Abstract
Background
The aim of this work was to describe utilization patterns of dopamine transporter (DaT) scan and its influence on patient management at a single movement disorders center. DaT scan helps differentiate between neurodegenerative from non‐neurodegenerative parkinsonism and essential tremor (ET). It has been recently approved in the United States in 2011.
Methods
We conducted a retrospective review of all patients, observed by movement disorders neurologists, who received a DaT scan. Demographic data, medication use, and prescan diagnosis were collected.
Results
A total of 216 DaT scans were performed at our center from 1 June 2011 to 31 October 2012. A total of 175 scans were included for analysis. Rates of DaT scan utilization varied from 5 to 33 per 100 new patients observed. When our specialists suspected neurodegenerative parkinsonism before the scan (N = 70), the scan was abnormal in 57%. When non‐neurodegenerative parkinsonism was prescan diagnosis (N = 46), the scan was normal in 65%. When essential/dystonic tremor was suspected (N = 14), the scan was normal in 79%. When psychogenic disorder was the prescan diagnosis (N = 15), the scan was normal in only 47%. Only 4% of patients with abnormal scan remained off anti‐PD medications, whereas 24% of patients with negative scan were still on anti‐PD medications.
Conclusions
DaT scan utilization among specialists varied greatly. Scan results correlated most when prescan diagnosis was ET than when working diagnosis was neurodegenerative parkinsonism or other non‐neurodegenerative parkinsonism. Scan result was least consistent when prescan diagnosis was psychogenic disorder. Finally, DaT scans influenced medical treatment more when it was abnormal, compared to when it was normal.
Keywords: dopamine transporter single‐photon emission computed tomography (SPECT) scan, parkinsonism, neuroimaging
Parkinson's disease (PD) is the second‐most common neurodegenerative disease with incidence of approximately 17 per 100,000.1 Diagnosis is based on clinical criteria, which can lead to inaccurate diagnosis. In a recent community‐based study of 502 individuals with presumed PD, 26% were found not to have parkinsonism.2
Neurodegenerative parkinsonian syndromes, such as idiopathic multiple system atrophy (MSA), progressive supranuclear palsy (PSP), and corticobasal degeneration (CBD), can sometimes be difficult to differentiate from non‐neurodegenerative parkinsonism etiologies, such as vascular parkinsonism, drug‐induced parkinsonism, and essential tremors (ETs). Dopamine transporter (DaT) scan has been approved to aid in the differentiation between parkinsonian syndromes and ET in European countries since 2000,2 but has been approved by U.S. Food and Drug Administration for use in the Unites States just recently, in 2011.
DaT scan is performed by single‐photon emission computed tomography (SPECT) using radioactive pharmaceutical [123I] FP‐CIT (ioflupane I123) that binds to DaT proteins located in the presynaptic membrane on the terminals of dopaminergic projections from the SN to the striatum, providing a marker for dopamine terminal innervation.2, 3 In two large studies comparing degenerative parkinsonism and nondegenerative tremor disorders, the positive percent agreement (i.e., having an abnormal scan when the clinical diagnosis is a neurodegenerative parkinsonian syndrome) was up to 97% and negative percent agreement (i.e., having a normal scan when the clinical diagnosis is a non‐neurodegenerative parkinsonism or ET) was 74% to 97%.4, 5
In this study, we looked at the utilization pattern of DaT scan and its effect on clinical practice among movement disorders specialists in a single center.
Patients and Methods
Subjects
We performed a retrospective chart review of all patients who received DaT scan at our center since its availability on 1 June 2011 until 31 October 2012. Data were obtained through electronic medical record (Epic system). Exclusion criteria were: (1) DaT scans that were ordered by non–movement disorder specialists; (2) the reason for DaT scan was related to research trials; and (3) a second/repeat DaT scan on the same patient.
Information on each patient, including age, sex, race, cardinal signs of parkinsonism (tremor, bradykinesia, rigidity, and postural instability), and the ordering physician, were collected. Medications used, including antiparkinsonian medications, ET treatment, and drugs that may interact with DaT scan results, including amoxapine, amphetamine, benztropine, bupropion, buspirone, citalopram, cocaine, mazindol, methamphetamine, methylphenidate, norephedrine, phentermine, phenylpropanolamine, selegiline, sertraline, and Paroxetine6 were recorded.
The ordering physician's visit note of each patient was reviewed in detail to determine the working diagnosis preceding DaT scan. The pre‐DaT scan diagnoses were classified into four categories, including: (1) neurodegenerative parkinsonism (e.g., idiopathic PD, MSA, PSP, and CBD); (2) non‐neurodegenerative parkinsonism, for example, drug‐induced parkinsonism, vascular parkinsonism, normal pressure hydrocephalus (NPH), psychogenic parkinsonism, and parkinsonism caused by structural lesions (e.g., tumor); (3) essential/dystonic tremor; and (4) uncertain diagnosis (the ordering physician was not sure about the diagnosis and did not lean toward one diagnosis category than the others). Post DaT‐scan follow‐up visit notes and medications were reviewed to identify whether the patients were continued, initiated, or discontinued from antiparkinsonian medications.
DaT Scan
SPECT imaging was performed 3 to 4.5 hours after intravenous injection of 123I‐ioflupane (111–185 MBq; DaTSCAN; GE Healthcare, Waukesha, WI). Nuclear medicine physicians who were blinded to the prescan diagnosis interpreted the images. Image interpretation was based on visual assessment. Normal images were characterized by a largely symmetrical uptake of the tracer in both right and left putamen and caudate nuclei. Abnormal images included those with asymmetrical uptake, or reduced uptake in both right and left putamen alone or also in the caudate nuclei. The scan results were divided into normal, abnormal, and indeterminate.
The flow chart of the study is shown in Figure 1.
Figure 1.
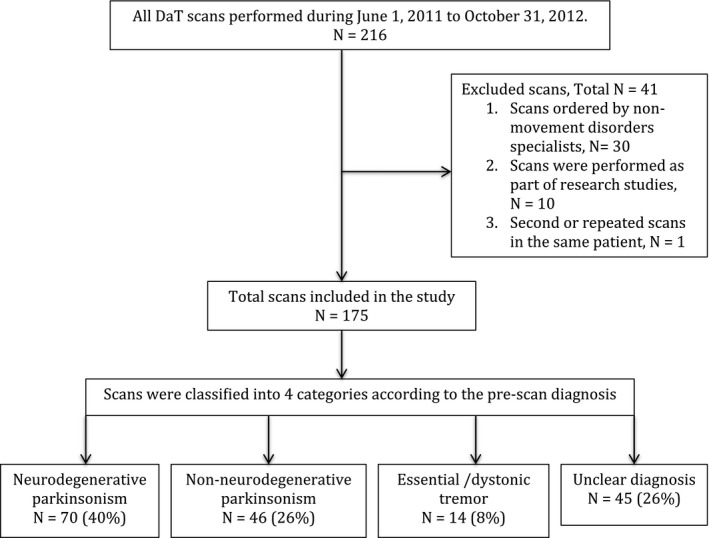
Study flowchart.
Results
A total of 216 DaT scans were performed during the period of 1 June 2011, when the DaT scan was first available at our institution, to 31 October 2012. Forty‐one scans were excluded because of: indication for DaT scan was to comply with a research protocol (30 scans); multiple scans in same patient (one scan); and the scans that were ordered by non–movement disorders specialists (10 scans). All the scans included in the study are all obtained through patient's private or government insurance without commercial funding.
Study Population
A total 175 patients were included in the study. Patients' age ranged between 33 and 88 years (mean = 63). Ninety‐three (53%) were men and 83 (47%) were women. Ninety‐four percent (166) were Caucasian, 3% were African American, and 4% had other ethnicity.
There are seven fellowship‐trained adult movement disorders specialists in our center. During the period of 17 months, each specialist saw a total of 415 to 2,269 patients (old or new). The rate of DaT scan utilization was highly variable per specialist with a range of 5 to 33 per 100 new patients seen. Note that one of the physicians who saw the least number of patients was research oriented and only had clinic once a week.
Of the 175 patients included in the study, 122 (70%) had tremor, 144 had bradykinesia (82%), 124 (71%) had rigidity, and 57 (33%) had postural instability.
The pre‐DaT scan diagnosis was neurodegenerative parkinsonism in 40% (n = 70), non‐neurodegenerative parkinsonism in 26% (n = 46), ET in 8% (n = 14), and uncertain diagnosis in 26% (n = 45). Non‐neurodegenerative parkinsonism diagnoses included drug‐induced parkinsonism, vascular parkinsonism, NPH, hypermanganese, structural lesions, stiff‐person syndrome, toxic‐metabolic, Fragile X–associated ataxia syndrome, and psychogenic parkinsonism.
Fifty‐seven percent (n = 99) of patients were on antiparkinsonian medications preceding the scan. Nine percent (n = 16) were on ET medications. Sixty percent (n = 42) of patients with pre‐DaT scan working diagnosis of neurodegenerative parkinsonism, and 61% (n = 28) of patients with pre‐DaT presumed diagnosis of non‐neurodegenerative parkinsonism were on antiparkinsonian medications preceding the scan, respectively.
DaT Scan Result
Forty‐five percent (n = 78) of patients had an abnormal DaT scan, 54% (n = 95) were normal, and 1% (n = 2) were reported as indeterminate. For the indeterminate scans, 1 showed mildly asymmetric decreased uptake in the posterior putamen and had a prescan diagnosis of psychogenic symptoms. Another reported as minimal asymmetric uptake with slight decrease in left putamen and a prescan diagnosis of drug‐induced parkinsonism. In both cases, the physician interpreted the results as non‐neurodegenerative parkinsonism.
When the prescan diagnosis was neurodenegerative parkinsonism, the scans were abnormal in only 57%. When non‐neurodegenerative parkinsonism was the prescan diagnosis (N = 46), the scans were indeed normal in 65%. When ET was specifically suspected (N = 14), the scan was also normal in 79%. When psychogenic disorder was the prescan diagnosis (N = 15), the scan was normal in only 47%. When physicians were totally unsure of the diagnosis, 58% had normal scans.
Results are shown in Table 1.
Table 1.
Result of DaT scan and relationship to the prescan diagnosis
| Pre‐DaTscan Diagnosis | Total (N) | DaTscan Result | ||
|---|---|---|---|---|
| Abnormal N (%) | Normal N (%) | Indeterminate N (%) | ||
| Neurodegenerative parkinsonism | 70 | 40 (57) | 30 (43) | 0 |
| Non‐neurodegenerative parkinsonism | 46 | 16 (35) | 28 (65) | 2 (0.04) |
| Psychogenic disorders (subanalysis of non‐neurodegenerative) | 15 | 7 (47) | 7 (47) | 1 (7) |
| Essential/dystonic tremor | 14 | 3 (21) | 11 (79) | 0 |
| Uncertain | 45 | 19 (42) | 26 (58) | 0 |
Postscan Clinical Management
During the last follow‐up, only 4% (n = 3) of patients with abnormal scans were not on antiparkinsonian medications whereas 24% (n = 23) were still on antiparkinsonian medications despite having had normal DaT scan.
The most common reasons for using anti‐PD medications despite a normal DaT scan were: delayed improvement of drug‐induced parkinsonism despite discontinuation of offending drug for more than 6 months; drug‐induced parkinsonism with reported improvement on levodopa/carbidopa; NPH and psychogenic parkinsonism with worsening of symptoms when weaned off anti‐PD medications; physician's belief that the patient has PD despite the normal scan; physician's belief that the patient has ET with parkinsonism; idiopathic camptocormia responsive to l‐dopa/carbidopa; and gait disorder of unclear etiology. One patient was suspected to have MSA‐P despite negative scan and 1 patient was thought to have hepatolenticular degeneration‐associated parkinsonism. Two patients took anti‐PD medications for other reasons (RLS).
Of the 3 patients who were not on anti‐PD medications despite abnormal scans, 2 were because of minimal symptoms not requiring symptomatic therapy whereas 1 patient was thought to have an abnormal DaT scan result possibly owing to an interaction with a medication.
Forty‐nine of the patients in our cohort remained on medications that may interfere with the results of DaT scan (usually by decreasing radioligand uptake, thereby resulting in a false‐positive scan7), including sertraline, buspirone, paroxetine, citalopram, bupropion, methylphenidate, benztropine, selegiline, and amphetamine. In our study, 28 of 49 (57%) patients exposed to “contraindicated” medication that may interfere with the scan, potentially causing a falsely abnormal result, still had a normal scan
Discussion
Our study aimed to assess the movement disorder specialists' behavior in utilizing DaT scan as a tool to assist in the diagnosis of parkinsonian syndromes, and its effect on patient management.
We found highly variable physician utilization of DaT scans to facilitate their diagnosis from 5 to 33 per 100 new patients seen. The variable in the rate of DaT scan utilization appears to relate to physician preference rather than the number of years of experience.
Prescan clinical diagnosis was consistent with DaT scan result in only 57% when predicting neurodegenerative parkinsonism (i.e., pre‐DaT diagnosis of neurodegenerative parkinsonism with an abnormal DaT scan result) and 65% when non‐neurodegenerative parkinsonism was the prescan diagnosis. It would not be proper to calculate sensitivity/specificity/positive and negative predictive values of the scan in this study given that the cases included in this “real‐world” experience were clinically ambiguous/challenging (hence the request for the DaT scan) despite the thorough evaluation of the referring fellowship‐trained movement disorders neurologists. The accuracy of our diagnoses was lower than some studies that were previously reported on (70–90%).3, 7 However, Catafau et al., as an example, also reported that their scans did not correlate well with the initial suspected diagnosis. In their study, the imaging results were not consistent with the prescan diagnoses in 36% of patients with presynaptic parkinsonian syndrome (PS) and 54% with nonpresynaptic PS. After imaging, diagnosis was changed in 52% of patients.8
Interestingly, movement disorders clinicians were most accurate in suspecting ET (with a normal scan in 79% of cases) and least accurate in suspecting psychogenic parkinsonism, given that only 47% of the scans were normal. Our study underscores the difficulty of providing the correct diagnosis, and the significant percentage of disagreement between the prescan diagnosis and the scan results, even among fellowship‐trained movement disorders neurologists, especially when atypical features are present and psychogenic disorder is suspected.
Although not absolute, based on our study, DaT scan appears to have a significant impact on the physician's decision on initiating or continuing on antiparkinsonian medications. Ninety‐six percent of patients who have abnormal scan were maintained on antiparkinsonian medications compared to only 60% of those with prescan diagnosis of neurodegenerative parkinsonism. The result is similar to a previous study by Kupsch et al. that DaT scan has a significant impact on clinical management and diagnosis of patients with clinically uncertain parkinsonian syndromes.1
Of interest, 24% of patients were started or continued on antiparkinsonian medications despite a normal DaT scan. We found that the most common reasons were parkinsonism that improved with dopamine replacement or worsened with dopamine withdrawal. There were also a few cases where the clinician did not believe the scan results.
Our study has several strengths, including the high volume of DaT scans from a single, tertiary referral center and surveying a large number of movement disorder specialists; our electronic medical record system allowed us to accurately include all scans obtained and assess in detail the pre‐ and postscan diagnoses, and the medication exposure of each patient. There are also several limitations. As mentioned, the study was retrospective in nature, with a great degree of selection bias. The pre‐ and postscan diagnosis was obtained from retrospective chart review. The scans were interpreted based on visual appearance only. Quantitative DaT‐binding technique may improve the accuracy of the results. Some of the medications, which the subjects were taking, could have altered radioligand uptake, although the majority of those exposed to these medications still managed to have a normal scan. Most of the scans obtained were presumably from atypical cases where even the movement disorders specialists were unsure of their diagnosis. Nonetheless, the study underscores the utility of DaT scans in assisting the diagnosis of neurodegenerative parkinsonism, even among movement disorders neurologists. In this limited, retrospective, center‐specific data, DaT scan utilization varied from specialist to specialist. It appeared to have had a significant impact on the medical management of the patients. DaT scan was most useful when the suspecting prescan diagnosis was psychogenic parkinsonism (given that the majority had an abnormal scan, refuting the diagnosis), but was also useful in other scenarios. In addition, there remained several cases where the clinicians prioritized the clinical presentation over the scan result. Specifically, clinicians were less willing to discontinue anti‐PD medications if their patients showed continued improvement (or worsening of symptoms when medications were tapered) despite a normal DaT scan.
In summary, DaT scans can be helpful in proving (or disproving) the diagnosis of neurodegenerative parkinsonism when patients present with atypical or subtle features; however, it is still not viewed by clinicians as a test with 100% certainty and the results remain to be interpreted within the clinical context. Large, randomized, control trials studying the correlation between DaT scan and neuropathology, which is a gold standard of diagnosis of neurodegenerative parkinsonism, are needed.
Author Roles
(1) Research Project: A. Conception, B. Organization, C. Execution; (2) Statistical Analysis: A. Design, B. Execution, C. Review and Critique; (3) Manuscript Preparation: A. Writing of the First Draft, B. Review and Critique.
S.O.: 1A, 1B, 1C, 2A, 2B, 3A
L.B.: 1C
G.W.: 3A
A.A.: 3B
I.I.: 3B
S.C.: 3B
M.G.: 3B
J.R.: 3B
K.A.: 3B
P.S.: 3B
H.F.: 1A, 2C, 3B
Disclosures
Funding Sources and Conflicts of Interest: The authors report no sources of funding and no conflicts of interest.
Financial Disclosures for previous 12 months: The authors declare that there are no disclosures to report.
Relevant disclosures and conflicts of interest are listed at the end of this article.
References
- 1. Kupsch AR, Bajaj N, Weiland F, et al. Impact of DaTscan SPECT imaging on clinical management, diagnosis, confidence of diagnosis, quality of life, health resource use and safety in patients with clinically uncertain parkinsonian syndromes: a prospective 1‐year follow‐up of an open‐label controlled study. J Neurol Neurosurg Psychiatry 2012;83:620–628. [DOI] [PubMed] [Google Scholar]
- 2. Hauser RA, Grosset DG. [123I]FP‐CIT (DaTscan) SPECT brain imaging in patients with suspected parkinsonian syndromes. J Neuroimaging 2012;22:225–230. [DOI] [PubMed] [Google Scholar]
- 3. Poewe W, Scherfler C. Role of dopamine transporter imaging in investigation of parkinsonian syndromes in routine clinical practice. Mov Disord 2003;18(Suppl 7):S16–S21. [DOI] [PubMed] [Google Scholar]
- 4. Marshall VL, Reininger CB, Marquardt M, et al. Parkinson's disease is overdiagnosed clinically at baseline in diagnostically uncertain cases: a 3‐year European multicenter study with repeat [123I]‐FP‐CIT SPECT. Mov Disord 2009;24:500–508. [DOI] [PubMed] [Google Scholar]
- 5. Benamer HTS, Patterson J, Grosset DG. Accurate differentiation of parkinsonism and essential tremor using visual assessment of [123I]‐FP‐CIT SPECT imaging: the [123I]‐FP‐CIT SPECT study group. Mov Disord 2000;15:503–510. [PubMed] [Google Scholar]
- 6. GE Healthcare . DaTscan™ ioflupane I 123 injection. Highlights of prescribing information. Waukesha, WI: GE Healthcare. [Google Scholar]
- 7. Kägi G, Bhatia KP, Tolosa E. The role of DAT‐SPECT in movement disorders. J Neurol Neurosurg Psychiatry 2010;81:5–12. [DOI] [PubMed] [Google Scholar]
- 8. Catafau AM, Tolosa E; DaTSCAN Clinically Uncertain Parkinsonian Syndromes Study Group . Impact of dopamine transporter SPECT using 123I‐ioflupane on diagnosis and management of patients with clinically uncertain parkinsonian syndromes. Mov Disord 2004;19:1175–1182. [DOI] [PubMed] [Google Scholar]


