Fallible Logic: ‘Some Exercise is Good, More Must Be Better’
Aerobic exercise and fitness has been generally viewed in a positive light among the lay public and health care providers for decades.1 The impressive and consistent reductions in cardiovascular (CV) mortality among those fit compared to sedentary individuals has lead to many conclusions which now appear to be challenged with recent studies.2 The previous chain of logic was that if CV morbidity and mortality is reduced among those with higher physical activity (PA) and exercise training (ET) and who are more fit (See Table 1),3 then there must be a reduction in atherosclerosis in terms of presence or absence or potentially a reduction in the general plaque burden. Furthermore, if some exercise is good, then more should be better. Thus, marathoners, among all recreational athletes, should be most free of atherosclerosis. The report by Schwartz and colleagues4 in this issue of Missouri Medicine is a sobering reminder that all forms of deduction or chains of logic in clinical medicine should be challenged with scientific investigation.
Table 1.
Potential Benefits of Physical Activity and Exercise Training
Improvements in Exercise Capacity
|
Improvements in Lipids
|
Reduction in Obesity Indices
|
Improvements in Blood Rheology
|
Improvement in Psychosocial Factors
|
Major Morbidity and Mortality
|
Among those with considerable experience as marathoners (25 or more races completed), the cases in this study undoubtedly had many years of endurance training and cumulatively logged distances traveled that could be 100-fold greater than average sedentary individuals. Thus, the summative physiological environment of the marathoners was no doubt extremely different than the control group of sedentary individuals. As the authors pointed out, exercise is a transient oxidative stress on the systemic vasculature, creates greater shear stress in the coronary arteries, and is associated with a variety of additional adverse effects which are short-term, provided the aerobic activity is brief. 4 The important point is that marathoners have sustained increases in aerobic activity and cardiac demand for hours at a time. Therefore, the biologic plausibility for these factors to promote atherosclerosis is tenable, despite improved risk factor profiles, and this thread of concern has been evident in the literature for several decades.5 It is important that CV risk factors were developed as associated variables for binary events of nonfatal myocardial infarction (MI) or CV death, not for the presence or absence of atherosclerosis.6 Thus, despite the healthier CV risk profiles on the surface, the burden of atherosclerosis and potentially worrisome noncalcified plaques which could be more susceptible to rupture and result in MI is a reality that must be understood among adult marathoners and their physicians.7
Sudden Cardiac Death
Besides potential detrimental changes in the coronary arteries, there are several other forms of cardiotoxicity associated with marathon running or extreme endurance exercise (EEE).2, 8–10 Perhaps the most serious is sudden cardiac death (SCD). Although episodes of SCD often generate considerable publicity in major running road races or other long distance endurance events, SCD remains relatively uncommon.
A recent study reviewed all marathons and half-marathons in the United States from 2000 – 2010 (10.9 million runners; 59 cardiac arrests) and reported that SCD occurred in only 0.54/100,000 participants.11 Although other studies suggest that the true occurrence may be two-to four-fold higher than this,12,13 due to the fact that the Kim et al.11 data may be contaminated by large numbers of half marathoners and only accounts for SCD during the race itself and not soon afterwards, still the fatality in marathons is relatively uncommon, but still “too high.” The fatality rate of triathlons is approximately two-fold higher than that of marathons, but largely because of increased CV events and SCD during the swim portion of the race.14 The high catecholamine state of competition superimposed on forms of either preexisting training-induced structural myocardial abnormalities is the most tractable explanation for cases of SCD after common causes such as hypertrophic cardiomyopathy, coronary artery disease, anomalous coronary arteries, channelopathies, and other etiologies are excluded.
Adverse Effects of Cardiac Structure and Function
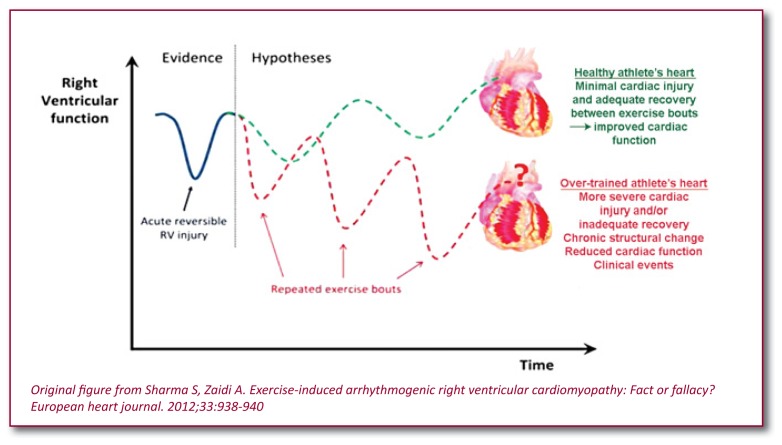
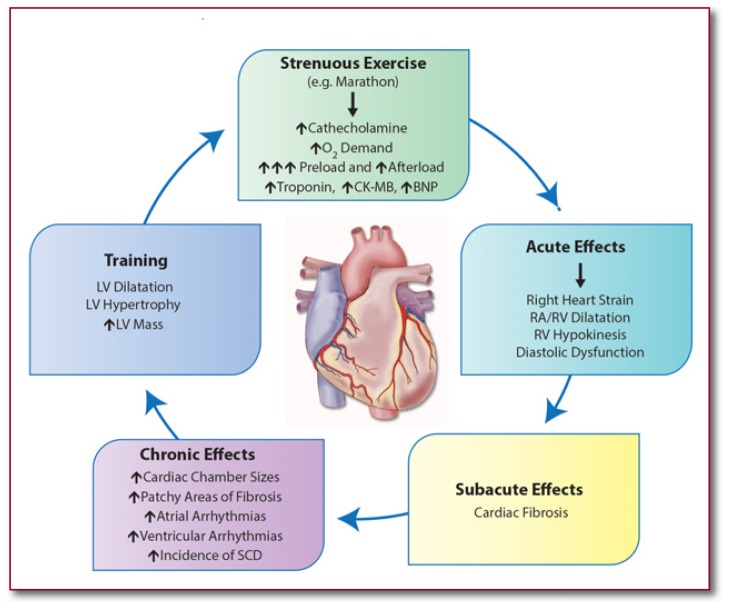
Besides potential adverse effects on CAD discussed above, EEE has potential adverse effects on cardiac structure and function (See Figures 1 and 2).2,8–10 In fact, animal studies have suggested considerable potential cardiotoxicity of EEE.15,16 In one recent study, rats were trained to run strenuously for 60 consecutive minutes daily for 16 weeks.16 Compared with control rats, the exercise rats developed left ventricular (LV) hypertrophy, right ventricular (RV) hypertrophy, diastolic dysfunction, and dilation of both atria, as well as collagen deposition in the cardiac chambers. Ventricular tachyarrhythmias were inducible in 42% of the running rats compared with only 6% of the controls (p=0.05). After de-training, the adverse changes and elevated electrical irritability largely reversed.16
Figure 1.
Potential impact of repeated bouts of ultra-endurance exercise on right ventricular structure and function. Reproduced from Patil et al.10
Figure 2.
Proposed pathogenesis of endurance athlete’s cardiomyopathy. RA=Right atrium, RV= Right ventricle, LV= Left ventricle, SCD= Sudden Cardiac Death. Reproduced from Patil et al. 10
Similarly, adverse structural remodeling following EEE has been noted in humans.2,8–10 For example, following a marathon, studies have demonstrated that almost 30% of runners develop acute dilation of cardiac structures, especially the RV and right atrium, and dysfunction of both the LV (at least in the ventricular septum) and, especially, the RV.2,8–10,17,18 Serologic markers of cardiac damage, including cardiac troponin and creatinine kinase myocardial band, two enzymes released in acute MI and used to diagnose MI, and B-type natriuretic peptide (or BNP), which is used to monitor patients for heart failure, are elevated in close to 30% and up to 50% of participants during a marathon.2,8–10,17,19–22 Although these abnormalities typically reverse within days of an acute bout of EEE, concern has been expressed that repeated episodes may lead to myocardial cell damage at sites of myocyte slippage of one cell above another due to loss of integrity of desmosome connections, and chronic multiple injuries may lead to stimulation of resident fibroblasts to produce extracellular collagen resulting in patches of fibrosis, the substrate for anisotropy and lethal arrhythmias. The predisposing genetic substrate, dose, and duration of endurance training and competition are all unknown, but based on the totality of evidence, we believe that high levels of EEE may predispose some individuals to long-term cardiotoxicity resulting in more extensive coronary atherosclerosis and calcification as well as myocardial fibrosis.23
Proarrhythmic Environment of Training and Competition
It appears that in some athletes, the adverse cardiac remodeling induced by EEE can create an arrhythmogenic substrate, some of which may increase the risk of dangerous ventricular arrhythmias and SCD.2, 8–10,18,24 At times, malignant ventricular arrhythmias can develop in competitive athletes, similar to that present in patients with familial arrhythmogenic RV dysplasia, possibly due to sustained volume overload of the right sided cardiac chambers for several hours. 25 This in combination with high levels of catecholamines may alter the arrhythmogenic potential in some patients. In addition, it has been reported that heavy endurance exercise, including EEE, increases the rate of atrial fibrillation by as much as five-fold, presumably due to similar mechanisms of periodic and sustained volume overloading of the left atrium resulting in fibrosis and electromechanical remodeling. 2, 26–29
Current Recommendations
Clearly, the United States and most of the Westernized World are currently plagued by lack of physical activity and exercise training. 23 Certainly, lack of physical activity and exercise training are much greater problems for our society than is the potential adverse effects of excessive endurance exercise. We must recognize that most participants in excessive endurance exercise, including marathon runners, are not doing this activity for health reasons alone, but are driven by the thrill of competition, fellowship, and the attainment of personal goals. In a similar vein, people jump from planes and mountains, race cars and boats, and participate in many other sports or recreational activities, without the primary purpose being health improvement. We should stress that the benefits of PA and ET seem to occur and be maximized after the first 40–60 minutes, 2, 8–10,23 and more prolonged ET, such as EEE in marathon runners and triathletes, improves athletic performance and burns calories, but does not typically promote additional health benefits and as we have pointed out, may cause harm including greater risk of CAD as reported by Schwartz and colleagues, 4 and cardiac fibrosis and SCD as published by others. 2, 8–10 Simply stated, the platform of “more is better” for aerobic exercise training recommendations is not supportable at this time.
Future research will need to take this work a step further to really understand the relative stability or instability of atherosclerosis among various patient populations. It is possible that the original chain of logic is still somewhat intact; that is, marathoners may have relative freedom from myocardial infarct, not because they are free of atherosclerosis, but because atherosclerosis that forms in those who exercise regularly is in some way “protected” against instability and MI. In addition to better phenotypic characterization, the future holds the promise for genetic susceptibility testing to understand individual profiles that are very favorable towards endurance training and those that potentially indicate harm to both the coronaries and the myocardium with this form of exercise and competition.30 To summate present knowledge in early 2014, studies support a potential increased risk of coronary artery disease, myocardial fibrosis, and sudden cardiac death in marathoners. 2,5, 8–10,31–33
Biography
Peter A. McCullough, MD, MPH, (left) is at the Baylor University Medical Center, Baylor Heart and Vascular Institute, Baylor Jack and Jane Hamilton Heart and Vascular Hospital, Dallas, TX, The Heart Hospital, Plano, Texas. Carl J. Lavie, MD, (right) is Professor of Medicine, Department of Cardiovascular Diseases, John Ochsner Heart and Vascular Institute, Ochsner Clinical School-The University of Queensland School of Medicine & The Department of Preventive Cardiology, Pennington Biomedical Research Center, Louisiana State University System, Baton Rouge, Louisiana.
Contact: peteramccullough@gmail.com

Footnotes
Disclosures
None reported.
References
- 1.Haskell Wl, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1423–34. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 2.O’Keefe JH, Patil HR, Lavie CJ, Magalski A, Vogel RA, McCullough PA. Potential adverse cardiovascular effects from excessive endurance exercise. Mayo Clin Proc. 2012;87(6):587–95. doi: 10.1016/j.mayocp.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Menezes AR, Lavie CJ, Milani RV, Forman DE, King M, Williams MA. Cardiac rehabilitation in the United States. Prog Cardiovasc Dis. 2013 doi: 10.1016/j.pcad.2013.09.018. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz RS, Kraus SM, Schwartz JG, et al. Increased coronary artery plaque volume among male marathon runners. Mo Med. 2014 Mar-Apr; in press. [PMC free article] [PubMed] [Google Scholar]
- 5.Noakes TD. Heart disease in marathon runners: a review. Med Sci Sports Exerc. 1987;19(3):187–94. [PubMed] [Google Scholar]
- 6.Lloyd-Jones DM, Wilson PW, Larson MG, Beiser A, Leip EP, D’Agostino RB, Levy D. Framingham risk score and prediction of lifetime risk for coronary heart disease. Am J Cardiol. 2004;94(1):20–24. doi: 10.1016/j.amjcard.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 7.Yamamoto H, Kitagawa T, Ohashi N, Utsunomiya H, Kunita E, Oka T, Urabe Y, Tsushima H, Awai K, Kihara Y. Noncalcified atherosclerotic lesions with vulnerable characteristics detected by coronary CT angiography and future coronary events. J Cardiovasc Comput Tomogr. 2013;7(3):192–199. doi: 10.1016/j.jcct.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 8.O’Keefe JH, Lavie CJ. Run for your life … at a comfortable speed and not too far. Heart. 2013;99(8):516–519. doi: 10.1136/heartjnl-2012-302886. [DOI] [PubMed] [Google Scholar]
- 9.O’Keefe JH, Schnohr P, Lavie CJ. The dose of running that best confers longevity. Heart. 2013;99(8):588–590. doi: 10.1136/heartjnl-2013-303683. [DOI] [PubMed] [Google Scholar]
- 10.Patil HR, O’Keefe JH, Lavie CJ, Magalski A, Vogel RA, McCullough PA. Cardiovascular damage resulting from chronic excessive endurance exercise. Mo Med. 2012;109(4):312–321. [PMC free article] [PubMed] [Google Scholar]
- 11.Kim JH, Malhotra R, Chiampas G, et al. Cardiac arrest during long-distance running races. NEJM. 2012;366(2):130–140. doi: 10.1056/NEJMoa1106468. [DOI] [PubMed] [Google Scholar]
- 12.Roberts WO, Roberts DM, Lunos S. Marathon related cardiac arrest risk differences in men and women. Br J Sports Med. 2013;47(3):168–71. doi: 10.1136/bjsports-2012-091119. [DOI] [PubMed] [Google Scholar]
- 13.Redelmeier DA, Greenwald JA. Competing risks of mortality with marathons: retrospective analysis. BMJ. 2007;335(7633):1275–1277. doi: 10.1136/bmj.39384.551539.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris KM, Henry JT, Rohman E, Haas TS, Maron BJ. Sudden death during the triathlon. JAMA. 2010;303(13):1255–125. doi: 10.1001/jama.2010.368. [DOI] [PubMed] [Google Scholar]
- 15.Praphatsorna P, Thong-Ngama D, Kulaputanaa O, Klaikaewb N. Effects of intense exercise on biochemical and histological changes in rat liver and pancreas. Asian Biomedicine. 2010;4(4):619–625. [Google Scholar]
- 16.Benito B, Gay-Jordi G, Serrano-Mollar A, et al. Cardiac arrhythmogenic remodeling in a rat model of long-term intensive exercise training. Circulation. 2011;123(1):13–22. doi: 10.1161/CIRCULATIONAHA.110.938282. [DOI] [PubMed] [Google Scholar]
- 17.Trivax JE, Franklin BA, Goldstein JA, et al. Acute cardiac effects of marathon running. J Applied Physiolog. 2010;108(5):1148–1153. doi: 10.1152/japplphysiol.01151.2009. [DOI] [PubMed] [Google Scholar]
- 18.La Gerche A, Burns AT, Mooney DJ, Inder WJ, Taylor AJ, Bogaert J, Macisaac AI, Heidbuchel H, Prior DL. Exercise-induced right ventricular dysfunction and structural remodelling in endurance athletes. European heart journal. 2012;33:998–1006. doi: 10.1093/eurheartj/ehr397. [DOI] [PubMed] [Google Scholar]
- 19.Scherr J, Braun S, Schuster T, et al. 72-h kinetics of high-sensitive troponin T and inflammatory markers after marathon. Med Science Sports Exercise. 2011;43(10):1819–1827. doi: 10.1249/MSS.0b013e31821b12eb. [DOI] [PubMed] [Google Scholar]
- 20.Neumayr G, Gaenzer H, Pfister R, et al. Plasma levels of cardiac troponin I after prolonged strenuous endurance exercise. Am J Cardio. 2001;87(3):369–371. A310. doi: 10.1016/s0002-9149(00)01382-5. [DOI] [PubMed] [Google Scholar]
- 21.Shave R, Baggish A, George K, et al. Exercise-induced cardiac troponin elevation: evidence, mechanisms, and implications. J Am Coll Cardiol. 2010;56(3):169–176. doi: 10.1016/j.jacc.2010.03.037. [DOI] [PubMed] [Google Scholar]
- 22.Neilan TG, Januzzi JL, Lee-Lewandrowski E, et al. Myocardial injury and ventricular dysfunction related to training levels among nonelite participants in the Boston marathon. Circulation. 2006;114(22):2325–2333. doi: 10.1161/CIRCULATIONAHA.106.647461. [DOI] [PubMed] [Google Scholar]
- 23.Lavie CJ. Cardiosource World News. Feb, 2014. Exercise and Cardiovascular Disease – Can too much of a good thing become toxic? in press. [Google Scholar]
- 24.La Gerche A, Robberecht C, Kuiperi C, et al. Lower than expected desmosomal gene mutation prevalence in endurance athletes with complex ventricular arrhythmias of right ventricular origin. Heart. 2010;96(16):1268–1274. doi: 10.1136/hrt.2009.189621. [DOI] [PubMed] [Google Scholar]
- 25.Heidbuchel H, Hoogsteen J, Fagard R, et al. High prevalence of right ventricular involvement in endurance athletes with ventricular arrhythmias. Role of an electrophysiologic study in risk stratification. Eur Heart J. 2003;24(16):1473–1480. doi: 10.1016/s0195-668x(03)00282-3. [DOI] [PubMed] [Google Scholar]
- 26.Mont L, Elosua R, Brugada J. Endurance sport practice as a risk factor for atrial fibrillation and atrial flutter. Europace : European pacing, arrhythmias, and cardiac electrophysiology : journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the Europ Soc Cardio. 2009;11(1):11–17. doi: 10.1093/europace/eun289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aizer A, Gaziano JM, Cook NR, Manson JE, Buring JE, Albert CM. Relation of vigorous exercise to risk of atrial fibrillation. Amer J Cardio. 2009;103(11):1572–1577. doi: 10.1016/j.amjcard.2009.01.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Menezes AR, Lavie CJ, DiNicolantonio JJ, et al. Atrial fibrillation in the 21st century: a current understanding of risk factors and primary prevention strategies. Mayo Clin Proc. 2013;88(4):394–409. doi: 10.1016/j.mayocp.2013.01.022. [DOI] [PubMed] [Google Scholar]
- 29.Menezes AR, Lavie CJ, DiNicolantonio JJ, et al. Cardiometabolic risk factors and atrial fibrillation. Rev Cardiovasc Med. 2013;14(2–4):e73–e81. doi: 10.3909/ricm0693. [DOI] [PubMed] [Google Scholar]
- 30.Wilson GD, Geddes TJ, Pruetz BL, Thibodeau BJ, Murawka A, Colar JM, McCullough PA, Trivax JE. SELDI-TOF-MS Serum Profiling Reveals Predictors of Cardiac MRI Changes in Marathon Runners. Int J Proteomics. 2012;2012:679301. doi: 10.1155/2012/679301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Möhlenkamp S, Lehmann N, Breuckmann F, et al. Running: the risk of coronary events: prevalence and prognostic relevance of coronary atherosclerosis in marathon runners. Eur Heart J. 2008;29(15):1903–1910. doi: 10.1093/eurheartj/ehn163. [DOI] [PubMed] [Google Scholar]
- 32.Möhlenkamp S, Böse D, Mahabadi AA, Heusch G, Erbel R. On the paradox of exercise: coronary atherosclerosis in an apparently healthy marathon runner. Nat Clin Pract Cardiovasc Med. 2007;4(7):396–401. doi: 10.1038/ncpcardio0926. [DOI] [PubMed] [Google Scholar]
- 33.Plicht B, Erbel R, Möhlenkamp S. Is there a preventive value in non-invasive cardiac imaging? Debate on the case of a marathon runner. Dtsch Med Wochenschr. 2009;134(40):e1–e5. doi: 10.1055/s-0029-1237553. [DOI] [PubMed] [Google Scholar]