Abstract
Cognitive impairment results from a complex interplay of many factors. The most important independent predictor of cognitive decline is age but other contributing factors include demographic, genetic, socio-economic, and environmental parameters, including nutrition. The number of persons with cognitive decline and dementia will increase in the next decades in parallel with aging of the world population. Effective pharmaceutical treatments for age-related cognitive decline are lacking, emphasizing the importance of prevention strategies. There is extensive evidence supporting a relationship between diet and cognitive functions. Thus, nutritional approaches to prevent or slow cognitive decline could have a remarkable public health impact. Several dietary components and supplements have been examined in relation to their association with the development of cognitive decline. A number of studies have examined the role of dietary patterns on late-life cognition, with accumulating evidence that combinations of foods and nutrients may act synergistically to provide stronger benefit than those conferred by individual dietary components. Higher adherence to the Mediterranean dietary pattern has been associated with decreased cognitive decline and incident AD. Another dietary pattern with neuroprotective actions is the Dietary Approach to Stop Hypertension (DASH). The combination of these two dietary patterns has been associated with slower rates of cognitive decline and significant reduction in incident AD. This review evaluates the evidence for the effects of some dietary components, supplements, and dietary patterns as neuroprotective, with potential to delay cognitive decline and the onset of dementia. (www.actabiomedica.it)
Keywords: Alzheimer, cognitive decline, aging, diet, nutrition, inflammation, oxidative stress
Introduction
Aging of the world population is an undeniable contemporary reality. The recently published World Report on Aging and Health (1) asserts that, for the first time in the history of mankind, most people around the world can expect to live over 60 years. Biodemographic data suggest that half of the children alive in 2010 in countries with the highest life expectancies may reach the age of 100 years (2). The dark side of this successful story is that the number of persons with cognitive decline will increase exponentially in the coming decades (3, 4) in parallel with aging of the world population. This implies remarkable finance and human burden because dementia is one of the greatest causes of disability (4). Worldwide, 47 million persons are currently affected by dementia with about 8 million newly diagnosed cases annually. Most of them, 60-75%, have Alzheimer’s disease (AD), followed by vascular and Lewy bodies dementia (3, 4). Even if the general care of people with dementia has improved, the availability of effective interventions to significantly modify the disease is still lacking (5). Even if cognitive decline occur generally in old age, the causal brain pathology develops years before, which gives room to preventive strategies. Not only preventing, but even delaying the onset of dementia, would have profound effects on public health. Nevertheless, a very recent systematic review of 51 trials with low-moderate risk of bias concluded that the available evidence does not support the use of pharmacological treatments (i.e., dementia medications, antihypertensive and diabetes drugs, anti-inflammatory medications, and estrogen/progestin agents) for the prevention of cognitive decline in persons with normal cognition or with mild cognitive impairment (MCI) (6). Two systematic reviews, one on cognitive training including 11 trials (7), and another on exercise including 16 trials (8), concluded that evidence for prevention of cognitive decline or dementia with these strategies is insufficient. Interestingly, a multidomain intervention including physical activity, diet, and cognitive training improved several cognitive outcomes (9).
The impact of diet and nutrition on age-associated cognitive decline is becoming a growing field as a potential modifiable contributor (10). Various minerals, micronutrients, vitamins with antioxidant/anti-inflammatory properties have been studied (11). Dietary essential fatty acids forming neuronal membranes with antioxidant, anti-excitotoxic, and inti-inflammatory actions have been tested as well (12, 13). Similar studies suggest biological plausibility and cognitive effects of other single or multi-ingredient supplements, which recently has been judged as insufficient (14). In addition, diverse dietary patterns have been studied in relation to their association with cognitive functions alluding that the benefit of nutritional factors may derive from synergistic interactions of different components contained in a food pattern (15).
In this article, we review possible mechanisms and evidence for the actions of dietary components, supplements, and dietary patterns on cognitive decline and dementia.
Possible mechanisms mediating the effects of diet on cognitive decline and AD
Overweight and obesity in adulthood and late-onset cognitive decline
Traditional risk factors for cardiovascular disease (CVD) and type 2 diabetes (T2D), both in isolation and combined, are also risk factors for the development of cognitive decline and AD (16). The clustering of risk factors (i.e., central obesity, hyperglycemia, hypertension, atherogenic dyslipidemia, and a prothrombotic state), or metabolic syndrome, is directly related to the accumulation of visceral adiposity in midlife linked to overeating and sedentarism with deleterious consequences in late-life (17). Obesity has become an epidemic at all ages. In the current industrial era, there is extensive accessibility to abundant inexpensive calorie-rich food, which together with a sedentary lifestyle has paradoxically contributed to the increased life expectancy in the last century. Overeating and sedentarism have led to chronic non-communicable diseases (18), which develop easily but are very challenging to treat and may become unsustainable. A systematic review of 28 longitudinal studies conducted from 2003 to 2013 with follow-up of 5-40 years showed an increased risk of late-onset dementia in overweight and obese participants in midlife (up to 2.44 fold risk) (19). The mechanism behind this association is not yet clarified, but several possible mediators have been suggested. Overweight and obesity-related vascular consequences, i.e., hypertension, atherogenic dyslipidemia, and/or diabetes, are also risk factors for dementia (16). Yet, most analyses in the studies take into account these potential confounder. High levels of plasma amyloid proteins have been found in obese persons (20). A longitudinal study showed that being overweight or obese in midlife was associated with lower blood brain barrier (BBB) integrity almost 25 years later (21).
The accumulation and activation of macrophages in outsized adipose tissue may trigger systemic and neuroinflammation. Immune cells in adipose tissue can secrete pro-inflammatory [e.g., tumor necrosis factor (TNF), interleukin (IL)-1b, IL-6] and anti-inflammatory cytokines (adiponectin and IL-10), which maintain low-grade chronic inflammation (22). Obesity has been also linked to a switch from M2 macrophages to the proinflammatory M1 phenotype (23).
Dietary fats, specially saturated fatty acids (SFA), induce inflammatory responses on microglia, with local cytokine production, i.e., hypothalamic nuclear factor kappa B (NF-kB), which may lead to apoptosis of neurons involved in body weight control, central regulation of energy balance, blood pressure, and glucose homeostasis (24). Obesity may also induce modifications in the developing brain of children and adolescents (25), with long-term negative consequences.
Conversely, low-calorie diets, weight reduction or frequent consumption of food rich in antioxidant/anti-inflammatory properties, or food patterns with combinations of them, have been associated with reduced markers of systemic and adipose tissue inflammation (26). Diet studies in humans have shown a link between insulin resistance and cognition (27), as well as T2D glucose regulation abnormalities and cognitive function (28). Diet interventions that improved insulin resistance have been associated with decreased inflammatory cytokines and improved cognition (29, 30).
Oxidative stress and chronic metabolic inflammation
A pro-oxidant, pro-inflammatory state is characteristic of aging and age-related degenerative diseases resulting in harmful damage on cellular components. The brain is particularly susceptible to oxidative damage. Cerebral metabolism needs large amounts of energy, and it is dependent on aerobic conditions; it is also rich in polyunsaturated fatty acids (PUFAs), which are oxidizable, and in transition metals, which facilitate free radicals generation. Moreover, the brain has low levels of antioxidant systems compared to other body structures. This might render brain tissue prone to damage due to accumulation of neurotoxic peptides such as amyloid-beta (31). Autoptic studies have shown increased protein oxidative damage, lipid peroxidation, glycol-oxidation, and reduced antioxidant enzyme systems in brain tissue from AD patients (32).
Increasing evidence suggests neuroinflammation as the origin of AD. Aggregated and misfolded proteins (e.g., amyloid) bind to microglia toll-like receptors (TLRs) and CD4, initiating innate immune responses with production of inflammatory mediators (33). Microglia surrounding amyloid plaques and tangles were already described by Alois Alzheimer, but only in recent times the role of microglia inflammation has been studied. Neuroinflammation is a key protective mechanism; yet, when uncontrolled and chronic, it may become harmful by the incessant release of free radicals, proteolytic enzymes, nitric oxide, complementary factors, cytokines, or excitatory amino acids (34). Amyloid-beta accretion induces neuroinflammation, which consecutively produces more amyloid-beta, propagating the injury (35). Increased neuroinflammation has been shown in MCI and AD patients vs. healthy controls using positron emission tomography and imaging with radioligand C-11-DAA1106 (36). Amyloid-beta may lead to a preponderance of M1 cells vs. M2 (anti-inflammatory cells) and loss of the ability to switch phenotypes and lessen destruction (34). Nitric oxide (NO) in excess may induce inflammatory signals, identified as key players in neurodegenerative diseases with consequent neuronal death (37).
Autophagy and prothrombotic state
Autophagy mediates degradation and recycling and of cellular proteins, whose efficiency declines with age. It involves clearance of misfolded proteins and aggregates such as amyloid, which is altered in AD (38). There is evidence that the mammalian target of rapamycin (mTOR) signaling, a key player of cellular senescence, affects glucose metabolism, energy production, mitochondrial function, and autophagy in the brain. These events are central in age-associated cognitive decline and AD (39).
Other features of AD are vascular disorders (e.g., decreased cerebral blood flow, BBB disruption, and cerebrovascular dysfunction) and a prothrombotic state (e.g., clot formation, activated platelets, decreased fibrinolysis). Fibrinogen accumulates with amyloid-beta, which promotes amyloid beta fibrillization and generation of fibrin resistant to degradation. A recent study showed higher platelet activating factor acetylhydrolase activity and higher oxidized-LDL levels when compared AD patients with control subjects (40).
Dietary components and supplements with suggested effects on cognitive decline and AD
Omega-3 fatty acids
The PUFAs are essential constituents of neuronal cell membranes, preserving membrane fluidity for neurotransmitter communication and synaptic vesicle fusion. They may be precursors for lipid messengers in signaling processes to promote neuroprotection or neuronal damage (41). There is evidence of PUFAs deficit in the hippocampus, cortex, and cerebellum in the aged brain, which may be worse in AD (42). The most widely studied PUFAs regarding cognitive decline are omega-3 PUFAs with dissimilar results. A systematic review reported data supporting a role for long-chain omega-3 PUFAs in the reduction of cognitive decline in persons without dementia (43). Nevertheless, other trials have shown negative results. The “Supplementation with Folate, vitamin B6 and B12 and/or OMega-3 fatty acids” trial including 1,748 participants with a history of CVD reported no significant effects of vitamin B and omega-3 fatty acid supplementation on cognitive function (44). A double-blind RCT involving 302 cognitively intact persons aged ≥65 years assigned to 1,8 g/day eicosapentaenoic (EPA)-docosahexaenoic (DHA), 0.4 g/day EPA-DHA, or placebo for a short period (26 weeks) found no significant effects (45). A meta-analysis of results from 3,536 persons aged >60 years without cognitive dysfunction at baseline supplemented with omega-3 PUFAs reported no significant effects on cognitive function (46). An epidemiological study of Chinese adults showed that persons aged ≥65 years who consumed ≥100 g/week of fish had a reduction of about 65% in the mean annual rate of global cognitive decline with no associations among adults aged 55-64 years (47). Recently, the “Multidomain Alzheimer Preventive Trial” reported that multidomain intervention and omega-3 PUFAs supplementation, either alone or in combination, had no significant effects on cognitive decline over 3 years in 1525 participants (48).
Curcuminoids
Curcumin is a polyphenolic compound from the rhizome of Curcuma longa c ontained in curry spice turmeric, considered an effective therapy for several conditions in traditional Indian medicine, widely used in that population, and a potent antioxidant (49). In 2000, a study by Ganguli et al. (50) reported a lower prevalence of AD in the Indian population compared to the US population. Ng et al. found that older healthy people who consume more frequently curry had better cognitive performance (51). Numerous experimental studies confirmed the potent anti-oxidant and anti-inflammatory properties of curcumin and its protection on AD animal models. Three RCTs have been so far completed. Baum et al. (52) enrolled 34 patients with AD receiving either 1 or 4 g/day of curcumin or placebo for 6 months and reported no significant effects in Mini Mental State Examination (MMSE). Ringman et al. (53), randomized 36 patients with dementia to 2 or 4 g/day of Curcumin C3 Complex (95% of curcuminoids) or placebo for 24 weeks, extended to 48 weeks as an open-label trial with Curcumin C3 Complex for the placebo arm. The authors did not observe any significant difference between treatment groups and placebo in any of the scores (ADAS-Cog, NPI, ADCS-ADL, MMSE) or cerebrospinal fluid markers. Hishikawa et al. (54) showed that 3 dementia patients treated with 100 mg/day of curcumin and donepezil had a lower NPI score after 12 weeks of therapy. Supplements of curcumin have limited bioavailability, which has been suggested to improve with lipidated formulations (55).
Magnesium
Compelling evidence shows that magnesium (Mg) deficiency results in increased free radicals production in various tissues, increased oxidative tissue damage, increased superoxide anion production by inflammatory cells, decreased antioxidant enzyme expression and activity, decreased cellular and tissue antioxidant levels, and increased oxygen peroxide production (56, 57); Mg is essential for synaptic conduction, affects N-methyl-D-aspartate (NMDA) receptor response to excitatory amino acids (58), inhibits calcium channels, calcium influx, and glutamate release, and has effects on stability and viscosity of cell membranes (56). Mg insufficiency produces vasospasm while elevated Mg induces tone relaxation in cerebral arteries (59). Due to the above mentioned reasons, the role of Mg in cognitive decline and dementia has been examined in recent years. Former studies showed low serum Mg levels (60) and autoptic brain tissue concentrations in AD patients (61). We observed reduced ionized free Mg concentrations in plasma obtained from AD patients (62), which were related to cognitive dysfunction severity. Cilliler et al. (63) reported negative associations of serum Mg levels and 2 rating AD severity scales (Global Deterioration Scale and Clinical Dementia Rating), further confirming a potential protective role of Mg on cognitive function. There are no specific trials with Mg supplements in the prevention or therapy of cognitive disorders; hence, whether Mg supplementation may exert protective effects against AD remains to be further elucidated in well-design trials.
Cocoa and cocoa-derived products
Cocoa is a rich source of flavonoids, which has shown cardiovascular benefits. Some small acute and short-term chronic trials have suggested neuroprotective properties. A study in 18 persons aged 50-65 years reported significant increases in regional perfusion across the brain following consumption of the high flavanol drink (494 mg), particularly in the anterior cingulate cortex and the central opercular cortex of the parietal lobe measured with spin labelling functional MRI (64). A small study of 34 healthy persons (mean age 72±6 years) showed an increased blood flow velocity in the middle cerebral artery after one (8%) and two weeks (10%) of flavanol-rich cocoa consumption using transcranial Doppler ultrasound (65). In an RCT, healthy persons aged 50-69 years who consumed a high cocoa flavanol-containing diet for 3 months exhibited enhanced dentate gyrus function, as measured by functional MRI and by cognitive testing (66). A prospective study involving 531 participants aged ≥65 years followed for median 48 months showed that chocolate intake was associated with a 41% lower risk of cognitive decline after adjustment for confounders (67).
The mechanisms proposed to explain the potential benefit of cocoa and derived products are: 1) direct interactions with cellular signaling that promote neurogenesis, neuronal function and brain connectivity, and 2) blood-flow improvement and angiogenesis in the brain and sensory systems. The preliminary evidence shown above underscores the need for further well-design and large RCT on these interesting compounds.
Tea and (-)-Epigallocatechin-3-gallate (EGCG)
Tea is traditionally indicated as a cognitive stimulator in Asian cultures. This effect has been confirmed in some studies and has been linked to antioxidants contained in tea, such as EGCG, L-theanine, and caffeine (68). Tea may also exert neuroprotective actions by regulation of stress hormones and inhibition of acetylcholinesterase (69). However, there is currently inconsistent evidence with no definitive conclusion on its neuroprotective actions (70). Bioactive compounds, such as L-theanine and EGCG, may have some potential due to their anti-amyloidogenic and antioxidant properties in vitro, but the evidence for their use as nutraceuticals is limited and there is no recommendation currently for their use in clinical practice.
Caffeine
There is evidence of antioxidant (71) and amyloid-beta suppressive properties of caffeine in animal models of AD (72). The reduction in amyloid-plaques is associated with a stimulation of protein kinase A activity, increased phosphor-CREB levels, and reduced phosphor-JNK and phosphor-ERK expression in mouse models of AD, promoting survival cascades in the brain (72, 73). It is well-known that coffee and caffeine strengthen short-term memory and cognition, but there is limited evidence suggesting long-term effects. A case-control study of 124 older persons with MCI showed that high serum levels of caffeine were associated with lack of progression to dementia (74). Another study reported that consumption of 3-5 cups of coffee per day reduced incident AD and dementia by 65% (75). Among 3494 men from the Honolulu-Asia Aging Study, deceased men in the highest quartile of caffeine intake were less likely to have any neuropathological dementia lesion vs. men in the lowest quartile. Yet, coffee and caffeine intake in midlife were not associated with risk of cognitive impairment, overall dementia, AD, vascular dementia, or moderate/high levels of neuropathological lesions (76).
A meta-analysis of studies exploring the relationship of caffeine consumption and cognitive decline reported nonsignificant effects (77), but few and largely heterogeneous studies were included. A Portuguese study reported an association of caffeine consumption with slower cognitive decline (78), while a study from France found no association (79). A longitudinal study reported less cognitive decline among coffee consumers but no dose response (80). Another showed no relationship (81). There is no evidence from RCTs.
Phytoestrogen compounds
Studies on soy isoflavones usually include mixtures of them, such as genistein and daidzein, which impede to discriminate the effects of specific components on cognition. Studies of soy consumption and phytoestrogen supplements on cognitive function have reported variable and inconclusive results (82), with overall absence of adverse events (83). An initial positive cognitive effect in adult age appears to reverse in older women; in men the data are even more equivocal (82). Discrepancies may be explained by the use of different isoflavone supplements at variable doses in small short-term trials. Studies showing no effect of phytoestrogens on cognition are mostly from European cohorts, with low dietary soy consumption. Studies of older Asian populations with higher consumption of soy-derived foods show lower rates of cognitive decline. After oral intake of conjugated isoflavones, dadzein is converted to S-equol by a gut biotransformation. About 70% of older Japanese persons are “equol producers” (84), which may help explain the different results in Asian vs. Europeans studies.
In the Women’s Isoflavone Soy Health (WISH) trial, 313 postmenopausal women aged 45-92 years were randomized to receive 25 g/d of isoflavone-rich soy protein (containing genistein, daidzein, and glycitein) or milk protein-matched placebo. Cognitive function was assessed at baseline and after 2.5 years. There were no differences between the groups in cognition change from baseline. Nevertheless, women within 5-10 years of menopause in the isoflavone group showed a nonsignificant (p=0.07) trend toward cognitive improvement, and a significant improvement in verbal episodic memory. Consistent producers of urinary S-equol showed a nonsignificant (p=0.08) trend toward cognitive improvement (85). Further studies are necessary to validate these findings. There are no RCTs of phytoestrogens for the prevention or treatment of AD.
Resveratrol
This hytoalexin is a polyphenol contained in berries. Most dietary resveratrol in humans comes from grapes and red wine (86). Biological properties of resveratrol include antioxidant and anti-inflammatory actions (87). Studies in animal models of AD have shown reduced hippocampal neurodegeneration and increased memory performance, but human clinical trials of resveratrol on cognition are limited. A placebo-control study in 22 healthy adults showed a dose-dependent (250-500 mg/day) increase in cerebral blood flow in the prefrontral cortex during cognitive tasks (88). Another small study including 23 overweight persons, aged 50-75 years, receiving resveratrol (200 mg/d) for 26 weeks vs. a group receiving placebo, reported improved memory performance and higher functional connectivity of the hippocampus in neuroimaging with resveratrol treatment (89). There are several ongoing clinical trials on resveratrol investigating its potential effects on cognitive function, MCI and AD (90). At present, there is no data on toxicity of chronic resveratrol supplementation. There is no sufficiently substantiated evidence for prescribing this supplement to improve cognitive function.
Gingko biloba
An RCT included 3,069 participants randomized into Gingko biloba treatment or placebo to determine whether G. biloba supplementation could prevent dementia among older adults who were cognitively intact or had mild cognitive impairment at baseline. Participants were followed for a median of 6.1 years, and study results indicated no difference in the rate of cognitive decline for the two treatment groups (91).
Garlic (Allium sativum)
Garlic extracts have shown antioxidant properties and protection against amyloid-beta-induced neurotoxic effects in experimental animals (92). Allicin, an organosulfur compound contained in garlic, inhibited cholinesterase enzymes and upregulated brain acetylcholine levels in vitro (93). Nevertheless, there are no clinical trials for these compounds. In the Doetinchem Cohort Study, including 2613 participants aged 43-70 years, higher consumption of allium (onion, garlic, and leek) was associated with worse scores on cognitive flexibility and speed of cognitive processes in cross-sectional analyses, while in longitudinal analyses, allium consumption was not associated with cognitive decline (94).
Vitamins
In 4,052 participants from the Physicians’ Health Study and Physicians’ Health Study II, there was no significant effect on cognitive function with short-term beta-carotene (provitamin A) treatment and beneficial effect with longer-term (18-year) administration (95).
Studies on the effect of vitamin B on cognition have produced mixed results. An RCT of 299 men >75 years showed no significant effect on cognitive function of 2-year supplementation with folic acid, vitamin B6, and B12 (96). Similarly, a meta-analysis of 9 RCTs (n=2,835) indicated no significant effect of folic acid with or without other B vitamins on cognitive function (97). Conversely, an RCT of 900 persons aged 60–74 years showed that folic acid+vitamin B12 were significantly superior vs. placebo for improving cognitive tests (98).
A number of studies have examined the combined effects of vitamins C and E on cognitive function in healthy populations with conflicting results. The Women’s Health Study (6,377 women over 65 years) showed no significant effect on cognitive function of vitamin E supplementation (99). Analyses of 616 over 65-years-old participants of the Duke Established Populations for Epidemiologic Studies showed that vitamins C and/or E supplements had no influence on incident dementia or AD (100). On the contrary, the Canadian Study of Health and Aging (894 participants aged ≥65 years) reported that a combination of vitamins C and E significantly decreased the rate of cognitive decline (101). A recent study analyzed the relations of alpha- and gamma-tocopherol brain concentrations with AD neuropathology among 115 deceased participants of the prospective Rush Memory and Aging Project. Gamma-tocopherol concentrations were associated with lower amyloid load and lower neurofibrillary tangle severity, while alpha-tocopherol concentrations were not associated with neuropathology (102).
The Third National Health and Nutrition Examination Survey showed an association of vitamin D deficiency with an increased risk of cognitive decline in the US (103). However, the Women’s Health Initiative showed no significant effect of vitamin D and calcium supplementation on cognitive function in 2,034 women aged over 65 years, followed for a mean of 7.8 years (104).
Results from the Age-Related Eye Disease Study including 2,166 participants followed for 6.9 years showed that a combination of antioxidant vitamins (vitamins E and C, beta-carotene), zinc, and copper had no significant effects on any of six tests of cognitive function (105). Similarly, the Women’s Antioxidant Cardiovascular Study that included 2,824 women with or at risk for CVD who received a combination of vitamin E, beta-carotene, and vitamin C or placebo showed no effects on cognition with the multivitamin supplementation (106).
Dietary patterns
The incidence of chronic diseases, including dementia and AD, has been assessed in relation to dietary patterns in populations of various ethnicity, culture, or religious beliefs. There is no single dietary or lifestyle intervention proven in RCTs to prevent incident AD. Nevertheless, epidemiological data suggest that adopting a healthy, balanced diet and lifestyle known to improve cardiovascular risk may help delay incident AD (107).
Mediterranean diet (MeDiet)
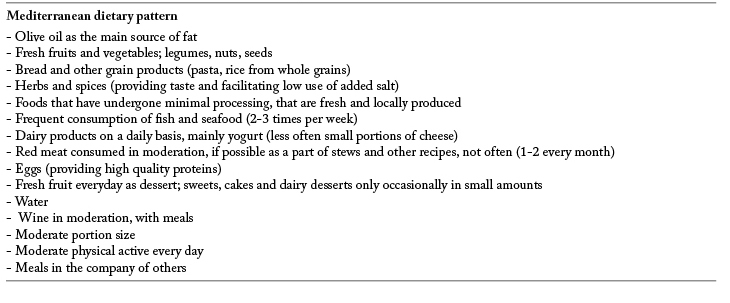
The dietary pattern consumed traditionally by populations bordering the Mediterranean Sea has been extensively reported as a model of healthy eating. MeDiet characteristics are shown in Table 1. A greater adherence to MeDiet has been associated with a reduced incidence of overall mortality, cardiovascular mortality, cardiovascular events incidence, cancer mortality and/or incidence, and incident Parkinson’s disease and AD (108).
Table 1.
Characteristics of the Mediterranean dietary pattern.
A recent systematic review of longitudinal cohorts examining MeDiet effects on cognition found that participants in the highest tertile of adherence to MeDiet had 33% less risk of MCI or AD when vs. those in the lowest tertile (109). The RCT PREDIMED (Prevención con Dieta Mediterranea), including adults aged 55-80 years at high cardiovascular risk, showed that participants on a MeDiet supplemented with either EVOO or nuts, had a reduced incidence of cardiovascular events vs. participants following a low-fat diet over 5-years of follow-up (110). Two subanalysis of this RCT have reported improved cognitive function with the MeDiet supplemented with either EVOO oil or nuts vs. low-fat diet (111, 112).
Several longitudinal studies have examined the effects of MeDiet on AD in cohorts from the US (113-117), and France (118, 119). Two reviews (108, 120) concluded that even if there is some evidence that adherence to MeDiet is associated with a reduced risk of AD, additional confirmation in populations with different ethnicities and dietary habits is necessary. The Personality and Total Health (PATH) through Life longitudinal study (121) of healthy participants from Australia found no protection of MeDiet for cognitive decline, while the Australian Imaging, Biomarkers and Lifestyle (AIBL) study (122) showed that participants with AD and MCI had lower adherence to MeDiet than healthy controls. A 7-year longitudinal study (123) evaluated adherence to HEI-2005 or to MeDiet in relation to cognitive change in 3,790 adults aged >65 years from the ongoing Chicago Health and Aging Project longitudinal study. The results showed that white participants had higher energy-adjusted MeDiet scores but lower HEI-2005 scores compared to black participants. Higher MeDiet scores, adjusted for confounders, were associated with slower rates of cognitive decline, but no association was found for HEI-2005 scores. MeDiet encompasses other cultural and lifestyle components, such as physical activity, adequate rest, social engagement, and culinary activities (124). These lifestyle factors have shown positive effects on delaying cognitive decline. Future studies should consider all MeDiet lifestyle factors into their design.
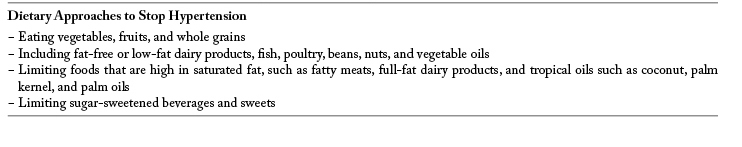
Dietary approaches to stop hypertension (DASH)
This balanced eating plan effectively lowers cardiovascular outcomes (125). DASH characteristics are shown in Table 2. A prospective study examined the associations between DASH and MeDiet with age-related cognitive changes in 3831 participants aged >65 years, followed for >11 years. Higher adherence to DASH and MeDiet and greater consumption of whole grains, nuts and legumes were significantly associated with higher average MMSE scores (126). A combined dietary pattern of MeDiet and DASH (or MIND) in 960 participants of the Memory and Aging Project followed for a mean of 4.7 years was positively associated with slower decline in global and 5 single cognitive domains, after adjusting for confounders (127). In 923 participants, aged 58-98 years, followed for average 4.5 years, there was a significant reduction in incident AD for the second and third tertile of adherence scores to MIND diet vs. the lowest tertile (128). Replications of these positive results with DASH and MIND are needed in other populations to confirm their relevance to brain health.
Table 2.
Characteristics of DASH (Dietary Approaches to Stop Hypertension)
Other dietary patterns with no proven or conflicting effects on cognitive function or prevention of cognitive decline
Several dietary patterns with confirmed benefit for diverse health outcomes (e.g., cardiovascular health, total mortality, incident cancer, body weight control) have not definitely proven effects on the prevention of cognitive decline or dementia.
Healthy Eating Index-2005 (HEI-2005) (Dietary Guidelines for Americans) - Two cross-sectional studies (129, 130) showed associations of HEI-2005 and improvements in cognition. However two longitudinal studies (123, 131) followed up to 7.6 years showed no association. A longer study (132) (11-year follow-up) showed less cognitive decline with increased HEI scores, indicating that a longer duration may be needed to disclose effects of diet on cognition.
Okinawa Diet - Notwithstanding this dietary pattern is followed by populations with some of the longest life expectancies in the world, there is still no solid evidence for its effects on prevention of cognitive decline and AD. A study showed a higher incident dementia in 157 migrants from Okinawa to Brazil vs. 2,217 residents of Okinawa (133). The 9-year difference between the studies and dissimilar sample size may have affected the results.
Vegetarian Diets - The incidence of dementia in those consuming vegetarian diets and meat-eating diets was compared in two cohort sub-studies of the Adventist Health Study (134). The first study showed that persons who ate meat were more than twice as likely to become demented as their vegetarian counterparts. A second analysis showed no significant difference in the incidence of dementia between vegetarian and meat-eating subjects, with no clear explanation for the difference between the two sub-studies. There was no clear evidence of any standardized cognitive assessment during the study.
Paleolithic Diet- A study of 20 overweight postmenopausal women compared the effects of Paleolithic diet vs. Nordic Nutrition Recommendations followed for 6 months on parameters of functional MRI, episodic memory tasks, and weight loss. There was a significant improvement in episodic memory performance after both dietary interventions, which was associated with increased hippocampal activity, decreased waist circumference and reduced plasma FFA without differences between the diets (135). There are no studies on the effects of Paleolithic diet on incident AD.
Ketogenic Diet- This dietary pattern has been associated with neuroprotective effects in some forms of epilepsy. While there is no current evidence of AD prevention with ketogenic diet, a small double-blind placebo-controlled study of 20 patients with MCI or AD showed memory scores improvement in patients receiving medium-chain triglycerides in non- APOEε4 patients but not in APOEε4 positive patients (136). A clinical trial of 152 participants showed similar results (137). Most findings with KD come from animal studies and a solid validation in human trials is still warranted.
Low-copper Diet- A longitudinal study of 3718 participants showed that high intakes of copper, mostly supplements, together with a high-fat diet resulted in more rapid cognitive decline after 5.5. years follow-up (138). In 32 patients with mild to moderate AD, those with low plasma Cu had significantly higher ADAS-cog scores (139) Squitti et al. suggest that the promotion of a low-Cu diet may potentially reduce the risk of AD (140). Nevertheless, there is no evidence that depletion or supplementation of Cu may modify AD incidence or pathology.
Conclusions
Results from large-scale epidemiologic studies and clinical trials generally do not demonstrate an independent role for most of the nutritional and dietary factors that have been examined for the prevention of cognitive decline or AD. Further research is needed to clarify the possible benefits of the single dietary components.
The effects of MeDiet and DASH on cardiovascular health are well established, and there is moderately convincing evidence that adherence to these dietary patterns is associated with a reduced risk of AD, especially with the combination of both dietary patterns. Further confirmation in populations with different ethnicities and different dietary behaviors is needed. There is at present no clear evidence to support effects of HEI-2005, Okinawa, vegetarian, Paleolithic, ketogenic, or low-copper diets on the prevention of cognitive decline or AD.
Studying dietary patterns may help understand possible synergistic actions of foods and nutrients combinations in order to prevent or delay the onset of cognitive decline and dementia.
References
- 1.Beard JR. Officer A. de Carvalho IA. Sadana R. Pot AM. Michel JP. Lloyd-Sherlock P. Epping-Jordan JE. Peeters G. Mahanani WR. Thiyagarajan JA. Chatterji S. The world report on ageing and health: A policy framework for healthy ageing. Lancet. 2016;387:2145–2154. doi: 10.1016/S0140-6736(15)00516-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vaupel JW. Biodemography of human ageing. Nature. 2010;464:536–542. doi: 10.1038/nature08984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.2014 alzheimer’s disease facts and figures. Alzheimers Dement. 2014;10:e47–92. doi: 10.1016/j.jalz.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 4.Prince MJ. Wu F. Guo Y. Gutierrez Robledo LM. O’Donnell M. Sullivan R. Yusuf S. The burden of disease in older people and implications for health policy and practice. Lancet. 2015;385:549–562. doi: 10.1016/S0140-6736(14)61347-7. [DOI] [PubMed] [Google Scholar]
- 5.Feldman HH. Haas M. Gandy S. Schoepp DD. Cross AJ. Mayeux R. Sperling RA. Fillit H. van de Hoef DL. Dougal S. Nye JS. Alzheimer’s disease research and development: A call for a new research roadmap. Ann N Y Acad Sci. 2014;1313:1–16. doi: 10.1111/nyas.12424. [DOI] [PubMed] [Google Scholar]
- 6.Fink HA. Jutkowitz E. McCarten JR. Hemmy LS. Butler M. Davila H. Ratner E. Calvert C. Barclay TR. Brasure M. Nelson VA. Kane RL. Pharmacologic interventions to prevent cognitive decline, mild cognitive impairment, and clinical alzheimer-type dementia: A systematic review. Ann Intern Med. 2018;168:39–51. doi: 10.7326/M17-1529. [DOI] [PubMed] [Google Scholar]
- 7.Butler M. McCreedy E. Nelson VA. Desai P. Ratner E. Fink HA. Hemmy LS. McCarten JR. Barclay TR. Brasure M. Davila H. Kane RL. Does cognitive training prevent cognitive decline?: A systematic review. Ann Intern Med. 2018;168:63–68. doi: 10.7326/M17-1531. [DOI] [PubMed] [Google Scholar]
- 8.Brasure M. Desai P. Davila H. Nelson VA. Calvert C. Jutkowitz E. Butler M. Fink HA. Ratner E. Hemmy LS. McCarten JR. Barclay TR. Kane RL. Physical activity interventions in preventing cognitive decline and alzheimer-type dementia: A systematic review. Ann Intern Med. 2018;168:30–38. doi: 10.7326/M17-1528. [DOI] [PubMed] [Google Scholar]
- 9.Ngandu T. Lehtisalo J. Solomon A. Levalahti E. Ahtiluoto S. Antikainen R. Backman L. Hanninen T. Jula A. Laatikainen T. Lindstrom J. Mangialasche F. Paajanen T. Pajala S. Peltonen M. Rauramaa R. Stigsdotter-Neely A. Strandberg T. Tuomilehto J. Soininen H. Kivipelto M. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (finger): A randomised controlled trial. Lancet. 2015;385:2255–2263. doi: 10.1016/S0140-6736(15)60461-5. [DOI] [PubMed] [Google Scholar]
- 10.Norton S. Matthews FE. Barnes DE. Yaffe K. Brayne C. Potential for primary prevention of alzheimer’s disease: An analysis of population-based data. Lancet Neurol. 2014;13:788–794. doi: 10.1016/S1474-4422(14)70136-X. [DOI] [PubMed] [Google Scholar]
- 11.Meydani M. Antioxidants and cognitive function. Nutr Rev. 2001;59:S75–80. doi: 10.1111/j.1753-4887.2001.tb05505.x. discussion S80-72. [DOI] [PubMed] [Google Scholar]
- 12.Farooqui AA. Ong WY. Horrocks LA. Chen P. Farooqui T. Comparison of biochemical effects of statins and fish oil in brain: The battle of the titans. Brain Res Rev. 2007;56:443–471. doi: 10.1016/j.brainresrev.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 13.Lukiw WJ. Bazan NG. Docosahexaenoic acid and the aging brain. J Nutr. 2008;138:2510–2514. doi: 10.3945/jn.108.096016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Butler M. Nelson VA. Davila H. Ratner E. Fink HA. Hemmy LS. McCarten JR. Barclay TR. Brasure M. Kane RL. Over-the-counter supplement interventions to prevent cognitive decline, mild cognitive impairment, and clinical alzheimer-type dementia: A systematic review. Ann Intern Med. 2018;168:52–62. doi: 10.7326/M17-1530. [DOI] [PubMed] [Google Scholar]
- 15.Jacobs DR., Jr Orlich MJ. Diet pattern and longevity: Do simple rules suffice? A commentary. Am J Clin Nutr. 2014;100(Suppl 1):313S–319S. doi: 10.3945/ajcn.113.071340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de la Torre JC. Vascular risk factors: A ticking time bomb to alzheimer’s disease. Am J Alzheimers Dis Other Demen. 2013;28:551–559. doi: 10.1177/1533317513494457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dominguez LJ. Barbagallo M. The biology of the metabolic syndrome and aging. Curr Opin Clin Nutr Metab Care. 2016;19:5–11. doi: 10.1097/MCO.0000000000000243. [DOI] [PubMed] [Google Scholar]
- 18.Sepulveda J. Murray C. The state of global health in 2014. Science. 2014;345:1275–1278. doi: 10.1126/science.1257099. [DOI] [PubMed] [Google Scholar]
- 19.Emmerzaal TL. Kiliaan AJ. Gustafson DR. 2003-2013: A decade of body mass index, alzheimer’s disease, and dementia. J Alzheimers Dis. 2015;43:739–755. doi: 10.3233/JAD-141086. [DOI] [PubMed] [Google Scholar]
- 20.Jahangiri A. Wilson PG. Hou T. Brown A. King VL. Tannock LR. Serum amyloid a is found on apob-containing lipoproteins in obese humans with diabetes. Obesity (Silver Spring) 2013;21:993–996. doi: 10.1002/oby.20126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gustafson DR. Karlsson C. Skoog I. Rosengren L. Lissner L. Blennow K. Mid-life adiposity factors relate to blood-brain barrier integrity in late life. J Intern Med. 2007;262:643–650. doi: 10.1111/j.1365-2796.2007.01869.x. [DOI] [PubMed] [Google Scholar]
- 22.Grant RW. Dixit VD. Adipose tissue as an immunological organ. Obesity (Silver Spring) 2015;23:512–518. doi: 10.1002/oby.21003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harford KA. Reynolds CM. McGillicuddy FC. Roche HM. Fats, inflammation and insulin resistance: Insights to the role of macrophage and t-cell accumulation in adipose tissue. Proc Nutr Soc. 2011;70:408–417. doi: 10.1017/S0029665111000565. [DOI] [PubMed] [Google Scholar]
- 24.Velloso LA. Folli F. Saad MJ. Tlr4 at the crossroads of nutrients, gut microbiota, and metabolic inflammation. Endocr Rev. 2015;36:245–271. doi: 10.1210/er.2014-1100. [DOI] [PubMed] [Google Scholar]
- 25.Liang J. Matheson BE. Kaye WH. Boutelle KN. Neurocognitive correlates of obesity and obesity-related behaviors in children and adolescents. Int J Obes (Lond) 2014;38:494–506. doi: 10.1038/ijo.2013.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Calder PC. Ahluwalia N. Brouns F. Buetler T. Clement K. Cunningham K. Esposito K. Jonsson LS. Kolb H. Lansink M. Marcos A. Margioris A. Matusheski N. Nordmann H. O’Brien J. Pugliese G. Rizkalla S. Schalkwijk C. Tuomilehto J. Warnberg J. Watzl B. Winklhofer-Roob BM. Dietary factors and low-grade inflammation in relation to overweight and obesity. Br J Nutr. 2011;106(Suppl 3):S5–78. doi: 10.1017/S0007114511005460. [DOI] [PubMed] [Google Scholar]
- 27.Cholerton B. Baker LD. Craft S. Insulin, cognition, and dementia. Eur J Pharmacol. 2013;719:170–179. doi: 10.1016/j.ejphar.2013.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Geijselaers SL. Sep SJ. Stehouwer CD. Biessels GJ. Glucose regulation, cognition, and brain mri in type 2 diabetes: A systematic review. Lancet Diabetes Endocrinol. 2015;3:75–89. doi: 10.1016/S2213-8587(14)70148-2. [DOI] [PubMed] [Google Scholar]
- 29.Kelly KR. Haus JM. Solomon TP. Patrick-Melin AJ. Cook M. Rocco M. Barkoukis H. Kirwan JP. A low-glycemic index diet and exercise intervention reduces tnf(alpha) in isolated mononuclear cells of older, obese adults. J Nutr. 2011;141:1089–1094. doi: 10.3945/jn.111.139964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bayer-Carter JL. Green PS. Montine TJ. VanFossen B. Baker LD. Watson GS. Bonner LM. Callaghan M. Leverenz JB. Walter BK. Tsai E. Plymate SR. Postupna N. Wilkinson CW. Zhang J. Lampe J. Kahn SE. Craft S. Diet intervention and cerebrospinal fluid biomarkers in amnestic mild cognitive impairment. Arch Neurol. 2011;68:743–752. doi: 10.1001/archneurol.2011.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kapogiannis D. Mattson MP. Disrupted energy metabolism and neuronal circuit dysfunction in cognitive impairment and alzheimer’s disease. Lancet Neurol. 2011;10:187–198. doi: 10.1016/S1474-4422(10)70277-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mao P. Reddy PH. Aging and amyloid beta-induced oxidative DNA damage and mitochondrial dysfunction in alzheimer’s disease: Implications for early intervention and therapeutics. Biochim Biophys Acta. 2011;1812:1359–1370. doi: 10.1016/j.bbadis.2011.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Heneka MT. Carson MJ. El Khoury J. Landreth GE. Brosseron F. Feinstein DL. Jacobs AH. Wyss-Coray T. Vitorica J. Ransohoff RM. Herrup K. Frautschy SA. Finsen B. Brown GC. Verkhratsky A. Yamanaka K. Koistinaho J. Latz E. Halle A. Petzold GC. Town T. Morgan D. Shinohara ML. Perry VH. Holmes C. Bazan NG. Brooks DJ. Hunot S. Joseph B. Deigendesch N. Garaschuk O. Boddeke E. Dinarello CA. Breitner JC. Cole GM. Golenbock DT. Kummer MP. Neuroinflammation in alzheimer’s disease. Lancet Neurol. 2015;14:388–405. doi: 10.1016/S1474-4422(15)70016-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cherry JD. Olschowka JA. O’Banion MK. Neuroinflammation and m2 microglia: The good, the bad, and the inflamed. J Neuroinflammation. 2014;11(98) doi: 10.1186/1742-2094-11-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karran E. Mercken M. De Strooper B. The amyloid cascade hypothesis for alzheimer’s disease: An appraisal for the development of therapeutics. Nat Rev Drug Discov. 2011;10:698–712. doi: 10.1038/nrd3505. [DOI] [PubMed] [Google Scholar]
- 36.Yasuno F. Ota M. Kosaka J. Ito H. Higuchi M. Doronbekov TK. Nozaki S. Fujimura Y. Koeda M. Asada T. Suhara T. Increased binding of peripheral benzodiazepine receptor in alzheimer’s disease measured by positron emission tomography with [11c]daa1106. Biol Psychiatry. 2008;64:835–841. doi: 10.1016/j.biopsych.2008.04.021. [DOI] [PubMed] [Google Scholar]
- 37.Yuste JE. Tarragon E. Campuzano CM. Ros-Bernal F. Implications of glial nitric oxide in neurodegenerative diseases. Front Cell Neurosci. 2015;9(322) doi: 10.3389/fncel.2015.00322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Martinez-Vicente M. Autophagy in neurodegenerative diseases: From pathogenic dysfunction to therapeutic modulation. Semin Cell Dev Biol. 2015;40:115–126. doi: 10.1016/j.semcdb.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 39.Perluigi M. Di Domenico F. Butterfield DA. Mtor signaling in aging and neurodegeneration: At the crossroad between metabolism dysfunction and impairment of autophagy. Neurobiol Dis. 2015 doi: 10.1016/j.nbd.2015.03.014. [DOI] [PubMed] [Google Scholar]
- 40.Bacchetti T. Vignini A. Giulietti A. Nanetti L. Provinciali L. Luzzi S. Mazzanti L. Ferretti G. Higher levels of oxidized low density lipoproteins in alzheimer’s disease patients: Roles for platelet activating factor acetyl hydrolase and paraoxonase-1. J Alzheimers Dis. 2015 doi: 10.3233/JAD-143096. [DOI] [PubMed] [Google Scholar]
- 41.Bazan NG. Lipid signaling in neural plasticity, brain repair, and neuroprotection. Mol Neurobiol. 2005;32:89–103. doi: 10.1385/MN:32:1:089. [DOI] [PubMed] [Google Scholar]
- 42.Liu JJ. Green P. John Mann J. Rapoport SI. Sublette ME. Pathways of polyunsaturated fatty acid utilization: Implications for brain function in neuropsychiatric health and disease. Brain Res. 2015;1597:220–246. doi: 10.1016/j.brainres.2014.11.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fotuhi M. Mohassel P. Yaffe K. Fish consumption, long-chain omega-3 fatty acids and risk of cognitive decline or alzheimer disease: A complex association. Nat Clin Pract Neurol. 2009;5:140–152. doi: 10.1038/ncpneuro1044. [DOI] [PubMed] [Google Scholar]
- 44.Andreeva VA. Kesse-Guyot E. Barberger-Gateau P. Fezeu L. Hercberg S. Galan P. Cognitive function after supplementation with b vitamins and long-chain omega-3 fatty acids: Ancillary findings from the su.Fol.Om3 randomized trial. Am J Clin Nutr. 2011;94:278–286. doi: 10.3945/ajcn.110.006320. [DOI] [PubMed] [Google Scholar]
- 45.van de Rest O. Geleijnse JM. Kok FJ. van Staveren WA. Dullemeijer C. Olderikkert MG. Beekman AT. de Groot CP. Effect of fish oil on cognitive performance in older subjects: A randomized, controlled trial. Neurology. 2008;71:430–438. doi: 10.1212/01.wnl.0000324268.45138.86. [DOI] [PubMed] [Google Scholar]
- 46.Sydenham E. Dangour AD. Lim WS. Omega 3 fatty acid for the prevention of cognitive decline and dementia. Cochrane Database Syst Rev. 2012;6:CD005379. doi: 10.1002/14651858.CD005379.pub3. [DOI] [PubMed] [Google Scholar]
- 47.Qin B. Plassman BL. Edwards LJ. Popkin BM. Adair LS. Mendez MA. Fish intake is associated with slower cognitive decline in chinese older adults. J Nutr. 2014;144:1579–1585. doi: 10.3945/jn.114.193854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Andrieu S. Guyonnet S. Coley N. Cantet C. Bonnefoy M. Bordes S. Bories L. Cufi MN. Dantoine T. Dartigues JF. Desclaux F. Gabelle A. Gasnier Y. Pesce A. Sudres K. Touchon J. Robert P. Rouaud O. Legrand P. Payoux P. Caubere JP. Weiner M. Carrie I. Ousset PJ. Vellas B. Effect of long-term omega 3 polyunsaturated fatty acid supplementation with or without multidomain intervention on cognitive function in elderly adults with memory complaints (mapt): A randomised, placebo-controlled trial. Lancet Neurol. 2017;16:377–389. doi: 10.1016/S1474-4422(17)30040-6. [DOI] [PubMed] [Google Scholar]
- 49.Sikora E. Scapagnini G. Barbagallo M. Curcumin, inflammation, ageing and age-related diseases. Immun Ageing. 2010;7(1) doi: 10.1186/1742-4933-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ganguli M. Chandra V. Kamboh MI. Johnston JM. Dodge HH. Thelma BK. Juyal RC. Pandav R. Belle SH. DeKosky ST. Apolipoprotein e polymorphism and alzheimer disease: The indo-us cross-national dementia study. Arch Neurol. 2000;57:824–830. doi: 10.1001/archneur.57.6.824. [DOI] [PubMed] [Google Scholar]
- 51.Ng TP. Chiam PC. Lee T. Chua HC. Lim L. Kua EH. Curry consumption and cognitive function in the elderly. Am J Epidemiol. 2006;164:898–906. doi: 10.1093/aje/kwj267. [DOI] [PubMed] [Google Scholar]
- 52.Baum L. Lam CW. Cheung SK. Kwok T. Lui V. Tsoh J. Lam L. Leung V. Hui E. Ng C. Woo J. Chiu HF. Goggins WB. Zee BC. Cheng KF. Fong CY. Wong A. Mok H. Chow MS. Ho PC. Ip SP. Ho CS. Yu XW. Lai CY. Chan MH. Szeto S. Chan IH. Mok V. Six-month randomized, placebo-controlled, double-blind, pilot clinical trial of curcumin in patients with alzheimer disease. J Clin Psychopharmacol. 2008;28:110–113. doi: 10.1097/jcp.0b013e318160862c. [DOI] [PubMed] [Google Scholar]
- 53.Ringman JM. Frautschy SA. Teng E. Begum AN. Bardens J. Beigi M. Gylys KH. Badmaev V. Heath DD. Apostolova LG. Porter V. Vanek Z. Marshall GA. Hellemann G. Sugar C. Masterman DL. Montine TJ. Cummings JL. Cole GM. Oral curcumin for alzheimer’s disease: Tolerability and efficacy in a 24-week randomized, double blind, placebo-controlled study. Alzheimers Res Ther. 2012;4:43. doi: 10.1186/alzrt146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hishikawa N. Takahashi Y. Amakusa Y. Tanno Y. Tuji Y. Niwa H. Murakami N. Krishna UK. Effects of turmeric on alzheimer’s disease with behavioral and psychological symptoms of dementia. Ayu. 2012;33:499–504. doi: 10.4103/0974-8520.110524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Begum AN. Jones MR. Lim GP. Morihara T. Kim P. Heath DD. Rock CL. Pruitt MA. Yang F. Hudspeth B. Hu S. Faull KF. Teter B. Cole GM. Frautschy SA. Curcumin structure-function, bioavailability, and efficacy in models of neuroinflammation and alzheimer’s disease. J Pharmacol Exp Ther. 2008;326:196–208. doi: 10.1124/jpet.108.137455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Barbagallo M. Belvedere M. Dominguez LJ. Magnesium homeostasis and aging. Magnes Res. 2009;22:235–246. doi: 10.1684/mrh.2009.0187. [DOI] [PubMed] [Google Scholar]
- 57.Barbagallo M. Dominguez LJ. Magnesium and aging. Curr Pharm Des. 2010;16:832–839. doi: 10.2174/138161210790883679. [DOI] [PubMed] [Google Scholar]
- 58.Choi DW. Ionic dependence of glutamate neurotoxicity. J Neurosci. 1987;7:369–379. doi: 10.1523/JNEUROSCI.07-02-00369.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Altura BT. Altura BM. Withdrawal of magnesium causes vasospasm while elevated magnesium produces relaxation of tone in cerebral arteries. Neurosci Lett. 1980;20:323–327. doi: 10.1016/0304-3940(80)90168-8. [DOI] [PubMed] [Google Scholar]
- 60.Lemke MR. Plasma magnesium decrease and altered calcium/magnesium ratio in severe dementia of the alzheimer type. Biol Psychiatry. 1995;37:341–343. doi: 10.1016/0006-3223(94)00241-T. [DOI] [PubMed] [Google Scholar]
- 61.Durlach J. Magnesium depletion and pathogenesis of alzheimer’s disease. Magnes Res. 1990;3:217–218. [PubMed] [Google Scholar]
- 62.Barbagallo M. Belvedere M. Di Bella G. Dominguez LJ. Altered ionized magnesium levels in mild-to-moderate alzheimer’s disease. Magnes Res. 2011;24:S115–121. doi: 10.1684/mrh.2011.0287. [DOI] [PubMed] [Google Scholar]
- 63.Cilliler AE. Ozturk S. Ozbakir S. Serum magnesium level and clinical deterioration in alzheimer’s disease. Gerontology. 2007;53:419–422. doi: 10.1159/000110873. [DOI] [PubMed] [Google Scholar]
- 64.Lamport DJ. Pal D. Moutsiana C. Field DT. Williams CM. Spencer JP. Butler LT. The effect of flavanol-rich cocoa on cerebral perfusion in healthy older adults during conscious resting state: A placebo controlled, crossover, acute trial. Psychopharmacology (Berl) 2015;232:3227–3234. doi: 10.1007/s00213-015-3972-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sorond FA. Lipsitz LA. Hollenberg NK. Fisher ND. Cerebral blood flow response to flavanol-rich cocoa in healthy elderly humans. Neuropsychiatr Dis Treat. 2008;4:433–440. [PMC free article] [PubMed] [Google Scholar]
- 66.Brickman AM. Khan UA. Provenzano FA. Yeung LK. Suzuki W. Schroeter H. Wall M. Sloan RP. Small SA. Enhancing dentate gyrus function with dietary flavanols improves cognition in older adults. Nat Neurosci. 2014;17:1798–1803. doi: 10.1038/nn.3850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Moreira A. Diogenes MJ. de Mendonca A. Lunet N. Barros H. Chocolate consumption is associated with a lower risk of cognitive decline. J Alzheimers Dis. 2016;53:85–93. doi: 10.3233/JAD-160142. [DOI] [PubMed] [Google Scholar]
- 68.Einother SJ. Martens VE. Acute effects of tea consumption on attention and mood. Am J Clin Nutr. 2013;98:1700S–1708S. doi: 10.3945/ajcn.113.058248. [DOI] [PubMed] [Google Scholar]
- 69.Chen D. Milacic V. Chen MS. Wan SB. Lam WH. Huo C. Landis-Piwowar KR. Cui QC. Wali A. Chan TH. Dou QP. Tea polyphenols, their biological effects and potential molecular targets. Histol Histopathol. 2008;23:487–496. doi: 10.14670/hh-23.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Song J. Xu H. Liu F. Feng L. Tea and cognitive health in late life: Current evidence and future directions. J Nutr Health Aging. 2012;16:31–34. doi: 10.1007/s12603-011-0139-9. [DOI] [PubMed] [Google Scholar]
- 71.Azam S. Hadi N. Khan NU. Hadi SM. Antioxidant and prooxidant properties of caffeine, theobromine and xanthine. Med Sci Monit. 2003;9:BR325–330. [PubMed] [Google Scholar]
- 72.Arendash GW. Mori T. Cao C. Mamcarz M. Runfeldt M. Dickson A. Rezai-Zadeh K. Tane J. Citron BA. Lin X. Echeverria V. Potter H. Caffeine reverses cognitive impairment and decreases brain amyloid-beta levels in aged alzheimer’s disease mice. J Alzheimers Dis. 2009;17:661–680. doi: 10.3233/JAD-2009-1087. [DOI] [PubMed] [Google Scholar]
- 73.Zeitlin R. Patel S. Burgess S. Arendash GW. Echeverria V. Caffeine induces beneficial changes in pka signaling and jnk and erk activities in the striatum and cortex of alzheimer’s transgenic mice. Brain Res. 2011;1417:127–136. doi: 10.1016/j.brainres.2011.08.036. [DOI] [PubMed] [Google Scholar]
- 74.Cao C. Loewenstein DA. Lin X. Zhang C. Wang L. Duara R. Wu Y. Giannini A. Bai G. Cai J. Greig M. Schofield E. Ashok R. Small B. Potter H. Arendash GW. High blood caffeine levels in mci linked to lack of progression to dementia. J Alzheimers Dis. 2012;30:559–572. doi: 10.3233/JAD-2012-111781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Eskelinen MH. Ngandu T. Tuomilehto J. Soininen H. Kivipelto M. Midlife coffee and tea drinking and the risk of late-life dementia: A population-based caide study. J Alzheimers Dis. 2009;16:85–91. doi: 10.3233/JAD-2009-0920. [DOI] [PubMed] [Google Scholar]
- 76.Gelber RP. Petrovitch H. Masaki KH. Ross GW. White LR. Coffee intake in midlife and risk of dementia and its neuropathologic correlates. J Alzheimers Dis. 2011;23:607–615. doi: 10.3233/JAD-2010-101428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Santos C. Costa J. Santos J. Vaz-Carneiro A. Lunet N. Caffeine intake and dementia: Systematic review and meta-analysis. J Alzheimers Dis. 2010;20(Suppl 1):S187–204. doi: 10.3233/JAD-2010-091387. [DOI] [PubMed] [Google Scholar]
- 78.Santos C. Lunet N. Azevedo A. de Mendonca A. Ritchie K. Barros H. Caffeine intake is associated with a lower risk of cognitive decline: A cohort study from portugal. J Alzheimers Dis. 2010;20(Suppl 1):S175–185. doi: 10.3233/JAD-2010-091303. [DOI] [PubMed] [Google Scholar]
- 79.Ritchie K. Carriere I. de Mendonca A. Portet F. Dartigues JF. Rouaud O. Barberger-Gateau P. Ancelin ML. The neuroprotective effects of caffeine: A prospective population study (the three city study) Neurology. 2007;69:536–545. [Google Scholar]
- 80.Arab L. Biggs ML. O’Meara ES. Longstreth WT. Crane PK. Fitzpatrick AL. Gender differences in tea, coffee, and cognitive decline in the elderly: The cardiovascular health study. J Alzheimers Dis. 2011;27:553–566. doi: 10.3233/JAD-2011-110431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Laitala VS. Kaprio J. Koskenvuo M. Raiha I. Rinne JO. Silventoinen K. Coffee drinking in middle age is not associated with cognitive performance in old age. Am J Clin Nutr. 2009;90:640–646. doi: 10.3945/ajcn.2009.27660. [DOI] [PubMed] [Google Scholar]
- 82.Soni M. Rahardjo TB. Soekardi R. Sulistyowati Y. Lestariningsih Yesufu-Udechuku A. Irsan A. Hogervorst E. Phytoestrogens and cognitive function: A review. Maturitas. 2014;77:209–220. doi: 10.1016/j.maturitas.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 83.Alekel DL. Genschel U. Koehler KJ. Hofmann H. Van Loan MD. Beer BS. Hanson LN. Peterson CT. Kurzer MS. Soy isoflavones for reducing bone loss study: Effects of a 3-year trial on hormones, adverse events, and endometrial thickness in postmenopausal women. Menopause. 2015;22:185–197. doi: 10.1097/GME.0000000000000280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Jackson RL. Greiwe JS. Schwen RJ. Emerging evidence of the health benefits of s-equol, an estrogen receptor beta agonist. Nutr Rev. 2011;69:432–448. doi: 10.1111/j.1753-4887.2011.00400.x. [DOI] [PubMed] [Google Scholar]
- 85.Henderson VW. St John JA. Hodis HN. Kono N. McCleary CA. Franke AA. Mack WJ. Long-term soy isoflavone supplementation and cognition in women: A randomized, controlled trial. Neurology. 2012;78:1841–1848. doi: 10.1212/WNL.0b013e318258f822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Baur JA. Sinclair DA. Therapeutic potential of resveratrol: The in vivo evidence. Nat Rev Drug Discov. 2006;5:493–506. doi: 10.1038/nrd2060. [DOI] [PubMed] [Google Scholar]
- 87.Park EJ. Pezzuto JM. The pharmacology of resveratrol in animals and humans. Biochim Biophys Acta. 2015;1852:1071–1113. doi: 10.1016/j.bbadis.2015.01.014. [DOI] [PubMed] [Google Scholar]
- 88.Kennedy DO. Wightman EL. Reay JL. Lietz G. Okello EJ. Wilde A. Haskell CF. Effects of resveratrol on cerebral blood flow variables and cognitive performance in humans: A double-blind, placebo-controlled, crossover investigation. Am J Clin Nutr. 2010;91:1590–1597. doi: 10.3945/ajcn.2009.28641. [DOI] [PubMed] [Google Scholar]
- 89.Witte AV. Kerti L. Margulies DS. Floel A. Effects of resveratrol on memory performance, hippocampal functional connectivity, and glucose metabolism in healthy older adults. J Neurosci. 2014;34:7862–7870. doi: 10.1523/JNEUROSCI.0385-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tome-Carneiro J. Larrosa M. Gonzalez-Sarrias A. Tomas-Barberan FA. Garcia-Conesa MT. Espin JC. Resveratrol and clinical trials: The crossroad from in vitro studies to human evidence. Curr Pharm Des. 2013;19:6064–6093. doi: 10.2174/13816128113199990407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Snitz BE. O’Meara ES. Carlson MC. Arnold AM. Ives DG. Rapp SR. Saxton J. Lopez OL. Dunn LO. Sink KM. DeKosky ST. Ginkgo biloba for preventing cognitive decline in older adults: A randomized trial. JAMA. 2009;302:2663–2670. doi: 10.1001/jama.2009.1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ray B. Chauhan NB. Lahiri DK. The “aged garlic extract:” (age) and one of its active ingredients s-allyl-l-cysteine (sac) as potential preventive and therapeutic agents for alzheimer’s disease (ad) Curr Med Chem. 2011;18:3306–3313. doi: 10.2174/092986711796504664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kumar S. Dual inhibition of acetylcholinesterase and butyrylcholinesterase enzymes by allicin. Indian J Pharmacol. 2015;47:444–446. doi: 10.4103/0253-7613.161274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Nooyens AC. Bueno-de-Mesquita HB. van Boxtel MP. van Gelder BM. Verhagen H. Verschuren WM. Fruit and vegetable intake and cognitive decline in middle-aged men and women: The doetinchem cohort study. Br J Nutr. 2011;106:752–761. doi: 10.1017/S0007114511001024. [DOI] [PubMed] [Google Scholar]
- 95.Grodstein F. Kang JH. Glynn RJ. Cook NR. Gaziano JM. A randomized trial of beta carotene supplementation and cognitive function in men: The physicians’ health study ii. Arch Intern Med. 2007;167:2184–2190. doi: 10.1001/archinte.167.20.2184. [DOI] [PubMed] [Google Scholar]
- 96.Ford AH. Flicker L. Alfonso H. Thomas J. Clarnette R. Martins R. Almeida OP. Vitamins b(12), b(6), and folic acid for cognition in older men. Neurology. 2010;75:1540–1547. doi: 10.1212/WNL.0b013e3181f962c4. [DOI] [PubMed] [Google Scholar]
- 97.Wald DS. Kasturiratne A. Simmonds M. Effect of folic acid, with or without other b vitamins, on cognitive decline: Meta-analysis of randomized trials. Am J Med. 2010;123:522–527 e522. doi: 10.1016/j.amjmed.2010.01.017. [DOI] [PubMed] [Google Scholar]
- 98.Walker JG. Batterham PJ. Mackinnon AJ. Jorm AF. Hickie I. Fenech M. Kljakovic M. Crisp D. Christensen H. Oral folic acid and vitamin b-12 supplementation to prevent cognitive decline in community-dwelling older adults with depressive symptoms--the beyond ageing project: A randomized controlled trial. Am J Clin Nutr. 2012;95:194–203. doi: 10.3945/ajcn.110.007799. [DOI] [PubMed] [Google Scholar]
- 99.Kang JH. Cook N. Manson J. Buring JE. Grodstein F. A randomized trial of vitamin e supplementation and cognitive function in women. Arch Intern Med. 2006;166:2462–2468. doi: 10.1001/archinte.166.22.2462. [DOI] [PubMed] [Google Scholar]
- 100.Fillenbaum GG. Kuchibhatla MN. Hanlon JT. Artz MB. Pieper CF. Schmader KE. Dysken MW. Gray SL. Dementia and alzheimer’s disease in community-dwelling elders taking vitamin c and/or vitamin e. Ann Pharmacother. 2005;39:2009–2014. doi: 10.1345/aph.1G280. [DOI] [PubMed] [Google Scholar]
- 101.Maxwell CJ. Hicks MS. Hogan DB. Basran J. Ebly EM. Supplemental use of antioxidant vitamins and subsequent risk of cognitive decline and dementia. Dement Geriatr Cogn Disord. 2005;20:45–51. doi: 10.1159/000085074. [DOI] [PubMed] [Google Scholar]
- 102.Morris MC. Schneider JA. Li H. Tangney CC. Nag S. Bennett DA. Honer WG. Barnes LL. Brain tocopherols related to alzheimer’s disease neuropathology in humans. Alzheimers Dement. 2015;11:32–39. doi: 10.1016/j.jalz.2013.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Llewellyn DJ. Lang IA. Langa KM. Melzer D. Vitamin d and cognitive impairment in the elderly u.S. Population. J Gerontol A Biol Sci Med Sci. 2011;66:59–65. doi: 10.1093/gerona/glq185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Rossom RC. Espeland MA. Manson JE. Dysken MW. Johnson KC. Lane DS. LeBlanc ES. Lederle FA. Masaki KH. Margolis KL. Calcium and vitamin d supplementation and cognitive impairment in the women’s health initiative. J Am Geriatr Soc. 2012;60:2197–2205. doi: 10.1111/jgs.12032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yaffe K. Clemons TE. McBee WL. Lindblad AS. Impact of antioxidants, zinc, and copper on cognition in the elderly: A randomized, controlled trial. Neurology. 2004;63:1705–1707. doi: 10.1212/01.wnl.0000142969.19465.8f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kang JH. Cook NR. Manson JE. Buring JE. Albert CM. Grodstein F. Vitamin e, vitamin c, beta carotene, and cognitive function among women with or at risk of cardiovascular disease: The women’s antioxidant and cardiovascular study. Circulation. 2009;119:2772–2780. doi: 10.1161/CIRCULATIONAHA.108.816900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mucke L. Neuroscience: Alzheimer’s disease. Nature. 2009;461:895–897. doi: 10.1038/461895a. [DOI] [PubMed] [Google Scholar]
- 108.Sofi F. Abbate R. Gensini GF. Casini A. Accruing evidence on benefits of adherence to the mediterranean diet on health: An updated systematic review and meta-analysis. Am J Clin Nutr. 2010;92:1189–1196. doi: 10.3945/ajcn.2010.29673. [DOI] [PubMed] [Google Scholar]
- 109.Singh B. Parsaik AK. Mielke MM. Erwin PJ. Knopman DS. Petersen RC. Roberts RO. Association of mediterranean diet with mild cognitive impairment and alzheimer’s disease: A systematic review and meta-analysis. J Alzheimers Dis. 2014;39:271–282. doi: 10.3233/JAD-130830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Estruch R. Ros E. Salas-Salvado J. Covas MI. Corella D. Aros F. Gomez-Gracia E. Ruiz-Gutierrez V. Fiol M. Lapetra J. Lamuela-Raventos RM. Serra-Majem L. Pinto X. Basora J. Munoz MA. Sorli JV. Martinez JA. Martinez-Gonzalez MA. Primary prevention of cardiovascular disease with a mediterranean diet. N Engl J Med. 2013;368:1279–1290. doi: 10.1056/NEJMc1806491. [DOI] [PubMed] [Google Scholar]
- 111.Valls-Pedret C. Sala-Vila A. Serra-Mir M. Corella D. de la Torre R. Martinez-Gonzalez MA. Martinez-Lapiscina EH. Fito M. Perez-Heras A. Salas-Salvado J. Estruch R. Ros E. Mediterranean diet and age-related cognitive decline: A randomized clinical trial. JAMA Intern Med. 2015;175:1094–1103. doi: 10.1001/jamainternmed.2015.1668. [DOI] [PubMed] [Google Scholar]
- 112.Martinez-Lapiscina EH. Clavero P. Toledo E. Estruch R. Salas-Salvado J. San Julian B. Sanchez-Tainta A. Ros E. Valls-Pedret C. Martinez-Gonzalez MA. Mediterranean diet improves cognition: The predimed-navarra randomised trial. J Neurol Neurosurg Psychiatry. 2013;84:1318–1325. doi: 10.1136/jnnp-2012-304792. [DOI] [PubMed] [Google Scholar]
- 113.Scarmeas N. Stern Y. Tang MX. Mayeux R. Luchsinger JA. Mediterranean diet and risk for alzheimer’s disease. Ann Neurol. 2006;59:912–921. doi: 10.1002/ana.20854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Scarmeas N. Luchsinger JA. Mayeux R. Stern Y. Mediterranean diet and alzheimer disease mortality. Neurology. 2007;69:1084–1093. doi: 10.1212/01.wnl.0000277320.50685.7c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Scarmeas N. Stern Y. Mayeux R. Manly JJ. Schupf N. Luchsinger JA. Mediterranean diet and mild cognitive impairment. Arch Neurol. 2009;66:216–225. doi: 10.1001/archneurol.2008.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Scarmeas N. Luchsinger JA. Schupf N. Brickman AM. Cosentino S. Tang MX. Stern Y. Physical activity, diet, and risk of alzheimer disease. JAMA. 2009;302:627–637. doi: 10.1001/jama.2009.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Gu Y. Luchsinger JA. Stern Y. Scarmeas N. Mediterranean diet, inflammatory and metabolic biomarkers, and risk of alzheimer’s disease. J Alzheimers Dis. 2010;22:483–492. doi: 10.3233/JAD-2010-100897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Feart C. Samieri C. Rondeau V. Amieva H. Portet F. Dartigues JF. Scarmeas N. Barberger-Gateau P. Adherence to a mediterranean diet, cognitive decline, and risk of dementia. JAMA. 2009;302:638–648. doi: 10.1001/jama.2009.1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Feart C. Torres MJ. Samieri C. Jutand MA. Peuchant E. Simopoulos AP. Barberger-Gateau P. Adherence to a mediterranean diet and plasma fatty acids: Data from the bordeaux sample of the three-city study. Br J Nutr. 2011;106:149–158. doi: 10.1017/S0007114510005805. [DOI] [PubMed] [Google Scholar]
- 120.Solfrizzi V. Panza F. Frisardi V. Seripa D. Logroscino G. Imbimbo BP. Pilotto A. Diet and alzheimer’s disease risk factors or prevention: The current evidence. Expert Rev Neurother. 2011;11:677–708. doi: 10.1586/ern.11.56. [DOI] [PubMed] [Google Scholar]
- 121.Cherbuin N. Anstey KJ. The mediterranean diet is not related to cognitive change in a large prospective investigation: The path through life study. Am J Geriatr Psychiatry. 2012;20:635–639. doi: 10.1097/JGP.0b013e31823032a9. [DOI] [PubMed] [Google Scholar]
- 122.Gardener S. Gu Y. Rainey-Smith SR. Keogh JB. Clifton PM. Mathieson SL. Taddei K. Mondal A. Ward VK. Scarmeas N. Barnes M. Ellis KA. Head R. Masters CL. Ames D. Macaulay SL. Rowe CC. Szoeke C. Martins RN. Adherence to a mediterranean diet and alzheimer’s disease risk in an australian population. Transl Psychiatry. 2012;2:e164. doi: 10.1038/tp.2012.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Tangney CC. Kwasny MJ. Li H. Wilson RS. Evans DA. Morris MC. Adherence to a mediterranean-type dietary pattern and cognitive decline in a community population. Am J Clin Nutr. 2011;93:601–607. doi: 10.3945/ajcn.110.007369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Yannakoulia M. Kontogianni M. Scarmeas N. Cognitive health and mediterranean diet: Just diet or lifestyle pattern? Ageing Res Rev. 2015;20:74–78. doi: 10.1016/j.arr.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 125.Tyson CC. Nwankwo C. Lin PH. Svetkey LP. The dietary approaches to stop hypertension (dash) eating pattern in special populations. Curr Hypertens Rep. 2012;14:388–396. doi: 10.1007/s11906-012-0296-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Wengreen H. Munger RG. Cutler A. Quach A. Bowles A. Corcoran C. Tschanz JT. Norton MC. Welsh-Bohmer KA. Prospective study of dietary approaches to stop hypertension- and mediterranean-style dietary patterns and age-related cognitive change: The cache county study on memory, health and aging. Am J Clin Nutr. 2013;98:1263–1271. doi: 10.3945/ajcn.112.051276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Morris MC. Tangney CC. Wang Y. Sacks FM. Barnes LL. Bennett DA. Aggarwal NT. Mind diet slows cognitive decline with aging. Alzheimers Dement. 2015 doi: 10.1016/j.jalz.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Morris MC. Tangney CC. Wang Y. Sacks FM. Bennett DA. Aggarwal NT. Mind diet associated with reduced incidence of alzheimer’s disease. Alzheimers Dement. 2015 doi: 10.1016/j.jalz.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Huijbregts PP. Feskens EJ. Rasanen L. Fidanza F. Alberti-Fidanza A. Nissinen A. Giampaoli S. Kromhout D. Dietary patterns and cognitive function in elderly men in finland, italy and the netherlands. Eur J Clin Nutr. 1998;52:826–831. doi: 10.1038/sj.ejcn.1600654. [DOI] [PubMed] [Google Scholar]
- 130.Correa Leite ML. Nicolosi A. Cristina S. Hauser WA. Nappi G. Nutrition and cognitive deficit in the elderly: A population study. Eur J Clin Nutr. 2001;55:1053–1058. doi: 10.1038/sj.ejcn.1601270. [DOI] [PubMed] [Google Scholar]
- 131.Shatenstein B. Ferland G. Belleville S. Gray-Donald K. Kergoat MJ. Morais J. Gaudreau P. Payette H. Greenwood C. Diet quality and cognition among older adults from the nuage study. Exp Gerontol. 2012;47:353–360. doi: 10.1016/j.exger.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 132.Wengreen HJ. Neilson C. Munger R. Corcoran C. Diet quality is associated with better cognitive test performance among aging men and women. J Nutr. 2009;139:1944–1949. doi: 10.3945/jn.109.106427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Yamada T. Kadekaru H. Matsumoto S. Inada H. Tanabe M. Moriguchi EH. Moriguchi Y. Ishikawa P. Ishikawa AG. Taira K. Yamori Y. Prevalence of dementia in the older japanese-brazilian population. Psychiatry Clin Neurosci. 2002;56:71–75. doi: 10.1046/j.1440-1819.2002.00931.x. [DOI] [PubMed] [Google Scholar]
- 134.Giem P. Beeson WL. Fraser GE. The incidence of dementia and intake of animal products: Preliminary findings from the adventist health study. Neuroepidemiology. 1993;12:28–36. doi: 10.1159/000110296. [DOI] [PubMed] [Google Scholar]
- 135.Boraxbekk CJ. Stomby A. Ryberg M. Lindahl B. Larsson C. Nyberg L. Olsson T. Diet-induced weight loss alters functional brain responses during an episodic memory task. Obes Facts. 2015;8:261–272. doi: 10.1159/000437157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Reger MA. Henderson ST. Hale C. Cholerton B. Baker LD. Watson GS. Hyde K. Chapman D. Craft S. Effects of beta-hydroxybutyrate on cognition in memory-impaired adults. Neurobiol Aging. 2004;25:311–314. doi: 10.1016/S0197-4580(03)00087-3. [DOI] [PubMed] [Google Scholar]
- 137.Henderson ST. Vogel JL. Barr LJ. Garvin F. Jones JJ. Costantini LC. Study of the ketogenic agent ac-1202 in mild to moderate alzheimer’s disease: A randomized, double-blind, placebo-controlled, multicenter trial. Nutr Metab (Lond) 2009;6:31. doi: 10.1186/1743-7075-6-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Morris MC. Evans DA. Tangney CC. Bienias JL. Schneider JA. Wilson RS. Scherr PA. Dietary copper and high saturated and trans fat intakes associated with cognitive decline. Arch Neurol. 2006;63:1085–1088. doi: 10.1001/archneur.63.8.1085. [DOI] [PubMed] [Google Scholar]
- 139.Pajonk FG. Kessler H. Supprian T. Hamzei P. Bach D. Schweickhardt J. Herrmann W. Obeid R. Simons A. Falkai P. Multhaup G. Bayer TA. Cognitive decline correlates with low plasma concentrations of copper in patients with mild to moderate alzheimer’s disease. J Alzheimers Dis. 2005;8:23–27. doi: 10.3233/jad-2005-8103. [DOI] [PubMed] [Google Scholar]
- 140.Squitti R. Siotto M. Polimanti R. Low-copper diet as a preventive strategy for alzheimer’s disease. Neurobiol Aging. 2014;35(Suppl 2):S40–50. doi: 10.1016/j.neurobiolaging.2014.02.031. [DOI] [PubMed] [Google Scholar]
- 141.Loef M. Walach H. Copper and iron in alzheimer’s disease: A systematic review and its dietary implications. Br J Nutr. 2012;107:7–19. doi: 10.1017/S000711451100376X. [DOI] [PubMed] [Google Scholar]


