Abstract
Scapular fractures are one of the most difficult fractures to diagnose on radiographs. Detection can be challenging because of the obscuration by the overlying structures or incomplete imaging due to difficult patient collaboration. Familiarity with imaging characteristics of these abnormalities will allow radiologists to better diagnose and characterize scapular fractures. Three-dimensional computed tomographic scans are considered the gold standard for scapular diagnoses. Treatment strategies differ depending on the type of scapular fractures, but the site and degree of displacement will determine whether surgical intervention should be considered. Complications can occur in fractures that are undiagnosed or improperly evaluated. The purpose of this article is to describe imaging features of traumatic scapular injury, and discuss the role of diagnostic imaging in clinical decision making after shoulder trauma. (www.actabiomedica.it)
Keywords: scapula, fractures, diagnostic imaging
Scapular fractures are uncommon, accounting for only 3-5% of shoulder girdle fractures and for less than 1% of all fractures (1-3). Such fractures have the potential to cause long term complications such significant chronic pain and to alter normal function of the shoulder girdle as a result of malunion, nonunion, rotator cuff dysfunction, scapulothoracic dyskinesis, or impingement.
High-energy trauma is the most common cause, and for this reason scapular fractures are frequently associated with other acute injuries (4-7). Direct force may cause fractures in all regions of the scapula, while indirect force via impaction of the humeral head into the glenoid fossa can cause both glenoid and scapular neck fractures.
Patients with scapular fractures present with the upper extremity adducted against the body and protected from movement. Range of motion of the shoulder results limited, particularly with abduction.
Diagnosis
Imaging plays a key role in identifying and classifying scapular fractures and thus guides clinical decision-making.
The earliest opportunity to diagnose a scapular fracture may be on the initial routine supine anteroposterior (AP) chest radiograph taken in most trauma patients.
Up to 43% of scapular fractures in trauma patients are not recognized on the initial chest radiograph because they are often overlooked, not included in the study, or superimposed by other structures or artifacts (8-11).
Therefore, all patients with suspected scapular fractures should have dedicated scapular projections radiographs.
Radiographs
An appropriate set of radiographs in the setting of acute scapular trauma includes AP, Grashey, axillary, and lateral scapular (Y) views (12-14). This radiographic series allows diagnosis of scapular and ipsilateral clavicle fractures, as well as acromioclavicular and glenohumeral joint injuries. Grashey and axillary views are particularly useful for detection of intra-articular scapular fractures by providing direct visualization of the glenoid fossa and glenohumeral joint space. Acquisition of additional axillary views increases diagnostic sensitivity for difficult to see acromion and coracoid process fractures.
Scapula AP view
Position: AP view should be perpendicular to the plane of the scapula. Erect, sit or supine patient position can be performed even if the first one should be more comfortable for patient; posterior surface of shoulder is in direct contact with table without or with slight rotation of thorax to the examined side.
Arm should be gently abducted of 90 degrees and hand supinated.
Correct criteria: A complete representation of the scapula is obtained; the lateral scapular border should be visualized without costal superposition.
Demonstrated structures: Scapular parts including acromion, coracoid process, spine, as double almost parallel lines, and body; lateral distal third of the clavicle, scapulo-humeral joint, proximal third of the humerus, acromion-clavicular joint (Figure 1)
Figure 1.
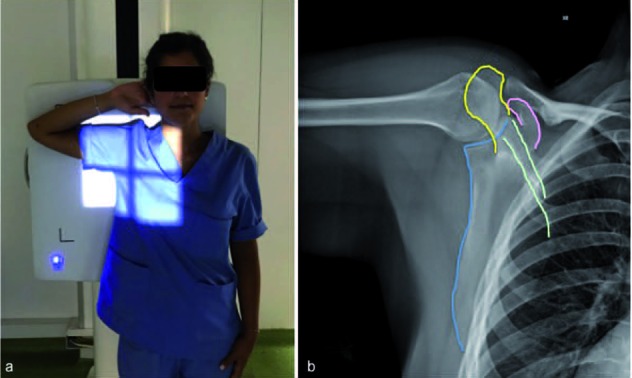
Scapula AP view. a) Patient position: posterior surface of shoulder is in direct contact with table; arm abducted of 90 degrees and hand supinated. b) On X-Ray demonstrated Scapular parts include acromion (yellow line), coracoid process (pink line), spine (green line), as double almost parallel lines, and body of which the lateral scapular border should be visualized without costal superposition (blue line)
AP oblique (Grashey view)
Position
The Grashey view is obtained with the patient rotated 35-45 degrees and his back, scapular body, up against the imaging detector.
Correct criteria: normal AP oblique internal rotation view is also known as a “true AP” view since the view is AP to the scapular instead of AP to the patient.
Demonstrated structures: This view allows assessing glenohumeral joint space (Figure 2)
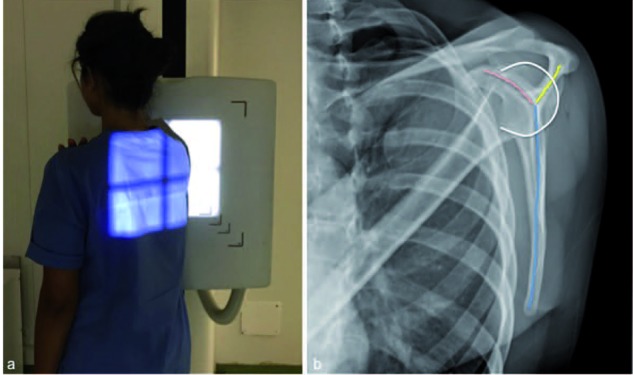
Figure 2.

Scapula AP Oblique (Grashey) view. In a) patient rotated 35-45 degrees and his back, scapular body, up against the imaging detector. On X-Ray in b) this is the “true” AP views since the views is AP to the scapular instead of AP to the patient and allows assessing glenohumeral joint space (blue double line)
Scapula Lateral view (Y)
Position
The lateral scapula (“Y” view) techniques can be divided into antero-posterior (AP) and postero-anterior (PA). The techniques can be further divided according to the patient’s arm position.
- The PA Approach (erect position)
- - “Arm on hip”: the patient’s chest is in a very lateral position.
- - “Napoleon technique”: cross arm adduction with hand of the affected arm placed on the opposite shoulder. The examined scapula tends to roll into the lateral position with very little rotation of the chest.
Caudal angulation could be adopted since patients tend to lean or stoop forward when positioned for lateral scapula radiography.
- The AP Approach (supine position)
- - “Patient’s Affected Arm in Neutral Position”: in this case the patient must be rotated considerably to achieve a true lateral scapula position. This has disadvantages in terms of difficulty of positioning, radiation dose and contrast/scatter degradation of the image.
- - “Patient’s Affected Arm in the “Napoleon” Position”: with this position, there is very little rotation of the chest required to achieve a true lateral scapula position.
Correct criteria: A complete representation of the scapula is obtained; the lateral and medial borders of the scapula are superimposed without other structures overlapped.
Demonstrated structures: The acromion and coracoid form a “Y” or “peace sign” shape with the body of the scapula. The head of the humerus should be normally centered to the middle of the “Y” shape. The acromion and distal end of the clavicle form a “roof” over the shoulder joint (Figure 3).
Figure 3.
Scapula Lateral view (Y). Example of PA approach with “Napoleon technique”: cross arm adduction with hand of the affected arm placed on the opposite shoulder (a). In b) on X-Ray a complete representation of the scapula is obtained; the lateral and medial borders of the scapula are superimposed without other structures overlapped. The acromion (yellow line) and coracoid (pink line) form a “Y” or “peace sign” shape with the body of the scapula. The head of the humerus (wite line) should be normally centered to the middle of the “Y” shape
True axillary view
Position
In supine patient this view is taken with arm abducted, not necessarily to 90 degree, which is optimal; cassette is placed on the superior aspect of the shoulder.
Arm is abducted enough to allow the radiographic beam to pass between chest and the arm in a direction perpendicular to cassette from shoulder.
Correct criteria: when properly done, it is possible to assess the anterior and posterior glenoid rim. This allows identifying glenoid rim lesions as well as wears patterns on the glenoid. A proper True Axillary View should have an “eye” created by the acromion and posterior glenoid. Absence of this “eye” indicates that we are not viewing the true anterior and posterior edges of the glenoid.
Demonstrated structures: the true axillary view allows measuring the glenohumeral joint space. Lesser tuberosity is seen anteriorly as a small inverted V on anterior surface of the humeral head (Figure 4).
Figure 4.
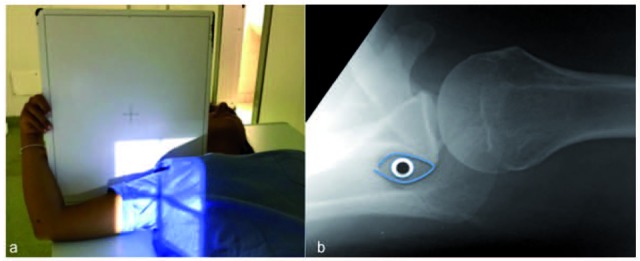
Scapula Axillary view. Arm abducted, not necessarily to 90 degree, which is optimal; cassette is placed on the superior aspect of the shoulder (a). X-Ray in b): when properly done, it is possible to assess the anterior and posterior glenoid rim. This allows identifying glenoid rim lesions. A proper True Axillary View should have an “eye”(figure) created by the acromion and posterior glenoid. Absence of this “eye” indicates that we are not viewing the true anterior and posterior edges of the glenoid
CT Scan
A computed tomography (CT) scan is recommended for complex fractures and for fractures with significant displacement (15-17). CT scans allow clinicians to evaluate the size, location, degree of displacement of fracture lines and to confirm the position of the humeral head in relation to the glenoid fossa and to evaluate the presence of intrarticular glenohumeral fragments. Furthermore, three-dimensional reconstructions of the CT scan can be extremely helpful in visualizing complex fracture patterns and planning for operative treatment.
Scapular Fractures Classification
Intra-articular Scapular Fractures
Intra-articular fractures constitute 10-30% of all scapular fractures (18-20), accounting for the vast majority of open reduction and internal fixation (ORIF) procedures performed for management of scapular fracture (21-23)
Glenoid fossa fractures are consequence of an impact between humeral head and glenoid fossa (24-26). A shoulder dislocation is an additional mechanism associated with intra-articular fractures of the anterior glenoid.
The Ideberg classification is the most widely used classification, later modified by Goss, consisting of 6 main fractures (27-29)
Type I: An isolated fracture of the anteroinferior glenoid, which may involve complete dislocation.
Type II: Fractures through the inferior surface of the glenoid that extend in a transverse plane along the glenoid neck to under the base of the coracoid.
Type III: Fractures involving the inferior or inferoposterior surface of the glenoid along with a portion of the lateral scapular border
Type IV: A fracture pattern that consists of an inferior fracture through the articular surface that extends in a stellate pattern to involve the scapular body. These fractures may be associated with spine fractures.
Type V: This fracture type is defined as a Type IV fracture pattern with an additional fracture through the coracoid, acromion, or superior articular component.
Type VI: comminuted glenoid fracture
Most nondisplaced intra-articular glenoid fractures are managed nonoperatively. However, displaced fractures demand consideration for operative fixation, because the various myotendinous units attaching to the scapula pull in different directions and contribute to distraction and rotational malalignment (30-32) (Figure 5). Nevertheless, the criteria for surgical management remain controversial, and the decision whether to perform ORIF is dependent on the surgeon’s preference and patient comorbidity, age, hand dominance, overall health, activities of daily living, and level of physical activity (1, 33, 34). The most common goals for ORIF of displaced intraarticular scapular fracture are to reduce joint incongruity and prevent longterm posttraumatic osteoarthritis, instability, chronic pain, and decreased range of motion (35-39). Indications for surgery include at least 4 mm of displacement at the articular surface and at least 20% involvement of the glenoid, although operative intervention is still considered to address instability even when these criteria are not met (1, 27, 40) Other relative indications include an anterior rim fracture of greater than 25% of the articular surface or a posterior rim fracture of greater than 33%, fractures extending to the medial border of the scapula with displacement, glenoid rim fractures with associated persistent glenohumeral instability, and open fractures (1, 27, 41, 42).
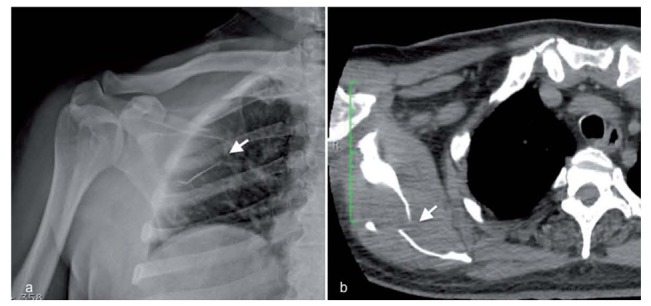
Figure 5.

Combined glenoid fracture (white arrow), type V with displacement of fragments, and scapula fracture (blue arrowheads). Note the associated clavicular fracture (asterics)
Extra-articular Scapular Fractures
Extraarticular fractures of the coracoid process, acromion process, neck, body, and spine account for the majority of scapular fractures. Traditionally, management of nonarticular scapular fractures has been conservative in nature. ORIF of displaced fractures has been touted as an avenue to decrease long-term pain, weakness, and functional disability (43-49).
- Scapular body and spine fractures are the most frequent (50% of the cases) (Figures 6, 7). The rim fracture could be transversal, involving the supra or infraspinous fossa, or vertical named trans-spinal fracture. The isolated spine fracture is rare accounting for 6–11% of scapular fractures (50-53).
Figure 6.
Transversal fracture involving the infraspinous fossa. Note the “extra line” on X-Ray in a and the body interruption on CT in b (white arrows)
Figure 7.
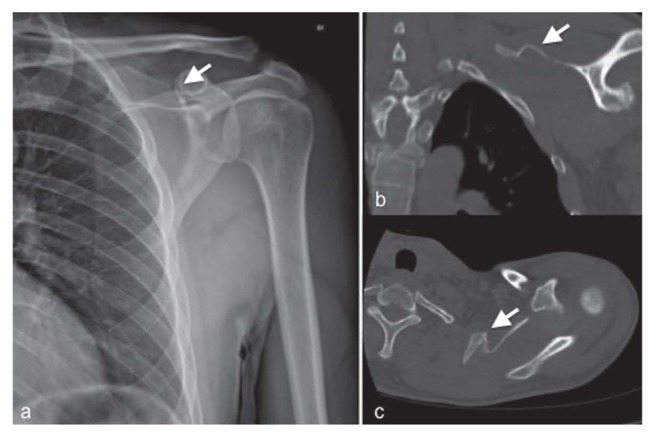
Transversal fracture involving the supraspinous fossa (white arrows on X-Ray and CT)
Isolated scapular body fractures result stable, fast consolidating after a brief immobilization of about ten days, even with significant misalignment.
- Anatomic and surgical neck fractures. The scapular neck is second only to the body as the most common fracture site, accounting for 26-29% (Figure 8). In this case the glenoid articular surface is detached en bloc, remaining intact. The surgical neck fractures are the most frequent among them (54) Nondisplaced scapular neck and spine fractures have favorable long-term outcomes with nonoperative management (27, 55-57) Surgeons may choose to perform ORIF in certain instances. Biomechanical studies have suggested that displaced scapular neck fractures negatively affect the stability of the glenohumeral joint by altering the length of rotator cuff muscles during certain phases of movement (58). Pain and weakness also have been reported in patients with significant displacement and malalignment of scapular neck fractures (59).
Figure 8.
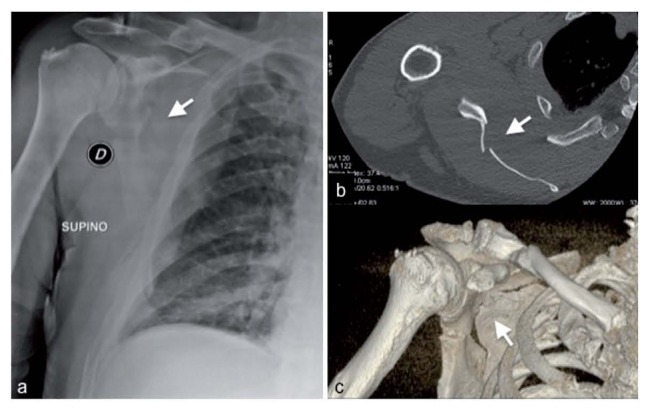
Scapular neck fracture also involving the infraspinous fossa (white arrows) on Xray a), planar b) and volume rendering c) CT
Grading of scapular neck displacement and rotation misalignment can be determined from radiographs or CT using the following parameters (1) (Figure 9):
Gleno-polar angle (GPA): is a measure of rotational malalignment of the glenoid in relation to the anteroposterior axis perpendicular to the plane of the scapula (19, 37, 44). On AP view, the GPA angle is calculated by drawing a line from the inferior to the superior pole of the glenoid fossa and another line from the superior pole to the apex of the scapula body’s inferior angle. Normal glenopolar angle is 30-45°, and a glenopolar angle of up to 20-22°, in isolation or in combination with other shoulder girdle injuries, is used as a relative indication for surgery to avoid long-term pain, weakness, and reduced capacity for activities of daily living (1, 43, 44).
Lateral border offset: it is often referred to as medialization and corresponds to the distance of mediolateral displacement between the lateral margins of the superior and inferior scapular neck fractures. It is measured on AP view by tracing a perpendicular line from the lateral most extent of the inferior fragment and another perpendicular line from where it originally was located on the superior fragment. The distance between these two lines is the lateral border offset: a value of at least 1-2 cm is a relative indication for ORIF.
Angulation: is a measure of angular deformity obtained in the plane parallel to the mediolateral axis of the scapula. It is determined using the scapular Y view and the angle is formed by intersection of a line running parallel to the proximal fragment and a line running parallel to the distal fragment borders. An angular deformity of at least 40-45° is a relative indication for surgery (1, 43, 47).
- Translation: is defined by the distance of anteroposterior displacement between the superior and inferior scapular neck fractures fragments. It is measured on Y scapular view by tracing a distance between superior and inferior fragment anterior cortexes.
Figure 9.
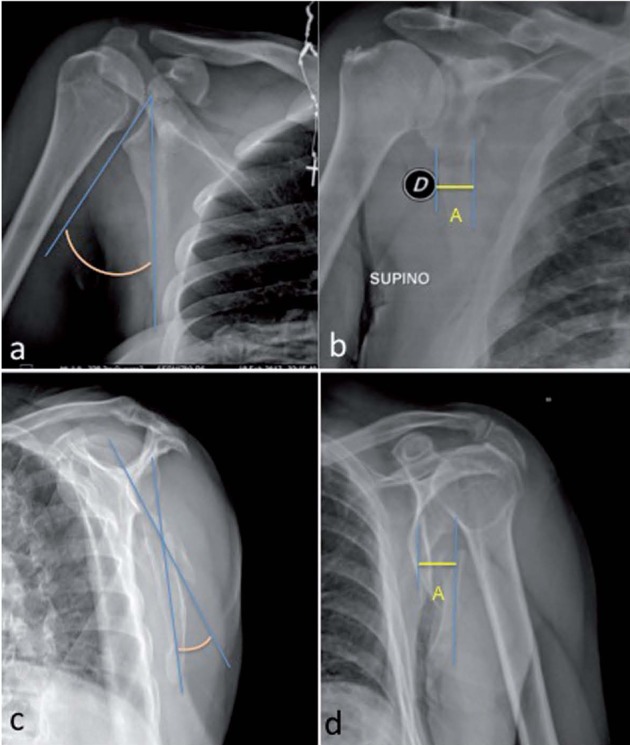
X-ray and 3-D images illustrating displacement measurements. Measurements of glenopolar angle (a) and lateral border offset (b), which are measured on the Grashey x-ray view or 3-D oriented in the true AP plane. Measurements of angulation (c) and translation (d), which are measured on the scapula Y X-ray or 3-D CT views
Figure 10.
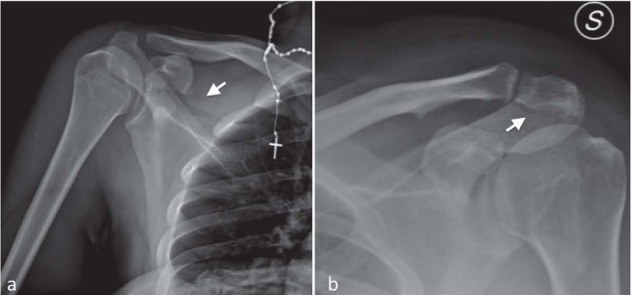
In a) fracture of superior scapular fossa and the base of coracoid process (white arrow) with involvement if superior border of glenoid fossa. In b) fracture of acromion process (white arrow)
Surgical management is considered for fractures with more than 1 cm of displacement or intraarticular extension (62, 63).
Ogawa et al. (62) described a functional method of classification based on the anatomic relationship of the fracture to the coracoclavicular ligament:
Ogawa type I coracoid process fractures are posterior to the coracoclavicular ligament. These fractures are more common and have a greater tendency to be unstable.
Ogawa type II fractures are anterior to the coracoclavicular ligament (62-64).
ORIF may also be considered after failed conservative management if the displaced bone fragment produces chronic irritation of the adjacent soft tissues or if the coracoid fragment or fragments cause an obstruction to the reduction of a shoulder dislocation (65, 66).
- Acromion process fractures. They represent 8-16% of scapular fractures (67, 68) and involve above all the basis of the acromion (69) Acromion fractures could be conservatively managed in case of non displacement
Kuhn et al. (70) described an alternative functional method based on the presence or absence of subacromial impingement:
Kuhn type I fractures are minimally displaced, type II fractures are significantly displaced without subacromial space narrowing, and type III fractures are significantly displaced with subacromial space narrowing. Patients with Kuhn type III acromion fractures are prone to develop decreased range of motion and rotator cuff injury (71, 72)
Acromion-clavicular luxation due to traction mechanism from coraco-clavicular ligaments, which frequently remain intact, or to an anterior gleno-humeral luxation which should be always researched (61, 70, 71)
Floating Shoulder Injuries
Floating shoulder injuries are rare and represent less than 0.2% of shoulder girdle fracture patterns (16, 23, 25, 73).
A floating shoulder injury occurs with two or more displaced fractures involving the superior shouldersuspensory complex: the scapularneck and clavicle, acromion process, orcoracoid process or disruption of the acromioclavicularjoint and coracoclavicular ligament (46, 47, 74, 75). A single injury of the superior shoulder suspensory complex is usually treated conservatively.
However, two or more disruptions may have a negative impact on long-term healing and function (15, 63, 76)
Displacements smaller than 1 cm for double disruptions of the superior shoulder suspensory complex usually have good outcomes with conservative treatment (77-79). Poor outcomes are most likely to occur in the setting of significant displacement at one or more sites in the ring. The criteria for superior shoulder suspensory complex double disruption ORIF remain controversial because no uniform standards exist, and nonoperative management of extra-articular scapular fractures has been the traditional norm (27, 58, 74, 80).
Conclusion
Knowledge of scapular anatomy, function, injury patterns, imaging appearance, and clinical management is important for the radiologist to the care of patients who present with acute shoulder trauma.
Acknowledgements
Acknowledgement to radiographer Silvia Cinque, Department of Radiology, Private Hospital “Villa dei Fiori,” Acerra, Naples, Italy.
References
- 1.Cole PA, Freeman G, Dubin JR. Scapula fractures. Curr Rev Musculoskelet Med. 2013;6:79–87. doi: 10.1007/s12178-012-9151-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Battipaglia G, Avilia S, Morelli E, Caranci F, Perna F, Camera A. Posterior reversible encephalopathy syndrome (PRES) during induction chemotherapy for acute myeloblastic leukemia (AML) Ann Hematol. 2012;91:1327–1328. doi: 10.1007/s00277-011-1398-6. [DOI] [PubMed] [Google Scholar]
- 3.Caranci F, Tedeschi E, Leone G, et al. Errors in neuroradiology. Radiol Med. 2015;120:795–801. doi: 10.1007/s11547-015-0564-7. [DOI] [PubMed] [Google Scholar]
- 4.Cellerini M, Mangiafico S, Ammannati F, et al. Ruptured, dissecting posterior inferior cerebellar artery aneurysms: Endovascular treatment without parent vessel occlusion. Neuroradiology. 2008;50:315–320. doi: 10.1007/s00234-007-0333-y. [DOI] [PubMed] [Google Scholar]
- 5.Nurzynska D, DiMeglio F, Castaldo C, et al. Flatfoot in children: Anatomy of decision making. Ital J Anat Embryol. 2012;117:98–106. [PubMed] [Google Scholar]
- 6.Muccio CF, Di Blasi A, Esposito G, Brunese L, D’Arco F, Caranci F. Perfusion and spectroscopy magnetic resonance imaging in a case of lymphocytic vasculitis mimicking brain tumor. Pol J Radiol. 2013;78:66–69. doi: 10.12659/PJR.884011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Muccio CF, Caranci F, D’Arco F, et al. Magnetic resonance features of pyogenic brain abscesses and differential diagnosis using morphological and functional imaging studies: A pictorial essay. J Neuroradiol. 2014;41:153–167. doi: 10.1016/j.neurad.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 8.Harris RD, Harris JH. Jr. The prevalence and significance of missed scapular fractures in blunt chest trauma. AJR Am J Roentgenol. 1988;151:747–50. doi: 10.2214/ajr.151.4.747. [DOI] [PubMed] [Google Scholar]
- 9.Briganti F, Delehaye L, Leone G, et al. Flow diverter device for the treatment of small middle cerebral artery aneurysms. J Neurointervent Surg. 2016;8:287–294. doi: 10.1136/neurintsurg-2014-011460. [DOI] [PubMed] [Google Scholar]
- 10.Caranci F, Briganti F, La Porta M, et al. Magnetic resonance imaging in brachial plexus injury. Musculoskeletal Surg. 2013;97:S181–S190. doi: 10.1007/s12306-013-0281-0. [DOI] [PubMed] [Google Scholar]
- 11.Briganti F, Leone G, Panagiotopoulos K, et al. Endovascular treatment of cerebral aneurysms using the hydrocoil embolic system. Neuroradiol J. 2013;26:420–427. doi: 10.1177/197140091302600407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ropp AM, Davis DL. Scapular Fractures: What Radiologists Need to Know. AJR Am J Roentgenol. 2015;205:491–501. doi: 10.2214/AJR.15.14446. [DOI] [PubMed] [Google Scholar]
- 13.Guarnieri G, Vassallo P, Pezzullo MG, Laghi F, Zeccolini F, Ambrosanio G, Galasso R, Muto M, Izzo R. A comparison of minimally invasive techniques in percutaneous treatment of lumbar herniated discs a review. Neuroradiol J. 2009;22:108–121. doi: 10.1177/197140090902200116. [DOI] [PubMed] [Google Scholar]
- 14.Limbucci N, Rossi F, Salvati F, Pistoia LM, Barile A, Masciocchi C. Bilateral Suprascapular nerve entrapment by glenoid labral cysts associated with rotator cuff damage and posterior instability in an amateur weightlifter. J Sports Med Phys Fitness. 2010;50:64–67. [PubMed] [Google Scholar]
- 15.McAdams TR, Blevins FT, Martin TP, DeCoster TA. The role of plain films and computed tomography in the evaluation of scapular neck fractures. J Orthop Trauma. 2002;16:7–11. doi: 10.1097/00005131-200201000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Barile A, Lanni G, Conti L, et al. Lesions of the biceps pulley as cause of anterosuperior impingement of the shoulder in the athlete: Potentials and limits of MR arthrography compared with arthroscopy. Radiol Med. 2013;118:112–122. doi: 10.1007/s11547-012-0838-2. [DOI] [PubMed] [Google Scholar]
- 17.Barile A, Bruno F, Arrigoni F, et al. Emergency and Trauma of the Ankle. Semin Musculoskelet Radiol. 2017;21:282–289. doi: 10.1055/s-0037-1602408. [DOI] [PubMed] [Google Scholar]
- 18.Ideberg R, Grevsten S, Larsson S. Epidemiology of scapular fractures. Incidence and classification of 338 fractures. Acta Orthop Scand. 1995;66:395–7. doi: 10.3109/17453679508995571. [DOI] [PubMed] [Google Scholar]
- 19.Zappia M, Castagna A, Barile A, et al. Imaging of the coracoglenoid ligament: a third ligament in the rotator interval of the shoulder. Skelet Radiol. 2017;46:1101–1111. doi: 10.1007/s00256-017-2667-9. [DOI] [PubMed] [Google Scholar]
- 20.Floridi C, Reginelli A, Capasso R, Fumarola E, Pesapane F, Barile A, Zappia M, Caranci F, Brunese L. Percutaneous needle biopsy of mediastinal masses under C-arm conebeam CT guidance: diagnostic performance and safety. Med Oncol. 2017;34 doi: 10.1007/s12032-017-0911-8. [DOI] [PubMed] [Google Scholar]
- 21.Zlowodzki M, Bhandari M, Zelle BA, Kregor PJ, Cole PA. Treatment of scapula fractures: systematic review of 520 fractures in 22 case series. J Orthop Trauma. 2006;20:230–3. doi: 10.1097/00005131-200603000-00013. [DOI] [PubMed] [Google Scholar]
- 22.Reginelli A, Zappia M, Barile A, Brunese L. Strategies of imaging after orthopedic surgery. Musculoskeletal Surg. 2017;101 doi: 10.1007/s12306-017-0458-z. [DOI] [PubMed] [Google Scholar]
- 23.Barile A, Bruno F, Mariani S, et al. What can be seen after rotator cuff repair: a brief review of diagnostic imaging findings. Musculoskeletal Surg. 2017;101:3–14. doi: 10.1007/s12306-017-0455-2. [DOI] [PubMed] [Google Scholar]
- 24.Goss TP. Fractures of the glenoid cavity. J Bone Joint Surg Am. 1992;74:299–305. [PubMed] [Google Scholar]
- 25.De Filippo M, Pesce A, Barile A, et al. Imaging of postoperative shoulder instability. Musculoskeletal Surg. 2017;101:15–22. doi: 10.1007/s12306-017-0461-4. [DOI] [PubMed] [Google Scholar]
- 26.Barile A, La Marra A, Arrigoni F, et al. Anaesthetics, steroids and platelet-rich plasma (PRP) in ultrasound-guided musculoskeletal procedures. Br J Radiol. 2016;89 doi: 10.1259/bjr.20150355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Oostveen DP, Temmerman OP, Burger BJ, van Noort A, Robinson M. Glenoid fractures: a review of pathology, classification, treatment and results. Acta Orthop Belg. 2014;80:88–98. [PubMed] [Google Scholar]
- 28.Miele V, Piccolo CL, Trinci M, Galluzzo M, Ianniello S, Brunese L. Diagnostic imaging of blunt abdominal trauma in pediatric patients. Radiol Med. 2016;121:409–430. doi: 10.1007/s11547-016-0637-2. [DOI] [PubMed] [Google Scholar]
- 29.Piccolo CL, Ianniello S, Trinci M, et al. Diagnostic Imaging in pediatric thoracic trauma. Radiol Med. 2017 doi: 10.1007/s11547-017-0783-1. [DOI] [PubMed] [Google Scholar]
- 30.Nork SE, Barei DP, Gardner MJ, Schildhauer TA, Mayo KA, Benirschke SK. Surgical exposure and fixation of displaced type IV, V, and VI glenoid fractures. J Orthop Trauma. 2008;22:487–93. doi: 10.1097/BOT.0b013e31817d5356. [DOI] [PubMed] [Google Scholar]
- 31.Reginelli A, Russo A, Maresca D, Martiniello C, Cappabianca S, Brunese L. Imaging Assessment of Gunshot Wounds. Semin Ultrasound CT MRI. 2015;36:57–66. doi: 10.1053/j.sult.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 32.Piccolo CL, Galluzzo M, Ianniello S, et al. Pediatric musculoskeletal injuries: role of ultrasound and magnetic resonance imaging. Musculoskelet Surg. 2017;101:85–102. doi: 10.1007/s12306-017-0452-5. [DOI] [PubMed] [Google Scholar]
- 33.Miele V, Di Giampietro I. Diagnostic imaging in emergency. Salute Soc. 2014:127–141. [Google Scholar]
- 34.Miele V, Andreoli C, Grassi R. The management of emergency radiology: Key facts. Eur J Radiol. 2006;59:311–314. doi: 10.1016/j.ejrad.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 35.Herrera DA, Anavian J, Tarkin IS, Armitage BA, Schroder LK, Cole PA. Delayed operative management of fractures of the scapula. J Bone Joint Surg Br. 2009;91:619–26. doi: 10.1302/0301-620X.91B5.22158. [DOI] [PubMed] [Google Scholar]
- 36.Schandelmaier P, Blauth M, Schneider C, Krettek C. Fractures of the glenoid treated by operation. A 5- to 23-year follow-up of 22 cases. J Bone Joint Surg Br. 2002;84:173–7. doi: 10.1302/0301-620x.84b2.12357. [DOI] [PubMed] [Google Scholar]
- 37.Cole PA, Gauger EM, Herrera DA, Anavian J, Tarkin IS. Radiographic follow-up of 84 operatively treated scapula neck and body fractures. Injury. 2012;43:327–33. doi: 10.1016/j.injury.2011.09.029. [DOI] [PubMed] [Google Scholar]
- 38.Zappia M, Carfora M, Romano AM, et al. Sonography of chondral print on humeral head. Skelet Radiol. 2016;45:35–40. doi: 10.1007/s00256-015-2238-x. [DOI] [PubMed] [Google Scholar]
- 39.Zappia M, Aliprandi A, Pozza S, Doniselli FM, Gitto S, Sconfienza LM. How is shoulder ultrasound done in Italy? A survey of clinical practice. Skeletal Radiol. 2016;45:1629–1634. doi: 10.1007/s00256-016-2477-5. [DOI] [PubMed] [Google Scholar]
- 40.Zappia M, Di Pietto F, Aliprandi A, et al. Multi-modal imaging of adhesive capsulitis of the shoulder. Insights Imaging. 2016;7:365–71. doi: 10.1007/s13244-016-0491-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.van der Byl G, di Giacomo V, Miele V. Herlyn Werner Wunderlich syndrome (HWWS): An unusual presentation of acute abdominal pain. J Ultrasound. 2014;17:171–174. doi: 10.1007/s40477-014-0092-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zappia M, Castagna A, Barile A, Chianca V, Brunese L, Pouliart N. Imaging of the coracoglenoid ligament: a third ligament in the rotator interval of the shoulder. Skeletal Radiol. 2017;46:1101–1111. doi: 10.1007/s00256-017-2667-9. [DOI] [PubMed] [Google Scholar]
- 43.Romero J, Schai P, Imhoff AB. Scapular neck fracture--the influence of permanent malalignment of the glenoid neck on clinical outcome. Arch Orthop Trauma Surg. 2001;121:313–6. doi: 10.1007/s004020000224. [DOI] [PubMed] [Google Scholar]
- 44.Goss TP. Double disruptions of the superior shoulder suspensory complex. J Orthop Trauma. 1993;7:99–106. doi: 10.1097/00005131-199304000-00001. [DOI] [PubMed] [Google Scholar]
- 45.Dialetto G, Reginelli A, Cerrato M, Rossi G, Covino FE, Manduca S, Lassandro F. Endovascular stent-graft treatment of thoracic aortic syndromes: a 7-year experience. Eur J Radiol. 2007;64:65–72. doi: 10.1016/j.ejrad.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 46.Owens BD, Goss TP. The floating shoulder. J Bone Joint Surg Br. 2006;88:1419–24. doi: 10.1302/0301-620X.88B11.17997. [DOI] [PubMed] [Google Scholar]
- 47.Bozkurt M, Can F, Kirdemir V, Erden Z, Demirkale I, Basbozkurt M. Conservative treatment of scapular neck fracture: the effect of stability and glenopolar angle on clinical outcome. Injury. 2005;36:1176–81. doi: 10.1016/j.injury.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 48.Zappia M, Reginelli A, Russo A, et al. Long head of the biceps tendon and rotator interval. Musculoskeletal Surg. 2013;97:S99–S108. doi: 10.1007/s12306-013-0290-z. [DOI] [PubMed] [Google Scholar]
- 49.Ada JR, Miller ME. Scapular fractures. Analysis of 113 cases. Clin Orthop Relat Res. 1991:174–80. [PubMed] [Google Scholar]
- 50.Romeo A, Pinto A, Cappabianca S, Scaglione M, Brunese L. Role of Multidetector Row Computed Tomography in the Management of Mandible Traumatic Lesions. Semin Ultrasound CT MRI. 2009;30:174–180. doi: 10.1053/j.sult.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 51.Brunese L, Reginelli A, Caranci F. Strategies to reduce errors in radiology, Errors in Radiology. Springer-Verlag Milan. 2012:303–308. [Google Scholar]
- 52.Pinto A, Brunese L, Pinto F, Reali R, Daniele S, Romano L. The Concept of Error and Malpractice in Radiology. Semin Ultrasound CT MRI. 2012;33:275–279. doi: 10.1053/j.sult.2012.01.009. [DOI] [PubMed] [Google Scholar]
- 53.Splendiani A, Bruno F, Patriarca L, et al. Thoracic spine trauma: advanced imaging modality. Radiol Med. 2016;121:780–792. doi: 10.1007/s11547-016-0657-y. [DOI] [PubMed] [Google Scholar]
- 54.Barile A, Limbucci N, Splendiani A, Gallucci M, Masciocchi C. Spinal injury in sport. Eur J Radiol. 2007;62:68–78. doi: 10.1016/j.ejrad.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 55.Nordqvist A, Petersson C. Fracture of the body, neck, or spine of the scapula. A long-term follow-up study. Clin Orthop Relat Res. 1992:139–44. [PubMed] [Google Scholar]
- 56.Pinto A, Brunese L, Scaglione M, Scuderi MG, Romano L. Gunshot Injuries in the Neck Area: Ballistics Elements and Forensic Issues. Semin Ultrasound CT MRI. 2009;30:215–220. doi: 10.1053/j.sult.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 57.Caranci F, Brunese L, Reginelli A, Napoli M, Fonio P, Briganti F. Neck Neoplastic Conditions in the Emergency Setting: Role of Multidetector Computed Tomography. Semin Ultrasound CT MRI. 2012;33:443–448. doi: 10.1053/j.sult.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 58.Chadwick EK, van Noort A, van der Helm FC. Biomechanical analysis of scapular neck malunion--a simulation study. Clin Biomech (Bristol, Avon) 2004;19:906–12. doi: 10.1016/j.clinbiomech.2004.06.013. [DOI] [PubMed] [Google Scholar]
- 59.Izzo R, Muto M. Biomechanics of the spine and etiopathogenesis of spinal pain, Interventional Neuroradiology of the Spine: Clinical Features, Diagnosis and Therapy. Springer-Verlag Milan. 2013:1–25. [Google Scholar]
- 60.Ogawa K, Yoshida A, Takahashi M, Ui M. Fractures of the coracoid process. J Bone Joint Surg Br. 1997;79:17–9. doi: 10.1302/0301-620x.79b1.6912. [DOI] [PubMed] [Google Scholar]
- 61.Ogawa K, Matsumura N, Ikegami H. Coracoid fractures: therapeutic strategy and surgical outcomes. J Trauma Acute Care Surg. 2012;72:E20–6. [PubMed] [Google Scholar]
- 62.Anavian J, Wijdicks CA, Schroder LK, Vang S, Cole PA. Surgery for scapula process fractures: good outcome in 26 patients. Acta Orthop. 2009;80:344–50. doi: 10.3109/17453670903025394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Eyres KS, Brooks A, Stanley D. Fractures of the coracoid process. J Bone Joint Surg Br. 1995;77:425–8. [PubMed] [Google Scholar]
- 64.Caranci F, Cicala D, Cappabianca S, Briganti F, Brunese L, Fonio P. Orbital Fractures: Role of Imaging. Semin Ultrasound CT MRI. 2012;33:385–391. doi: 10.1053/j.sult.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 65.Goss TP. The scapula: coracoid, acromial, and avulsion fractures. Am J Orthop (Belle Mead NJ) 1996;25:106–15. [PubMed] [Google Scholar]
- 66.Wong-Chung J, Quinlan W. Fractured coracoid process preventing closed reduction of anterior dislocation of the shoulder. Injury. 1989;20:296–7. doi: 10.1016/0020-1383(89)90173-3. [DOI] [PubMed] [Google Scholar]
- 67.Hill BW, Anavian J, Jacobson AR, Cole PA. Surgical management of isolated acromion fractures: technical tricks and clinical experience. J Orthop Trauma. 2014;28:e107–13. doi: 10.1097/BOT.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 68.Izzo R, Guarnieri G, Guglielmi G, Muto M. Biomechanics of the spine. Part II: Spinal instability. Eur J Radiol. 2013;82:127–138. doi: 10.1016/j.ejrad.2012.07.023. [DOI] [PubMed] [Google Scholar]
- 69.Delfaut EM, Carlier C, Cotten A. Osteo-articular imaging. J Radiol. 1999;80:542–4. [PubMed] [Google Scholar]
- 70.Kuhn JE, Blasier RB, Carpenter JE. Fractures of the acromion process: a proposed classification system. J Orthop Trauma. 1994;8:6–13. doi: 10.1097/00005131-199402000-00002. [DOI] [PubMed] [Google Scholar]
- 71.Guiral J, Real JL, Curto JM. Isolated fracture of the coracoid process of the scapula. Acta Orthop Belg. 1996;62:60–1. [PubMed] [Google Scholar]
- 72.Masciocchi C, Conchiglia A, Conti L, Barile A. Imaging of insufficiency fractures, Geriatric Imaging. Springer-Verlag Berlin Heidelberg. 2013:83–91. [Google Scholar]
- 73.Herscovici D, Jr., Fiennes AG, Allgower M, Ruedi TP. The floating shoulder: ipsilateral clavicle and scapular neck fractures. J Bone Joint Surg Br. 1992;74:362–4. doi: 10.1302/0301-620X.74B3.1587877. [DOI] [PubMed] [Google Scholar]
- 74.Rikli D, Regazzoni P, Renner N. The unstable shoulder girdle: early functional treatment utilizing open reduction and internal fixation. J Orthop Trauma. 1995;9:93–7. doi: 10.1097/00005131-199504000-00001. [DOI] [PubMed] [Google Scholar]
- 75.Mangano K, Vergalito F, Mammana S, et al. Evaluation of hyaluronic acid-P40 conjugated cream in a mouse model of dermatitis induced by oxazolone. Exp Ther Med. 2017;14:2439–2444. doi: 10.3892/etm.2017.4810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Camperchioli A, Mariani M, Bartollino S, et al. Investigation of the Bcl-2 multimerisation process: structural and functional implications. Biochim Biophys Acta. 2011;1813:850–7. doi: 10.1016/j.bbamcr.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 77.Edwards SG, Whittle AP, Wood GW. Nonoperative treatment of ipsilateral fractures of the scapula and clavicle. J Bone Joint Surg Am. (2nd) 2000;82:774–80. doi: 10.2106/00004623-200006000-00003. [DOI] [PubMed] [Google Scholar]
- 78.Ramos L, Mencia R, Alonso A, Ferrandez L. Conservative treatment of ipsilateral fractures of the scapula and clavicle. J Trauma. 1997;42:239–42. doi: 10.1097/00005373-199702000-00009. [DOI] [PubMed] [Google Scholar]
- 79.Cristofano A, Sapere N, La Marca G, et al. Serum Levels of Acyl-Carnitines along the Continuum from Normal to Alzheimer’s Dementia. PLoS ONE. 2016;11:e0155694. doi: 10.1371/journal.pone.0155694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Paglia G, Miedico O, Cristofano A, et al. Distinctive Pattern of Serum Elements During the Progression of Alzheimer’s Disease. Sci Rep. 2016;6:22769. doi: 10.1038/srep22769. [DOI] [PMC free article] [PubMed] [Google Scholar]


