Abstract
Background:
This study aimed to determine the impact of the preceptorship program on self-efficacy and learning outcomes and the association between self-efficacy and learning outcomes in nursing students.
Materials and Methods:
This quasi-experimental study was conducted on 112 nursing students in 2012–2013. The subjects were selected through convenience sampling from the School of Nursing and Midwifery of Shiraz University of Medical Sciences, Iran. The general self-efficacy scale and the perception of overall learning outcomes scale were used to measure the students' perception of self-efficacy and achievement of learning outcomes. The data were analyzed using Pearson's correlation coefficient and linear regression analysis.
Results:
The students' mean [standard deviation (SD)] scores of self-efficacy and learning outcomes were 30.69 (5.88) and 4.10 (0.82), respectively, after taking part in the preceptorship program. The results showed a significant association between the mean scores of self-efficacy and learning outcomes (r = 0.30, p = 0.002). In addition, self-efficacy was predicted by gender (β = −0.19, p = 0.030) and the components of “understand ethical aspects of patient care” (β = 0.31, p = 0.010), “work more systematically” (β = −0.44, p = 0.005), and “use of nursing research” (β = 0.34, p = 0.020).
Conclusions:
Although the nursing students who participated in the preceptorship program demonstrated high mean scores of self-efficacy and learning outcomes, the lack of control group led to the conclusion about the effectiveness of the program to be made in caution. However, this program is suggested to be retained in nursing students' curriculum.
Keywords: Iran, learning, nursing, preceptorship, self-efficacy, students
Introduction
Preceptorship as an effective strategy facilitates clinical practice learning in healthcare professions such as nursing.[1] This program develops personal, communication, and clinical skills.[2] Moreover, the preceptorship program improved students' competency,[3] and confidence to practice,[4] and participants' knowledge of clinical teaching.[5] Moreover, the researchers stated that the turnover rate among new nurses and their related costs decreased after conducting the preceptorship program. A decrease was also observed in the rate of medication errors made by new nurses as well as in the incident rate of adverse events and faults.[6] Additionally, it improved the experience of nurses during the first year of clinical practice,[7] and led to desirable outcomes, such as critical thinking,[8] practice opportunities, and self-efficacy.
In the literature review, a limited number of studies were found to have been conducted on the effect of the preceptorship program on improving nursing students' self-efficacy.[9] However, researchers believed that change in nursing curriculum and enhancement of the motivation in clinical practice might improve nurses' self-efficacy.[10] Self-efficacy was associated with achievement motivation, job satisfaction, and intention to stay in a profession.[11] It helps nurses to be more competent in clinical settings[12] and accept challenging clinical roles.[13] It has also been reported that individuals with high self-efficacy and sufficiency preferred difficult tasks, could motivate themselves to achieve these goals and had better critical thinking abilities.[14,15,16]
Evidence has also shown that efficacy beliefs were effective in the achievement of and persistence in certain educational tasks.[17] Researchers indicated that nursing students who experienced the preceptorship program reported their mean score of learning outcome to be more than 80% of the expected score.[18] Moreover, in another study, the preceptorship program was found to facilitate learning.[19]
Although some studies have been carried out on self-efficacy[20] and learning outcomes in nursing students,[9] a limited number of studies have addressed nursing students' self-efficacy[4,9] and learning outcomes[18,21] during the preceptorship program. Moreover, no studies have assessed the association between self-efficacy and learning outcomes during the preceptorship program. Therefore, the aims of this study were to determine the impact of the preceptorship program on self-efficacy and learning outcomes and the association between self-efficacy and learning outcomes in nursing students. The preceptorship program began in the School of Nursing and Midwifery of Shiraz University of Medical Sciences, Iran, in 2012.[22] In addition, the program was previously used for nursing students in clinical practice teaching in some cities of Iran such as Khorasan Razavi in 2010[23] and Shahr-Kord in 2011.[24]
Materials and Methods
This was a quasi-experimental study with one group, posttest-only design. It was conducted from October 2012 to June 2013. The target population of the study consisted of all the nursing students who participated in the preceptorship program. The subjects were selected from the School of Nursing and Midwifery of Shiraz University of Medical Sciences, Shiraz, Iran using convenience sampling and census method. The participants of the study consisted of all fourth year (seventh and eighth terms) nursing students who had an apprenticeship in one of the previously dedicated wards [emergency room, recovery room, internal ward (gastrointestinal, endocrine, and kidney), burn, intensive care unit, cardiac care unit, dermatology, hematology, and oncology] and had spent their clinical course with a preceptor. In total, 140 students were enrolled into the study. However, 28 questionnaires were not returned or completed. Thus, 112 questionnaires were used for data analysis.
The preceptorship program has become the leading method for the nursing students' clinical training since 2012. The program consists of nursing students, preceptors, and faculties. After many meetings and much planning, the handbook of the preceptorship program for preceptors, faculty members, and students was prepared. Accordingly, the criteria for preceptors were B.Sc. or M.Sc. degree in nursing, more than 1 year of experience as a nursing staff in the same unit where they worked as a preceptor, more than 3 years of experience as a nursing staff, and participation in a 2-day workshop on clinical teaching and assessment. Moreover, the preceptors' competences and their clinical nursing, professional, and personality characteristics were approved by the nursing services manager and faculty members of the School of Nursing and Midwifery. In each shift, the preceptor conducted seven students. Moreover, the faculty members had to have M.Sc. or Ph.D. degrees and more than 3 years of experience as a nursing instructor in the School of Nursing and Midwifery.
The preparation courses for preceptors were offered for 8 h in September 2012. During the preparation period, the preceptors were orientated with their duties in the program, institute's guidelines and policies, teaching logarithms, and library resources. Moreover, information about the purpose of curricula, the course objectives, and learning goals was provided in the workshop. In addition, the preceptors were trained regarding evaluation methods and techniques of communication with students during the clinical practice. Then, 2 h, one-on-one meeting sessions were organized between the faculty members and preceptors in order to clarify the learning goals, course content, expectations, teaching strategies, and evaluation of skills.
The nursing students' orientation day was offered by one of the faculty members in the presence of the corresponding preceptor. During this day, the students were familiarized with the course's learning goals, assignments, evaluation, and clinical environment. Every 3 days, the faculty made on-site visits to discuss the students' progress and observe their skills in the current clinical objectives. The assignments were assessed by both the preceptors and the faculty. Evaluation was also performed by both of them.
The study data were collected using a demographic characteristics form, and the general self-efficacy (GSE) scale and perception of overall learning outcomes scale. The demographic characteristics form included questions on gender, age, marital status, and previous experience of the preceptorship program. In order to assess a general sense of perceived self-efficacy, the GSE was used. The German version of the GSE was developed by Matthias Jerusalem and Ralf Schwarzer in 1979. It was later revised and translated into 26 other languages by many authors.[25] Ellie Nezami, Ralf Schwarzer, and Matthias Jerusalem (http://userpage.fu-berlin.de/~health/persean.htm) translated the GSE into Persian in 1996.
The GSE consists of 10 items responded through a four-point scale (1 = not at all true, 2 = hardly true, 3 = moderately true, and 4 = exactly true). The final score of the scale is computed by summing up the scores of the 10 items and ranges from 10 to 40. On average, it takes 4 minutes to complete this scale.[25] In this study, in order to determine the levels of self-efficacy, GSE was divided into three levels (10–20 = low, 21–30 = moderate, and 31–40 = high).
Criterion-related validity of the GSE has been demonstrated in many studies where positive coefficients indicated favorable emotions, dispositional optimism, and work satisfaction. Negative coefficients, on the contrary, were reported for depression, anxiety, stress, burnout, and health complaints.[25] Among the participants from 23 nations, the Cronbach's alphas ranged from 0.76 to 0.90, with the majority of the coefficients being above 0.80.[25] This scale has also been used in a study in Iran.[26] In this study, the 2-week test–retest reliability of the GSE was 0.89 in nursing students. In addition, the Cronbach's alpha for the Persian version of the GSE was 0.91 among these students.
Moreover, the eight-item perception of overall learning outcome scale was used to measure learning outcomes in nursing students. This scale was designed and used by Lofmark et al. in 2012.[27] The items of this scale included address the patient's need, feel confident, develop independence, develop responsibility, use nursing research, become aware of the importance of critical thinking, work more systematically, and understand ethical aspects of patient care. The subjects were asked to answer the items using a Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree). The mean scores of the perception of overall learning outcomes scale ranged from 1 to 5.[18] Kristofferzon et al. showed that the scale was reliable.[18] Moreover, in a study on nursing students, the Cronbach's alpha coefficient for the scale was reported to be 0.90.[28] In the present study, the content and face validities of the scale were approved by 10 faculty members of the School of Nursing and Midwifery. Moreover, the Cronbach's alpha coefficient of the Persian version of this scale was 0.94 in the nursing students.
Permission to conduct the study was obtained from the School of Nursing and Midwifery of Shiraz University of Medical Sciences. Then, the list of names of the nursing students who were taking part in the perceptorship program was received from the Education Development Organization (EDO). On the last day of the clinical education period, the students were asked to refer to the EDO to complete the study questionnaires. If this was not possible for some students, reminders were sent to them within the following 3–10 days via short message service (SMS).
The study data were analyzed using the SPSS statistical software (version 16, SPSS Inc., Chicago, IL, USA). Descriptive statistics was applied for the demographic characteristics and the self-efficacy data. In addition, Pearson's correlation coefficient was used to determine the relationship between the self-efficacy scores and learning outcomes. Moreover, to assess the factors predicting self-efficacy, linear regression analysis was used. p < 0.05 were considered as statistically significant.
Ethical considerations
This study was approved by the Ethics Committee of Shiraz University of Medical Sciences (EC-P-92-5531, Date: 18 August 2013). Written informed consent form were signed by all the subjects. In these forms, the study objectives and procedure as well as the possibility of sharing the study findings after completion of the study were explained to the study participants. It was also emphasized that participation in this study was voluntary, and participation–nonparticipation in this study did not affect their grades or training.
Results
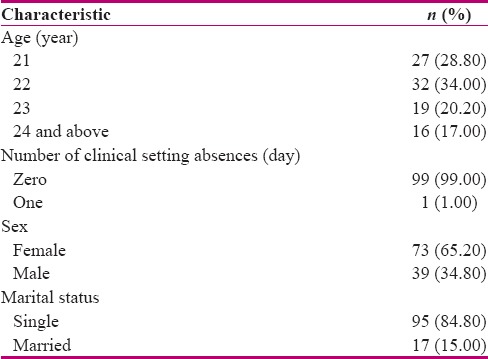
The results of this study showed that most of the students were women (n = 73, 65.20%). The subjects' age ranged from 19 to 43 years [mean (SD): 22.31 (2.71)]. Moreover, most of the students were single (n = 95, 84.80%). The mean number of clinical setting absences during the course was 0.1 day, ranging from 0 to 1 day, and 99 (99.00%) students were present all through the course [Table 1].
Table 1.
Characteristics of the nursing students participating in the preceptorship program
The mean score of the students' self-efficacy was 30.69 (5.88) after participation in the preceptorship program. Moreover, 82 (75.20%), 25 (23.00%), and 2 (1.80%) nursing students gained high, moderate, and low self-efficacy scores, respectively.
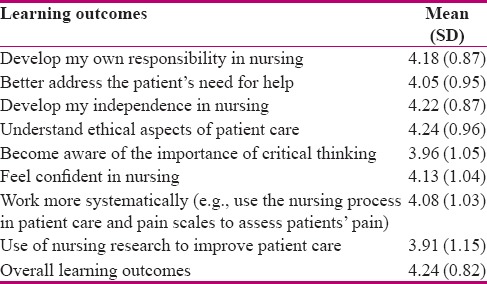
In this study, the mean score of the perception of overall learning outcomes scale was 4.10 (0.82). Table 2 shows the mean scores of the perception of overall learning outcomes scale. The results of Pearson's correlation coefficient indicated a significant relationship between the total mean score of self-efficacy and learning outcomes (r = 0.30, p = 0.002). Moreover, self-efficacy was associated with learning outcomes components, such as developing responsibility (r = 0.20, p = 0.002), addressing the patient's need (r = 0.23, p = 0.014), developing independence (r = 0.25, p = 0.007), understanding ethical aspects of patient care (r = 0.34, p < 0.001), feeling confident (r = 0.26, p = 0.006), and use of nursing research (r = 0.26, p = 0.007). However, no significant association was observed between self-efficacy and other learning outcomes components, such as “become aware of the importance of critical thinking” (r = 0.17, p = 0.070) and “work more systematically” (r = 0.17, p = 0.080).
Table 2.
Mean and standard deviation of the nursing students’ overall learning outcomes achieved during the preceptorship program
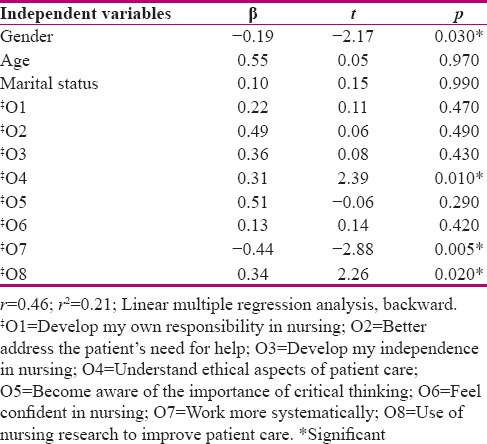
In this study, backward linear regression analysis was used to determine the contribution of each variable to self-efficacy in the nursing students. The predictor variables were age, gender, marital status, and the eight components of learning outcomes. The adequacy of the model was approved using the Durbin–Watson test for uncorrelated residuals (2.3), Kolmogorov–Smirnov = 0.71, p = 0.680 for normality, and collinearity diagnostics [variance inflection factor >2]. Moreover, the stability of variance was approved graphically. The findings of the regression analysis showed that 21% of the variance of self-efficacy was determined by these variables. In addition, self-efficacy was predicted by gender (β = −0.19, p = 0.030) and the components of “understand ethical aspects of patient care” (β = 0.31, p = 0.010), “work more systematically” (β = −0.44, p = 0.005), and “use of nursing research” (β = 0.34, p = 0.020). However, other variables indicated no contribution to the prediction of self-efficacy [Table 3].
Table 3.
Predictors of self-efficacy in nursing students after taking part in the preceptorship program
Discussion
The study results indicated that most of the nursing students had high self-efficacy and perceived that preceptors led to the achievement of learning outcomes to a great extent. Moreover, the results revealed a relationship between self-efficacy and learning outcomes in the nursing students.
In this study, the students' mean score of self-efficacy was 30.69 after taking part in the preceptorship program. Furthermore, most of the participants reported high scores of self-efficacy. A study indicated that the baccalaureate nursing students' self-efficacy scores increased significantly after the 12-week preceptorship program.[9] Teaching experience, personal qualities, interaction with students, and professional development were the four primary characteristics of an effective instructor.[29] Thus, a preceptor with the characteristics of an effective instructor could be effective on the nursing students' self-efficacy.
In this study, the mean score of the perception of overall learning outcomes scale was 4.10, which is approximately similar to that reported in a previous study performed in Sweden (4.22).[18] Moreover, all, except two, of the learning outcomes items obtained a score of higher than 4. In the aforementioned study, the mean scores of the learning outcomes items, except for one, were higher than 4. Consistent with the present study, the mentioned study indicated that the students felt they had largely achieved the learning outcomes during the preceptorship program.[18] Other researchers also concluded that positive preceptor experiences improved learning in the nursing students.[30] Learning may occur by increasing competence, encouraging students to ask questions, taking on challenges, and problem solving during the preceptorship program.[18]
The current study findings showed an association between self-efficacy and learning outcomes, including developing responsibility and independence, feeling confident, addressing the patient's need, using nursing research, and understanding ethical aspects of patient care, in nursing students during the preceptorship program. Moreover, self-efficacy was predicted by understanding ethical aspects of patient care, using nursing research, and working more systematically. Self-efficacy has an impact on academic motivation, learning,[31] skill and knowledge development,[32] and career progress.[31] The study findings also showed a positive association between self-efficacy and responsibility.[33] Individuals with high self-efficacy could motivate themselves to achieve their goals.[14] Individuals with a higher self-efficacy had a strong tendency toward efficient planning and demonstrating better performance, welcomed new ideas more, and were more interested in trying novel approaches to meet other people's needs.[34] Hilli et al., in a qualitative study on student nurses during the preceptorship program, indicated that “a caring relationship based on caring ethics,” was the foundation for learning and development in clinical education.[35] Experienced preceptors, as role models and supporters, might improve responsibility, independence, confidentiality, and understanding of ethical care and patient's need, eventually leading to the enhancement of nursing students' self-efficacy.
The present study findings may be useful for the clinical educators, clinical staff, faculty members, preceptors, and mentors in the identification of preceptors' role in the improvement of nursing students' self-efficacy and achievement of learning outcomes. In the School of Nursing and Midwifery of Shiraz University of Medical Sciences, the design of the nursing students' curriculum was changed 4 years ago. We hope that this change can improve nursing students' self-efficacy and learning outcomes, enhance their competence, autonomy, and acceptance of their role in the future, and decrease “reality shock” and “theory and practice gap” in the clinical setting. This program might also be effective in enhancing the preceptors' competence. Therefore, other studies are required to determine the effect of the preceptorship program on these variables.
One of the limitations of this study was its quasi-experimental, one group, and posttest-only design. As the preceptorship program is executed in the seventh and eighth terms in our university, it was not possible to have a control group or pretest observation. Therefore, there may have been multiple threats to the internal validity of data. Moreover, it could not be concluded that high self-efficacy and learning outcomes might be related to the preceptorship program.
Conclusion
The main finding of this study was that the nursing students who participated in the preceptorship program reported high mean scores of self-efficacy and learning outcomes. In addition, an association was observed between the nursing students' self-efficacy and learning outcomes. Due to the lack of control group and pretest–posttest measurements in this study, conducting other clinical trials with the aim to determine the effect of the preceptorship program on learning outcomes is suggested. Moreover, it is suggested that this program be incorporated in the nursing students' curriculum.
Financial support and sponsorship
Shiraz University of Medical Sciences, Shiraz, Iran
Conflicts of interest
Nothing to declare.
Acknowledgements
This study was a research project approved by Shiraz University of Medical Sciences, Shiraz, Iran (92-01-21-5531). The authors would like to thank Shiraz University of Medical Sciences for their financial support. In addition, special thanks go to the Student Research Committee of Shiraz University of Medical Sciences for their approval of the project. The authors also wish to acknowledge all the nursing students for contributing their time and effort to this study. Moreover, the authors would like to thank the preceptors and faculty members who conducted this program and the members who planned and managed the preceptorship program in the School of Nursing and Midwifery of Shiraz University of Medical Sciences. The assistance of Ms. A. Keivanshekouh at the Research Improvement Center of Shiraz University of Medical Sciences in improving the use of English in the manuscript is also appreciated.
References
- 1.McQueen KA, Poole K, Raynak A, McQueen A. Preceptorship in a nurse practitioner program: The student perspective? Nurse Educ. 2017 doi: 10.1097/NNE.0000000000000498. doi: 10.1097/NNE.0000000000000498. [DOI] [PubMed] [Google Scholar]
- 2.Muir J, Ooms A, Tapping J, Marks-Maran D, Phillips S, Burke L. Preceptors' perceptions of a preceptorship programme for newly qualified nurses. Nurse Educ Today. 2013;33:633–8. doi: 10.1016/j.nedt.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 3.Kim KH. Clinical competence among senior nursing students after their preceptorship experiences. J Prof Nurs. 2007;23:369–75. doi: 10.1016/j.profnurs.2007.01.019. [DOI] [PubMed] [Google Scholar]
- 4.Jordan R, Farley CL. The confidence to practice midwifery: Preceptor influence on student self-efficacy. J Midwifery Women's Health. 2008;53:413–20. doi: 10.1016/j.jmwh.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 5.Al-Hussami M, Saleh MY, Darawad M, Alramly M. Evaluating the effectiveness of a clinical preceptorship program for registered nurses in Jordan. J Contin Educ Nurs. 2011;42:569–76. doi: 10.3928/00220124-20110901-01. [DOI] [PubMed] [Google Scholar]
- 6.Lee TY, Tzeng WC, Lin CH, Yeh ML. Effects of a preceptorship programme on turnover rate, cost, quality and professional development. J Clin Nurs. 2009;18:1217–25. doi: 10.1111/j.1365-2702.2008.02662.x. [DOI] [PubMed] [Google Scholar]
- 7.Forde-Johnston C. Developing and evaluating a foundation preceptorship programme for newly qualified nurses. Nurs Stand. 2017;31:42–52. doi: 10.7748/ns.2017.e10413. [DOI] [PubMed] [Google Scholar]
- 8.Forneris SG, Peden-McAlpine C. Creating context for critical thinking in practice: The role of the preceptor. J Adv Nurs. 2009;65:1715–24. doi: 10.1111/j.1365-2648.2009.05031.x. [DOI] [PubMed] [Google Scholar]
- 9.Goldenberg D, Iwasiw C, MacMaster E. Self-efficacy of senior baccalaureate nursing students and preceptors. Nurse Educ Today. 1997;17:303–10. doi: 10.1016/s0260-6917(97)80061-5. [DOI] [PubMed] [Google Scholar]
- 10.Soudagar S, Rambod M, Beheshtipour N. Factors associated with nurses' self-efficacy in clinical setting in Iran, 2013. Iran J Nurs Midwifery Res. 2015;20:226–31. [PMC free article] [PubMed] [Google Scholar]
- 11.Lee TW, Ko YK. Effects of self-efficacy, affectivity and collective efficacy on nursing performance of hospital nurses. J Adv Nurs. 2010;66:839–48. doi: 10.1111/j.1365-2648.2009.05244.x. [DOI] [PubMed] [Google Scholar]
- 12.Ke YT, Kuo CC, Hung CH. The effects of nursing preceptorship on new nurses' competence, professional socialization, job satisfaction and retention: A systematic review. J Adv Nurs. 2017;73:2296–305. doi: 10.1111/jan.13317. [DOI] [PubMed] [Google Scholar]
- 13.Alavi NM. Self-efficacy in nursing students. Nurs Midwifery Stud. 2014;3:25881. doi: 10.17795/nmsjournal25881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Babenko-Mould Y, Iwasiw CL, Andrusyszyn MA, Laschinger HK, Weston W. Effects of clinical practice environments on clinical teacher and nursing student outcomes. J Nurs Educ. 2012;51:217–25. doi: 10.3928/01484834-20120323-06. [DOI] [PubMed] [Google Scholar]
- 15.Leh SK. Nursing students' preconceptions of the community health clinical experience: Implications for nursing education. J Nurs Educ. 2011;50:620–7. doi: 10.3928/01484834-20110729-01. [DOI] [PubMed] [Google Scholar]
- 16.Gloudemans HA, Schalk RMJD, Reynaert W. The relationship between critical thinking skills and self-efficacy beliefs in mental health nurses. Nurse Education Today. 2013;33:275–80. doi: 10.1016/j.nedt.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 17.Doménech-Betoret F, Abellán-Roselló L, Gómez-Artiga A. Self-efficacy, satisfaction, and academic achievement: The mediator role of students' expectancy-value beliefs. Front Psychol. 2017;8:1193. doi: 10.3389/fpsyg.2017.01193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kristofferzon ML, Martensson G, Mamhidir AG, Lofmark A. Nursing students' perceptions of clinical supervision: The contributions of preceptors, head preceptors and clinical lecturers. Nurse Educ Today. 2013;33:1252–7. doi: 10.1016/j.nedt.2012.08.017. [DOI] [PubMed] [Google Scholar]
- 19.Hendricks SM, Wallace LS, Narwold L, Guy G, Wallace D. Comparing the effectiveness, practice opportunities, and satisfaction of the preceptored clinical and the traditional clinical for nursing students. Nurs Educ Perspect. 2013;34:310–4. doi: 10.5480/1536-5026-34.5.310. [DOI] [PubMed] [Google Scholar]
- 20.Orgun F, Karaoz B. Epistemological beliefs and the self-efficacy scale in nursing students. Nurse Educ Today. 2014;34:37–40. doi: 10.1016/j.nedt.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 21.Paravattil B. Preceptors' Self-assessment of their ability to perform the learning objectives of an experiential Program. Am J Pharm Educ. 2012;76:169. doi: 10.5688/ajpe769169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rambod M, Sharif F, Khademian Z, Javanmardi Fard S, Raiesi H. Nursing students' satisfaction with supervision from preceptors during clinical practice. Iran J Nurs. 2016;29:23–32. [Google Scholar]
- 23.Heydari A, Alizadeh B, Mazloum SR. The effect of preceptorship program on clinical skills of undergraduate nursing students. Iran J Med Educ. 2013;13:588–600. [Google Scholar]
- 24.Aein F, Hasheminia SA, Moghadasi J. Preceptors and student's experiences on the implementation of preceptorship model in clinical practice. J Nurs Educ. 2012;1:25–37. [Google Scholar]
- 25.Schwarzer R, Jerusalem M. Generalized self-efficacy scale. In: Weinman J, Wright S, Johnston M, editors. Measures in health psychology: A user's portfolio causal and control beliefs. Windsor, UK: Nfer-Nelson; 1995. pp. 35–7. [Google Scholar]
- 26.Poortaghi S, Baghernia A, Golzari SE, Safayian A, Atri SB. The effect of home-based cardiac rehabilitation program on self efficacy of patients referred to cardiac rehabilitation center. BMC Res Notes. 2013;6:287. doi: 10.1186/1756-0500-6-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lofmark A, Thorkildsen K, Raholm MB, Natvig GK. Nursing students' satisfaction with supervision from preceptors and teachers during clinical practice. Nurse Educ Pract. 2012;12:164–9. doi: 10.1016/j.nepr.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 28.Palsson Y, Martensson G, Swenne CL, Adel E, Engstrom M. A peer learning intervention for nursing students in clinical practice education: A quasi-experimental study. Nurse Educ Today. 2017;51:81–7. doi: 10.1016/j.nedt.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 29.Singh S, Pai DR, Sinha NK, Kaur A, Soe HH, Barua A. Qualities of an effective teacher: What do medical teachers think? BMC Med Educ. 2013;13:128. doi: 10.1186/1472-6920-13-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bradbury-Jones C, Sambrook S, Irvine F. Nursing students and the issue of voice: A qualitative study. Nurse Educ Today. 2011;31:628–32. doi: 10.1016/j.nedt.2010.10.030. [DOI] [PubMed] [Google Scholar]
- 31.Lauder W, Holland K, Roxburgh M, Topping K, Watson R, Johnson M, et al. Measuring competence, self-reported competence and self-efficacy in pre-registration students. Nurs Stand. 2008;22:35–43. doi: 10.7748/ns2008.01.22.20.35.c6316. [DOI] [PubMed] [Google Scholar]
- 32.Zarshenas L, Keshavarz T, Momennasab M, Zarifsanaiey N. Interactive multimedia training in osteoporosis prevention of female high school students: An interventional study. Acta Med Iran. 2017;55:514–20. [PubMed] [Google Scholar]
- 33.Gutierrez Sanmartin M, Escarti Carbonell A, Pascual Banos C. Relationships among empathy, prosocial behavior, aggressiveness, self-efficacy and pupils' personal and social responsibility. Psicothema. 2011;23:13–9. [PubMed] [Google Scholar]
- 34.Peterson-Graziose V, Bryer J, Nikolaidou M. Self-esteem and self-efficacy as predictors of attrition in associate degree nursing students. J Nurs Educ. 2013;52:351–4. doi: 10.3928/01484834-20130520-01. [DOI] [PubMed] [Google Scholar]
- 35.Hilli Y, Salmu M, Jonsen E. Perspectives on good preceptorship: A matter of ethics. Nurs Ethics. 2014;21:565–75. doi: 10.1177/0969733013511361. [DOI] [PubMed] [Google Scholar]


