Abstract
Coronary artery disease is a major cause of morbidity and mortality in patients with diabetes mellitus and remains one of the largest burdens on health care resources. Prevalence of asymptomatic CAD in this population is high and poses a diagnostic challenge due to lack of overt clinical complaints. At this time there is no clear algorithm to screen for silent myocardial ischemia in diabetics. In this article we review various diagnostic tools available for assessment and propose a step wise approach for risk stratification in these patients.
Introduction
Currently, almost 11 percent (>25 million) of the adults in the United States have diabetes and 90–95 percent represents type II Diabetes (DMII).1 The epidemic of diabetes is on an exponential rise as by the year 2030, 4.4 percent (366 million) of the world is projected to have diabetes from an estimated 2.8 percent (171 million) in 2000.2 Coronary artery disease (CAD) is a major cause of morbidity and mortality and the biggest contributor to direct and indirect costs of diabetes.3 Individuals with DMII have increased risk, faster progression and greater extent of CAD compared to non-diabetics.4 Diabetes is considered a CAD risk equivalent, as the risk of myocardial infarction (MI) in a diabetic patient without prior history of MI is similar to the risk of re-infarction in a non-diabetic individual with a previous infarction.5, 6 This confers a greater than 20 percent risk per 10 years for major coronary events, which is considered the highest risk category 5. The age of transition to high-risk category in DMII occurred approximately 15 years earlier for both men (at age 41) and women (at age 38) compared to non-diabetics.7 Individuals with diabetes also have higher incidence of multi-vessel CAD (66 versus 46 percent) and a greater number of diseased vessels compared to non-diabetics.8
Cardiovascular death is the most common cause of death in diabetes and outcomes of coronary artery disease are worst in diabetics. The Multiple Risk Factor Intervention Trial (MRFIT) showed that over 12 years, cardiovascular disease caused 9.7 percent of the deaths in diabetic men compared to 2.6 percent in non-diabetic men and this difference was independent of age, ethnic group, cholesterol level, systolic blood pressure, and smoking history.9 Post-myocardial infarction, diabetes patients have twofold increase in 30-day and five-year mortality.10, 11 In addition to the increased cardiovascular risk, one of the biggest concerns in diabetic patients is the high prevalence of asymptomatic CAD.
Prevalence of Asymptomatic CAD in Diabetes
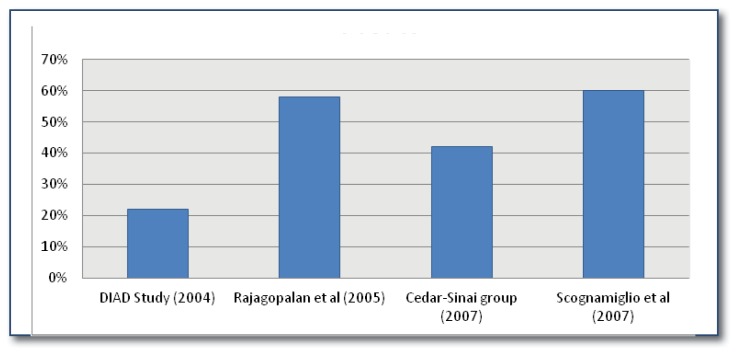
An important aspect of cardiovascular disease in diabetes is the prevalence of asymptomatic CAD. Diabetics have increased incidence of silent ischemia and myocardial infarction that has been attributed to prolonged anginal perception threshold due to autonomic neuropathy involving sympathetic fibers innervating the heart. 12, 13, 14 Figure 1 illustrates the rates of asymptomatic CAD detected in several studies summarized here. In the Framingham Heart Study, diabetic men had almost twice the rate of clinically unrecognized infarctions compared to non-diabetic men (39 percent versus 18 percent).15 In the Detection of Silent Myocardial Ischemia in Asymptomatic Diabetics (DIAD) study, 22% of the asymptomatic patients with type II diabetes had evidence of ischemia on stress myocardial perfusion imaging.13 Another study reported 58% of asymptomatic diabetics had an abnormal positive stress single-photon emission computed tomography (SPECT) scan.16 The Cedar-Sinai group reported in 42% abnormal SPECT scan with no differences between patients with angina and asymptomatic disease.17 In a retrospective observational study by Scognamiglio et al., 60% of asymptomatic diabetic patients had an abnormal myocardial contrast echocardiography (MCE) and follow up coronary angiography was abnormal in 65 percent of the patients with an abnormal MCE.18 It is important to note that the difference in the prevalence of asymptomatic CAD in these studies can be attributed to selection bias in study design and the fact that retrospective studies showed higher prevalence than prospective studies. Even with the wide range in prevalence of asymptomatic coronary artery disease (20–60%), we can deduce that asymptomatic CAD has a high prevalence in individuals with DMII. These observations support the argument for screening for asymptomatic CAD in diabetic patients. In the remainder of this paper we will review the current data and guidelines on screening for CAD in diabetic patients.
Figure 1.
Rate of Asymptomatic CAD in Diabetics
Studies on Screening for Asymptomatic CAD in Diabetics
The DIAD study was a prospective, randomized, multicenter trial investigating the screening of CAD in asymptomatic diabetics.13 In this study, 22% had myocardial perfusion defects with 6% of cohorts comprising moderate or large perfusion defects. This study also showed that the conventional risk factor screening approach recommended by the ADA did not predict an abnormal MPI.
The second part of the DIAD study showed that myocardial ischemia may reverse over time. In 56 (79%) of the 71 individuals (out of 358) with initial MPI abnormalities had resolution of ischemia at three-year follow-up and 10% of the individuals with normal initial MPI had abnormal MPI.19 These changes were attributed to intensive risk factor reduction with increased use of ACE inhibitors, statins and aspirin in the group that demonstrated resolution of ischemia.
The third part of the study looked at effect of screening on cardiac event rates.20 The overall cardiac event rate was 2.9 % at five years and did not differ significantly between the screened versus non-screened groups. The presence of perfusion defects predicted outcomes as individuals with moderate or large defects had 2.4% per year adverse event rate compared to 0.4% per year in the normal to mildly abnormal MPI. Even though there was no difference in clinical outcomes in the screened versus non-screened individuals, it is important to realize that this was a low risk group of patients.
Another prospective study used coronary artery calcium (CAC) score and SPECT MPI to determine the rate of silent ischemia in DMII.21 It concluded that coronary calcium score was a better predictor of silent ischemia and short-term cardiovascular events than established cardiovascular risk factors. In addition, CAC and MPI can be used synergistically to predict adverse cardiovascular events but the effect on clinical outcome of patients is unknown.
These two studies do not make a strong argument for screening asymptomatic diabetics for CAD due to failure to show improved outcomes from screening for silent ischemia. However, it is important to note that the patients in the DIAD study were at a low risk for cardiovascular events and the sample size was relatively small.
Various Screening Modalities
As noted earlier, individuals with diabetes are at increased risk of asymptomatic CAD and CAD is the leading cause of morbidity and mortality. With the incidence of diabetes rising at an epidemic proportions, it is important to risk stratify individuals to better manage cardiovascular outcomes. In the following sections we review the various modalities available to screen for CAD.
Exercise Electrocardiography
Exercise Electrocardiography (ECG) stress test offers good prognostic value. Poor prognosticators include poor exercise ability (<5 METS), exercise induce angina, low peak BP, fall in BP during exercise, chronotropic incompetence and ventricular arrhythmias.22 Patients might not be able to satisfactorily perform a standard treadmill test due to reduced exercise capacity or presence of peripheral artery disease. ECG abnormalities might occur late in the ischemic cascade leading to lower accuracy of exercise ECG. ECG stress testing has 50% sensitivity and 80% specificity and it may be considered for CV risk assessment in intermediate-risk asymptomatic adults.23
Myocardial Contrast Echocardiography
Several studies have shown prevalence of ischemia using myocardial contrast echocardiography (MCE) in diabetic individuals.18, 24 Sixty percent of asymptomatic diabetic patients had abnormal MCE that was irrespective of the number of risk factors and 65 % of them had CAD on angiography.18 This study showed that significant CAD existed in asymptomatic diabetics that were independent of the risk factor profile. Patients with two or more risk factors had higher rate of three-vessel disease, diffuse disease and vessel occlusion indicating more severe disease.18 MCE has an overall sensitivity and specificity of 89% and 52% respectively for detection of CAD in diabetic patients. 24
Coronary Artery Calcium Score
Coronary Artery Calcium (CAC) score can be measured via Electron-Beam Computed Tomography (EBCT) and Multi-Slice Computed Tomography (MSCT) as noninvasive quantification of coronary atherosclerosis burden to identify asymptomatic patients at high risk for CAD. Several studies have shown that CAC measurement can be used a predictor of cardiovascular events in asymptomatic diabetic patients and can extend beyond conventional risk factors.21, 25, 26, 27 In 10,377 individuals (903 diabetic patients), Raggi et al., concluded that diabetics had a higher CAC and mortality (3.5% versus 2.0%) compared to non-diabetics over a five year follow-up.25 Mortality increased in proportion to screening CAC in asymptomatic diabetic patients. Interestingly, with a CAC of zero, the survival rates for diabetics and non-diabetics were similar.
In a study by Anand et al., one-third of the patients had a coronary calcium score of >400 and 28 percent of those had inducible ischemia.21 The Diabetes Heart Study showed that CAC was an independent predictor of mortality with the risk of mortality increasing with increased level of CAC.26
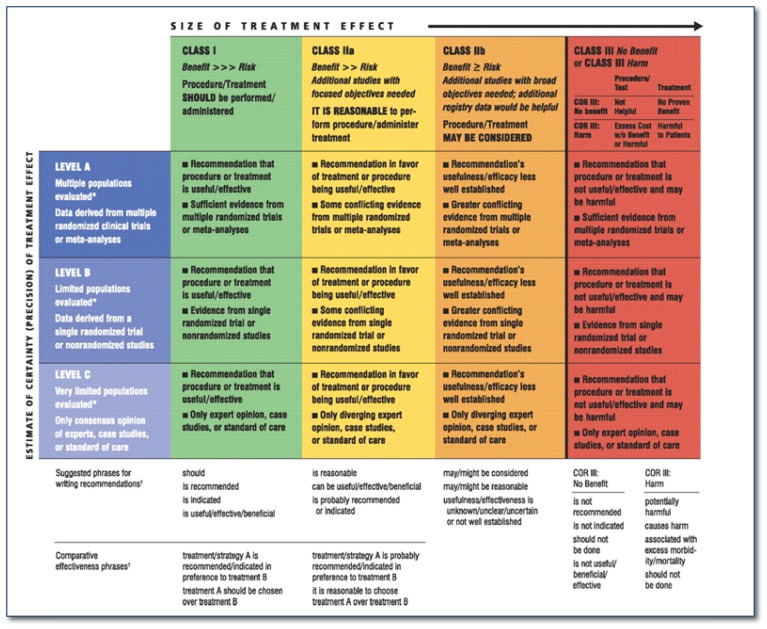
CAC score can be used as an initial screening test in high-risk individuals at risk for inducible ischemia, but is less predictive in patients with renal insufficiency and the elderly even though they have high prevalence of coronary calcification, limiting the diagnostic value.28 To optimize screening of asymptomatic diabetic patients, those with CAC score >400 should be further evaluated using other imaging modality to assess myocardial perfusion or wall motion abnormalities.28 According to the ACCF/AHA guidelines for assessment of cardiovascular risk in asymptomatic adults, CAC score measurement can be used for cardiovascular risk assessment in asymptomatic diabetics >40 years of age (class IIa, level of evidence B. Check Figure 2 for details on the classification).23
Figure 2.
ACCF/AHA Applying Classification of Recommendations and Level of Evidence 22
Myocardial Perfusion Imaging
Myocardial Perfusion Imaging (MPI) defects as a marker for CAD can be analyzed via single-photon emission computed tomography (SPECT) and Positron Emission Tomography (PET) scan. Stress SPECT has been shown to be useful in detection of asymptomatic CAD in DMII patients. Studies have reported22, 33, 42 and 58 percent abnormal SPECT rates in asymptomatic diabetics.13, 29, 16, 17 In addition, several studies have confirmed that stress SPECT provides incremental prognostic value to achieve adequate risk stratification in diabetics.30, 31, 32 SPECT has similar sensitivity and specificity in diabetic and non-diabetic individuals. Kang et al., reported a sensitivity and specificity of 86 and 56 percent in 138 diabetic patients, which is similar in non-diabetics.33
More recently, the J-ACCESS 2 investigation evaluated the prognostic value of gated myocardial perfusion imaging on asymptomatic Japanese DMII patients.34 The study showed that patients with summed stress scores greater or equal to 9 had 1.9-fold increase in rates of cardiovascular events or death, hence abnormal MPI may have high prognostic value to predict increased risk of CV disease in asymptomatic diabetic patients.
One prospective randomized trial (DIAD study) has concluded that initial screening with stress MPI did not affect the five-year outcomes in screened versus non-screened asymptomatic diabetic patients as mentioned earlier. 20
Although stress SPECT scan has been shown to have prognostic value it does have some drawbacks. One of the concerns is that the extent and severity of perfusion abnormalities exceeds that predicted by coronary angiography in diabetic patients. For example, in the study by Rajagopalan et al., 40% of the patients with high-risk MPI had mild angiographic CAD.16 Normal stress SPECT is associated with higher risk in diabetic compared to nondiabetics.17, 31, 35 SPECT and PET scans expose patients to ionizing radiation and should only be used in those whom the benefits outweigh the risks. One way to enhance the yield of stress SPECT in asymptomatic DMII patients is to combine it with CAC score. As mentioned earlier, Anand, used coronary artery calcium (CAC) score and SPECT MPI to determine the rate of silent ischemia in DMII. Myocardial ischemia was detected on SPECT MPI in 48 and 71.4 percent of diabetic patients with CAC >400 and >1000 respectively.21 They concluded that CAC and MPI can be used synergistically to predict adverse cardiovascular events but the effect on clinical outcome of patients is unknown. It is also important to consider that diabetics have a faster progression of atherosclerosis as cardiac events can occur two years after a normal stress MPI.35 According to the ACCF/AHA guidelines for assessment of cardiovascular risk in asymptomatic adults, stress MPI may be considered for CV risk assessment in asymptomatic diabetics and those with CAC >400 (Level of evidence: C).23
Coronary Computed Tomography Angiography
Coronary Computed Tomography Angiography (CCTA) provides a morphologic examination of the coronary arteries. CCTA has sensitivity and specificity of 85–95% and a negative predictive value of >98%.23,36 A study of 140 asymptomatic diabetic patients who underwent CCTA concluded that the prevalence of CAD is higher in DMII patients compared to nondiabetics resulting in three-fold higher rate of cardiac events (1.8% versus 0.5 percent per year) and that CCTA can provide predictive value in addition to traditional risk factors in diabetics.36 Choi, et al. concluded that a significant number of diabetics with normal ECG, SPECT and no peripheral artery disease had evidence of occult CAD on CCTA.37 The drawbacks of CCTA include the risk of contrast nephropathy, radiation exposure, lack of information concerning ischemia and sub-optimal view of vessel distal bed. CCTA is not recommended to assess need for revascularization as MPI provides better functional assessment compared to CCTA. Current ACCF/AHA guidelines do not recommend CCTA for CV risk assessment in asymptomatic adults (Class III, Level of evidence: C).23
Magnetic Resonance Imaging
Magnetic Resonance Imaging (MRI) can be used as a non-invasive coronary angiogram and can also provide functional (myocardial perfusion) and anatomical (ventricular function, wall motion) information without radiation exposure. MRI is less accurate than CT for diagnosing coronary stenosis especially in vessel distal bed analysis. In a prospective trial of 752 patients cardiovascular magnetic resonance imaging (CMR) was superior to SPECT in detection of clinically significant CAD with higher sensitivity (86.5 versus 66.5 percent), specificity (83.4 versus 82.6 percent) and positive (77.2 versus 71.4 percent) and negative predictive values (90.5 versus 79.1 percent).38 MRI has the potential to provide information on atherosclerosis plaque vulnerability to identify individuals at high risk for acute coronary syndrome.39 Coupling of non-invasive imaging of coronary arteries with pharmacological stress test to assess the intensity and location of ischemia could make MRI the gold standard for CAD detection. Although the above study showed positive results for the use of MRI, further studies are needed in asymptomatic individuals, especially diabetics. Current ACCF/AHA guidelines do not recommend use of MRI for risk assessment in asymptomatic adults (Class III, Level of evidence: C).23
Should We Screen Asymptomatic Patients?
Studies have shown the prevalence of asymptomatic CAD to be 20–60% in diabetics providing a rationale for screening this population. Before screening can be recommended, certain criteria should be met: the prevalence of CAD in the population should be high, screening test should accurately differentiate between low and high risk patient, identification of individuals with disease should lead to treatment with better outcomes and the screening strategy must be cost-effective.40 There is lack of evidence of improved outcomes in asymptomatic diabetic patients to supports screening for silent ischemia at this time.
Current Recommendations & Guidelines on CAD Screening
The 1998 ADA guidelines for diagnosis of coronary artery disease in patients with diabetes are shown in Table 1.41 Since the 1998 guidelines, several studies have shown that the risk stratification according to the number of risk factors has not been shown to be effective in asymptomatic diabetics.13,16,18 A recent post hoc analysis of the high-risk participants in DIAD study found that annual cardiac event rate was not altered by routine screening for silent ischemia. 42 With the currently available evidence, one must question the cost effectiveness of indiscriminant screening. It is unclear what the implications are beyond risk stratification. The American Diabetes Association does not recommend routine screening for CAD in diabetic patients, as it does not improve outcomes as long as the cardiovascular disease risk factors are treated. 3 In our opinion a stepwise screening with CAC score followed by SPECT, if necessary, is reasonable and may allow for optimal risk stratification of asymptomatic diabetics based on currently available data.
Table 1.
ADA Guidelines for diagnosis of CAD in Diabetic Patients
| Typical or atypical cardiac symptoms |
| Resting EKG suggestive of ischemia or infarction |
| Peripheral or carotid occlusive arterial disease |
| Sedentary lifestyle, age >35 years, and plans to begin a vigorous exercise program |
Two or more of the risk factors listed below (a–e) in addition to diabetes
|
Medical Interventions
Since diabetes is already established as a CAD risk equivalent, screening for CAD will not alter medical treatment as it already warrants optimal medical therapy. The ADA guidelines recommend cardiovascular risk assessment annually and treatment of these abnormal risk factors (risk factors include dyslipidemia, hypertension, smoking, coronary disease and presence of micro-or macro-albuminuria).3 Patients with known CAD should be treated with Angiotensin Converting Enzyme (ACE) inhibitor, aspirin and statin to decrease risk of cardiovascular events.
The Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial did not show a reduction in the risk of death, myocardial infarction, or other major cardiovascular events with PCI in addition to optimal medical therapy.43 Diabetics comprised 33 percent of the patients in this study but they had stable coronary artery disease.
The Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) study showed that compared to intensive medical therapy alone, prompt coronary revascularization in addition to intensive medical therapy did not reduce all-cause mortality or the composite of death, myocardial infarction or stroke.44 COURAGE and BARI 2D trials shown that optimal medical therapy is comparable to revascularization in diabetic patients diagnosed with stable CAD.
Conclusion
Coronary artery disease is a major cause of morbidity and mortality in patients with diabetes mellitus. The rate of asymptomatic CAD in this patient population is high. There is a lack of evidence to support screening for silent myocardial ischemia in diabetics and the ADA guidelines do not recommend screening for asymptomatic CAD. After reviewing the data, we feel that stepwise screening with CAC score followed by SPECT MPI if necessary is a reasonable option for risk stratification in diabetic patients. Future prospective trials are needed to provide better guidelines on this issue.
Biography
Paramdeep S. Baweja MD, Pratik B. Sandesara, and M. Javed Ashraf, MD, MPH, (above), MSMA member since 2014, are in the Department of Medicine, Cardiology Division at the Truman Medical Center, and the University of Missouri - Kansas City School of Medicine
Contact: mjaved_ashraf@yahoo.com
Footnotes
Disclosure
None reported.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 3.American Diabetes A. Standards of medical care in diabetes--2013. Diabetes Care. 2013;36(Suppl 1):S11–66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clark LT, Baweja P, Dim UR. McGraw-Hill Education, Cardiovascular Disease and Diabetes. Mar, 2007. Diabetes as a Coronary Risk Equivalent. [Google Scholar]
- 5.Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339:229–34. doi: 10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- 6.National Cholesterol Education Program Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 7.Booth GL, Kapral MK, Fung K, Tu JV. Relation between age and cardiovascular disease in men and women with diabetes compared with non-diabetic people: a population-based retrospective cohort study. Lancet. 2006;368:29–36. doi: 10.1016/S0140-6736(06)68967-8. [DOI] [PubMed] [Google Scholar]
- 8.Granger CB, Califf RM, Young S, et al. Outcome of patients with diabetes mellitus and acute myocardial infarction treated with thrombolytic agents. The Thrombolysis and Angioplasty in Myocardial Infarction (TAMI) Study Group. J Am Coll Cardiol. 1993;21:920–5. doi: 10.1016/0735-1097(93)90348-5. [DOI] [PubMed] [Google Scholar]
- 9.Stamler J, Vaccaro O, Neaton JD, Wentworth D. Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care. 1993;16:434–44. doi: 10.2337/diacare.16.2.434. [DOI] [PubMed] [Google Scholar]
- 10.Miettinen H, Lehto S, Salomaa V, et al. Impact of diabetes on mortality after the first myocardial infarction. The FINMONICA Myocardial Infarction Register Study Group. Diabetes Care. 1998;21:69–75. doi: 10.2337/diacare.21.1.69. [DOI] [PubMed] [Google Scholar]
- 11.Herlitz J, Karlson BW, Lindqvist J, Sjolin M. Rate and mode of death during five years of follow-up among patients with acute chest pain with and without a history of diabetes mellitus. Diabet Med. 1998;15:308–14. doi: 10.1002/(SICI)1096-9136(199804)15:4<308::AID-DIA579>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 12.Nesto RW, Phillips RT, Kett KG, et al. Angina and exertional myocardial ischemia in diabetic and nondiabetic patients: assessment by exercise thallium scintigraphy. Ann Intern Med. 1988;108:170–5. doi: 10.7326/0003-4819-108-2-170. [DOI] [PubMed] [Google Scholar]
- 13.Wackers FJ, Young LH, Inzucchi SE, et al. Detection of silent myocardial ischemia in asymptomatic diabetic subjects: the DIAD study. Diabetes Care. 2004;27:1954–61. doi: 10.2337/diacare.27.8.1954. [DOI] [PubMed] [Google Scholar]
- 14.Niakan E, Harati Y, Rolak LA, Comstock JP, Rokey R. Silent myocardial infarction and diabetic cardiovascular autonomic neuropathy. Arch Intern Med. 1986;146:2229–30. [PubMed] [Google Scholar]
- 15.Kannel WB. Lipids, diabetes, and coronary heart disease: insights from the Framingham Study. Am Heart J. 1985;110:1100–7. doi: 10.1016/0002-8703(85)90224-8. [DOI] [PubMed] [Google Scholar]
- 16.Rajagopalan N, Miller TD, Hodge DO, Frye RL, Gibbons RJ. Identifying high-risk asymptomatic diabetic patients who are candidates for screening stress single-photon emission computed tomography imaging. J Am Coll Cardiol. 2005;45:43–9. doi: 10.1016/j.jacc.2004.06.078. [DOI] [PubMed] [Google Scholar]
- 17.Zellweger MJ, Hachamovitch R, Kang X, et al. Prognostic relevance of symptoms versus objective evidence of coronary artery disease in diabetic patients. Eur Heart J. 2004;25:543–50. doi: 10.1016/j.ehj.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 18.Scognamiglio R, Negut C, Ramondo A, Tiengo A, Avogaro A. Detection of coronary artery disease in asymptomatic patients with type 2 diabetes mellitus. J Am Coll Cardiol. 2006;47:65–71. doi: 10.1016/j.jacc.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 19.Wackers FJ, Chyun DA, Young LH, et al. Resolution of asymptomatic myocardial ischemia in patients with type 2 diabetes in the Detection of Ischemia in Asymptomatic Diabetics (DIAD) study. Diabetes Care. 2007;30:2892–8. doi: 10.2337/dc07-1250. [DOI] [PubMed] [Google Scholar]
- 20.Young LH, Wackers FJ, Chyun DA, et al. Cardiac outcomes after screening for asymptomatic coronary artery disease in patients with type 2 diabetes: the DIAD study: a randomized controlled trial. JAMA. 2009;301:1547–55. doi: 10.1001/jama.2009.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anand DV, Lim E, Hopkins D, et al. Risk stratification in uncomplicated type 2 diabetes: prospective evaluation of the combined use of coronary artery calcium imaging and selective myocardial perfusion scintigraphy. Eur Heart J. 2006;27:713–21. doi: 10.1093/eurheartj/ehi808. [DOI] [PubMed] [Google Scholar]
- 22.Chopra S, Peter S. Screening for coronary artery disease in patients with type 2 diabetes mellitus: An evidence-based review. Indian J Endocrinol Metab. 2012;16:94–101. doi: 10.4103/2230-8210.91202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Greenland P, Alpert JS, Beller GA, et al. ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2010;2010;56:e50–103. doi: 10.1016/j.jacc.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 24.Elhendy A, Tsutsui JM, O’Leary EL, Xie F, McGrain AC, Porter TR. Noninvasive diagnosis of coronary artery disease in patients with diabetes by dobutamine stress real-time myocardial contrast perfusion imaging. Diabetes Care. 2005;28:1662–7. doi: 10.2337/diacare.28.7.1662. [DOI] [PubMed] [Google Scholar]
- 25.Raggi P, Shaw LJ, Berman DS, Callister TQ. Prognostic value of coronary artery calcium screening in subjects with and without diabetes. J Am Coll Cardiol. 2004;43:1663–9. doi: 10.1016/j.jacc.2003.09.068. [DOI] [PubMed] [Google Scholar]
- 26.Agarwal S, Morgan T, Herrington DM, et al. Coronary calcium score and prediction of all-cause mortality in diabetes: the diabetes heart study. Diabetes Care. 2011;34:1219–24. doi: 10.2337/dc11-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elkeles RS, Godsland IF, Feher MD, et al. Coronary calcium measurement improves prediction of cardiovascular events in asymptomatic patients with type 2 diabetes: the PREDICT study. Eur Heart J. 2008;29:2244–51. doi: 10.1093/eurheartj/ehn279. [DOI] [PubMed] [Google Scholar]
- 28.Bax JJ, Young LH, Frye RL, et al. Screening for coronary artery disease in patients with diabetes. Diabetes Care. 2007;30:2729–36. doi: 10.2337/dc07-9927. [DOI] [PubMed] [Google Scholar]
- 29.Scholte AJ, Schuijf JD, Kharagjitsingh AV, et al. Prevalence and predictors of an abnormal stress myocardial perfusion study in asymptomatic patients with type 2 diabetes mellitus. Eur J Nucl Med Mol Imaging. 2009;36:567–75. doi: 10.1007/s00259-008-0967-y. [DOI] [PubMed] [Google Scholar]
- 30.Berman DS, Kang X, Hayes SW, et al. Adenosine myocardial perfusion single-photon emission computed tomography in women compared with men. Impact of diabetes mellitus on incremental prognostic value and effect on patient management. J Am Coll Cardiol. 2003;41:1125–33. doi: 10.1016/s0735-1097(03)00085-8. [DOI] [PubMed] [Google Scholar]
- 31.Giri S, Shaw LJ, Murthy DR, et al. Impact of diabetes on the risk stratification using stress single-photon emission computed tomography myocardial perfusion imaging in patients with symptoms suggestive of coronary artery disease. Circulation. 2002;105:32–40. doi: 10.1161/hc5001.100528. [DOI] [PubMed] [Google Scholar]
- 32.Kang X, Berman DS, Lewin HC, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography in patients with diabetes mellitus. Am Heart J. 1999;138:1025–32. doi: 10.1016/s0002-8703(99)70066-9. [DOI] [PubMed] [Google Scholar]
- 33.Kang X, Berman DS, Lewin H, et al. Comparative ability of myocardial perfusion single-photon emission computed tomography to detect coronary artery disease in patients with and without diabetes mellitus. Am Heart J. 1999;137:949–57. doi: 10.1016/s0002-8703(99)70421-7. [DOI] [PubMed] [Google Scholar]
- 34.Yamasaki Y, Nakajima K, Kusuoka H, et al. Prognostic value of gated myocardial perfusion imaging for asymptomatic patients with type 2 diabetes: the J-ACCESS 2 investigation. Diabetes Care. 2010;33:2320–6. doi: 10.2337/dc09-2370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hachamovitch R, Hayes S, Friedman JD, et al. Determinants of risk and its temporal variation in patients with normal stress myocardial perfusion scans: what is the warranty period of a normal scan? J Am Coll Cardiol. 2003;41:1329–40. doi: 10.1016/s0735-1097(03)00125-6. [DOI] [PubMed] [Google Scholar]
- 36.Hadamitzky M, Hein F, Meyer T, et al. Prognostic value of coronary computed tomographic angiography in diabetic patients without known coronary artery disease. Diabetes Care. 2010;33:1358–63. doi: 10.2337/dc09-2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Choi EK, Chun EJ, Choi SI, et al. Assessment of subclinical coronary atherosclerosis in asymptomatic patients with type 2 diabetes mellitus with single photon emission computed tomography and coronary computed tomography angiography. Am J Cardiol. 2009;104:890–6. doi: 10.1016/j.amjcard.2009.05.026. [DOI] [PubMed] [Google Scholar]
- 38.Greenwood JP, Maredia N, Younger JF, et al. Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): a prospective trial. Lancet. 2012;379:453–60. doi: 10.1016/S0140-6736(11)61335-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Matter CM, Stuber M, Nahrendorf M. Imaging of the unstable plaque: how far have we got? Eur Heart J. 2009;30:2566–74. doi: 10.1093/eurheartj/ehp419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Miller TD, Redberg RF, Wackers FJ. Screening asymptomatic diabetic patients for coronary artery disease: why not? J Am Coll Cardiol. 2006;48:761–4. doi: 10.1016/j.jacc.2006.04.076. [DOI] [PubMed] [Google Scholar]
- 41.Consensus development conference on the diagnosis of coronary heart disease in people with diabetes: 10–11 February 1998, Miami, Florida. American Diabetes Association. Diabetes Care. 1998;21:1551–9. doi: 10.2337/diacare.21.9.1551. [DOI] [PubMed] [Google Scholar]
- 42.Bansal S, Wackers FJ, Inzucchi SE, et al. Five-year outcomes in high-risk participants in the Detection of Ischemia in Asymptomatic Diabetics (DIAD) study: a post hoc analysis. Diabetes Care. 2011;34:204–9. doi: 10.2337/dc10-1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Boden WE, O’Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:1503–16. doi: 10.1056/NEJMoa070829. [DOI] [PubMed] [Google Scholar]
- 44.Group BDS, Frye RL, August P, et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med. 2009;360:2503–15. doi: 10.1056/NEJMoa0805796. [DOI] [PMC free article] [PubMed] [Google Scholar]