Abstract
Purpose
Diagnostic I-131 MIBG scintigraphy is an important imaging modality for evaluation of patients with neuroblastoma (NB) especially in centers where I-123 MIBG is not available. Single photon emission computed tomography/computed tomography (SPECT/CT) could potentially improve lesion detection over planar scintigraphy, but studies regarding its usefulness as an add-on to diagnostic I-131 MIBG scintigraphy are limited. This study aimed to determine the usefulness and factors related to usefulness of SPECT/CT in diagnostic I-131 MIBG scintigraphy in NB patients.
Methods
Usefulness of SPECT/CT for lesion detection, lesion localization, resolving suspicious findings, and clarifying the nature of lesions on anatomical imaging were retrospectively reviewed in 86 diagnostic planar I-131 MIBG scintigrams with add-on SPECT/CT.
Results
SPECT/CT detected additional lesions in 23.2%(20/86), helped localize lesions in 21.1%(8/38), resolved suspicious findings in 85.7%(6/7), determined functional status of lesions on anatomical imaging in 94.4%(17/18), and changed diagnosis from a negative to a positive study in 19.5%(8/41). Independent predictors of SPECT/CT being useful included presence of suspicious findings on planar imaging (OR 99.08; 95% C.I. 6.99–1404.41; p = 0.001), positive findings on planar imaging (OR 4.61; 95% C.I. 1.05, 20.28; p < 0.001), and presence of structural lesions on anatomical imaging (OR 32.54; 95% C.I. 5.37–196.96; p < 0.001).
Conclusion
SPECT/CT is a useful add-on to diagnostic planar I-131 MIBG scintigraphy. Predictors of usefulness of SPECT/CT include suspicious or positive findings on planar scintigraphy and the presence of structural lesions on anatomical imaging.
Keywords: Diagnostic I-131 MIBG scintigraphy, MIBG, Neuroblastoma, Radionuclide imaging, SPECT/CT
Background
Neuroblastoma (NB) is one of the most common early childhood malignancies with an incidence ranging from 2.7 to 12 per million [1]. Originating from neural crest cells, NB arises from the adrenal glands in approximately half of cases but can occur at any site along the sympathetic nervous system including the abdomen, chest, neck, and pelvis [2]. Patients are treated with multimodality therapy. Diagnostic imaging plays a crucial role throughout the course of treatment. Anatomical imaging including computed tomography (CT), magnetic resonance imaging (MRI), and ultrasonography (US) are used for evaluation of local disease staging and monitoring [3]. Whole body radionuclide imaging with metaiodobenzylguanidine (MIBG) labeled with either iodine-123 (I-123) or iodine-131 (I-131) is important for detection and staging of distant metastasis, as well as provides insight into tumor function [4]. MIBG is an analogue of norepinephrine and can be taken up into cells of neural crest tumors including neuroblastoma. Due to a more favorable gamma radiation energy, I-123 MIBG results in higher quality images than I-131 MIBG and is the preferred imaging agent [5], although I-123 requires cyclotron for production and is considerably more expensive. I-131 MIBG plays a key role as a systemic radionuclide therapeutic agent but diagnostic imaging using I-131 MIBG is still used in centers where I-123 MIBG is not available. Both I-123 and I-131 MIBG scintigraphy has been found to have high sensitivity for detection of NB lesions with specificity approaching 100% [6–8], although it has been reported that I-123 MIBG is able to detect more lesions than I-131 MIBG [9].
In recent years, hybrid imaging has played an increasing role in radionuclide imaging. Single photon emission tomography/computed tomography (SPECT/CT) provides both functional anatomical information. In I-123 MIBG scintigraphy, SPECT/CT has been reported to detect more functioning lesions than planar imaging [10, 11] as well as allowed better correlation with anatomical imaging [12]. A study done in I-123 MIBG scintigraphy in pheochromocytoma found that adding SPECT/CT lead to revision of original CT, MRI, or planar scintigraphy diagnosis in 6 out of 22 cases [13]. Similar benefits of SPECT/CT have also been reported in post-therapeutic I-131 MIBG scintigraphy [11]. Although newer SPECT/CT systems allow faster image acquisition, SPECT/CT in addition to planar scintigraphy still increases imaging time which may lead to increased need for patient sedation. The CT portion of SPECT/CT also imparts considerable additional radiation to patients which is a concern especially in NB patients which are mostly young children. For these reasons, adding SPECT/CT cannot be implemented routinely and must be tailored on an individual basis [14]. Diagnostic I-131 MIBG is still used for evaluation of patients with NB in centers where I-123 is not available, but the role of adding SPECT/CT to diagnostic planar I-131 MIBG scintigraphy has not been clearly defined. Findings in studies done in I-123 MIBG scintigraphy may not be applicable to I-131 MIBG scintigraphy since the image quality of the SPECT portion obtained from I-131 is inferior to that obtained from I-123. The objectives of this study were to determine the benefit of SPECT/CT in diagnostic I-131 MIBG scintigraphy and to determine factors related to its usefulness.
Methods
Patients
This cross-sectional retrospective medical record review was approved by the authors’ institutional Ethics Committee for Human Research (Ref. HE611069). Patients who underwent diagnostic planar I-131 MIBG scintigraphy with additional SPECT/CT at the author’s institution from 1 June 2013 to 31 December 2017 were included. Clinical data including age, sex, disease staging, and treatment received were obtained from the patient database of our center.
I-131 MIBG Scintigraphy
Patients were instructed to take 1 drop of 5% Lugol’s solution per 5 kg of body weight per day with a maximum dose of 3 drops per day, starting 3 days prior to I-131 MIBG administration and continued for 7 days after. Medications that could interfere with MIBG uptake were discontinued. I-131 MIBG at doses ranging from 20 to 40 MBq was intravenously injected slowly over 5 min. Anterior and posterior whole body planar scintigraphic images were acquired using Discovery NM/CT 670 dual-headed gamma camera system with SPECT/CT capability (GE Healthcare, IL, USA) equipped with high energy parallel hole collimator, with an energy peak set at 364 keV ± 10%, 256 × 256 imaging matrix, using continuous acquisition mode with detector speed of 4 cm per minute. Images were acquired at 24, 48, and optionally, 72 h after radiotracer administration. SPECT/CT was obtained at 48 or 72 h. The SPECT portion was acquired by step and shoot mode with 60 steps for each detector, at 3 degrees and 30 s/step with an imaging matrix of 64 × 64. Iterative reconstruction of SPECT images was done using OSEM (3 iterations × 6 subsets). Butterworth filter was used (cutoff frequency, 0.35; power, 10.00). Attenuation correction using CT data, scatter correction, as well as resolution recovery were also employed. Reconstruction was done using the Xeleris 3.0 software suite provided by the manufacturer. The CT portion was acquired using tube voltage of 100 kV with automatic exposure control and slice thickness of 2.5 mm for the chest and 3.75 mm for the abdomen. In the authors’ center, SPECT/CT is not routinely done in every patient. Whether or not to perform add-on SPECT/CT after planar imaging depended on the judgment of the nuclear medicine physician on duty on the day of examination, based on the findings of the planar images.
Image Interpretation
Planar scintigraphy was categorized in to three categories. A “positive” planar study contained at least one lesion with I-131 MIBG uptake more intense than the liver. A “negative” planar study contained no abnormal I-131 MIBG accumulation apart from physiological uptake. A “suspicious” planar study had possible abnormal I-131 MIBG uptake but the uptake is faint or indistinct. The sites and number of abnormal uptake was also noted. Usefulness of SPECT/CT was evaluated in different scenarios including detection of additional lesions over planar imaging, aiding anatomical localization, confirmation or exclusion of suspicious lesions detected in planar imaging, determination of functional status of lesions detected by CT, MRI, or US, and overall usefulness in terms of diagnostic interpretation. All planar and SPECT/CT images were read by an experienced nuclear medicine physician with 7 years of experience in reading diagnostic I-131 MIBG scintigraphic studies.
Statistical Analysis
Patient characteristics, treatment, results of planar I-131 MIBG scintigraphy and SPECT/CT were summarized using mean, standard deviation, and percentage. Univariable and multivariable logistic regression were used to explore factors that are related to usefulness of SPECT/CT. Only variables with P values > 0.25 in the univariable analysis were included in the multivariable analysis. Statistical analysis was carried out using Stata version 10 (StataCorp LLC, TX, USA). A P value of < 0.05 indicated statistical significance. Accompanying 95% confidence intervals (95% C.I.) were reported where appropriate.
Results
Patients
From 1 June 2013 to 31 December 2017, I-131 MIBG scintigraphy studies were done in 62 patients. Seven patients were excluded due to unavailable or incomplete histopathological diagnosis, leaving 55 patients who underwent 161 studies. A total of 86 SPECT/CT studies were done in 36 patients. Table 1 describes the characteristics of 36 patients. The group of patients had an average age of 4.8 ± 3.8 years and had a slight male predilection. Almost all patients had neuroblastoma with only two having ganglioneuroma. The most common primary site was the adrenal glands. Almost all patients had stage 4 disease. Table 2 summarizes treatment in relation to MIBG scintigraphy studies. The majority of MIBG scintigraphy studies were done after partial or complete tumor removal. Almost all MIBG scintigraphy studies were done after chemotherapy with only 4 done before start of chemotherapy. The average number of chemotherapeutic sessions was 9 ± 7.8. The average time window between MIBG scintigraphy and the most recent preceding chemotherapy session was 341 ± 485.9 days. Approximately 30% of MIBG scintigraphy studies was preceded by radiation therapy.
Table 1.
Patient characteristics
| Characteristics | Value | SD/percent |
|---|---|---|
| Age (years) | ||
| Mean | 4.8 | 3.8 |
| Median | 3.7 | |
| Range | 0.5–18.4 | |
| Sex | ||
| Male | 21 | 58.3% |
| Female | 15 | 41.7% |
| Histology | ||
| Neuroblastoma | 34 | 94.4% |
| Ganglioneuroma | 2 | 5.6% |
| Primary site | ||
| Adrenal | 27 | 75.0% |
| Mediastinum | 5 | 13.9% |
| Extra-adrenal, intra-abdominal | 2 | 5.6% |
| Neck | 1 | 2.8% |
| Other | 1 | 2.8% |
| Stage | ||
| Stage 2 | 1 | 2.8% |
| Stage 3 | 1 | 2.8% |
| Stage 4 | 32 | 88.8% |
| Stage 4s | 2 | 5.6% |
Table 2.
Treatment in relation to diagnostic I-131 MIBG scintigraphy
| Treatment | Value | SD/percent |
|---|---|---|
| Surgery prior to MIBG scintigraphy | ||
| No surgery | 10 | 11.6% |
| Partial tumor removal | 33 | 38.4% |
| Complete tumor removal | 43 | 50.0% |
| Chemotherapy sessions preceding MIBG scintigraphy | ||
| No preceding chemotherapy | 4 | 4.6% |
| Preceding chemotherapy | 82 | 95.4% |
| Number of chemotherapy sessions | ||
| Mean | 9 | ± 7.8 |
| Median | 7 | |
| Range | 1–29 | |
| Time from closest chemotherapy to MIBG scintigraphy (days) | ||
| Mean | 341 | ± 485.9 |
| Median | 108.5 | |
| Range | 0–2361 | |
| Radiation therapy preceding MIBG scintigraphy | ||
| No | 60 | 69.8% |
| Yes | 26 | 30.2% |
Results of Planar Imaging and Added Value of SPECT/CT
Of the 86 planar studies with add-on SPECT/CT, 41 (47.7%), 38 (44.2%), and 7 (8.1%) were negative, positive, and suspicious, respectively. On the other hand, among the 75 planar studies where add-on SPECT/CT was not deemed necessary, 57 (76%) were negative and 18 (24%) were positive, and none had suspicious findings. Only the 86 studies with both planar imaging and SPECT/CT were analyzed further. Description of planar scintigraphy and SPECT/CT are summarized in Table 3. Among the 38 positive planar studies, a total of 190 positive sites were found (mean ± SD, 5 ± 5.3). Soft tissue lesions accounted for 23.2% and bone metastases accounted for 76.8% of positive lesions. Of the 86 additional SPECT/CT studies, 71 included the whole abdomen, 7 included the upper abdomen, 2 included the lower abdomen, 29 included the chest, 6 included the neck, and 1 was done to examine the upper extremities. From 86 SPECT/CT studies, 20 detected a total of 25 additional functioning lesions (mean ± SD, 1.25 ± 0.64). The most common site of additional functioning lesions found by SPECT/CT were functioning intra-abdominal lymph node metastases followed by additional sites of bone metastases. When examining the usefulness of SPECT/CT in addition to planar scintigraphy, Table 4 describes the usefulness in different scenarios. As mentioned, SPECT/CT detected additional functioning lesions in only about a quarter of cases. In one case, SPECT/CT detected a small non-MIBG avid lung nodule which subsequently disappeared on follow-up diagnostic chest CT. When planar imaging was already unequivocally positive for functioning lesions, SPECT/CT detected additional sites of functioning lesions in 34.2% (13/38) and helped with localization in 21.1% (8/38) while providing no additional benefit in 44.7% (17/38). When planar imaging was unequivocally negative for functioning lesions, SPECT/CT changed the diagnosis to a positive study by demonstrating functioning lesions in only 19.5% (8/41) of cases and did not alter the diagnostic interpretation in the remaining 80.5% (33/41).
Table 3.
Findings of diagnostic planar I-131 MIBG scintigraphy and SPECT/CT
| Findings | Value | SD/percent |
|---|---|---|
| Results of planar scintigraphy | ||
| Positive | 38 | 44.2% |
| Negative | 41 | 47. 7% |
| Suspicious | 7 | 8.1% |
| Positive lesions in planar imaging | ||
| Total lesions (from 38 positive planar scintigrams) | 190 | |
| Mean | 5 | ± 5.3 |
| Median | 2 | |
| Range | 1–19 | |
| Site of positive lesions | ||
| Soft tissue lesions | 44 | 23.2% |
| Adrenal | 18 | 9.5% |
| Extra-adrenal intra-abdominal | 15 | 7.9% |
| Head and neck | 6 | 3.2% |
| Thorax and mediastinum | 5 | 2.6% |
| Bone metastasis | 146 | 76.8% |
| Spine | 30 | 15.8% |
| Humerus | 26 | 13.7% |
| Femur | 24 | 12.6% |
| Leg | 21 | 11.1% |
| Pelvic bones | 14 | 7.4% |
| Forearm | 13 | 6.8% |
| Skull | 11 | 5.8% |
| Thoracic cage | 4 | 2.1% |
| Foot | 3 | 1.6% |
| Additional functioning lesions detected by SPECT/CT | ||
| Total additional lesions (from 20 SPECT/CT studies) | 25 | |
| Mean | 1.25 | ± 0.64 |
| Median | 1 | |
| Range | 1–3 | |
| Site of additional lesions | ||
| Intra-abdominal lymph node metastasis | 12 | 48.0% |
| Bone metastasis | 7 | 28.0% |
| Adrenal mass | 4 | 16.0% |
| Liver metastasis | 1 | 4.0% |
| Mediastinal mass | 1 | 4.0% |
Table 4.
Usefulness of SPECT/CT in relation to planar scintigraphy
| Application of SPECT/CT | Usefulness of SPECT/CT | Number | Percent |
|---|---|---|---|
| Detection of additional lesions over planar MIBG | Number of cases that underwent SPECT/CT | 86 | 100.0% |
| Detected no additional lesions | 65 | 75.6% | |
| Detected additional non-functioning lesions | 1 | 1.2% | |
| Detected additional functioning lesions | 20 | 23.2% | |
| Studies with positive planar MIBG | Number of cases with positive lesions seen on planar imaging | 38 | 100.0% |
| SPECT/CT detected additional site of functioning lesions | 13 | 34.2% | |
| SPECT/CT helped with localization | 8 | 21.1% | |
| SPECT/CT provided no additional benefit | 17 | 44.7% | |
| Studies with negative planar MIBG | Number of negative planar studies | 41 | 100.0% |
| SPECT/CT changed diagnosis to a positive study | 8 | 19.5% | |
| SPECT/CT did not change diagnosis | 33 | 80.5% | |
| Studies with suspicious planar MIBG | Number of cases with suspicious findings on planar imaging | 7 | 100.0% |
| SPECT/CT helped confirm functioning lesion | 2 | 28.6% | |
| SPECT/CT helped exclude functioning lesion | 4 | 57.1% | |
| SPECT/CT could not resolve suspicious finding | 1 | 14.3% | |
| Studies with suspicious lesions in anatomical imaging and negative or suspicious planar MIBG | Number with suspicious lesions seen in anatomical imaging | 18 | 100.0% |
| SPECT/CT confirms functioning lesion | 15 | 83.3% | |
| SPECT/CT excludes functioning lesion | 2 | 11.1% | |
| SPECT/CT could not resolve suspicious finding | 1 | 5.6% | |
| Overall usefulness of SPECT/CT | Number of cases that underwent SPECT/CT | 86 | 100.0% |
| SPECT/CT added crucial diagnostic information and could not be omitted* | 14 | 16.3% | |
| SPECT/CT added non-crucial diagnostic information** | 21 | 24.4% | |
| SPECT/CT added no diagnostic information† | 51 | 59.3% |
*Examples of this category include SPECT/CT detected functional lesion(s) when planar scintigraphy was negative, thus changing the diagnosis from a negative study to a positive study; SPECT/CT confirmed or excluded suspicious findings on planar scintigraphy
**Examples of this category include SPECT/CT helped correctly localize lesions detected on planar scintigraphy; SPECT/CT detected additional lesions when planar scintigraphy was already positive
†Examples of this category include SPECT/CT detected no lesions in an already negative planar scintigraphy; SPECT/CT detected no additional lesions in an already positive planar scintigraphy
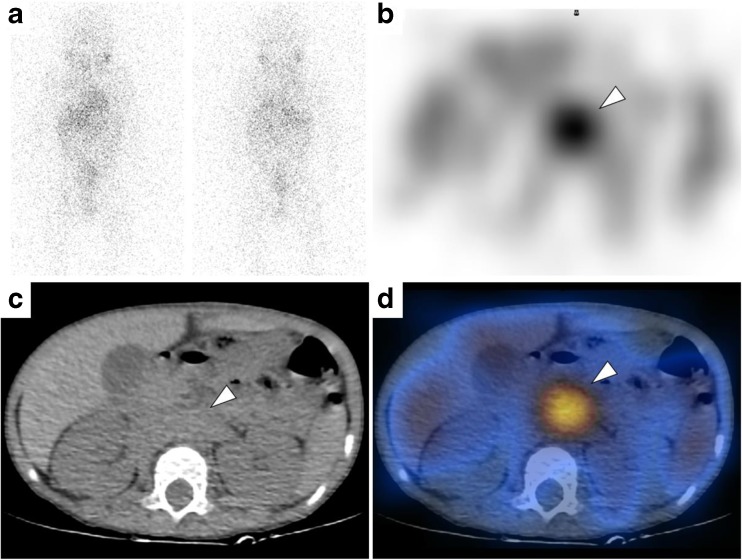
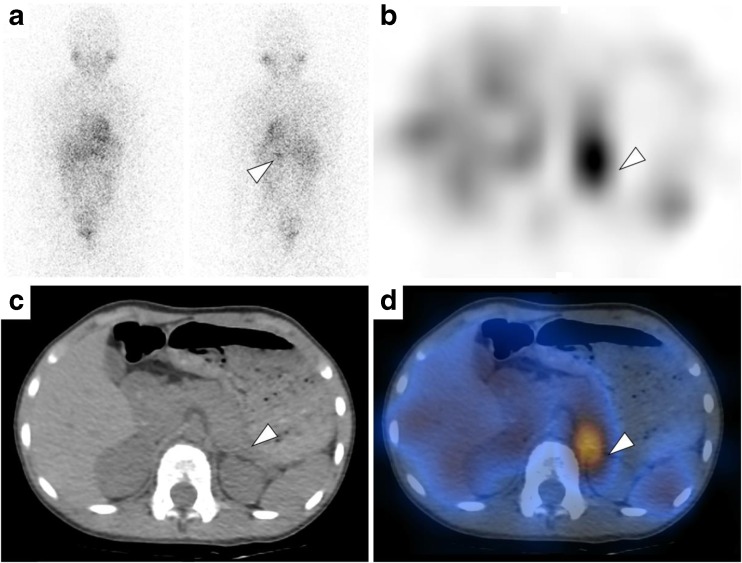
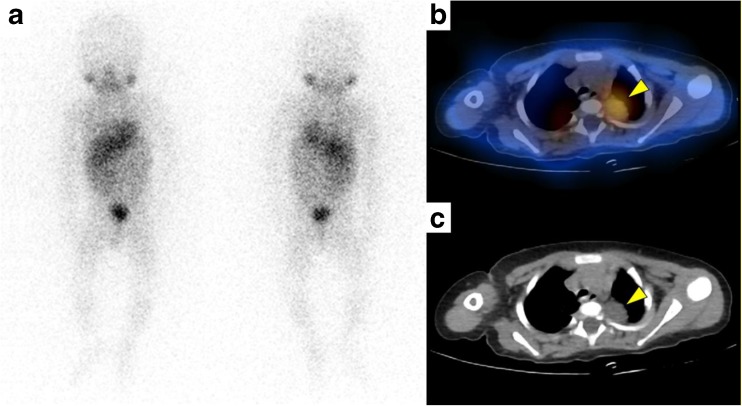
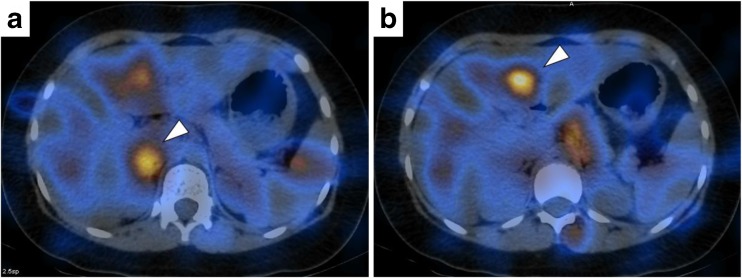
Figure 1 is an example of SPECT/CT that demonstrated a functioning tumor in a negative planar study. SPECT/CT was particularly useful in 7 cases where planar imaging yielded suspicious findings. Five cases were subtle uptake at the suprarenal regions. SPECT/CT resolved these findings by demonstrating that the uptake was in normal adrenal glands in 3 cases and confirmed that the uptake was in a residual tumor in 2 cases. Figure 2 is an example of SPECT/CT that clarified uptake in planar imaging as physiological uptake in the left adrenal gland. In one case, SPECT/CT clarified that focal uptake at the right side of the abdomen was physiological bowel activity. In another case where planar imaging revealed faint uptake at the right side of the neck, SPECT/CT still demonstrated faint equivocal uptake and could not resolve the suspicious finding. Further diagnostic CT found no abnormality and the uptake resolved in follow-up I-131 MIBG scintigraphy without further treatment. SPECT/CT was very useful in 18 cases where recent anatomical imaging including US, CT, or MRI detected structural lesions. SPECT/CT demonstrated that 15 cases (83.3%) was functioning due to definite I-131 MIBG uptake and excluded functioning lesions in 2 (11.1%) cases. There was only one case (5.6%) where SPECT/CT could not resolve suspicious findings on anatomical imaging. Figure 3 is an example of SPECT/CT that helped determine positive function in a mediastinal tumor detected on MRI, but planar imaging revealed no definite abnormal uptake. The overall usefulness and impact of SPECT/CT on the final diagnostic interpretation was divided into three categories. SPECT/CT added crucial diagnostic information and could not be omitted in only 16.3% (14/86) of cases. Another 24.4% (21/86) of SPECT/CT studies added non-crucial information over planar imaging e.g. detected additional lesions in an already unequivocally positive planar scan. The majority of SPECT/CT studies, 59.3% (51/86), added no diagnostic information and was deemed unnecessary and could be omitted entirely without changing diagnostic interpretation over planar imaging alone such as cases where planar imaging was already negative and SPECT/CT did not detect any additional positive lesions. There was one instance where addition of SPECT/CT led to false positive findings. In this particular case, illustrated in Fig. 4, the planar imaging was negative, but SPECT/CT found apparent hotspots in segment 4 and caudate of the liver which resulted in the study being read as positive for functioning liver metastasis. Further US and MRI did not find any anatomical lesions in these segments and follow-up I-131 MIBG imaging did not demonstrate progression of these lesions. Upon closer examination of the SPECT/CT images, it was likely that the focal uptake at the caudate was likely physiological uptake in the nearby right adrenal gland and the focal hotspot in segment 4 was due to irregularity of appearance of radiotracer distribution brought on by the poor quality of I-131 SPECT imaging.
Fig. 1.
Planar and SPECT/CT I-131 MIBG imaging for treatment response evaluation in a 2-year-old boy with neuroblastoma treated with partial tumor removal and chemotherapy. a Planar imaging reveals no definite abnormal uptake. b SPECT portion reveals intense uptake at the mid-upper abdominal region. c Non-contrast CT portion. d Fused SPECT/CT images correlated the focal uptake with soft tissue thickening. Findings are consistent with residual functioning intra-abdominal lymph node metastasis
Fig. 2.
Planar and SPECT/CT I-131 MIBG imaging for post-treatment surveillance in an 8-year-old boy with neuroblastoma who was treated with complete tumor removal, completion of chemotherapy, and autologous stem cell transplantation resulting in disease remission. a Planar imaging revealed a distinct focal uptake at the left supra renal region seen in the posterior projection. b SPECT portion. c Non-contrast CT portion. d Fused SPECT/CT revealed that the uptake is located at the left suprarenal region with no evidence of a mass lesion on the CT portion of the image. Overall findings suggest physiological uptake in the left adrenal gland
Fig. 3.
Interim response evaluation SPECT/CT I-131 MIBG imaging in a 1-year-old boy with neuroblastoma being treated with chemotherapy. a Planar scintigraphy showing no discernible abnormal uptake. b Fused SPECT/CT. c Non-contrast CT reveal definite I-131 MIBG uptake in a posterior mediastinal mass already demonstrated in a recent MRI, a finding which indicated that the tumor was likely still viable and functioning
Fig. 4.
Surveillance I-131 MIBG imaging in a 9-year-old girl with neuroblastoma. The planar imaging was negative, but SPECT/CT resulted in apparent hotspots in segment 4 and caudate of the liver which resulted in the study being read as positive for functioning liver metastasis. Further US and MRI did not find any anatomical lesions in these segments and follow-up I-131 MIBG imaging revealed no change of these lesions
Predictors of Usefulness of SPECT/CT
To better understand the circumstances in which SPECT/CT would be useful, the overall usefulness of SPECT/CT was regrouped into two groups. The “useful” group (35/86) consisting of cases where SPECT/CT provided either crucial, or non-crucial information. The “not useful” group (51/86) are studies where SPECT/CT added no diagnostic information over planar imaging and could be omitted. Simple logistic regression was used to test possible predictors that would predict a useful SPECT/CT. Predictors tested included completeness of surgical removal of the primary tumor, number of chemotherapy sessions received before imaging, time window between imaging and the most recent preceding chemotherapy, receiving radiation therapy at any timepoint before imaging, results of planar imaging, and presence of structural lesions on recent anatomical imaging. Only three predictors seemed to be related with SPECT/CT usefulness including results of planar imaging, time window between imaging and the most recent preceding chemotherapy, and presence of structural lesions on recent anatomical imaging. Table 5 demonstrates results of logistic regression. Result of planar imaging was an independent predictor of the usefulness of SPECT/CT. Compared with cases with negative planar imaging, SPECT/CT was significantly more likely to be useful in cases with positive and suspicious findings. In the univariable analysis, the time window between chemotherapy and imaging seemed to be related to SPECT/CT usefulness with cases with the most recent chemotherapy of more than 6 months being less likely to benefit from SPECT/CT; however, this relationship was lost in the multivariable analysis. Another independent predictor of SPECT/CT usefulness was the presence of structural lesions on recent anatomical imaging which significantly increased the odds of SPECT/CT being useful in both the univariable and multivariable analysis.
Table 5.
Results of multiple logistic regression analysis to determine predictors of a useful SPECT/CT in addition to planar MIBG scintigraphy
| Predictor | Not useful | Useful | Percent useful | Univariable analysis | Multivariable analysis | ||||
|---|---|---|---|---|---|---|---|---|---|
| Crude OR | 95% C.I. | P value | Adjusted OR | 95% C.I. | P value | ||||
| Results of planar imaging | |||||||||
| Negative | 33 | 8 | 19.5% | 1.00 | 1.00 | ||||
| Positive | 17 | 21 | 55.3% | 5.10 | 1.87, 13.89 | 0.001 | 4.61 | 1.05, 20.28 | 0.043 |
| Suspicious | 1 | 6 | 85.7% | 24.75 | 2.60, 235.64 | 0.005 | 99.08 | 6.99, 1404.41 | 0.001 |
| Time from last chemotherapy | |||||||||
| < 1 month | 13 | 17 | 56.7% | 1.00 | 1.00 | ||||
| 1–6 months | 13 | 8 | 38.1% | 0.47 | 0.15, 1.47 | 0.195 | 0.58 | 0.14, 2.47 | 0.462 |
| > 6 months | 24 | 7 | 22.6% | 0.22 | 0.07, 0.68 | 0.008 | 0.27 | 0.04, 1.65 | 0.155 |
| Before start of chemotherapy | 1 | 3 | 75.0% | 2.29 | 0.21, 24.68 | 0.493 | 3.80 | 0.31, 46.20 | 0.294 |
| Lesion on anatomical imaging | |||||||||
| No | 49 | 19 | 27.9% | 1.00 | 1.00 | ||||
| Yes | 2 | 16 | 88.9% | 20.63 | 4.32, 98.42 | < 0.001 | 32.54 | 5.37, 196.96 | < 0.001 |
For this binary logistic regression analysis, usefulness of SPECT/CT was divided into two groups. “Not useful” are studies where SPECT/CT added no diagnostic information. “Useful” include studies where SPECT/CT added crucial diagnostic information and could not be omitted and studies where SPECT/CT added non-crucial diagnostic information
Discussion
In this study, the authors aimed to determine the usefulness of SPECT/CT in addition to diagnostic I-131 MIBG planar scintigraphy. Although I-123 MIBG is preferred over I-131 MIBG for diagnostic imaging, the cost of production of I-123 is high and may not be available in some centers; thus, diagnostic I-131 MIBG scintigraphy is still a relevant imaging modality. To the authors’ best knowledge, this is one of the first studies in published literature to investigate the role of SPECT/CT in diagnostic I-131 MIBG scintigraphy. Although SPECT/CT is a very useful modality that can provide a more detailed depiction of radiotracer uptake in relation to anatomical details, implementing SPECT/CT routinely in pediatric patients cannot be done due to increased radiation burden and increased imaging time which could lead to the increased need for sedation [14]. This study aimed to determine the usefulness of SPECT/CT and the circumstances that the modality would be most useful. In diagnostic I-123 MIBG scintigraphy, tomographic imaging using SPECT alone without hybrid CT increased the number of detectable lesions compared with planar imaging [15] and increased certainty of lesion localization [16]. Our study similarly found that SPECT/CT resulted in detection of more lesions than planar imaging and increased confidence of lesion localization which is expected of SPECT/CT with the increased contrast resolution of SPECT and anatomical information from CT. However, compared with a study done in I-123 MIBG scintigraphy, SPECT/CT detected additional lesions in 54% of the patients not visible in the planar scan [17] which was higher than our study which SPECT/CT detected additional functioning lesions in only 23.2% of cases. This could be due to the poorer imaging characteristics of I-131 compared with I-123. The most common site of added detection by SPECT/CT is the intra-abdominal lymph nodes. This is in line with a previous study that found that I-131 MIBG had limitations in detection of nodal disease [18]. To better understand the usefulness of SPECT/CT in relation to planar imaging, we rated the usefulness of SPECT/CT in cases where planar imaging was positive, negative, and suspicious. We also took into account results of anatomical imaging and how it may be related to SPECT/CT usefulness. Effect of clinical factors including type of surgery, number and timing of chemotherapy, and receiving radiation therapy was also analyzed. Multivariable logistic regression determined two independent factors that predict that added SPECT/CT would be useful i.e. findings on planar imaging and the structural lesions on anatomical imaging such as US, CT, or MRI. SPECT/CT was most useful when there was suspicious finding on planar imaging or when structural lesions were present on another anatomical imaging. This corresponds to a previous study which determined that the value of SPECT/CT lies within its ability to bridge the gap between planar MIBG scintigraphy and diagnostic anatomical imaging [12]. In 8 negative planar studies where SPECT/CT detected functioning lesions which changed the diagnosis to a positive study, closer examination revealed that, 7 out of 8 cases had structural lesions on a recent anatomical imaging. Conversely, of the 33 cases where SPECT/CT did not add benefit to an already negative planar study, none of them had lesions on anatomical imaging. This further strengthens the notion that presence of a structural lesion is an important predictor of SPECT/CT usefulness. Although a positive planar study was an independent predictor of SPECT/CT being useful, closer examination revealed that in 20 of 21 positive planar scans, the usefulness was only adding non-crucial information e.g. detection of additional functioning lesions, with only one case that SPECT/CT added crucial information by increasing confidence that intense suprarenal uptake seen in the planar scan was indeed a functioning residual tumor. Due to the physiological uptake of MIBG in the liver, limitations of MIBG scintigraphy in evaluation for liver lesions have been reported [19]. In this group of patients, we found one instance that SPECT/CT introduced a false positive reading in the liver. This pitfall has been previously described and attributed to inhomogeneities in the SPECT image resulting in apparent hotspots [20]. The CT portion of the SPECT/CT was low-dose and non-contrast-enhanced; thus, it was not adequate for assessment of structural liver lesions. Our study has several limitations. Due to its retrospective nature, selection bias cannot be avoided as performance of SPECT/CT was up to the decision of the nuclear medicine physician on duty. The decision of whether or not to perform add-on SPECT/CT was mainly dependent on results of planar imaging. Cases which received additional SPECT/CT had more positive and suspicious findings on planar imaging whereas cases that did not receive additional SPECT/CT were mostly cases with negative planar imaging. At our center, diagnostic I-131 MIBG scintigraphy has a waiting time of up to 1 month; therefore, performance of the study may not be within the standard timing. For example, some studies for initial disease staging were done after chemotherapy was already started which can cause reduction of tumor uptake of MIBG [21, 22]. Another limitation is that the correctness of planar and SPECT/CT readings could not be determined. As confirmation of imaging findings with further histopathological tissue diagnosis is rarely done, indices of diagnostic accuracy including sensitivity and specificity could not be calculated.
Conclusion
SPECT/CT in addition to diagnostic I-131 MIBG planar scintigraphy is a useful diagnostic modality but its use needs to be tailored in order to gain the most benefit while avoiding unnecessary radiation and increased imaging time. SPECT/CT would likely be useful in patients with suspicious findings on planar scintigraphy or when there is evidence of structural lesions on anatomical imaging.
Conflict of Interest
Daris Theerakulpisut, Yutapong Raruenrom, Nantaporn Wongsurawat, and Charoonsak Somboonporn declare that they have no conflict of interest. No funding was received for conduction of this study.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
The institutional review board of our institute approved this retrospective study, and the requirement to obtain informed consent was waived.
Contributor Information
Daris Theerakulpisut, Phone: +66(0)43363895, Email: daris.th@gmail.com.
Yutapong Raruenrom, Phone: +66(0)43363895, Email: yutapongkku@gmail.com.
Nantaporn Wongsurawat, Phone: +66(0)43363895, Email: dr.nantaporn@gmail.com.
Charoonsak Somboonporn, Phone: +66(0)43363895, Email: charoonsak.som@gmail.com.
References
- 1.Heck JE, Ritz B, Hung RJ, Hashibe M, Boffetta P. The epidemiology of neuroblastoma: a review. Paediatr Perinat Epidemiol. 2009;23:125–143. doi: 10.1111/j.1365-3016.2008.00983.x. [DOI] [PubMed] [Google Scholar]
- 2.Cohn SL, Pearson ADJ, London WB, Monclair T, Ambros PF, Brodeur GM, et al. The international neuroblastoma risk group (INRG) classification system: an INRG task force report. J Clin Oncol. 2009;27:289–297. doi: 10.1200/JCO.2008.16.6785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brisse HJ, McCarville MB, Granata C, Krug KB, Wootton-Gorges SL, Kanegawa K, et al. Guidelines for imaging and staging of neuroblastic tumors: consensus report from the international neuroblastoma risk group project. Radiology. 2011;261:243–257. doi: 10.1148/radiol.11101352. [DOI] [PubMed] [Google Scholar]
- 4.Bombardieri E, Giammarile F, Aktolun C, Baum RP, Bischof Delaloye A, Maffioli L, et al. 131I/123I-metaiodobenzylguanidine (mIBG) scintigraphy: procedure guidelines for tumour imaging. Eur J Nucl Med Mol Imaging. 2010;37:2436–2446. doi: 10.1007/s00259-010-1545-7. [DOI] [PubMed] [Google Scholar]
- 5.Parisi MT, Eslamy H, Park JR, Shulkin BL, Yanik GA. 131I-Metaiodobenzylguanidine theranostics in neuroblastoma: historical perspectives; practical applications. Semin Nucl Med. 2016;46:184–202. doi: 10.1053/j.semnuclmed.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 6.Feine U, Müller-Schauenburg W, Treuner J, Klingebiel T. Metaiodobenzylguanidine (MIBG) labeled with 123I/131I in neuroblastoma diagnosis and follow-up treatment with a review of the diagnostic results of the international workshop of pediatric oncology held in Rome, September 1986. Med Pediatr Oncol. 1987;15:181–187. doi: 10.1002/mpo.2950150408. [DOI] [PubMed] [Google Scholar]
- 7.Jacobson AF, Deng H, Lombard J, Lessig HJ, Black RR. 123I-meta-iodobenzylguanidine scintigraphy for the detection of neuroblastoma and pheochromocytoma: results of a meta-analysis. J Clin Endocrinol Metab. 2010;95:2596–2606. doi: 10.1210/jc.2009-2604. [DOI] [PubMed] [Google Scholar]
- 8.Bleeker G, Tytgat GAM, Adam JA, Caron HN, Kremer LCM, Hooft L, et al. 123I-MIBG scintigraphy and 18F-FDG-PET imaging for diagnosing neuroblastoma. Cochrane Database Syst Rev. 2015;9. 10.1002/14651858.CD009263.pub2. [DOI] [PMC free article] [PubMed]
- 9.Kushner BH, Kramer K, Modak S, Cheung N-KV. Sensitivity of surveillance studies for detecting asymptomatic and unsuspected relapse of high-risk neuroblastoma. J Clin Oncol. 2009;27:1041–1046. doi: 10.1200/JCO.2008.17.6107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Franzius C, Hermann K, Weckesser M, Kopka K, Juergens KU, Vormoor J, et al. Whole-body PET/CT with 11C-meta-hydroxyephedrine in tumors of the sympathetic nervous system: feasibility study and comparison with 123I-MIBG SPECT/CT. J Nucl Med. 2006;47:1635–1642. [PubMed] [Google Scholar]
- 11.Fukuoka M, Taki J, Mochizuki T, Kinuya S. Comparison of diagnostic value of I-123 MIBG and high-dose I-131 MIBG scintigraphy including incremental value of SPECT/CT over planar image in patients with malignant pheochromocytoma/paraganglioma and neuroblastoma. Clin Nucl Med. 2011;36:1–7. doi: 10.1097/RLU.0b013e3181feeb5e. [DOI] [PubMed] [Google Scholar]
- 12.Rozovsky K, Koplewitz BZ, Krausz Y, Revel-Vilk S, Weintraub M, Chisin R, et al. Added value of SPECT/CT for correlation of MIBG scintigraphy and diagnostic CT in neuroblastoma and pheochromocytoma. Am J Roentgenol. 2008;190:1085–1090. doi: 10.2214/AJR.07.2107. [DOI] [PubMed] [Google Scholar]
- 13.Meyer-Rochow GY, Schembri GP, Benn DE, Sywak MS, Delbridge LW, Robinson BG, et al. The utility of metaiodobenzylguanidine single photon emission computed tomography/computed tomography (MIBG SPECT/CT) for the diagnosis of pheochromocytoma. Ann Surg Oncol. 2010;17(2):392–400. doi: 10.1245/s10434-009-0850-5. [DOI] [PubMed] [Google Scholar]
- 14.Nadel HR. SPECT /CT in pediatric patient management. Eur J Nucl Med Mol Imaging. 2014;41(Suppl 1):S104–S114. doi: 10.1007/s00259-014-2697-7. [DOI] [PubMed] [Google Scholar]
- 15.Rufini V, Giordano A, Di Giuda D, Petrone A, Deb G, De Sio L, et al. [123I]MIBG scintigraphy in neuroblastoma: a comparison between planar and SPECT imaging. Q J Nucl Med. 1995;39:25–28. [PubMed] [Google Scholar]
- 16.Gelfand MJ, Elgazzar AH, Kriss VM, Masters PR, Golsch GJ. Iodine-123-MIBG SPECT versus planar imaging in children with neural crest tumors. J Nucl Med. 1994;35:1753–1757. [PubMed] [Google Scholar]
- 17.Černý I, Prášek J, Kašpárková H. Superiority of SPECT/CT over planar 123I-mIBG images in neuroblastoma patients with impact on Curie and SIOPEN score values. Nuklearmedizin. 2016;55:151–157. doi: 10.3413/Nukmed-0743-15-05. [DOI] [PubMed] [Google Scholar]
- 18.Dhull VS, Sharma P, Patel C, Kundu P, Agarwala S, Bakhshi S, et al. Diagnostic value of 18F-FDG PET/CT in paediatric neuroblastoma: comparison with 131I-MIBG scintigraphy. Nucl Med Commun. 2015;36:1007–1013. doi: 10.1097/MNM.0000000000000347. [DOI] [PubMed] [Google Scholar]
- 19.Dessner DA, DiPietro MA, Shulkin BL. MIBG detection of hepatic neuroblastoma: correlation with CT, US and surgical findings. Pediatr Radiol. 1993;23:276–280. doi: 10.1007/BF02010914. [DOI] [PubMed] [Google Scholar]
- 20.Rufini V, Fisher GA, Shulkin BL, Sisson JC, Shapiro B. Iodine-123-MIBG imaging of neuroblastoma: utility of SPECT and delayed imaging. J Nucl Med. 1996;37:1464–1468. [PubMed] [Google Scholar]
- 21.Maurea S, Fiumara G, Pellegrino T, Zampella E, Assante R, Mainenti P, et al. MIBG molecular imaging for evaluating response to chemotherapy in patients with malignant pheochromocytoma: preliminary results. Cancer Imaging. 2013;13:155–161. doi: 10.1102/1470-7330.2013.0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maurea S, Lastoria S, Caracò C, Indolfi P, Casale F, di Tullio MT, et al. Iodine-131-MIBG imaging to monitor chemotherapy response in advanced neuroblastoma: comparison with laboratory analysis. J Nucl Med. 1994;35:1429–1435. [PubMed] [Google Scholar]