Abstract
Renal cell carcinoma (RCC) encompasses a wide spectrum of morphologically and molecularly distinct (>10) cancer subtypes originated from the kidney epithelium. Metastatic RCC (mRCC) is lethal and refractory to conventional chemotherapeutic agents. The incorporation of targeted therapies and immune checkpoint inhibitors into the current practice of mRCC has markedly improved the median overall survival of clear cell RCC (ccRCC) patients, the most common subtype, but not rare kidney cancer (RKC or non-ccRCC, nccRCC). Varied treatment response in mRCC patients is observed, which presents clinical challenges/opportunities at the modern mRCC therapeutic landscape consisting of 12 approved drugs representing 6 different effective mechanisms. Key contributing factors include inter- and intra-RCC heterogeneity. With the advances in pan-omics technologies, we now have a better understanding of the molecular pathobiology of individual RCC subtype. Here, we attempt to classify ccRCC based on contemporary molecular features with emphasis on their respective potential significance in clinical practice.
Keywords: Kidney cancer, genomics, transcriptomics, proteomics, metabolomics, therapeutics, molecular classification, biomarkers, precision medicine
INTRODUCTION
Renal cell carcinoma (RCC) is a heterogeneous group of cancers of the kidney parenchyma consisting of different subtypes with the most frequent and best studied being clear cell RCC (ccRCC, ∼75%), followed by papillary (pRCC, ∼15%), chromophobe (chRCC, ∼5%), unclassified RCC (uRCC, ∼4%) and even rarer (<1%) RCC entities such as medullary RCC (mdRCC), collecting duct RCC (cdRCC), MiT family translocation RCC (mtfRCC), and SDHB RCC (sdRCC) [1–12]. The classification of the numerous subtypes has been repeatedly revised in the past two decades, due to advances in the histological and molecular characterization of this disease [13–15]. Currently, the latest World Health Organization Classification of renal tumors from the year 2016 counts 12 recognized subtypes and several provisional entities awaiting to be fully recognized [1, 16]. Pan-RCC analysis demonstrated major genetic and molecular differences and minor similarities among major subtypes [17].
Localized RCC can potentially be treated with curative intent surgically by partial or radical removal of the involved kidney. However, 30% of the patients present with metastatic disease at time of diagnosis and further 30% will eventually develop metastases during the course of the disease [2]. The knowledge obtained from molecular characterization of ccRCC has led to the regulatory approval of 12 systemic therapeutic agents encompassing 6 different effective mechanisms [2]. Despite these marked advances, mRCC remains lethal and clinical benefit varies greatly among patients receiving the same therapeutic agents. Potential contributing factors include tumor/host heterogeneity and cancer evolution [18–21]. Facing the recent explosive growth in both molecular understandings and effective treatments of RCC [2, 22], further molecular sub-classification of RCC with emphasis on clinical association in addition to current prognostic models based on clinical parameters [23] could impact future clinical management of kidney cancer patients with either localized disease or distant metastasis. With these questions in mind, this review focuses on recent molecular analyses of ccRCC shown to influence clinical outcomes.
MOLECULAR CLASSIFICATION OF CLEAR CELL RENAL CELL CARCINOMA ACCORDING TO INDIVIDUAL OMICS
Genomic classification of ccRCC
Contemporary ccRCC genomic studies demonstrated that loss of heterozygosity (LOH) of chromosome 3p occurs at >90% and mutations/methylation of VHL, residing at 3p25, occurs at >70%/10–15%, confirming that inactivation of VHL serves as the fundamental driver event of human ccRCC [3, 24, 25]. The VHL E3 ligase complex targets hypoxia inducible factors (HIFs) for proteasome-mediated degradation. HIFs are transcription activator and upon stabilization/activation due to low oxygen stress such as tissue injury they trigger new blood vessel formation through activating vascular endothelial growth factor (VEGF) [26–28]. The pathological loss of VHL underlies the highly vascular nature of ccRCC and explains why anti-VEGF/VEGF receptor (VEGFR) drugs including bevacizumab, sorafenib, sunitinib, pazopanib, axitinib, lenvatinib, and cabozantinib constitute the most effective mainstream therapy for metastatic ccRCC patients [2]. However, most metastatic ccRCC patients eventually progressed and succumbed to their disease [22].
Despite the quintessential role of VHL loss during the cancer initiation process and its subsequent impact on therapeutics, genetic evidence from studying human VHL syndrome [29] and mouse VHL deficiency model [30] suggest the involvement of additional genetic drivers. Large efforts have been undertaken in the past >10 years to discover additional genetic and epigenetic events leading to metastatic ccRCC [31]. These efforts were made possible by the rapid progress in next-generation sequencing technologies and large-scale consortium efforts, revealing several novel gene mutations in ccRCC, including the tumor suppressor genes PBRM1 (40%), SETD2 (15%), BAP1 (15%), and KDM5C (7%), and the oncogene MTOR (5%) [3, 24, 32–35]. Of note, PBRM1, SETD2, and BAP1 reside at 3p21, and VHL at 3p25, thereby through the loss of one copy of chromosome 3p, 4 tumor suppressor genes are lost simultaneously [35]. Furthermore, KDM5C resides at X chromosome, thereby mutations on the sole wild type allele in male patients cause complete loss of function of KDM5C, which could contribute to the 2 : 1 male predominance in ccRCC [2].
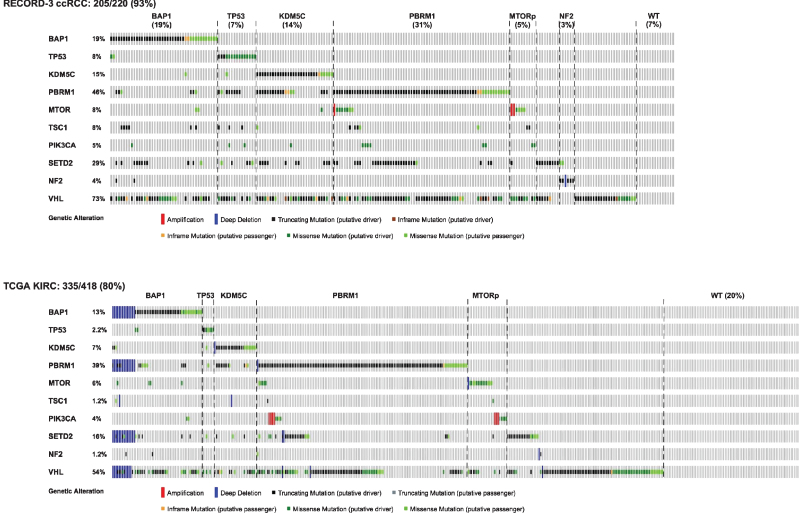
Several retrospective studies have reported interesting clinical correlation between cancer somatic gene mutations and clinical/therapeutic outcome in ccRCC, which offers insights regarding outcome-based molecular classification of ccRCC and warrants future validations. Ten genes, VHL, PBRM1, BAP1, SETD2, KDM5C, TP53, PIK3CA, MTOR, TSC1, and NF2 altogether mutated in 93% of ccRCC, are included for the discussion/classification in this review (Fig. 1). VHL inactivation is the fundamental driver event and VHL mutation occurs in >70% [24, 25, 33]. Accordingly, VHL mutation can serve as a good diagnostic tool but carries no clinical impact for ccRCC in subset analysis [2].
Fig.1.
Somatic mutation landscape of ccRCC based on 10 genes that are selected for either prevalent mutations or shown prognostic/therapeutic significances. Top panel represents 220 metastatic ccRCC patients in the reported NGS cohort of RECORD3 [25], and bottom panel represents 418 ccRCC patients of all stages in the reported TCGA KIRC cohort [3]. MTORp denotes MTORC1 pathway.
BAP1 mutations are associated with high grade, large tumors, and poor overall clinical outcome even on targeted therapy [25, 33, 36–38]. For example, progression free survival (PFS) of BAP1 mutant (MT) vs. BAP1 wild-type (WT) patients on first line sunitinib, a VEGFR TKI, was 8.1 vs. 11.0 months, and on first line everolimus, an MTORC1 inhibitor, was 4.9 vs. 10.5 months in RECORD-3 trial, one large randomized phase II study [25], suggesting that BAP1 mutant patients may not benefit from everolimus. Furthermore, BAP1 mutated mouse ccRCC tumors exhibited high grade features [39].
TP53 mutations occur at lower frequency (2.2%) in the primary tumors of non-metastatic ccRCC patients [3], at higher frequency (8%) in primaries of metastatic ccRCC [25], and at even higher frequencies (>10%) when multiple regions [40] or matched primary-metastasis pairs were sequenced (Hsieh et al. unpublished data). TP53 mutation in ccRCC associate with high grade in both human [40] and mouse [41] ccRCC tumors and significantly decreased cancer specific survival even after correction for SSIGN (stage, size, grade, and necrosis) score [42].
KDM5C mutations occurred mainly in male patients and were associated with much longer 1st line PFS (PFS1L) on sunitinib (20.6 months) than everolimus (9.8 months) whereas KDM5C wild-type patients exhibited similar PFS1L on either sunitinib (8.3 months) or everolimus (8.2 months) [25]. Enrichment of KDM5C mutation tumors in responders to anti-VEGF/VEGFR agents was also reported by independent researchers [43]. Notably, KDM5C mutations tend to co-occur with PBRM1 mutations [25], whereas both KDM5C and PBRM1 mutations tend to occur in a mutually exclusive manner with BAP1 mutations [25, 33].
PBRM1, a SWI/SNF chromatin remodeling complex protein, is the second most commonly mutated (∼40%) gene in ccRCC [2, 25, 32]. PBRM1 mutations in small renal masses (<4 cm) were associated with tumor invasiveness [34], and mice bearing mutations in VHL and PBRM1 (VHL–/–;PBRM1–/–) developed ccRCC [44]. Mechanistic and mouse genetic studies of PBRM1 further unveiled the tumor suppressor activity of PBRM1 in preventing the self-perpetuating over-amplification of HIF1 oncogenic signals [44, 45]. Of note, a long latency period for mouse kidney epithelium with deletion of both VHL and PBRM1 to develop ccRCC was observed, and the preferred third driver event for the development of ccRCC was the activation of MTORC1 [44]. Of note, PBRM1 mutant patients experienced longer PFS1L on everolimus (12.8 months) than the whole cohort receiving everolimus (8.3 months) [25]. Remarkably, data from both human cancer genomics [44] and therapeutics [25] further support a three-driver event orchestrating the step-by-step pathogenesis of ccRCC, entailing VHL loss (1st), PBRM1 loss (2nd), and MTORC1 activation (3rd).
MTOR gene mutations occur in ∼5% of ccRCC [3] that cluster at conserve domains [46] and result in enhanced MTORC1 signaling [46, 47]. MTORC1 is a key regulator of kidney cancer cell growth [44, 46, 48], functioning downstream to the PI3K activating and the TSC1/TSC2 repressing signals [49]. Accordingly, mutations in MTOR, TSC1, TSC2, and PI3K were enriched in ccRCC patients most benefited from treatment with mTORC1 inhibitors everolimus and temsirolimus [50–52]. However, several factors are important in predicting sensitivity to targeted therapy [48], e.g. mutations detected in metastasis were shown to be superior to primary in treatment prediction and should be weighed differently for precision cancer therapy [21].
SETD2 mutations in ccRCC are the best example highlighting intra-tumor heterogeneity and convergent evolution [18], i.e. through multi-region sequencing of tumors from the same patient multiple variants of SETD2 mutation were identified [40]. In fact, despite seemingly chaotic branched evolution of cancer acquiring random mutations, convergent evolution takes root during tumorigenesis and occurs at gene, pathway, function, and phenotype levels that could be exploited for therapeutic interventions [21]. Several lines of evidence indicate the importance of SETD2 mutations in ccRCC progression, especially in metastasis, thereby impacting cancer survival. Genomic analysis of the primary tumors from TCGA 421 patients and MSK 188 patients that consists patients of all stages, SETD2 mutations (11.6% TCGA, 7.4% MSK) were associated with worse cancer specific survival [37], which was later validated with a combined cohort of 1049 patients [42]. Furthermore, examination of the primary tumors of metastatic ccRCC patients demonstrated enrichment of SETD2 mutations to 30% [25]. Of note, although SETD2 mutations were associated with metastasis of ccRCC, they were not associated poor targeted treatment outcome contrasting patients with BAP1 mutations [25, 38]. Mechanistically, it was reported that SETD2 loss promotes renal cancer branched evolution through replication stress and impaired DNA repair [53]. Interestingly, SETD2 mutations also occur in other RCC types [17], and co-occur with NF2 mutations in unclassified RCC [6]. Moreover, two cases of cancer of unknown primary carry concurrent SETD2 and NF2 mutations and exhibit clear cell morphology and positivity for CA9 [54].
Altogether, mutation profiles between RECORD-3 and TCGA ccRCC cohorts are similar (Fig. 1), suggesting that ccRCC might be classified based on a specific subset of genes that carry prognostic and therapeutic significance.
Transcriptomic classification of ccRCC
In addition to the understanding of the mutational landscape of ccRCC, approaches based on the quantification of mRNA transcripts have also been developed at a high-throughput level.
ccA/ccB & ClearCode 34 transcription classification of ccRCC were initially proposed by Rose Brannon and colleagues based on gene expression microarray data [55]. They performed an unsupervised consensus clustering in a discovery cohort of 48 RCC which allowed to identify two robust subtypes ccA and ccB with differentiating biological signatures and distinct prognoses. Then, they identified a small gene set by logical analysis of data (LAD), which allowed to assign individual tumors within the ccA/ccB classification. Finally they validated it in an independent cohort of 177 patients with RCC and confirmed that ccA tumors had a markedly better prognosis than ccB. Moreover molecular subtype was found to be significantly associated with survival in both univariate and multivariate analysis. The ccA/ccB classification was subsequently validated in a meta-analysis of 480 ccRCC tumors, suggesting this profile may have value for risk stratification [56]. The gene set used to classify RCC tumors in ccA/ccB was then optimized and simplified by Brooks and colleagues using a centroid-based classification algorithm (called prediction analysis of microarray (PAM)) to end with a 34-gene expression classifier named ClearCode34 [57]. The classifier was applied to RNA-sequencing data from 380 nonmetastatic ccRCC samples from the Cancer Genome Atlas (TCGA), and to 157 formalin-fixed (FFPE) clinical samples collected at the University of North Carolina. Finally, the authors developed a recurrence risk model with the addition of stage and Fuhrman grade to the ClearCode34 sub-classification. C-index analysis showed that ClearCode34 model better predict disease-specific events compared to the University of California, Los Angeles (UCLA) Integrated Staging System (UISS) [58] and the Mayo Clinic Stage, Size, Grade, and Necrosis (SSIGN) score [59]. Moreover, this model was also additive independently of both UISS and SSIGN indicating added prognostic information for disease-specific outcomes. Thus, using ClearCode34 enhances risk stratification, which may guide future clinical planning regarding patient surveillance and adjuvant therapy. Recently de Velasco and colleagues assessed the predictive power of ClearCode34 in the setting of systemic therapy for metastatic ccRCC [60]. They found that ccB remained independently associated with a worse OS (p = 0.044) after adjusting for IMDC groups. They found also that the joint model of ccA/ccB and IMDC had higher accuracy (C-Index 0.63, 95% CI = 0.51–0.75) than a model with IMDC alone (0.60, 95% CI = 0.47–0.72).
Although ClearCode34 might be ready to be used prospectively in a clinical trial, a major limitation has emerged: the intra-tumoral heterogeneity (ITH). Regarding driver mutations and somatic copy number aberrations, Marco Gerlinger and colleagues from Charles Swanton’s group has already shown the high frequency of ITH toward intra-tumor multi-region sequencing. They also found a high ITH of the ccA/ccB signature. They reanalysed their published gene expression data of 63 tumor regions from 10 stage II–IV ccRCCs [18, 40] and mapped the results onto the phylogenetic trees previously published for these tumors [40]. Only two tumors homogeneously expressed the ccA signature; the other eight tumors were heterogeneous with ccA and ccB components detectable, suggesting the need to sample multiple tumor regions to reliably detect poor prognostic clones [61]. More recently a team from the Mayo Clinic has evaluated both intra- and inter-tumor molecular heterogeneity in a large cohort of resected metastatic ccRCC tumors [62]. The authors found that ccA or ccB subtype differed across longitudinal metastatic tumors from the same patient in 23% (7/30) of patients and across patient-matched primary and metastatic tumors in 43% (35/80) of patients. Among these 35 patients, 80% had a primary tumor that was classified as ccA and at least one metastatic tumor classified as ccB. Conversely, seven (20%) patients had a primary tumor classified as ccB and at least one metastatic tumor classified as ccA. These data suggest that molecular classification performed on primary tumor does not reflect the biology of the metastasis in a large proportion of cases.
The TCGA m1-m4 mRNA classification of ccRCC was reported by the KIRC analysis working group [3]. In this study, multi-platform analyses were performed to identify somatic alterations, DNA methylation status and mRNA/miRNA expression signatures on 446 patients. Regarding mRNA expression, an unsupervised clustering method identified four subsets (m1–m4). The m1 subtype was characterized by gene sets associated with chromatin remodeling processes and a higher frequency of PBRM1 mutations (39% in m1 vs. 27% in others, P = 0.027). Deletion of CDKN2A (53% vs. 26%; P < 0.0001) and mutations in PTEN (11% vs 1%; P < 0.0001) were more frequent in m3 tumours. The m4 group showed higher frequencies of BAP1 mutations (17% vs. 7%; P = 0.002) and base-excision repair; however, this group also harboured more mTOR mutations (12% vs. 4%; P = 0.01) and ribosomal gene sets. Supervised clustering revealed an overlap between these new subsets to the previously reported ccA and ccB expression subtypes, with cluster m1 corresponding to ccA and ccB divided between m2 and m3. Cluster m4 probably accounts for the roughly 15% of tumors previously unclassified in the ccA/ccB classification scheme. Similarly, the survival advantage previously observed for ccA cases was again identified for m1 tumours.
CC-e.1, 2, 3 classification of ccRCC was recently reported by Chen et al., reported the comprehensive molecular analysis of 894 primary renal cell carcinomas [17]. The authors identified nine subtypes defined by systematic analysis of five genomic data platforms (mRNA expression, DNA methylation, DNA copy, microRNA (miRNA) expression, and protein expression). ccRCC clustered into 3 different subtypes designated as CC-e.1, 2 and 3 associated with intermediate, better and worse patient survival. Genomic subtypes made across TCGA ccRCC cases showed high concordance with other subtype designations previously called for the same samples, on the basis of gene expression profiles. The previously reported [55] ccA and ccB clear cell RCC expression subtypes corresponded to CC-e.2 (better prognosis) and CC-e.3 (worse prognosis), respectively. Of the four mRNA-expression-based subtypes, m1/m2/m3/m4, defined previously in the original KIRC study, m1 and m3 overlapped with CC-e.2 and CC-e.3, respectively, while CC-e.1 overlapped significantly with m2 and m4. All collaborative efforts made by The Cancer Genome Atlas Research Network were dedicated to provide a comprehensive characterization of RCC and to bring some molecular insights to identify the opportunities for disease treatment. Thus, the TCGA mRNA signature has not been yet assessed in a prospective clinical trial. Indeed, mRNA expression analyses were performed on frozen tumor samples using mainly RNA sequencing which is a major limitation for its use within a clinical trial.
ccrcc1-4 classification was proposed in 2007 when the French association ”La Ligue contre le Cancer“ launched the Tumor Identity Card (”Carte d’Identité des Tumeurs“) to molecularly characterize solid tumors. Stéphane Oudard’s team together with Hervé Fridman’s team took advantage of this program to propose the characterization of molecular features of metastatic ccRCC patients. Transcriptomic analysis (microarray gene expression) of the primary tumor from 53 metastatic ccRCC patients treated with sunitinib was performed [63]. Using an unsupervised clustering analysis, 4 molecular groups (ccrcc1 to 4) were identified with distinct pathological features and mutational profiles. For example, ccrcc4 tumors had a significant higher inflammation score, a higher frequency of sarcomatoid component, a low frequency of VHL mutation and the absence of PBRM1 mutation. At the opposite ccrcc3 had the lower inflammation score and the lower frequency of sarcomatoid component but has also low frequencies of VHL and PBRM1 mutations. Importantly, the 4 groups appeared to have significantly different prognoses with ccrcc 1 and 4 having reduced progression free, overall survival and the poorer response to sunitinib, suggesting to be a good tool to predict response to TKI. A classifier of 35 genes was constructed using a step-by-step strategy with a first centroid-based predictor to assign a sample one of the three following groups ccrcc1&4/ccrcc2/ccrcc3; a second centroid-based predictor was used for samples predicted as ccrcc1&4. The classifier was tested on the 51 patients with available microarray data and using qRT-PCR and then validated on additional 47 patients with qRT-PCR only. Finally the gene set was tested in the TCGA samples. Somatic PBRM1 mutations were most frequently identified in ccrcc1/ccrcc2 tumors but rarely found in ccrcc3/ccrcc4 tumors. In both series, somatic VHL mutations were more frequently distributed in ccrcc1/ccrcc2 tumors. The BAP1 and SETD2 mutations also showed association with the molecular subtypes: BAP1 was most mutated in the ccrcc4 tumors (p = 0.0098) and SETD2 was most mutated in the ccrcc1 tumors (p = 0.06). As in the,,in-house“ dataset ccrcc2/ccrcc3 tumors display the best survival, ccrcc1 tumors an intermediate survival, and ccrcc4 tumors the poorest survival (p < 0.0001).
A 16-gene assay to predict recurrence after surgery in localized RCC was reported by Rini et al. in 2015 [64]. In this study, the expression of 732 genes was measured in 942 patients presented with Stage I-III diseases, and correlated with the risk of recurrence cancer-specific survival. Among 516 significantly altered genes, 11 genes that involve vascular, cell growth/division, immune response, and inflammation were selected along with 5 reference genes to develop the recurrence score, which was then validated in another 626 patients. In multivariable analyses, the 16-gene score was significantly associated with recurrence (p < 0.0001) after stratification by stage and adjustment for size, grade, or Leibovich score.
With the rapid development of checkpoint inhibitors in RCC, interestingly we found that some immune cell infiltrates, evaluated with mRNA expression, were associated with molecular groups [65]. For instance ccrcc4 tumors, which were associated with sunitinib resistance, were the most highly infiltrated tumors by T cells. In addition ccrcc4 had the highly expression of immunosuppressive markers such as PD-L1, PD-1, LAG-3, TIM-3, suggesting a high fraction of exhausted T cells within these tumors. Conversely, ccrcc1 tumors, which were also associated with poor prognosis, had the poorest T cell infiltration and a global low expression of T cell inhibition markers. ccrcc1 could be considered as immune-desert or immune-cold tumors.
Based on these results, a French academic and multicentric molecular-driven randomized phase 2 trial named Bionikk (phase 2 BIOmarker driven trial with Nivolumab and Ipilimumab or VEGFR TKI in naïve metastatic Kidney cancer, NCT02960906) was recently launched. Main objective is to evaluate the ability of the CIT classification to select patients to have either a TKI, or a checkpoint inhibitor alone or in combination. Primary endpoint is overall response rate within each arm. 150 patients with a metastatic ccRCC naïve of any systemic therapy with available frozen tumor are planned to be included. Molecular classification is determined within 2 weeks and patients are then randomized according to their group: ccrcc1 and 4 are randomized between nivolumab plus ipilimumab and nivolumab alone, and ccrcc2 and 3 are randomized between nivolumab plus ipilimumab and TKI (sunitinib or pazopanib). Among main secondary objectives including overall survival and progression free survival, according to treatment arm and group, many exploratory biomarkers will be evaluated. One of them is the comparison between molecular groups obtained from FFPE samples versus those obtained from frozen samples. Completion of the study is planned to be around mid 2020.
Metabolomic classification of ccRCC
mCluster 1–4 (metabolomics cluster) of ccRCC with distinct metabolic features and clinical outcomes were identified when global profiling of 877 metabolites was performed on 138 primary kidney tumor and adjacent normal pairs [66]. Worse clinical outcomes were associated with high glutathione-related metabolites observed in mCluster 2 or with high dipeptides in mCluster 3, whereas better clinical outcomes were associated with low glutathione in mCluster 4 and low dipeptide in mCluster 1, which may present therapeutic opportunity through further disrupting the redox or lysosome pathways, respectively [66]. Furthermore, grade-dependent metabolic reprogramming of ccRCC was also observed when a combined metabolomics and proteomics approach was performed [67]. The intra-tumor heterogeneity concerning ccRCC metabolism was recently reported through profiling multiple spatially separated samples [68]. In this small cohort study, global metabolomics was performed on 32 kidney tumor samples and 12 adjacent normal tissues representing 12 patients in conjunction with tissue tracer studies, demonstrating that different regions of primary RCC tumor tissues possess different metabolic characteristics and might contribute to intratumor treatment heterogeneity.
Immunogenomic profiling of ccRCC
As immune checkpoint inhibition has shown great promise in ccRCC, many efforts have been devoted to analyze tumor transcriptome and estimate the composition of the tumor microenvironment [69]. Recent methods aim at providing highly precise quantitative information about the cell content of heterogeneous samples using deconvolution techniques and has provided an immune atlas of ccRCC [70]. Furthermore, stringent and robust gene signatures for 8 immune cell types, as well as fibroblasts and vessels have recently been reported [65, 71] and used them in a method called MCP-counter, which scores are proportional to the cell amounts within the samples. As checkpoint inhibitors act primarily on immune cells, these new techniques that allow accurately quantify these cells could help us to predict response to therapy. Encouragingly, in a recently reported IMmotion150 phase II clinical trial where 305 metastatic patients were randomized to Sunitinib, Atezolimumab (anti-PD-L1), or Atezolimumab plus Bevacizumab (anti-VEGF), PD-L1+ was detected in 54% of patients, and among these patients the PFS HR form atezolimumab plus bevacizumab vs. sunitinib was 0.64 but did not reach statistical significance (p = 0.095) [72]. Notably, in a small (n = 13) cohort study, the intratumoral balance between metabolic and immunologic gene expression was shown to associate with anti-PD-1 treatment response [73].
CONCLUSION
Given the unpredictability on the efficacy of currently available drugs for treating individual metastatic kidney cancer patients, there is an unmet medical need to improve the therapeutic approach for patients affected by this disease. Although the mutational landscape of ccRCC has dramatically evolved in the past 10 years, major limitations dampen their use to select the right therapy for the right patient. First, most of mutated genes are tumor suppressor genes and mutations lead to loss of function. Consequently these mutated genes are not directly targetable. Second, several events can inactivate a gene such as methylation, copy number loss, miRNA regulation and thus may lead to a loss of function in wild type (WT) genes that would evade select DNA mutation platforms. Third, ccRCC are highly heterogeneous tumors and even early events, e.g. PBRM1 or BAP1 mutations could be different when sequencing primary vs. metastatic tumors [21]. Hence, improvement may be achieved, such as through the development and the employment of methods to perform tumor-specific molecular stratification of renal cell carcinoma, and offers the most effective treatment to the select patient based on a combination of different molecular characteristics.
Novel insights into the molecular underpinnings of renal cell carcinoma have unraveled a far more complex classification than those simply based on histopathological criteria. Recent results on gene expression and mutation analysis were able to provide new subgroups within clear cell, but also papillary and chromophobe renal cell carcinoma [2, 74, 75]. The described subgroups define not only on different clinical risk groups, but also, to a lesser extent, on predictive biomarkers for current treatments of ccRCC. Prior to the tumor omics era, serum protein profiles and IHC constituted major biomarker efforts in kidney cancer translational research [76]. Currently, we are not yet ready to benchmark classification with biomarkers. Nevertheless, it is foreseeable that a combination strategy consisting of serum analysis, gene expression analysis, and mutation analysis platforms could be developed in the future to stratify patients with either localized or metastatic RCC, which aims at defining the characteristics and prognosis of an individual tumor or metastasis in a single patient in order to provide the best possible follow-up and treatment plan.
RELEVANT DISCLOSURES
J.J.H. is a consultant for Novartis, Eisai and Chugai and received research funding from Pfizer, Novartis, Eisai and Cancer Genomics Inc. Y.A.V is a consultant for Bristol-Myers Squibb, Pfizer, Novartis, Ipsen, Sanofi, Astellas, Janssen and Roche.
ACKNOWLEDGMENTS
J.J.H. is supported by the J. Randall & Kathleen L. MacDonald Family Research Fund, the Tom and Mila Tuttle Family Research Fund, the Jill and Rafic Dahan Family Research Fund, and the Jill and Jeffrey Weiss Family Research Fund for the cure of metastatic kidney cancer.
REFERENCES
- [1]. Moch H, Cubilla AL, Humphrey PA, Reuter VE, Ulbright TM. The 2016 WHO classification of tumours of the urinary system and male genital organs-part A: Renal, penile, and testicular tumours. Eur Urol 2016;70:93–105. [DOI] [PubMed] [Google Scholar]
- [2]. Hsieh JJ, Purdue MP, Signoretti S, Swanton C, Albiges L, Schmidinger M, et al. Renal cell carcinoma. Nat Rev Dis Primers 2017;3:17009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3]. Cancer Genome Atlas Research N. Comprehensive molecular characterization of clear cell renal cell carcinoma. Nature 2013;499:43–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. Cancer Genome Atlas Research N, Linehan WM, Spellman PT, Ricketts CJ, Creighton CJ, Fei SS, et al. Comprehensive molecular characterization of papillary renal-cell carcinoma. N Engl J Med 2016;374:135–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5]. Davis CF, Ricketts CJ, Wang M, Yang L, Cherniack AD, Shen H, et al. The somatic genomic landscape of chromophobe renal cell carcinoma. Cancer Cell 2014;26:319–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Chen YB, Xu J, Skanderup AJ, Dong Y, Brannon AR, Wang L, et al. Molecular analysis of aggressive renal cell carcinoma with unclassified histology reveals distinct subsets. Nat Commun 2016;7:13131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7]. Calderaro J, Masliah-Planchon J, Richer W, Maillot L, Maille P, Mansuy L, et al. Balanced translocations disrupting SMARCB1 are hallmark recurrent genetic alterations in renal medullary carcinomas. Eur Urol 2016;69:1055–61. [DOI] [PubMed] [Google Scholar]
- [8]. Carlo MI, Chaim J, Patil S, Kemel Y, Schram AM, Woo K, et al. Genomic characterization of renal medullary carcinoma and treatment outcomes. Clin Genitourin Cancer 2017; 10.1016/j.clgc.2017.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9]. Pal SK, Choueiri TK, Wang K, Khaira D, Karam JA, Van Allen E, et al. Characterization of clinical cases of collecting duct carcinoma of the kidney assessed by comprehensive genomic profiling. Eur Urol 2016;70:516–21. [DOI] [PubMed] [Google Scholar]
- [10]. Malouf GG, Monzon FA, Couturier J, Molinie V, Escudier B, Camparo P, et al. Genomic heterogeneity of translocation renal cell carcinoma. Clin Cancer Res 2013;19:4673–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11]. Argani P. MiT family translocation renal cell carcinoma. Seminars in Diagnostic Pathology 2015;32:103–13. [DOI] [PubMed] [Google Scholar]
- [12]. Lee CH, Gundem G, Lee W, Chen YB, Cross JR, Dong Y, et al. Persistent severe hyperlactatemia and metabolic derangement in lethal SDHB-mutated metastatic kidney cancer: Clinical challenges and examples of extreme warburg effect. Precision Oncology 2017;1:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13]. Kovacs G, Akhtar M, Beckwith BJ, Bugert P, Cooper CS, Delahunt B, et al. The Heidelberg classification of renal cell tumours. The Journal of Pathology 1997;183:131–3. [DOI] [PubMed] [Google Scholar]
- [14]. Lopez-Beltran A, Scarpelli M, Montironi R, Kirkali Z. 2004 WHO classification of the renal tumors of the adults. Eur Urol 2006;49:798–805. [DOI] [PubMed] [Google Scholar]
- [15]. Srigley JR, Delahunt B, Eble JN, Egevad L, Epstein JI, Grignon D, et al. The International Society of Urological Pathology (ISUP) vancouver classification of renal neoplasia. Am J Surg Pathol 2013;37:1469–89. [DOI] [PubMed] [Google Scholar]
- [16]. Udager AM, Mehra R. Morphologic, molecular, and taxonomic evolution of renal cell carcinoma: A conceptual perspective with emphasis on updates to the 2016 world health organization classification. Archives of Pathology & Laboratory Medicine 2016;140:1026–37. [DOI] [PubMed] [Google Scholar]
- [17]. Chen FJ, Zhang YQ, Senbabaoglu Y, Ciriello G, Yang LX, Reznik E, et al. Multilevel genomics-based taxonomy of renal cell carcinoma. Cell Rep 2016;14:2476–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18]. Gerlinger M, Rowan AJ, Horswell S, Larkin J, Endesfelder D, Gronroos E, et al. Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N Engl J Med 2012;366:883–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19]. Gerlinger M, McGranahan N, Dewhurst SM, Burrell RA, Tomlinson I, Swanton C. Cancer: Evolution within a lifetime. Annu Rev Genet 2014;48:215–36. [DOI] [PubMed] [Google Scholar]
- [20]. Sankin A, Hakimi AA, Mikkilineni N, Ostrovnaya I, Silk MT, Liang YP, et al. The impact of genetic heterogeneity on biomarker development in kidney cancer assessed by multiregional sampling. Cancer Med-Us 2014;3:1485–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21]. Hsieh JJ, Manley BJ, Khan N, Gao J, Carlo MI, Cheng EH. Overcome tumor heterogeneity-imposed therapeutic barriers through convergent genomic biomarker discovery: A braided cancer river model of kidney cancer. semin cell dev biol. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22]. Choueiri TK, Motzer RJ. Systemic therapy for metastatic renal-cell carcinoma. N Engl J Med 2017;376:354–66. [DOI] [PubMed] [Google Scholar]
- [23]. Heng DY, Xie W, Regan MM, Harshman LC, Bjarnason GA, Vaishampayan UN, et al. External validation and comparison with other models of the International Metastatic Renal-Cell Carcinoma Database Consortium prognostic model: A population-based study. Lancet Oncol 2013;14:141–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24]. Sato Y, Yoshizato T, Shiraishi Y, Maekawa S, Okuno Y, Kamura T, et al. Integrated molecular analysis of clear-cell renal cell carcinoma. Nat Genet 2013;45:860–7. [DOI] [PubMed] [Google Scholar]
- [25]. Hsieh JJ, Chen D, Wang PI, Marker M, Redzematovic A, Chen YB, et al. Genomic biomarkers of a randomized trial comparing first-line everolimus and sunitinib in patients with metastatic renal cell carcinoma. Eur Urol 2017;71:405–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26]. Kaelin WG Jr. The von Hippel-Lindau tumour suppressor protein: O2 sensing and cancer. Nat Rev Cancer 2008;8:865–73. [DOI] [PubMed] [Google Scholar]
- [27]. Semenza GL. HIF-1 mediates metabolic responses to intratumoral hypoxia and oncogenic mutations. J Clin Invest 2013;123:3664–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28]. Masson N, Ratcliffe PJ. Hypoxia signaling pathways in cancer metabolism: The importance of co-selecting interconnected physiological pathways. Cancer Metab 2014;2:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29]. Fisher R, Horswell S, Rowan A, Salm MP, de Bruin EC, Gulati S, et al. Development of synchronous VHL syndrome tumors reveals contingencies and constraints to tumor evolution. Genome Biol 2014;15:433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30]. Kapitsinou PP, Haase VH. The VHL tumor suppressor and HIF: Insights from genetic studies in mice. Cell Death Differ 2008;15:650–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31]. Wei EY, Hsieh JJ. A river model to map convergent cancer evolution and guide therapy in RCC. Nat Rev Urol 2015;12:706–12. [DOI] [PubMed] [Google Scholar]
- [32]. Varela I, Tarpey P, Raine K, Huang D, Ong CK, Stephens P, et al. Exome sequencing identifies frequent mutation of the SWI/SNF complex gene PBRM1 in renal carcinoma. Nature 2011;469:539–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33]. Pena-Llopis S, Vega-Rubin-de-Celis S, Liao A, Leng N, Pavia-Jimenez A, Wang S, et al. BAP1 loss defines a new class of renal cell carcinoma. Nat Genet 2012;44:751–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34]. Hakimi AA, Chen YB, Wren J, Gonen M, Abdel-Wahab O, Heguy A, et al. Clinical and pathologic impact of select chromatin-modulating tumor suppressors in clear cell renal cell carcinoma. Eur Urol 2013;63:848–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35]. Hakimi AA, Pham CG, Hsieh JJ. A clear picture of renal cell carcinoma. Nat Genet 2013;45:849–50. [DOI] [PubMed] [Google Scholar]
- [36]. Kapur P, Pena-Llopis S, Christie A, Zhrebker L, Pavia-Jimenez A, Rathmell WK, et al. Effects on survival of BAP1 and PBRM1 mutations in sporadic clear-cell renal-cell carcinoma: A retrospective analysis with independent validation. Lancet Oncol 2013;14:159–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37]. Hakimi AA, Ostrovnaya I, Reva B, Schultz N, Chen YB, Gonen M, et al. Adverse outcomes in clear cell renal cell carcinoma with mutations of 3p21 epigenetic regulators BAP1 and SETD A report by MSKCC and the KIRC TCGA research network. Clin Cancer Res 2013;19:3259–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38]. Tennenbaum DM, Manley BJ, Zabor E, Becerra MF, Carlo MI, Casuscelli J, et al. Genomic alterations as predictors of survival among patients within a combined cohort with clear cell renal cell carcinoma undergoing cytoreductive nephrectomy. Urologic Oncology: Seminars and Original Investigations: Elsevier, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39]. Gu YF, Cohn S, Christie A, McKenzie T, Wolff NC, Do QN, et al. Modeling renal cell carcinoma in mice: Bap1 and Pbrm1 inactivation drive tumor grade. Cancer Discov 2017; 10.1158/2159-8290.CD-17-0292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40]. Gerlinger M, Horswell S, Larkin J, Rowan AJ, Salm MP, Varela I, et al. Genomic architecture and evolution of clear cell renal cell carcinomas defined by multiregion sequencing. Nat Genet 2014;46:225–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41]. Harlander S, Schonenberger D, Toussaint NC, Prummer M, Catalano A, Brandt L, et al. Combined mutation in Vhl, Trp53 and Rb1 causes clear cell renal cell carcinoma in mice. Nat Med 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42]. Manley BJ, Zabor EC, Casuscelli J, Tennenbaum DM, Redzematovic A, Becerra MF, et al. Integration of recurrent somatic mutations with clinical outcomes: A pooled analysis of 1049 patients with clear cell renal cell carcinoma. European Urology Focus 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43]. Ho TH, Choueiri TK, Wang K, Karam JA, Chalmers Z, Frampton G, et al. Correlation between molecular subclassifications of clear cell renal cell carcinoma and targeted therapy response. Eur Urol Focus 2016;2:204–9. [DOI] [PubMed] [Google Scholar]
- [44]. Nargund AM, Pham CG, Dong Y, Wang PI, Osmangeyoglu HU, Xie Y, et al. The SWI/SNF protein PBRM1 restrains VHL-loss-driven clear cell renal cell carcinoma. Cell Rep 2017;18:2893–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45]. Gao W, Li W, Xiao T, Liu XS, Kaelin WG Jr.. Inactivation of the PBRM1 tumor suppressor gene amplifies the HIF-response in VHL-/- clear cell renal carcinoma. Proc Natl Acad Sci U S A 2017;114:1027–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46]. Xu J, Pham CG, Albanese SK, Dong Y, Oyama T, Lee CH, et al. Mechanistically distinct cancer-associated mTOR activation clusters predict sensitivity to rapamycin. J Clin Invest 2016;126:3526–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47]. Grabiner BC, Nardi V, Birsoy K, Possemato R, Shen K, Sinha S, et al. A diverse array of cancer-associated MTOR mutations are hyperactivating and can predict rapamycin sensitivity. Cancer Discov 2014;4:554–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48]. Voss MH, Hsieh JJ. Therapeutic guide for mTOuRing through the braided kidney cancer genomic river. Clin Cancer Res 2016;22:2320–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49]. Saxton RA, Sabatini DM. mTOR signaling in growth, metabolism, and disease. Cell 2017;169:361–71. [DOI] [PubMed] [Google Scholar]
- [50]. Kwiatkowski DJ, Choueiri TK, Fay AP, Rini BI, Thorner AR, De Velasco G, et al. Mutations in TSC1, TSC2, and MTOR are associated with response to rapalogs in patients with metastatic Renal Cell Carcinoma. Clin Cancer Res 2016;22(10):2445–52. 10.1158/1078-0432.CCR-15-2631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51]. Voss MH, Hakimi AA, Pham CG, Brannon AR, Chen YB, Cunha LF, et al. Tumor genetic analyses of patients with metastatic renal cell carcinoma and extended benefit from mTOR inhibitor therapy. Clin Cancer Res 2014;20:1955–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52]. Lim SM, Park HS, Kim S, Kim S, Ali SM, Greenbowe JR, et al. Next-generation sequencing reveals somatic mutations that confer exceptional response to everolimus. Oncotarget 2016;7:10547–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53]. Kanu N, Gronroos E, Martinez P, Burrell RA, Yi Goh X, Bartkova J, et al. SETD2 loss-of-function promotes renal cancer branched evolution through replication stress and impaired DNA repair. Oncogene 2015;34:5699–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54]. Wei EY, Chen YB, Hsieh JJ. Genomic characterisation of two cancers of unknown primary cases supports a kidney cancer origin. BMJ Case Rep 2015;2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55]. Brannon AR, Reddy A, Seiler M, Arreola A, Moore DT, Pruthi RS, et al. Molecular stratification of clear cell renal cell carcinoma by consensus clustering reveals distinct subtypes and survival patterns. Genes & Cancer 2010;1:152–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56]. Brannon AR, Haake SM, Hacker KE, Pruthi RS, Wallen EM, Nielsen ME, et al. Meta-analysis of clear cell renal cell carcinoma gene expression defines a variant subgroup and identifies gender influences on tumor biology. Eur Urol 2012;61:258–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57]. Brooks SA, Brannon AR, Parker JS, Fisher JC, Sen O, Kattan MW, et al. ClearCode A prognostic risk predictor for localized clear cell renal cell carcinoma. Eur Urol 2014;66:77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58]. Zisman A, Pantuck AJ, Wieder J, Chao DH, Dorey F, Said JW, et al. Risk group assessment and clinical outcome algorithm to predict the natural history of patients with surgically resected renal cell carcinoma. J Clin Oncol 2002;20:4559–66. [DOI] [PubMed] [Google Scholar]
- [59]. Zigeuner R, Hutterer G, Chromecki T, Imamovic A, Kampel-Kettner K, Rehak P, et al. External validation of the Mayo Clinic stage, size, grade, and necrosis (SSIGN) score for clear-cell renal cell carcinoma in a single European centre applying routine pathology. Eur Urol 2010;57:102–9. [DOI] [PubMed] [Google Scholar]
- [60]. de Velasco G, Culhane AC, Fay AP, Ari Hakimi A, Voss MH, Tannir NM, et al. Molecular subtypes improve prognostic value of international metastatic renal cell carcinoma database consortium prognostic model. Oncologist 2017;22:286–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61]. Gulati S, Martinez P, Joshi T, Birkbak NJ, Santos CR, Rowan AJ, et al. Systematic evaluation of the prognostic impact and intratumour heterogeneity of clear cell renal cell carcinoma biomarkers. Eur Urol 2014;66:936–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62]. Serie DJ, Joseph RW, Cheville JC, Ho TH, Parasramka M, Hilton T, et al. Clear cell type A and B molecular subtypes in metastatic clear cell renal cell carcinoma: Tumor heterogeneity and aggressiveness. Eur Urol 2017;71:979–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63]. Beuselinck B, Job S, Becht E, Karadimou A, Verkarre V, Couchy G, et al. Molecular subtypes of clear cell renal cell carcinoma are associated with sunitinib response in the metastatic setting. Clin Cancer Res 2015;21:1329–39. [DOI] [PubMed] [Google Scholar]
- [64]. Rini B, Goddard A, Knezevic D, Maddala T, Zhou M, Aydin H, et al. A 16-gene assay to predict recurrence after surgery in localised renal cell carcinoma: Development and validation studies. Lancet Oncol 2015;16:676–85. [DOI] [PubMed] [Google Scholar]
- [65]. Becht E, Giraldo NA, Lacroix L, Buttard B, Elarouci N, Petitprez F, et al. Estimating the population abundance of tissue-infiltrating immune and stromal cell populations using gene expression. Genome Biol 2016;17:218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66]. Hakimi AA, Reznik E, Lee CH, Creighton CJ, Brannon AR, Luna A, et al. An integrated metabolic atlas of clear cell renal cell carcinoma. Cancer Cell 2016;29:104–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67]. Wettersten HI, Hakimi AA, Morin D, Bianchi C, Johnstone ME, Donohoe DR, et al. Grade-dependent metabolic reprogramming in kidney cancer revealed by combined proteomics and metabolomics analysis. Cancer Res 2015;75:2541–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68]. Okegawa T, Morimoto M, Nishizawa S, Kitazawa S, Honda K, Araki H, et al. Intratumor heterogeneity in primary kidney cancer revealed by metabolic profiling of multiple spatially separated samples within tumors. EBioMedicine 2017;19:31–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69]. Senbabaoglu Y, Gejman RS, Winer AG, Liu M, Van Allen EM, de Velasco G, et al. Tumor immune microenvironment characterization in clear cell renal cell carcinoma identifies prognostic and immunotherapeutically relevant messenger RNA signatures. Genome Biol 2016;17:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70]. Chevrier S, Levine JH, Zanotelli VRT, Silina K, Schulz D, Bacac M, et al. An immune atlas of clear cell renal cell carcinoma. Cell 2017;169:736-49 e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71]. Becht E, Giraldo NA, Beuselinck B, Job S, Marisa L, Vano Y, et al. Prognostic and theranostic impact of molecular subtypes and immune classifications in renal cell cancer (RCC) and colorectal cancer (CRC). Oncoimmunology 2015;4:e1049804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72]. Atkins MB, McDermott DF, Powles T, Motzer RJ, Rini BI, Fong L, et al. IMmotion150: A phase II trial in untreated metastatic renal cell carcinoma (mRCC) patients (pts) of atezolizumab (atezo) and bevacizumab (bev) vs and following atezo or sunitinib (sun). American Society of Clinical Oncology 2017. [Google Scholar]
- [73]. Ascierto ML, McMiller TL, Berger AE, Danilova L, Anders RA, Netto GJ, et al. The intratumoral balance between metabolic and immunologic gene expression is associated with anti-PD-1 response in patients with renal cell carcinoma. Cancer Immunol Res 2016;4:726–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74]. Joshi S, Tolkunov D, Aviv H, Hakimi AA, Yao M, Hsieh JJ, et al. The genomic landscape of renal oncocytoma identifies a metabolic barrier to tumorigenesis. Cell Rep 2015;13:1895–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75]. Casuscelli J, Weinhold N, Gundem G, Wang L, Zabor EC, Drill E, et al. Genomic landscape and evolution of metastatic chromophobe renal cell carcinoma. JCI insight 2017;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76]. Funakoshi T, Lee CH, Hsieh JJ. A systematic review of predictive and prognostic biomarkers for VEGF-targeted therapy in renal cell carcinoma. Cancer Treat Rev 2014;40:533–47. [DOI] [PubMed] [Google Scholar]