (BMI), hot flashes, and perceived stress level. However, they did not determine the relationships among multiple variables associated with menopausal symptoms in different racial/ethnic groups.
The purpose of the present study, therefore, was to examine the relationships of multiple factors to menopausal symptoms in different racial/ethnic groups of midlife women. In this study, we relied on women’s self-reports of the symptoms that they experienced during the menopausal transition. This secondary analysis was conducted using data from two larger national Internet surveys on midlife women’s health issues conducted in four racial/ethnic groups of U.S. midlife women from 2005 to 2013 (Non-Hispanic [NH] Whites, NH African Americans, NH Asians, and Hispanics) (Authors 2010; Authors 2012).
Theoretical framework
As the theoretical basis of the study, the Asian immigrant women’s menopausal symptom experience in the U.S. (AIMS) theory was adopted (Figure 1) (Im 2010). The AIMS theory was developed based on a systematic integrated literature review of menopausal symptoms and a large survey study among Asian American midlife women. The AIMS theory was specifically chosen for this analysis because it comprehensively included multiple possible concepts related to menopausal symptoms that had been previously reported in the literature through a systematic integrated literature review (Im 2010). Subsequently, the AIMS could provide a basis for race/ethnic-specific modeling in each racial/ethnic group. Among the major concepts of the AIMS theory, this study focused on “transition conditions” and “patterns of response” (Im 2010). Transition conditions include “facilitators” for or “barriers” to eventually attaining a successful transition without any health concerns. The AIMS theory suggests “genetic, demographic, lifestyle, and health and menopausal factors” as four sub-concepts of the transition conditions.
Figure 1.
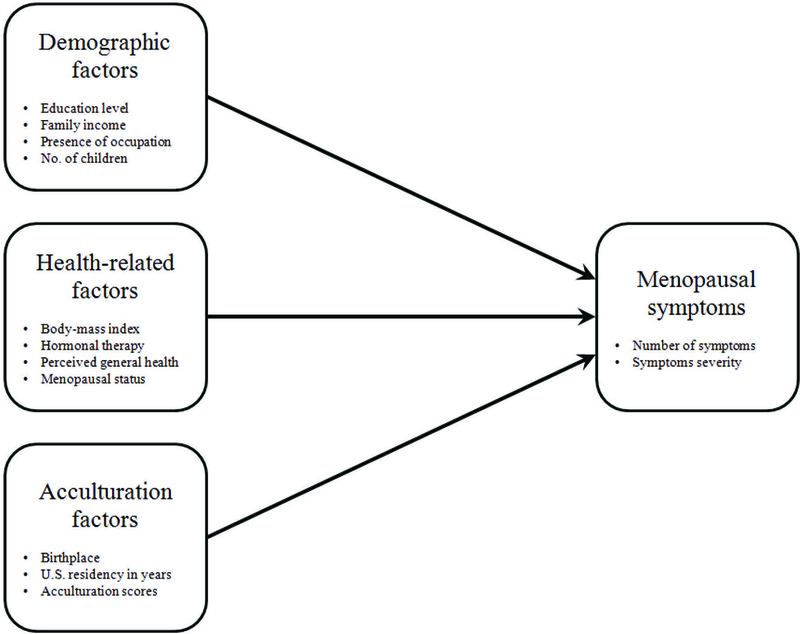
The theoretical framework based on the AIMS theory (Im, 2010)
In this analysis, “genetic and lifestyle factors” were excluded because they were not included in the data. However, two sub-concepts of “demographic and health and menopausal factors” were included. In this study, “acculturation factors,” one of the demographic factors, was conceptualized as an associated factor in Asian participants, Hispanic participants, and all participants because only Asian participants, Hispanic participants, and all participants included immigrants. The concept of “patterns of response”—another major concept of the AIMS theory—includes menopausal symptoms characteristics, such as “type and the number of symptoms, symptoms severity, and unique cultural responses” (Im 2010). For this analysis, only “the number of symptoms” and “symptoms severity” were adopted because the data did not include any variables related to “unique cultural response.”
METHODS
This secondary analysis used the data from two national Internet surveys on midlife women’s health issues (Authors 2010; Authors 2012). Institutional review board approval of the study protocol was acquired from the institutions with which the researchers were affiliated.
Participants
This secondary analysis included only the data from 980 women (294 NH White, 222 NH African American, 223 NH Asian, and 241 Hispanic women) who completely answered the questions on menopausal symptoms. The participants of the parent studies were recruited through Internet communities/groups for midlife women on a volunteer basis. The original studies included a total of 1,245 women, and the response rate (the number of participants as a proportion of the number of visitors at the project website) was 95~96%. The women were 40 to 60 years old, were able to read and write English, and reported themselves as NH White, NH African American, NH Asian, or Hispanic. About 95% of the potential participants who visited the project website met the inclusion criteria. The sample size was pre-decided due to the nature of the secondary analysis.
According to Kline (2011), at least 200 participants or five to ten participants per variable are required for a structural equation modeling analysis. Thus, for this study, 200 or 55 to 110 women (11 variables) would be needed to conduct a structural equation modeling analysis. Thus, 980 was an adequate sample size for the SEM that was conducted in this study.
Instruments
The original studies used multiple instruments. Only the data measured using the following instruments were included in the present analyses.
Demographic factors.
Demographic factors included age, the level of education, marital status, employment, perceived family income, and the number of children.
Acculturation factors.
The participants were first asked if they were born in the U.S. and how many years they had resided in the United States. The level of acculturation was quantified using the modified Suinn-Lew Asian Self-Identity Acculturation scale (Im et al. 2008; Im et al. 2005; Suinn et al. 1987; Suinn, Ahuna, and Khoo 1992). The modified scale consisted of five 5-point Likert scale questions about foods, music, customs, languages, and friends. A higher mean score means more acculturated to the main culture of the United States. Cronbach’s alpha coefficient of this modified scale was 0.84 in a previous study (Im et al. 2008) and 0.97 in this study. For those who were born in the U.S., the length of stay in the U.S. (in years) and the level of acculturation scores were replaced with their age and 5-points (which means complete acculturation to the culture of the United States), respectively.
Health and menopausal status.
Self-reported height and weight (used to generate body-mass index in kg/m2) and perceived general health (on a 5-point Likert scale) were asked to assess the women’s health status. Self-reported menopausal status was measured with seven questions on the length of time from the first day of the last menstrual period, regularity of menstrual periods, and flow of menstruation. In addition, the women were requested to answer whether they used hormone therapy to relieve menopausal symptoms. Information from these questions were used to classify participants into one of four menopausal stages based on the criteria by the SWAN (Avis et al. 2001). The pre-menopausal stage was defined as having menstrual periods in the past 3 months with no change in regularity. Having periods in the past 3 months but experiencing some irregularity in cycle during the past year constituted the early peri-menopausal stage. No periods of menstruation in the past three months but having a period in the past 12 months constituted the late peri-menopausal stage, and no menstrual period for more than 12 months (not related to medication, pregnancy, or severe weight loss) constituted the post-menopausal stage. Those who had a hysterectomy and/or a bilateral oophorectomy were excluded in the original studies; so, they were not included in these analyses as well. All peri- and premenopausal women who used steroid hormones in the past three months were also excluded in the original studies and thus also in these analyses, because their menstrual status could be obscured by the hormone therapy.
Menopausal symptoms.
The Midlife Women’s Symptoms Index (MSI) (Im 2006) was used to assess menopausal symptoms. The MSI is composed of 73 items about physical, psychological, and psychosomatic symptoms related to the menopausal transition. For each of 73 items of the MSI, the women were asked to respond to two questions about the presence of menopausal symptoms (no = 0, yes = 1, the total number of symptoms ranging from zero to 73) and symptom severity (the severity sub-scale on a 5-point Likert scale [“not at all”= 0 to “extremely”= 4], the total severity scores ranging from zero to 292). Higher scores meant higher numbers of menopausal symptoms and greater severity of menopausal symptoms. The psychometric properties, such as reliability and validity for multi-racial/ethnic groups of midlife women, have been obtained in previous studies (Im 2006; Lee, Im, and Chee 2010; Kang et al. 2015). Kuder Richardson-20 of the MSI in this analysis was 0.94 for the prevalence sub-scale. Cronbach’s alpha of the MSI in this analysis was 0.96 for the severity sub-scale.
Data collection
The data collection in the two original studies was conducted through the Internet. The study websites that were constructed with the affiliated institutes’ standard security and safety measures provided the checklist for inclusion criteria, informed consent, and questionnaires to the participants. Midlife women who were recruited from online communities visited and browsed the study websites, and then responded to the Internet surveys following consent to participate and passing the screening questions against the inclusion criteria. Only electronic consent was obtained through the Internet; the participants were asked to review an electronic informed consent sheet on the project website, and asked to click “I agree to participate” to give their consent to participate. More detailed procedures on data collection could be found elsewhere (Authors 2010; Authors 2012).
Data analysis
The analyses of the data were conducted using the SPSS and AMOS programs. First, descriptive statistics for all variables were calculated to identify quantitative features of the data. Next, to construct structural equation models in each racial/ethnic group and in total participants, the normality of all variables was assessed. Pearson’s correlation analyses were conducted to check multicollinearity among the variables. Then, based on the estimation and analysis of the model, which were performed using a maximum likelihood method, standardized regression weights and coefficients of multiple determination (squared multiple correlation, R2) were obtained. At that time, acculturation factors were entered in the models for NH Asian, Hispanic, and all participants.
The SEM requires following the model that is chosen for the analysis rather than separating specific variables from the model (Bae, 2009). Also, even when some variables do not have significant paths in the SEM analyses, the variables are still retained in the model (Bae, 2009; Wan, 2002). Accordingly, the variables for this study were chosen from the AIMS theory and were entered into each SEM simultaneously. Subsequently, socioeconomic status was included as one of the demographic characteristics in the SEM process, rather than separating it from the demographic characteristics. Also, all variables were retained regardless of their statistical significance in relation to the dependent variable. Additionally, the SEM analyses were conducted separately for three different types of symptoms: physical, psychological, and psychosomatic. However, this did not reveal any new or additional information in the models, and the fit indices of the all models became too low, indicating these separate models did not fit the data well. The overall fit of the models was evaluated using a set of fit indices that included the goodness of fit index (GFI), adjusted goodness of fit index (AGFI), normed fit index (NFI), comparative fit index (CFI), and the root mean square error of approximation (RMSEA).
RESULTS
Characteristics of the Participants
The mean age of participants for these analyses was 48.9 (SD=5.7) years in total participants (Table 1). Over 61% of the participants had completed college or graduate degrees. About 69% of participants were married or partnered, and 75% were employed. Approximately 44% of the participants indicated that their family income was enough to pay for basics (e.g., food, housing, heat, etc.). While all NH White and NH African American women were born in the U.S., approximately 27% of NH Asians and 77% of Hispanics were born in the U.S. The mean length of stay in the U.S. was 26.5 (SD=17.4) years in NH Asians and 44.2 (SD=11.5) years in Hispanics. While the average acculturation score in NH Asians was 3.3 (SD=1.1), the average acculturation score in Hispanics was 4.5 (SD=1.0) (Table 1).
Table 1.
Distributions of demographic and acculturation factors by race/ethnicity (N=980).
| Variables (range) | African American N (%) |
Asian American N (%) |
Hispanic N (%) |
White N (%) |
Total N (%) |
|---|---|---|---|---|---|
| n | 222 | 223 | 241 | 294 | 980 |
| Age, years (mean±SD) | 49.3±5.7 | 48.5±6.0 | 48.9±5.4 | 49.1±5.7 | 48.9±5.7 |
| Level of education | |||||
| ≤ High school (HS) | 17 (7.7) | 28 (12.6) | 41 (17.0) | 50 (17.0) | 136 (13.9) |
| HS < ≤ CO | 55 (24.3) | 25 (11.2) | 75 (31.1) | 87 (29.6) | 241 (24.6) |
| > College (CO) | 151 (68.0) | 170 (76.2) | 125 (51.9) | 157 (53.4) | 603 (61.5) |
| Marital status | |||||
| Yes | 124 (55.9) | 187 (83.9) | 163 (67.6) | 197 (67.0) | 671 (68.5) |
| No | 98 (44.1) | 36 (16.1) | 78 (25.2) | 97 (33.0) | 309 (31.5) |
| Employed | |||||
| Yes | 184 (82.9) | 137 (61.4) | 197 (81.7) | 212 (72.1) | 730 (74.5) |
| No | 38 (17.1) | 86 (38.6) | 44 (18.3) | 82 (27.9) | 250 (25.5) |
| Perceived family income | |||||
| Not enough | 29 (13.1) | 20 (9.0) | 40 (16.6) | 80 (27.2) | 169 (17.2) |
| Average | 88 (39.6) | 82 (36.8) | 99 (41.1) | 107 (36.4) | 376 (38.4) |
| Enough | 105 (47.3) | 121 (54.3) | 102 (42.3) | 107 (36.4) | 435 (44.4) |
| No. of children | |||||
| None | 46 (20.7) | 32 (14.3) | 37 (15.4) | 62 (21.1) | 177 (18.1) |
| 1–2 | 89 (40.1) | 142 (63.7) | 123 (51.0) | 149 (50.7) | 503 (51.3) |
| 3 or more | 87 (39.2) | 49 (22.0) | 81 (33.6) | 83 (27.7) | 300 (30.6) |
| Born in the US | |||||
| Yes | 222 (100.0) | 59 (26.5) | 186 (77.2) | 294 (100.0) | 761 (77.7) |
| No | 0 | 164(73.5) | 55 (22.8) | 0 | 219 (22.3) |
| Length of stay in the U.S., years (mean±SD) |
- | 26.5±17.4 | 44.2±11.5 | - | 14.2 |
| Level of acculturation (0–5) (mean±SD) |
- | 3.3±1.1 | 4.5±1.0 | - | 4.5±1.0 |
The mean BMI ranged from 23.5 (in NH Asian Americans) to 31.7 (in NH African Americans) (Table 2). Over 50% of the participants reported that they were healthy. Over 39% of the participants were postmenopausal, and about 90% did not use hormone therapy to relieve menopausal symptoms. The mean scores of menopausal symptoms ranged from 18.7 (in NH African American women) to 22.0 (in NH White women), and the mean severity scores of menopausal symptoms ranged from 41.7 (in NH Asian American women) to 68.1 (in NH White women) (Table 2).
Table 2.
Distributions of health and menopausal status by race/ethnicity (N=980).
| Variables (range) | African American N (%) |
Asian American N (%) |
Hispanic N (%) |
White N (%) |
Total N (%) |
|---|---|---|---|---|---|
| n | 222 | 223 | 241 | 294 | 980 |
| Body-mass index, kg/m2, (mean±SD) |
31.7±7.7 | 23.5±4.1 | 29.6±7.4 | 29.4±8.1 | 28.5±7.6 |
| Perceived general health | |||||
| Extremely unhealthy | 4 (1.8) | 3 (1.3) | 8 (3.3) | 19 (6.5) | 34 (3.5) |
| Unhealthy | 26 (11.7) | 27 (12.1) | 49 (20.3) | 50 (17.0) | 152 (15.5) |
| No idea | 16 (7.2) | 23 (10.3) | 15 (6.2) | 19 (6.5) | 73 (7.4) |
| Healthy | 144 (64.9) | 134 (60.1) | 130 (53.9) | 161 (54.8) | 569 (58.1) |
| Extremely healthy | 32 (14.4) | 36 (16.2) | 39 (16.3) | 45 (15.2) | 152 (15.5) |
| Menopausal status | |||||
| Premenopausal | 55 (24.8) | 73 (32.7) | 67 (27.8) | 70 (23.8) | 265 (27.0) |
| Early menopausal | 54 (24.3) | 57 (25.6) | 59 (24.5) | 69 (23.5) | 239 (24.4) |
| Late menopausal | 19 (8.6) | 16 (7.2) | 25 (10.4) | 33 (11.2) | 93 (9.5) |
| Postmenopausal | 94 (42.3) | 77 (34.5) | 90 (37.3) | 122 (41.5) | 383 (39.1) |
| Usages of hormone | |||||
| Yes | 18 (8.1) | 9 (4.0) | 23 (9.5) | 38 (12.9) | 88 (9.0) |
| No | 204 (91.9) | 214 (96.0) | 218 (90.5) | 256 (87.1) | 892 (91.0) |
| Menopausal symptoms (mean±SD) |
|||||
| Number (0–73) | 18.7±12.7 | 14.7±11.8 | 20.2±13.7 | 22.0±13.9 | 19.2±13.4 |
| MS severity (0–292) | 56.3±44.6 | 41.7±40.6 | 61.3±50.4 | 68.1±52.3 | 57.7±48.6 |
Structural Equation Modeling on Menopausal Symptoms
The structural equation model for total participants showed that demographic factors (β=−0.335), specifically higher level of education, higher perceived family income, being employed, and having fewer children, and greater perceived general health (β=−0.172), were negatively related to menopausal symptoms (Figure 2 and Table 3). Additionally, acculturation factors (β=0.084; being born in the U.S. and longer stay in the U.S.) and greater BMI (β=0.117), were positively related to menopausal symptoms (Figure 2 and Table 3).
Figure 2.
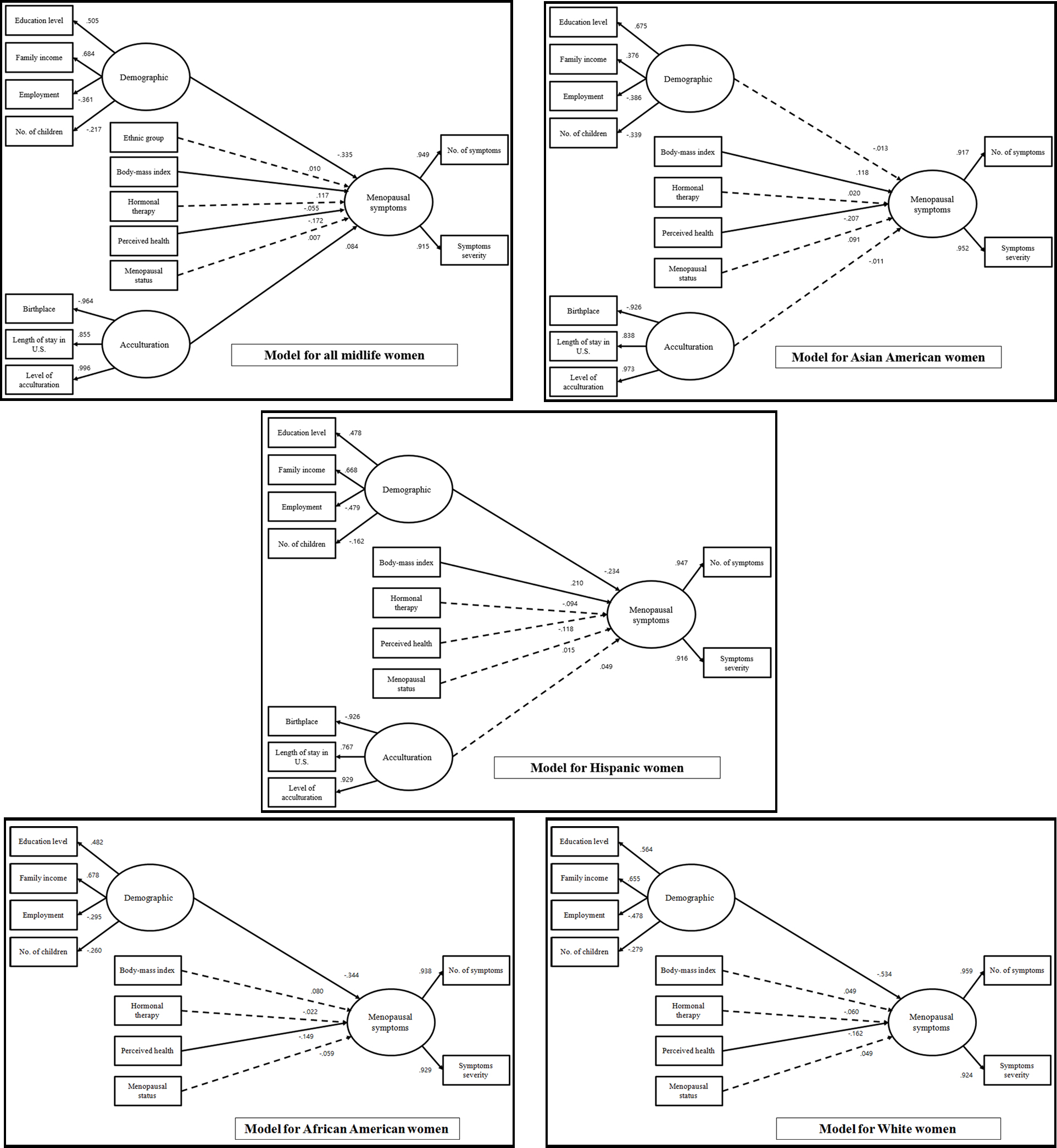
The structural equation models for menopausal symptoms in midlife women
Note: Significant pathways are represented as solid lines while not significant ones are represented as dotted lines.
Table 3.
Path coefficients among the variables by race/ethnicity (N=980).
| Variables | Endogenous variables |
African American |
Asian American |
Hispanic | White | Total |
|---|---|---|---|---|---|---|
| Demographic factors§ | Menopausal symptoms |
−0.344** | −0.013 | −0.234* | −0.534** | −0.335** |
| Racial/ethnic group | - | - | - | - | 0.010 | |
| Body-mass index | −0.080 | 0.118* | 0.210** | 0.049 | 0.117** | |
| Usage of hormone therapy |
−0.022 | 0.020 | −0.094 | −0.060 | −0.055 | |
| Perceived general health | −0.149* | −0.207* | −0.118 | −0.162* | −0.172** | |
| Menopausal status | −0.059 | 0.091 | 0.015 | 0.049 | 0.007 | |
| Acculturation factors | - | −0.011 | 0.049 | - | 0.084* | |
| Squared multiple correlations (R2) for menopausal symptoms |
20% | 7% | 16% | 41% | 24% | |
Note. Path coefficients were presented as standard regression weights; §Demographic factors consisted of the level of education, perceived family income, employment, and the number of children.
p<.05/
p<.01
The models for NH White and NH African American women showed that demographic factors (indicative of a higher level of education, higher perceived family income, being employed, and having fewer children; β=−0.534 for NH Whites and β =−0.344 for NH African Americans) and better perceived general health (β=−0.162 for NH Whites and β=−0.149 for NH African Americans) were significantly negatively associated with reporting menopausal symptoms (Figure 2). The model for Hispanic women also showed that having a higher level of education and higher perceived family income, being employed, and having fewer children (β=−0.234) were negatively related to reporting menopausal symptoms (Figure 2 and Table 3). In addition, Hispanic women with higher BMI (β=0.210) reported significantly more severe menopausal symptoms (Table 3). Lastly, the model for NH Asian women showed that higher BMI (β=0.118) and poorer perceived general health (β=−0.207) were positively related to reporting menopausal symptoms.
The squared multiple correlations for the models were 24% for total participants, 41% for NH Whites, 20% for NH African Americans, 7% for NH Asians, and 16% for Hispanics. Fit indices for all five models were satisfactory based on the standard guidelines that were recommended by Bae (2010) (see Table 4).
Table 4.
Fit indices of the structural equation models by race/ethnicity (N=980).
| African American |
Asian American |
Hispanic | White | Total | |
|---|---|---|---|---|---|
| Goodness of fit index (GFI) | 0.968 | 0.931 | 0.923 | 0.981 | 0.948 |
| Adjusted goodness of fit index (AGFI) | 0.928 | 0.879 | 0.865 | 0.957 | 0.910 |
| Normed fit index (NFI) | 0.952 | 0.928 | 0.924 | 0.974 | 0.950 |
| Comparative fit index (CFI) | 0.982 | 0.962 | 0.951 | 0.995 | 0.956 |
| Toot mean square error of approximation (RMSEA) |
0.050 | 0.067 | 0.082 | 0.026 | 0.078 |
DISCUSSION
The findings presented in this paper indicated prominent racial/ethnic differences in the relationships of multiple covariates to menopausal symptoms. In all racial/ethnic groups except NH Asian women, demographic factors—especially those related to socioeconomic status—were significantly associated with the women’s menopausal symptoms. Although the significant associations between demographic factors and reporting menopausal symptoms have been confirmed in the literature, the direction of the associations was inconsistent. One group of studies reported that those with low educational attainment or homemakers were more likely to report menopausal symptoms (Gold et al 2006; Huseth-Zosel, Strand, and Perry 2014). The other group of studies reported that those who were employed or had higher levels of education or income were more likely to report menopausal symptoms (Bawar et al. 2013). The findings of this study agree with the results of the first group of studies. Because the data in these secondary analyses were collected through national approaches that have rarely been adopted in existing studies, the fact that the findings of this analysis agree with those of the first group of studies, some of which were also conducted on samples from multiple areas of the U.S., could add important information to the current literature.
In all racial/ethnic groups except Hispanic women, poor perceived health status was significantly associated with greater likelihood to report menopausal symptoms. Prior studies have reported that, regardless of their actual health status or symptom experience, Hispanic women perceive their health as poor when they do not have a healthy lifestyle (Smith, Glazier, and Sibley 2010; Svedberg et al. 2006). Thus, even when they are actually healthy and do not have any symptoms, they may perceive their health as poor if they do not have a healthy lifestyle. Subsequently, these ethnic-specific attitudes could have influenced the association of perceived health status to menopausal symptoms in Hispanic women differently from other racial/ethnic groups. However, this inference tends to be new to the literature, so further investigations are necessary.
Only in NH Asians and Hispanics was BMI significantly positively associated with menopausal symptoms, which is a new finding added to the literature. Significant differences in the perception of body weight between NH Whites and NH African-Americans have been reported; NH African-American women tend to report positive cultural attitudes toward large body sizes (high BMI), which usually makes them not worry about their weight (Hendley et al. 2011; Shoneye et al. 2011). However, attitudes toward body weight have rarely been studied in Hispanic or NH Asian women, although they could provide an answer for the question about why BMI was significantly associated with menopausal symptoms only in Hispanic and NH Asian women. In a recent study on NH Asian women’s attitudes toward physical activity, NH Asian women had cultural attitudes related to body weight that were similar to NH White women’s (Im et al. 2012b). In another study on Hispanic women’s attitudes toward physical activity, Hispanic women reportedly had cultural attitudes related to body weight that were similar to NH African American women’s (Im et al. 2010b). Thus, it would be difficult to interpret the finding based on the existing literature.
Interestingly, the level of acculturation was not significantly associated with menopausal symptoms in NH Asians and Hispanics, but it was one of the significant factors related to menopausal symptoms among total participants. A plausible rationale would be the absence of variations in the level of acculturation in each racial/ethnic group, which would be a limitation of this study as a secondary analysis of the Internet survey data (e.g., homogeneity of Internet populations).
The findings also suggested that the AIMS model would work better (with higher model fit indices) in NH White midlife women compared with in other racial/ethnic minorities, although the original model was developed for NH Asian midlife women. A conceivable reason would be that the major concepts of the AIMS were developed mainly based on a systematic integrated review of existing studies, and the major concepts from the literature might reflect NH White midlife women’s menopausal symptoms better than other racial/ethnic minority groups’. Indeed, studies have reported that the current knowledge on menopausal symptom experience in the literature still tends not to reflect menopausal symptom experience of racial/ethnic minorities (Ayers, Forshaw, and Hunter, 2010; Hoga et al. 2015). Yet, this would be one of the first studies that actually examined a model from the literature in different racial/ethnic groups using SEM analyses.
The study included several limitations because it was a secondary analysis. First, the sample size was predetermined, and the researchers did not have any control over the data collected so that some important variables, such as those pertaining to lifestyle, were not included, which could have resulted in residual confounding and could thus have affected the accuracy of the findings. Second, the sample size, when stratified on race/ethnicity or type of symptoms, might not have been large enough to detect some modest associations as statistically significant, particularly those that have been noted in larger studies. Third, the study participants of the original studies were a select group of midlife women. Although a quota sampling method was used in the original studies, the study participants still tended to be high income and highly educated women. Also, the women were required to be able to read and write in English, which definitely restricts the generalizability of the study findings. In addition, this study did not include lifestyle factors (e.g., smoking), which have been significantly related to symptoms during the menopause transition in a number of prior studies. Finally, the cross-sectional design of the study limits the interpretation of the study findings because of the inability to determine temporal relations and thus causality.
CONCLUSIONS
This study supported that significant factors related to reporting menopausal symptoms were different in different racial/ethnic groups. Also, the findings supported that the model based on the literature would work better in explaining the menopausal symptom experience of NH White midlife women. These findings suggest the following implications for future research and practice with multi-racial/ethnic groups of midlife women in menopausal transition. First, health care providers and researchers need to reflect on the racial/ethnic differences in the relationships of multiple factors to menopausal symptoms so that they can provide appropriate and adequate health care for the women while considering the differences. As the findings indicated, multiple factors could be differently associated with menopausal symptom experiences of midlife women in each racial/ethnic group. Thus, health care intervention (e.g., health education, coaching/support) for a specific racial/ethnic group of midlife women needs to incorporate these different factors in its design, structure, content, and implementation. Also, further cultural studies on the associations of racial/ethnic-specific significant factors (e.g., perceived health status, BMI) to menopausal symptoms would help grasp the possible causes for the existing racial/ethnic differences in the significant factors influencing menopausal symptoms. In addition, further studies are needed to explore racial/ethnic differences in the associations by types of symptoms because the associations could be different depending on the types of symptoms (e.g., vasomotor symptoms, musculoskeletal symptoms). Finally, the study has limitations in its generalizability as discussed above. Thus, more research with various groups of the major racial/ethnic groups could also help solve the puzzle around the racial/ethnic differences in the covariates of menopausal symptoms in different racial/ethnic groups.
Acknowledgement:
The data for this study came from two larger studies funded by the National Institutes of Health (NIH/NINR/NIA; R01NR008926 and NIH/NINR/ NHLBI; R01NR010568). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The authors have no conflict of interest/financial disclosure.
REFERENCES
- Andrist LC, and MacPherson KI. 2001. Conceptual models for women’s health research: reclaiming menopause as an exemplar of nursing’s contributions to feminist scholarship. Annual Review of Nursing Research 19:29–60. [PubMed] [Google Scholar]
- Authors. 2010. Reference blinded for the review
- Authors. 2012. Reference blinded for the review
- Avis NE, Stellato R, Crawford S, Bromberger J, Ganz P, Cain V, and Kagawa-Singer M. 2001. Is there a menopausal syndrome? Menopausal status and symptoms across racial/ethnic groups. Social Science & Medicine 52(3):345–356. [DOI] [PubMed] [Google Scholar]
- Ayers B, Forshaw M, and Hunter MS. 2010. The impact of attitudes towards the menopause on women’s symptom experience: A systematic review. Maturitas 65 (1): 28–36. 10.1016/j.maturitas.2009.10.016. [DOI] [PubMed] [Google Scholar]
- Bae BL. (2009). Structural equation modeling with Amos 17.0: principles and practice Seoul: Cheunglam. [Google Scholar]
- Bagozzi RP and Yi Y. 2012. Specification, evaluation, and interpretation of structural equation models. Journal of the Academy of Marketing Science 40(1): 8–34. 10.1007/s11747-011-0278-x [DOI] [Google Scholar]
- Bawar S, Sadaf F, Rahim R, and Faiz NR. 2013. Comparison of vasomotor symptoms in postmenopausal women with different socio-economic status. Gomal Journal of Medical Science 11 (2): 195–8. [Google Scholar]
- Elavsky S, and Gold CH. 2009. Depressed mood but not fatigue mediate the relationship between physical activity and perceived stress in middle-aged women. Maturitas 64(4): 235–240. 10.1016/j.maturitas.2009.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman EW 2015. Depression in the menopause transition: risks in the changing hormone milieu as observed in the general population. Women’s Midlife Health 1:2 10.1186/s40695-015-0002-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold EB, Colvin A, Avis N et al. 2006. Longitudinal analysis of vasomotor symptoms and race/ethnicity across the menopausal transition: Study of Women’s Health Across the Nation (SWAN). Am J Public Health 96:1226–35. PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold EB, Bair Y, Block G, Greendale GA, Harlow SD, Johnson S,… and Zhang G. 2007. Diet and lifestyle factors associated with premenstrual symptoms in a racially diverse community sample: Study of Women’s Health Across the Nation (SWAN). Journal of Women’s Health 16(5): 641–656. 10.1089/jwh.2006.0202 [DOI] [PubMed] [Google Scholar]
- Gold EB, Crawford SL, Shelton JF, Tepper PG, Crandall CJ, Greendale GA,… and Avis NE. 2017. Longitudinal analysis of changes in weight and waist circumference in relation to incident vasomotor symptoms: the Study of Women’s Health Across the Nation (SWAN). Menopause 24(1):9–26. 10.1097/GME.0000000000000723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold EB, Sternfeld B, Kelsey JL, Brown C, Mouton C, Reame N,… and Stellato R. 2000. Relation of demographic and lifestyle factors to symptoms in a multi-racial/ethnic population of women 40–55 years of age. American Journal of Epidemiology 152(5):463–473. [DOI] [PubMed] [Google Scholar]
- Haines CJ, Xing S-M, Park K-H, Holinka CF, and Ausmanas MK. 2005. Prevalence of menopausal symptoms in different ethnic groups of Asian women and responsiveness to therapy with three doses of conjugated estrogens/medroxyprogesterone acetate: the Pan-Asia Menopause (PAM) study. Maturitas 52(3–4):264–276. 10.1016/j.maturitas.2005.03.012 [DOI] [PubMed] [Google Scholar]
- Hendley Y, Zhao L, Coverson DL, Din-Dzietham R, Morris A, Quyyumi AA, Gibbons GH, and Vaccarino V. 2011. Differences in weight perception among blacks and whites. Journal of Women’s Health 20 (12): 1805–11. 10.1089/jwh.2010.2262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoga L, Rodolpho J, Goncalves B, and Quirino B. Women’s experience of menopause: A systematic review of qualitative evidence. JBI Database of Systematic Reviews and Implementation Reports 13 (8):250–337. 10.11124/jbisrir-2015-1948. [DOI] [PubMed] [Google Scholar]
- Huseth-Zosel A, Strand M, and Perry J. 2014. Socioeconomic differences in the menopausal experience of Chinese women. Post Reproductive Health 20(3): 98–103. 10.1177/2053369114544729. [DOI] [PubMed] [Google Scholar]
- Im EO 2006. The midlife women’s symptom index (MSI). Health Care for Women International 27(3): 268–87. 10.1080/07399330500506600. [DOI] [PubMed] [Google Scholar]
- Im EO 2010. A situation-specific theory of Asian immigrant women’s menopausal symptom experience in the United States. ANS. Advances in Nursing Science 33(2):143–157. 10.1097/ANS.0b013e3181dbc5fa [DOI] [PMC free article] [PubMed] [Google Scholar]
- Im E-O, and Chee W. 2005. A descriptive Internet survey on menopausal symptoms: five ethnic groups of Asian American university faculty and staff. Journal of Transcultural Nursing 16(2):126–135. 10.1177/1043659604273550 [DOI] [PubMed] [Google Scholar]
- Im EO, Chee W, Bender M, Cheng CY, Tsai HM, Kang NM, and Lee H. 2005. The psychometric properties of pen-and-pencil and internet versions of the midlife women’s symptom index (MSI). International Journal of Nursing Studies 42(2):167–77. 10.1016/j.ijnurstu.2004.06.005. [DOI] [PubMed] [Google Scholar]
- Im EO, Chee W, Lim HJ, Liu Y, and Kim HK. 2008. Midlife women’s attitudes toward physical activity. Journal of Obstetric, Gynecologic, and Neonatal Nursing 37(2):203–13. 10.1097/nnr.0b013e31825da85a. [DOI] [PubMed] [Google Scholar]
- Im EO, Ko Y, Hwang H, Chee W, Stuifbergen A, Lee H, and Chee E. 2012. Asian American midlife women’s attitudes toward physical activity. Journal of Obstetric, Gynecologic, and Neonatal Nursing 41(5):650–8. 10.1111/j.1552-6909.2012.01392.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Im EO, Lee B, Chee W, Brown A, and Dormire S. 2010. Menopausal symptoms among four major ethnic groups in the United States. Western Journal of Nursing Research 32(4):540–565. 10.1177/0193945909354343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Im EO, Lee B, Chee W, Dormire S, and Brown A. 2010. A National Multiethnic Online Forum Study on Menopausal Symptom Experience. Nursing Research 59(1):26–33. 10.1097/NNR.0b013e3181c3bd69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Im EO, Lee B, Hwang H, Yoo KH, Chee W, Stuifbergen A, Walker L, et al. 2010b. “A waste of time”: Hispanic women’s attitudes toward physical activity. Women & Health 50(6):563–79. 10.1080/03630242.2010.510387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones EK, Jurgenson JR, Katzenellenbogen JM, and Thompson SC. 2012. Menopause and the influence of culture: another gap for Indigenous Australian women? BMC Women’s Health 12:43 10.1186/1472-6874-12-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang Y, Han YR, Chang SJ, Chee W, and Im EO. 2015. The psychometric properties of the midlife women’s symptom index. Journal of Obstetric, Gynecologic, & Neonatal Nursing 44(5):600–9. 10.1111/1552-6909.12741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kagawa-Singer M, Wu K, Kawanishi Y, Greendale GA, Kim S, Adler SR, and Wongvipat N. 2002. Comparison of the Menopause and Midlife Transition between Japanese American and European American Women. Medical Anthropology Quarterly 16(1):64–91. 10.1525/maq.2002.16.1.64 [DOI] [Google Scholar]
- Kardia SR, Chu J, and Sowers MR. 2006. Characterizing variation in sex steroid hormone pathway genes in women of 4 races/ethnicities: the Study of Women’s Health Across the Nation (SWAN). The American Journal of Medicine 119(9 Suppl 1):S3–15. 10.1016/j.amjmed.2006.07.001 [DOI] [PubMed] [Google Scholar]
- Kline RB 2011. Principles and practice of structural equation modeling New York: Guilford Press. [Google Scholar]
- Kravitz HM, and Joffe H. 2011. Sleep during the perimenopause: a SWAN story. Obstetrics and Gynecology Clinics of North America 38(3):567–586. 10.1016/j.ogc.2011.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llaneza P, García-Portilla MP, Llaneza-Suárez D, Armott B, and Pérez-López FR. 2012. Depressive disorders and the menopause transition. Maturitas 71(2):120–130. 10.1016/j.maturitas.2011.11.017 [DOI] [PubMed] [Google Scholar]
- Lee B, Im EO, and Chee W. 2010. Psychometric evaluation of the midlife women’s symptom index in multiethnic groups. Western Journal of Nursing Research 32(8):1091–111. 10.1177/0193945910362066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melby MK, Lock M, and Kaufert P. 2005. Culture and symptom reporting at menopause. Human Reproduction Update 11(5):495–512. 10.1093/humupd/dmi018. [DOI] [PubMed] [Google Scholar]
- Mitchell ES, Woods NF, and Mariella A. 2000. Three stages of the menopausal transition from the Seattle Midlife Women’s Health Study: toward a more precise definition. Menopause 7(5):334–349. [DOI] [PubMed] [Google Scholar]
- Pimenta F, Leal I, Maroco J, and Ramos C. 2011. Perceived control, lifestyle, health, socio-demographic factors and menopause: Impact on hot flashes and night sweats. Maturitas 69(4):338–342. 10.1016/j.maturitas.2011.05.005 [DOI] [PubMed] [Google Scholar]
- Pimenta F, Leal I, Maroco J, and Ramos C. 2012a. Menopausal symptoms: Do life events predict severity of symptoms in peri- and post-menopause? Maturitas 72(4):324–331. 10.1016/j.maturitas.2012.04.006 [DOI] [PubMed] [Google Scholar]
- Pimenta F, Leal I, Maroco J, and Ramos C. 2012b. Menopause symptoms’ predictors: the influence of lifestyle, health- and menopause-related, and sociodemographic characteristics. Journal of Women & Aging 24(2):140–151. 10.1080/08952841.2012.639653 [DOI] [PubMed] [Google Scholar]
- Pimenta F, Maroco J, Ramos C, and Leal I. 2014. Menopausal Symptoms: Is Spirituality Associated with the Severity of Symptoms? Journal of Religion and Health 53(4):1013–1024. 10.1007/s10943-013-9696-z [DOI] [PubMed] [Google Scholar]
- Seib C, Anderson D, Lee K, and Humphreys J. 2013. Predictors of mental health in post-menopausal women: Results from the Australian healthy aging of women study. Maturitas 76(4):377–383. 10.1016/j.maturitas.2013.09.003 [DOI] [PubMed] [Google Scholar]
- Shoneye C, Johnson F, Steptoe A, and Wardle J. 2011. A qualitative analysis of black and white British women’s attitudes to weight and weight control. Journal of Human Nutrition and Dietetics 24(6):536–42. 10.1111/j.1365-277x.2011.01198.x. [DOI] [PubMed] [Google Scholar]
- Smith PM, Glazier RH, and Sibley LM. 2010. The predictors of self-rated health and the relationship between self-rated health and health service needs are similar across socioeconomic groups in Canada. Journal of Clinical Epidemiology 63(4):412–21. 10.1016/j.jclinepi.2009.08.015. [DOI] [PubMed] [Google Scholar]
- Suinn RM, Rickard-Figueroa K, Lew S, and Vigil P. 1987. The Suinn-Lew Asian self-identity acculturation scale: An initial report. Educational and Psychological Measurement 47:401–407. 10.1177/0013164487472012. [DOI] [Google Scholar]
- Suinn RM, Ahuna C, and Khoo G. 1992. The Suinn-Lew Asian self-identity acculturation scale: Concurrent and factorial validation. Educational and Psychological Measurement 52(4):1041–6. 10.1177/0013164492052004028. [DOI] [Google Scholar]
- Svedberg P, Bardage C, Sandin S, and Pedersen NL. 2006. A prospective study of health, life-style and psychosocial predictors of self-rated health. European Journal of Epidemiology 21(10):767–76. 10.1007/s10654-006-9064-3. [DOI] [PubMed] [Google Scholar]
- Thurston RC, Sowers MR, Chang Y, Sternfeld B, Gold EB, Johnston JM, and Matthews KA. 2008. Adiposity and reporting of vasomotor symptoms among midlife women: the study of women’s health across the nation. American Journal of Epidemiology 167(1): 78–85. 10.1093/aje/kwm244 [DOI] [PubMed] [Google Scholar]
- Thurston RC, Sowers MR, Sutton-Tyrrell K, Everson-Rose SA, Lewis TT, Edmundowicz D, and Matthews KA. 2008. Abdominal adiposity and hot flashes among midlife women. Menopause 15(3):429–434. 10.1097/gme.0b013e31815879cf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan TTH. (2002). Evidence-based health care management. Multivariate modeling approach New York: Kluwer Academic Publisher. [Google Scholar]


