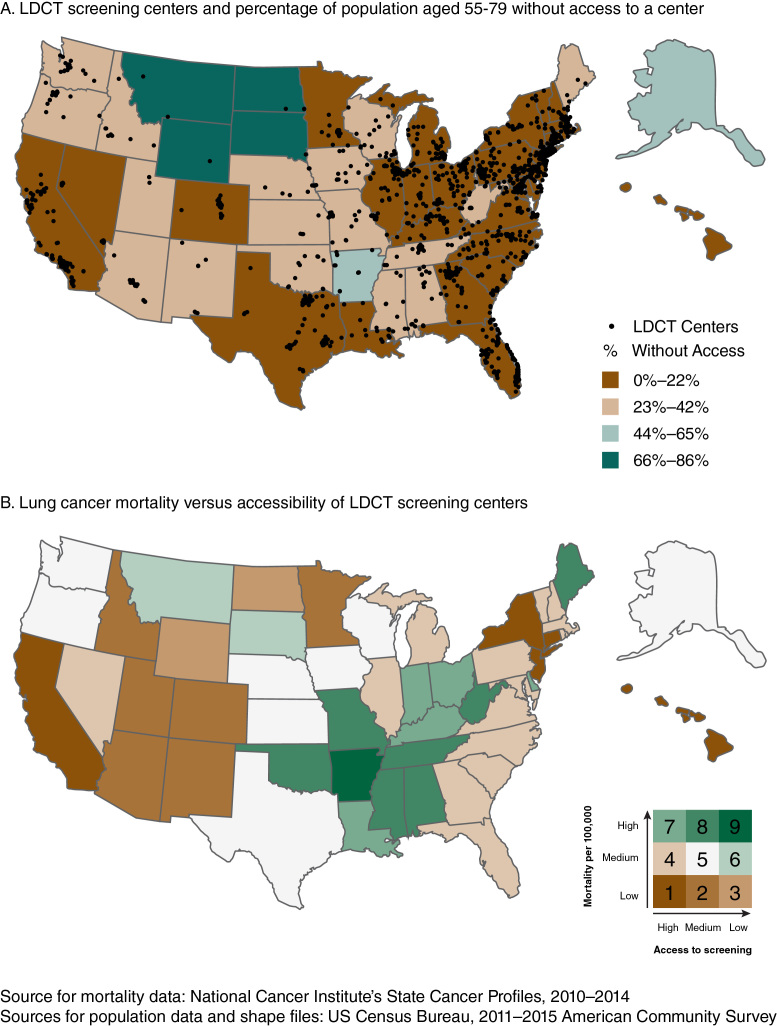
Panel A. Location of low-dose computed tomography (LDCT) screening centers in the United States and percentage of US population aged 55 to 79 who live without access to a screening center within 30 miles. Symbol indicates location of a LDCT screening center. Panel B. Lung cancer mortality per 100,000 persons and percentage of US population aged 55 to 79 without access to a screening center within 30 miles. Mortality and accessibility scores were classified into 3 groups (low, medium, high), each based on the natural breaks method, and combined for bivariate mapping: 1) high mortality/high access, 2) high mortality/medium access, 3) high mortality/low access, 4) medium mortality/high access, 5) medium mortality/medium access, 6) medium mortality/low access, 7) low mortality/high access, 8) low mortality/ medium access, and 9) low mortality/low access. These maps highlight state-level variation in LDCT screening availability and accessibility, as well as lung cancer mortality among persons of LDCT screening age. The maps help identify areas in need of LDCT screening program creation and/or expansion, particularly in rural areas.
| Panel A. State Name (Including District of Columbia) | No. of Centers | Lung Cancer Mortality Per 100,000 Persons | Proportion of Population Aged 55-79 Outside 30-Mile Buffer, % |
|---|---|---|---|
| Alabama | 23 | 55.5 | 31 |
| Alaska | 3 | 47.6 | 49 |
| Arizona | 22 | 36.1 | 23 |
| Arkansas | 10 | 60.1 | 52 |
| California | 109 | 33.4 | 8 |
| Colorado | 33 | 31.7 | 20 |
| Connecticut | 40 | 39.4 | 0 |
| Delaware | 20 | 51.1 | 0 |
| District of Columbia | 3 | 40.3 | 0 |
| Florida | 114 | 43.8 | 5 |
| Georgia | 53 | 47.7 | 14 |
| Hawaii | 5 | 32.1 | 17 |
| Idaho | 9 | 37.0 | 38 |
| Illinois | 55 | 47.6 | 11 |
| Indiana | 45 | 55.1 | 11 |
| Iowa | 15 | 46.0 | 34 |
| Kansas | 9 | 46.6 | 38 |
| Kentucky | 49 | 69.6 | 13 |
| Louisiana | 21 | 55.1 | 12 |
| Maine | 6 | 52.5 | 33 |
| Maryland | 49 | 43.2 | 1 |
| Massachusetts | 57 | 43.7 | 2 |
| Michigan | 54 | 49.8 | 13 |
| Minnesota | 21 | 39.7 | 21 |
| Mississippi | 9 | 58.8 | 42 |
| Missouri | 28 | 55.3 | 27 |
| Montana | 2 | 41.2 | 82 |
| Nebraska | 11 | 43.1 | 32 |
| Nevada | 16 | 46.6 | 12 |
| New Hampshire | 10 | 46.2 | 15 |
| New Jersey | 81 | 39.8 | 0 |
| New Mexico | 4 | 31.6 | 42 |
| New York | 143 | 40.1 | 5 |
| North Carolina | 64 | 50.7 | 8 |
| North Dakota | 3 | 40.2 | 78 |
| Ohio | 78 | 52.8 | 7 |
| Oklahoma | 8 | 56.5 | 34 |
| Oregon | 18 | 44.0 | 27 |
| Pennsylvania | 134 | 46.4 | 1 |
| Rhode Island | 17 | 48.8 | 0 |
| South Carolina | 30 | 50.4 | 12 |
| South Dakota | 2 | 43.9 | 74 |
| Tennessee | 34 | 58.6 | 27 |
| Texas | 101 | 40.6 | 21 |
| Utah | 3 | 20.0 | 33 |
| Vermont | 5 | 47.1 | 17 |
| Virginia | 58 | 45.5 | 14 |
| Washington | 31 | 42.2 | 22.5 |
| West Virginia | 14 | 60.3 | 29 |
| Wisconsin | 18 | 44.2 | 32 |
| Wyoming | 1 | 36.7 | 86 |
| Panel B. State Name (Including District of Columbia) | State Mortality and Access Classification | Legend Reference |
|---|---|---|
| Delaware | High Mortality/High Access | 7 |
| Indiana | High Mortality/High Access | 7 |
| Kentucky | High Mortality/High Access | 7 |
| Louisiana | High Mortality/High Access | 7 |
| Ohio | High Mortality/High Access | 7 |
| Alabama | High Mortality/Medium Access | 8 |
| Mississippi | High Mortality/Medium Access | 8 |
| Missouri | High Mortality/Medium Access | 8 |
| Oklahoma | High Mortality/Medium Access | 8 |
| Tennessee | High Mortality/Medium Access | 8 |
| West Virginia | High Mortality/Medium Access | 8 |
| Maine | High Mortality/Medium Access | 8 |
| Arkansas | High Mortality/Low Access | 9 |
| Florida | Medium Mortality/High Access | 4 |
| Georgia | Medium Mortality/High Access | 4 |
| Illinois | Medium Mortality/High Access | 4 |
| Maryland | Medium Mortality/High Access | 4 |
| Massachusetts | Medium Mortality/High Access | 4 |
| Michigan | Medium Mortality/High Access | 4 |
| Nevada | Medium Mortality/High Access | 4 |
| New Hampshire | Medium Mortality/High Access | 4 |
| North Carolina | Medium Mortality/High Access | 4 |
| Pennsylvania | Medium Mortality/High Access | 4 |
| Rhode Island | Medium Mortality/High Access | 4 |
| South Carolina | Medium Mortality/High Access | 4 |
| Vermont | Medium Mortality/High Access | 4 |
| Virginia | Medium Mortality/High Access | 4 |
| Alaska | Medium Mortality/Medium Access | 5 |
| Iowa | Medium Mortality/Medium Access | 5 |
| Kansas | Medium Mortality/Medium Access | 5 |
| Nebraska | Medium Mortality/Medium Access | 5 |
| Oregon | Medium Mortality/Medium Access | 5 |
| Texas | Medium Mortality/Medium Access | 5 |
| Washington | Medium Mortality/Medium Access | 5 |
| Wisconsin | Medium Mortality/Medium Access | 5 |
| Montana | Medium Mortality/Low Access | 6 |
| South Dakota | Medium Mortality/Low Access | 6 |
| California | Low Mortality/High Access | 1 |
| Connecticut | Low Mortality/High Access | 1 |
| District of Columbia | Low Mortality/High Access | 1 |
| Hawaii | Low Mortality/High Access | 1 |
| New Jersey | Low Mortality/High Access | 1 |
| New York | Low Mortality/High Access | 1 |
| Minnesota | Low Mortality/Medium Access | 2 |
| Arizona | Low Mortality/Medium Access | 2 |
| Colorado | Low Mortality/Medium Access | 2 |
| Idaho | Low Mortality/Medium Access | 2 |
| New Mexico | Low Mortality/Medium Access | 2 |
| Utah | Low Mortality/Medium Access | 2 |
| North Dakota | Low Mortality/Low Access | 3 |
| Wyoming | Low Mortality/Low Access | 3 |
Background
Lung cancer is the leading cause of cancer-related death among men and women in the United States, with more than 234,000 persons diagnosed yearly (1). Most diagnoses are made at a late stage when the cancer is more difficult to treat (1). Until 2011, there was not broad evidence that any one type of screening reduced lung cancer mortality. However, the National Lung Screening Trial clearly demonstrated that annual low-dose computed tomography (LDCT) can reduce lung cancer deaths by up to 20% in high-risk populations (ie, people aged 55–74 y who have a ≥30-pack-year smoking history and who, if former smokers, had quit within the previous 15 years) (2). Subsequently, in 2014, the US Preventive Services Task Force (USPSTF) (3) endorsed LDCT screening for high-risk persons, resulting in changes to the reimbursement policies of private and public insurers.
Despite endorsements and new reimbursement policies favoring LDCT screening, uptake is low among high-risk persons (3.9% based on the 2015 National Health Interview Survey) (4). In 2014, we showed that the United States had 203 active LDCT screening centers and that most were in the Northeast and the East North Central states (5). In 2015, the Centers for Medicare & Medicaid Services introduced insurance coverage and associated billing codes for LDCT screening. An updated assessment of the landscape of LDCT screening in the United States is now needed to determine the extent of geographic variation in LDCT screening availability and to identify regions for program expansion based on potential demand.
Methods
In January 2017, we obtained the names and locations of LDCT screening centers that meet/attest to quality standards set by the Lung Cancer Alliance (ie, Screening Centers of Excellence) and/or the American College of Radiology (ie, ACR Designated Lung Cancer Screening Centers). The business addresses of each LDCT screening center was geocoded using Esri’s World Geocoding Service and ArcGIS Desktop version 10.2.
The primary geographic unit was the census block group. Block groups were classified as urban or rural areas according to 2010 Rural–Urban Commuting Area (RUCA) codes established by the US Department of Agriculture’s Economic Research Service. Each block group was assigned an urban or rural designation according to whether its centroid (ie, geographic center of a polygon) was inside the census-tract boundaries in which it was nested. RUCA codes of 1, 2, and 3 were categorized as urban, and codes 4 through 10 were categorized as rural. We used population estimates for the number of persons aged 55 to 79 to approximate the USPSTF-recommended screening age (ie, 55–80 y). We obtained population estimates at the block group level from the US Census Bureau’s Integrated Public Use Microdata Series, specifying data from the 2011–2015 American Community Survey (6).
Data on state lung cancer mortality rates (aggregated data from 2010 through 2014), extracted from the National Cancer Institute’s State Cancer Profiles website (7), were overlaid with data on LDCT screening center locations to determine whether areas of high need had equitable access to services. We measured spatial accessibility to screening by using a 30-mile Euclidean distance buffer (ie, a circle around a point 30 miles in any direction) to identify the number of persons aged 55 to 79 who reside within and outside the facility catchment area. A centroid was created for each block group and was assigned a corresponding block group population. To calculate the population residing within and outside of each buffer, we assumed that if a census block group’s centroid was inside the 30-mile buffer, then the population in that block group would have access to that screening center. We aggregated block group estimates to compute accessibility for all 50 states and the District of Columbia and by level of rurality (urban or rural). For the first map, the proportion of persons aged 55 to 79 without access to a designated LDCT screening center within 30 miles was categorized into 4 groups in equal intervals; the breaks occurred at 22%, 43%, and 65%. For a second map, lung cancer mortality and accessibility scores were classified into 3 groups by using the natural breaks method. For lung cancer mortality, these groups were classified as low (20.0 to 40.3 deaths per 100,000), medium (40.6 to 50.7 deaths per 100,000), and high (51.1 to 69.6 deaths per 100,000). For accessibility, the groups were classified as low (51%–86%), medium (20%–48%), and high (0%–17%). These categories resulted in 9 combinations of lung cancer mortality and accessibility, presented in bivariate map format. Finally, we performed a sensitivity analysis to examine accessibility based on a 30-minute driving distance.
Main Findings
The number of designated LDCT screening centers increased from an estimated 203 in 2014 to 1,748 in early 2017. The mean number of designated LDCT screening centers per state was 34. Nine states (Alaska, Hawaii, Montana, New Mexico, North Dakota, South Dakota, Utah, Vermont, and Wyoming) and the District of Columbia had 5 or fewer designated centers.
Across all states, an average 14.9% of persons aged 55 to 79 did not have access to a designated screening center within 30 miles, and an average 28.1% did not have access within a 30-minute drive. In most states (27 states and the District of Columbia), 0% to 22% of the population aged 55 to 79 did not have access to a designated screening center within 30 miles; 66% to 86% of this population did not have access to these services within 30 miles in 4 states (North Dakota, South Dakota, Montana, and Wyoming) clustered in the upper Midwest (Panel A). In 9 states (Connecticut, Delaware, Florida, Maryland, Massachusetts, New Jersey, New York, Pennsylvania, and Rhode Island) and the District of Columbia, 95% or more of the population aged 55 to 79 had access to a designated LDCT screening center within 30 miles. Rural residents were less likely than urban residents to have access to a designated LDCT screening center within 30 miles (47.5% rural vs 93.7% urban) or a 30-minute drive (22.2% rural vs 83.2% urban).
Lung cancer mortality was highest in the eastern interior of the United States. A cluster of high mortality stretches north to south from West Virginia to Louisiana and west to east from Oklahoma to West Virginia. Despite their high rate of lung cancer mortality, Alabama, Arkansas, Mississippi, Oklahoma, Tennessee, and West Virginia had low to medium levels of access to LDCT screening. All the states along the eastern seaboard and in the Northeast, except Maine, had high access to LDCT screening (Panel B).
Action
These maps update an assessment of the geographic variation of LDCT screening availability in the United States and extend research by using spatial proximity of persons aged 55 to 79 to designated screening centers to identify disparities in access (5,8). Findings indicate that although the number of designated LDCT screening centers increased by more than 8 times since 2014, pronounced disparities in the distribution of centers exist, particularly between rural and urban areas. This disparity in access is concerning, given the large proportion of high-risk persons in rural areas. We hope that the geographic patterns illustrated in these maps stimulate further research into ways to improve equitable access to high-quality screening services in high-need regions.
Acknowledgments
This publication was made possible in part by grant no. T32-GM081740 from the National Institutes of Health–National Institute of General Medical Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health or the National Institute of General Medical Sciences. No copyrighted images, materials, surveys, instruments, or tools were used in this study.
Footnotes
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions.
Suggested citation for this article: Eberth JM, Bozorgi P, Lebrón LM, Bills SE, Hazlett LJ, Carlos RC, et al. Geographic Availability of Low-Dose Computed Tomography for Lung Cancer Screening in the United States, 2017. Prev Chronic Dis 2018;15:180241. DOI: https://doi.org/10.5888/pcd15.180241.
References
- 1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin 2018;68(1):7–30. 10.3322/caac.21442 [DOI] [PubMed] [Google Scholar]
- 2. Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365(5):395–409. 10.1056/NEJMoa1102873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Moyer VA; US Preventive Services Task Force. Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2014;160(5):330–8. 10.7326/M13-2771 [DOI] [PubMed] [Google Scholar]
- 4. Jemal A, Fedewa SA. Lung cancer screening with low-dose computed tomography in the United States — 2010 to 2015. JAMA Oncol 2017;3(9):1278–81. 10.1001/jamaoncol.2016.6416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Eberth JM, Qiu R, Adams SA, Salloum RG, Bell N, Arrington AK, et al. Lung cancer screening using low-dose CT: the current national landscape. Lung Cancer 2014;85(3):379–84. 10.1016/j.lungcan.2014.07.002 [DOI] [PubMed] [Google Scholar]
- 6. Ruggles S, Genadek K, Goeken R, Grover J, Sobek M. Integrated public use microdata series: version 7.0. Minneapolis (MN): University of Minnesota, 2017. 10.18128/D010.V7.0. Accessed July 19, 2018. [DOI]
- 7.National Cancer Institute, Center for Disease Control and Prevention. State cancer profiles. https://statecancerprofiles.cancer.gov. Accessed July 19, 2018.
- 8. Charkhchi P, Kolenic GE, Carlos RC. Access to lung cancer screening services: preliminary analysis of geographic service distribution using the ACR lung cancer screening registry. J Am Coll Radiol 2017;14(11):1388–95. 10.1016/j.jacr.2017.06.024 [DOI] [PMC free article] [PubMed] [Google Scholar]