Abstract
Health expectancy is an essential population health indicator and can be used to monitor changes and/or assess differences in population health. This article provides a brief overview of health expectancy and the issues to be considered in operationalizing and interpreting health expectancy. The article introduces the concept of health expectancy, discusses measures used to compute health expectancy, and methods of calculation. The discussion of measures relates health expectancy to the concept of “health” and clarifies that values of health expectancy depend on how “health” is defined. Software available to compute health expectancy including IMaCh, SPACE and ELECT are also briefly introduced.
Keywords: Health expectancy, summary measures of population health, Sullivan method, multistate life table
1. Introduction
Over the years, health expectancy has been gaining ground in both research and policy making. A book devoted to health expectancy research was compiled in 2003 [1] by REVES1 members who had been leading research on health expectancy. The second edition of a standard text book for demographers, The Methods and Materials of Demography2 [2], added a section on health expectancy. Now, Eurostat, run by the European Commission, includes health expectancy as an indicator of population health.
Within the European Innovation Partnership on Active and Healthy Ageing, the European Commission has set the target for a two-year increase in healthy life years at birth from 2010 to 2020 in the European Union (EU). In the US, “Healthy People 2000” released by the US Department of Health and Human Services in 1990 included healthy life years among its targets for the first time. Since then, the target has been updated in “Healthy People 2010” and “Healthy People 2020”. In Japan in 2012, the Ministry of Health, Labor and Welfare released their health promotion guideline for the next decade, and its first priority is to increase healthy life years.
This article is a brief introduction to health expectancy and the issues to be considered in health expectancy research. We will introduce the concept of health expectancy first. In subsequent sections, we will discuss the concepts and measures of health used in health expectancy research, data sources and methods for computing health expectancy, and software available for estimating health expectancy. Then, we will discuss issues to be considered on defining health, measures used and calculation method, when we conduct research on health expectancy.
2. Concept of health expectancy
Health expectancy is the analysis of both healthy and unhealthy years of life where health can be defined along various dimensions. For instance, a life expectancy of 86 years composed of 82 healthy years and 4 unhealthy years would mean that on average a person had 4 unhealthy years over the entire 86 years. However the 4 unhealthy years do not necessarily mean the last 4 consecutive years of life. In theory, the 4 unhealthy years could include days with injuries from sports activities in youth, car accidents at working ages, or disability caused by stroke at old ages. Life expectancy can also be divided into more than two health states, such as healthy years, mildly disabled years, and severely disabled years, as long as the states are mutually exclusive. One of the confusions surrounding health expectancy research has resulted from the fact that researchers coin their own terms for “healthy years” depending on the measures used to de-fine health status. Commonly used terms for healthy years are disability-free life expectancy [3,4], active life expectancy [5,6], healthy life years [7], and healthy life expectancy [8–10]. The measures used in defining health status and the terms used for healthy years will be discussed further in this article.
The concept of health expectancy was introduced in the 1960s by Sanders [11] and Sullivan [12]. This was because life expectancy no longer served its original purpose in developed countries. Life expectancy has been used as an indicator of population health for a long time. It is a summary measure of mortality at all ages adjusted for population age structure. Life expectancy is very easy to understand and is expressed by one number, the average number of years expected to live at birth. However, as infectious diseases, which were the main cause of death among populations, became less threatening, and the proportion of people with chronic and degenerative diseases was increasing, life expectancy was not as tightly tied to health. Thus, in order to assess and monitor the state of population health, researchers as well as policy makers were searching for a population health indicator that would combine both mortality and morbidity.
Sullivan introduced such an indicator in 1971 by proposing a method of computing health expectancy based on life table models and using days with activity limitation and institutionalization (life free of disability) and number of bed days (life free of bed disability) as measures defining health status. Since the introduction of this approach, research on health expectancy has been propelled forward on two occasions. The first was around 1980 with the introduction of the debate between “compression of morbidity” put forth by Fries [13] and “expansion of morbidity” by Gruenberg [14] and Kramer [15]. In order to find empirical evidence for the arguments central to this debate, health expectancy was computed to examine whether people were living longer healthy lives. The main question addressed was whether people were living longer healthy lives as well as longer lives.
The establishment of REVES in 1989 as a research network was the second occasion. When REVES started, its membership was about 50 researchers and policy makers from six countries. Recent figures from their home page show that this number has increased to over 150 researchers and policy makers from more than 30 countries. REVES’ contribution has been the dissemination of the concept of health expectancy and the harmonization of measures and methods of computing health expectancy.
Recently, an additional force in promoting the use of health expectancy arises from an increased tendency to emphasize quality of life (health expectancy) rather than quantity of life (life expectancy). In addition, endorsement of the International Classification of Functioning, Disability and Health (in short ICF) in 2001 may have contributed to moving health expectancy research forward by providing an opportunity to develop a common set of instruments to measure “health”. According to the home page of the World Health Organization (WHO), “the ICF puts the notions of ‘health’ and ‘disability’ in a new light (http://www.who.int/classifications/icf/en/).” The Washington Group on Disability Statistics (WG) (http://www.cdc.gov/nchs/washington_group.htm), one of the United Nations’ city groups, developed a short set of instruments based on ICF to measure “disability” for censuses and surveys [16]. Members of Euro-REVES, a regional group of members of REVES in Europe, also developed a single instrument to measure “disability”, the Global Activity Limitation Indicator (GALI), based on ICF as a conceptual framework [17,18]. GALI was included in 2004 in the survey on EU Statistics on Income and Living Conditions (EU-SILC) among EU countries, and health expectancy was computed annually using GALI since then. As mentioned above, health expectancy is listed as a population health indictor in EUROSTAT. One of the issues health expectancy research has encountered over the years is the large number of indicators used to define health status. The advent of this common set of instruments could promote cross country comparative research on health expectancy.
3. Concept and measures of health in health expectancy
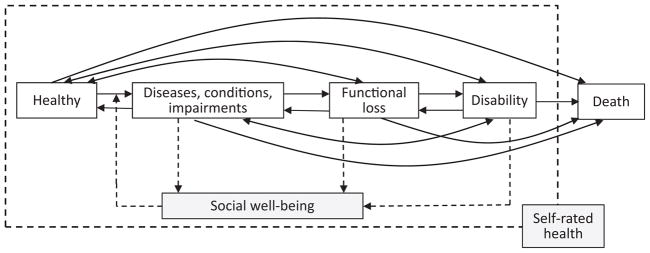
Defining health is one of the issues in developing for health expectancy research. The measure used for computing life expectancy is death; there is no other measure for life expectancy. In contrast, there are many operational definitions of health status. Health is de-fined as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” [19]. However, operationalization of this definition to measure the concept of health as a single index for monitoring population health has not been successful. Having said that, we are not even sure whether we can or need to have a single index for population health. Social well-being is often missing in the operationalization of defining health. In addition, health is a multifaceted state as is demonstrated in many proposed models of disablement [20–25] and morbidity process [26]. Figure 1 is a conceptual model of health states and health transitions. Social well-being has been included in the definition of health by WHO, but it can be affected by physical and mental health states. At the same time, social well-being is a risk factor for physical and mental ill-health. At least, five dimensions of physical and mental health shown in solid lined boxes can be identified, i.e., “healthy”, “diseases, conditions, or impairments”, “functional loss”, “disability”, and “death” [27]. Health expectancy can be computed based on these health states or transitions among health states.
Fig. 1.
Conceptual model of health states and health transitions according to the disablement process.
Research on health expectancy has used diseases, conditions, impairments, and functional loss or disability together with death to define health status and compute health expectancy. If having a particular disease, for instance stroke or dementia, is used as an operational definition of health status, other diseases and disabilities are not be considered in the computation of health expectancy. If having a disability is used to define health status, having diseases or conditions are ignored. Even if the same conceptual definition is used to define health status, differences in the wording of the question or response categories used can lead to differences in computed health expectancies. For example, disability can be measured in four categories, i.e., “none”, “mild”, “moderate” and “severe”. To compute health expectancy, health status can be defined by selecting only those with severe disability as opposed to all others, those with moderate and severe vs. those with none and mild, or those with none against others. Operational definitions of health status may differ across studies, but each measure used to compute health expectancy will result in a different estimate. Therefore, researchers have to state clearly their operational definition of health status, and the audience should understand that different operational definitions of health status in health expectancy research will yield differences in estimated health expectancies. Ideally, harmonization of population health measures used in computing health expectancy aids comparisons, and the development of the GALI or the six questions compiled by the WG may lead to a common set of measures for population health.
Although the list is not exhaustive, measures most often used in health expectancy research are described briefly in the following section.
3.1. Self-rated health
Self-rated or self-perceived health provides an indicator of the self-assessed overall health status of individuals. People are likely to evaluate their own health holistically, taking into account a variety of social, physical, and emotional factors that impact their health as well as specific cultural factors. Despite this, previous studies have shown that self-rated health is a good predictor of a variety of health outcomes such as illness, fall, hospitalization, and mortality [28–33]. When self-rated health is used as a measure of health in health expectancy research, healthy years of life expectancy are often called “healthy life expectancy”. The wording for questions on self-rated health in surveys is, for instance, “Would you say your health in general is excellent, very good, good, fair, or poor?” Healthy life expectancy has been computed for Austria [8], the Netherlands [34], Scotland [35], Japan [10], six Asian countries [36], and Eastern European countries [37]. Note that two main sets of response categories have been used, “excellent, very good, good, fair, or poor” as above, generally used in English speaking countries and in Nordic European countries, and “very good, good, fair, bad and very bad” used in the European Union following WHO’s recommendation [33]. In many cases, the item “fair” is difficult to translate. OECD, a key player in health measures harmonization, proposed to rescale the response categories using conversion tables to make the two sets more comparable [38,39].
3.2. Diseases, conditions, and impairments
Although WHO defines health as a state of complete physical, mental, and social well-being, people tend to consider health in terms of not having diseases, conditions, or impairments. In the Global Burden of Disease (GBD) Project, Christopher Murray and colleagues developed a unit called “disability-adjusted life years” (DALY) to measure health status in terms of disease prevalence, adjusted by specific disability weights, among a population [40]. Based on the DALY approach, WHO computed health expectancy called “disability-adjusted life expectancy” in the 2000 World Health Report and “health-adjusted life expectancy” in the 2001 World Health Report. These summary measures are also called “healthy life expectancy” in the most recently published work by Salomon et al. [41]. Although the term used for health expectancy was changed, the measure used to compute health expectancy remained the same, DALY. Conceptually, the weights used for estimating DALYs are based on the expected disabling burden of various conditions (disease stages). The prevalence of specific diseases, conditions, or impairments, such as heart disease [42], stroke [43], dementia [44], cataracts [45], depression [46], and cognitive impairment [47,48], was also used as an operational definition of health status.
3.3. Limitation of activities
This measure was used for the first time by Sullivan [3] in his seminal work on health expectancy. “Disability-free life expectancy” is the corresponding term for healthy years. Disability-free life expectancy is often computed at birth because it is based on a measure that is appropriate across the whole age range. Because disability is the inability to perform socially expected roles, and because the expected social roles (e.g. work, go to school, or perform self-care) vary by age, it means having a definition that changes across ages. For instance, a question in the National Health Interview Survey in the US asked about limitation in major activities which differed by respondents’ ages until 1997. Disability-free life expectancy has been computed for Australia [49], Canada [50], China [51], France [52], Japan [53], the UK [54,55], and the US [4,56,57].
3.4. Global Activity Limitation Index (GALI)
GALI is also a measure of activity limitation developed by members of Euro-REVES [17,18,58]. However, when GALI is used to compute healthy years of life expectancy, it is termed “healthy life years”. An individual is asked, “For the past six months at least, to what extent have you been limited because of a health problem in activities people usually do?” There are three possible responses including not limited, limited but not severely, or severely limited. The question was developed for people older than 15 years of age. Studies on healthy life years utilizing GALI have been conducted mainly for EU countries [7,59].
3.5. WG short set of questions on disability
The questions cover six functional domains or basic actions plus self-care: seeing, hearing, walking, cognition, self-care, and communication [16]. The short question set reads, “The next questions ask about difficulties you may have doing certain activities because of a health problem.” “Do you have difficulty seeing even if wearing glasses?” Then, five questions follow. Each question has four response categories including “no difficulty”, “some difficulty”, “a lot of difficulty” and “cannot do it at all”. The WG short set of questions has been included in censuses and surveys over the years, and health expectancies computed based on these instruments have been published [60] and reported at conferences [61].
3.6. Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs)
Both ADLs [62] and IADLs [63] are measures of performance of essential activities for an independent life at older ages. Also, both measures involve items on multiple activities. ADLs include activities such as bathing, dressing, eating, toileting, transferring from/to bed/chair, and walking inside the home. IADLs include activities such as preparing own meals, using the telephone, shopping for personal items, managing money, and managing medication. An individual is often asked in surveys, “Do you have any difficulty performing _____ (each activity listed) because of health reasons?” Answers to the question are yes or no, but if the individual responded yes to the previous question, a subsequent question often asks for degrees of difficulty (such as a little, some, a lot, unable). The wording of the question varies by survey and the differences that need attention. Alternative wordings are: “Can you do _____?” and “Do you need help in performing _____?” When they computed health expectancy using a composite measure of ADLs, Katz et al. [5] coined the term “active life expectancy” for the healthy part of life expectancy. Studies often include both ADLs and IADLs to construct a composite measure for functioning problems. This is partly because composite measures provide more levels of disability with a more comprehensive range of activities compared with measures limited to either ADLs or IADLs [64]. Active life expectancy has been computed for many countries including China [65], Indonesia [66], Japan [6,67], the Philippines [68], the UK [69], and the US [70–72].
One of the most recent health concepts introduced in health expectancy research is the concept of frailty, an emerging concept in geriatrics [73]. Two studies of health expectancy based on frailty were presented at the REVES meeting in Austin, Texas in 2013 [74,75].
4. Data sources used to compute health expectancy
There are two major types of data sources used in health expectancy research, namely, cross-sectional and panel/longitudinal. Cross sectional data include censuses, cross-sectional surveys, and administrative data compiled by national and local governments. A census can be used to obtain information on population health status. As mentioned above, in some countries, the WG short set of questions has been included in censuses. However, a census tends to be conducted every 10 years, and the number of questions asked is limited. In many countries, in order to monitor population health status, national health surveys and national disability surveys have been conducted with shorter time intervals and more questions. Repeated cross-sectional surveys such as the National Health Interview Survey in the US are valuable sources for health expectancy research and have been used for computing health expectancy. Cross-sectional data sources provide information on prevalence of diseases, conditions, impairments, functional loss, and disability. Administrative data can be also used to compute health expectancy. One such example is the use of the National Long-Term Care Insurance data in Japan [76]. Basically, cross-sectional data sources can provide information on the current population health structure.
Panel/longitudinal data for health expectancy research include panel/longitudinal surveys, surveillance systems, registration data, and administrative data. Panel/longitudinal surveys have been conducted mainly in the US and include the Panel Study of Income Dynamics (PSID) and the Longitudinal Study of Aging (LSOA). An increase in available longitudinal survey data in recent years is remarkable especially for the middle and older adult population. The Health and Retirement Study (HRS) is one such survey, and data from sister surveys of HRS such as the Survey of Health, Ageing, and Retirement in Europe (SHARE), the English Longitudinal Study of Ageing (ELSA), and the Chinese Health and Retirement Longitudinal Study (CHARLS) are becoming available for use. In many developing countries such as Bangladesh and Tanzania, health and demographic surveillance systems have been associated with the INDEPTH network (http://www.indepth-network.org/) and could be a good longitudinal data source for health expectancy research. In more than 40 sites in developing countries, people have been followed for many years and have provided comprehensive and accurate health data. Although the use of data is limited, specific disease registration systems, such as a cancer or stroke registry, they can be used for the computation of disease specific health expectancy. The sample size of data seems to be enormous in countries like the UK and the US. Finally, administrative data such as the Danish National Health Service Register and the Administrative Register Data available to researchers in Denmark can be utilized for health expectancy research. Data availability in Denmark and other Nordic countries is astonishing. Certainly, longitudinal data can be constructed from administrative data, such as the National Long-Term Care Insurance administrative data in Japan. Health expectancy can be computed using such data.
5. Methods of computing health expectancy
While defining health is one issue in conducting health expectancy research, another issue is choosing a method for computing health expectancy. There are many ways to compute health expectancy although the computational methods appropriate are closely linked with the types of data sources. When cross-sectional data are used, a prevalence-based method, often called the Sullivan method, is applied. When panel/longitudinal data are used, the Sullivan method but also other methods of computing health expectancy can be applied. Methods used to compute health expectancy include the double decrement life table method [5], the multistate life table method [77], the grade of membership (GoM) approach [78], the micro simulation method [79,80], and the Bayesian approach [81,82]. The double decrement life table method has a limitation in estimating health expectancy and the GoM approach has been applied less frequently to compute health expectancy. Because of the availability of longitudinal survey data and software in recent years, the multistate life table method and the micro simulation method have been used in health expectancy research. We describe in the following section two commonly used methods of computing health expectancy, the Sullivan method and the multistate life table method. Please refer to the cited studies for other methods of computing health expectancy.
5.1. Sullivan method
Computing health expectancy by the Sullivan method requires life tables and information on the age-specific proportions of the population in healthy or unhealthy states, generally gathered in censuses and cross-sectional surveys. These proportions are prevalence measures of the actual and current health status of a real population and are used to divide years lived in the life table population, implied by current mortality rates, into healthy and unhealthy years. The original approach designed by Sullivan can be adapted to include any number of unhealthy states: short term and long term disability, with and without disease, severe and less severe disability, and institutionalization. All that is necessary is to divide the population into mutually exclusive health categories. A brief discussion of the computational process for the Sullivan method is offered using life table terminology. Let lx, nLx, Tx, ex denote the surviving population at exact age x, the number of person-years lived between exact age x and x + n, the number of person-years lived after exact age x, and life expectancy at age x, respectively. Superscript T, H and U denote total, healthy state, and unhealthy state, respectively. Prevalence rates of the unhealthy population between age x and x + n is denoted by nPREVx. The number of person-years lived between exact age x and x + n in the unhealthy state is computed by Eq. (1).
| (1) |
Then, these numbers are summed from exact age x to maximum age in the available or open-ended age group in the life table.
| (2) |
The mean number of expected years to live for the unhealthy population is computed by Eq. (3).
| (3) |
Because total life expectancy at exact age x is already given by the life table, the mean number of expected years to live in a healthy state is computed by subtracting expected unhealthy years from total life expectancy at exact age x.
| (4) |
A detailed description of the method is available at the REVES home page including how to estimate standard errors [83].
5.2. Multistate life table method
For a long time, this method was also known as the increment-decrement life table method by demographers, since the multistate life table method was developed in response to a desire to model dynamic processes that involve multiple and recurrent events. The method has been applied to a number of topics such as marital status [84], migration [85], and labor force participation [86,87]. The multistate life table method was first applied to health expectancy research by Rogers, Rogers, and Branch in 1989 [77]. The basic features of the multistate life table method that make it a valuable tool for analysis in health expectancy research are: 1) it is based on incidence measures representing current health transitions; 2) it allows movement in both directions between all surviving health states; 3) it allows death rates to differ by health state [77,88–90].
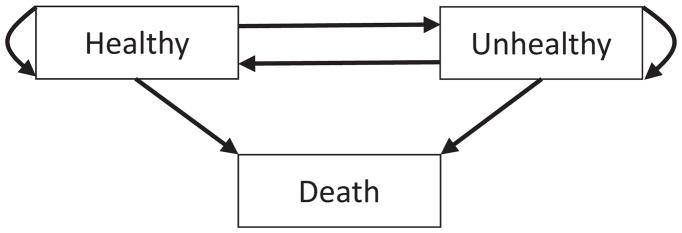
Health expectancy by the multistate life table method is derived from a set of transition schedules to and from healthy and unhealthy states and to death estimated using panel/longitudinal type data sources. As an example, possible transitions among two health states and an absorbing state of death are shown in Fig. 2. As represented by each arrow, there are six transitions including two retention schedules for each age or age group used in a study. The multistate approach is especially well suited to examine health expectancy since people experience both declines and improvements in health status as they age. Moreover, it takes into account the different mortality profiles by health status.
Fig. 2.
Depiction of possible transitions among health states.
Construction of multistate life tables starts with sets of transition rates (mx’s) or sets of transition probabilities (px’s) depending on methods used to obtain these transition schedules. If the sets of transition rates are estimated, the matrix of transition rates (Mx) is used to calculate a transition probability matrix, Px, by an equation suggested by Rogers and Ledent [91].
| (5) |
If the sets of transition probabilities are estimated directly from available data, this step can be ignored. Elements of the transition probability matrix, ijPx, represent the probability that a person in state i at exact age x will be in state j at exact age x + n, including an absorbing state, death. The computed transition probability matrix allows the specification of the familiar life table relationship from which survivorship values for all ages can be calculated [85,92,93]:
| (6) |
where nlx is a survivorship matrix whose elements represent the number of persons in state i at exact age x who will be in state j at exact age x + n. Please note that the matrix is called a survivorship matrix, but this matrix includes number of deaths (absorbing state) from each health state. Once the elements of the matrix are rearranged and number of deaths is excluded from the matrix, the number of life table population at each surviving health state at exact age x + n can be computed. Then, this matrix becomes lx for the next age group, which is a survivorship matrix similar to nlx but whose elements, ijlx, represent the number of persons in both state i and j at exact age x (i.e., ijlx = 0 where i ≠ j) such that its diagonal elements represent the number of survivors in state i at exact age x.
Other familiar life table functions also can be expressed in matrix notation. A life table stable population can be obtained by assuming linearity in the gross flow functions,
| (7) |
This allows the calculation of state-specific life expectancy estimates. Specifically, life expectancy in state i at age x is calculated as follows:
| (8) |
where iTx is the number of person-years lived in state i beyond exact age x by the cohort who survived to age x; and iex is life expectancy in state i at exact age x. Total life expectancy is the sum of life expectancies in each of the health states.
Multistate life tables can be either population-based, where we assume that the population enters the life table with the distribution over the healthy and unhealthy states observed at the radix age [71,90], or status-based, where we assume that everyone enters a life table in a given health state [77,88]. Population-based multistate life tables describe the potential life cycle events for the whole population; while status-based tables can be used to compare the prospective life cycles of those who reach specified ages in different health states. It is not difficult to imagine that those who are unhealthy at age 65 would have a shorter life and healthy life expectancy and a longer unhealthy life expectancy compared to those who are healthy at the same age.
We started the section on multistate life tables with health transition schedules as a given. Estimating health transition schedules is imperative to compute health expectancy by multistate life table methods. There are a few methods of estimating health transition schedules such as a logistic regression approach [80,94] and a discrete-time hazard modeling approach [90]. The former approach estimates transition probabilities, and the latter approach estimates transition rates. In the following section we discuss available software to compute health expectancy. Some of this software includes procedures to estimate transition schedules.
Most of the previous studies using multistate life table methods have adopted the Markovian assumption that there are no effects of prior history and duration in a health state. In other words, age-specific health transition schedules are estimated regardless of a person’s previous health experiences, although some studies have indicated a duration effect on health transitions [95,96]. Employing a semi-Markov model, studies by Cai and colleagues incorporated effects of lengths of duration in health states to compute health expectancy [97,98].
Another issue in estimating health transition schedules is that in increasing the number of living health states in the model, the number of transition schedules to be estimated increases multiplicatively. As shown in Fig. 2, the number of transition schedules depends on the number of states of health included in the model. When we have two living health states, we need to estimate six transition schedules. With three living health states, we need to estimate 12 transition schedules, and with four living states, 20 transition schedules. We need a large enough sample size for estimating stable health transition schedules.
6. Available software to compute health expectancy
There are at least five freely available computer programs and software to compute health expectancy. Four of them compute health expectancy using multistate life table methods and another one uses the Bayesian approach. Here, we briefly introduce these programs. Willekens and Putter [99] discuss some of software introduced here in detail in a recently published article in Demographic Research.
IMaCh (a Maximum Likelihood Computer Program using Interpolation of Markov Chains) was developed by Nicolas Brouard and Agnès Lièvre when both were at the Institut National d’Etudes Démographiques (INED, Paris, France). The manual for the program and the package program can be downloaded from http://euroreves.ined.fr/imach/, and the program is described in detail in Lièvre et al. [94]. Once text data in required format are input, IMaCh first estimates the transition probabilities (px’s) using multinomial logistic regression with a maximum likelihood technique. Based on these estimated transition probabilities, IMaCh constructs both population-based and status-based multistate life tables and provides many statistics including standard errors and graphs automatically. Many studies, such as Yong and Saito [6] and Crimmins et al. [100], have been conducted using IMaCh as a tool for statistical analyses.
STATA codes written by Weden [101] to construct multistate life tables are available at http://ideas.repec.org/c/boc/bocode/s453001.html. Data required to construct multistate life tables are age-specific transition probabilities. These codes should be very useful for those who use STATA for their statistical analyses.
The SPACE (Stochastic Population Analysis for Complex Events) program was developed by Liming Cai when at the National Center for Health Statistics, US Center for Disease Control and Prevention. Both the SPACE program and the manual are available at http://www.cdc.gov/nchs/data_access/space.htm#journal. SPACE is written in SAS codes. SPACE first estimates either the transition probabilities or the transition rates using longitudinal survey data. Then, based on the estimated transition schedules, SPACE uses either the deterministic or simulation approach to construct multistate life tables with standard errors estimated by the bootstrap approach. A detailed description of the SPACE program and its application can be found in Cai et al. [102]. Studies, such as Diehr et al. [103] and Payne et al. [104], have been conducted using the SPACE program.
ELECT is a set of functions in R and can be used to construct multistate life tables. A manual, written by Ardo van den Hout, for constructing multistate life tables with ELECT is available at http://www.ucl.ac.uk/~ucakadl/ELECT_Manual_13_02_2013.pdf, and command lines used in the manual are also available at http://www.ucl.ac.uk/~ucakadl/indexELECT.html. ELECT utilizes the msm package for R developed by Jackson [105] to compute transition probabilities based on the Markov assumption. ELECT has been used in studies such as that of Van den Hout and Matthews [43].
GSMLT (Gibbs Sampler for Multistate Life Tables Software) was developed by Lynch and Brown [106] using the Bayesian approach, and the manual is available at REVES URL. The software is available from the developer of the program. A detailed description of the program can be found in the study by Lynch and Brown [82].
7. Discussion
There are several issues to be considered in conducting and understanding research on health expectancy. These issues, however, mainly depend on the data available to researchers. Unless researchers conduct their own survey and choose the definition of health to compute health expectancy, they must utilize the health measures available in censuses, existing surveys, or statistics from national or local governments. Censuses and surveys contain health measures intended to monitor population health. The concept of health expectancy was developed as a summary measure of population health (SMPH) which combines both mortality and morbidity in a single index to examine levels and changes in population health. However, the concept of health expectancy can be applied to sub groups of a population or specific age groups of a population.
7.1. How to define health states
The first issue in health expectancy research is to operationally define the health states based on the available health measures in the data sources. If we are interested in examining trends in population health, we have to find population health measures which have been asked repeatedly in censuses or surveys over time. The wording of the questions has to remain unchanged over the period studied and, ideally, the location of the questions in the questionnaire, as well as the main features of the survey design, should remain unchanged. Changes in the wording of the questions, in the order of the response categories, or in the location of the questions in the questionnaire may cause changes in responses which cannot be distinguished from actual changes in population health. Unfortunately, it is not easy to find health measures with the same wording and which remain unchanged in surveys for long periods of time. Self-rated general health and limitation of activities are good examples of such health measures.
It is also not easy to find health measures which are applicable to all age groups. For instance, self-rated general health may not be applicable to children. Allowing proxy responses, limitation of activities asked in the National Health Interview Survey in the US covers a whole population. But as we already mentioned before, the main activities asked about differ by age groups. Similar questions asked in the Japanese national survey (Comprehensive Survey of Living Conditions) cover ages 6 and above. WG’s set of six questions on disability is a relatively new health measure, so they have not yet been used as measures for examining trends in disability for a population. The use of these questions in censuses and surveys seems to be promising, but, again, they may not be applicable to certain age groups. Recently, a census conducted in Vietnam asked questions on WG’s set of questions to those aged 5 and above. ADLs and IADLs are often used as health measures in health expectancy research and may be good health measures for examining the health status of older adults. However, these measures may not be good for an entire population. A disease-based GBD approach covers the entire population. Monitoring population health through the morbidity load (prevalence of diseases and various health conditions) raises several issues. Indeed, changes in disease prevalence may be caused by advances in medical technology leading to earlier diagnoses or reducing the lethality of specific morbid conditions, such as stroke. Stroke incidence may remain unchanged but prevalence can increase because survival after stroke is improved. Note that over time, many factors impacting the knowledge and reporting of diseases are changing, i.e., health literacy, number of medical contacts, level of expectation, etc. Prevalence measures of population health using the Sullivan method are affected by these factors to some extent. Functional health status is not impacted to the same extent by these changing factors, although environmental modifications can impact the level of activity.
If we are interested in differences in health expectancy across countries, we have to find comparable health measures. Differences and similarities across countries in the concept of health have to be carefully examined. Apparently, identical questions may not mean the same to people across countries, and the response pattern may also differ by countries independently of actual health differences. Therefore, translation of questions should be conducted with caution if languages used differ among countries under study. Differences in the response pattern to questions on self-rated general health have been noted with North American and European Nordic people tending more often to answer being in good health, the European Mediterranean people tending more often to report being in poor health, and the Japanese people tending more often to report being in the middle of the response categories [39]. Protocols for scientific translations of self-perceived health (SPH) questions in all European languages can limit these issues but cannot eliminate them. However, questions on activity limitations, such as the GALI in Europe, are thought to be less sensitive to cultural factors. ADLs and IADLs could be used in cross-country comparative studies. For such studies, we must pay attention to the wording of questions, to the set of activities proposed, and to the response categories. The meaning of toileting may be the same, but the relative difficulty of toileting may differ considerably depending on whether a sitting or squatting toilet is used. Eating is another example. For those who are accustomed to using chop-sticks for eating meals as a part of their culture, fork and spoon might be seen as assistive devices. Differences in health insurance systems, health utilization, and levels of medical technologies may strongly impact knowledge and reporting of diseases and the known prevalence of morbidity.
The Sullivan method has been used in almost all health expectancy research dealing with time trends studies and cross country comparisons. This is partly because population health measures, repeatedly available and/or internationally comparable, mainly came from censuses and cross-sectional surveys. In addition, health expectancy can be used to examine health inequality among a country’s sub populations such as by sex, by region, by race/ethnicity, and/or by socioeconomic status. The Sullivan method has often been used for this purpose. However, the Sullivan method has its limitations for this purpose because the method requires matching life tables by sub populations of interest. Life tables are often available by sex, by region, and/or race/ethnicity for many countries in the world, but it is rare to find life tables, for instance, by education, by income, or by occupation.
Panel/longitudinal surveys have been used for health expectancy research on differences in health among sub populations by applying multistate life table methods. By using panel/longitudinal surveys, transition schedules including mortality schedules can be computed for a wide variety of covariates assumed to affect the transition outcomes. Some of these could be lifelong characteristics of individuals (e.g. sex and race/ethnicity) and others could be time-varying characteristics (e.g. education and marital status).
7.2. Which method to use
The Sullivan method has been used only when cross-sectional data along with life tables are available to compute health expectancy. While censuses cover entire populations, many sample surveys often exclude institutionalized populations. The effects of computing health expectancy without paying attention to institutionalized populations may be negligible in countries with very small institutionalized populations, but the effects may be very large in countries with large institutionalized populations. For instance, the treatment of institutionalized populations was handled differently from the original Sullivan method in studies by Wilkins and Adams [50] and Crimmins [4].
If panel/longitudinal survey data are available, we have a choice of methods for computing health expectancy including the Sullivan method and multistate life table methods. One of the advantages of using panel/longitudinal survey data for computing health expectancy is that it is possible to construct life tables according to the characteristics of interest among the sample populations. If the number of transitions among health states in the sample population is relatively small, the Sullivan method can be used to combine the constructed life tables with prevalence measures of health in the survey to compute health expectancy. Or, one can simply apply multistate life table methods or other methods of computing health expectancy which require panel/longitudinal survey data. One disadvantage of these methods is the necessity of a large sample size for computing health expectancy. Sample attrition is also an issue for these longitudinal approaches.
On the one hand, health expectancy computed with the Sullivan method reflects the current health composition of a real population adjusted for current mortality levels. But, the results of the Sullivan method are limited in that they indicate nothing about the expected life cycle events of individuals exposed to current morbidity conditions. On the other hand, health expectancy computed by multistate life table methods is a summary measure of expected health for members of a synthetic cohort who live all of their remaining life exposed to current conditions of mortality and morbidity. Therefore, this measure provides a strong indication of the impact of current transition rates for individual life cycles and population. However, health expectancy derived from multistate methods does not indicate the current population distribution of health status. Health expectancies computed with population-based multi-state life table methods can be identical to those computed with the Sullivan method only when the population under study is a stable population from a demographic and an epidemiological perspective.
Many countries have repeated cross-sectional health surveys designed to provide regular estimates of population health composition. The Sullivan method has been used to compute health expectancy which indicates population health composition. However, In order to fully understand the health processes that reflect the outlook for individual lives and the implications of current conditions for future changes in population health structure, countries need to collect panel/longitudinal data that will allow them to compute incidence-based health expectancy, not just for estimating life expectancy but also for understanding the processes that affect it. In both cases special attention should be given to institutionalized populations often excluded from surveys.
7.3. Whether weights should be used
What we discuss here are not sampling weights but values of life in different health states. A number of attempts have been made to use the Sullivan method along with weighting factors to estimate a global indicator of health expectancy where some health-states years are not valued as a whole year but are weighted as to their value relative to a year of “perfect” health [50, 107]. Members of REVES have discussed at some length the weighting systems used in the work of Torrance [108] and in the Global Burden of Disease project [109,110]. These discussions have clarified that the weighting system is closely related to the estimates of healthy life and that the derivation of weights is a highly controversial topic. Questions have arisen not only about how to derive weights methodologically but also about whose views should be used to weight the value of life years – questions that have no agreed upon answers. Murray [111] added another dimension to the issue of weights, that is age weighting. The value of a year of life lived at different ages varies with the peek at around age 20. Essentially, what this means is that the value of life lived by babies or older adults is less than the value of life lived by adults at age 20. One should be aware that these kinds of weights may be applied in computing health expectancy. The meaning of health expectancy computed with such weights has to be carefully considered.
7.4. The necessary number of summary measures
The last issue we would like to discuss is how many summary measures of population health we need and whether it is possible to operationalize the WHO’s definition of health, that is physical, mental, and social well-being. Molla and colleagues [112] suggest that multiple indicators of population health based on health expectancy are needed. The supporting materials [113] of the health promotion guideline announced in 2012 by the Ministry of Health, Labor and Welfare of Japan called “Health Japan 21 (2nd edition)” suggest paying attention not only to healthy life expectancy based on activity limitations but also to self-rated general health. Given that health is a multifaceted concept, we may need to have more than one population health measure. We may also need to pay attention to specific age groups in a population by computing partial healthy life expectancy [37,114] instead of simply computing healthy life expectancy at birth.
8. Conclusion
Health expectancy is an essential population health indicator as well as a life cycle indicator. As the then Director-General of WHO stated in the mid 1990’s, “Increased longevity without quality of life is an empty prize. Health expectancy is more important than life expectancy” [79]. However, we should keep in mind that values of health expectancy vary by definition, measures of health, and methods of calculation. We should also note that the proportion of healthy life expectancy to total life expectancy is an important indicator of population health as well. The length of both healthy life expectancy and total life expectancy could increase, but the proportion of healthy life expectancy could decrease. Making length of healthy life expectancy alone the target of health policy may not achieve the intended goal.
Because health expectancy is an indicator of population health, we can monitor changes and/or assess differences in population health. However, we have to further understand what factors affect these changes and differences. Even if we identify the factors affecting such changes and differences, such as education, we need to examine what are the mechanisms involving these factors while impacting health expectancy. Otherwise, we will not be able to suggest ways to improve population health.
Acknowledgments
The earlier version of this study was presented at the 59th World Statistics Congress in Hong Kong, August 25–30, 2013. This study was supported by Japan Society for the Promotion of Science (Grant-in-Aid for Scientific Research 25293121).
Footnotes
REVES is the French acronym for the International Network on Health Expectancy and the Disablement Process (Réseau Espérance de Vie en Santé). Information on health expectancy and REVES can be found at the following URL: http://reves.site.ined.fr/en/.
The original version was published in 1971. Full citation for the book is Shryock, H., J. Siegel and Associates, 1971. The Methods and Materials of Demography. Washington, DC: U.S. Census Bureau/U.S. Government Print Office.
References
- 1.Robine J-M, Jagger C, Mathers CD, Crimmins EM, Richard MS, editors. Determining Health Expectancies. John Wiley & Sons Ltd; England: 2003. [Google Scholar]
- 2.Siegel JS, Swanson DA, editors. The Methods and Materials of Demography. 2. Elsevier, Academic Press; San Diego: 2004. [Google Scholar]
- 3.Sullivan DF. A single Index of mortality and morbidity. HSMHA Health Reports. 1971;86:347–354. [PMC free article] [PubMed] [Google Scholar]
- 4.Crimmins EM, Saito Y, Ingegneri D. Changes in life expectancy and disability-free expectancy in the United States. Population and Development Review. 1989;15:235–267. [Google Scholar]
- 5.Katz S, Branch LG, Branson MN, Papsidero JA, Beck JC, Greer DS. Active life expectancy. New England Journal of Medicine. 1983;309:1218–1224. doi: 10.1056/NEJM198311173092005. [DOI] [PubMed] [Google Scholar]
- 6.Yong V, Saito Y. Are there education differentials in disability and mortality transitions and active life expectancy among Japanese older adults? Findings from a 10-year prospective cohort study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2012;67:343–353. doi: 10.1093/geronb/gbs029. [DOI] [PubMed] [Google Scholar]
- 7.Jagger C, Gillies C, Moscone F, Cambois E, Van Oyen H, Nusselder W, Robine J-M the EHLES team. Inequalities in healthy life years in the 25 countries of the European Union in 2005: A cross-national meta-regression analysis. Lancet. 2008;372:2124–2131. doi: 10.1016/S0140-6736(08)61594-9. [DOI] [PubMed] [Google Scholar]
- 8.Doblhammer G, Kytir J. Compression or expansion of morbidity? Trends in healthy life expectancy in the elderly Austrian population between 1978 and 1998. Social Science and Medicine. 2001;52:385–391. doi: 10.1016/s0277-9536(00)00141-6. [DOI] [PubMed] [Google Scholar]
- 9.Wood R, Sutton M, Clark D, McKeon A, Bain M. Measuring inequalities in health: the case for healthy life expectancy. Journal of Epidemiology and Community Health. 2006;60:1089–1092. doi: 10.1136/jech.2005.044941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yong V, Saito Y. Trends in healthy life expectancy in Japan: 1986–2004. Demographic Research. 2009;20:467–494. [Google Scholar]
- 11.Sanders B. Measuring community health level. American Journal of Public Health. 1964;54:1063–1970. doi: 10.2105/ajph.54.7.1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sullivan DF. Conceptual Problems in Developing an Index of Health, Vital and Health Statistics. 17. National Centre for Health Statistics; Washington, DC: 1966. Series 2. [PubMed] [Google Scholar]
- 13.Fries J. Aging, natural health, and the compression of morbidity. New England Journal of Medicine. 1980;303:130–135. doi: 10.1056/NEJM198007173030304. [DOI] [PubMed] [Google Scholar]
- 14.Gruenberg EM. The failures of success. Milbank Memorial Fund Quarterly. 1977;55:3–24. [PubMed] [Google Scholar]
- 15.Kramer K. The rising pandemic of mental disorders and associated chronic diseases and disabilities. Acta Psychiatrica Scandinavica. 1980;62:382–397. [Google Scholar]
- 16.Madans JH, Loeb ME, Altman BA. Measuring disability and monitoring the UN Convention on the Rights of Persons with Disabilities: The work of the Washington Group on Disability Statistics. BMC Public Health. 2011;11:S4. doi: 10.1186/1471-2458-11-S4-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robine J-M, Jagger C Euro-REVES Group. Creating a coherent set of indicators to monitor health across Europe: The Euro-REVES 2 project. European Journal of Public Health. 2003;13:6–14. doi: 10.1093/eurpub/13.suppl_1.6. [DOI] [PubMed] [Google Scholar]
- 18.Van Oyen H, Heyden JD, Perenboom R, Jagger C. Monitoring population disability: evaluation of a new Global Activity Limitation Indicator (GALI) Soz Praventivmed. 2006;51:153–161. doi: 10.1007/s00038-006-0035-y. [DOI] [PubMed] [Google Scholar]
- 19.WHO. Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference; New York. 19–22 June, 1946; signed on 22 July 1946 by the representatives of 61 States (Official Records of the World Health Organization, no. 2, p. 100) and entered into force on 7 April, 1948. [Google Scholar]
- 20.Wood PHN. Classification of impairments and handicaps. WHO; Geneva: 1975. (WHO/ICD 9/REV. CONF/75.15) [Google Scholar]
- 21.Nagi SZ. An epidemiology of disability among adults in the United States. The Milbank Memorial Fund Quarterly. Health and Society. 1976;54:439–467. [PubMed] [Google Scholar]
- 22.Nagi SZ. Disability concepts revisited: implication for prevention. In: Pope AM, Tarlov AR, editors. Disability in America: Toward a National Agenda for Prevention. National Academy Press; Washington, DC: 1991. [Google Scholar]
- 23.Verbrugge LM, Jette AM. The disablement process. Social Science and Medicine. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 24.World Health Organization. International classification of impairments, disabilities, and handicaps: A manual of classification relating to the consequences of disease. WHO; Geneva: 1980. [Google Scholar]
- 25.World Health Organization. International classification of functioning, disability and health: ICF. Geneva: WHO; 2001. [Google Scholar]
- 26.Crimmins EM, Kim JK, Vasunilashorn S. Biodemography: new approaches to understanding trends and differences in population health and mortality. Demography. 2010;47S:S41–S64. doi: 10.1353/dem.2010.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Crimmins EM, Seeman T. Committee on Population, editor. Integrating biology into demographic research on health and aging. In: Finch CE, Vaupel JW, Kinsella K, editors. Cells and Surveys: Should Biological Measures be Included in Social Science Research? Commission on Behavioral and Social Sciences and Education; Washington, D.C: National Academy Press; 2000. [Google Scholar]
- 28.Idler EL, Benyami Y. Self rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- 29.Benjamins MR, Hummer RA, Eberstein IW, Nam CB. Self-reported health and adult mortality risk: An analysis of cause-specific mortality. Social Science and Medicine. 2004;59:1297–1306. doi: 10.1016/j.socscimed.2003.01.001. [DOI] [PubMed] [Google Scholar]
- 30.Lyyra TM, Heikkinen E, Lyyra AL, Jylha M. Self-rated health and mortality: Could clinical and performance-based measures of health and functioning explain the association? Archives of Gerontology and Geriatrics. 2006;42:277–288. doi: 10.1016/j.archger.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 31.DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Clinical review: Mortality prediction with a single general self-rated health question. Journal of General Internal Medicine. 2006;21:267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miller TR, Wolinsky FD. Self-rated health trajectories and mortality among older adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2007;62B:S22–S27. doi: 10.1093/geronb/62.1.s22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization. Health interview surveys: towards international harmonization of methods and instruments. World Health Organization Regional Office for Europe; Copenhagen: 1996. [PubMed] [Google Scholar]
- 34.Groenewegen PP, Westert GP, Boshuizen HC. Regional differences in healthy life expectancy in the Netherlands. Public Health. 2003;117:424–429. doi: 10.1016/S0033-3506(03)00100-8. [DOI] [PubMed] [Google Scholar]
- 35.Wood R, Sutton M, Clark D, McKeon A, Bain M. Measuring inequalities in health: the case for healthy life expectancy. Journal of Epidemiology and Community Health. 2006;60:1089–1092. doi: 10.1136/jech.2005.044941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ofstedal MB, Zimmer Z, Cruz G, Chan A, Chuang YL. Self-assessed health expectancy among older adults: A comparison of six Asian settings. Hallym International Journal of Aging. 2004;6:95–117. [Google Scholar]
- 37.Minagawa Y. Inequalities in healthy life expectancy in Eastern Europe. Population and Development Review. 2013;39:649–671. [Google Scholar]
- 38.Jürges H, Avendano M, Mackenbach JP. Are different measures of self-rated health comparable? An assessment in five European countries. European Journal of Epidemiology. 2008;23:773–781. doi: 10.1007/s10654-008-9287-6. [DOI] [PubMed] [Google Scholar]
- 39.Organization for Economic Co-operation and Development. Self-rated general health: progress in data collection and developmental work to improve data comparability. DELSA/HEA/HD(2013)4. [Google Scholar]
- 40.Murray CJL, Lopez AD, editors. The global burden of disease. Harvard School of Public Health, Harvard University Press; 1996. [Google Scholar]
- 41.Solomon JA, Wang H, Freeman MK, Vos T, Flaxman AD, Lopez AD, Murray CJL. Healthy life expectancy for 187 counties, 1990–2010: A systematic analysis for the global burden of disease study 2010. Lancet. 2012;380:2144–2162. doi: 10.1016/S0140-6736(12)61690-0. [DOI] [PubMed] [Google Scholar]
- 42.Crimmins EM, Hayward MD, Ueda H, Saito Y, Kim JK. Life with and without heart disease among women and men over 50. Journal of Women & Aging. 2008;20:5–19. doi: 10.1300/j074v20n01_02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hout AVD, Matthews FE. Estimating stroke-free and total life expectancy in the presence of non-ignorable missing values. Journal of the Royal Statistical Society: Series A (Statistics in Society) 2010;173:331–349. doi: 10.1111/j.1467-985X.2009.00610.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ritchie K, Robine J-M, Letenneur L, Dartigues JF. Dementia-free life expectancy in France. American Journal of Public Health. 1994;84:232–236. doi: 10.2105/ajph.84.2.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yong V, Gu D, Chen M, Saito Y. Expected lifetime with and without cataract among older adults in China. Journal of Population Ageing. 2011;4:65–79. [Google Scholar]
- 46.Pérès K, Jagger C, Matthews FE MRC CFAS. Impact of late-life self-reported emotional programs on disability-free life expectancy: results from the MRC Cognitive Function and Ageing Study. International Journal of Geriatric Psychiatry. 2008;23:643–649. doi: 10.1002/gps.1955. [DOI] [PubMed] [Google Scholar]
- 47.Matthews FE, Jagger C, Miller LL, Brayne C MRC CFAS. Education differences in life expectancy with cognitive impairment. Journals of Gerontology, Series A, Biological Sciences and Medical Sciences. 2009;64:125–131. doi: 10.1093/gerona/gln003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lièvre A, Alley D, Crimmins EM. Educational differentials in life expectancy with cognitive impairment among the elderly in the United States. Journal of Aging and Health. 2008;20:456–477. doi: 10.1177/0898264308315857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mathers CD. Australia Institute of Health: Health Differentials Series. 1. 1990. Disability-Free and Handicap-Free Life Expectancy in Australia. [Google Scholar]
- 50.Wilkins R, Adams OB. Health expectancy in Canada, late 1970s: demographic, regional, and social dimensions. American Journal of Public Health. 1983;73:1073–1080. doi: 10.2105/ajph.73.9.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lieu J, Chen C, Song X, Chi I, Zheng S. Trends in disability-free life expectancy among Chinese older adults. Journal of Aging and Health. 2009;21:266–285. doi: 10.1177/0898264308328978. [DOI] [PubMed] [Google Scholar]
- 52.Colvez A, Robine J-M. L’esperance de vie sans incapacite en France en 1982. Population. 1986;41:1025–1042. [Google Scholar]
- 53.Hashimoto S, Kawado M, Seko R, Murakami Y, Hayashi M, Kato M, Noda T, Ojima T, Nagai M, Tsuji I. Trends in disability-free life expectancy in Japan, 1995–2004. Journal of Epidemiology. 2010;20:308–312. doi: 10.2188/jea.JE20090190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bebbington AC. The expectation of life without disability in England and Wales. Social Science and Medicine. 1988;27:321–326. doi: 10.1016/0277-9536(88)90265-1. [DOI] [PubMed] [Google Scholar]
- 55.Bebbington AC. The expectation of life without disability in England and Wales: 1976–88. Population Trends. 1991;66:26–29. doi: 10.1016/0277-9536(88)90265-1. [DOI] [PubMed] [Google Scholar]
- 56.Crimmins EM, Saito Y, Ingegneri D. Trends in disability-free life expectancy in the United States, 1970–1990. Population and Development Review. 1997;23:555–572. [Google Scholar]
- 57.Crimmins EM, Saito Y. Trends in healthy life expectancy in the United States, 1970–1990: gender, racial, and education. Social Science & Medicine. 2001;52:1629–1641. doi: 10.1016/s0277-9536(00)00273-2. [DOI] [PubMed] [Google Scholar]
- 58.Jagger C, Gillies C, Cambois E, Van Oyen H, Nusselder W, Robine J-M the EHLEIS Team. The Global Activity Limon and disabilitation Index measured function and disability similarly across European countries. Journal of Clinical Epidemiology. 2010;63:892–899. doi: 10.1016/j.jclinepi.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 59.Jagger C, McKee M, Christensen K, Lagiewka K, Nusselder W, Van Oyen H, Cambois E, Jeune B, Robine J-M. Mind the gap – reaching the European target of a 2-year increase in healthy life years in the next decade. European Journal of Public Health. 2013;23:829–833. doi: 10.1093/eurpub/ckt030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tareque MI, Begum S, Saito Y. Gender differences in disability-free life expectancy at old ages in Bangladesh. Journal of Aging and Health. 2013;25:1299–1312. doi: 10.1177/0898264313501388. [DOI] [PubMed] [Google Scholar]
- 61.Nguyen LT, Saito Y, Phan HTM, Nguyen LTN. Health expectancy and its variations in Vietnam. Paper presented at REVES meeting; Taichung, Taiwan. 2012. [Google Scholar]
- 62.Katz S, Ford A, Moskowitz R, Jackson B, Jaffe M. Studies of illness in the aged: the index of ADL: A standardized measure of biological and psychosocial function. The Journal of the American Medical Association. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 63.Lawton M, Brody E. Assessment of older people: self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 64.Spector W, Fleishman J. Combining activities of daily living with instrumental activities of daily living to measure functional disability. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 1998;53:46–57. doi: 10.1093/geronb/53b.1.s46. [DOI] [PubMed] [Google Scholar]
- 65.Gu D, Zeng Y. Sociodemographic effects on the onset and recovery of ADL disability among Chinese oldest-old. Demographic Research. 2004;11:1–42. [Google Scholar]
- 66.Hidajat MM, Hayward MD, Saito Y. Indonesia’s social capacity for population health: the educational gap in active life expectancy. Population Research and Policy Review. 2007;26:219–234. [Google Scholar]
- 67.Liu X, Liang J, Muramatsu N, Sugisawa H. Transitions in functional status and active life expectancy among older people in Japan. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 1995;50:383–394. doi: 10.1093/geronb/50b.6.s383. [DOI] [PubMed] [Google Scholar]
- 68.Cruz GT, Saito Y, Natividad J. Active life expectancy and functional health status among Filipino older people. Canadian Studies in Population. 2007;34:29–47. [Google Scholar]
- 69.Jagger C, Goyder E, Clarke M, Brouard N, Arthur A. Active life expectancy in people with and without diabetes. Journal of Public Health. 2003;25:42–46. doi: 10.1093/pubmed/fdg009. [DOI] [PubMed] [Google Scholar]
- 70.Guralnik J, Land K, Blazer D, Fillenbaum G, Branch L. Educational status and active life expectancy among older blacks and whites. American Journal of Epidemiology. 1993;329:110–116. doi: 10.1056/NEJM199307083290208. [DOI] [PubMed] [Google Scholar]
- 71.Crimmins EM, Hayward MD, Saito Y. Differentials in active life expectancy in the older population of the United States. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 1996;51:111–120. doi: 10.1093/geronb/51b.3.s111. [DOI] [PubMed] [Google Scholar]
- 72.Hayward MD, Crimmins EM, Saito Y. Cause of death and active life expectancy in the older population of the United States. Journal of Aging and Health. 1998;10:192–213. [Google Scholar]
- 73.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiner J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA for the Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: Evidence for a phenotype. Journal of Gerontology: Medical Sciences. 2001;56A:M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 74.Romano-Ortuno R, Fouweather T, Jagger C. Cross-national disparities in sex differences in life expectancy with and without frailty. Age and Ageing. 2014;43:222–228. doi: 10.1093/ageing/aft115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Deeg DJH, Puts MTE. Frailty free life expectancy in the older population: The Netherlands. paper presented at the 25th REVES meeting; Austin, Texas, USA. 2013. [Google Scholar]
- 76.Seko R, Hashimoto S, Kawado M, Murakami Y, Hayashi M, Kato M, Noda T, Ojima T, Nagai M, Tsuji I. Trends in life expectancy with care needs based on long-term care insurance data in Japan. Journal of Epidemiology. 2012;22:238–243. doi: 10.2188/jea.JE20110069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rogers A, Rogers R, Branch LG. A multistate analysis of active life expectancy. Public Health Reports. 1989;104:222–226. [PMC free article] [PubMed] [Google Scholar]
- 78.Manton KG, Stallard E, Liu K. Forecasts of active life expectancy: policy and fiscal implications. The Journal of Gerontology. 1993;48:11–26. doi: 10.1093/geronj/48.special_issue.11. [DOI] [PubMed] [Google Scholar]
- 79.Wolf DA, Laditka SB. Papers in Microsimulation Series Paper No. 4. Maxwell Center for Demography and Economics of Aging, Center for Policy Research, Maxwell School of Citizenship and Public Affairs, Syracuse University; New York: 1997. Stochastic modeling of active life and its expectancy. [Google Scholar]
- 80.Laditka SB, Wolf DA. New methods for modeling and calculation active life expectancy. Journal of Aging and Health. 1998;10:214–241. [Google Scholar]
- 81.Lynch SM, Brown JS, Harmsen KG. The effect of altering ADL thresholds on active life expectancy estimates for older persons. Journals of Gerontology: Social Sciences. 2003;58:S171–S178. doi: 10.1093/geronb/58.3.s171. [DOI] [PubMed] [Google Scholar]
- 82.Lynch SM, Brown JS. A new approach to estimating life tables with covariates and constructing interval estimates of life table quantities. Sociological Methodology. 2006;35:177–225. [Google Scholar]
- 83.Jagger C, Cox B, Roy SL the EHEMU team. Health expectancy calculation by the Sullivan method: A practical guide. 2007 http://www.ined.fr/fichier/t_telechargement/13746/telechargement_fichier_en_sullivan_guide_final_jun2007.pdf.
- 84.Schoen R. Constructing increment-decrement life tables. Demography. 1975;12:313–324. [PubMed] [Google Scholar]
- 85.Rogers A. Introduction to multi-regional mathematical demography. Wiley; New York: 1975. [Google Scholar]
- 86.Willekens F. Multistate analysis: tables of working life. Environment and Planning. 1980;A12:563–588. [Google Scholar]
- 87.Hayward MD, Grady WR, McLaughlin SD. Changes in the retirement process among women in the United States: changes in the 1970s. Research on Aging. 1988;10:358–382. doi: 10.1177/0164027588103004. [DOI] [PubMed] [Google Scholar]
- 88.Rogers A, Rogers RG, Branch LG. Longer life but worse health? Measurement and Dynamics. The Gerontolo-gist. 1990;30:640–649. doi: 10.1093/geront/30.5.640. [DOI] [PubMed] [Google Scholar]
- 89.Rogers RG, Rogers A, Belanger A. Active Life among the elderly in the United States: multistate life table estimates and population projections. The Milbank Memorial Fund Quarterly. 1989;67:370–411. [PubMed] [Google Scholar]
- 90.Crimmins EM, Hayward MD, Saito Y. Changing mortality and morbidity rates and the health status and life expectancy of the older population. Demography. 1994;31:159–175. [PubMed] [Google Scholar]
- 91.Rogers A, Ledent J. Increment-decrement life tables: A comment. Demography. 1976;13:287–290. [PubMed] [Google Scholar]
- 92.Schoen R, Woodrow K. Labor force status life tables for the United States, 1972. Demography. 1980;17:297–322. [PubMed] [Google Scholar]
- 93.Hayward MD, Grady WR. Work and retirement among a cohort of older men in the United States, 1966–1983. Demography. 1990;27:337–356. [PubMed] [Google Scholar]
- 94.Lièvre A, Brouard N, Heathcote C. The estimation of health expectancies from cross-longitudinal surveys. Mathematical Population Studies. 2003;10:211–248. [Google Scholar]
- 95.Crimmins EM, Saito Y. Getting better and getting worse: transitions in functional status among older Ameri-cans. Journal of Aging and Health. 1993;5:3–36. [Google Scholar]
- 96.Maddox GL, Clark DO, Steinhauser K. Dynamics of functional impairment in late adulthood. Social Science and Medicine. 1994;38:925–936. doi: 10.1016/0277-9536(94)90425-1. [DOI] [PubMed] [Google Scholar]
- 97.Cai L, Schenker N, Lubitz J. Analysis of functional status transitions by using a semi-Markov process model in the presence of left-censored spells. Journal of the Royal Statistical Society Series C (Applied Statistics) 2006;55:477–491. [Google Scholar]
- 98.Cai L, Schenker N, Lubitz J, Diehr P, Arnold A, Fried LP. Evaluation of a method for fitting a semi-Markov process model in the presence of left-censored spells using the Cardiovascular Health Study. Statistics in Medicine. 2008;27:5509–5524. doi: 10.1002/sim.3382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Willekens F, Putter H. Software for multistate analysis. Demographic Research. 2014;31:381–420. [Google Scholar]
- 100.Crimmins EM, Hayward MD, Hagedorn A, Saito Y, Brouard N. Change in Disability-Free Life Expectancy for Americans 70 Years Old and Over. Demography. 2009;40:627–646. doi: 10.1353/dem.0.0070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Weden MM. Multistate life table analysis, Programs, Examples and Supporting Documentation for lxpct_2 from Stata at Research Papers in Economics. 2005 http://ideas.repec.org/c/boc/bocode/s453001.html.
- 102.Cai L, Hayward MD, Saito Y, Lubitz J, Hagedorn A, Crimmins E. Estimation of multi-state life table functions and their variability from complex survey data using the SPACE Program. Demographic Research. 2010;22:129–158. doi: 10.4054/DemRes.2010.22.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Diehr P, Derleth A, Cai L, Newman AB. The effect of different public health interventions on longevity, morbidity, and years of healthy life. BMC Public Health. 2007:7–52. doi: 10.1186/1471-2458-7-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Payne CF, Mkandawire J, Kohler H-P. Disability transitions and health expectancies among adults 45 years and older in Malawi: A cohort-based model. Plos Medicine. 2013;10 doi: 10.1371/journal.pmed.1001435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Jackson CH. Multi-state models for panel data: the msm package for R. Journal of Statistical Package. 2011;38 [Google Scholar]
- 106.Lynch SM, Brown JS. Gibbs sampler for multistate life tables software (GSMLT v.90) 2005. [Google Scholar]
- 107.Erickson P, Wilson R, Shannon I. Years of Healthy Life. Healthy People 2000: Statistical Notes. 1995;7:1–15. doi: 10.1037/e583992012-001. [DOI] [PubMed] [Google Scholar]
- 108.Berthelot JM, Roberge R, Wolfson MC. The calculation of health-adjusted life expectancy for a Canadian Province using a multi-attribute utility function: A first attempt. In: Robine JM, Bone MR, Romieu I, editors. Calculation of Health Expectancies: Harmonization, Consensus Achieved and Future Perspectives. John Libbey Eurotext; Montrouge, France: 1993. pp. 161–174. [Google Scholar]
- 109.World Bank. World Development Report 1993: Investing in health. Oxford University Press; New York: 1993. [Google Scholar]
- 110.van Ginneken JK. Potential of the Global Burden of Disease Project for Determining Health Expectancy. In: Mathers CD, McCallum J, Robine JM, editors. Advances in Heath Expectancies. Canberra: Australian Institute of Health and Welfare; 1994. pp. 170–181. [Google Scholar]
- 111.Murray CJ. Rethinking DALYs. In: Murray, Lopez, editors. The Global Burden of Disease. Cambridge: Harvard University Press; 1996. [Google Scholar]
- 112.Molla MT, Madans JH, Wagener DK, Crimmins EM. Summary measures of population health: Report of findings on methodologic and data issues. National Center for Health Statistics; Hyattsville, Maryland: 2003. [Google Scholar]
- 113.Ministry of Health, Labor and Welfare. Supporting materials for “Health Japan 21 (2nd edition)”. 2012 http://www.mhlw.go.jp/bunya/kenkou/dl/kenkounippon21_02.pdf.
- 114.Cambois E, Blachier A, Robine J-M. Aging and health in France: An unexpected expansion of disability in mid-adulthood over recent years. European Journal of Public Health. 2013;23:575–581. doi: 10.1093/eurpub/cks136. [DOI] [PubMed] [Google Scholar]