Clinical Data
An otherwise healthy 57-year-old male was diagnosed with pancreatic adenocarcinoma in May of 2016. He had a CA19–9 level of 2700 units/ml at diagnosis and was deemed unresectable due to superior mesenteric artery (SMA) encasement and superior mesenteric vein (SMV) occlusion. Over the ensuing 8 months, he received 2 cycles of gemcitabine and paclitaxel protein-bound (Abraxane, Celgene Corporation), followed by external beam radiation with concurrent paclitaxel protein-bound on protocol, and an additional 2 cycles of doublet chemotherapy. Serial imaging showed no evidence of metastases, a decrease in primary tumor size, and diminished SMA involvement (< 180 abutment), but persistent unreconstructible SMVocclusion (Figs. 1 and 2). His CA19–9 level decreased to 8 units/ml. Re-evaluation with new imaging at our institution revealed a patent porto-splenic confluence and extensive venous collateralization (Figs. 2 and 3). Though his primary lesion remained locally advanced pancreatic cancer (LAPC) by currently accepted definitions, a thorough evaluation in our multidisciplinary pancreas cancer clinic determined exploration possible given his excellent therapy response and robust collateralization.
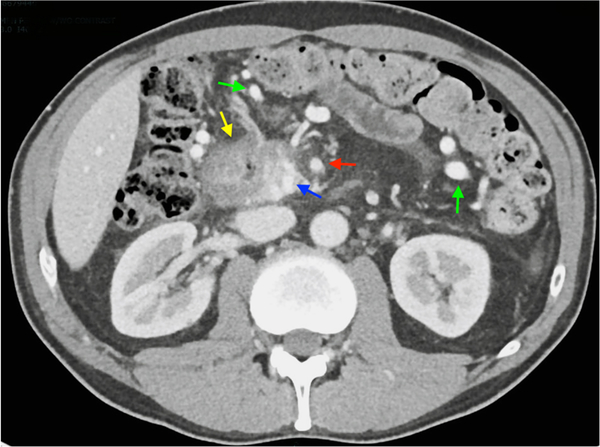
Fig. 1.
Venous phase axial CT image 8 months after diagnosis. Yellow arrow identifies a pancreatic head and uncinate mass. Blue arrow identifies SMV, just distal to occlusion. Red arrow identifies SMA. Green arrows identify right- and left-sided mesocolonic venous collaterals
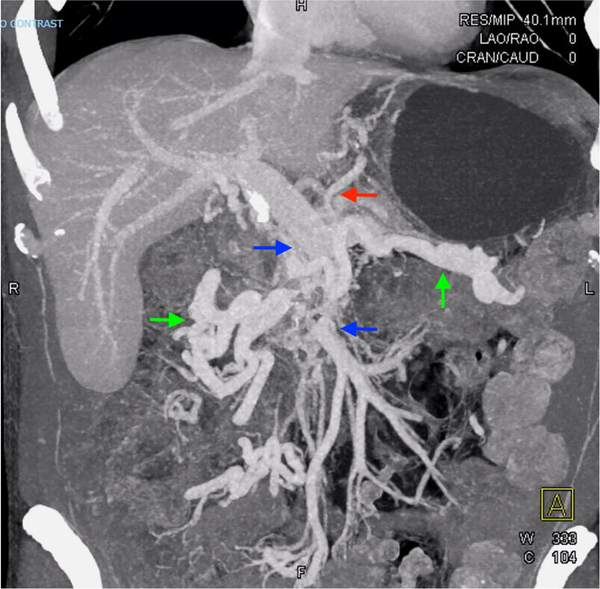
Fig. 2.
Three dimensional CT reconstruction 8 months after diagnosis, showing persistent SMV occlusion and robust venous collateralization. Blue arrows identify the portal-splenic confluence and the distal SMV, with intervening occlusion. Green arrows identify large right and left mesocolonic collaterals that communicate with the distal SMV. The red arrow identifies a dilated gastric vein that communicates between left mesocolonic collaterals and the splenic vein through retroperitoneal collaterals (not seen)
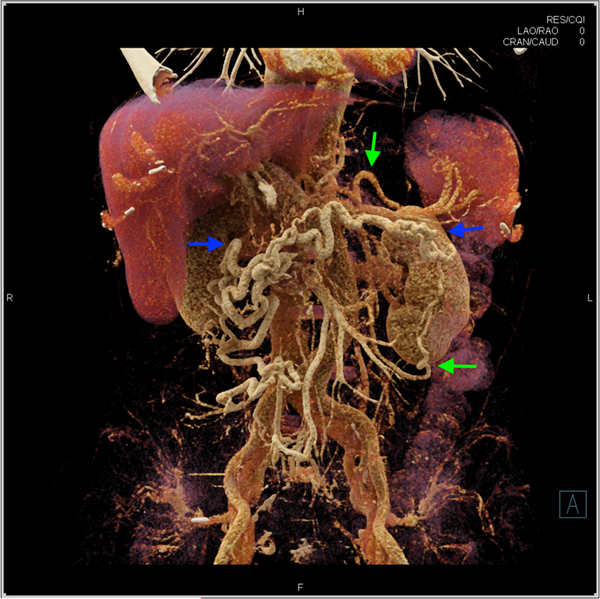
Fig. 3.
Cinematic rendering of CT scan 8 months after diagnosis. Blue arrows identify robust venous collateralization through right and left mesocolonic veins. Green arrows identify retroperitoneal collaterization between left mesocolonic collaterals and the distal splenic vein
Nine months following diagnosis, the patient underwent exploration and a classic pancreaticoduodenectomy and portal lymphadenectomy were performed. To address venous involvement, the portal vein was controlled with a curved Cooley clamp distal to the confluence of the portal and splenic veins. The SMV was resected en bloc, and the portal vein was closed while ensuring patency of the porto-splenic junction. Distal SMV branches were occluded. The patient had an uneventful post-operative course and was discharged on postoperative day seven. His pathology returned with a pathologic complete response: no viable tumor identified, nine negative lymph nodes, no venous/lymphatic or perineural invasion, and microscopically negative margins. His TNM stage classification was ypT0N0M0R0. He is currently alive and well, with no evidence of disease 20 months after pancreatic cancer diagnosis and 11 months after resection.
Discussion
Complete surgical resection is a patient’s best chance for prolonged survival following a pancreatic cancer diagnosis. As systemic therapies and perioperative care have improved over time, definitions of resectability have evolved to increase the number of patients potentially eligible for resection. Currently, pancreatic cancers with venous involvement are classified as borderline resectable (and are thus eligible for exploration and resection) based primarily on the technical considerations of venous reconstruction. Patients with unreconstructible venous involvement are classified as locally advanced and considered unresectable, and are treated in a palliative paradigm. In this report, we describe a technical approach to select LAPC patients with unreconstructible porto-mesenteric venous involvement. In patients with a pancreatic head mass and prolonged venous occlusion with subsequent mesocolonic and left-sided venous collateralization, pancreaticoduodenectomy and vein resection without reconstruction can be performed if collateral veins can be identified and preserved. The success of this approach is highly dependent on high-quality cross-sectional imaging, careful patient selection, and a thoughtful operative approach.
Our enthusiasm for this technique is derived from recent studies evaluating both resection rates and outcomes following neoadjuvant therapy in LAPC patients. Hackert et al. evaluated 575 LAPC patients that received neoadjuvant treatment at the University of Heidelberg, and reported successful resection was achieved in 50.8% of all patients, with higher rates in patients that received FOLFIRINOX (61%).1 In addition, they reported a median survival of 15.3 months in resected patients receiving neoadjuvant therapy, compared to 8.5 months in those undergoing exploration only (P < 0.0001).1 Similarly, Dholakia and colleagues reported a median overall survival of 22.9 months in resected LAPC patients, compared to 13.0 months in unresected patients (P < 0.001),2 while a recent meta-analysis of resection versus palliative treatments in LAPC patients with vein involvement reported increased survival and decreased costs in the resection group.3
Conclusions
Recent studies suggest an aggressive surgical approach in highly selected LAPC patients can improve survival. This approach to LAPC patients with extensive venous involvement, occluded mesenteric venous return, and collateralization allows for the possibility of margin-negative resection in a subset of patients otherwise destined for palliative therapies. Additional studies will be needed to investigate the long-term outcomes of resection in this subset of patients with locally advanced disease.
Footnotes
Compliance with Ethical Standards
Conflict of Interest The authors declare that they have no conflict of interest.
References
- 1.Hackert T, Sachsenmaier M, Hinz U, Schneider L, Michalski CW, Springfeld C et al. Locally Advanced Pancreatic Cancer: Neoadjuvant Therapy With Folfirinox Results in Resectability in 60% of the Patients. Ann Surg. 2016;264(3):457–63. 10.1097/SLA.0000000000001850. [DOI] [PubMed] [Google Scholar]
- 2.Dholakia AS, Hacker-Prietz A, Wild AT, Raman SP, Wood LD, Huang P et al. Resection of borderline resectable pancreatic cancer after neoadjuvant chemoradiation does not depend on improved radiographic appearance of tumor–vessel relationships. Journal of Radiation Oncology. 2013;2(4):413–25. 10.1007/s13566-013-0115-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gurusamy KS, Kumar S, Davidson BR, Fusai G. Resection versus other treatments for locally advanced pancreatic cancer. Cochrane Database Syst Rev. 2014(2):CD010244 10.1002/14651858.CD010244.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]