Abstract
Background and aim of the work: The calcaneus, the more lower bone of the body, has the task of supporting the axial load from the weight of the body. Calcaneal fractures represent about 1-2% of all fractures and 60% of the tarsal bones fractures. The articular involvement has been associated with a poor functional outcome. The aim of this work is to describe the radiologic evaluation, the classification systems, the morphological preoperative diagnostic imaging features of calcaneal fractures, highlighting the correlation with the choice of treatment and predictive capacity for the fracture surgical outcome. Methods: A PubMed search was performed for the terms Imaging calcaneus fracture, selecting articles in English language, published in the last two years, where preoperatively diagnostic imaging of fractures of the calcaneus are described. Case reports have not been included. Results: We have collected a number of data that provide important help in preoperative evaluation of calcaneal fractures, such as the new classification system created by Harnroongroj et al, the association of calcaneal fractures with fractures of other bone structures or soft tissue impairment, the use of calcaneotalar ratio in assessing the length of heel. Conclusions: These data suggest an approach geared to the specific choice of treatment and to improving patient outcomes. (www.actabiomedica.it)
Keywords: trauma, trauma imaging, calcaneal fractures, conventional X-Ray, Computed Tomography, CT
Introduction
The calcaneus is the greatest tarsal bone, and has the function of sustaining the body (1). Fractures of the calcaneus represent about 1-2% of all fractures and 60% of the tarsal bones fractures (1-5). The mechanism of injury can range from high energy trauma (falls from height) to low energy trauma (sport). There are several causes that determine the calcaneal fractures. Over 60% of the cases are caused by an axial load, usually due to falling from a height with landing on the feet, with a bilateral compromise of less than 10% (2, 6-10). An example of type intra- or extra-articular calcaneal fractures, due to falling from a height, is the “lover’s fracture” or “Don Juan fracture”. The names of this fractures of calcaneal body originate from the fact that the suitor can jump from great heights to escape from the lover’s consort (1, 8, 11-15). Another cause of calcaneal fractures are vehicle accidents where the passenger’s feet are pressed firmly against the vehicle floor (16-20). Risk factors for the occurrence of this type of fractures are osteoporosis, diabetes mellitus, peripheral neuropathy, osteomalacia, and long-term immunosuppressive therapy (21-25).
As the ankle and the rearfoot are positioned along the load line of the lower limbs, the force that primarily contributes to the fracture mechanism is the axial load (26-30). The biomechanics of the foot and ankle have been studied with the experimentation of a high axial load (27). Fracture of the calcaneus was the most frequent fracture shown in cadaveric studies (26). Excessive axial load in the Gissane’s angle (GA) determines a primary fracture line that reaches the neutral triangle (area with sparse trabeculae located under the subtalar joint thalamic bone). With a greater force can be generated a second fracture line that generally reaches the upper or lower calcaneus surface (Fig. 1) (31).
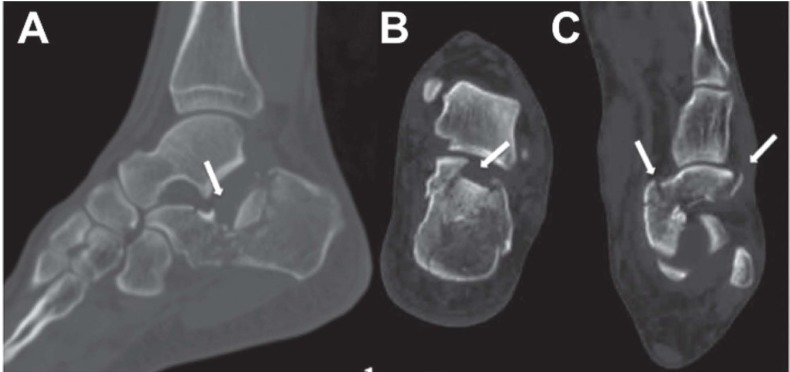
Figure 1.
Conventional radiographies in lateral projection of the ankle show the GA, neutral triangle (A) and the biomechanics of some kinds of calcaneal fractures. The increase in the axial load compresses the lateral process of the talus (arrow) (B)
In children aged 8 to 14 years, the 60% of the fractures are extra-articular; while in children younger than 7 years, more than 90% of calcaneal fractures are extra-articular (32-40). Adult man in a working age represents the typical patient. In this patients, most calcaneal fractures are intra-articular (about 75%) (2, 41-45). The articular involvement has been associated with a poor functional outcome. An adult patient who has suffered this fracture, takes the risk to not return to work with full capacity due to postoperative complications. For this reason these fractures are very important from a clinical perspective (41, 46-50).
The Sanders classification system is the most used system for classifying intra-articular calcaneal fractures. This classification system uses computed tomography (CT) because of its three-dimensional approach is critical to classify this type of fractures (1, 2, 11, 31, 51). Extra-articular fractures are classified by the anatomical division of the heel in three parts (1). CT with multiplanar reconstructions (MPR) and volume rendering (VR) reconstructions allows classification of these fractures, allowing better visualization and characterization of fracture lines and displacement of bone fragments. Once the type of fracture is classified, we can choose the type of treatment (conservative or surgical) (52-55).
Herein, we describe the radiologic assessment, the classification systems and the morphological diagnostic imaging features of calcaneal fractures, highlighting the correlation with the choice of treatment and predictive capacity for the fracture surgical outcome.
A PubMed search was performed for the terms Imaging calcaneus fracture, selecting articles in English language, published in the last two years, where preoperatively diagnostic imaging of fractures of the calcaneus are described. Case reports have not been included.
Radiologic assessment
The first assessment of the calcaneus suspected fractures is performed with conventional radiography, performed with axial heel (Harris projection). The best known classification system based on conventional radiography is the Essex-Lopresti system (56).
CT has changed the evaluation of calcaneal fractures because it allows better visualization of subtlar joint (31). Through MPR and VR reconstruction is possible to assess accurately the fracture lines, dislocation, crushing, the morphology and the involvement of the articular surfaces, allowing to choose the appropriate treatment and have a better prognostic evaluation. The split between intra- and extra-articular fractures is based on the involvement of the subtalar joint (4, 18, 31, 57, 58).
Classification system
Sanders system is the most used fractures classification system.
The system is based on coronal CT images, and subdivides intra-articular fractures into 4 types, depending on the number of fractures and the fracture line position at the posterior calcaneal facet (Fig. 2, 3, 4, 5) (59, 60).
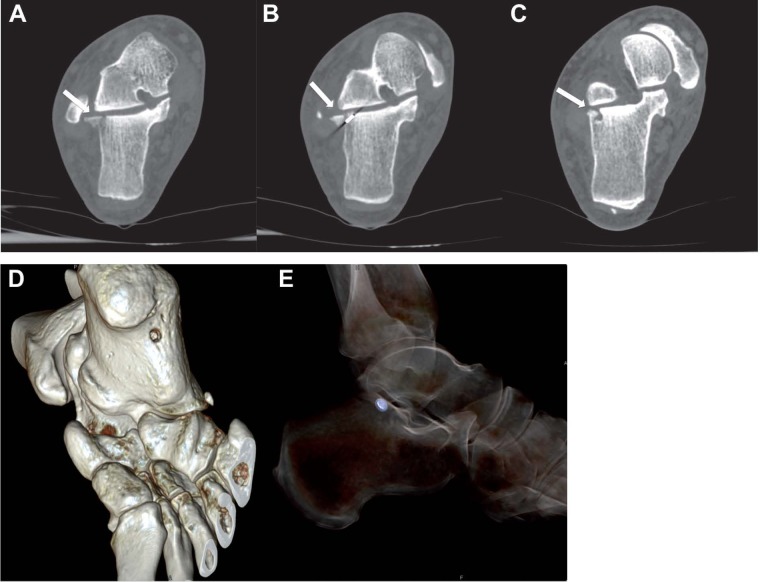
Figure 2.
CT images with MPR in sagittal (A) para-axial (B) and para-coronal planes (C), show multiple intra-articular fracture (white arrows)
Figure 3.
VR reconstruction shows three intra-articular fracture lines
Figure 4.
CT images in axial plane and VR reconstructions show an intra-articular fracture due to bone perforation by a foreign metallic body (A, B and C) (white arrows). VR reconstructions show the inlet hole of the foreign body, with course inside the calcaneal body and the foreign body located near the posterior articular facet (D and E)
Figure 5.
CT images with MPR in sagittal (A) para-axial (B) and para-coronal planes (C) show intra-articular line fracture in correspondence of the central portion of the posterior facet (white arrows). The excessive impact force generated additional extra-articular fracture lines in correspondence of the posterior heel (red arrows). VR reconstruction, posterior view, better shows extra-articular fractures (D)
Badillo et al evaluated the classification through axial and coronal CT images placed parallel and perpendicular, respectively, to the posterior facet of the subtalar joint (31).
Sanders classification system:
- Type 1: Non-displaced fractures (displacement <2 mm).
- Type 2: Two part fracture with one fracture line and is divided into three subtypes based on the side of the fracture line: lateral (IIA), central (IIB), or medial (IIC).
- Type 3: Three part fractures from two lines of fracture, divided into subtypes IIIAB (with two primary lines, one lateral and one central relative to the posterior facet and subtalar joint), IIIAC (two primary fracture lines, one lateral and one medial relative to the posterior facet and subtalar joint), IIIBC (two primary fracture lines, one central and one medial relative to the posterior facet and subtalar joint).
- Type 4: Four part or more than three lines of fracture (31).
The extra-articular fractures are fractures that do not involve the posterior facet of the subtalar and represent 25% of heel fractures (Fig. 5 and 6) (2).
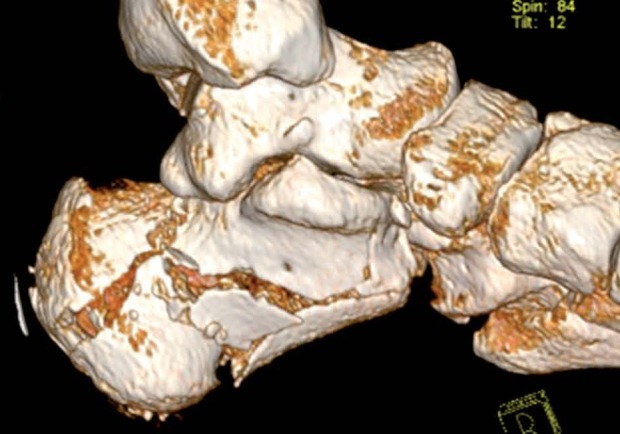
Figure 6.

CT images with MPR in sagittal (A) and coronal (B) shows an extra-articular fracture of the posterior portion of the calcaneus (white arrows)
These are divided:
- Type A: fracture involving the anterior process of the calcaneus.
- Type B: fracture involving the midcalcaneus or body, including lateral process, sustentaculum tali or trochlear process.
- Type C: fracture involving the posterior calcaneus, including medial tubercle and posterior tuberosity (31).
Imaging of calcaneus fracture
Baptista et al have attempted to evaluate the predictive capacity of imaging for the fracture surgical outcome regardless of the type of treatment (61, 62).
In this study, 44 patients with surgically treated calcaneal fracture were included. Böhler’s angle (BA) (Fig. 7) and GA, were measured in pre- and post-operative lateral radiographs; tibiotalar angle and talocalcaneal height were measured before surgical intervention in lateral radiographs. Coronal CT scans were evaluated for the classification of fractures with the Sanders system. Only postoperative measurements of BA correlated with the clinical outcome. None of the remaining measurements (pre- and post-operative) was capable to predict clinical outcomes. Higher postoperative values of BA included skin-related complications during the first follow-up. This datum contradicts the literature which states that restoring BA positively influences the function (63-65). The authors state that the open surgery used allowed a greater restorations of BA but also determined association with skin related complications, which however did not affect the long-term clinical outcome of calcaneus fractures. Finally, type 4 fractures according to Sanders system, predicted the event of any hazard during follow-up (61).
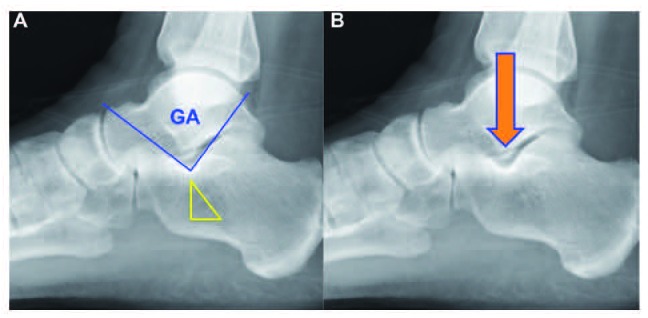
Figure 7.

Measurement of the BA on the radiography in lateral projection
Yu et al showed the aspect features and mechanisms of the calcaneal avulsion fractures, dividing them for sites of vulnerability (66).
In particular, avulsion fractures of the calcaneal tuberosity constitute only 1.3-2.7% of calcaneus fractures (67). They are caused by a shear-compression or avulsion (66).
There are 4 types of avulsion fractures:
- type 1: simple avulsion with bone fragment of variable size.
- type 2: beak fracture with a horizontal fracture which reaches the posterior body.
- type 3: infrabursal avulsion by the superficial fibers quota of the half third of the Achilles tendon.
- type 4: tiny beak fracture avulsed from the deep fibers quota of the tendon (67).
Rupture of plantar fascia is uncommon (68, 69). Fractures in the medial calcaneus process can happen. Most of these types of fractures are due to compression mechanisms, rarely to an avulsion of the medial plantar process (56, 70). The radiographic aspect is a small fleck of bone from the donor site at the level of the inferior surface of the calcaneal tuberosity or a break in correspondence of the medial process cortex (66).
Another type of fracture is the one involving the anterior calcaneal process. The anterior calcaneal process constitutes the proximal insertion of the bifurcated ligament (66). The fracture of this process occurs in 5% of patients with ankle fracture (71-73). Mechanisms that generate such a lesion are impaction forces or compression and extreme tensile forces (74). In many cases CT or MRI are mandatory, as this type of fracture is very difficult to detect (74-76). A lateral radiograph helps identify the fracture that appears vertically through the process. Oblique projection can help (71).
Fractures of the front processes are classified into three types:
- type 1: non-displaced small fracture (<1 cm).
- type 2: minimal displacement (>2 mm) without evidence of involvement of calcaneo-cuboid joint.
- type 3: comminuted or large with evidence of calcaneo-cuboid joint involvement (>25%) (66).
Types 1 and 2 fractures of the anterior calcaneal process are generally avulsive, while most of the type 3 fractures are compressive (66).
Another calcaneal fracture described by Yu et al is the avulsion of the origin of the extensor digitorum brevis muscle. This type of lesion is generated by forced inversion of the foot. This results in tearing of the muscle with an avulsion fracture (77, 78).
Finally, the authors described the fracture avulsion of the calcaneo-cuboid joint. This joint is covered by an articular capsule stabilized by the calcaneo-cuboid limb of the bifurcated ligament, by the dorsal (dorsolateral) calcaneo-cuboid ligament, by the plantar calcaneo-cuboid ligament and by the long plantar ligament (79, 80). Most of these avulsion fractures are observed at the insertion of the dorsal calcaneo-cuboid ligament (66). Andermahr et al has classified these lesions into four types:
- type 1: no evidence of fracture and an increased angle of 5-10°
- type 2: occasional fracture flake and evidence of angulation greatest of 10°
- type 3: the most important osseous fragment of 5 mm and the angulation greatest of 10°
- type 4: evidence of compression fracture of medial cuboid and major distraction of joint (81).
This type of fracture is shown by the radiographs of the foot in frontal and oblique projection, appearing as small linear cortical fragments. Magnetic resonance imaging (MRI) can be used to confirm the diagnosis (66).
David et al have proposed a new method for evaluating the heels length by radiographic measurements, defining the calcaneo-talar length ratio (82). One-hundred patients were included in the study. The calcaneo-talar ratio, in fact, has shown good self-observation reliability, being consistent at 1.3. In many cases, it is difficult to reconstruct the lateral calcaneal wall, particularly in multifragmented fractures and in open fractures (83). Most surgeons have internally fixed these fractures by using lateral calcaneal locking plates (84, 85). The length of these plates is between 50 mm and 89 mm. Measuring the heel length intraoperatively can be difficult because of the loss of normal anatomy in very crushed fractures. Knowing the length of the heel will lead to the choice of a plate of the ideal length, not a shorter plate. David et al in this study have shown that knowing preoperatively that radiographic heel length is equal to talus length plus a third allows to choose a plate with a proper length (82).
Wedmore et al have described emergency department evaluation and management of foot and ankle pain. Describing hindfoot injuries have highlighted some key points. In particular they highlighted the role of CT to be considered for the evaluation of hindfoot fractures; explained how calcaneus fractures are often associated with other lesions, such as lower dorsal and lumbar spine fractures. They also explained that the BA of less than 25 has a 100% sensitivity for a heel fracture (86). The settling of the posterior facet corresponds to a decrease in the BA (87, 88).
Gonzalez et have assessed the specific demographic and surgical causal factors that correlate with the settling of the posterior facet (89). In this study 234 intra-articular calcaneal fractures (141 operably treated and 93 treated unoperatively) were evaluated. BA was measured on non-weight-bearing postoperative radiographs and on the latest weight-bearing radiography available after 5 months of surgical intervention. For non-operatively treated patients, BA was measured on weight-bearing radiography available after 5 months of trauma. The fractures have been classified using the Essex-Lopresti and Sanders classification systems. The study showed a decrease in BA time in both categories of patients with an average variation of 8 degrees in BA. This decrease was not related to energy trauma, severity of fracture type (based on Sanders classification), surgeon-based factors, osteoporosis or rheumatoid arthritis. While patient-based variables such as diabetes, increased age and alcohol abuse, were statistically significant increased magnitude of posterior facet settling independently of the treatment type (89).
Worsham et al evaluated the association of open calcaneus fractures with lesions associated with a retrospective study performed on 62 patients (64 fractures) (90). The most common causes were motor vehicle accidents (56.4%) and falls from height (24.1%), while the other causes were motorcycle crashes, crush injuries, and pedestrian versus automotive accidents.
A total of 44 open calcaneal fractures were located on the right, while 22 fractures were located in the left lower extremity. Open calcaneus bilateral fractures were present in 2 patients. The associated lesions were divided into two categories: orthopedic and non-orthopedic. A total of 57 patients had 1 additional orthopedic injuries. In particular, 16 patients had metatarsal fractures, 15 patients had upper extremity fractures, 14 patients with an ipsilateral ankle fracture, 12 patients had talus fractures, 11 patients had a midfoot fracture, 9 patients had spinal fractures (6 of which were located at lumbar spine), 8 patients had a femoral shaft fracture, 5 patients had a cuboid fracture and 4 patients had a posterior tibialis arterial injuries.
A total of 36 patients had an additional non-orthopedic injury. In particular, 10 patients had head injuries, 7 patients had a facial trauma, 6 patients had abdominal trauma (2 liver lacerations, 2 splenic injuries and 2 adrenal hematomas). 13 patients had a traumatic chest (with evidence of pneumothorax in 8 of these patients).
Worsham et al, in this study, stressed that rapid recognition of open calcaneus fractures and their association with other lesions is very important as it could prevent potential life and limb complications (90).
Chang et al described MR Imaging findings in heel pain (91). In particular, among the various causes of heel pain, they showed MR imaging fractures of stress calcanues fractures. This type of fracture is found in cases where the bone does not have time to adapt to the rapid increase in stress, such as in sedentary physical exercise patients (92-94). Radiographs can show a sclerosis often with a vertical orientation, but 24% of them are negative (93). These fractures appear to MRI as a line that reaches the cortex and appears hypointense in T1-weighted and T2-weighted images with bone marrow edemigenic imbibition around (hypointense in T1-weighted and hyperintense in T2-weighted images) (Fig. 8) (91).
Figure 8.
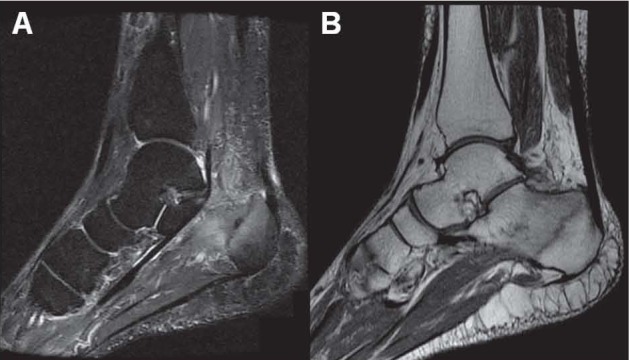
MRI: sagittal image with STIR (Short TI Inversion Recovery) sequence (A) shows a hypointense fracture line, and a diffuse bone marrow edemigenic imbibition of the calcaneal body and anterior portion of Kager’s triangle, which appears hyperintense. Sagittal image obtained with T1-weighted sequence (B) shows the hypointense fracture line and the hypointense edemigenic imbibition
Wong-Chung et al evaluated the incidence of dislocation or subluxation of the peronal tendon in patients with calcaneus fractures (95). Of a total of 79 calcaneal fractures (76 patients, 3 of which with bilateral fractures), 19 exhibited dislocation or subluxation of the peroneal tendons found in CT or surgery (24%). Other present injuries were dislocation of tibialis posterior tendon, fractures of the talar neck, cuboid, medial malleolus and metatarsals. In 9 patients, the dislocation was recognized and/or treated at initial presentation (either on CT or by probing at surgery); in the remaining10 patients, the tendon dislocation was not recognized and/or treated at initial presentation. A bony fleck sign was showed in 11 ankles (5 big fleck and 6 small fleck). Peroneal tendon dislocation was detected before the wound closure in 3 patients treated with surgery (2 patients treated with open reduction with internal fixation and superior peroneal retinaculum repair, and 1 patient treated with open reduction with internal fixation). Both in these 3 patients treated with surgery, and in three other untreated patients, they could notice that the distended tendon was relocated spontaneously. Relocated tendons appeared to peep around the posterolateral corner of the distal fibula.
Finally, all 19 patients with tendon dislocation had swelling at the lateral malleol except one case; in addition, 22 patients with swelling in the lateral malleolar side had no associated tendon dislocation. Out of a total of 30 patients with swelling in the calcaneal area, only one patient had tendon dislocation (95).
Ballard et al evaluated the incidence of tendon entrapments and dislocations in ankle and hindfoot fractures using CT. In a total of 398 patients, 64 patients showed tendon entrapment and/or dislocation. In particular, 30 patients had 40 tendon entrapments, 31 patients had 59 tendon dislocations, and 3 patients showed both tendon entrapment (n=4) and dislocation (n=6). There were 31 patients with tendon dislocation, and 27 of these patients showed peroneal tendon dislocation. A total of 23 out of 27 peroneal dislocations were associated with calcaneus fractures: 19 Sanders type IV fractures, 2 Sanders Type III AC fractures, 1 Sanders type III AB fracture and 1 Sanders type II A fracture (96).
Golshani et al evaluated the incidence of visible tendon lesions by CT images, in patients with complex ankle or hindfoot fractures (97). Calcaneus fractures were classified by the Essex-Lopresti system and a joint depression type fracture was considered to have BA less than 20°. A total of 410 patients were included in the study, 33 of whom had calcaneus fractures (27 joint depression and 6 isolated impaction of the anterior calcaneus process). Calcaneus fractures showed increased risk of peroneus brevis tendon (11.86 times), peroneus longus tendon (10.71 times), and flexor halluci longus tendon (5.21 times) injuries (97).
Otero et al reported intra-class correlation coefficient and tolerance limits for BA and GA (59). In particular, four orthopedics performed such measurements pre- and post-operative lateral radiographs of the foot. Intra-class correlation coefficient was used to calculate intra- and inter-observer reliability. They also calculated the frequency of consensus given to an agreed discrepancy. The study showed the limitations in reliability of both the BA and the GA. Even with optimal settings, in fact, there was a common disagreement in radiographic interpretations. For these results, the authors advise the use of caution when applying the BA to direct clinical decisions. Finally they suggest that three-dimensional imaging could be used to increase the reliability of BA (98).
Gorbachova et al evaluated the significance of plantar talar head injury in predicting bone lesions or soft ankle tissue (99). Fourty-one MRI of the ankle of patients with plantar talar head injury (20 were fractures and 21 were bone contusions) were evaluated in the study, which showed a significant association of plantar talar head injury with the anterior process of calcaneus injuries (24% of the cases) (99).
Harnroongroj et al have created a new classification system for intra-articular calcaneus fractures (100). In particular, the elements considered were the sustentacular fragment (a medial fragment of the calcaneal body fracture that remains attached to the talus) created by the compressive load, the fracture of the posterior calcaneal facet and of calcaneal body (101, 102). The creation of this new classification was based on the fact that the Sanders and Essex-Lopresti classification system did not correlate with the choice of treatment (56, 59, 103). In particular, these classification systems do not consider the relationship between calcaneal facet and body fractures, important for the choice of treatment for intra-articular calcaneus fractures (104, 105).
The sustentacular fragment was configured with axial CT images in three types:
- type A: sustentaculum tali fragment containing middle calcaneal facet.
- type B: sustentaculum tali containing middle calcaneal facet and included medial aspect of the posterior calcaneal facet as a single unit.
- type C: sustentaculum tali containing middle calcaneal facet and entire posterior calcaneal facet as a single unit.
Types A and B have been subdivided into 4 subtypes using axial and sagittal CT images. The subtypes were classified considering the fracture of the posterior calcaneal facet in terms of intact articular surface or intra-articular fracture of the posterior calcaneal facet and the association with the components of the calcaneal body fracture. Type C had no subtype, had no separated fragment of posterior calcaneal facet.
In this study 112 patients with 126 displaced intra-articular calcaneus fractures (51 type A, 53 type B and 22 type C) were enrolled.
Type C fracture showed a better quality of fracture reduction compared to type B fracture which showed the worst quality of fracture reduction. This is due to the type of fracture configuration. The type C fracture has a simple configuration, unlike the type B fracture that has a complex configuration. This classification system has shown correlation with implant fixation, quality of fracture reduction and choice of treatment (100).
Schiller et al have evaluated the lower extremity avulsion fractures in the pediatric and adolescent athlete (106). In particular, in describing calcaneal avulsion fractures, the authors state that this type of lesion is rare, as the hepatic apophysis is well protected by the cutting forces that cause the fracture. These injuries can also be mistakenly diagnosed as with muscle strain or Sever disease. Finally, they claim that these lesions must be handled on a case-by-case basis, and no recommendations can be made because of the limited available cases (106).
Mandell et al evaluated stress fractures of the foot and ankle (107). The authors state that stress fractures mainly involve the posteromidial distal tibia, the calcaneus, and the metatarsals. In particular, heel is involved with the anterior tibia in patients who are jumping in activities like basketball players (108). It is also a common cause of heel pain in soldiers undergoing basic training (109). The authors explain the layout of the calcaneal trabecular is composed of perpendicular arches to the posterior cortex. The calcaneal stress fractures are perpendicular to the trabecules, presenting as sclerosis on radiographs (10 days after the onset of the symptomatology), and as a hypointense line to the MRI with surrounding edema. Most of these types of fractures are located posteriorly (56% has posterior location, 18% is located at the middle heel and 26% at the anterior portion of the calcaneus) (110, 111). Anteriorly, the curvature of the trabecules, results in horizontal fracture lines (107). The first attempt is conservative treatment, the displacement is rare (112). There may also be an association with the rupture of the plantar fascia (107).
Analysis of recent calcaneal fracture studies leads to a diagnostic approach geared to the choice of treatment and improvement of patient outcomes. In particular, the classification of Harnroongroj et al could change the diagnostic approach to this type of lesion, having a direct correlation with choice of treatment and the quality of fracture reduction. Further studies have shown correlation of calcaneal fractures with fractures of other bone structures or soft tissue impairment (peroneal tendon dislocation or increased risk of developing peroneus brevis and peroneus longus tendons injuries). In this context, the measurement of the calcaneotalar ratio plays an important role, providing the possibility of performing a targeted surgery to the actual size of the heel of the patient. These data suggest an approach geared to the specific choice of treatment and to improving patient outcomes.
References
- 1.Daftary A, Haims AH, Baumgaertner MR. Fractures of the calcaneus: a review with emphasis on CT. Radiographics. 2005;25(5):1215–26. doi: 10.1148/rg.255045713. [DOI] [PubMed] [Google Scholar]
- 2.Stoller DW, Tirman PFJ, Bredella M. Ankle and foot, osseous fractures, calcaneal fractures. Diagnostic imaging: orthopaedics. Salt Lake City. 2004:70–4. [Google Scholar]
- 3.De Filippo M, Corsi A, Evaristi L, Bertoldi C, Sverzellati N, Averna R, et al. Critical issues in radiology requests and reports. Radiol Med. 2011;116(1):152–62. doi: 10.1007/s11547-010-0587-z. [DOI] [PubMed] [Google Scholar]
- 4.de Filippo M, Azzali E, Pesce A, Saba L, Mostardi M, Borgia D, et al. CT arthrography for evaluation of autologous chondrocyte and chondral-inductor scaffold implantation in the osteochondral lesions of the talus. Acta Biomedica. 2016;87(3):51–6. [PubMed] [Google Scholar]
- 5.De Filippo M, Rovani C, Sudberry JJ, Rossi F, Pogliacomi F, Zompatori M. Magnetic resonance imaging comparison of intra-articular cavernous synovial hemangioma and cystic synovial hyperplasia of the knee. Acta Radiol. 2006;47(6):581–4. doi: 10.1080/02841850600767724. [DOI] [PubMed] [Google Scholar]
- 6.Lee P, Hunter TB, Taljanovic M. Musculoskeletal colloquialisms: how did we come up with these names. Radiographics. 2004;24(4):1009–27. doi: 10.1148/rg.244045015. [DOI] [PubMed] [Google Scholar]
- 7.Grassi R, Lombardi G, Reginelli A, Capasso F, Romano F, Floriani I, et al. Coccygeal movement: assessment with dynamic MRI. Eur J Radiol. 2007;61(3):473–9. doi: 10.1016/j.ejrad.2006.07.029. [DOI] [PubMed] [Google Scholar]
- 8.Pinto A, Reginelli A, Pinto F, Lo Re G, Midiri F, Muzj C, et al. Errors in imaging patients in the emergency setting. Br J Radiol. 2016;89(1061) doi: 10.1259/bjr.20150914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ierardi AM, Xhepa G, Duka E, Laganà D, Ianniello A, Floridi C, et al. Ethylene-vinyl alcohol polymer trans-arterial embolization in emergency peripheral active bleeding: Initial experience. Int Angiol. 2015;34(6):28–35. [PubMed] [Google Scholar]
- 10.Pinto A, Brunese L, Pinto F, Acampora C, Romano L. E-learning and education in radiology. Eur J Radiol. 2011;78(3):368–371. doi: 10.1016/j.ejrad.2010.12.029. [DOI] [PubMed] [Google Scholar]
- 11.Janzen DL, Connell DG, Munk PL, Buckley RE, Meek RN, Schechter MT. Intraarticular fractures of the calcaneus: value of CT findings in determining prognosis. AJR Am J Roentgenol. 1992;158(6):1271–4. doi: 10.2214/ajr.158.6.1590122. [DOI] [PubMed] [Google Scholar]
- 12.Pinto A, Brunese L, Pinto F, Acampora C, Romano L. E-learning and education in radiology. Eur J Radiol. 2011;78(3):368–371. doi: 10.1016/j.ejrad.2010.12.029. [DOI] [PubMed] [Google Scholar]
- 13.Nurzynska D, Di Meglio F, Castaldo C, Latino F, Romano V, Miraglia R, et al. Flatfoot in children: anatomy of decision making. Ital J Anat Embryol. 2012;117(2):98–106. [PubMed] [Google Scholar]
- 14.Zappia M, Castagna A, Barile A, Chianca V, Brunese L, Pouliart N. Imaging of the coracoglenoid ligament: a third ligament in the rotator interval of the shoulder. Skelet Radiol. 2017;46(8):1101–11. doi: 10.1007/s00256-017-2667-9. [DOI] [PubMed] [Google Scholar]
- 15.Perrotta FM, Astorri D, Zappia M, Reginelli A, Brunese L, Lubrano E. An ultrasonographic study of enthesis in early psoriatic arthritis patients naive to traditional and biologic DMARDs treatment. Rheumatol Int. 2016;36(11):1579–83. doi: 10.1007/s00296-016-3562-8. [DOI] [PubMed] [Google Scholar]
- 16.Benson E, Conroy C, Hoyt DB, Eastman AB, Pacyna S, Smith J, et al. Calcaneal fractures in occupants involved in severe frontal motor vehicle crashes. Accid Anal Prev. 2007;39(4):794–9. doi: 10.1016/j.aap.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 17.Seipel RC, Pintar FA, Yoganandan N, Boynton MD. Biomechanics of calcaneal fractures: a model for the motor vehicle. Clin Orthop Relat Res. 2001;388:218–24. [PubMed] [Google Scholar]
- 18.Barile A, La Marra A, Arrigoni F, Mariani S, Zugaro L, Splendiani A, et al. Anaesthetics, steroids and platelet-rich plasma (PRP) in ultrasound-guided musculoskeletal procedures. Br J Radiol. 2016;89(1065) doi: 10.1259/bjr.20150355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zappia M, Carfora M, Romano AM, Reginelli A, Brunese L, Rotondo A, et al. Sonography of chondral print on humeral head. Skelet Radiol. 2016;45(1):35–40. doi: 10.1007/s00256-015-2238-x. [DOI] [PubMed] [Google Scholar]
- 20.Zappia M, Di Pietto F, Aliprandi A, Pozza S, De Petro P, Muda A, et al. Multi-modal imaging of adhesive capsulitis of the shoulder. Insights Imaging. 2016;7(3):365–71. doi: 10.1007/s13244-016-0491-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hedlund LJ, Maki DD, Griffiths HJ. Calcaneal fractures in diabetic patients. J Diabetes Complications. 1998;12(2):81–7. doi: 10.1016/s1056-8727(97)00052-4. [DOI] [PubMed] [Google Scholar]
- 22.Martini F, Kremling E, Sell S. Bilateral atraumatic avulsion fracture of the calcaneal tubercle in osteomalacia during fluoride therapy--a case report. Acta Orthop Scand. 1999;70(1):91–2. doi: 10.3109/17453679909000968. [DOI] [PubMed] [Google Scholar]
- 23.Squires B, Allen PE, Livingstone J, Atkins RM. Fractures of the tuberosity of the calcaneus. J Bone Joint Surg Br. 2001;83(1):55–61. doi: 10.1302/0301-620x.83b1.11184. [DOI] [PubMed] [Google Scholar]
- 24.Russo A, Reginelli A, Zappia M, Rossi C, Fabozzi G, Cerrato M, et al. Ankle fracture: radiographic approach according to the Lauge-Hansen classification. Musculoskelet Surg. 2013;97(2):S155–60. doi: 10.1007/s12306-013-0284-x. [DOI] [PubMed] [Google Scholar]
- 25.Zappia M, Cuomo G, Martino MT, Reginelli A, Brunese L. The effect of foot position on Power Doppler Ultrasound grading of Achilles enthesitis. Rheumatol Int. 2016;36(6):871–4. doi: 10.1007/s00296-016-3461-z. [DOI] [PubMed] [Google Scholar]
- 26.Schepers T, Ginai AZ, Van Lieshout EM, Patka P. Demographics of extra-articular calcaneal fractures: including a review of the literature on treatment and outcome. Arch Orthop Trauma Surg. 2008;128(10):1099–106. doi: 10.1007/s00402-007-0517-2. [DOI] [PubMed] [Google Scholar]
- 27.Inokuchi S, Usami N, Hiraishi E, Hashimoto T. Calcaneal fractures in children. J Pediatr Orthop. 1998;18(4):469–74. [PubMed] [Google Scholar]
- 28.Cuomo G, Zappia M, Iudici M, Abignano G, Rotondo A, Valentini G. The origin of tendon friction rubs in patients with systemic sclerosis: a sonographic explanation. Arthritis Rheum. 2012;64(4):1291–3. doi: 10.1002/art.34319. [DOI] [PubMed] [Google Scholar]
- 29.Russo A, Zappia M, Reginelli A, Carfora M, D’Agosto GF, La Porta M, et al. Ankle impingement: a review of multimodality imaging approach. Musculoskelet Surg. 2013;97(2):S161–8. doi: 10.1007/s12306-013-0286-8. [DOI] [PubMed] [Google Scholar]
- 30.Aliprandi A, Di Pietto F, Minafra P, Zappia M, Pozza S, Sconfienza LM. Femoro-acetabular impingement: what the general radiologist should know. Radiol Med. 2014;119(2):103–12. doi: 10.1007/s11547-013-0314-7. [DOI] [PubMed] [Google Scholar]
- 31.Badillo K, Pacheco JA, Padua SO, Gomez AA, Colon E, Vidal JA. Multidetector CT evaluation of calcaneal fractures. Radiographics. 2011;31(1):81–92. doi: 10.1148/rg.311105036. [DOI] [PubMed] [Google Scholar]
- 32.Schmidt TL, Weiner DS. Calcaneal fractures in children. An evaluation of the nature of the injury in 56 children. Clin Orthop Relat Res. 1982;171:150–5. [PubMed] [Google Scholar]
- 33.Sanders R. Displaced intra-articular fractures of the calcaneus. J Bone Joint Surg Am. 2000;82(2):225–50. doi: 10.2106/00004623-200002000-00009. [DOI] [PubMed] [Google Scholar]
- 34.Segal D, Marsh JL, Leiter B. Clinical application of computerized axial tomography (CAT) scanning of calcaneus fractures. Clin Orthop Relat Res. 1985;199:114–23. [PubMed] [Google Scholar]
- 35.Piccolo CL, Galluzzo M, Ianniello S, Trinci M, Russo A, Rossi E, et al. Pediatric musculoskeletal injuries: role of ultrasound and magnetic resonance imaging. Musculoskelet Surg. 2017;101(1):85–102. doi: 10.1007/s12306-017-0452-5. [DOI] [PubMed] [Google Scholar]
- 36.Piccolo CL, Galluzzo M, Trinci M, Ianniello S, Tonerini M, Brunese L, et al. Lower Limbs Trauma in Pediatrics. Semin Musculoskelet Radiol. 2017;21(3):175–83. doi: 10.1055/s-0037-1602417. [DOI] [PubMed] [Google Scholar]
- 37.Zappia M, Reginelli A, Russo A, D’Agosto GF, Di Pietto F, Genovese EA, et al. Long head of the biceps tendon and rotator interval. Musculoskeletal Surg. 2013;97(2):S99–S108. doi: 10.1007/s12306-013-0290-z. [DOI] [PubMed] [Google Scholar]
- 38.Cappabianca S, Colella G, Russo A, Pezzullo M, Reginelli A, Iaselli F, et al. Maxillofacial fibrous dysplasia: personal experience with gadoliniumenhanced magnetic resonance imaging. Radiol Med. 2008;113(8):1198–210. doi: 10.1007/s11547-008-0329-7. [DOI] [PubMed] [Google Scholar]
- 39.Cappabianca S, Scuotto A, Iaselli F, Pignatelli di Spinazzola N, Urraro F, Sarti G, et al. Computed tomography and magnetic resonance angiography in the evaluation of aberrant origin of the external carotid artery branches. Surg Radiol Anat. 2012;34(5):393–9. doi: 10.1007/s00276-011-0926-3. [DOI] [PubMed] [Google Scholar]
- 40.Cappabianca S, Colella G, Pezzullo MG, Russo A, Iaselli F, Brunese L, et al. Lipomatous lesions of the head and neck region: Imaging findings in comparison with histological type. Radiol Med. 2008;113(5):758–70. doi: 10.1007/s11547-008-0258-5. [DOI] [PubMed] [Google Scholar]
- 41.Furey A, Stone C, Squire D, Harnett J. Os calcis fractures: analysis of interobserver variability in using Sanders classification. J Foot Ankle Surg. 2003;42(1):21–3. doi: 10.1053/jfas.2003.49999. [DOI] [PubMed] [Google Scholar]
- 42.Cirillo M, Caranci F, Tortora F, Corvino F, Pezzullo F, Conforti R, et al. Structural neuroimaging in dementia. Journal Alzh Dis. 2012;29(1):16–19. [Google Scholar]
- 43.Muccio CF, Di Blasi A, Esposito G, Brunese L, D’Arco F, Caranci F. Perfusion and spectroscopy magnetic resonance imaging in a case of lymphocytic vasculitis mimicking brain tumor. Pol J Radiol. 2013;78(3):66–9. doi: 10.12659/PJR.884011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Caranci F, Briganti F, La Porta M, Antinolfi G, Cesarano E, Fonio P, et al. Magnetic resonance imaging in brachial plexus injury. Musculoskeletal Surg. 2013;97(2):S181–S90. doi: 10.1007/s12306-013-0281-0. [DOI] [PubMed] [Google Scholar]
- 45.Di Zazzo E, Porcile C, Bartollino S, Moncharmont B. Critical Function of PRDM2 in the Neoplastic Growth of Testicular Germ Cell Tumors. Biology (Basel) 2016;5(4) doi: 10.3390/biology5040054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dragoni S, Turin I, Laforenza U, Potenza DM, Bottino C, Glasnov TN, et al. Store-operated Ca2+ entry does not control proliferation in primary cultures of human metastatic renal cellular carcinoma. Biomed Res Int. 2014;2014:739494. doi: 10.1155/2014/739494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ronco V, Potenza DM, Denti F, Vullo S, Gagliano G, Tognolina M, et al. A novel Ca(2)(+)-mediated cross-talk between endoplasmic reticulum and acidic organelles: implications for NAADP-dependent Ca(2)(+) signalling. Cell Calcium. 2015;57(2):89–100. doi: 10.1016/j.ceca.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 48.Potenza DM, Guerra G, Avanzato D, Poletto V, Pareek S, Guido D, et al. Hydrogen sulphide triggers VEGF-induced intracellular Ca(2)(+) signals in human endothelial cells but not in their immature progenitors. Cell Calcium. 2014;56(3):225–34. doi: 10.1016/j.ceca.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 49.Barile A, Arrigoni F, Bruno F, Guglielmi G, Zappia M, Reginelli A, et al. Computed Tomography and MR Imaging in Rheumatoid Arthritis. Radiol Clin North Am. 2017 doi: 10.1016/j.rcl.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 50.Barile A, Bruno F, Arrigoni F, Splendiani A, Di Cesare E, Zappia M, et al. Emergency and Trauma of the Ankle. Semin Musculoskelet Radiol. 2017;21(3):282–9. doi: 10.1055/s-0037-1602408. [DOI] [PubMed] [Google Scholar]
- 51.Funk JR, Crandall JR, Tourret LJ, MacMahon CB, Bass CR, Patrie JT, et al. The axial injury tolerance of the human foot/ankle complex and the effect of Achilles tension. J Biomech Eng. 2002;124(6):750–7. doi: 10.1115/1.1514675. [DOI] [PubMed] [Google Scholar]
- 52.Forman JL, Lopez-Valdes FJ, Duprey S, Bose D, Del Pozo de Dios E, Subit D, et al. The tolerance of the human body to automobile collision impact - a systematic review of injury biomechanics research, 1990-2009. Accid Anal Prev. 2015;80:7–17. doi: 10.1016/j.aap.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 53.Reginelli A, Zappia M, Barile A, Brunese L. Strategies of imaging after orthopedic surgery. Musculoskeletal Surg. 2017;101 doi: 10.1007/s12306-017-0458-z. [DOI] [PubMed] [Google Scholar]
- 54.Di Pietto F, Chianca V, de Ritis R, Cesarano E, Reginelli A, Barile A, et al. Postoperative imaging in arthroscopic hip surgery. Musculoskeletal Surg. 2017;101:43–9. doi: 10.1007/s12306-017-0459-y. [DOI] [PubMed] [Google Scholar]
- 55.Barile A, Bruno F, Mariani S, Arrigoni F, Brunese L, Zappia M, et al. Follow-up of surgical and minimally invasive treatment of Achilles tendon pathology: a brief diagnostic imaging review. Musculoskeletal Surg. 2017;101:51–61. doi: 10.1007/s12306-017-0456-1. [DOI] [PubMed] [Google Scholar]
- 56.Essex-Lopresti P. The mechanism, reduction technique, and results in fractures of the os calcis. Br J Surg. 1952;39(157):395–419. doi: 10.1002/bjs.18003915704. [DOI] [PubMed] [Google Scholar]
- 57.Reginelli A, Capasso R, Ciccone V, Croce MR, Di Grezia G, Carbone M, et al. Usefulness of triphasic CT aortic angiography in acute and surveillance: Our experience in the assessment of acute aortic dissection and endoleak. Int J Surg. 2016;33:S76–S84. doi: 10.1016/j.ijsu.2016.05.048. [DOI] [PubMed] [Google Scholar]
- 58.Masciocchi C, Arrigoni F, Barile A. Role of conventional RX, CT, and MRI in the evaluation of prosthetic joints. Imaging of Prosthetic Joints: A Combined Radiological and Clinical Perspective: Springer-Verlag Milan. 2014:63–9. [Google Scholar]
- 59.Sanders R, Fortin P, DiPasquale T, Walling A. Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop Relat Res. 1993;290:87–95. [PubMed] [Google Scholar]
- 60.Masciocchi C, Conchiglia A, Conti L, Barile A. Imaging of insufficiency fractures. Geriatric Imaging: Springer-Verlag Berlin Heidelberg; 2013:83–91. [Google Scholar]
- 61.Baptista M, Pinto R, Torres J. Radiological predictive factors for the outcome of surgically treated calcaneus fractures. Acta Orthop Belg. 2015;81(2):218–24. [PubMed] [Google Scholar]
- 62.Masciocchi C, Conti L, D’Orazio F, Conchiglia A, Lanni G, Barile A. Errors in musculoskeletal MRI. Errors in Radiology: Springer-Verlag Milan. 2012:209–17. [Google Scholar]
- 63.De Groot R, Frima AJ, Schepers T, Roerdink WH. Complications following the extended lateral approach for calcaneal fractures do not influence mid- to long-term outcome. Injury. 2013;44(11):1596–600. doi: 10.1016/j.injury.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 64.Makki D, Alnajjar HM, Walkay S, Ramkumar U, Watson AJ, Allen PW. Osteosynthesis of displaced intra-articular fractures of the calcaneum: a long-term review of 47 cases. J Bone Joint Surg Br. 2010;92(5):693–700. doi: 10.1302/0301-620X.92B5.23542. [DOI] [PubMed] [Google Scholar]
- 65.Rammelt S, Zwipp H, Schneiders W, Durr C. Severity of injury predicts subsequent function in surgically treated displaced intraarticular calcaneal fractures. Clin Orthop Relat Res. 2013;471(9):2885–98. doi: 10.1007/s11999-013-3062-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yu SM, Yu JS. Calcaneal Avulsion Fractures: An Often Forgotten Diagnosis. AJR Am J Roentgenol. 2015;205(5):1061–7. doi: 10.2214/AJR.14.14190. [DOI] [PubMed] [Google Scholar]
- 67.Lee SM, Huh SW, Chung JW, Kim DW, Kim YJ, Rhee SK. Avulsion fracture of the calcaneal tuberosity: classification and its characteristics. Clin Orthop Surg. 2012;4(2):134–8. doi: 10.4055/cios.2012.4.2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Leach R, Jones R, Silva T. Rupture of the plantar fascia in athletes. J Bone Joint Surg Am. 1978;60(4):537–9. [PubMed] [Google Scholar]
- 69.Pai VS. Rupture of the plantar fascia. J Foot Ankle Surg. 1996;35(1):39–40. doi: 10.1016/s1067-2516(96)80010-x. [DOI] [PubMed] [Google Scholar]
- 70.Pelletier JP, Kanat IO. Avulsion fracture of the calcaneus at the origin of the abductor hallucis muscle. J Foot Surg. 1990;29(3):268–71. [PubMed] [Google Scholar]
- 71.Yu JS, Cody ME. A template approach for detecting fractures in adults sustaining low-energy ankle trauma. Emerg Radiol. 2009;16(4):309–18. doi: 10.1007/s10140-009-0796-8. [DOI] [PubMed] [Google Scholar]
- 72.Agnholt J, Nielsen S, Christensen H. Lesion of the ligamentum bifurcatum in ankle sprain. Arch Orthop Trauma Surg. 1988;107(5):326–8. doi: 10.1007/BF00451515. [DOI] [PubMed] [Google Scholar]
- 73.Renfrew DL, el-Khoury GY. Anterior process fractures of the calcaneus. Skeletal Radiol. 1985;14(2):121–5. doi: 10.1007/BF00349747. [DOI] [PubMed] [Google Scholar]
- 74.Ouellette H, Salamipour H, Thomas BJ, Kassarjian A, Torriani M. Incidence and MR imaging features of fractures of the anterior process of calcaneus in a consecutive patient population with ankle and foot symptoms. Skeletal Radiol. 2006;35(11):833–7. doi: 10.1007/s00256-006-0154-9. [DOI] [PubMed] [Google Scholar]
- 75.Robbins MI, Wilson MG, Sella EJ. MR imaging of anterosuperior calcaneal process fractures. AJR Am J Roentgenol. 1999;172(2):475–9. doi: 10.2214/ajr.172.2.9930806. [DOI] [PubMed] [Google Scholar]
- 76.Gilheany MF. Injuries to the anterior process of the calcaneum. The Foot. 2002;12(3):142–9. [Google Scholar]
- 77.Petrover D, Schweitzer ME, Laredo JD. Anterior process calcaneal fractures: a systematic evaluation of associated conditions. Skeletal Radiol. 2007;36(7):627–32. doi: 10.1007/s00256-006-0262-6. [DOI] [PubMed] [Google Scholar]
- 78.Norfray JF, Rogers LF, Adamo GP, Groves HC, Heiser WJ. Common calcaneal avulsion fracture. AJR Am J Roentgenol. 1980;134(1):119–23. doi: 10.2214/ajr.134.1.119. [DOI] [PubMed] [Google Scholar]
- 79.Melao L, Canella C, Weber M, Negrao P, Trudell D, Resnick D. Ligaments of the transverse tarsal joint complex: MRI-anatomic correlation in cadavers. AJR Am J Roentgenol. 2009;193(3):662–71. doi: 10.2214/AJR.08.2084. [DOI] [PubMed] [Google Scholar]
- 80.Patil V, Ebraheim N, Wagner R, Owens C. Morphometric dimensions of the dorsal calcaneocuboid ligament. Foot Ankle Int. 2008;29(5):508–12. doi: 10.3113/FAI-2008-0508. [DOI] [PubMed] [Google Scholar]
- 81.Andermahr J, Helling HJ, Maintz D, Monig S, Koebke J, Rehm KE. The injury of the calcaneocuboid ligaments. Foot Ankle Int. 2000;21(5):379–84. doi: 10.1177/107110070002100504. [DOI] [PubMed] [Google Scholar]
- 82.David V, Stephens TJ, Kindl R, Ang A, Tay WH, Asaid R, et al. Calcaneotalar ratio: a new concept in the estimation of the length of the calcaneus. J Foot Ankle Surg. 2015;54(3):370–2. doi: 10.1053/j.jfas.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 83.Lawrence SJ. Open calcaneal fractures: assessment and management. Foot Ankle Clin. 2005;10(3):491–502. doi: 10.1016/j.fcl.2004.11.005. vi. [DOI] [PubMed] [Google Scholar]
- 84.Frankel JP, Anderson CD. The use of a calcaneal reconstruction plate in intra-articular calcaneal fractures. J Foot Ankle Surg. 1996;35(4):318–30. doi: 10.1016/s1067-2516(96)80081-0. discussion 70. [DOI] [PubMed] [Google Scholar]
- 85.Basile A. Operative versus nonoperative treatment of displaced intra-articular calcaneal fractures in elderly patients. J Foot Ankle Surg. 2010;49(1):25–32. doi: 10.1053/j.jfas.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 86.Wedmore I, Young S, Franklin J. Emergency department evaluation and management of foot and ankle pain. Emerg Med Clin North Am. 2015;33(2):363–96. doi: 10.1016/j.emc.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 87.Bakker B, Halm JA, Van Lieshout EM, Schepers T. The fate of Bohler’s angle in conservatively-treated displaced intra-articular calcaneal fractures. Int Orthop. 2012;36(12):2495–9. doi: 10.1007/s00264-012-1706-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Buckley RE. Evidence for the best treatment for displaced intra-articular calcaneal fractures. Acta Chir Orthop Traumatol Cech. 2010;77(3):179–85. [PubMed] [Google Scholar]
- 89.Gonzalez TA, Lucas RC, Miller TJ, Gitajn IL, Zurakowski D, Kwon JY. Posterior Facet Settling and Changes in Bohler’s Angle in Operatively and Nonoperatively Treated Calcaneus Fractures. Foot & Ankle International. 2015;36(11):1297–309. doi: 10.1177/1071100715592448. [DOI] [PubMed] [Google Scholar]
- 90.Worsham JR, Elliott MR, Harris AM. Open Calcaneus Fractures and Associated Injuries. J Foot Ankle Surg. 2016;55(1):68–71. doi: 10.1053/j.jfas.2015.06.015. [DOI] [PubMed] [Google Scholar]
- 91.Chang CD, Wu JS. MR Imaging Findings in Heel Pain. Magn Reson Imaging Clin N Am. 2017;25(1):79–93. doi: 10.1016/j.mric.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 92.Lawrence DA, Rolen MF, Morshed KA, Moukaddam H. MRI of heel pain. AJR Am J Roentgenol. 2013;200(4):845–55. doi: 10.2214/AJR.12.8824. [DOI] [PubMed] [Google Scholar]
- 93.Mayer SW, Joyner PW, Almekinders LC, Parekh SG. Stress Fractures of the Foot and Ankle in Athletes. Sports Health. 2014;6(6):481–91. doi: 10.1177/1941738113486588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wilson ES, Jr., Katz FN. Stress fractures. An analysis of 250 consecutive cases. Radiology. 1969;92(3):481–6. doi: 10.1148/92.3.481. passim. [DOI] [PubMed] [Google Scholar]
- 95.Wong-Chung J, Marley WD, Tucker A, O’Longain DS. Incidence and recognition of peroneal tendon dislocation associated with calcaneal fractures. Foot Ankle Surg. 2015;21(4):254–9. doi: 10.1016/j.fas.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 96.Ballard DH, Campbell KJ, Blanton LE, Williams JT, Sangster G, Hollister AM, et al. Tendon entrapments and dislocations in ankle and hindfoot fractures: evaluation with multidetector computed tomography. Emerg Radiol. 2016;23(4):357–63. doi: 10.1007/s10140-016-1411-4. [DOI] [PubMed] [Google Scholar]
- 97.Golshani A, Zhu L, Cai C, Beckmann NM. Incidence and Association of CT Findings of Ankle Tendon Injuries in Patients Presenting With Ankle and Hindfoot Fractures. AJR Am J Roentgenol. 2017;208(2):373–9. doi: 10.2214/AJR.16.16657. [DOI] [PubMed] [Google Scholar]
- 98.Otero JE, Westerlind BO, Tantavisut S, Karam MD, Phisitkul P, Akoh CC, et al. There is poor reliability of Bohler’s angle and the crucial angle of Gissane in assessing displaced intra-articular calcaneal fractures. Foot Ankle Surg. 2015;21(4):277–81. doi: 10.1016/j.fas.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 99.Gorbachova T, Wang PS, Hu B, Horrow JC. Plantar talar head contusions and osteochondral fractures: associated findings on ankle MRI and proposed mechanism of injury. Skeletal Radiol. 2016;45(6):795–803. doi: 10.1007/s00256-016-2358-y. [DOI] [PubMed] [Google Scholar]
- 100.Harnroongroj T, Harnroongroj T, Suntharapa T, Arunakul M. The new intra-articular calcaneal fracture classification system in term of sustentacular fragment configurations and incorporation of posterior calcaneal facet fractures with fracture components of the calcaneal body. Acta Orthop Traumatol Turc. 2016;50(5):519–26. doi: 10.1016/j.aott.2016.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Harnroongroj T, Chuckpaiwong B, Angthong C, Nanakorn P, Sudjai N, Harnroongroj T. Displaced articular calcaneus fractures: classification and fracture scores: a preliminary study. J Med Assoc Thai. 2012;95(3):366–77. [PubMed] [Google Scholar]
- 102.Gitajn IL, Abousayed M, Toussaint RJ, Ting B, Jin J, Kwon JY. Anatomic Alignment and Integrity of the Sustentaculum Tali in Intra-Articular Calcaneal Fractures: Is the Sustentaculum Tali Truly Constant. J Bone Joint Surg Am. 2014;96(12):1000–5. doi: 10.2106/JBJS.M.00330. [DOI] [PubMed] [Google Scholar]
- 103.Zwipp H, Tscherne H, Thermann H, Weber T. Osteosynthesis of displaced intraarticular fractures of the calcaneus. Results in 123 cases. Clin Orthop Relat Res. 1993;290:76–86. [PubMed] [Google Scholar]
- 104.Schepers T, van Lieshout EM, Ginai AZ, Mulder PG, Heetveld MJ, Patka P. Calcaneal fracture classification: a comparative study. J Foot Ankle Surg. 2009;48(2):156–62. doi: 10.1053/j.jfas.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 105.Swords MP, Alton TB, Holt S, Sangeorzan BJ, Shank JR, Benirschke SK. Prognostic value of computed tomography classification systems for intra-articular calcaneus fractures. Foot Ankle Int. 2014;35(10):975–80. doi: 10.1177/1071100714548196. [DOI] [PubMed] [Google Scholar]
- 106.Schiller J, DeFroda S, Blood T. Lower Extremity Avulsion Fractures in the Pediatric and Adolescent Athlete. J Am Acad Orthop Surg. 2017;25(4):251–9. doi: 10.5435/JAAOS-D-15-00328. [DOI] [PubMed] [Google Scholar]
- 107.Mandell JC, Khurana B, Smith SE. Stress fractures of the foot and ankle, part 2: site-specific etiology, imaging, and treatment, and differential diagnosis. Skeletal Radiol. 2017;46(9):1165–86. doi: 10.1007/s00256-017-2632-7. [DOI] [PubMed] [Google Scholar]
- 108.Daffner RH, Pavlov H. Stress fractures: current concepts. AJR Am J Roentgenol. 1992;159(2):245–52. doi: 10.2214/ajr.159.2.1632335. [DOI] [PubMed] [Google Scholar]
- 109.Pester S, Smith PC. Stress fractures in the lower extremities of soldiers in basic training. Orthop Rev. 1992;21(3):297–303. [PubMed] [Google Scholar]
- 110.Wall J, Feller JF. Imaging of stress fractures in runners. Clin Sports Med. 2006;25(4):781–802. doi: 10.1016/j.csm.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 111.Sormaala MJ, Niva MH, Kiuru MJ, Mattila VM, Pihlajamaki HK. Stress injuries of the calcaneus detected with magnetic resonance imaging in military recruits. J Bone Joint Surg Am. 2006;88(10):2237–42. doi: 10.2106/JBJS.E.01447. [DOI] [PubMed] [Google Scholar]
- 112.Coughlin M, Saltzman C, Anderson RB. Mann’s Surgery of the Foot and Ankle: Elsevier Inc. 2014 [Google Scholar]