Abstract
MYD88 mutations are one of the most recurrent mutations in hematologic malignancies. However, recent mouse models suggest that MYD88L265P alone may not be sufficient to induce tumor formation. Interplay between MYD88L265P and other genetic events is further supported by the fact that TNFAIP3 (A20) inactivation often accompanies MYD88L265P. However, we are still lacking information about the consequence of MYD88L265P in combination with TNFAIP3 loss in human B cell lymphoma. Review of our genetic data on diffuse large B cell lymphoma (DLBCL) and Waldenstrom macroglobulinemia (WM), found that a large percentage of DLBCL and WM cases that have a MYD88 mutation also harbor a TNFAIP3 loss, 55% DLBCL and 28% of WM, respectively. To mimic this combination of genetic events, we used genomic editing technology to knock out TNFAIP3 in MYD88L265P non-Hodgkin’s lymphoma (NHL) cell lines. Loss of A20 expression resulted in increased NF-κB and p38 activity leading to upregulation of the NF-κB target genes BCL2 and MYC. Furthermore, we detected the increased production of IL-6 and CXCL10 which led to an upregulation of the JAK/STAT pathway. Overall, these results suggest that MYD88L265P signaling can be enhanced by a second genetic alteration in TNFAIP3 and highlights a potential opportunity for therapeutic targeting.
Introduction
Next-generation sequencing data has revealed that MYD88 mutations are one of the most recurrent mutations in hematologic malignancies and are found in 20% of lymphomas (COSMIC data base1). While it is detected in many subtypes of B cell malignancies, its prevalence is highest in Waldenstrom macroglobulinemia (90–100%, WM), primary CNS lymphomas (79%), and the activated B cell subtype of diffuse large B cell lymphoma (39%, ABC-DLBCL)2–4. The most common MYD88 mutation described thus far is a single base pair mismatch resulting in an amino acid switch from lysine to proline at position 265 (MYD88L265P). MYD88 is an adaptor protein which acts downstream of the Toll-like receptor (TLR) and interleukin-1 pathways5. MYD88 activation leads to IRAK1/4 recruitment and further downstream activation and phosphorylation of TRAF6 and TAK1 resulting in NF-κB activation6. MYD88L265P is a constitutively active form of the protein and its expression leads to dysregulated NF-κB and STAT3 signaling2. Additionally, we have shown in a recent study that TAK1 is an essential player in the MYD88L265P pathway and that it contributes to cell proliferation and cytokine secretion7. Together, these data suggest that mutant forms of MYD88 drive development of lymphoma. However, it has recently been shown in mouse models that MYD88L265P alone is not sufficient to induce tumor formation and requires additional genetic hits, such as loss of the TNFAIP3 tumor suppressor (encodes for the A20 protein) or BCL2 upregulation8,9.
Deletion or mutations in TNFAIP3 on 6q23 are commonly found in DLBCL and WM10,11, and when combined with a MYD88 mutation may further lead to deregulated NF-κB activation. A20 is an inducible ubiquitin-modifying enzyme and part of the NF-κB-induced negative feedback loop12. Its role as a tumor suppressor gene in hematological malignancies has been shown in various studies, where restoring of A20 expression in A20 deficient cell lines lead to induction of apoptosis, cell growth arrest, and downregulation of NF-κB target genes10,13,14. Furthermore, it has been shown that A20 expression is rapidly induced in cells to counteract MYD88-driven proliferation and NF-κB activation8.
The mechanistic interplay and downstream consequence of MYD88L265P in combination with additional genetic hits have not been fully defined in human lymphoma models of MYD88L265P. From a clinical perspective, further insight on MYD88-driven proliferation is important for therapeutic targeting of this pathway. TLR signaling inhibitors have been shown to have an effect on tumor growth in MYD88 mutant cell line models and patient-derived DLBCL tumor xenograft mouse models15,16. Additionally, in a recent phase I/II clinical trial in relapsed or refractory ABC-DLBCL it was shown that 80% of patients who harbor a MYD88 together with a CD79B mutation were sensitive to the B cell receptor (BCR) signaling inhibitor ibrutinib. The same study also showed that inactivation of TNFAIP3 reduced ibrutinib response17. Novel therapeutic agents continue to be developed to target the MYD88L265P pathway in both DLBCL and WM and delineation of the mechanism of how this mutation impacts tumor cells alone, or in combination with additional genetic hits, is of clinical significance. Therefore, the aim of this study is to investigate the cellular consequences of MYD88L265P in combination with TNFAIP3 inactivation in WM and DLBCL. Our studies demonstrate that co-occurrence of both genetic events has a significant impact on activation of NF-κB and p38. Additionally, we show that loss of A20 leads to elevated secretion of IL-6 and CXCL10, which further drives the activation of JAK/STAT3 pathway. Identification of patients who harbor both of these genetic variants may lead to the development of a genetic biomarker for individualized therapy.
Material and methods
Patients, whole-exome sequencing, and copy number analysis
This study was reviewed and approved by the human subjects review board of Mayo Clinic and the University of Iowa, and written informed consent was obtained from all participants. For DLBCL, identification of MYD88 mutant cases was done using whole exome sequencing (WES) data from 145 newly diagnosed DLBCL tumors. WES data from tumor-normal pairs (n = 56)7,18 and tumors embedded in FFPE (n = 89) were combined and analyzed together as described in Supplemental Methods. TNFAIP3 copy number loss was identified using WES (n = 56) or whole genome copy number data (n = 89) from the OncoScan array (Affymetrix, Santa Clara, CA, USA) and analyzed as described in Supplemental Methods. The cell of origin was determined using the Hans algorithm, gene expression profiling, or NanoString technology19–21. For WM, identification of MYD88 mutant cases has been described previously using WES or allele-specific PCR (ASO-PCR)7 and TNFAIP3 copy number loss was assessed using real-time quantitative PCR. Briefly, genomic DNA was extracted from 29 WM patients and a TaqMan™ copy number assays probe (Thermo Scientific, Waltham, MA) for TNFAIP3 were used. All qPCR reactions were performed using BioRad CXF96 instrument and the results are expressed as relative units based on calculation 2−ΔΔCT, which gives the relative amount of target gene normalized to the endogenous control. A copy number loss was defined using a cutoff based the mean of the normal controls (n = 5) minus 4 standard deviations, a value of 0.8 was defined as the cutoff for TNFAIP3 loss (Supplemental Figure 1).
Cell lines and establishment of TNFAIP3 knockout clones
The MWCL cell line was established and characterized at Mayo Clinic22. The BCWM cell line was a kind gift from Dr. Steve Treon and the HBL-1 cell line was kindly provided by Dr. Thomas Witzig. Cell line authentication is described in Supplemental Methods. All cells lines were maintained in RPMI 1640 medium with 10–20% fetal bovine serum (FBS), penicillin (50 U/ml), and streptomycin (50 µg/ml) were added. Cells were periodically checked for mycoplasma by PCR and were found to be negative. All cell lines were cultivated at 37 °C and 5% CO2. Transcription activator-like effector nuclease (TALENs) specific for targeting exon 5 of the TNFAIP3 gene were designed by the Mayo Clinic Genetics and Model Systems Core using the FusX system as previously described23. Exon 5 was targeted because it is present in all reported TNFAIP3 isoforms. Cells were transfected with 10 μg of each TALEN vector arm by using the AMAXA® nucleofection system (Amaxa, Cologne, Germany). To track successful transfection, cells were co-transfected with a 2 μg GFP expressing plasmid. After 48 h, cells that have incorporated the GFP expression plasmids were isolated by single cell sorting at the Mayo Flow Cytometry Facility. Restriction enzyme digest was used to initially identify clones that carried the frameshift mutation.
Quantitative real-time PCR and RNA-Seq
Total RNA was extracted using the RNeasy Mini Plus Kit (Qiagen GmbH, Hilden, Germany) according to the manufacturer’s protocol. cDNA was synthesized using the SuperScript III First-Strand Synthesis kit (Invitrogen, Waltham, MA, USA). Quantitative reverse transcriptase-PCR was performed using either TaqMan probes (Applied Biosystems, Invitrogen, Carlsbad, CA) or probe-based predesigned qPCR primers (IDT, Coralville, IA, USA). All qPCR reactions were performed using BioRad CXF96 instrument. The results are expressed as relative units based on calculation 2−ΔΔCT, which gives the relative amount of target gene normalized to the endogenous control. For RNAseq, total RNA was extracted using the miRNeasy Mini Plus Kit (Qiagen GmbH, Hilden, Germany). Library preparation and RNA-sequencing were carried out by the Mayo Clinic Genome Analysis Core. Library preparation was done using the Standard TruSeq v2 for mRNA (Illumina, San Diego, CA, USA) and sequencing was carried out on Illumina HiSeq 4000 (Illumina, San Diego, CA, USA). Data analysis was performed by the Mayo Clinic Bioinformatics Core using the Mayo Clinic mRNA-Seq analysis pipeline MAPRSeq (v2.1.1.). A detailed description of the secondary analysis can be found in Supplemental Methods.
Western blot analysis
Cells were lysed in RIPA buffer (Thermo Scientific, Waltham, MA, USA) with protease and phosphatase inhibitor cocktail (Thermo Scientific, Waltham, MA). Protein extracts were clarified by centrifugation, resolved by SDS-PAGE using PROTEAN® TGX™ gels (Bio-Rad Laboratories, Hercules, CA), and transferred to PVDF membranes. Antibodies used in the study are listed in Supplemental Methods.
Cytokine expression analysis
Cells where cultured for 48 h under normal culturing conditions and samples were analyzed using the Human ProcartaPlex™ Simplex Kit for IL-6 and CXCL10 (Invitrogen, Waltham, MA, USA). Samples were run in duplicate and the assay was performed according the manufacturer’s instructions. Plates were read on a Luminex-200 system (Luminex, Austin, TX, USA) and analyzed using Star Station software (Applied Cytometry, Sheffield, UK).
Proliferation assay
Proliferation assay methods have been described previously7. Briefly, cell lines were plated (10 or 25 × 103 cells/well) in culture media in the presence of either DMSO (Thermo Scientific, Waltham, MA, USA) or ibrutinib (Chemitek, Indianapolis, IN, USA) at the indicated doses for 48 h. After 20 h of incubation, cells were pulsed with 0.05 mCi tritiated thymidine (Amersham, Piscataway, NJ, USA) and 3H-thymidine incorporation levels were determined using a MicroBeta TriLux (PerkinElmer, Waltham, MA, USA). All raw counts were normalized to the DMSO control by setting DMSO control to 100.
Statistics
Statistical analyses were performed using GraphPad Prism 7.0 (GraphPad Software, USA). p-Values for all experiments have either been calculated using the 2-tailed Student t-test, or if applicable, the Wilcoxon–Mann–Whitney test was used. Fisher’s exact test was used to compare the correlation between genomic events. p-Value of ≤0.05 was considered to be statistically significant. All error bars are shown as standard deviation (SD).
Results
MYD88 and TNFAIP3 genetic alterations in DLBCL and WM
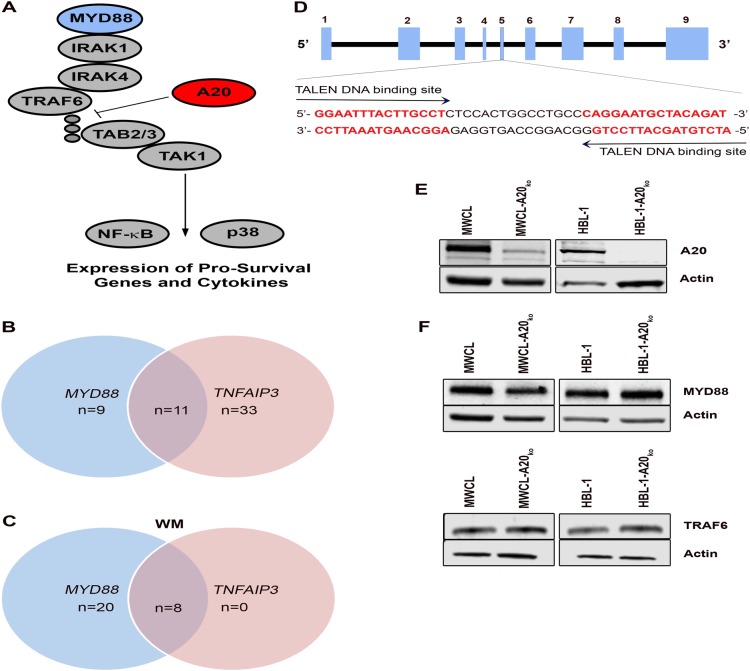
Deubiquitinating enzymes such as A20 counteract E3-ligase activity, inhibit TRAF6 activity, and negatively regulate MYD88-driven TAK1, NF-κB, and p38 activation (Fig. 1a)12,24. To better understand the impact of TNFAIP3 loss on MYD88L265P in DLBCL and WM, we first wanted to determine the frequency of MYD88 mutations in combination with TNFAIP3 genetic alterations. Using genetic data from 145 cases of DLBCL, we found that 20 (13%) of the cases carried a MYD88 mutation. 70% were ABC/non-GCB (nGCB)-DLBCL, 15% germinal center B cell DLBCL (GCB), and 15% unknown. Eleven of the 20 (55%) MYD88 mutant DLBCL cases had a TNFAIP3 loss (Fig. 1b). Taking a closer look at those cases, 73% had a MYD88L265P mutation (ABC/nGCB-DLBCL, n = 5; GCB-DLBCL, n = 1; and unknown, n = 2) followed by 18% with MYD88S243N (ABC/nGCB-DLBCL, n = 1 and GCB-DLBCL, n = 1), and 9% with MYD88M233T (ABC/nGCB-DLBCL, n = 1). TNFAIP3 loss was the most frequent (55%) copy number loss in our cohort of MYD88 mutant cases (Supplemental Figure 2A). Other frequent losses in our MYD88 mutant cases where CDKN2A (50%), ARID1B (45%), ZNF292 (45%), and PRDM1 (45%). Other genetic events that frequently occurred in combination with MYD88 mutations included copy number gains of BCL2 and KLHL14 (45%) and mutations in KMT2D and CD79B (40%) (Supplemental Figure 2B and C). For our analysis of WM, we used genetic data from 29 cases and found that 97% (n = 28) carried a MYD88 mutation. Of those, 28% (n = 8) had a TNFAIP3 loss (Fig. 1c). The high incidence of TNFAIP3 loss combined with MYD88 mutations suggests a relationship between these genetic events. Statistical analyses of our data suggest that TNFAIP3 loss and MYD88 mutations are positively correlated in DLBCL (p = 0.017), but not WM (p = 1.0) WM, although our sample size was small. We were able to validate our findings in DLBCL using available data from the Chapuy et al.25 study which reported 6q or 6q23.3 loss and MYD88 mutation in n = 304 patients (p < 0.0001). Together these data suggest that TNFAIP3 loss is one of the most frequent genetic alterations in MYD88 mutant DLBCL and WM.
Fig. 1. Frequency of MYD88 mutations in combination with TNFAIP3 genetic alterations in DLBCL and WM patients.
a Schematic representation of the MYD88 signaling pathway. b Venn diagram of MYD88 mutant and overlapping TNFAIP3 loss in DLBCL patients. DLBCL MYD88 mutation status was assessed by whole exome sequencing (WES) and TNFAIP3 loss was determined by WES (n = 56) and OncoScan (n = 89) data. c Venn diagram of MYD88 mutant and overlapping TNFAIP3 loss in WM patients. MYD88 status in WM patients was done by Sanger sequencing and TNFAIP3 status was detected by gene copy number analysis. d Schematic representation of the genomic structure of the TNFAIP3 gene. Exons are indicated by light blue boxes. TALENs were designed to target sequences in exon 5 and sequences of TALENs binding sites are highlighted in bold red. e Western blot analysis showed a reduction of TNFAIP3 (A20) in the newly generated cell lines, compared to their wild type counterpart. β-Actin was used as a loading control (n = 3). f Western blot analysis of MYD88 and TRAF6 in MWCL and HBL-1 A20 knock out cell lines and their wild type counterpart. β-Actin was used as a loading control (n = 3)
To further understand the cellular consequence of MYD88L265P in combination with TNFAIP3 loss in human models of WM and DLBCL, we used TALENs genome editing technology to genetically modify the WM cell line MWCL and the ABC-DLBCL cell line HBL-1, both of which harbor a MYD88L265P mutation, but have a wild type TNFAIP3. To introduce a TNFAIP3 loss in those cell lines, we designed a unique pair of TALENs to target exon 5 of the TNFAIP3 gene to induce a double strand break resulting in a base pair deletions in exon 5 (Fig. 1d). TALENs and a GFP co-expressing plasmid were transfected into the cell lines and GFP positive cells were single cell sorted, expanded, and screened for A20 loss by western blot (Fig. 1e). Western blot analysis showed 80% reduction of A20 in the WM cells and a nearly complete loss of A20 in the DLBCL cells, hereafter referred to as MWCL-A20ko and HBL-1-A20ko, compared to their wild type counterpart. To ensure that A20 knockdown did not impact the expression of key MYD88 signaling molecules, we measured the expression of MYD88 and TRAF6 in each of the cell lines. We did not detect any changes in MYD88 or TRAF6 expression suggesting that the MYD88 signaling pathway is fully intact in MWCL-A20ko and HBL-1-A20ko cells (Fig. 1f) ensuring that signaling defects are specific for A20 loss.
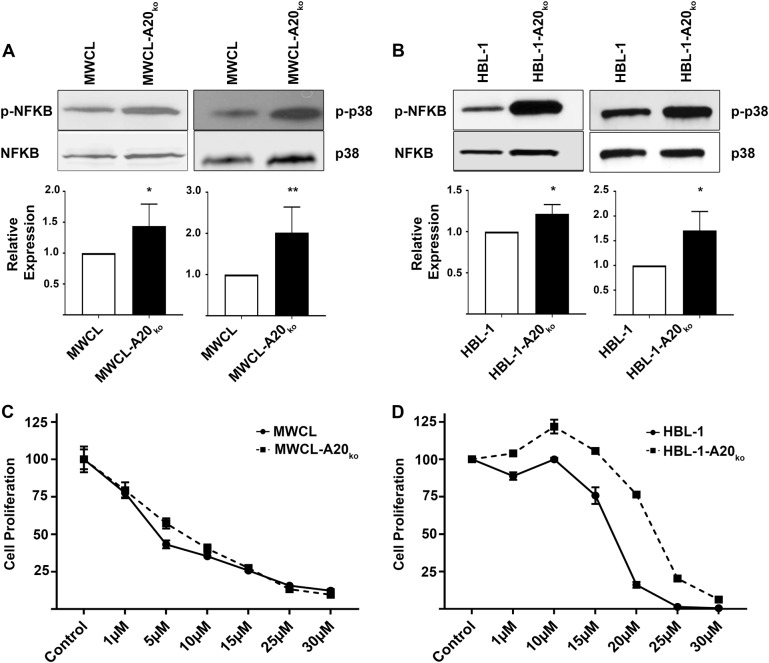
Loss of A20 enhances MYD88L265P -driven signaling and contributes to ibrutinib resistance
To explore the possibility that loss of A20 activates MYD88L265P-driven signaling, we measured the impact of TNFAIP3 deletion on activation of p38 and NF-κB in the MWCL-A20ko and HBL-1-A20ko cell lines. Western blot analysis revealed significant upregulation of phosphorylated p38 (2.02-fold in MWCL-A20ko, p = 0.006 and 1.71-fold in HBL-1-A20ko, p = 0.03) and NF-κB (1.44-fold in MWCL-A20ko, p = 0.05 and 1.22-fold in HBL-1-A20ko, p = 0.03) when compared to the wild type cell line controls (Fig. 2a, b). Graphical representation of multiple experiments is shown in the lower panel of each figure. These studies suggest that loss of A20 in human models of WM and DLBCL drives and enhanced MYD88L265P-driven signaling.
Fig. 2. Increased baseline NF-κB and p38 phosphorylation in MWCL-A20ko and HBL-1-A20ko cells impacts ibrutinib response.
a Western blot analysis of phosphorylated NF-κB in MWCL (n = 4) and HBL-1 (n = 3) A20 knock out cell lines and their wild type counterpart. Total NF-κB was used as a loading control. b Western blot analysis of phosphorylated p38 in MWCL (n = 5) and HBL-1 (n = 3) A20 knock out cell lines and their wild type counterpart. Total p38 was used as a loading control. Each bar represents the mean values of expression levels ± SD, *p ≤ 0.05, **p ≤ 0.01. c, d MWCL and HBL-1 cell lines were treated with indicated concentrations of ibrutinib or DMSO for 48 h and run in triplicate (n = 3). The representative independent experiment is shown and each point represents the mean normalized counts ± SD
A recent study on DLBCL patients17 suggests that TNFAIP3 inactivation negatively impacts therapeutic responses to ibrutinib, a BTK inhibitor known to inhibit B-cell receptor and NF-κB signaling26,27. Therefore, we next wanted to determine if ibrutinib responses were impacted by the loss of A20 in our cell models. The MWCL-A20ko and HBL-1-A20ko cell lines, along with their respective controls, were treated in a dose-dependent manner with ibrutinib and proliferation was measured after 48 h. We did not detect any significant differences in the response to ibrutinib in the WM cell lines (Fig. 2c, left panel). However, HBL-1-A20ko was significantly (p < 0.05) more resistant to ibrutinib single agent therapy than HBL-1 wild type cell line (Fig. 2d, right panel). This data suggests that DLBCL patients with a MYD88 mutation and an A20 loss are more resistant to ibrutinib single agent therapy.
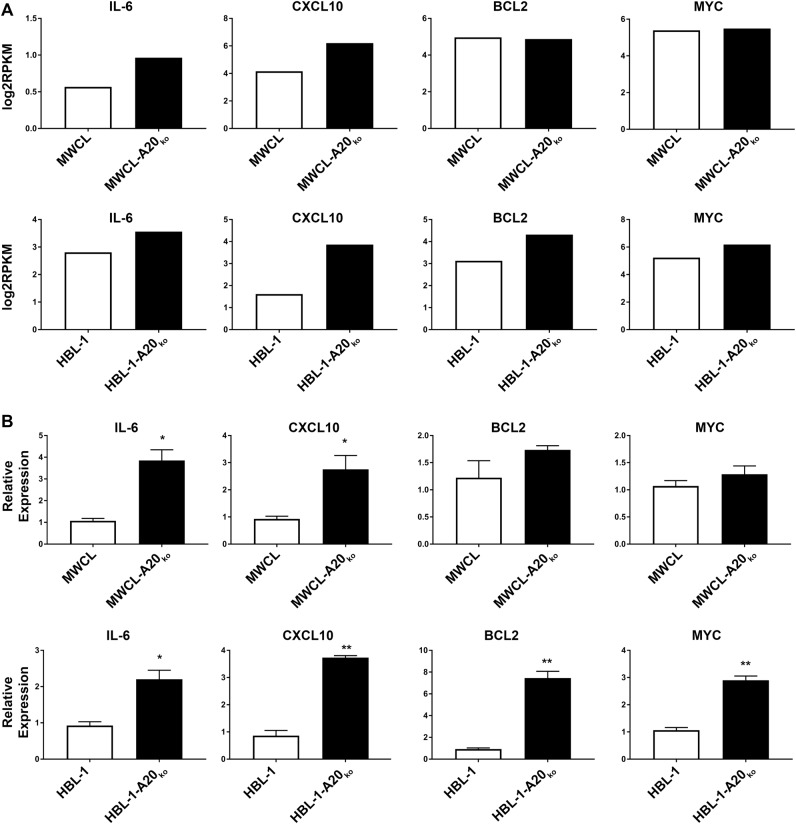
Loss of A20 induces upregulation of NF-κB target genes
To further study the effects of A20 knock out, we performed RNASeq analysis of MWCL-A20ko, HBL-1-A20ko, and their matched control cell lines. The RNASeq data revealed that the NF-κB target genes, IL-6, CXCL10, BCL2, and MYC are upregulated in the A20 knock out cell lines (Fig. 3a). To validate the RNASeq findings, we performed quantitative PCR experiments on the cell lines and saw that IL-6 and CXCL10 were significantly upregulated in both MWCL-A20ko and HBL-1-A20ko compared to cells with intact TNFAIP3 (Fig. 3b). BCL2 and MYC were significantly upregulated in the HBL-1-A20ko cells and showed a slight upregulation in the MWCL-A20ko. This data indicates that TNFAIP3 loss drives upregulation of NF-κB target genes in DLBCL and WM.
Fig. 3. Upregulation of NF-κB Target gene RNA expression in MWCL-A20ko and HBL-1-A20ko cells.
a Log(2) reads per kilobase per million mapped (RPKM) reads from RNASeq reveals up-regulation of the NF-κB target genes in MWCL-A20ko and HBL-1-A20ko cell lines (n = 1). b Bar graph representing fold increase of NF-κB target genes in MWCL-A20ko (IL-6, n = 6; CXCL10, n = 5; BCL2, n = 3; MYC, n = 3) and HBL-1-A20ko (IL-6, n = 5; CXCL10, n = 3; BCL2, n = 3; MYC, n = 3) cell lines determined by qPCR. The representative independent experiment is shown and all qPCR experiments were performed in duplicates. Each bar represents the mean values of expression levels ± SD. *p ≤ 0.05, **p ≤ 0.01
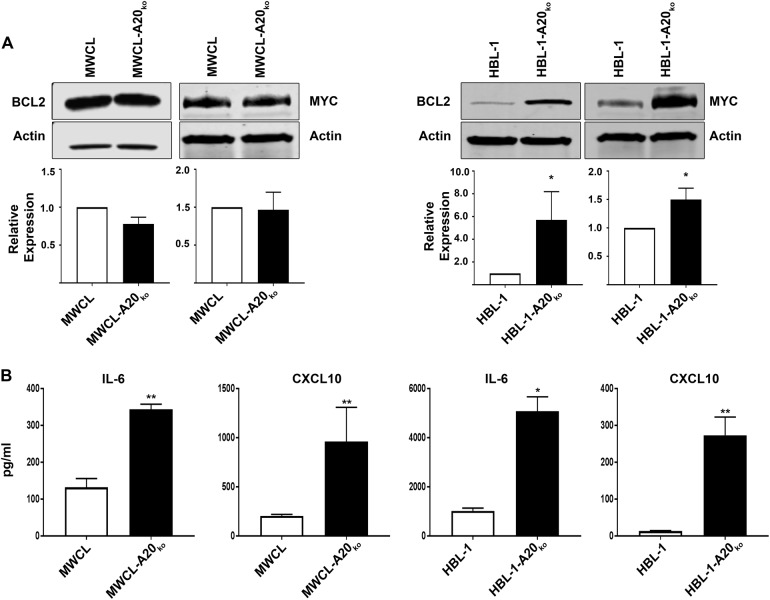
Upregulation of NF-κB target gene protein expression in A20 knock out cells
To further validate RNA expression data, we performed western blot analysis of BCL2 and MYC (Fig. 4a) and confirmed that both are significantly upregulated in the HBL-1-A20ko cell line. Graphical representation of multiple experiments is shown in the lower panel of each figure. There were no changes in the protein levels of BCL2 and MYC in the MWCL-A20ko suggesting that loss of A20 in DLBCL and WM may have different biologic effect in these two forms of NHL. Another possibility that may explain the differences in BCL2 and MYC protein upregulation in our knock out cell lines is the residual A20 protein expression found in the MWCL-A20ko compared to the HBL-1 cells. Therefore, we generated a second WM cell line with A20 loss (BCWM-A20ko) that has a 94% reduction in A20 expression (Supplemental Figure 3A). Again, we did not detect any changes in BCL2 or MYC (p = 0.1104 and p = 0.7624, n = 3) protein expression in the BCWM-A20ko compared to the control cells (Supplement Figure 3B and C). This data further supports the idea that A20 loss has differential effects in WM and DLBCL, which may be expected due to disease heterogeneity.
Fig. 4. Upregulation of NF-κB target gene protein expression in MWCL-A20ko and HBL-1-A20ko cells.
a Western blot analysis of NF-κB target genes BCL2 and MYC in MWCL (BCL2, n = 4; MYC, n = 3) and HBL-1 (BCL2, n = 3; MYC, n = 3) A20 knock out cell lines and their wild type counterpart β-actin was used as a loading control. b Upregulation of IL-6 and CXCL10 secretion in MWCL (n = 3) and HBL-1 (n = 3) A20 knock out cell lines and their wild type counterpart. The representative experiment is shown and cytokine assay was run in duplicates. Each bar represents the mean values of expression levels ± SD. *p ≤ 0.05, **p ≤ 0.01
To assess the expression of IL-6 and CXCL10, we carried out Luminex single plex assays (Fig. 4b). Cells were cultured for 48 h in standard media and supernatants were analyzed. Both IL-6 and CXCL10 were significantly upregulated in the media of MWCL-A20ko and HBL-1-A20ko cell lines compared to their wild type counterpart (Fig. 4b). These data validate our previous findings and indicate that loss of A20 drives expression of BCL2, MYC, IL-6, and CXCL10.
MYD88L265P and TNFAIP3 loss drives the JAK/STAT pathway
MYD88L265P has been shown to drive autocrine expression of cytokines resulting in the activation of the JAK/STAT pathway2,28. Therefore, we next sought to determine if our newly generated A20 knock out cell lines had increased STAT3 activation, a downstream target of IL-6. Western blot analysis of phosphorylated STAT3 levels showed that MWCL-A20ko and HBL-1-A20ko cell lines had significantly higher levels of p-STAT3 (1.47-fold in MWCL-A20ko, p = 0.0176 and 1.46-fold in HBL-1-A20ko, p = 0.0114) (Fig. 5). Graphical representation of multiple experiments is shown in the lower panel. These data suggest that upregulation of IL-6 induced by A20 loss drives activation of the JAK/STAT in WM and DLBCL cells.
Fig. 5. Increased baseline STAT3 phosphorylation in MWCL-A20ko and HBL-1-A20ko cells.
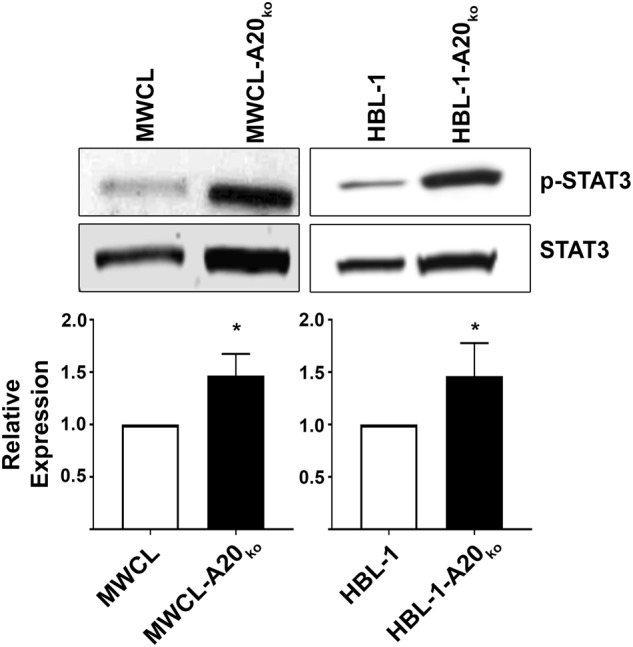
Western blot analysis of phosphorylated STAT3 in MWCL (n = 3) and HBL-1 (n = 5) A20 knock out cell lines and their wild type counterpart. Total STAT3 was used as a loading control. Each bar represents the mean values of expression levels ± SD. *p ≤ 0.05, **p ≤ 0.01
Discussion
In this study, we sought to better define the genetic profile and biologic impact of MYD88 mutations in combination with TNFAIP3 loss in WM and DLBCL. MYD88L265P drives cell proliferation, but it is rapidly shut down by a TNFAIP3 negative feedback loop, suggesting an important relationship between these proteins8. Our data show that a large percentage of DLBCL and WM cases that have a MYD88 mutation also harbor a TNFAIP3 loss, 55% DLBCL and 28%, respectively. These data are supported by previously published work showing that 11–55% of the MYD88 mutant DLBCL have a TNFAIP3 genetic alteration2,29,30 and 35–50% of WM patients harbor a TNFAIP3 loss31,32. The importance of gaining insight of the impact of MYD88 mutations in combination with other genomic events in lymphoma is further supported by recent findings showing a correlation between MYD88 mutation status and poor outcome in DLBCL33. Furthermore, in the study performed by Reddy et al. MYD88 mutations alone are a prognostic factor for the ABC-DLBCL subgroup29. However, additional studies counter these data and suggest a need for additional genetic and clinical analysis to further define the impact by MYD88 mutations in combination with other genetic alterations30,34–36. Two recent large-scale studies shed new insight on how genomic alterations contribute to overall survival in DLBCL patients25,37. Both analyses define novel and genomically unique subgroups of patients with inferior overall survival, MCD37 and C525. Both MCD and C5 share genetic enrichment for MYD88 and CD79B mutations. In the MCD classification, 2.9% of the patients also have a TNFAIP3 loss, where 46% of MYD88 mutant patients in the C5 group either have a 6q or 6q23.3 loss. Between these studies, it is not clear why there is such a large discrepancy in the rate of TNFAIP3 loss in the MYD88 mutant cases, although our study is in line with the 46% described by Chapuy et al. as well as other publications25,30. This variability is most likely due to the use of different copy number analysis platforms as well as tissue samples type (i.e., fresh frozen vs FFPE). Taken together, this data supports the possibility that loss of TNFAIP3 contributes to the MYD88 effect on outcome and future studies should further evaluate the clinical significance.
Using TALEN genome-editing technology, we were able to generate cell lines that allow for functional characterization of causal genetic variants. One benefit to genome editing of cell lines is that it allows for a direct comparison of a specific alteration in the same genetic background. This system also permitted us to design a genetic model in both DLBCL and WM cell lines, allowing for validation of our results across multiple cell lines. Using the MWCL-A20ko and HBL-1-A20ko, we were able to show that loss of TNFAIP3 enhances MYD88L265P-driven NF-κB and p38 signaling resulting in increased expression of NF-κB target genes IL-6 and CXCL10, known NF-κB target genes2,32,38,39, have both been shown to be significantly upregulated in WM and DLBCL, and higher serum levels correlate with an inferior survival38,40–43. Interestingly, in a new T-cell specific A20 knock out model, serum levels of CXCL10 were significantly increased supporting the idea that CXCL10 expression is regulated by A2044. The role of CXCL10 in B cell lymphomas has not been studied well, but it is known that its receptor CXCR3 is expressed on a small subset of B cells45,46. Additionally, we show that TNFAIP3 loss contributes to ibrutinib resistance in an ABC-DLBCL cell line. This data aligns with other studies showing that genetic aberrations contribute to ibrutinib resistance in hematological malignancies47–50. A recent study by Kuo et al. showed that ibrutinib resistance is marked by BCL2 upregulation and that combining ibrutinib with ABT-199, a BCL2 inhibitor, could overcome resistance in DLBCL51. Together, these studies suggest that genetic analysis of tumors may inform therapeutic choices and highlights the potential importance of individualized therapy based on genetic profiles.
IL-6 regulation by A20 has been shown in mouse models where TNFAIP3 was depleted in B cells. Mice lacking A20 had higher mRNA levels and secreted more IL-6 than mice having an intact TNFAIP3 locus after B cell activation52,53. Gene expression analysis of WM patients has shown that IL-6 is one of the most increased expressed genes and A20 is lost in a high percentage of WM patients indicating that A20 controls cytokine production in WM31,40. A previous study identified a subgroup of ABC-DLBCL with a high autocrine IL-6 production driving phosphorylation of STAT3. MYD88 mutations were highly enriched in this subgroup showing that IL-6 production is driven by dysregulated MYD88 signaling2,28. However, our data indicate that this dysregulation can be further driven by TNFAIP3 loss in patients with MYD88 mutations.
The importance of IL-6 and the autocrine mechanism by which IL-6 induces STAT3 activation in DLBCL has been shown in previous studies28,54. STAT3 overexpression is a prognostic marker for overall survival in DLBCL and high STAT3 and phosphorylated STAT3 in the nucleus correlates with inferior survival on those patients55,56. Furthermore, it has been shown that STAT3 upregulation contributes to IgM secretion in WM, which can cause severe complication in WM patients57,58. A recent study demonstrated how STAT3 acts as an activator of several oncogenic pathways as well as a suppressor for apoptosis59. Additionally, it has been shown that MYC and BCL2 overexpression significantly correlates with high phosphorylation of STAT3 in DLBCL60. Our data support these findings and extend to our mechanistic understanding of how MYD88 and A20 signaling can contribute to IL-6 secretion, STAT3 activation, and expression of pro-survival genes.
BCL2 and MYC are both well-studied oncogenes and are targets of recurrent chromosomal breakpoints in lymphomas61,62. If both MYC and BCL2 undergo rearrangement at the same time, they are referred to as double hit lymphoma, and often fall into the GCB-DLBCL subgroup63–66. However, there is also another subclass which is referred to as double expressers, where MYC and BCL2 are overexpressed independent of genetic rearrangement, and often fall into the ABC-DLBCL subgroup67. A recent study showed that BCL2 and MYC expression is significantly associated with MYD88 mutations in the ABC-DLBCL subgroup, however this study only looked at the MYD88 mutation status and no other genetic alterations in combination to BCL2 and MYC status30. Our data indicate that TNFAIP3 loss together with MYD88L265P drives upregulation of anti-apoptotic and cell survival signaling in DLBCL. It would be interesting to see if double expressing ABC-DLBCL also harbor a MYD88 mutation or TNFAIP3 loss or both together since our data indicate that both genetic aberrations contribute to BCL2 and MYC expression in ABC-DLBCL. On the other hand, recent studies have shown that expression levels of the BCL2 family in WM patients is almost the same as in healthy controls and that WM cell lines treated with ABT-737, a BCL2 inhibitor, lack sensitivity68,69. Together, this data supports the idea that the biological pathways activated by MYD88 and TNFAIP3 loss in WM and DLBCL are unique. In summary, we have established a new WM and DLBCL cell line model that mimics the effect of the MYD88L265P mutation in combination with a loss of the TNFAIP3 gene and A20 expression. We show that loss of TNFAIP3 results in a higher baseline phosphorylation of NF-κB, p38, and STAT3. Additionally, loss of TNFAIP3 impacts expression of IL-6 and CXCL10. Overall, results from this study contribute to our understanding of MYD88-driven lymphomas, suggests a possible clinical implication for those individuals that harbor both a MYD88 mutation and a loss of TNFAIP3, and also provides us with a useful model to study novel therapeutic strategies in patients who harbor these genetic variants.
Electronic supplementary material
Acknowledgements
This work was supported in part by the National Institutes of Health (P50 CA097274 to J.R.C. and A.J.N.; CA212162 to A.J.N. and J.R.C.), and the Predolin Foundation (to A.J.N.). We would like to thank the Mayo Clinic Center For Individualized Medicine for their support of the Bioinformatics Program and Biomarker Discovery Program. We would also like to thank the Mayo Clinic Center for Cell Signaling in Gastroenterology for helping to design the TALEN construct.
Author contributions
K.W., J.R.C., and A.J.N. designed, analyzed and interpreted the data, and drafted the paper. K.W., M.M., S.V., Y.A., P.T.G., H.R.S., and M.J.M. performed experiments, analyzed data, and edited the manuscript. E.B., S.L.S., T.E.W., and S.M.A. collected data, provided patient specimens, and edited the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary Information accompanies this paper at (10.1038/s41408-018-0130-3).
References
- 1.Forbes SA, et al. COSMIC: somatic cancer genetics at high-resolution. Nucleic Acids Res. 2017;45(D1):D777–D783. doi: 10.1093/nar/gkw1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ngo VN, et al. Oncogenically active MYD88 mutations in human lymphoma. Nature. 2011;470:115–119. doi: 10.1038/nature09671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Treon SP, et al. MYD88 L265P somatic mutation in Waldenstrom’s macroglobulinemia. N. Engl. J. Med. 2012;367:826–833. doi: 10.1056/NEJMoa1200710. [DOI] [PubMed] [Google Scholar]
- 4.Braggio E, et al. Genome-wide analysis uncovers novel recurrent alterations in primary central nervous system lymphomas. Clin. Cancer Res. 2015;21:3986–3994. doi: 10.1158/1078-0432.CCR-14-2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salcedo R, Cataisson C, Hasan U, Yuspa SH, Trinchieri G. MyD88 and its divergent toll in carcinogenesis. Trends Immunol. 2013;34:379–389. doi: 10.1016/j.it.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Landgren O, Tageja N. MYD88 and beyond: novel opportunities for diagnosis, prognosis and treatment in Waldenstrom’s macroglobulinemia. Leukemia. 2014;28:1799–1803. doi: 10.1038/leu.2014.88. [DOI] [PubMed] [Google Scholar]
- 7.Ansell SM, et al. Activation of TAK1 by MYD88 L265P drives malignant B-cell growth in non-Hodgkin lymphoma. Blood Cancer J. 2014;4:e183. doi: 10.1038/bcj.2014.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang JQ, Jeelall YS, Beutler B, Horikawa K, Goodnow CC. Consequences of the recurrent MYD88(L265P) somatic mutation for B cell tolerance. J. Exp. Med. 2014;211:413–426. doi: 10.1084/jem.20131424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Knittel G, et al. B-cell-specific conditional expression of Myd88p.L252P leads to the development of diffuse large B-cell lymphoma in mice. Blood. 2016;127:2732–2741. doi: 10.1182/blood-2015-11-684183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Compagno M, et al. Mutations of multiple genes cause deregulation of NF-kappaB in diffuse large B-cell lymphoma. Nature. 2009;459:717–721. doi: 10.1038/nature07968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Braggio E, et al. Identification of copy-number abnormalities and inactivating mutations in two negative regulators of NF-kB signaling pathways in Waldenström’s macroglobulinemia. Cancer Res. 2009;69:3579–3588. doi: 10.1158/0008-5472.CAN-08-3701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ma A, Malynn BA. A20: linking a complex regulator of ubiquitylation to immunity and human disease. Nat. Rev. Immunol. 2012;12:774–785. doi: 10.1038/nri3313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kato M, et al. Frequent inactivation of A20 in B-cell lymphomas. Nature. 2009;459:712–716. doi: 10.1038/nature07969. [DOI] [PubMed] [Google Scholar]
- 14.Schmitz R, et al. TNFAIP3 (A20) is a tumor suppressor gene in Hodgkin lymphoma and primary mediastinal B cell lymphoma. J. Exp. Med. 2009;206:981–989. doi: 10.1084/jem.20090528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kelly PN, et al. Selective interleukin-1 receptor–associated kinase 4 inhibitors for the treatment of autoimmune disorders and lymphoid malignancy. J. Exp. Med. 2015;212:2189. doi: 10.1084/jem.20151074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Booher RN, Samson ME, Xu GX, Cheng H, Tuck DP. Abstract 1168: Efficacy of the IRAK4 inhibitor CA-4948 in patient-derived xenograft models of diffuse large B cell lymphoma. Cancer Res. 2017;77(13 Supplement):1168. doi: 10.1158/1538-7445.AM2017-1168. [DOI] [Google Scholar]
- 17.Wilson WH, et al. Targeting B cell receptor signaling with ibrutinib in diffuse large B cell lymphoma. Nat. Med. 2015;21:922–926. doi: 10.1038/nm.3884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lohr JG, et al. Discovery and prioritization of somatic mutations in diffuse large B-cell lymphoma (DLBCL) by whole-exome sequencing. Proc. Natl Acad. Sci. USA. 2012;109:3879–3884. doi: 10.1073/pnas.1121343109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hans CP, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004;103:275–282. doi: 10.1182/blood-2003-05-1545. [DOI] [PubMed] [Google Scholar]
- 20.Wright G, et al. A gene expression-based method to diagnose clinically distinct subgroups of diffuse large B cell lymphoma. Proc. Natl Acad. Sci. USA. 2003;100:9991–9996. doi: 10.1073/pnas.1732008100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scott DW, et al. Determining cell-of-origin subtypes of diffuse large B-cell lymphoma using gene expression in formalin-fixed paraffin-embedded tissue. Blood. 2014;123:1214–1217. doi: 10.1182/blood-2013-11-536433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hodge LS, et al. Establishment and characterization of a novel Waldenstrom macroglobulinemia cell line, MWCL-1. Blood. 2011;117:e190–e197. doi: 10.1182/blood-2010-12-326868. [DOI] [PubMed] [Google Scholar]
- 23.Ma AC, et al. FusX: a rapid one-step transcription activator-like effector assembly system for genome science. Hum. Gene Ther. 2016;27:451–463. doi: 10.1089/hum.2015.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vereecke L, Beyaert R, van Loo G. The ubiquitin-editing enzyme A20 (TNFAIP3) is a central regulator of immunopathology. Trends Immunol. 2009;30:383–391. doi: 10.1016/j.it.2009.05.007. [DOI] [PubMed] [Google Scholar]
- 25.Chapuy B, et al. Molecular subtypes of diffuse large B cell lymphoma are associated with distinct pathogenic mechanisms and outcomes. Nat. Med. 2018;24:679–690. doi: 10.1038/s41591-018-0016-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Herman SE, et al. Ibrutinib inhibits BCR and NF-kappaB signaling and reduces tumor proliferation in tissue-resident cells of patients with CLL. Blood. 2014;123:3286–3295. doi: 10.1182/blood-2014-02-548610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rushworth SA, et al. BTK inhibitor ibrutinib is cytotoxic to myeloma and potently enhances bortezomib and lenalidomide activities through NF-κB. Cell Signal. 2013;25:106–112. doi: 10.1016/j.cellsig.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 28.Lam LT, et al. Cooperative signaling through the signal transducer and activator of transcription 3 and nuclear factor-κB pathways in subtypes of diffuse large B-cell lymphoma. Blood. 2008;111:3701–3713. doi: 10.1182/blood-2007-09-111948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reddy A, et al. Genetic and functional drivers of diffuse large B cell lymphoma. Cell. 2017;171:481–494. doi: 10.1016/j.cell.2017.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dubois S, et al. Biological and clinical relevance of associated genomic alterations in MYD88 L265P and non-L265P-mutated diffuse large B-cell lymphoma: analysis of 361 cases. Clin. Cancer Res. 2017;23:2232. doi: 10.1158/1078-0432.CCR-16-1922. [DOI] [PubMed] [Google Scholar]
- 31.Hunter ZR, et al. The genomic landscape of Waldenström macroglobulinemia is characterized by highly recurring MYD88 and WHIM-like CXCR4 mutations, and small somatic deletions associated with B-cell lymphomagenesis. Blood. 2014;123:1637–1646. doi: 10.1182/blood-2013-09-525808. [DOI] [PubMed] [Google Scholar]
- 32.Poulain S, et al. MYD88 L265P mutation in Waldenstrom macroglobulinemia. Blood. 2013;121:4504–4511. doi: 10.1182/blood-2012-06-436329. [DOI] [PubMed] [Google Scholar]
- 33.Fernandez-Rodriguez C, et al. MYD88 (L265P) mutation is an independent prognostic factor for outcome in patients with diffuse large B-cell lymphoma. Leukemia. 2014;28:2104–2106. doi: 10.1038/leu.2014.184. [DOI] [PubMed] [Google Scholar]
- 34.Treon SP, et al. Somatic mutations in MYD88 and CXCR4 are determinants of clinical presentation and overall survival in Waldenstrom macroglobulinemia. Blood. 2014;123:2791–2796. doi: 10.1182/blood-2014-01-550905. [DOI] [PubMed] [Google Scholar]
- 35.Abeykoon JP, et al. MYD88 mutation status does not impact overall survival in Waldenstrom macroglobulinemia. Am. J. Hematol. 2018;93:187–194. doi: 10.1002/ajh.24955. [DOI] [PubMed] [Google Scholar]
- 36.Yu S, et al. High frequency and prognostic value of MYD88 L265P mutation in diffuse large B-cell lymphoma with R-CHOP treatment. Oncol. Lett. 2018;15:1707–1715. doi: 10.3892/ol.2017.7472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schmitz R, et al. Genetics and pathogenesis of diffuse large B-cell lymphoma. N. Engl. J. Med. 2018;378:1396–1407. doi: 10.1056/NEJMoa1801445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yang G, et al. HCK is a survival determinant transactivated by mutated MYD88, and a direct target of ibrutinib. Blood. 2016;127:3237–3252. doi: 10.1182/blood-2016-01-695098. [DOI] [PubMed] [Google Scholar]
- 39.Harris DP, Bandyopadhyay S, Maxwell TJ, Willard B, DiCorleto PE. Tumor necrosis factor (TNF)-alpha induction of CXCL10 in endothelial cells requires protein arginine methyltransferase 5 (PRMT5)-mediated nuclear factor (NF)-kappaB p65 methylation. J. Biol. Chem. 2014;289:15328–15339. doi: 10.1074/jbc.M114.547349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chng WJ, et al. Gene-expression profiling of Waldenstrom macroglobulinemia reveals a phenotype more similar to chronic lymphocytic leukemia than multiple myeloma. Blood. 2006;108:2755–2763. doi: 10.1182/blood-2006-02-005488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Elsawa SF, et al. Comprehensive analysis of tumor microenvironment cytokines in Waldenstrom macroglobulinemia identifies CCL5 as a novel modulator of IL-6 activity. Blood. 2011;118:5540–5549. doi: 10.1182/blood-2011-04-351742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ansell SM, et al. Elevated pretreatment serum levels of interferon-inducible protein-10 (CXCL10) predict disease relapse and prognosis in diffuse large B-cell lymphoma patients. Am. J. Hematol. 2012;87:865–869. doi: 10.1002/ajh.23259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nacinovic-Duletic A, Stifter S, Dvornik S, Skunca Z, Jonjic N. Correlation of serum IL-6, IL-8 and IL-10 levels with clinicopathological features and prognosis in patients with diffuse large B-cell lymphoma. Int. J. Lab. Hematol. 2008;30:230–239. doi: 10.1111/j.1751-553X.2007.00951.x. [DOI] [PubMed] [Google Scholar]
- 44.Giordano M, et al. The tumor necrosis factor alpha-induced protein 3 (TNFAIP3, A20) imposes a brake on antitumor activity of CD8 T cells. Proc. Natl Acad. Sci. USA. 2014;111:11115–11120. doi: 10.1073/pnas.1406259111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jones D, Benjamin RJ, Shahsafaei A, Dorfman DM. The chemokine receptor CXCR3 is expressed in a subset of B-cell lymphomas and is a marker of B-cell chronic lymphocytic leukemia. Blood. 2000;95:627–632. [PubMed] [Google Scholar]
- 46.Nanki T, et al. Chemokine receptor expression and functional effects of chemokines on B cells: implication in the pathogenesis of rheumatoid arthritis. Arthritis Res. Ther. 2009;11:R149. doi: 10.1186/ar2823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Woyach JA, et al. Resistance mechanisms for the Bruton’s tyrosine kinase inhibitor ibrutinib. N. Engl. J. Med. 2014;370:2286–2294. doi: 10.1056/NEJMoa1400029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liu TM, et al. Hypermorphic mutation of phospholipase C, γ2 acquired in ibrutinib-resistant CLL confers BTK independency upon B-cell receptor activation. Blood. 2015;126:61. doi: 10.1182/blood-2015-02-626846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Xu L, et al. Acquired mutations associated with ibrutinib resistance in Waldenstrom macroglobulinemia. Blood. 2017;129:2519–2525. doi: 10.1182/blood-2017-01-761726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barretina J, et al. The Cancer Cell Line Encyclopedia enables predictive modelling of anticancer drug sensitivity. Nature. 2012;483:603–307. doi: 10.1038/nature11003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kuo HP, et al. Combination of ibrutinib and ABT-199 in diffuse large B-cell lymphoma and follicular lymphoma. Mol. Cancer Ther. 2017;16:1246–1256. doi: 10.1158/1535-7163.MCT-16-0555. [DOI] [PubMed] [Google Scholar]
- 52.Tavares RM, et al. The ubiquitin modifying enzyme A20 restricts B cell survival and prevents autoimmunity. Immunity. 2010;33:181–191. doi: 10.1016/j.immuni.2010.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chu Y, et al. B cells lacking the tumor suppressor TNFAIP3/A20 display impaired differentiation and hyperactivation and cause inflammation and autoimmunity in aged mice. Blood. 2011;117:2227. doi: 10.1182/blood-2010-09-306019. [DOI] [PubMed] [Google Scholar]
- 54.Ding BB, et al. Constitutively activated STAT3 promotes cell proliferation and survival in the activated B-cell subtype of diffuse large B-cell lymphomas. Blood. 2008;111:1515–1523. doi: 10.1182/blood-2007-04-087734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Huang X, et al. Activation of the STAT3 signaling pathway is associated with poor survival in diffuse large B-cell lymphoma treated with R-CHOP. J. Clin. Oncol. 2013;31:4520–4528. doi: 10.1200/JCO.2012.45.6004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wu ZL, Song YQ, Shi YF, Zhu J. High nuclear expression of STAT3 is associated with unfavorable prognosis in diffuse large B-cell lymphoma. J. Hematol. Oncol. 2011;4:31. doi: 10.1186/1756-8722-4-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hodge LS, et al. IL-21 in the bone marrow microenvironment contributes to IgM secretion and proliferation of malignant cells in Waldenstrom macroglobulinemia. Blood. 2012;120:3774. doi: 10.1182/blood-2012-03-419440. [DOI] [PubMed] [Google Scholar]
- 58.Gertz MA, Fonseca R, Rajkumar SV. Waldenström’s macroglobulinemia. Oncologist. 2000;5:63–67. doi: 10.1634/theoncologist.5-1-63. [DOI] [PubMed] [Google Scholar]
- 59.Lu L, et al. Gene regulation and suppression of type I interferon signaling by STAT3 in diffuse large B cell lymphoma. Proc. Natl Acad. Sci. USA. 2018;115:E498. doi: 10.1073/pnas.1715118115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ok CY, et al. Clinical implications of phosphorylated STAT3 expression in de novo diffuse large B-cell lymphoma. Clin. Cancer Res. 2014;20:5113. doi: 10.1158/1078-0432.CCR-14-0683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yip KW, Reed JC. Bcl-2 family proteins and cancer. Oncogene. 2008;27:6398. doi: 10.1038/onc.2008.307. [DOI] [PubMed] [Google Scholar]
- 62.Dang CV. MYC on the path to cancer. Cell. 2012;149:22–35. doi: 10.1016/j.cell.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Weiss LM, Warnke RA, Sklar J, Cleary ML. Molecular analysis of the t(14;18) chromosomal translocation in malignant lymphomas. N. Engl. J. Med. 1987;317:1185–1189. doi: 10.1056/NEJM198711053171904. [DOI] [PubMed] [Google Scholar]
- 64.Kramer MH, et al. Clinical relevance of BCL2, BCL6, and MYC rearrangements in diffuse large B-cell lymphoma. Blood. 1998;92:3152–3162. [PubMed] [Google Scholar]
- 65.Johnson NA, et al. Lymphomas with concurrent BCL2 and MYC translocations: the critical factors associated with survival. Blood. 2009;114:2273. doi: 10.1182/blood-2009-03-212191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kluin, P. M. B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma and Burkitt lymphoma. WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues. International Agency for Research on Cancer, 69008 Lyon, France, 265–266 (2008).
- 67.Hu S, et al. MYC/BCL2 protein coexpression contributes to the inferior survival of activated B-cell subtype of diffuse large B-cell lymphoma and demonstrates high-risk gene expression signatures: a report from The International DLBCL Rituximab-CHOP Consortium Program. Blood. 2013;121:4021. doi: 10.1182/blood-2012-10-460063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gaudette BT, et al. Low expression of pro-apoptotic Bcl-2 family proteins sets the apoptotic threshold in Waldenström Macroglobulinemia. Oncogene. 2016;35:479–490. doi: 10.1038/onc.2015.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chitta KS, et al. Heterogeneous Bcl-2 family expression In Waldenström Macroglobulinemia determines response to inducers of intrinsic apoptosis. Blood. 2013;122:4287. doi: 10.1182/blood-2013-08-524447. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.