Abstract
We report seven cases of successful treatment of acute migraine symptoms using beta blocker eye drops. The literature on beta blockers for acute migraine is reviewed. Oral beta blocker medication is not effective for acute migraine treatment. This is likely due to a relatively slow rate of achieving therapeutic plasma levels when taken orally. Topical beta blocker eye drops achieve therapeutic plasma levels within minutes of ocular administration which may explain their apparent effectiveness in relief of acute migraine symptoms.
Introduction
Sporadic case reports have suggested that beta blocker eye drops are effective for acute migraine treatment and chronic prevention of migraine attacks1–5 (See Table 1 and Figure 1). Although widely prescribed for glaucoma therapy, beta blocker eye drops are rarely used for acute or chronic migraine treatment. Recent comprehensive reviews on migraine therapy do not mention the potential therapeutic value of beta-blocker eye drops.6, 7, 8, 9
Table 1.
Topical Beta-blockers Commonly Used for Glaucoma Treatment
| Generic Name | Trade Name | Receptors | Concentration | Dose | Clinical Pearl |
|---|---|---|---|---|---|
| Timolol | Timoptic® | Beta 1 and 2 | 0.25%, 0.50% | BID | Former gold standard |
| Timolol | Timpotic XE® | Beta 1 and 2 | 0.25%, 0.50% | QD | XE is gel form |
| Timolol | Betimol® | Beta 1 and 2 | 0.25%, 0.50% | BID | Hemihydrate |
| Betaxolol | Betoptic® | Beta 1 | 0.50% | BID | Betaxon (newer) |
| Betaxolol | Betoptic S® | Beta 1 | 0.25% (susp) | BID | More selective |
| Levobunolol | Betagan® | Beta 1 and 2 | 0.25%, 0.50% | BID or QD | Longest half-life |
| Meti-pranolol | Optipranolol® | Beta 1 and 2 | 0.30% | BID | Rare uveitis risk |
| Carteolol | Ocupress® | Beta 1 and 2 | 1.0% | BID | Intrinsic sympathomimetic activity |
Figure 1.

Beta blocker eye drops are inexpensive, available worldwide, and have rapid trans-mucosal systemic absorption when taken topically. Sporadic case reports and the literature collectively 1–12 suggest that the success of beta blocker eye drops in treating acute migraine may be due to the rapidity of eye drops in achieving effective blood levels when instilled shortly after symptom onset.
Oral beta blocker medications are commonly and successfully used for chronic migraine prophylaxis.7, 8,9 However, beta blocker medications taken orally are not effective in treating acute migraine.10, 11 Topically applied beta blocker eye drops are systemically absorbed by the nasal mucosa and therapeutic plasma levels are achieved within minutes.4, 12, 13
In this paper we report seven cases which describe the successful use of beta blocker eye drops to abort or attenuate acute migraine symptoms. The scant published literature on using beta blocker eye drops to treat migraine is reviewed.1–5 We present an explanation of why beta blocker medication by topical eye drop, but not by oral administration, may be effective for acute migraine treatment.
Case Presentations
Case 1
CH is a 61-year-old female who has suffered from migraines for approximately 30 years. Her typical migraine is a throbbing, right-sided pain that radiates to her neck and shoulders, occasionally associated with nausea, and a preceding visual aura. Her headache will last one to two days if not treated. Previous trials of oral medications, the names of which she does not remember, did not give her sufficient relief, so she stopped using them. Approximately 15 years ago she began using at onset of acute migraine levobunolol 0.5% ophthalmic solution one drop in each eye along with ibuprofen 600 to 800 mg orally. She rates her headache relief as a 10 on a scale of 1 (no relief) to 10 (complete relief) since she started using topical beta blocker eye drops. She has had no side effects from the drops and only uses them for acute attacks.
Case 2
MM is a 66-year-old female who describes the onset of her migraines as throbbing, one-sided, pain sometimes lasting for up to three days. Nausea and sensitivity to light, sounds and smells are often associated with her headaches. Her symptoms began 32 years ago and for the past eight years she has used prophylactic topiramate 50 mg bid and nadolol 40 mg at bedtime. Approximately one year ago she began using topical timolol 0.5% ophthalmic solution one drop in each eye at the onset of her attack. Within 15 to 30 minutes she gets complete relief (10 on a scale of 1–10) of her symptoms. Occasionally, she will take Fioricet® with codeine along with her eye drops; most of the time does not. She has experienced no side effects from the drops and only uses them for an acute attack. She feels that the management of her migraines has been greatly improved with the addition of topical beta blocker eye drops.
Case 3
DW is 38-year-old female who first noticed the onset of her migraines about 25 years ago. She describes an acute attack as a constant pain that begins in her right temple and then radiates to a throbbing vein in her left temple. Associated symptoms include nausea, vomiting, blurred vision, light and noise sensitivity, diaphoresis, and confused mentation. Duration of attacks without treatment is 24 hours or more. She has tried several different oral drugs for the past 14 years and they would take several hours before she had any relief of symptoms. Most of the time she tries to fall asleep. Two years ago she began using topical timolol 0.25% ophthalmic solution one drop in each eye at the onset of a migraine. She noticed some slight shortness of breath and now only uses one drop in one eye and has no side effects. Symptom relief begins in about 10 to 20 minutes and she rates her relief as an 8 on a scale of 1 – 10. Although her symptoms are not completely relieved with one drop, she is at least able to function. If a migraine is particularly severe, she will take oral analgesic medications after instilling an eye drop.
Case 4
EM is a 61-year-old female who describes the onset of her migraines as a visual aura with a classic fortification scotoma that begins with blurred central vision then expands towards the periphery until her central vision clears. This is followed by a one-sided, constant headache associated with nausea, light and sound sensitivity, and pain behind her eyes. Untreated duration of these attacks is 24 hours or more. Prior to using eye drops, oral ibuprofen would give partial relief in about 30 to 60 minutes. Often, she would go to bed and try to fall asleep. About five years ago she began using topical timolol 0.5% ophthalmic solution one drop in each eye at the first onset of a visual aura. Within two minutes she rates her relief of symptoms as 9.5 on a scale of 1 – 10. If she does not instill the drops at the very first visual symptom, relief may take longer, but usually within 10 to 20 minutes. She continues to take ibuprofen along with her topical beta blocker eye drops and has had no systemic or ocular symptoms from the eye drops. She only uses the drops for an acute attack and does not use them prophylactically.
Case 5
JW is a 63-year-old female who had the onset of migraines 27 years ago. She describes a sudden, left-sided, pounding and throbbing temple pain that radiates into her left ear and jaw. Associated nausea, vomiting, and sound sensitivity will occasionally occur. She had previously tried many different oral medications and alternative treatments for her migraines including acupuncture, chiropractic manipulation, various diets, and a nasal-palatine block. Oral medications would take up to 60 minutes to obtain partial or complete relief of symptoms. She is currently taking duloxetine and topiramate for migraine prophylaxis which has reduced the frequency of her attacks. Approximately six years ago she began using topical levobunolol 0.5% ophthalmic solution two drops in each eye at the first onset of symptoms. She will repeat the drops in 15 minutes if she doesn’t get meaningful relief after the first set. She gets complete relief of symptoms in about 70 – 80 % of acute migraine attacks with levobunolol eye drops alone. If she obtained no relief, she would use oral medication. She tried using daily, topical levobunolol prophylactically, but it did not eliminate her attacks, so daily use was discontinued. No systemic or ocular side effects have been noted with topical beta blocker use.
Case 6
VB is a 57-year-old female with onset of frequent migraines at age five. She describes sparkling light aura lasting 10–20 minutes followed by severe right-sided pain above the eye, radiating into the temple and head. She had photophobia, nausea and difficulty with thinking clearly. The migraine would often last four to six hours followed by a “migraine hang-over” lasting a day or two. She treated these with Excedrin and lying quietly in a dark room. In her mid 30s she began using timolol 0.5% ophthalmic solution one or two drops sublingually at the first onset of her aura. She experienced improvement of her symptoms in about 10 minutes with complete relief in 30 to 45 minutes. Although she has asthma, she experienced no breathing problems or other side effects. She used the beta blocker eye drops till her mid to late 40s when she ceased to have further migraines.
Case 7
SW is a 76-year-old female whose migraines began in high school. Her typical attack begins with a visual aura of a “broken glass/mirror” followed by a left temporal pain that increases in intensity and radiates to both sides of her head. Nausea, vomiting, garbled speech, and post-migraine fatigue are often associated with her headaches. Symptoms would typically last from 24 to 72 hours. She began using topical timolol 0.5%, one drop in each eye, approximately five years ago. If she instills the drops within a few minutes from the onset of an aura, her symptom relief is immediate and complete. If there is a delay in eye drop instillation, she rates her relief as an 8 on a scale of 1 – 10. She does not take any oral medications along with her drops and she has not had any side effects.
Discussion
The literature on using beta blocker eye drops to treat migraine is sparse. A 1980 report stated that topical timolol 0.5% relieved symptoms of Horton cluster headaches compared with placebo in four patients.1 In 1999, a 59-year-old female with migraine and glaucoma had no improvement in migraine over 10 years on timolol drops although it controlled her glaucoma. She had a dramatic improvement of her migraines when carteolol beta blocker eye drops were substituted for timolol for better glaucoma control.2 In 2000, a 4-year-old girl with ophthalmoplegic migraine was treated successfully with 0.25% timolol maleate bid.3 A 64-year-old woman with classic migraine resistant to standard oral therapy was started on timolol maleate 0.5% eye drops to both eyes. She had been migraine free for 18 years when the case was reported in 2004.4 Lastly, a 52-year-old male with “normal tension glaucoma” and migraines had relief from his headaches when placed on Timoptol-LA once per day for glaucoma therapy.5
Physicians often consider migraine prophylaxis when three or more attacks occur per month. Other indications include intolerable migrainous side effects that may constitute a danger to the patient or unsuccessful acute migraine therapy.6, 7 Two of the four FDA approved oral drugs for migraine prophylaxis are beta blockers (timolol and propranolol).7 The non-beta blockers are topiramate and divalproex.7 Three other beta blockers are often used ‘off label’ (atenolol, metroprolol and nadalol) for chronic migraine prevention. Neurologists and general practitioners preferentially used oral beta blockers for migraine prophylaxis in a European study.8 However, two double-blind, and placebo controlled studies have shown that oral propranolol has no significant effect in aborting acute attacks of migraine when compared with placebo.10, 11
Timolol ophthalmic solution was the first topical beta blocker approved by the FDA for the treatment of glaucoma in 1978.9 It is a highly effective glaucoma medication with few ocular side effects and was for years the first line treatment for glaucoma world-wide. Several other ophthalmic beta blocking eye drops were subsequently approved. All of them have been used extensively (See Table 1). Beta blocker eye drops achieve pharmacologically active concentrations in the plasma.4 Ophthalmic beta blocker solutions applied topically to the eye are rapidly absorbed into the systemic circulation primarily by lacrimal duct transit into nasopharyngeal mucosa and, to a lesser extent, the conjunctival epithelium and the gastro-intestinal tract.12 Pharmacokinetic analysis has shown that one drop of timolol ophthalmic solution 0.5% in each eye will reach a plasma concentration of 2 ng/ml within 10–15 minutes.10 Beta 1 and beta 2 receptor blockade has been calculated to be approximately 80% with this plasma concentration.10 Our case reports support these observations with acute migraine symptom relief within minutes of beta blocker eye drop instillation especially if the drops are instilled as soon as possible after symptom onset.
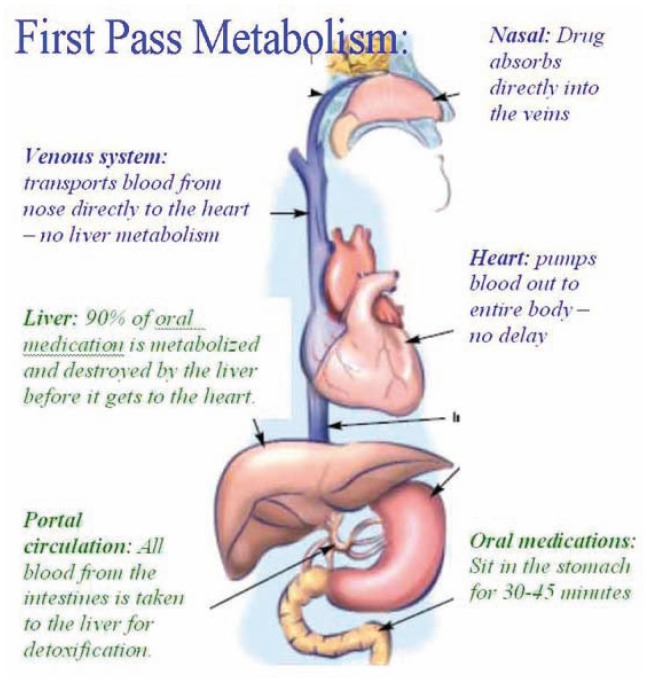
Our cases and the literature collectively1–12 suggest that the success of beta blocker eye drops in treating acute migraine may be due to the rapidity of eye drops in achieving effective blood levels. Oral beta blocker medication is subject to the “one pass effect,”16 i.e. inactivation of alimentary beta blocker by bacterial, gut and gut wall enzymes and hepatic metabolism (See Figure 2). In chronic migraine therapy, daily oral beta blocker medication attains effective blood levels for migraine prevention within hours to days. This would also explain the effectiveness of oral beta blockers on chronic migraine prevention.
Figure 2.
The success of beta blocker eye drops in treating acute migraine may be due to the rapidity of eye drops in achieving effective blood levels. Eye drops pass directly into circulation. Therapeutic blood levels occur in 4–10 minutes. Oral beta blocker medication is subject to first pass metabolism and takes several hours to reach therapeutic blood levels.
Source: http://intranasal.net
Beta Blocker Eye Drops Therapy for Acute Migraine
A migraine patient reported to one of the authors (CVM) that instilling a drop of beta blocker eye drop at the earliest onset of her aura aborted the migraine attack. Subsequently other acute migraine patients have been successfully treated with beta blocker eye drops taken as early as possible at migraine symptom onset. Seven of them filled out a questionnaire which is used as the basis for these case reports. The others did not complete the form or could not be specifically identified. Table 2 summarizes our case reports described in detail above.
Table 2.
Case Summaries
| Case | Typical Symptoms | Duration | Concurrent oral meds | Eye drops | Rated symptom relief with eye drops (1–10) | Side effects |
|---|---|---|---|---|---|---|
| 61 y/o female | Visual aura, right sided pain, nausea | 1 – 2 days | Ibuprofen | Levobunolol 0.5% both eyes | 10 | none |
| 66 y/o female | Unilateral headache, light, sound, and smell sensitivity | 1 – 3 days | Topiramate and nadolol daily | Timolol 0.5% both eyes | 10 | none |
| 38 y/o female | Right-sided headache, nausea, vomiting, light and sound sensitivity, confused mentation | 24 hrs or more | Occasional analgesics | Timolol 0.25% one eye | 8 | Shortness of breath if drops in both eyes |
| 61 y/o female | Visual aura, unilateral headache, nausea, light and sound sensitivity | 24 hrs or more | Ibuprofen | Timolol 0.5% both eyes | 9.5 | none |
| 63 y/o female | Unilateral headache, nausea, vomiting, sound sensitivity | Unknown | Duloxetine, topiramate | Levobunolol 0.5% both eyes | 8 – 10 | none |
| 57 y/o female | Visual aura, unilateral headache, nausea, photophobia, confused mentation | 4 – 6 hrs or more | none | Timolol 0.5% one or two drops sublingual | 10 | none |
| 76 yo female | Visual aura, unilateral radiating headache, nausea, vomiting, garbled speech | 24 – 72 hrs | None | Timolol 0.5% both eyes | 10 | none |
Patients undergo a medical history and ophthalmic examination prior to advising this method of treatment to ensure that they do not have contra-indications to beta blocker use.14, 15 As in glaucoma patients, the potential pulmonary and cardiovascular side-effects are discussed especially slowing of the pulse, wheezing and/or difficulty breathing. Patients are told that the eye drops are typically used in glaucoma patients and have been helpful in some patients who suffer from acute migraine attacks. They are advised to read the package insert and call if they have any questions or if symptoms develop. Treated patients have had an established, usually longstanding, diagnosis of migraine. Their physicians are informed of their acute migraine beta blocker eye drop use. New cases with symptoms suggestive of migraine are referred to their physicians for appropriate work-up to confirm the diagnosis.
Migraine patients typically put one drop of timolol ophthalmic solution 0.5% or a comparable beta blocker in each eye as early as possible in the aura or migraine evolution. Patients are advised to blink vigorously several times which encourages drop passage into the lacrimal drainage duct for enhanced systemic absorption. If no relief or partial relief of migraine symptoms occurs after 10 minutes, patients are instructed to instill another drop in each eye. If the drops do not work at this point, they are discontinued and other acute migraine medications previously prescribed by their physicians are utilized.
All of our reported cases had a complete eye examination by an ophthalmologist before therapy was started. Ideally before starting beta blocker eye drop therapy physicians should refer their patients to an ophthalmologist for a comprehensive eye examination. It is important to exclude glaucoma, lacrimal stenosis, punctal occlusion or external ocular disease.
Conclusion
Beta blocker eye drops (See Figure 1) are inexpensive, available worldwide, and have rapid trans-mucosal systemic absorption when taken topically. Used acutely at the start of a migraine, they would be expected to cause fewer side effects than oral beta blockers and other potent prescription migraine medication. If beta blocker eye drops are effective against acute migraine symptoms, this would be a welcome addition to migraine therapy.
As with this paper, all previous publications describing the beneficial effects of beta blocker eye drops for the treatment of migraine headaches are small case reports. No controlled, prospective or retrospective study has been done on acute migraine treatment by beta blocker eye drops; such a study was first called for in 1999.2 A prospective, masked, placebo controlled study, perhaps with a cross-over design, is both feasible and warranted.
Acknowledgment
We wish to thank Charles M. Lederer, MD, for review and useful suggestions and Evelyn Vail, medical librarian for her help with the literature search.
Biography
Carl V. Migliazzo, MD, (left) is a Kansas City ophthalmologist specializing in glaucoma treatment. John C. Hagan, III, MD, MSMA member since 1977, is a Kansas City ophthalmologist.
Contact: carl@migliazzo.com and jhagan@bizkc.rr.com


Footnotes
Disclosure
None reported.
References
- 1.Prusinsky A. Possibility of timolol use for immediate alleviation of Horton’s cluster headache. Preliminary report. Neurologia I Neurochirurgia Polska. 1980;14(2):191–193. [PubMed] [Google Scholar]
- 2.Shapiro MK, Gorn R. The possible treatment of migraine with carteolol hydrochloride. Headache. 1999;(2):138–139. [PubMed] [Google Scholar]
- 3.Ishikawa H, Yoshihara M, Mizuki K, Kashima Y. A pediatric case of ophthalmoplegic migraine with recurrent oculomotor nerve palsy. Jpn J Ophthalmol. 2000;44(5):576. doi: 10.1016/s0021-5155(00)00233-1. [DOI] [PubMed] [Google Scholar]
- 4.Bhagey J, James B. Topical timolol prevented migraine attacks. Eye. 2004;18(7):751. doi: 10.1038/sj.eye.6701303. [DOI] [PubMed] [Google Scholar]
- 5.Chiam PJT. Topical beta blocker treatment for migraine. Int Ophthalmol. 2012;32:85–88. doi: 10.1007/s10792-012-9516-6. [DOI] [PubMed] [Google Scholar]
- 6.Diener HCh. Pharmacological approaches to migraine. J Neural Transm Suppl. 2003;(64):35–63. doi: 10.1007/978-3-7091-6020-6_3. [DOI] [PubMed] [Google Scholar]
- 7.Shamliyan TA, Kane RL, Taylor FR. Migraine in adults: Preventive pharmacologic treatments. Agency for Healthcare Research and Quality (US); 2013. Apr, Report No.: 13-EHC068-EF http://www.ncbi.nlm.nih.gov/pubmed/23700633. [PubMed] [Google Scholar]
- 8.Rahimtoola H, Buurma H, Tijssen CC, Leufkens HG, Egberts AC. Incidence and determanents of migraine prophylactic medication in the Netherlands. Eur J Clin Pharmacol. 2002;58(2):149–55. doi: 10.1007/s00228-002-0443-8. [DOI] [PubMed] [Google Scholar]
- 9.Zimmerman TJ, Kaufman HD. Timolol. A Beta-adrenergic blocking agent for the treatment of glaucoma. Arch Ophthalmol. 1977;95(4):601–604. doi: 10.1001/archopht.1977.04450040067008. [DOI] [PubMed] [Google Scholar]
- 10.Banerjee M, Findley L. Propranolol in the treatment of acute migraine attacks. Cephalalgia. 1991 Sep;11(4):193–196. doi: 10.1046/j.1468-2982.1991.1104193.x. [DOI] [PubMed] [Google Scholar]
- 11.Fuller GN, Guiloff RJ. Propranolol in acute migraine: a controlled study. Cephalalgia. 1990 Oct;10(5):229–233. doi: 10.1046/j.1468-2982.1990.1005229.x. [DOI] [PubMed] [Google Scholar]
- 12.Nieminen T, Lehtimaki T, Maenpaa J, Ropo A, Uusitalo H, Kahonen Ophthalmic timolol: Plasma concentration and systemic cardiopulmonary effects. Scand j Clin Lab Invest. 2007;67:237–245. doi: 10.1080/00365510601034736. [DOI] [PubMed] [Google Scholar]
- 13.Yoshiyuki O, Yasuhiko Y, Miyuki N, Makoto A, Risa T. Pharmacokinectic and Pharmacodynamic Analysis of Systemic Effect of Topically Applied Timolol Maleate Ophthalmic Gelling Vehicle. Curr Eye Res. 2005;30:319–328. doi: 10.1080/02713680590923294. [DOI] [PubMed] [Google Scholar]
- 14.http://www.nlm.nih.gov/medlineplus/druginfo/meds/a682043.html#precautions
- 15.http://eurheartjsupp.oxfordjournals.org/content/11/suppl_A/A21.full
- 16.Pond SM, Tozer TN. First-pass elimination. Basic concepts and clinical consequences. Clin Pharmacokinet. 1984;1:1–25. doi: 10.2165/00003088-198409010-00001. [DOI] [PubMed] [Google Scholar]