Abstract
Background:
Imaging of the femoral trochlea has been inherently difficult because of its convex anatomy.
Purpose/Hypothesis:
The purpose of this study was to compare the diagnostic utility of a standard axial magnetic resonance imaging (MRI) sequence with an axial-oblique MRI sequence of the knee for the detection of trochlear articular cartilage lesions on a high-field 3-T MRI scanner. We hypothesized that axial-oblique MRI scans of the knee obtained along the true axis of the trochlea would significantly improve the detection of high-grade cartilage lesions.
Study Design:
Cohort study (diagnosis); Level of evidence, 2.
Methods:
Patients who underwent MRI and subsequent surgery for any indication were prospectively enrolled into this study between June 2014 and February 2015. The articular cartilage of the trochlea was evaluated independently by 3 raters on axial and axial-oblique MRI and compared with arthroscopic findings (gold standard). The interrater and intrarater reliability of mild (International Cartilage Repair Society [ICRS] grades 1 or 2) and severe (ICRS grades 3 or 4) lesions on MRI were assessed as well as the sensitivity, specificity, positive predictive value, and negative predictive value.
Results:
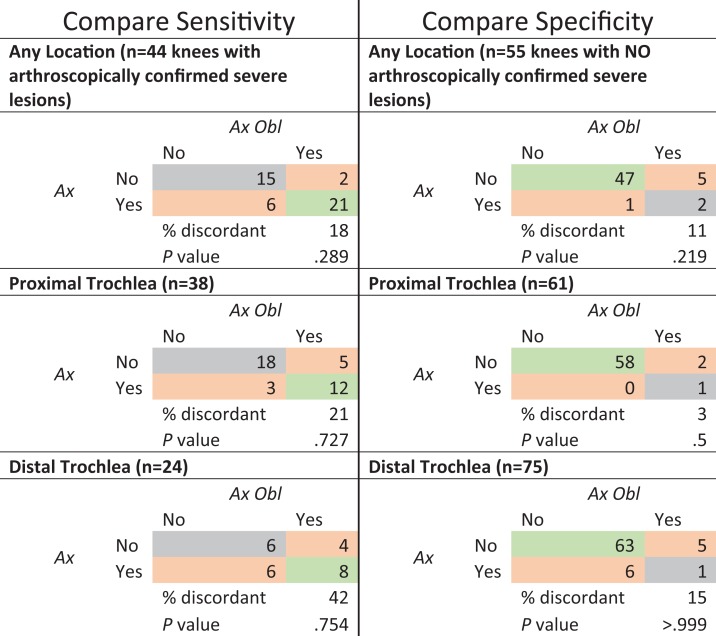
A total of 99 knees in 96 patients were included in the study. Interrater and intrarater agreement for the identification of severe lesions were moderate to good on the proximal trochlea and fair to moderate on the distal trochlea. No significant differences in sensitivity were found between axial and axial-oblique scans for any grade of lesion (55% vs 51%, respectively; P = .700) or for severe lesions (61% vs 52%, respectively; P = .289). Similarly, specificity for detecting severe lesions was not significantly different between axial and axial-oblique scans (95% vs 87%, respectively; P = .219). Last, no significant differences in sensitivity or specificity were found between MRI sequences when separately evaluating proximal and distal trochlear lesions (all P > .05).
Conclusion:
The axial-oblique sequence was unable to improve the sensitivity of MRI in detecting articular cartilage lesions on the trochlea. Both conventional axial and axial-oblique sequences, reviewed independently of the complete MRI series, had low sensitivity in detecting trochlear articular cartilage lesions. For this reason, clinicians should utilize all MRI planes to evaluate the articular cartilage of the trochlea. Future studies should focus on improving MRI techniques for detecting and characterizing cartilage lesions of the trochlea.
Keywords: patellofemoral, trochlea, cartilage, magnetic resonance imaging, MRI, axial, axial-oblique, ICRS
The clinical diagnosis of patellofemoral articular cartilage lesions is notoriously difficult because of the numerous conditions that may cause anterior knee pain. For example, overuse, abnormal patellar tilt, plicae, neuromas, tendinopathy, synovitis, retropatellar fat pad fibrosis, anterior interval scarring, and focal articular cartilage lesions can all present with the same subjective complaint of anterior knee pain.10,11 While articular cartilage defects of the patella can often be clinically diagnosed by translating the patella in the trochlear groove and feeling for crepitation while the knee is positioned in full extension, trochlear defects are harder to detect on a clinical examination because the patella does not translate sufficiently in the trochlear groove once the knee is flexed past approximately 15°. When there is a high degree of clinical suspicion based on symptoms, risk factors, and the physical examination, the presence or absence of an articular cartilage lesion may be visualized either noninvasively using magnetic resonance imaging (MRI) or invasively during arthroscopic surgery.
The awareness and assessment of patellofemoral articular cartilage defects are important because small changes in patellofemoral articular cartilage surfaces have been reported to have a profound activity-limiting effect on normal function.6,7 In addition, patellofemoral osteoarthritis accounts for approximately 65% of patients with symptomatic knee osteoarthritis.5 In spite of its high prevalence, patellofemoral osteoarthritis remains underdiagnosed clinically and on radiographic imaging studies.4,8,9 Crossley and Hinman4 have gone so far as to dub the patellofemoral joint “the forgotten joint in knee osteoarthritis.”
MRI has been proven to be a valuable noninvasive tool for the assessment of defect location, area, and depth, but the gold standard for the diagnosis and characterization of articular cartilage lesions continues to be arthroscopic surgery.12 Even on arthroscopic surgery however, trochlear defects are difficult to detect because of the complex 3-dimensional geometry, difficult surgical accessibility, changing surface congruity, and variable trochlear joint anatomy.12 Without early detection, surgical options for advanced patellofemoral chondral lesions may be limited to partial or total knee arthroplasty rather than biological knee resurfacing techniques. Therefore, utilizing MRI as a noninvasive diagnostic imaging modality to identify and describe chondral defects in the knee is important for the early detection and management of trochlear articular cartilage defects. In particular, high-field 3-T MRI can provide higher spatial resolution and thinner cartilage sections without sacrificing signal-to-noise ratios or increasing the MRI acquisition time. The early detection of these trochlear cartilage defects may be beneficial in delaying or preventing their progression to more advanced articular cartilage defects.
However, MRI of the articular cartilage of the trochlea has been reported to have several limitations. Previous studies3,5,9,12 have suggested that imaging of the trochlear cartilage is significantly more difficult than the patellar cartilage because of comparatively indistinct margins, irregularity of the curved surfaces, and slightly thinner cartilage. In a prospective study comparing MRI with arthroscopic grading for the evaluation of the entire knee joint, lesions of the trochlea demonstrated the lowest sensitivity (63% and 72%) and the lowest specificity (82% and 93%) between 2 raters.14 A meta-analysis by Harris et al12 reported that MRI performed significantly better for the detection of patellar articular cartilage defects compared with trochlear articular cartilage defects across all parameters and that the sensitivity for detecting trochlear cartilage defects was only 72%. The comparatively poor visualization of the distal trochlea may be explained by an axial plane, which does not provide imaging that is directly perpendicular to the cartilaginous surfaces of the trochlea. In light of these shortcomings, new research is needed and proposed to better visualize the trochlear articular cartilage on MRI.
The purpose of this study was to evaluate the ability of an axial-oblique MRI sequence on a high-field 3-T MRI scanner to detect trochlear articular cartilage lesions compared with the historical axial MRI sequence. The findings on MRI were compared with arthroscopic surgery as the gold standard for the verification of trochlear articular cartilage lesions. We hypothesized that axial-oblique MRI scans would better detect articular cartilage lesions in the trochlea because the sections are more perpendicular to the cartilage surface. We also hypothesized that the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) would be improved compared with standard axial MRI scans.
Methods
This study was approved by an institutional review board at Vail Valley Medical Center. A consecutive series of 100 patients between June 2014 and February 2015 who underwent MRI at our institution and had surgery on the same knee for any indication were enrolled in this study. All MRI scans were completed at our institution, and surgery was carried out by a single orthopaedic surgeon (R.F.L.). Patients were excluded if they were younger than 18 years, had a history of claustrophobia with MRI, had metallic implants, had artificial heart valves, had aneurismal clips, or had pacemakers. A total of 4 patients were dropped from the study because of motion artifacts that made reading of the MRI scans unsuitable for diagnostic purposes. A total of 99 knees in 96 patients (50 right knees, 49 left knees) met the criteria for the study. There was a mean time of 18.8 ± 23 days between MRI and surgery.
Imaging Protocol
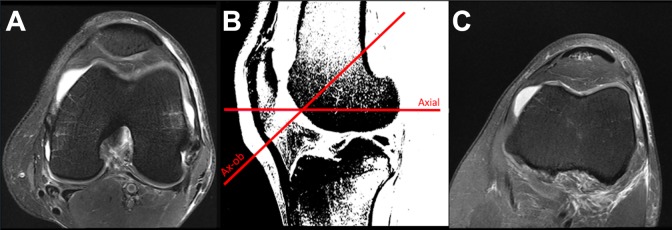
All patients underwent our institution’s standard MRI examination of the knee with the addition of an axial-oblique sequence on a 3-T MRI scanner (Magnetom Verio; Siemens). Cartilage grading was performed using the axial and axial-oblique T2-weighted turbo spin echo sequences with an acquisition time of 2 minutes and 20 seconds. The axial-oblique scan was acquired with slices angled 45° to the long axis of the femur and perpendicular to the midtrochlear articular cartilage surface and followed the same sequence parameters as the standard axial sequence, adding a total of 2 minutes and 20 seconds to the standard acquisition time.
Imaging Analysis
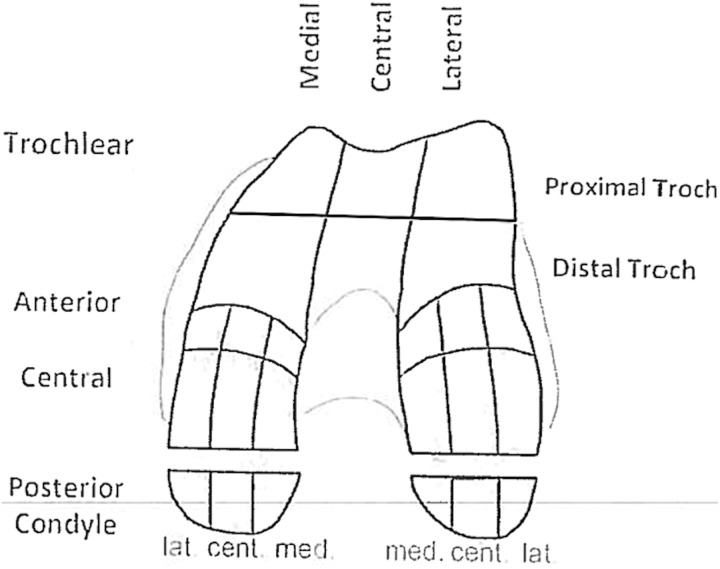
All images were deidentified using custom MATLAB software (MathWorks) and uploaded to OrthoPACS (Merge Healthcare). All measurements were completed on OrthoPACS by a board-certified musculoskeletal radiologist (E.F.-C.) and 2 orthopaedic surgeons (J.J.M., A.G.G.). The intrarater calculations were made utilizing 2 rounds of measurements by the musculoskeletal radiologist. Each rater evaluated the axial and axial-oblique sequences independent of all other images in the study using the International Cartilage Repair Society (ICRS) classification (Figure 1 and Table 1).2 A single static sagittal section was included with each series of images to determine the relative proximal and distal locations of the cartilage defects (Figure 2). The reference sagittal section was selected to demonstrate the central region of the knee and was converted to a black-and-white image with low resolution during the anonymization process to obscure diagnostic cartilage information that could influence the raters’ evaluation of the axial and axial-oblique scans.
Figure 1.
Trochlear zones used for both magnetic resonance imaging and arthroscopic cartilage grading.
TABLE 1.
International Cartilage Repair Society (ICRS) Grading
| Grade | Properties |
|---|---|
| 1 | Superficial lesions, issues, cracks, and indentations |
| 2 | Fraying, lesions extending down to <50% of cartilage depth |
| 3 | Partial loss of cartilage thickness, cartilage defects extending down >50% of cartilage depth as well as down to calcified layer |
| 4 | Complete loss of cartilage thickness |
Figure 2.
Comparison of (A) standard axial versus (C) axial-oblique sequences with reference lines on the sagittal image that was used for evaluations. (B) The reference sagittal image was a single section and was converted to a poor-contrast, low-resolution image to limit potential contributions to the assessment of chondral surfaces.
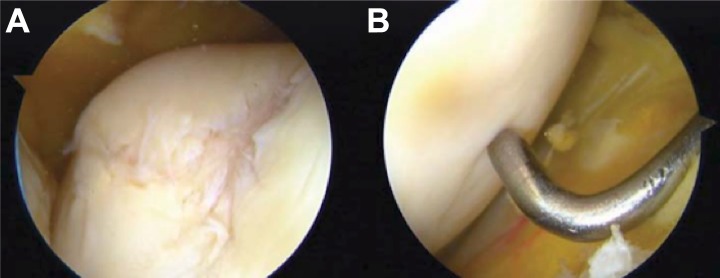
Arthroscopic Grading
Intraoperative grading of the trochlear articular cartilage was performed by a single orthopaedic surgeon in a systematic and methodical fashion by probing the entire trochlear cartilage surface with a calibrated probe during arthroscopic surgery for each patient (Figure 3). The presence of all trochlear articular cartilage defects was recorded based on the system previously outlined by the ICRS.2 Results of the arthroscopic examination of the trochlea were used as the gold standard for comparison of the preoperative axial and axial-oblique MRI scans.
Figure 3.
Arthroscopic images of the trochlear groove of a (A) left and (B) right knee. The left knee demonstrates an International Cartilage Repair Society (ICRS) grade 3 to 4 lesion, while the right knee demonstrates an ICRS grade 1 (softening only) lesion.
Statistical Analysis
Statistical power was considered before data collection and used to guide our required sample size. Assuming the use of the McNemar test for nominal paired data, 30% discordant pairs, and an alpha of .05, 50 participants with arthroscopically confirmed lesions (used to formally compare sensitivity) or 50 participants with arthroscopic confirmation of no lesion (used to compare specificity) were sufficient to detect an odds ratio of 5.4 with 80% statistical power. Twenty-five participants per group were sufficient to detect an odds ratio of 8.5 with 80% statistical power. Because the prevalence and grades of lesions were unknown before patient enrollment, we aimed to enroll 100 patients into this study.
The Fleiss kappa was used to assess interrater and intrarater agreement for the detection of severe (grade 3 or 4) lesions separately within each subregion and for each MRI sequence. Interrater agreement between the 3 raters and intrarater agreement between 2 rounds of a single rater were assessed using grade 3 and 4 lesions because these higher grade lesions were more likely to be treated clinically with an injection or surgery. The predictive accuracy, sensitivity, specificity, PPV, and NPV were reported for comparisons of MRI findings against the gold standard of arthroscopic surgery. Exact binomial tests were used to directly compare the sensitivity and specificity (with respect to arthroscopic surgery) of axial versus axial-oblique MRI. The exact binomial test is the recommended small sample alternative to the McNemar test for paired nominal data. The statistical software R was used for all analyses (R Foundation for Statistical Computing, with additional package psych).15,17
Results
A total of 99 knees in 96 patients met the inclusion criteria and were included in the study (Table 2). A breakdown of lesions observed during arthroscopic grading is included in Table 3. A cartilage lesion was identified in 94 knees, and at least 1 severe lesion was found in 44 knees. The 3 most prevalent locations for severe lesions were the central region of the proximal trochlea, the central region of the distal trochlea, and the medial region of the proximal trochlea.
TABLE 2.
Patient Demographicsa
| No. of Patients | Age, y | Body Mass Index, kg/m2 | |
|---|---|---|---|
| Total | 96 | 45.6 ± 15.7 | 25.1 ± 4.6 |
| Male | 57 | 45.3 ± 15.6 | 25.9 ± 3.6 |
| Female | 39 | 46.2 ± 16.1 | 24.1 ± 5.6 |
aData are shown as mean ± SD unless otherwise indicated. Three patients (all male) were bilateral but only counted once in this table.
TABLE 3.
Trochlear Lesions Assessed During Arthroscopic Surgery in 99 Knees (96 Patients) by Locationa
| Any Lesion | Mild Lesion | Severe Lesion | |
|---|---|---|---|
| Proximal trochlea | |||
| Lateral | 16 | 8 | 8 |
| Central | 81 | 55 | 26 |
| Medial | 37 | 16 | 21 |
| Distal trochlea | |||
| Lateral | 20 | 12 | 8 |
| Central | 79 | 57 | 22 |
| Medial | 22 | 12 | 10 |
| Any location | 94 | 50 | 44 |
aData are shown as No. Mild lesions defined as International Cartilage Repair Society (ICRS) grade 1 or 2. Severe lesions are defined as ICRS grade 3 or 4.
Fleiss kappa values for agreement are included in Table 4. Moderate to good interrater and intrarater agreement were found for the proximal trochlea on both axial and axial-oblique scans (Fleiss kappa = 0.554-0.757). Only fair to moderate agreement was found for the distal trochlea on axial scans, exhibiting lower interrater (Fleiss kappa = 0.223) and intrarater (Fleiss kappa = 0.490) reproducibility than the same measurements on axial-oblique scans.
TABLE 4.
Interrater and Intrarater Agreement Among 3 Raters and 2 Rounds of a Single Rater Using Fleiss Kappaa
| Interrater Kappa | Intrarater Kappa | |
|---|---|---|
| Proximal | ||
| Axial | 0.572 | 0.757 |
| Axial-oblique | 0.554 | 0.713 |
| Distal | ||
| Axial | 0.223 | 0.490 |
| Axial-oblique | 0.394 | 0.579 |
aAgreement based on identifying severe (grade 3 or 4) lesions compared with mild or no lesions (grade 0, 1, or 2).
Accuracy With Respect to Arthroscopic Surgery
Agreement of the MRI-based identification of lesions compared with the gold standard of arthroscopic surgery was explored in 2 ways. First, accuracy measurements were calculated for identifying any cartilage lesion (grades 1-4) and for identifying severe lesions (grade 3 or 4) only. For both axial and axial-oblique sequences, the sensitivity, specificity, and NPV were higher when considering severe lesions only (Table 5). Second, accuracy measurements were calculated for identifying severe cartilage lesions in the proximal and distal trochlear regions separately. Both axial and axial-oblique sequences exhibited higher specificity (90%-98%) than sensitivity (40%-58%) in both the proximal and distal subregions, respectively. A higher PPV than NPV was found in the proximal trochlea (85%-94% vs 72%-73%), while a higher NPV than PPV was found in the distal trochlea (85%-87% vs 67%) (Table 6). Limited numbers of lesions in the lateral, central, and medial subregions precluded more detailed subregional accuracy analysis.
TABLE 5.
Accuracy Measurements of Axial Versus Axial-Oblique 3-T Magnetic Resonance Imaging With Respect to Trochlear Lesion Gradesa
| Sensitivity | Specificity | Positive Predictive Value | Negative Predictive Value | |
|---|---|---|---|---|
| All lesions | ||||
| Axial | 55 | 80 | 98 | 8.7 |
| Axial-oblique | 51 | 60 | 96 | 6.1 |
| Severe lesions | ||||
| Axial | 61 | 95 | 90 | 75 |
| Axial-oblique | 52 | 87 | 77 | 70 |
aData are shown in percentages.
TABLE 6.
Accuracy Measurements of Axial Versus Axial-Oblique 3-T Magnetic Resonance Imaging With Respect to Trochlear Locationa
| Sensitivity | Specificity | Positive Predictive Value | Negative Predictive Value | |
|---|---|---|---|---|
| Proximal trochlea | ||||
| Axial | 40 | 98 | 94 | 72 |
| Axial-oblique | 45 | 95 | 85 | 73 |
| Distal trochlea | ||||
| Axial | 58 | 90 | 67 | 87 |
| Axial-oblique | 52 | 92 | 67 | 85 |
aData are shown in percentages.
Direct Accuracy Comparison of Axial and Axial-Oblique Scans
Contingency tables comparing the sensitivity and specificity between straight axial and axial-oblique sequences are included in Figure 4. No significant difference was found between straight axial and axial-oblique scans with respect to sensitivity (P = .29) or specificity (P = .22) for detecting grade 3 or 4 lesions anywhere on the trochlea. Likewise, no significant differences were found in the sensitivity or specificity when detecting severe lesions on the proximal or distal trochlea separately. The percentage of discordant pairs (disagreement between straight axial and axial-oblique sequences) was lower than the 30% assumed a priori for most scenarios, potentially limiting the statistical power for direct comparisons between images. The only exception was when comparing sensitivity in the distal trochlea, in which discordance was found for 42% of 24 knees with arthroscopically confirmed severe lesions in the distal trochlea. Even in this case, no significant difference in sensitivity was found between axial and axial-oblique scans (P = .754).
Figure 4.
Contingency tables demonstrating sensitivity and specificity comparisons between straight axial (Ax) and axial-oblique (Ax Obl) sequences. Only knees with arthroscopically confirmed severe (grade 3 or 4) lesions are used for sensitivity comparisons, and only knees with an arthroscopically confirmed lack of severe (grade 3 or 4) lesions are used for specificity comparisons. Green cells represent both images agreeing with the arthroscopic assessment, red cells represent only 1 image agreeing with arthroscopic surgery, and gray cells represent both images disagreeing with arthroscopic surgery. P value calculated via the exact binomial test.
Discussion
We found that the axial-oblique sequence did not improve the sensitivity of MRI for detecting articular cartilage lesions of the trochlea, rejecting our hypothesis. We also found that lower grade articular cartilage lesions were more difficult to detect on MRI than higher grade lesions. Overall, in spite of using a high-field 3-T MRI scanner, we did not find strong sensitivity or specificity for either the axial or axial-oblique sequences for the detection of high-grade articular cartilage trochlear lesions. Although this was found to be the case, the inclusion of sagittal imaging may improve diagnostic accuracy and the detection of such lesions moving forward. At this juncture, arthroscopic surgery remains the gold standard for the diagnosis of articular cartilage lesions of the trochlea until further advancements in MRI technology lead to enhanced articular cartilage spatial resolution, optimized slice thickness, and lower signal-to-noise ratios.
There has been a paucity of MRI studies evaluating the presence of trochlear articular cartilage lesions. However, in a systematic review of the use of MRI for the detection of patellofemoral articular cartilage defects, MRI was more sensitive in detecting patellar defects (87%) compared with trochlear cartilage defects (72%).12 This review particularly noted that volume averaging had a larger role on the irregular curved surface of the trochlea, resulting in a larger effective slice thickness and wider interslice gaps, which were theorized to contribute to the lower sensitivity for the detection of trochlear articular cartilage defects.12 It has been theorized that high-field 3-T MRI can increase the accuracy for detecting knee chondral lesions overall.9 However, a comparative study of 1.5-T and 3-T MRI found only a relatively limited role of field strength for evaluating articular cartilage defects in the knee.13 As higher field magnets are developed and utilized, diagnostic accuracy may improve, but the use of such technology is limited at this juncture. In the present study, contrary to our hypothesis, we did not find that the addition of axial-oblique scans improved the ability to detect trochlear articular cartilage defects. It was thought that by creating an imaging sequence in a perpendicular axis to the trochlea, lesions would be more readily visualized. However, it is possible that given the curved nature of this portion of the distal femur, the entirety of the sequence is not perpendicular to the trochlea and thus does not definitively capture all regions in which lesions may exist.
Improving the ability to define localized high-grade articular cartilage lesions of the trochlea is important. The trochlear groove acts to help guide the patella through increasing knee flexion. As the knee becomes increasingly flexed, the contact area in the patellofemoral joint increases by an average of 24%.1 In addition, activities such as climbing up or down stairs, squatting, lunging, kneeling, or engaging in prolonged flexion place an increased load on the patellofemoral joint. Previous biomechanical studies have estimated these loads at 3.3 times the body weight while climbing stairs, 7.6 times the body weight while squatting, and 20 times the body weight during jumping activities.1,8,16,18 Thus, it is important to be able to diagnose high-grade articular cartilage trochlear lesions, which may still be treatable with articular cartilage resurfacing procedures, before the progression of these lesions in size or potentially to involvement of the patella as well.
The evaluation of patients with a symptomatic patellofemoral joint through noninvasive imaging techniques is vital to properly diagnose, treat, and potentially delay the progression of cartilage degeneration. In this study, approximately 45% of patients evaluated demonstrated lesions within the patellofemoral joint. Despite this high percentage, not all patients with such lesions experience anterior knee pain or patellofemoral symptoms. This suggests that some patients may have subclinical lesions or are able to tolerate small or low-grade lesions. Improved imaging modalities may allow for early diagnosis and counseling for patients who may be at risk with aggressive sports or patellofemoral loading activities. Standard radiographic imaging of the knee (anteroposterior, lateral, and axial at 30° of flexion) is commonly used to evaluate the patellofemoral joint. Previous studies have correlated bony morphology on radiographs with patellofemoral chondral defects such as the congruence angle, quadriceps angle, patellar height, and patellar shape. However, because radiographs are not suitable for direct articular cartilage evaluation, indirect measurements such as joint space measurements are typically employed. Such measurements have limited utility because they may underestimate more localized articular cartilage defects, fissuring, and softening because of the inability to directly visualize cartilage and other surrounding soft tissues.3 The advancement in MRI technology, such as the development and use of T2 mapping and T1-rho techniques, may allow improved evaluation of articular cartilage and other intra-articular structures. Based on the findings in our study, further development of high-field MRI techniques for the evaluation of trochlear defects is required.
Conclusion
The axial-oblique sequence was unable to improve the sensitivity of MRI in detecting articular cartilage lesions on the trochlea. Both conventional axial and axial-oblique sequences, reviewed independently of the complete MRI series, had low sensitivity in detecting trochlear articular cartilage lesions. For this reason, clinicians should utilize all MRI planes to evaluate the articular cartilage of the trochlea. Future studies should focus on improving MRI techniques for detecting and characterizing cartilage lesions of the trochlea.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: R.F.L. is a consultant for and receives royalties from Arthrex, Ossur, and Smith & Nephew. J.J.M. and A.G.G. have received research and educational funding from Arthrex, Smith & Nephew, and DJO. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Vail Valley Medical Center Institutional Review Board.
References
- 1. Besier TF, Draper CE, Gold GE, Beaupré GS, Delp SL. Patellofemoral joint contact area increases with knee flexion and weight-bearing. J Orthop Res. 2005;23(2):345–350. [DOI] [PubMed] [Google Scholar]
- 2. Brittberg M, Winalski C. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;85:58–69. [DOI] [PubMed] [Google Scholar]
- 3. Chaisson CE, Gale DR, Gale E, Kazis L, Skinner K, Felson DT. Detecting radiographic knee osteoarthritis: what combination of views is optimal? Rheumatology (Oxford). 2000;39(11):1218–1221. [DOI] [PubMed] [Google Scholar]
- 4. Crossley KM, Hinman RS. The patellofemoral joint: the forgotten joint in knee osteoarthritis. Osteoarthritis Cartilage. 2011;19(7):765–767. [DOI] [PubMed] [Google Scholar]
- 5. Duncan R, Hay EM, Saklatvala J, Croft PR. Prevalence of radiographic osteoarthritis: it all depends on your point of view. Rheumatology (Oxford). 2006;45(6):757–760. [DOI] [PubMed] [Google Scholar]
- 6. Duncan R, Peat G, Thomas E, Wood L, Hay E, Croft P. Does isolated patellofemoral osteoarthritis matter? Osteoarthritis Cartilage. 2009;17(9):1151–1155. [DOI] [PubMed] [Google Scholar]
- 7. Duncan R, Peat G, Thomas E, Wood L, Hay E, Croft P. How do pain and function vary with compartmental distribution and severity of radiographic knee osteoarthritis? Rheumatology (Oxford). 2008;47(11):1704–1707. [DOI] [PubMed] [Google Scholar]
- 8. Dye SF. The pathophysiology of patellofemoral pain: a tissue homeostasis perspective. Clin Orthop Relat Res. 2005;(436):100–110. [DOI] [PubMed] [Google Scholar]
- 9. Figueroa D, Calvo R, Vaisman A, Carrasco MA, Moraga C, Delgado I. Knee chondral lesions: incidence and correlation between arthroscopic and magnetic resonance findings. Arthroscopy. 2007;23(3):312–315. [DOI] [PubMed] [Google Scholar]
- 10. Grelsamer RP, Dejour D, Gould J. The pathophysiology of patellofemoral arthritis. Orthop Clin North Am. 2008;39(3):269–274. [DOI] [PubMed] [Google Scholar]
- 11. Grelsamer RP, Stein DA. Patellofemoral arthritis. J Bone Joint Surg Am. 2006;88(8):1849–1860. [DOI] [PubMed] [Google Scholar]
- 12. Harris JD, Brophy RH, Jia G, et al. Sensitivity of magnetic resonance imaging for detection of patellofemoral articular cartilage defects. Arthroscopy. 2012;28(11):1728–1737. [DOI] [PubMed] [Google Scholar]
- 13. Kijowski R, Blankenbaker DG, Davis KW, Shinki K, Kaplan LD, De Smet AA. Comparison of 1.5 and 3.0-T MR imaging for evaluating the articular cartilage of the knee joint. Radiology. 2009;250(3):839–848. [DOI] [PubMed] [Google Scholar]
- 14. Li X, Yu C, Wu H, et al. Prospective comparison of 3D FIESTA versus fat-suppressed 3D SPGR MRI in evaluating knee cartilage lesions. Clin Radiol. 2009;64(10):1000–1008. [DOI] [PubMed] [Google Scholar]
- 15. R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing; Available at: https://www.R-project.org/. Accessed February 2, 2018. [Google Scholar]
- 16. Reilly DT, Martens M. Experimental analysis of the quadriceps muscle force and patellofemoral joint reaction force for various activities. Acta Orthop Scand. 1972;43(2):126–137. [DOI] [PubMed] [Google Scholar]
- 17. Revelle W. Psych: procedures for personality and psychological research. Northwestern University; Available at: http://CRAN.R-project.org/package=psychVersion=1.6.6. Accessed February 2, 2018. [Google Scholar]
- 18. Smith AJ. Estimates of muscle and joint force at the knee and ankle during jumping activities. J Hum Movement Stud. 1975;1:78–86. [Google Scholar]