Abstract
Aim: to finding what young patients with type-1 diabetes (T1D) knows about their body and also on their illness in perspective to tailor educational interventions to their real ability to understand. Methods: the present study involved 68 children with T1D , 5 to 14 years old with a duration of diabetes ranging from 2 to 6 years and a total HbA1c mean value of 7.96±0.87%. The sample was divided into two age Groups: 28 children 5 to 10 years old were gathered in the Group 1 and 40 teenagers aged from 11 to 14 years in the Group 2. These patients were invited to draw over a white paper using a black pencil “The human body as it is made inside”. Subsequently they were asked to explain: “what is diabetes?” and “where does insulin go?”. According to the methodology of the “interactive drawing”, the interviewer interacted with the children while drawing, forcing them to verbalize the reasons for their choices, to justify their proceeding, to explain their plan and then to explicit their theories. Drawings and replies were classified as Correct, Correct-but-Incomplete and Incorrect. Results: the overall production of correct/correct-but-incomplete drawings was 83.82% vs 16.20% of the incorrect ones. One-hundred of the children who have produced a correct drawing supplied also a correct verbal reply, whereas 100% of the children who have produced an incorrect drawing was unable to supply any information on diabetes or about insulin. Both younger and older subjects who produced a complete-but-incorrect drawing appeared to have misunderstood the action of insulin therapy (only 23% and 17% of correct replies). Children who produced incomplete drawings and provided incorrect replies to the questions about their disease showed also a HbA1c mean value higher (8.36±0.97%) compared to the children who drew and answered correctly (p=0.0023). Conclusions: the operative epistemic approach could represent a promising tool for a health professional team to verify the real understanding acquired by a child about T1D, and to provide pediatrician a guideline to directly communicate with his patient. (www.actabiomedica.it)
Keywords: Type 1 diabetes, medical-patient communication, Piagetian psycho-epistemology, infantile drawing, graphic representation, child
Introduction
The primary goal of a diabetes team is to ensure the patients reach and maintain a high level of their disease management. From this point of view, the quality of medical-patient communication is of crucial importance. The target is easy to be attained between a practitioner and an adult patient, but some barriers may obstruct or delay the achievement of same result between pediatrician and a child with Type-1 diabetes (T1D).
The pediatrician is faced with an individual with different cognitive and communicative abilities which continue to change during his development (1). The pediatrician has also to deal with a number of adult interlocutors (parents), who have an important cognitive and emotional influence for a child.
Given these barriers, it is difficult for a pediatrician to understand in which way a child with T1D has received and processed the messages relating to diabetes. An aid could result to him from methods and techniques borrowed from the developmental psychology, which could make easier to decode the information expressed by a child, and to verify his knowledge degree about diabetes and its management.
Psychologists regularly employ drawing as a technical tool to communicate with the child’s mental world (2, 3). Drawing is fun for a child, whereas for pediatricians or psychologists it may also become a “story” that the child tells about himself, about his disease, the theories on his disease, and on inner world and emotions (4, 5). These studies in T1D field are very few (6, 7), conversely for other diseases there is more documentation (7-9).
In this scenario we speculated that children with T1D who had correctly processed the received therapeutic information would be able to produce more adequate graphic representations of their body and disease than the children who had processed the same information in an inaccurate way. To test this hypothesis we referred to the operative epistemic interview, mediated by a graphic representation. According to Piagetian psycho-epistemology, drawing is an opportunity for a child not only to express his emotions but also his “theories” about the world around him and what is in him (10). To our knowledge, there are no studies on this type of approach aimed at finding what a young patient with T1D knows about his body and also on his illness in perspective to tailor information and educational interventions to his real ability to understand. Herein we reported the results of this unusual test.
Materials and methods
The present study involved children with T1D followed at the Regional Diabetes Center for children of the University Hospital of Parma, Italy, who met the following criteria: chronological age <14 years, diabetes duration >2 years, no diabetes-related complications, normal cognitive development, voluntary participation supported by patient assent and parents informed consent. At diagnosis, a standard integrated care package was made available to involved parents and patients by a multidisciplinary team. The team consisted of pediatric diabetologists, diabetes specialist nurses, dieticians, psychologists. Repeated educational advices on diabetes management, hypoglycemic episodes and diabetes ketoacidosis prevention were provided during hospitalization and in outpatient clinic. Sticks for capillary blood glucose determination, urine glucose assay, insulin and syringes were free distributed. An emergency toll-free telephone number was also provided (11). The patients were routinely followed in outpatient clinic regimen four times per year.
Experienced pediatricians or psychologists belonging to the same Diabetes Center invited recruited patients to draw over a white paper using a black pencil “The human body as it is made inside”. Subsequently they were asked to explain: “what is diabetes?” and “where does insulin go?”. Drawings and interviews were performed in a comfortable and soundproof environment, without the presence of parents. According to the methodology of the “interactive drawing”, the interviewer was interacting with the child while drawing, forcing him to verbalize the reasons for his choices, to justify his proceeding, to explain his plan and then to explicit his theories (12). The interviews were video-recorded and later analyzed by the same team. The explanations were literally transcribed.
The drawings and replies about both diabetes and insulin have been analyzed from a quantity and a quality point of view, and they have been classified into three categories: Correct, Correct but Incomplete and Incorrect.
Diabetes control was evaluated by the mean of Glycated hemoglobin (HbA1c) values collected during the 12 months preceding the recruitment in the study. HbA1c was assayed in out-patient clinic by Bayer DCA-2000 system (upper limit of normal value: 6.0%) (13).
Statistics
Data were summarized as numbers (n) and frequencies (%) if they were categorical and as mean and standard deviation (SD) if quantitative. If the data were normally distributed a two-tailed unpaired T-test or otherwise a non-parametric Mann-Whitney U-Test was applied in order to compare results between groups. Chi-square test (ξ2) or Fisher exact test was used to compare frequencies between groups. P-values less than 0.05 were considered as statistically significant.
Results
Sixty-height patients were enrolled in the study, 36 females, 5 to 14 years old (mean age: 9.24±1.6) with a duration of diabetes ranging from 2 to 6 years. The total HbA1c mean value was 7.96±0.87%. None of the patients experienced episodes of diabetic ketoacidosis nor severe hypoglycemia in the previous year. The sample was then divided into two age Groups: 28 children 5 to 10 years old were gathered in the Group 1 and 40 teenagers aged from 11 to 14 years in the Group 2. Their characteristics are summarized in the Table 1.
Table 1.
Characteristics of study participants
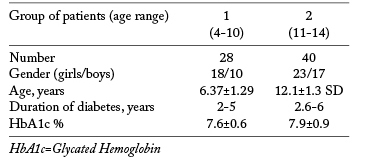
Table 2 lists the frequencies and relative percentage frequencies in the drawings classified as mentioned above. The overall production of correct/correct-but-incomplete drawings was 83.82% vs 16.20% of the incorrect ones. The Chi-square value was not significant (ξ2=3.83; gl=2; p=0.147). However, a higher trend in incorrect drawings production was found in younger compared to older children (25% vs 10%).
Table 2.
Classification of drawings produced by the two Groups of patients
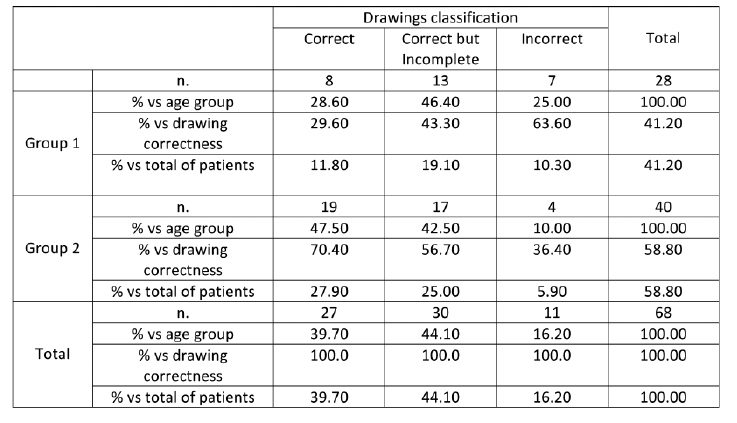
Table 3 displays the frequency of replies on the question “What is diabetes?” and the relationship with drawings correctness supplied by the two Groups of patients. One-hundred of the children who have produced a correct drawing supplied also a correct verbal reply, whereas 100% of the children who have produced an incorrect drawing was unable to supply any information on diabetes. Among those who produced a correct but incomplete drawing 30.8% provided in any case a correct reply, whereas 38.5% replied in an incorrect way and 30.8% was unable to give explanations. The Chi-square value calculation showed a significant correlation between the correctness of the drawings and that of the replies about diabetes furnished by the younger children (ξ2=25.259; gl=4; P=0.0001).
Table 3.
Relationship between drawings correctness and answers on “What is diabetes?” in the patients gathered in Groups 1 and 2
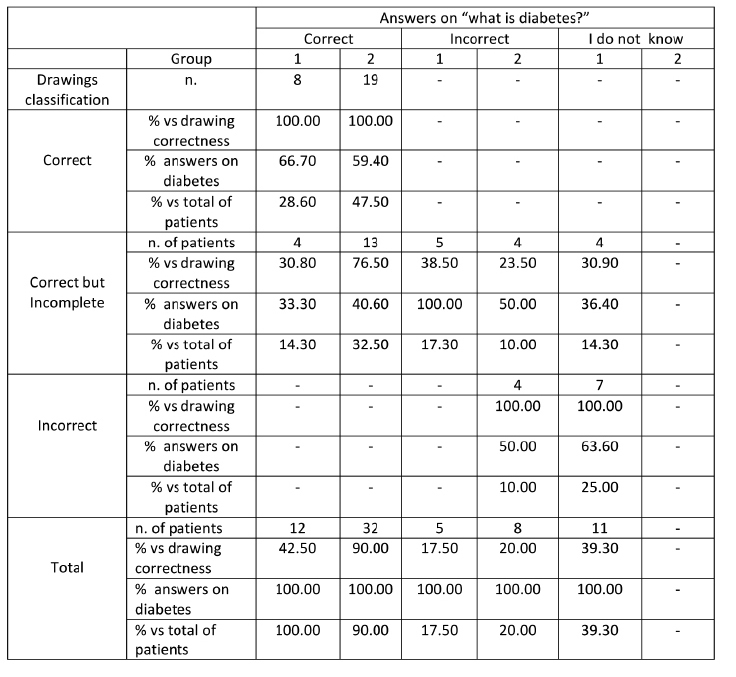
Also among the older children 100% of those who produced a correct drawing gave also a correct verbal reply, whereas 100% of those who produced an incorrect drawing was unable to provide any explanation on “What is diabetes”. Among those who produced a correct but incomplete drawing, 76.5% replied correctly, whereas 23.5% provided an incorrect reply. The Chi-square value calculation confirmed the existence of a significant correlation between the correctness of the drawing and that of the replies on diabetes supplied by the older children (ξ2=25.259; gl=4; P=0.0001).
Table 4 finally shows the frequencies distribution relating to the replies supplied on insulin, by the two Groups of children. With reference to the replies provided on insulin we found that 100% of children who produced a correct drawing also showed a correct verbal reply, whereas 100% of those who produced an incorrect drawing was unable to provide any explanation on insulin. Among those who produced a correct but incomplete drawing, 23.1% of children provided in any case a correct reply, whereas 69.2% gave an incorrect reply and 7.7% was unable to reply. The Chi-square value calculated on the frequencies observed in table 2 confirms the existence of a significant correlation between the correctness of the drawings and the correctness of the replies on insulin supplied by the younger children (ξ2=38.280; gl=4; P=.0001). Also among the older children we found that 100% of those who produced a correct drawing also supplied a correct verbal reply, whereas 75% of those who produced an incorrect drawing provides an incorrect reply on insulin. The remaining 25% was unable to reply. Among those who produced a correct but incomplete drawing, 17.6% provided in any case a correct reply, whereas 82.4% provides an incorrect reply. Also among the older children, the Chi-square value calculated on the observed frequencies confirmed the existence of a significant correlation between drawings correctness and the replies correctness on insulin (ξ2=37.93; gl=4; p=0.0001). Both younger and older subjects who produced a complete-but-incorrect drawing appeared to have misunderstood the action of insulin therapy (only 23% and 17% of correct replies). In particular, they state that insulin goes directly into the pancreas.
Table 4.
Relationship between drawings correctness and answers on “Where does insulin go?” in the patients gathered in Groups 1 and 2
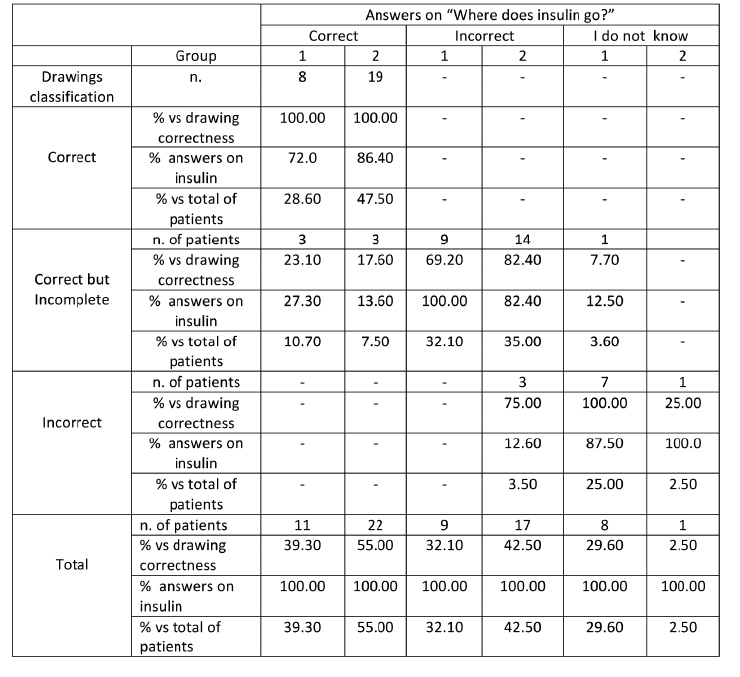
Children who produced incomplete drawings and provided incorrect replies to the questions about their disease also showed a HbA1c mean value higher (8.36±0.97%) compared to the children who correctly drew and answered (7.76±0.58%; p=3.17; p=0.0023).
Discussion
Three major findings come out from the present study: 1) 84% of children herein investigated showed to have a correct graphic representation of their body; 2) 100% of children who produced a correct drawing supplied also a correct verbal reply to the questions concerning their disease and relative treatment; 3) 100% of the children who made an incorrect drawing was unable to furnish any information on diabetes and insulin. These results could have a great practical value from the point of view of medical-patient communication.
It is in our opinion that a pediatric team might be able to modulate educational intervention in a child with T1D based on his cognitive development. According to J. Piaget, children spontaneously elaborate “their own theories” on the world around them and on what is inside them with a gradual evolution during their life (1). These theories are often in disagreement with the so-called “official theories” of adults. If this infantile theorization is neglected, medical-patient communication could result difficult, since medical advices will inevitably be filtered and distorted by the different spontaneous theories of the child.
A means of avoiding this conflict could be the use of the epistemic interview technique mediated by a graphical representation, called an interactive drawing, like that it was used in the present study. Interactive drawing is a technique in which children are asked to draw the object or concept in question (the human body in our case). During the meeting the interviewer could intervene in the drawing process to interrogate children about their work, in order to bring out the theories that are leading the representation and that, without interviewer intervention, would remain implicit and inaccessible (14 ). This is a different approach compared to the routine tests focused on the projective aspect of an infantile drawing in which the interviewer never intervenes during the drawing production, in order not to influence the drawing projective value, and delays his interpretation only after the drawing has been completed.
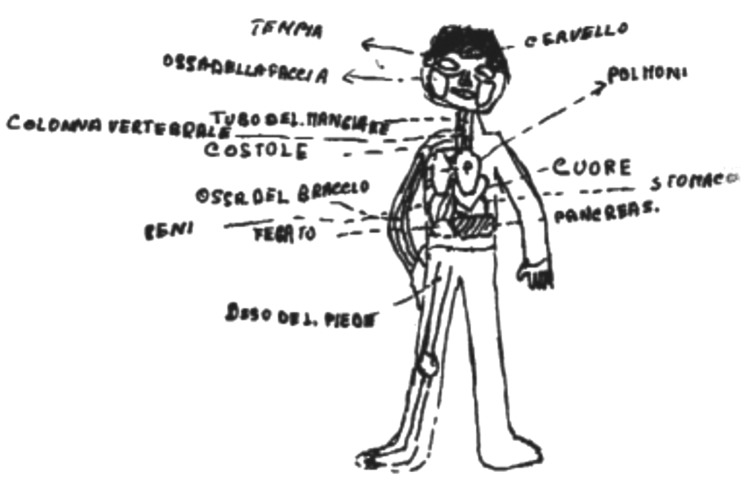
Faced with children who have theories very close to the official ones, the therapeutic team is facilitated in interacting with them to transmit information useful to understand the disease and its management. It is the case of Tommaso, a teenager of 10.6 years old, diabetic since the age of 5, who proposed a drawing that is almost an anatomical atlas (Figure 1). His representation is correct: To the question “What is diabetes?” he replied “The pancreas cannot work normally and to help it a stimulus is needed, so at 7 a small insulin syringe is made”. Who describes well his body also well explains his disease.
Figure 1.
Tommaso, 10.6 years old, proposed a drawing that is almost an anatomical atlas. To the question “What is diabetes?” he replied “The pancreas cannot work normally and to help it a stimulus is needed, so at 7 a small insulin syringe is made”.
Conversely, a child with limited representation skills will have a greater difficulty in understanding his illness and treatment. Filippo is 7 years old and showed little information about his body (Figure 2). To the question “what is diabetes?” he answered “A disease that can be bad. It affects the pancreas, is hit by a virus and gets sick so I have to make insulin bites”. A theory close enough to the official one. To the question “Where does insulin go?” he replied “Insulin goes to the pancreas”. This answer is consistent with his own theory of the sick pancreas.
Figure 2.
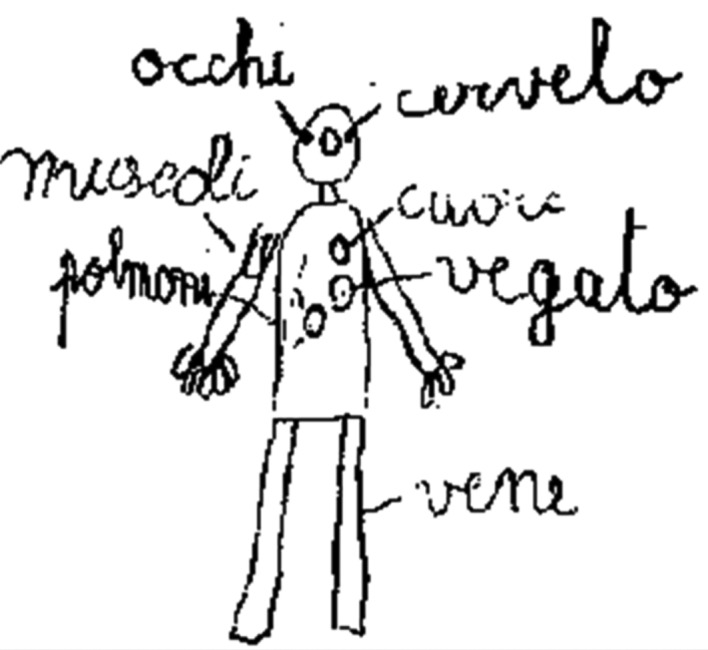
Filippo, 7 years old, showed little information about his body. To the question “What is diabetes?” he answered “A disease that can be bad. It affects the pancreas, is hit by a virus and gets sick so I have to make insulin bites”
Figure 3.

Luigi, 7 years old, his drawing showed a lack of body representation. To the question “What is diabetes?” he explained: “A disease ... there is chickenpox, the flu, sinusitis and diabetes”
Luigi is the same age as Filippo, his drawing showed a lack of representation and he did not have theories about the disease: “What is diabetes?”. He explained: “A disease ... there is chickenpox, the flu, sinusitis and diabetes. “Where does insulin go?” He replied: “In the body.” It is clear that some members of the team in this case have excessively minimized diabetes explanation by creating confusion in the theories of Luigi who he is now prone to underestimate his illness.
There is no doubt that given the representations and theories of Filippo and Luigi the diabetes team would have had to follow different educational procedures compared to those used with Tommaso. Using the operative epistemic approach the interviewer could have intervened during the drawing process asking Filippo and Luigi for explanations, observing anomalies, suggesting alternative hypotheses or helping the two patients to complete the drawing. Shortly, the interviewer could have interact with them to verbalize the reasons for their choices and to understand their theories in order to find the best information that would meet their cognitive resources.
A child who shows limited abilities in body representation has more difficulty of another to attaint good adherence to therapy. In fact children with incorrect drawings/replies had a poorer metabolic control than those children who grew/answered correctly. This finding would be sufficient to encourage the use of the operative epistemic approach to plan the educational program in children with T1D, especially in the younger ones, or with patients who refuse the disease. The pediatrician could use the same technique if he wants to check whether the children’s verbal statements are actually the result of their own personal interpretation on diabetes rather than verbal labels that have been dogmatically learnt. Children with T1D who have not rationalized the ineluctability of the manipulation of their body with insulin injections and repeated tests for the blood glucose measurement, not due to bad determination but due to cognitive immaturity, hardly gives emotional and operational guarantees necessary to achieve the objectives of good metabolic control
In conclusion, the operative epistemic approach seems to represent a promising tool for the pediatrician to communicate with his patient. The drawing could stimulate the collaboration of children, being a procedure particularly appreciated by the children. It could offer a direct interpretation of the real understanding acquired by the children, providing pediatrician a guideline to start a dialogue, overcoming any barrier due to the children’s difficulties in expressing themselves verbally. It could also help to reduce communication interferences caused by the parents interpretative mediation. Through this approach the pediatrician could finally build a direct dialogue with his patients, who through the graphic representation will express their own personal representation and interpretation of the events.
Acknowledgements
We are grateful to Dr. Rossana Di Marzio for the editorial support.
Footnotes
(*) In memory of Franca Cavara Medioli and Maria Gugliotta, Psychologists
References
- 1.Piaget J. Paris: Alcan; 1926. La représentation du monde chez l’enfant. [Google Scholar]
- 2.Corman L. Paris: Presses Universitaires de France; 1970. Le test du dessin de la famille. [Google Scholar]
- 3.Medioli Cavara F. Boringhieri: Esercitazioni psicodiagnostiche; 1986. Il disegno nell’età evolutiva. [Google Scholar]
- 4.Munari A. Filippini G. Regazzoni M. Visseur AS. L’anatomie de l’enfant: Etude épistémogénétique des notions anatomiques spontanées. Archives de Psychologie. 1976;44:115–134. [Google Scholar]
- 5.Fabbri MD. Usuelli L. Université de Genève, Mémoire de Diplôme; 1988. Nous sommes des usines à sucre: Qu’est-ce que c’est le diabète pour un adulte diabétique? # rero 1076506. [Google Scholar]
- 6.Pera PI. Lois MP. Lopez Matheu C, et al. Perceptions of diabetes obtained through drawing in childhood and adolescence. Patient Preference and Adherence. 2013;7:595–605. doi: 10.2147/PPA.S45130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rollins JA. Tell me about it: drawing as a communication tool for children with cancer. J Pediatr Oncol Nurs. 2005;22:203–221. doi: 10.1177/1043454205277103. [DOI] [PubMed] [Google Scholar]
- 8.Redelstein K. Dennis M. Copeland K, et al. Motor learning in children with spina bifida: dissociation between performance level and acquisition rate. J Int Neuropsychol Soc. 2004;10:877–887. doi: 10.1017/s1355617704106085. [DOI] [PubMed] [Google Scholar]
- 9.Gabriels RL. Wamboldt MZ. McCormick DR. Adams TL. McTaggart SR. Children’s illness drawings and asthma symptom awareness. J Asthma. 2000;37:565–574. doi: 10.3109/02770900009090811. [DOI] [PubMed] [Google Scholar]
- 10.Munari A. Il disegno infantile come strumento di dialogo fra il paziente e il team diabetologico- pediatrico. Milano: In Pagina; 2001. Il disegno interattivo: un terreno di incontro e di dialogo tra terapeuta e paziente. In Creatività e comunicazione; pp. 16–23. [Google Scholar]
- 11.Vanelli M. “Hello, diabetes.” Preventing DKA in children with a telephone hotline service. Diabetes Voice. 2008;53:22–24. [Google Scholar]
- 12.Frison D. The mediated interview: new developments of the cognitive critical interview of Jean Piaget. ECPS Journal. 2016;13:193–211. [Google Scholar]
- 13.Vanelli M. De Fanti A. Avantaggiato S, et al. Performance e utilità di un metodo immunologico rapido per il dosaggio dell’HbA1c nell’ambulatorio diabetologico. Minerva Pediatrica. 1993;9:373–77. [PubMed] [Google Scholar]
- 14.Fabbri D. Munari A. A psycho-cultural approach to health education. European Health Psychology Society Conference; 1991 August 28-30; Lausanne. [Google Scholar]