Abstract
Background:
Healthcare workers, especially nurses, are at a high risk of infection. By complying with infection control measures, a lot of infections can be prevented. This study examined the effects of a training program on knowledge, perception, and risk reduction regarding infection control among nurses.
Materials and Methods:
This study adopted a pretest–posttest quasi-experimental design. The samples consisted of 87 participants comprising 42 nurses in the experimental group and 45 nurses in the control group. The instruments used for data collection were a questionnaire on knowledge about infection control and a questionnaire on perception about infection control.
Results:
Findings showed that the mean (SD) age in the experimental group was 34.92 (8.99) whereas that of the control group was 47.43 (6.60). The mean (SD) years of experience in the experimental group was 10.42 (9.95) years whereas in the control group it was 21.89 (8.72) years. Findings further revealed that 26 participants (62.90%) in the postintervention group had high knowledge level compared to the preintervention where none had high knowledge. A significant difference was observed between the mean perception score on infection control in the experimental and control groups (t = 17.12; p = 0.001).
Conclusions:
This study has shown that a training program is very effective and that all nurses should be exposed to infection control training to equip them with the necessary knowledge and skills with which to fight against the spread of infection in the healthcare setting.
Keywords: Health education, infection control, Nigeria, nursing, risk reduction behavior
Introduction
Infection control is an aspect of healthcare delivery that deals with the curtailment of the spread of infection within the healthcare setting. Be it from patient-to-patient, patient-to-staff, staff-to-patients, or staff to staff contact, healthcare workers generally are at risk of infection. The World Health Organization (WHO)[1] reported that among the 35 million health workers worldwide, approximately 3 million sustain percutaneous exposures to blood-borne pathogens each year, including 2 million to hepatitis B virus (HBV), 0.9 million to hepatitis C virus (HCV), and 170,000 to human immunodeficiency virus (HIV). These injuries may result in 70,000 HBV; 15,000 HCV, and 5,000 HIV infections.
Nurses are at a higher risk of being infected with blood-borne pathogens from clinical blood exposure by injuries with sharp instruments and needle-stick injuries if infection control measures are not strictly followed. Studies have also shown evidence of clinical nurses becoming infected due to poor infection control measures.[2] Abdulraheem et al. (2012)[3] in their study among health workers in North Eastern Nigeria found that the level of knowledge and implementation of standard precautions was below standard to guarantee infection safety. They concluded that there is still much to learn and implement when it comes to infection control measures. It has also been reported that healthcare workers do not strictly adhere to the various infection control measures probably because they do not recognize such measures or they lack adequate knowledge or it could be due to poor attitude towards infection control measures including nonavailability of materials and equipment.[4] Amoran and Onwobe[4] found that inadequate workers' knowledge on infection control and environment-related problems is among the crucial issues that need urgent attention. Adly et al.[5] found that intervention influenced the compliance of nurses to infection control measures because of the knowledge gained during the intervention or training program.
Studies have also shown gaps in knowledge and a negative attitude towards infection control among health workers.[6,7] This study, therefore, focuses on the effect of nursing intervention on the knowledge and perception of nurses about infection control in two teaching hospitals in Ogun State, Nigeria. The theoretical framework applied in this study is the Precede Model. The acronym “Precede” stands for predisposing, reinforcing, enabling constructs in educational diagnosis and evaluation. For long, the Precede Model developed by Green et al.[8] has served as a conceptual framework in the formulation of health education plans aimed at diagnosing the health problems of a community, understanding the factors that influence the people's behavior, and developing interventions to promote healthy behavior.
Materials and Methods
This study was conducted from January to June 2017 and adopted a pretest–posttest quasi-experimental design. This design was considered appropriate because the collection of baseline data allowed researchers to be relatively confident inferring that posttest differences occur as a result of the intervention.[9] The population for this study included registered nurses in the two teaching hospitals in southwest Nigeria. Simple random sampling was used to select the experimental group and control group among the two teaching hospitals. The total number of nurses that met the inclusion criteria for the experimental group and control group were 125 and 190 participants, respectively. The sample size was calculated using Kish's formula with Zα = 95%, confidence level = 1.96, and Zβ 80% power = 0.84. The proportionate stratified random sampling technique was subsequently used to select the participants. Thirty-five percent of the nurses in each ward or unit were used for the selection of the experimental group, whereas 24% nurses in each ward or unit were used for selecting the control group. Based on the abovementioned proportion, both the experimental intervention group and the control group had 45 participants each. The experimental and control groups were carefully selected to avoid possibility of contact across group and prevent risk of contamination.
This study made use of self-report questionnaire for data collection. The instrument has a reliability value of 0.92 using Cronbach alpha (R). The instrument consisted of three sections – A, B, and C. Section A elicited responses on demographic variables of participants such as age, gender, marital status, and educational qualification among others. Section B elicited information on the participants' knowledge about standard precautions. The questionnaire elicited responses on hand washing, personal protective equipment (PPE), injection safety, cleaning, disinfection, and waste management. The total number of items was 33. Correct responses were scored as 1. The maximum obtainable score was 33. Scores 0–16 were classified as low knowledge, 17–27 as moderate knowledge, and 28–33 as high knowledge. Section C elicited information on participants' perception about infection control. This section was developed by the researchers. The questionnaire elicited responses on perceived susceptibility, perceived seriousness or threat, perceived benefits, as well as self-efficacy. There were 16 items and the maximum possible score was 64. Scores 0–31 were classified as poor perception, 32–54 as fair perception, and 55–64 as good perception. The questionnaire was pretested on 20 nurses at another teaching hospital in a different state in southwestern Nigeria. The data collected were used to estimate the reliability of the instrument using Cronbach alpha (R) to bring out the internal consistency and establish the validity of the instrument. The Cronbach alpha values for knowledge and perceptions were 0.79 and 0. 80, respectively.
Data were collected in three phases namely – pre-intervention visits, intervention sessions, and evaluation of intervention sessions. Preintervention visits were made in the experimental group and control group. This was to enable the researchers to obtain the number of nurses and the wards/units where they were assigned to. During the pre-intervention visits, the participants were informed about the date of commencement, and the time table for the training program was given to them through the nurse at charge in each ward/unit. The control group was also visited but they were not exposed to any training program. In the intervention sessions, the participants were exposed to four modules. Each module was held once a week and lasted for four consecutive weeks. The researchers met the experimental group as scheduled in the first week. The researchers introduced themselves to the participants; the pretest questionnaire was administered followed by the content of module one which included the importance of infection control, chain of infection, and components of standard precautions. The session lasted for 90 minutes. The method of teaching includes lecture, demonstration, and use of visual aids. In the second week, the participants were exposed to the contents of module two which consisted of hand hygiene, patient care equipment, and preparation of different strengths of JIK (3.5%) hypochlorite solution. The researchers visited the control group. No training was given to the participants. The researchers went to various wards/units to meet the participants. The objectives of the study were communicated to all participants. Interested participants were given the written consent form to complete. This was followed by the administration of the pretest questionnaire and the same were collected on the spot after completion. Participants were also informed that they would complete the posttest questionnaire after 4 weeks.
In the third week, participants were exposed to the contents of module three which consisted of PPE. In the fourth week they were exposed to the contents of module four which consisted of injection safety and health care waste management. They were told to come back after 4 weeks for the posttest which was the same used for the pretest. Evaluation of the intervention program was done 4 weeks post-intervention. All the participants were given the posttest to complete and were retrieved immediately. The researchers also visited the control group in their various wards/units to administer the posttest, and the filled-out questionnaires were collected immediately. Finally, the researchers held a brief meeting with the Director of Nursing Services to express their appreciation for the support. Completed questionnaires were collected, coded, and analyzed using SPSS version 21.0 (SPSS Inc. Chicago IL, USA). Descriptive statistics such as frequency counts, percentages, tables, mean scores, and standard deviation were used to analyze the demographic data of participants and provide answers to the research questions. Inferential statistics of t-test was used to test one hypothesis generated at 0.05 level of significance.
Ethical considerations
Ethical approval for this study was obtained from the institutional ethical committee with approval reference of BUHREC526/16. Participants were duly informed about the objectives of the study and participation was voluntary and all participants were informed of their rights to withdraw from the study at any point if they so desired. All participants signed the consent form and confidentiality of information was assured and upheld.
Results
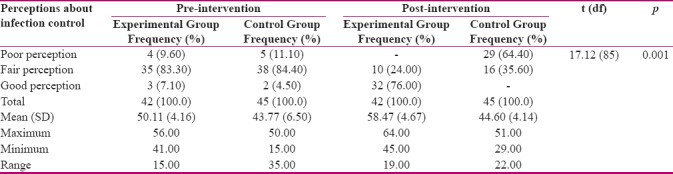
Table 1 shows that the mean (SD) for age in the experimental group was 34.92 (8.99) whereas that of the control group was 47.43 (6.60); regarding gender, there were more females in the control group. The mean (SD) for years of experience in the experimental group was 10.42 (9.95) whereas it was 21.89 (8.71) in the control group. Table 2 shows that in the post-intervention, 26 participants (62.90%) had high knowledge compared to none in the pre-intervention, whereas only 1 participant (2.40%) had low knowledge compared to 22 (52.30%) participants in the pre-intervention. The mean difference was 7.24. This indicates that the training had an effect on participants' knowledge. Table 3 shows that 25 participants (59.50%) have received hepatitis B virus vaccination in the experimental group whereas 12 participants (26.70%) received vaccination in the control group. Twenty-eight participants (66.70%) experienced sharp injury in the experimental group as compared to 20 participants (44.40) in the control group. Table 4 shows that 32 participants (76.20%) have received vaccination of hepatitis B virus in the experimental group while the number for the control group did not change from the baseline after the training program. Posttest results show that participants in the experimental group did not experience sharp injury within the 6 weeks whereas 5 participants (11.20%) in the control group had experience; only 3 participants (6.67%) reported the experience of needle stick injury. This indicates that the training had an effect on infection risk reduction in the experimental group (p = 0.001). The findings listed in table 5 show the descriptive statistics indicating the effects of training on participants' perceptions in the experimental and control groups. The mean pre-intervention perception scores were 50.11 and 43.77 in the intervention and control groups respectively. After the intervention, the mean perception scores were 58.47 and 48.60 in the intervention and control groups respectively. The results in table 5 show that t = 17.12, df = 85, p = 0.001. This indicates that there is a significant difference in the mean perception score of infection control between the experimental and control groups.
Table 1.
Demographic data of participants
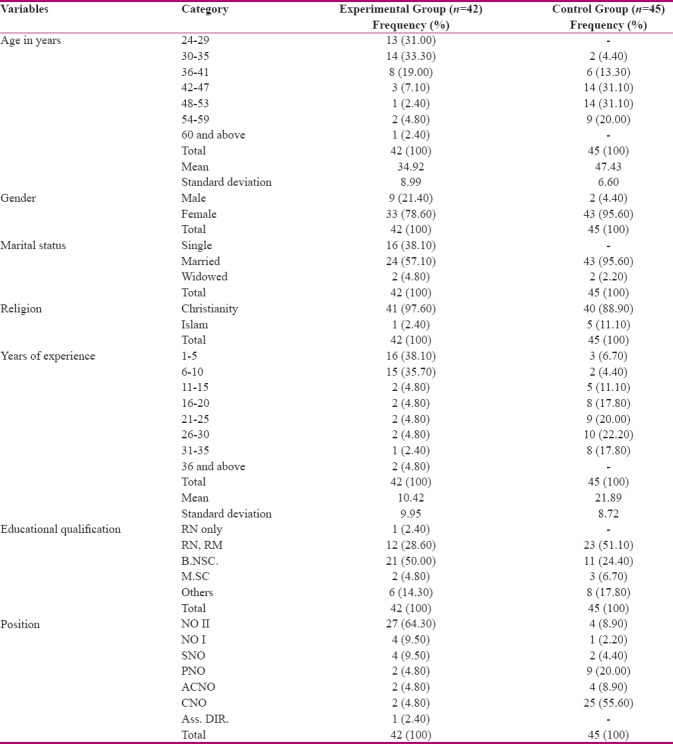
Table 2.
Descriptive statistics showing pre- and post-intervention responses of participants’ knowledge about infection control in the experimental and control group
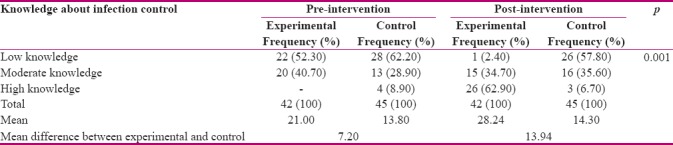
Table 3.
Descriptive statistics showing pre-intervention responses of participants on exposure or injury experience in experimental group and control group
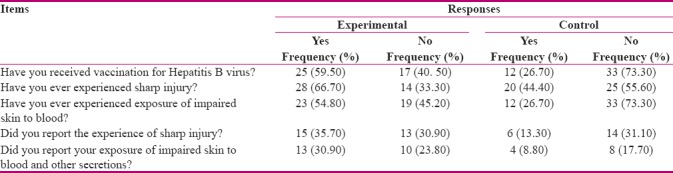
Table 4.
Post-intervention responses of participants on exposure or injury experience in experimental group and control group
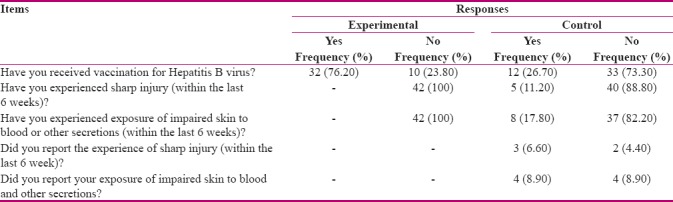
Table 5.
Statistics showing the effect of training program on perception about infection control among experimental and control groups
Discussion
The mean knowledge difference was 7.24. This indicates that the training had a positive effect on participants' knowledge about infection control. This result supports the findings of Burute et al.[10] in their study on the immediate impact of an educational intervention on knowledge about use of disinfectants, in which posttest percentage for use of disinfectants improved significantly. This result is also consistent with the findings of Adly et al.[5] in their study on knowledge and compliance with infection control among nurses. Similarly, Taha[11] found in a study in Sudan that a training program is effective in increasing participants' knowledge and application of standard precautions during labor. Prior to the training, the scores for applying standard precautions were 40.90%, but after the training program, the score increased to 52.20% for knowledge and attitude.
There was a reduction of risk to infection among the experimental group compared to the control group. This indicates that the knowledge acquired during the training made them to be conscious of their safety as indicated by the fact that they did not experience sharp injury within the 6 weeks of training program. On the other hand, in the control group, 5 participants (11.20%) had injury exposure or experience and only 3 participants (6.67%) reported the experience. These participants did not report because they were not exposed to any training programs that would have enhanced their knowledge about infection risk reduction. This finding supports a previous study by Ng et al.[12] conducted in Malaysia among interns. Their results showed that, after educational training, there was a significant reduction of bloodstream infection in the pediatric intensive care unit (PICU). They concluded that the intervention significantly reduced the risk of PICU-acquired bloodstream infection. This result is also consistent with the findings of Lee et al. (2015). In their study on efficacy of a simplified hand washing program, they found that the intervention group had a significant increase in the rating of hand washing.[13] Their target participants were children with intellectual disability and it was compared with sickness-related school absenteeism. It was found that hand washing affected the performance of the students and reduces absenteeism from school. Therefore, when there is no infection, there is good health which will allow a student to attend school.
The findings of this study also indicate that there is a significant difference in the mean perception score of infection control between the experimental and control groups. Therefore, this indicates that the training program has an effect on participants' perception. This finding is similar to the findings of Allegranzi et al.[14] in a study conducted in Mali on hand hygiene improvement strategy. The results showed that knowledge was enhanced significantly, and perception survey showed a high appreciation of each strategy. The researchers explained that the effect was associated with the training program.
From the discussions, it could be seen that the importance of training and retraining cannot be overemphasized. For instance, a previous study reported that a structured training program was effective in improving students' knowledge about Ebola virus disease.[15] Also, Galal et al. (2014),[16] came to similar conclusion in their study conducted in Egypt on the impact of an infection-control program on nurses' knowledge and attitude in PICU at Cairo University hospitals. Their findings showed that a significantly higher level of knowledge was revealed in the post-intervention phase as compared with the pre-intervention phase with regard to the types of nosocomial infections, the at-risk groups for acquiring, and the measures, applied to control nosocomial infections.
Nurses in the post-intervention phase had significantly more knowledge about the types of hand washing. A significantly higher percent of nurses in the post-intervention phase knew about the importance of avoiding recapping syringes and believed that infection control measures could protect them completely from acquiring infection. Statistically significant higher total knowledge and attitude scores were revealed in the post-intervention phase compared with the pre-intervention one. This clearly shows how effective an infection control training program can be in enhancing knowledge, attitude, and practice of infection control. Nwozichi (2016)[17] also reported that a training program was effective in enhancing students' knowledge about testicular cancer and testicular self-examination.
Overall, it was the training program that led the experimental group to have a mean gain of 7.24 on knowledge and 8.36 on perception. When all the factors are addressed this would lead to infection risk reduction. It should be noted, however, that the most important limitation of this study is the small sample size which is just a fraction of registered nurses in the whole of Nigeria, which has reduced the generalizability of the findings.
Conclusion
The structured training program was effective in improving nurses' knowledge and perception about infection control. Findings from this study showed that, after this training program, their risk reduction practice was enhanced. This study also showed that a training program is very effective and all nurses should be exposed to infection control training to be equipped with necessary knowledge and skills with which to fight against the spread of infection in the healthcare setting.
Financial support and sponsorship
The authors did not receive any financial supports or sponsorship for this study.
Conflicts of interest
Nothing to declare.
Acknowledgments
The authors wish to sincerely thank all the nurses who participated in the study despite their tight schedules. They also wish to thank the directors of Nursing services in the selected hospitals who assisted in organizing the nurses during the period of study. (BUHREC526/16)
References
- 1.World Health Organization (W.H.O.) (2016) Infection prevention and control in health care (for preparedness and response to outbreaks) [Last accessed on 2017 Jan 07]. Retrieved from: www.who.int/csr//infection on .
- 2.Sodhi K, Shrivastava A, Arya M, Kumar M. Knowledge of infection control practices among intensive care nurses in a tertiary care hospital. J Infect Public Health. 2013;6:269–75. doi: 10.1016/j.jiph.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 3.Abdulraheem IS, Amodu MO, Saka MJ, Bolarinwa OA, Uthman MMB. Knowledge, awareness and compliance with standard precautions among health workers in North Eastern Nigeria. Community Med Health Educ. 2012;2:131. [Google Scholar]
- 4.Amoran OE, Onwube OO. Infection control and practice of standard precautions among healthcare workers in Northern Nigeria. J Glob Infect Dis. 2013;5:156–65. doi: 10.4103/0974-777X.122010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adly RM, Amin FM, Abd El Aziz MA. Improving nurses' compliance with standard precautions of infection control in Paediatric Critical Care Units. World J Nurs Sci. 2014;35:1–9. [Google Scholar]
- 6.Parmeggian C, Abbate R, Marinelli P, Angelillo IF. Healthcare workers and health care-associated infections: Knowledge attitudes and behaviour in emergency departments in Italy. BMC Infect Dis. 2010;10:35. doi: 10.1186/1471-2334-10-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iliyasu G, Dayyab FM, Habib ZG, Tiamiyu AB, Abubakar S, Mijinyawa MS, et al. Knowledge and Practices of infection control among healthcare workers in a Tertiary Referral center in North-Western Nigeria. [Last accessed on 2017 Mar 17];Ann Afr. Med. 2016 15:34–40. doi: 10.4103/1596-3519.161724. Available from: http://www.annalsfrmed.org/text.asp?2016/15/1/34/161724 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Green LM, Kreuter MW, Deeds KS, Partridge K. Health Education Planning: A Diagnostic Approach. Palo Alto, CA: Mayfield; 1980. [Google Scholar]
- 9.Polit DF, Beck CT. Essentials of nursing research; Appraising Evidence for Nursing compliance with standard precautions. Am J Infect Control. 2014;44:4–7. [Google Scholar]
- 10.Burute SR, Murthy MB, Ramanand SJ, Pore SM, Karande VB, Akat PB. Immediate impact of an educational intervention on knowledge of use of disinfectants in nurses. Int J Basic Clin Pharmacol. 2014;3:507–11. [Google Scholar]
- 11.Taha ANF. Impact of universal precautions training programme on nurse midwives performance during labor in Khartoum state–Sudan 2006–2009. J US China Med Sci. 2014;11:94–107. [Google Scholar]
- 12.Ng YY, Abdel-Latif Mel-A, Gan CS, Siham A, Zainol H, Lum LC. Impact of infection control training for interns on PICU-acquired bloodstream infections in a middle-income country. Singapore Med J. 2015;56:506–12. doi: 10.11622/smedj.2015135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee RL, Leung C, Tong WK, Chen H, Lee PH. Comparative efficacy of a simplified handwashing program for improvement in hand hygiene and reduction of school absenteeism among children with intellectual disability. Am J Infect Control. 2015;43:907–12. doi: 10.1016/j.ajic.2015.03.023. [DOI] [PubMed] [Google Scholar]
- 14.Allegranzi B, Sax H, Bengal L, Richet H, Minta DK, Chraiti MN. Successful implementation of the World Health Organisation hand hygiene improvement strategy in a referral hospital in Mali. Control Hospital Epidemiol. 2015;31:133–41. doi: 10.1086/649796. [DOI] [PubMed] [Google Scholar]
- 15.Nwozichi CU, Ojewole FO, Farotimi AA, Ojediran TD. Effect of self-instructional module on knowledge about Ebola virus disease among Nigerian University students in Bengaluru, India. J Edu Health Promot. 2016;5:1–5. doi: 10.4103/2277-9531.184557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Galal YS, Labib JR, Abouelhamd WA. Impact of an infection-control program on nurses' knowledge and attitude in pediatric intensive care units at Cairo University hospitals. J Egypt Public Health Assoc. 2014;89:22–8. doi: 10.1097/01.EPX.0000444562.71691.06. [DOI] [PubMed] [Google Scholar]
- 17.Nwozichi CU. Effect of video-based teaching module on knowledge about testicular cancer and testicular self-examination among male undergraduate students. Arch Med Health Sci. 2015;3:215–26. [Google Scholar]


